MARSIPAN MAnagement of Really SIck Patients with Anorexia


- Slides: 47
MARSIPAN MAnagement of Really SIck Patients with Anorexia Nervosa Dr Matthew Cahill Consultant Psychiatrist in Eating Disorders CWP Eating Disorder Service
A Story……
SS n n 20 year old female Diagnosed with Ulcerative Colitis at age 8 Multiple hospital admissions and missed school Developed Anxiety Disorder and disordered eating
SS – ‘Disordered Eating’ n n n Overvaluation of bowel signals Petrified of diarrhoea and flare-ups Restricted eating Probable eliciting of care through sick role Overwhelming anxiety associated with eating and bowel habits Misuse of laxatives
SS – Early Years n n Multiple admissions to General and Mental Health Hospitals Episodes of severe low weight - mixture of inflammatory bowel disease, laxative abuse, and psychological difficulties Anxiety, OCD, panic attacks Under Gastroenterology Team at DGH – poor engagement
SS - 2018 n n May 2018 - Referred to Adult Eating Disorder Service Weight 35. 4 kg (BMI 11. 9) Scared of admission – affected engagement June 2018 – Admitted to Oaktrees EDU
Admission 1 June – August 2018 n n n n Blood Glucose 1. 9 – 3. 3 WCC 2. 2 Neutrophils 0. 9 Abnormal LFTs Attempts to regain weight unsuccessful Engaging in behaviours to avoid weight gain High levels of agitation and anxiety Constant negotiation over plan Constant requests for discharge
Admission 1 June – August 2018 n n Difficult decision between collaborative care versus coercive action Agreed to discharge at BMI 12. 2 to attempt community treatment
Admission 2 – September 2018 to February 2019 n n n Admitted BMI 11. 9 Denied anorexic cognitions Health anxiety but declined therapy Faecal incontinence (on supervised bathroom) Similar presentation to before but physical health more compromised
Admission 2 – September 2018 to February 2019 n n n n WCC 1. 9 Neutrophils 0. 7 Bradycardia 41 bpm Hypothermic 35. 2 degrees NEWS 6 Deranged LFTs Bone Scan – OSTEOPOROSIS
Admission 2 – September 2018 to February 2019 n n n n Only managed to get BMI to 13. 5 by February 2019 Bloods generally stabilised NEWS 1 -2 Completing 1800 calories Ongoing debates between voluntary versus coercive management Requested discharge Hands up…….
February 2019 – May 2019 n n Attempts to engage her in community EDS BMI 14. 4 May 2019 Reluctant to attend or engage in therapeutic work Discharged from Community EDS May 2019 at her request
July 2019 n n Contact from Specialist Dietitian (DGH) who was seeing SS for Ulcerative Colitis and low weight. Opening bowels 20 x day Weight loss down to BMI 13. 3, further fall to BMI 12. 6 Pulse 48, BP 99/65, Platelets 35
July 2019 n n n Admitted to DGH Unhappy about dietetic advice – self-discharged before Section 5(2) could be implemented Despite reluctance to engage with services – would frequently call Oaktrees EDU for advice
August 2019 n n Admitted to DGH due to low phosphate level (0. 6) Placed under Section 2 of MHA as requested discharge BMI 10. 9, continued to fall MARSIPAN Guidelines followed
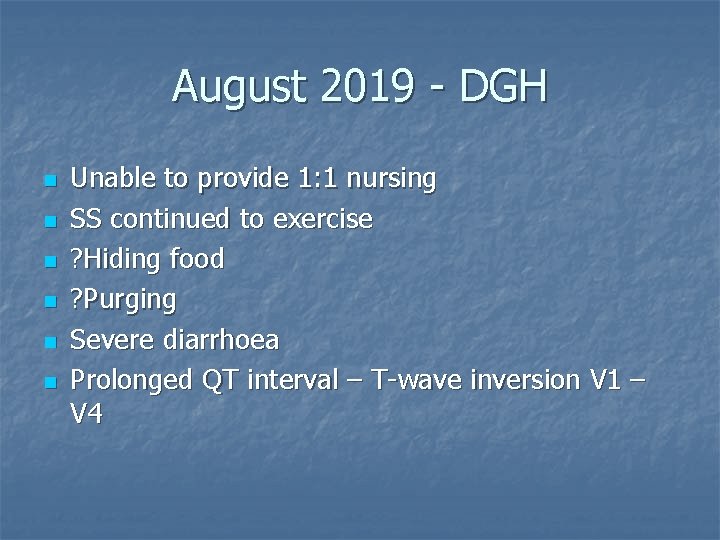
August 2019 - DGH n n n Unable to provide 1: 1 nursing SS continued to exercise ? Hiding food ? Purging Severe diarrhoea Prolonged QT interval – T-wave inversion V 1 – V 4
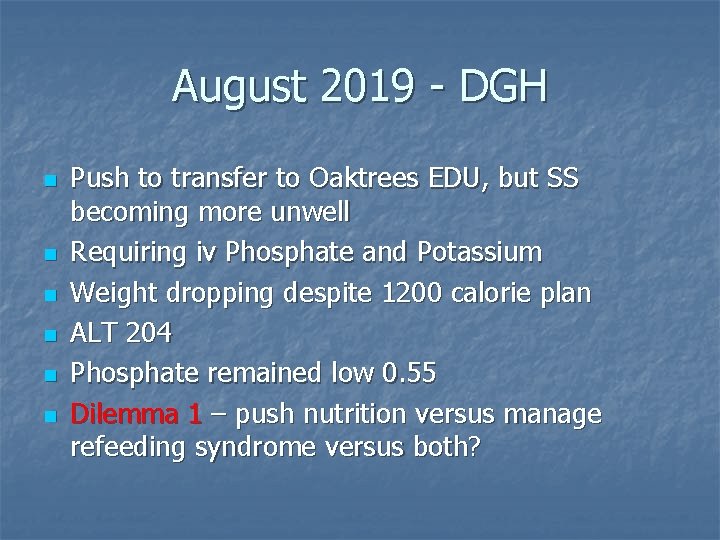
August 2019 - DGH n n n Push to transfer to Oaktrees EDU, but SS becoming more unwell Requiring iv Phosphate and Potassium Weight dropping despite 1200 calorie plan ALT 204 Phosphate remained low 0. 55 Dilemma 1 – push nutrition versus manage refeeding syndrome versus both?
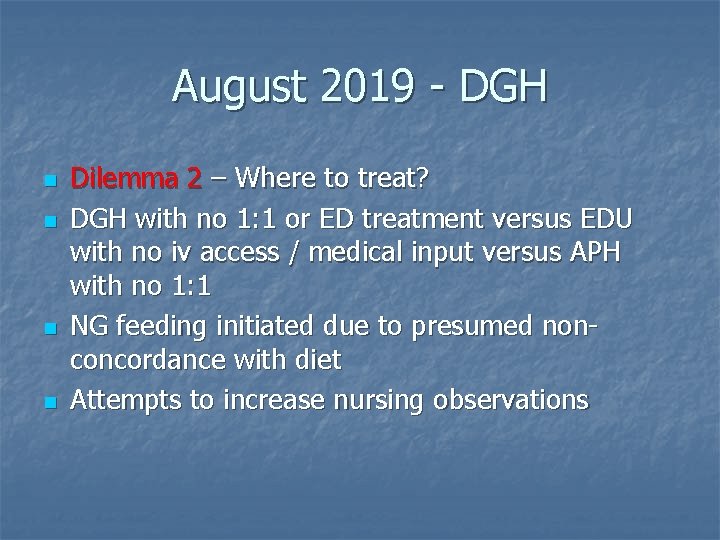
August 2019 - DGH n n Dilemma 2 – Where to treat? DGH with no 1: 1 or ED treatment versus EDU with no iv access / medical input versus APH with no 1: 1 NG feeding initiated due to presumed nonconcordance with diet Attempts to increase nursing observations
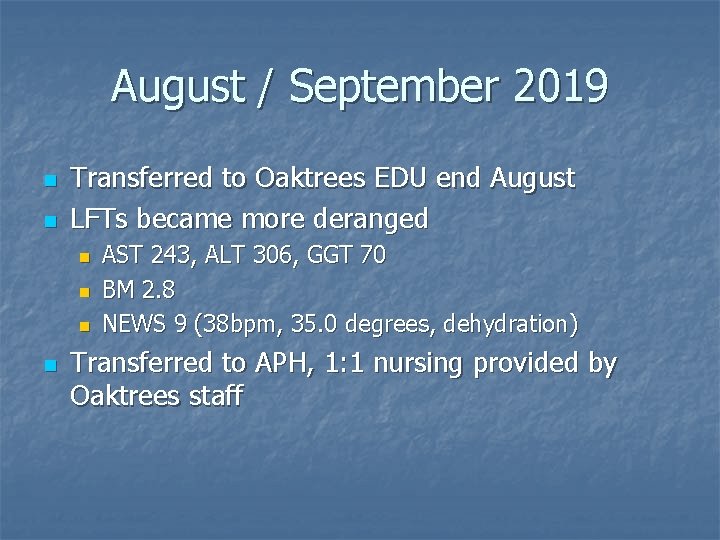
August / September 2019 n n Transferred to Oaktrees EDU end August LFTs became more deranged n n AST 243, ALT 306, GGT 70 BM 2. 8 NEWS 9 (38 bpm, 35. 0 degrees, dehydration) Transferred to APH, 1: 1 nursing provided by Oaktrees staff
September 2019 n n n BMI fell to 10. 8 Attempts to refeed affected by low phosphate despite replacement LFT deteriorating n n n (ALP 402, AST 2563, ALT 2567, GGT 218) Platelets 40 Phosphate 0. 45
September 2019 n n n n Tight communication between Oaktrees and APH staff LFT deteriorated n ALP 537, AST 4717, ALT 4149, GGT 250 S continued to negotiate diet plan. Did not feel she needed increase to 900 calories (NG fed at this point) Extensive diarrhoea when attempting to feed No evidence of UC flare-up Mobility impaired – more difficult to weigh Platelet count dropping to 30 Phosphate 0. 39
Mid-September 2019 n n n n Platelets reduced to 3 Haematemesis / PR bleeds / Nose Bleeds Oedema +++ BMI 11. 8 Discussion re OGD Transferred to ITU as tachycardic 150 Diet plan increased
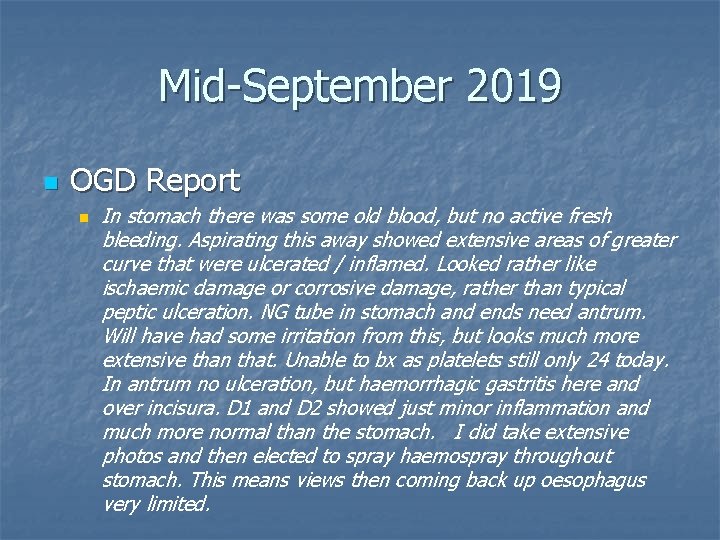
Mid-September 2019 n OGD Report n In stomach there was some old blood, but no active fresh bleeding. Aspirating this away showed extensive areas of greater curve that were ulcerated / inflamed. Looked rather like ischaemic damage or corrosive damage, rather than typical peptic ulceration. NG tube in stomach and ends need antrum. Will have had some irritation from this, but looks much more extensive than that. Unable to bx as platelets still only 24 today. In antrum no ulceration, but haemorrhagic gastritis here and over incisura. D 1 and D 2 showed just minor inflammation and much more normal than the stomach. I did take extensive photos and then elected to spray haemospray throughout stomach. This means views then coming back up oesophagus very limited.
September 2019 n n n n Debate around continued NG feed v TPN Some signs of improvement (transferred back to ward) Liver settled (ALP 87, AST 86, ALT 134, GGT 47) Increased anorexic drive and body image distortion But – haematemesis increased, Hb 60 Transferred back to ITU Blood transfusion
End September 2019 n n n CT Scan revealed an ischaemic bowel Decision to provide terminal care SS died 27 th September 2019 aged 20.
Anorexia Nervosa has the highest mortality rate of any psychiatric condition Arcelus J, Mitchell AJ, Wales J. et al, "Mortality Rates in Patients with Anorexia Nervosa and Other Eating Disorders: A Meta Analysis of 36 Studies. " Arch Gen Psychiatry 2011, 68: 724 -31. Sonnenville K, Micali N et al. , "Common Eating Disorders Predictive of Adverse Outcomes are Missed by the DSM-IV and DSM-5 Classifications. " Paediatrics 2012; 130: e 289 -95
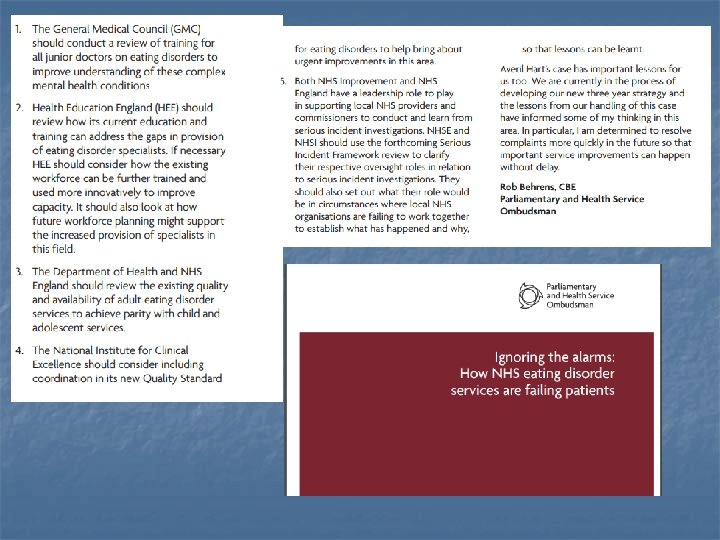
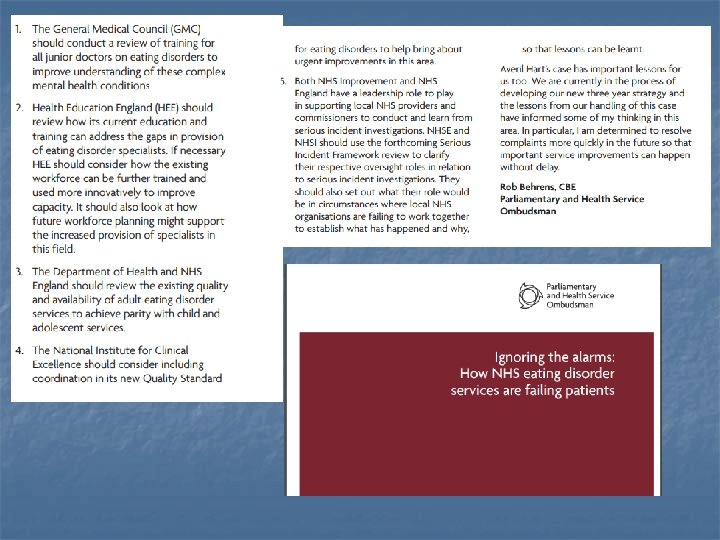
MARSIPAN n n n This case adhered to MARSIPAN Guidelines Outcome still tragic Many success stories over last 10 years Regional MARSIPAN group established Still lots of work to be done to prevent further deaths Lots can go wrong….
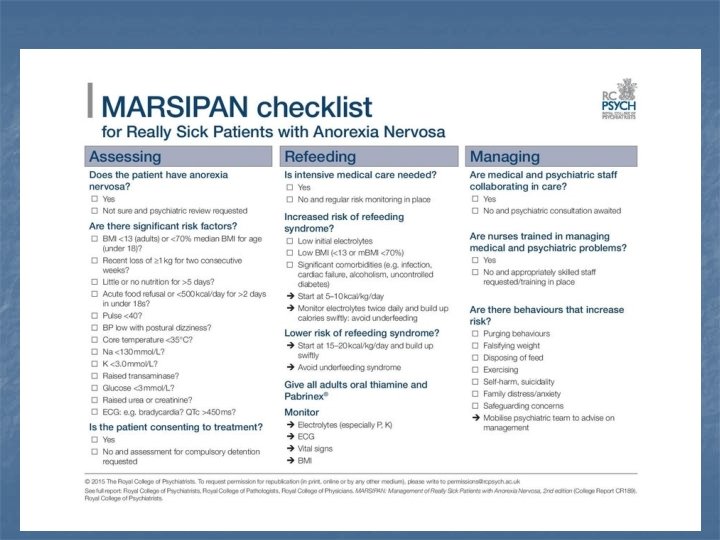
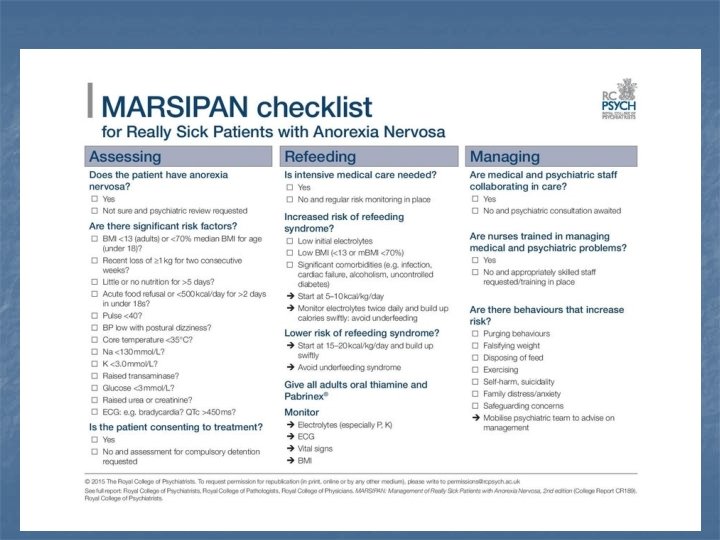
Who is at risk? Criteria for determining people at high risk of developing re-feeding problems (adapted from NICE 2006): Patient has one or more of the following: n n n Little or no nutritional intake for more than 10 days BMI < 16 kg/m 2 Weight loss >15% within last 3 – 6 months Low levels of potassium, phosphate or magnesium prior to feeding History of alcohol abuse or drugs including insulin, chemotherapy, antacids or diuretics The presence of purging behaviours Or patient has two or more of the following: n n n Little or no oral intake for more than 5 days BMI <18. 5 kg/m 2 Weight loss > 10% within last 3 – 6 months
Who Is at Risk? (My World) n n n n BMI less that 13 kg/m 2 Losing 1 kg/week or more Abnormal Blood film, Low WCC and Neutrophils Raised LFTs Reduced Pulse (<50 bpm) and BP (<90/50) Abnormal ECG Poor insight / lack of capacity Actively engaging in activities to promote weight loss
Awareness n n n 18 year old Anorexia Nervosa for 5 years Admitted with low weight after deteriorating in a general psychiatric ward Medical team re-fed but failed to diagnose refeeding syndrome Died of multiple organ failure Lessons n Non-specialist services should work closely with specialist services and hand over care when appropriate n Medical services need to be educated about MARSPIAN England
Diagnosis n n n n Age 37 Anorexia Nervosa for 20 years BMI 8. 9 Admitted to SEDU “Lack of regular physical observations or appropriate blood tests” Died after 4 weeks Lesson – Patients in high risk range must have regular physical observations n n n Pulse and BP Daily ECG Daily Blood Tests – Electrolytes, LFTs, Calcium, Magnesium and Phosphate England

Urgency n n Isabelle Caro “We want to do some tests but so as not to bother you we will let you have some sleep first” Died 48 hours later from severe dehydation Lesson – Make your risk assessment without delay France
Underfeeding Syndrome n n n n 21 year old 6 year history of AN Admitted to A+E with chest pain No cause found but admitted due to abnormal LFTs Not fed during admission through fear of refeedign syndrome Died after 7 days on 0 calories Lessons – Get patient to SEDU unless medical bed is essential n Avoid refeeding syndrome by refeeding slowly but reassess every 12 hours and increase feed England
Specialist Treatment n n n Age 20 Anorexia Nervosa for 9 years Admitted to General Psychiatry Ward as no SEDU beds Died at 32 kg Lesson – Admit to SEDU as soon as possible Australia
NG Tube? n n n 24 years old 6 year history of AN General Medical Ward Consultant refused to pass an NG tube against patient’s will Patient overexercised – developed fatal hypoglycemia Lesson – You may need to treat against patient’s will and/or use NG tube England
MARSIPAN
The MARSIPAN Reports Google MARSIPAN and anorexia
Food and Hydration are treatments under the Mental Health Act (1983)
Start Vitamins and Minerals n n Sanatogen A-Z or Forceval (2 daily) Calcichew D 3 Forte (2 daily) Thiamine 100 mg bd Vitamin B Co Strong (2 tds)
Anorexia Nervosa Re-feeding Syndrome n n The first 7 -10 days of feeding a seriously ill patient with anorexia nervosa poses a significant risk of developing re-feeding syndrome and its related complications Essential to re-feed slowly and gradually
How to Prevent and Treat Refeeding Syndrome n n n Recommend that an initial starting intake of 1520 Kcals/Kg of body weight (MARSIPAN Guidelines) is used. Where severity indicators are present, a lower starting intake may be required e. g. 10 Kcals/Kg body weight Monitor electrolytes by taking daily bloods (no need or point in giving electrolytes prior to commencing feeding even if blood levels low, as until CHO is present to stimulate insulin production which activates membrane pumps, any given prior to this will be excreted. ) Vitamin and trace element supplementation
What Should You Do? n n Access / familiarise MARSIPAN Guidelines Prepare! n n Does your hospital have a MARSIPAN pathway? Is there an identified lead? Are staff adequately trained / knowledgeable in this area? Are you aware of local eating disorders provision?
What Should You Do? n Act n n n n Use the Mental Health Act if appropriate Be mindful / suspicious of compensatory behaviours if not continually observed by nursing staff Keep a close eye of physical health and weight Weigh DAILY Get specialist eating disorder psychiatry help Keep communication tight Careful balance between underfeeding and overfeeding Be understanding towards Mental Health Eating Disorder services – we know our trade, and can assess/predict physical risk

Questions…
 Marsipan guidelines
Marsipan guidelines The sixth sick sheik's sixth sheep's sick lyrics
The sixth sick sheik's sixth sheep's sick lyrics Bullimia
Bullimia Junior marsipan
Junior marsipan Marsipan risk assessment framework
Marsipan risk assessment framework Peanøtt belgfrukt
Peanøtt belgfrukt Lippincott williams & wilkins
Lippincott williams & wilkins Management of patients with neurologic trauma
Management of patients with neurologic trauma Periodontal management of medically compromised patients
Periodontal management of medically compromised patients Winona ryder anorexia
Winona ryder anorexia Freud anorexia
Freud anorexia Long term effects of anorexia
Long term effects of anorexia Unit 3 nutrition lesson 6 anorexia nervosa and bulimia
Unit 3 nutrition lesson 6 anorexia nervosa and bulimia Male
Male Hetsätning självhjälp
Hetsätning självhjälp Anorexia nervosa ppt
Anorexia nervosa ppt Social learning theory anorexia
Social learning theory anorexia Bulimia vs anorexia usmle
Bulimia vs anorexia usmle Dominique anorexia
Dominique anorexia Definition of bullimia
Definition of bullimia Historia natural de la anorexia
Historia natural de la anorexia Cid transtornos alimentares
Cid transtornos alimentares Health consequences of anorexia
Health consequences of anorexia Excessive acid production
Excessive acid production Obesidad
Obesidad Anorexia nervosa
Anorexia nervosa Gisele bundchen anorexia
Gisele bundchen anorexia Anorexia nervosa syptoms
Anorexia nervosa syptoms The diagnostic term anorexia nervosa literally means
The diagnostic term anorexia nervosa literally means Anorexia athletica def
Anorexia athletica def Jeremy gillitzer
Jeremy gillitzer Anorexia, nausea and vomiting
Anorexia, nausea and vomiting Dr phil anorexia
Dr phil anorexia Dr hong-phuc tran
Dr hong-phuc tran Anorexia nervosa definition wikipedia
Anorexia nervosa definition wikipedia Bulimia nervosa ap psychology definition
Bulimia nervosa ap psychology definition Kate moss anorexia
Kate moss anorexia Kate bosworth eating disorder
Kate bosworth eating disorder Kode icd 10 anoreksia
Kode icd 10 anoreksia Mária tóthová
Mária tóthová Food pyramid with labels
Food pyramid with labels Anorexia nervosa is characterized
Anorexia nervosa is characterized Anorexia etimologia
Anorexia etimologia Anorexia and bulimia venn diagram
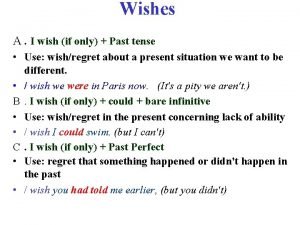
Anorexia and bulimia venn diagram Wish + past tense
Wish + past tense 150 000 scientific notation
150 000 scientific notation What leaders really do hbr
What leaders really do hbr Tell me what you really like
Tell me what you really like