Eating Disorders NICE update Dr Dominique Thompson GP




- Slides: 28
Eating Disorders: NICE update Dr Dominique Thompson GP& NICE ED Guideline Development Group 2015 -17
Why does it matter? Eating disorders are not about food, they are about CONTROL

725000 people in UK Up to 1: 4 are male Increasing numbers, and increasing admissions Context Poor quality of life, social isolation, impact on family/ carers/ friends 15% anorexia Remaining numbers are bulimia, binge eating disorder or OSFED (Other specified feeding & eating disorder) High mortality High co-morbidity rate (physical and psychological)

New classification DSM 5 Diagnosis/ types of ED Anorexia, Bulimia, BED, OSFED, Pica/Rumination Disorder, ARFID (Avoidant Restrictive Food Intake Disorder) As GP, don’t need to be 100% sure which type, need to know how urgently to refer!
Most common age of presentation; 13 -17, male and female, but ANY age possible Communication is key, with patient, and family/ carers Early intervention= better prognosis Identification/ presentation ‘Marathon not a sprint’ Do not rely solely on screening eg SCOFF Can present in many ways; gastro sx, psychological sx, ‘intolerances’, weight loss, amenorrhoea, delayed growth, puberty, pill ‘worries’, activities eg ballet If you don’t ask, you won’t find out (“I never see eating disorders”) Do not rely on single measures, eg BMI
Do you worry a lot about your weight? Maybe too much? You look quite slim. Does that worry you at all? But how do I bring it up? Do you spend a lot of time thinking about your weight and what you eat? Does your weight affect the way you feel about yourself? Have you lost control over what you eat/ do you eat in secret/ make yourself sick?
Physical measures eg malnutrition/ vomiting, BMI, ECG, DEXA Psychological history eg anxiety, mood, OCD, sleep Self harm, suicide risk Assessment ? Emergency referral Support from others Alcohol/ drug hx May need ongoing monitoring of bloods/ BMI in primary care
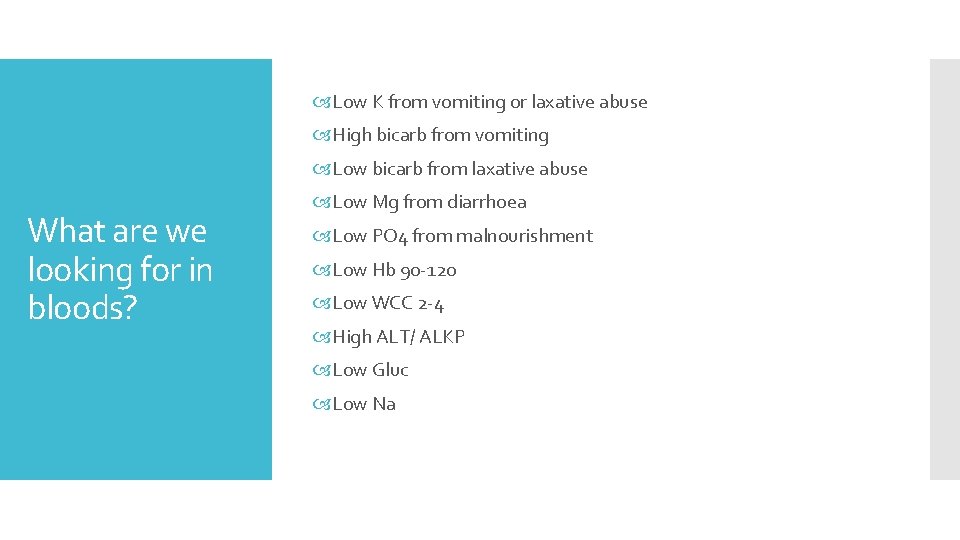
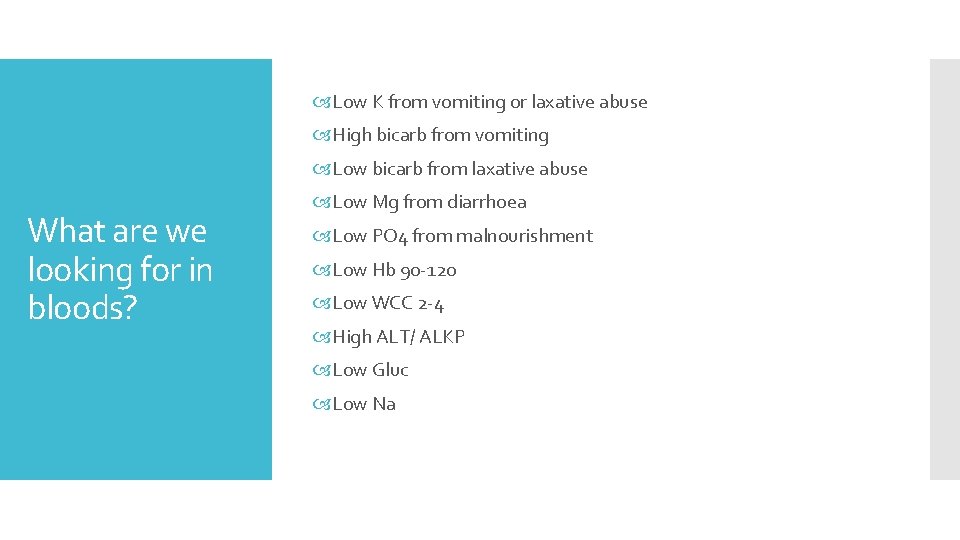
Low K from vomiting or laxative abuse High bicarb from vomiting Low bicarb from laxative abuse What are we looking for in bloods? Low Mg from diarrhoea Low PO 4 from malnourishment Low Hb 90 -120 Low WCC 2 -4 High ALT/ ALKP Low Gluc Low Na
If an eating disorder is suspected after an initial assessment, refer immediately to a community-based, age-appropriate eating disorder service for further assessment or treatment Referral. Quoted from NICE (useful for negotiating with colleagues) Provide acute medical care (including emergency admission) for people with an eating disorder who have severe electrolyte imbalance, severe malnutrition, severe dehydration or signs of incipient organ failure. Admit people with an eating disorder whose physical health is severely compromised to a medical inpatient or day patient service for medical stabilisation and to initiate refeeding, if these cannot be done in an outpatient setting. Do not use an absolute weight or BMI threshold when deciding whether to admit people with an eating disorder to day patient or inpatient care. Do not use inpatient care solely to provide psychological treatment for eating disorders Do not discharge people solely because they have reached a healthy weight. If a person's physical health is at serious risk due to their eating disorder, they do not consent to treatment, and they can only be treated safely in an inpatient setting, follow the legal framework for compulsory treatment in the Mental Health Act 1983
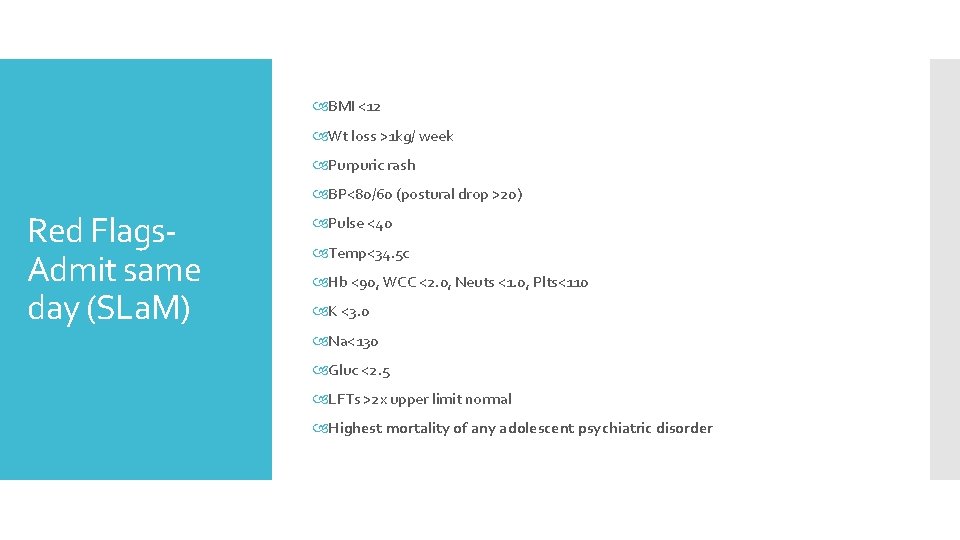
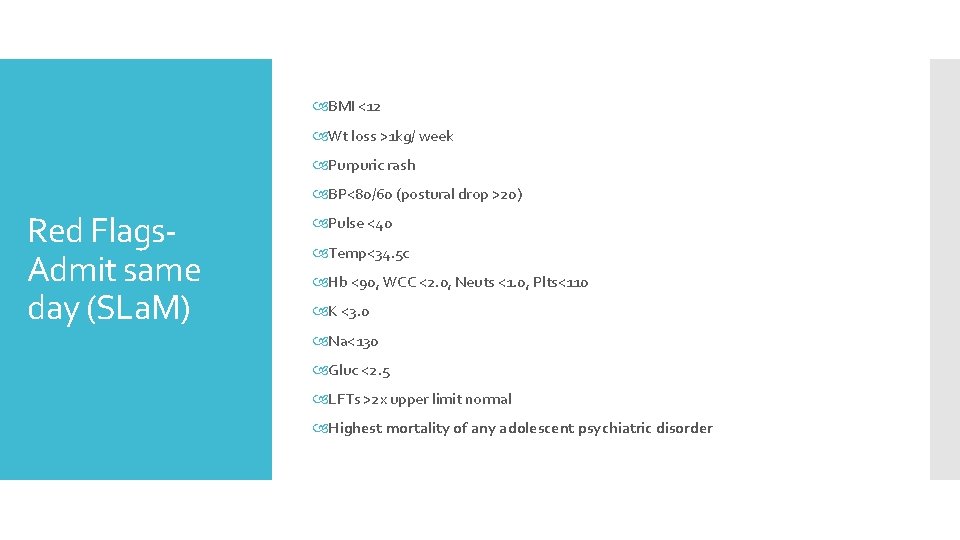
BMI <12 Wt loss >1 kg/ week Purpuric rash BP<80/60 (postural drop >20) Red Flags. Admit same day (SLa. M) Pulse <40 Temp<34. 5 c Hb <90, WCC <2. 0, Neuts <1. 0, Plts<110 K <3. 0 Na<130 Gluc <2. 5 LFTs >2 x upper limit normal Highest mortality of any adolescent psychiatric disorder
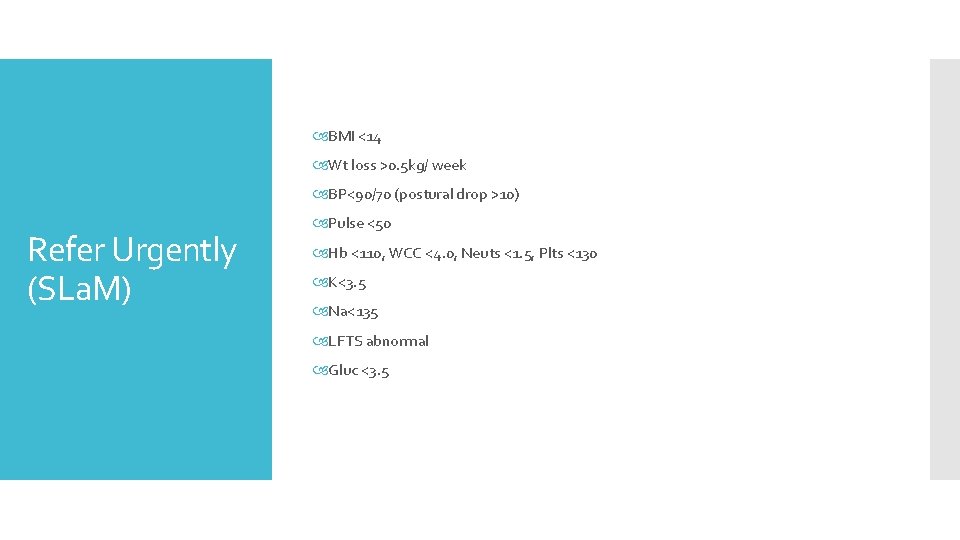
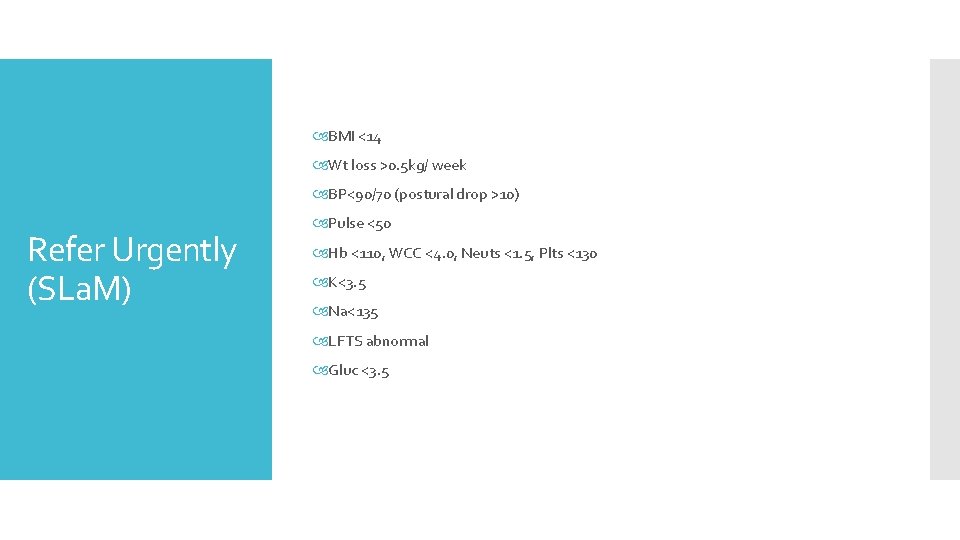
BMI <14 Wt loss >0. 5 kg/ week BP<90/70 (postural drop >10) Refer Urgently (SLa. M) Pulse <50 Hb <110, WCC <4. 0, Neuts <1. 5, Plts <130 K<3. 5 Na<135 LFTS abnormal Gluc <3. 5
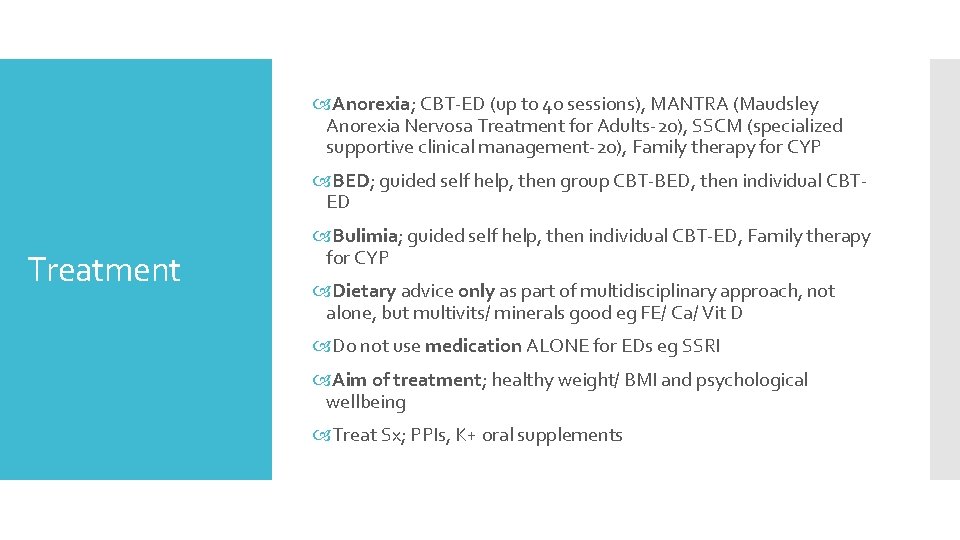
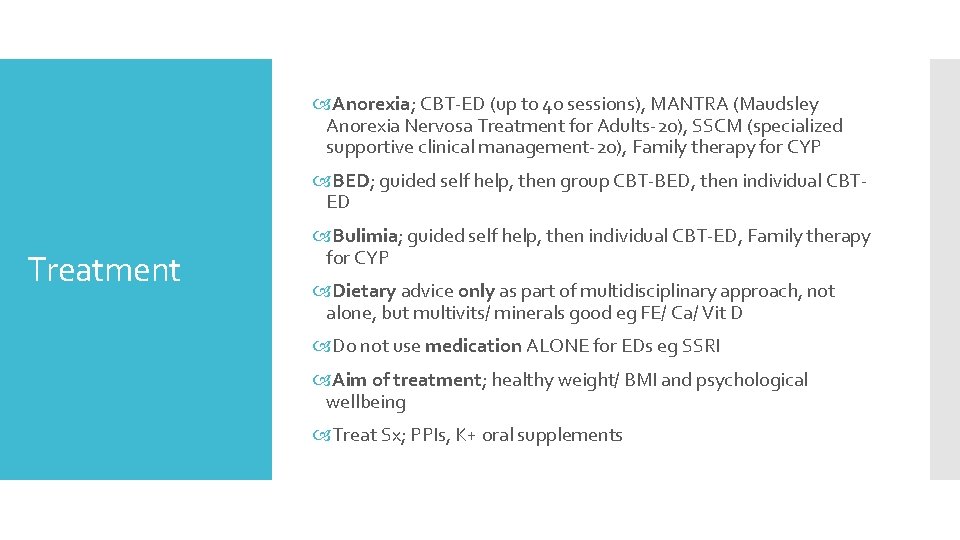
Anorexia; CBT-ED (up to 40 sessions), MANTRA (Maudsley Anorexia Nervosa Treatment for Adults-20), SSCM (specialized supportive clinical management-20), Family therapy for CYP BED; guided self help, then group CBT-BED, then individual CBTED Treatment Bulimia; guided self help, then individual CBT-ED, Family therapy for CYP Dietary advice only as part of multidisciplinary approach, not alone, but multivits/ minerals good eg FE/ Ca/ Vit D Do not use medication ALONE for EDs eg SSRI Aim of treatment; healthy weight/ BMI and psychological wellbeing Treat Sx; PPIs, K+ oral supplements
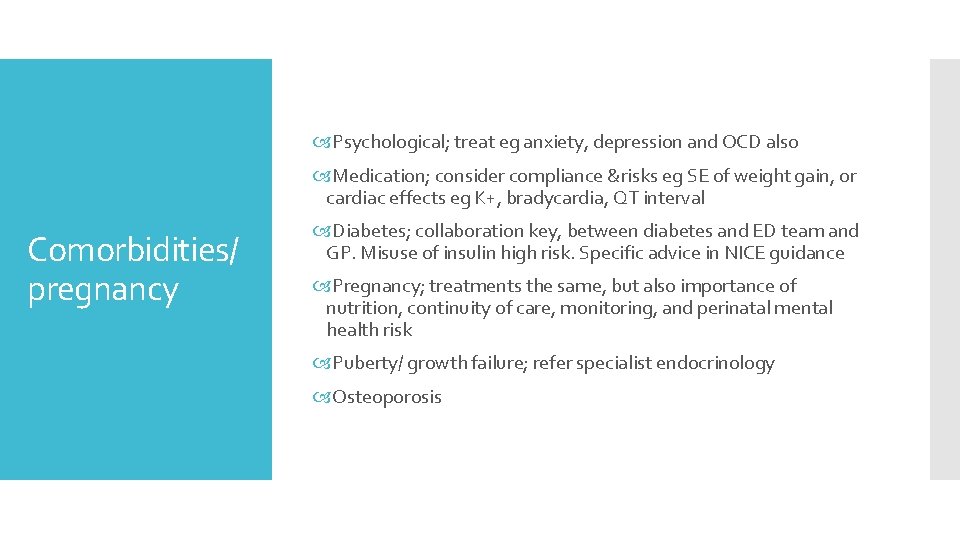
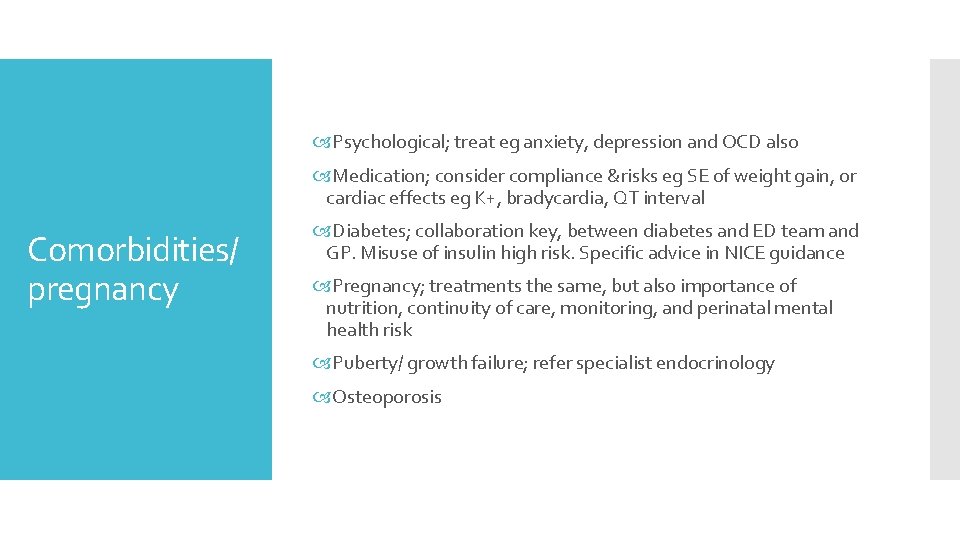
Psychological; treat eg anxiety, depression and OCD also Medication; consider compliance &risks eg SE of weight gain, or cardiac effects eg K+, bradycardia, QT interval Comorbidities/ pregnancy Diabetes; collaboration key, between diabetes and ED team and GP. Misuse of insulin high risk. Specific advice in NICE guidance Pregnancy; treatments the same, but also importance of nutrition, continuity of care, monitoring, and perinatal mental health risk Puberty/ growth failure; refer specialist endocrinology Osteoporosis
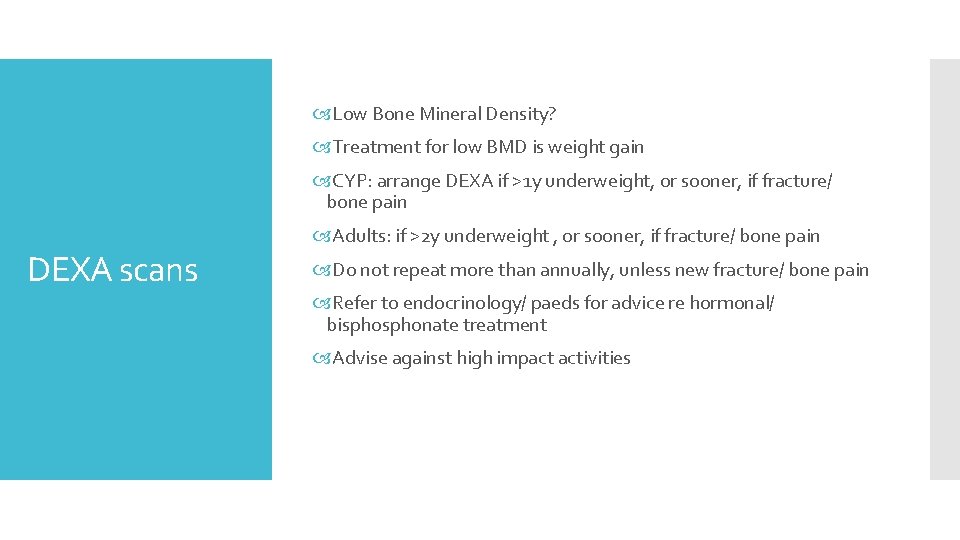
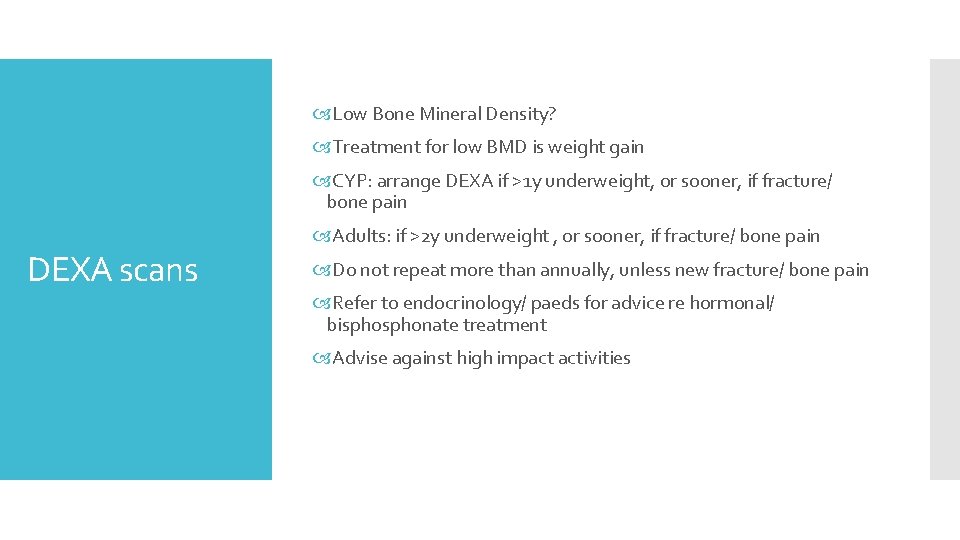
Low Bone Mineral Density? Treatment for low BMD is weight gain CYP: arrange DEXA if >1 y underweight, or sooner, if fracture/ bone pain DEXA scans Adults: if >2 y underweight , or sooner, if fracture/ bone pain Do not repeat more than annually, unless new fracture/ bone pain Refer to endocrinology/ paeds for advice re hormonal/ bisphonate treatment Advise against high impact activities
First assessment; BMI, P/BP, bloods (& ECG if wt loss+, brady, hypotensive, K+, purging, laxatives, muscle weakness) GPs should offer a physical and mental health review at least annually to people with anorexia nervosa who are not receiving ongoing treatment for their eating disorder. The review should include: weight or BMI (adjusted for age if appropriate) GP actions blood pressure relevant blood tests any problems with daily functioning assessment of risk (related to both physical and mental health) an ECG, for people with purging behaviours and/or significant weight changes a discussion of treatment options.
www. network-ed. org. uk NICE ‘Info for the Public’ on EDs Charities; ABC, B-eat, MEGEDT Books; “Lighter than my Shadow” by Katie Green “Seconds to Snap” by Tina Mc. Guff Further resources ESC Student App Article on EDs in Men RCGP e-learning module Dominique. thompson@me. com @Drdom. Thompson Twitter
Recovery

Dr Dominique Thompson GP& NICE ED Guideline Development Group 2015 -17

Eating disorders update – An Irish Perspective Dr Aoife O’Sullivan UCC Student Health April 2018
HSE National Clinical Programme for Eating Disorders https: //www. hse. ie/eng/about/who/cspd/ncps/mental-health/eating-disorders/ National Clinical Programme for Eating Disorders (NCP-ED) is a joint initiative between the HSE Clinical Strategy and Programmes Division and the Mental Health Division. An Eating Disorders Clinical Advisory Group from the College of Psychiatrists of Ireland also provides external clinical advice and support to the programme. This programme applies to HSE mental health services for children and adults with eating disorders in Ireland. Eating disorders include Anorexia Nervosa, Bulimia Nervosa, Binge Eating Disorders (BED), and other eating disorders. This NCP- ED applies to all clinical stages of eating disorders, from early recognition though treatment and into recovery. The programme does not encompass feeding disorders. The programme aims to work in integration with other HSE clinical programmes where collaborative solutions are needed to improve clinical service delivery for people with eating disorders e. g. paediatrics, primary care, acute medicine, palliative care, emergency medicine etc.
National Clinical Programme for eating disorders One of 5 mental health clinical programmes Develop a national model of care Collaborative practice/ pathways with other specialties Identify training needs evaluation Collaborative with patients Launched in January 2018 – 5 year plan!
What works? With evidence based treatment, remission can double to 45 -50% (Lock, 2015/16, RANZP, 2014) TAU in CAMHS is the most expensive in the long run and patients more dissatisfied (Gowers, 2006) Specialist psychiatric outpatient care is as effective as inpatient when medically stable (Gowers, 2006, RANZCP, 2014) ED Specialism needs lots of practice UK: 50 new cases/ year (NHS, 2015) Early intervention works Stepped levels of care
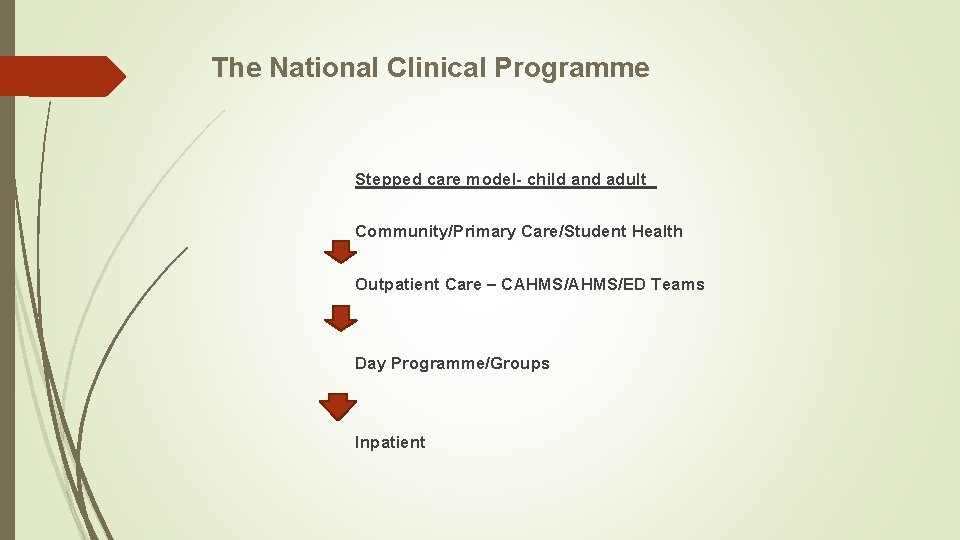
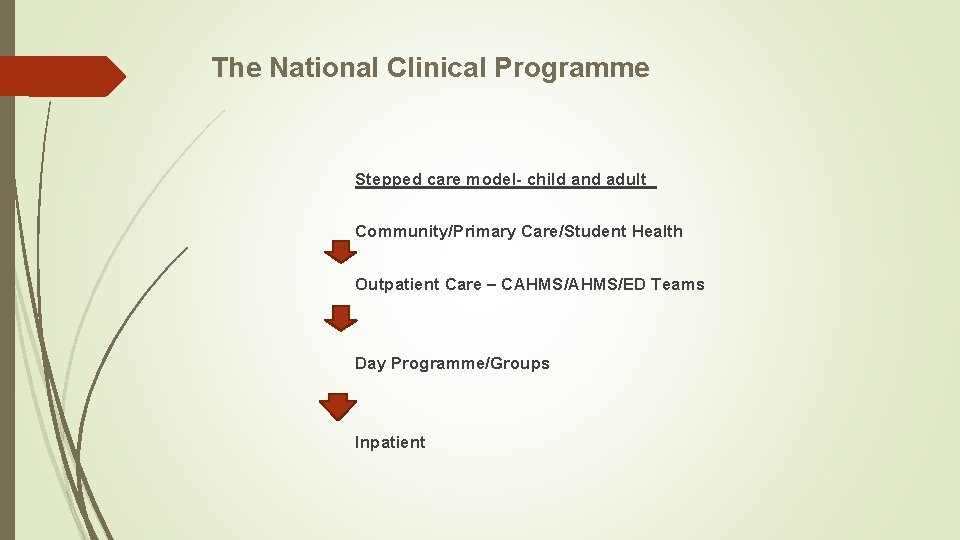
The National Clinical Programme Stepped care model- child and adult Community/Primary Care/Student Health Outpatient Care – CAHMS/ED Teams Day Programme/Groups Inpatient
Effective treatments • Evidence based treatment • Bodywhys as partner • Education and training • Integrated care pathways • Keyworker • Team coordinators
Primary Car/Student Health role Screening and Identifying ED patients Baseline History and Examination Early referral to ED Services (not yet existent) and follow up care Evidence shows that Early intensity of treatment improves outcomes The Treatment is Food and CBT-ED Medications rarely indicated unless co-morbidity
Marsipan Guidelines – Management of Really Sick Patients with Anorexia Nervosa Rapid exclusion of other conditions Risk assessment: BMI, SUSS test, Blood tests: full blood picture, urea and electrolytes, liver function tests, creatine kinase, glucose Refer if rapid weight loss or BMI<17. 5, urgently if BMI<15 If rapid re-feeding in the community, check electrolytes, phosphate and magnesium daily Monitor until appointment Consider referral to A&E if physical tests abnormal or deteriorating
Current Management If ED is suspected, open and complete the BMI screen and ED Care Screen. - Arrange the blood tests as above (usually make an appointment). -Arrange an ECG and DEXA scan if indicated. -Discuss the possible diagnosis and offer support and educational services e. g. Bodywhys, Bibliotherapy. -Discuss treatment options – Refeeding and Psychotherapy are the mainstay of treatment for most ED’s. -Encourage oral multi-vitamin (Centrum for men/women) and multi-mineral supplements (Thiamine = Vitamin B 1, 100 mg tds plus Sona B Complex tds x 1/12) until their diet improves. -Self Help Programmes can be used in Binge Eating Disorder (Bibliotherapy) -Fluoxetine can be used in Bulimia Nervosa but is not indicated in Anorexia Nervosa (unless comorbidities). -Consider Fitness to Study
Dr Aoife O’Sullivan UCC Student Health April 2018