Principles of Family Medicine The Patient Centered Clinical
- Slides: 17
Principles of Family Medicine The Patient Centered Clinical Method Saudi Diploma in Family Medicine Center of Post Graduate Studies in Family Medicine Presented by: Dr. Zekeriya Aktürk zekeriya. akturk@gmail. com www. aile. net 1 / 17
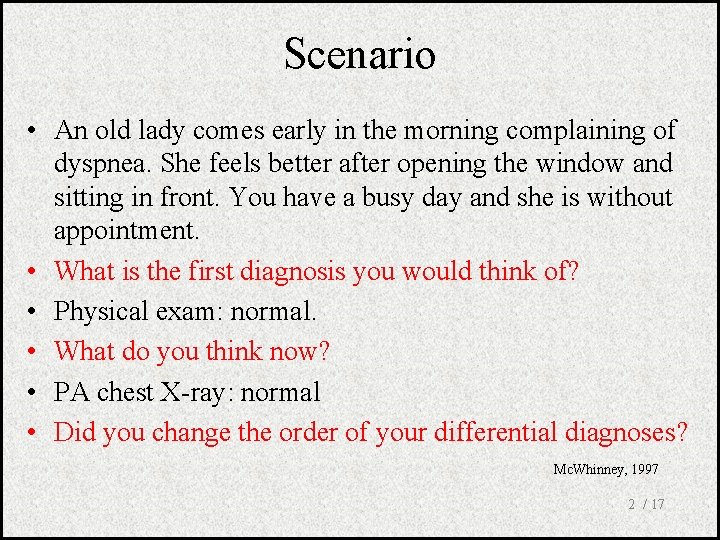
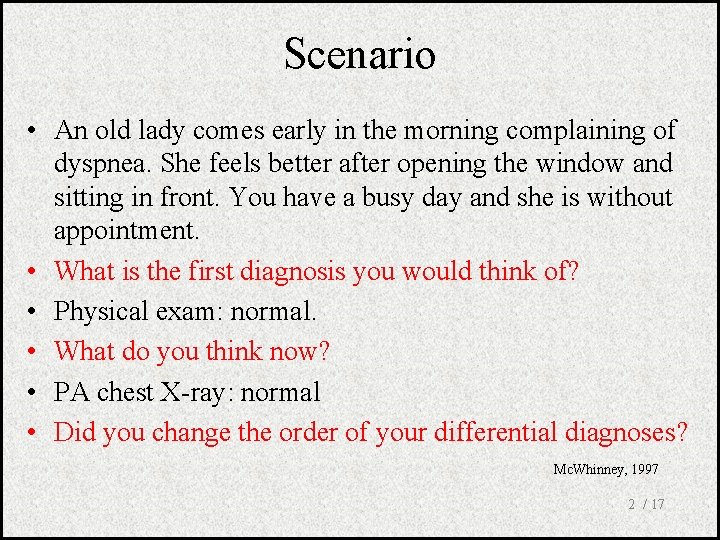
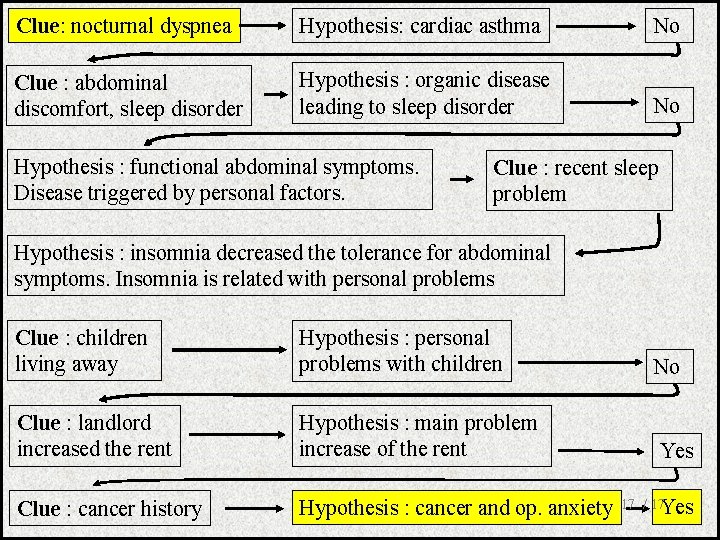
Scenario • An old lady comes early in the morning complaining of dyspnea. She feels better after opening the window and sitting in front. You have a busy day and she is without appointment. • What is the first diagnosis you would think of? • Physical exam: normal. • What do you think now? • PA chest X-ray: normal • Did you change the order of your differential diagnoses? Mc. Whinney, 1997 2 / 17
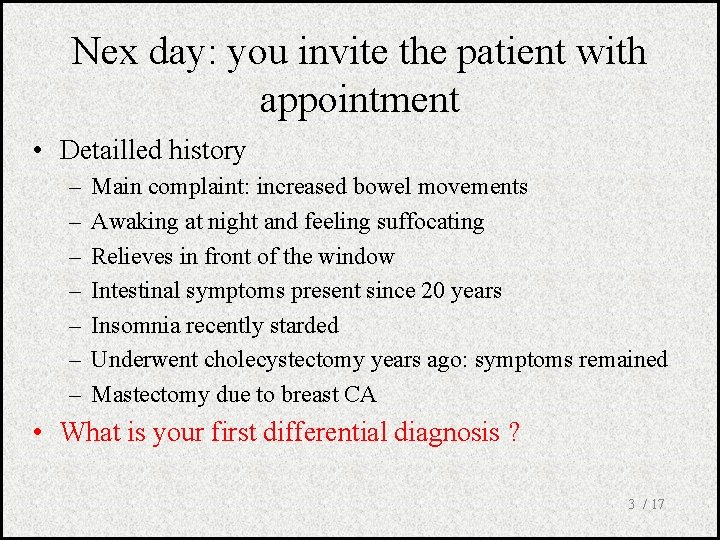
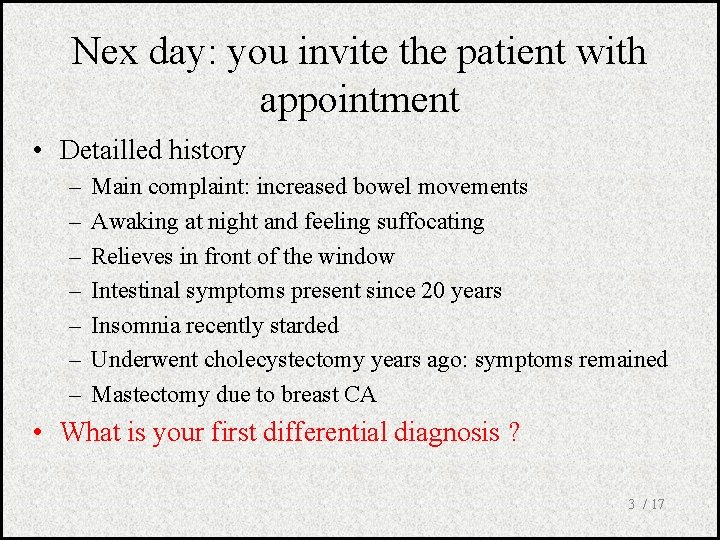
Nex day: you invite the patient with appointment • Detailled history – – – – Main complaint: increased bowel movements Awaking at night and feeling suffocating Relieves in front of the window Intestinal symptoms present since 20 years Insomnia recently starded Underwent cholecystectomy years ago: symptoms remained Mastectomy due to breast CA • What is your first differential diagnosis ? 3 / 17
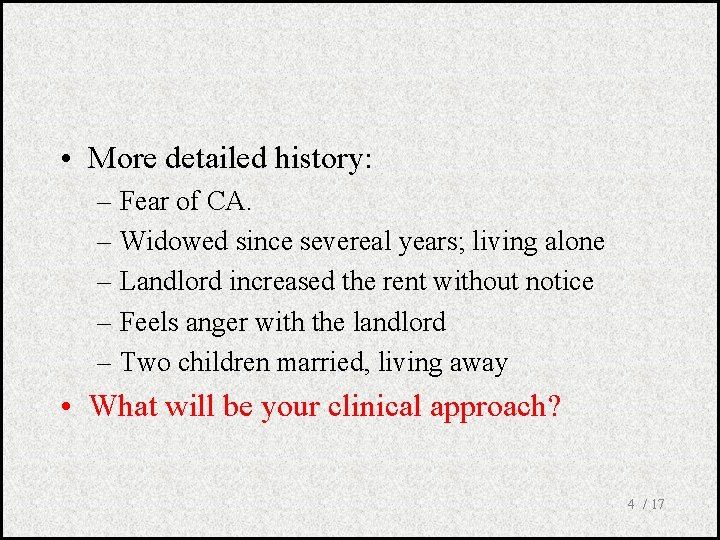
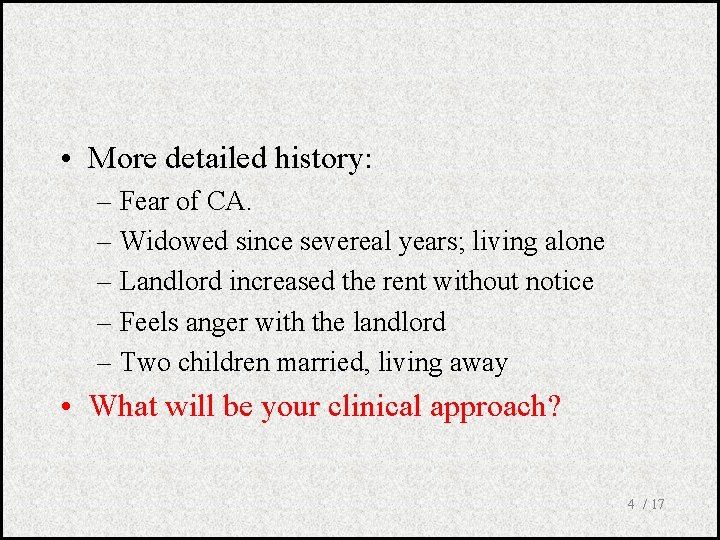
• More detailed history: – Fear of CA. – Widowed since severeal years; living alone – Landlord increased the rent without notice – Feels anger with the landlord – Two children married, living away • What will be your clinical approach? 4 / 17
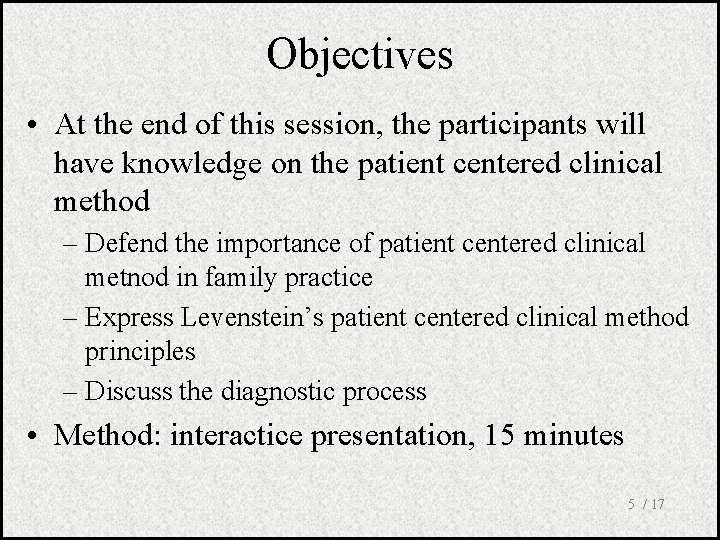
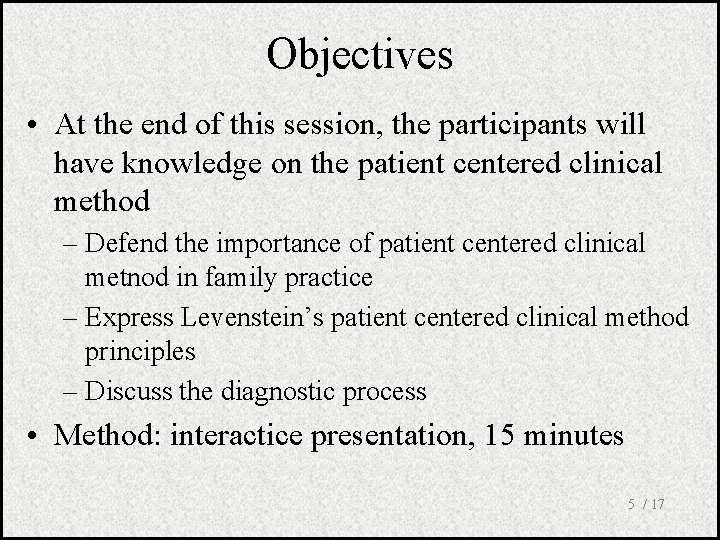
Objectives • At the end of this session, the participants will have knowledge on the patient centered clinical method – Defend the importance of patient centered clinical metnod in family practice – Express Levenstein’s patient centered clinical method principles – Discuss the diagnostic process • Method: interactice presentation, 15 minutes 5 / 17
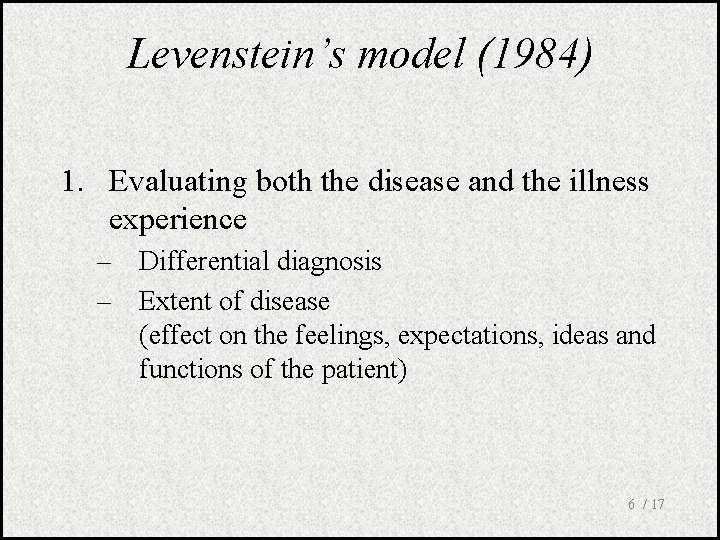
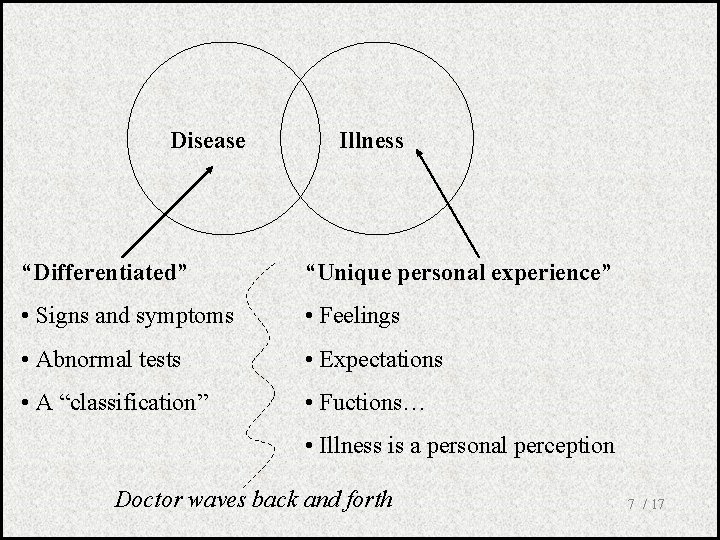
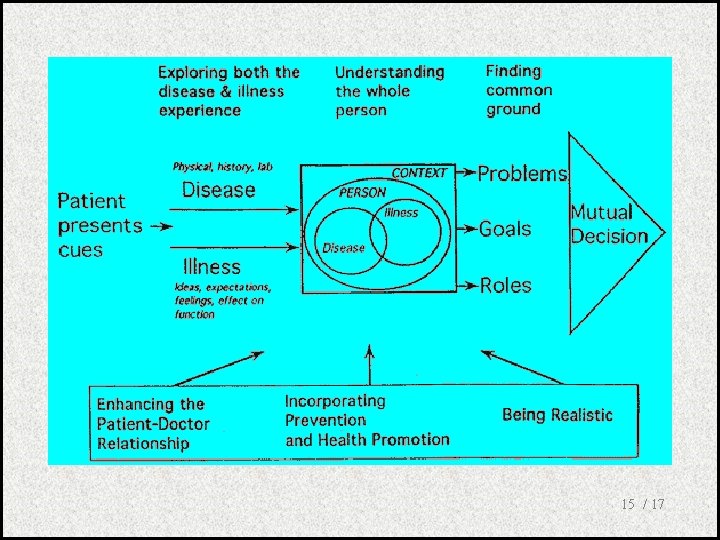
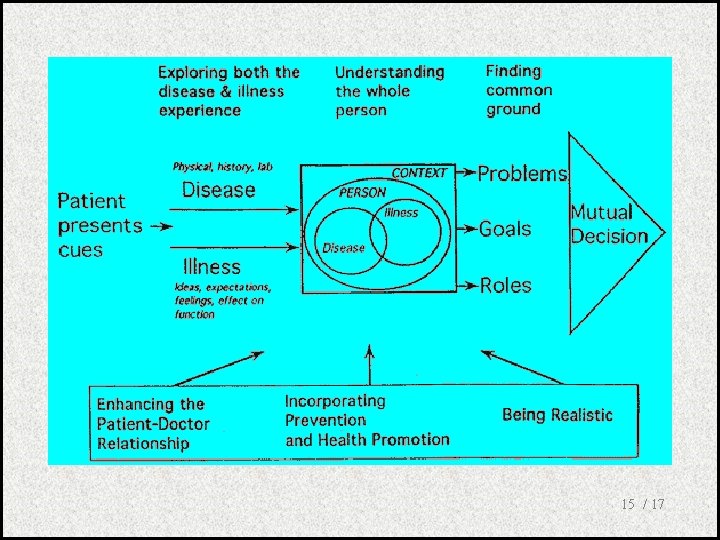
Levenstein’s model (1984) 1. Evaluating both the disease and the illness experience – Differential diagnosis – Extent of disease (effect on the feelings, expectations, ideas and functions of the patient) 6 / 17
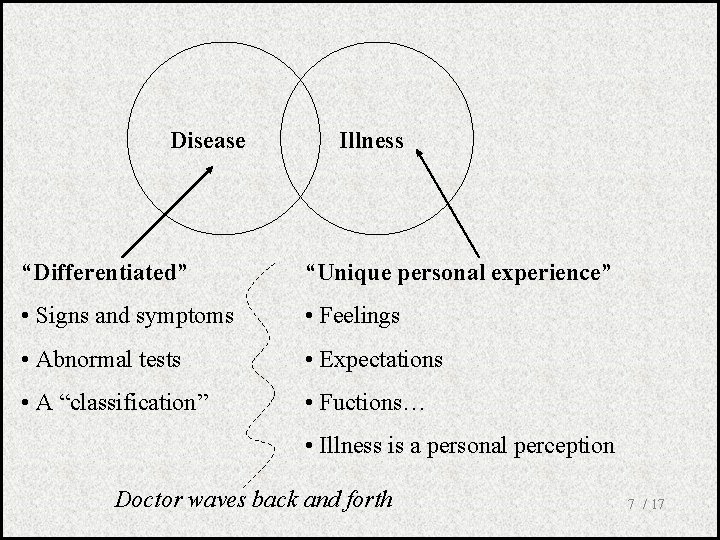
Disease Illness “Differentiated” “Unique personal experience” • Signs and symptoms • Feelings • Abnormal tests • Expectations • A “classification” • Fuctions… • Illness is a personal perception Doctor waves back and forth 7 / 17
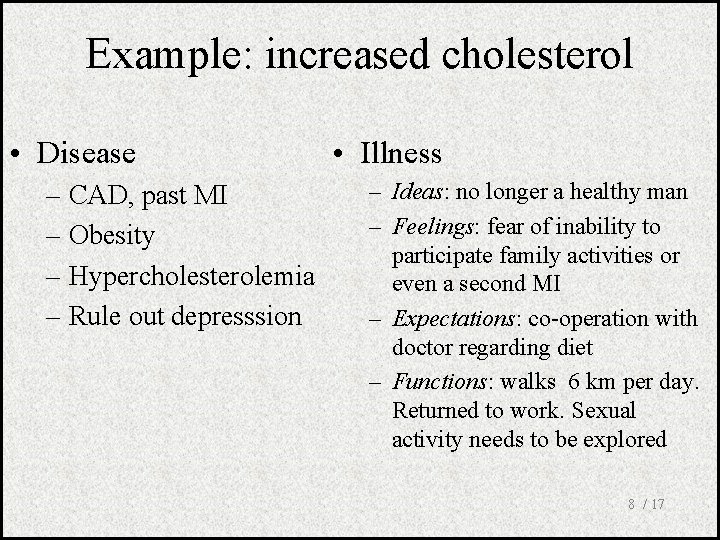
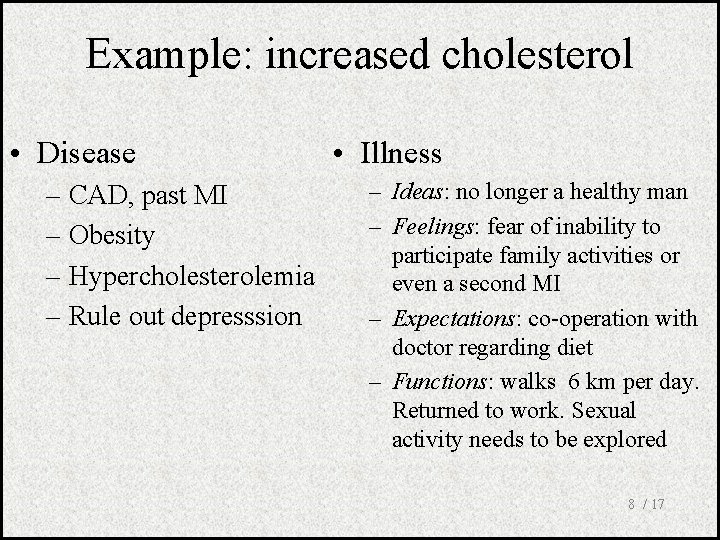
Example: increased cholesterol • Disease – CAD, past MI – Obesity – Hypercholesterolemia – Rule out depresssion • Illness – Ideas: no longer a healthy man – Feelings: fear of inability to participate family activities or even a second MI – Expectations: co-operation with doctor regarding diet – Functions: walks 6 km per day. Returned to work. Sexual activity needs to be explored 8 / 17
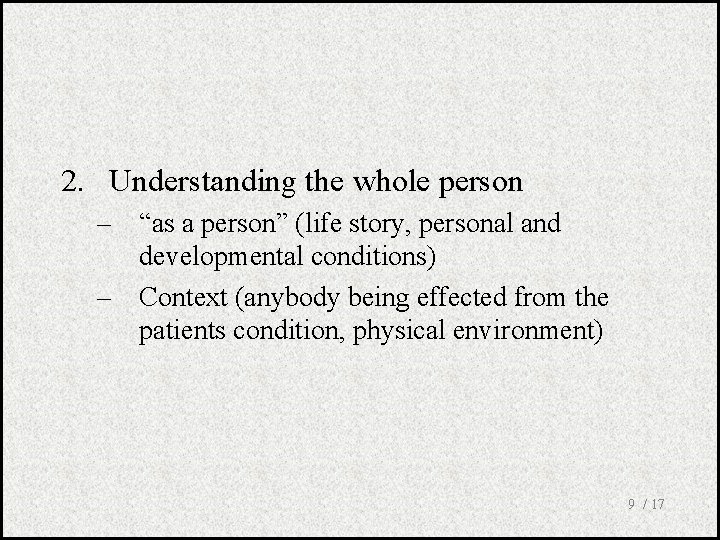
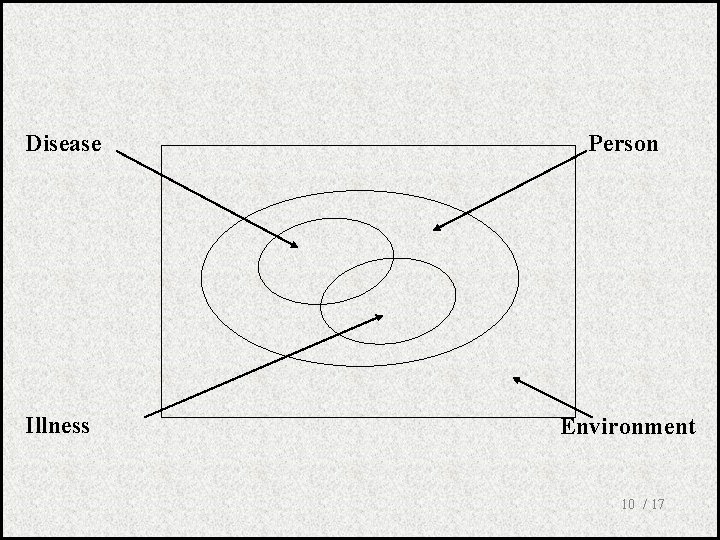
2. Understanding the whole person – “as a person” (life story, personal and developmental conditions) – Context (anybody being effected from the patients condition, physical environment) 9 / 17
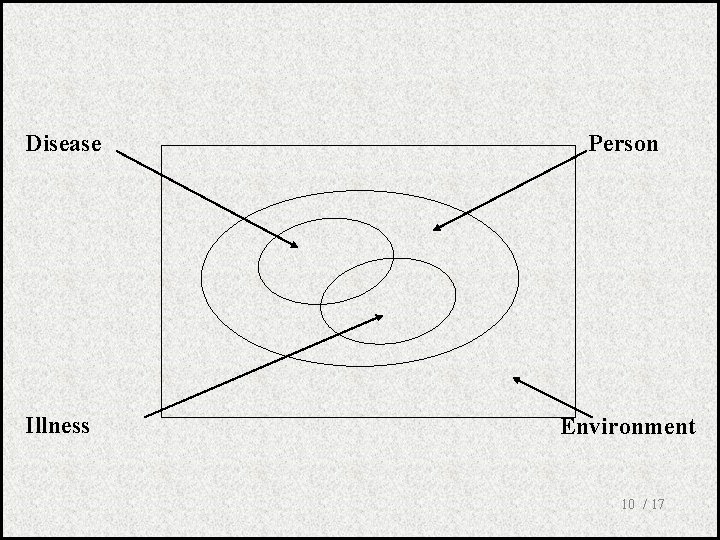
Disease Person Illness Environment 10 / 17
3. Finding common ground with the patient about the problem and its management – Problems and priorities – Treatment goals – Roles of doctor and patient in the treatment 11 / 17
4. Incorporating prevention and health promotion – – Health promotion Risk reduction Early diagnosis Decreasing complications 12 / 17
5. Enhancing the doctor-patient relationship – – – Features of therapeutic relationship Sharing of power Care and cure Self awareness Transference and countertransference 13 / 17
6. Being realistic – Time – Resources – Team 14 / 17
15 / 17
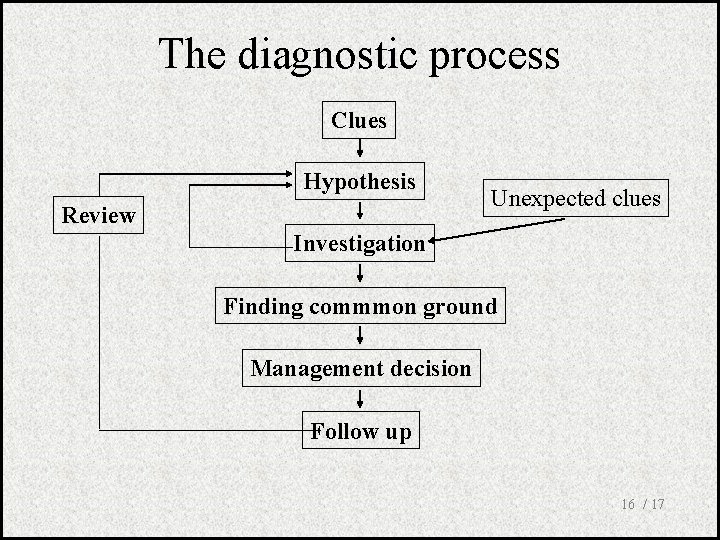
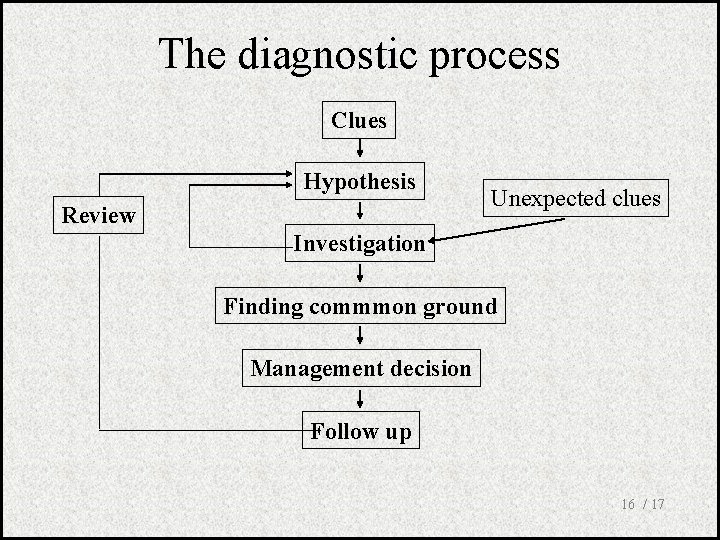
The diagnostic process Clues Hypothesis Review Unexpected clues Investigation Finding commmon ground Management decision Follow up 16 / 17
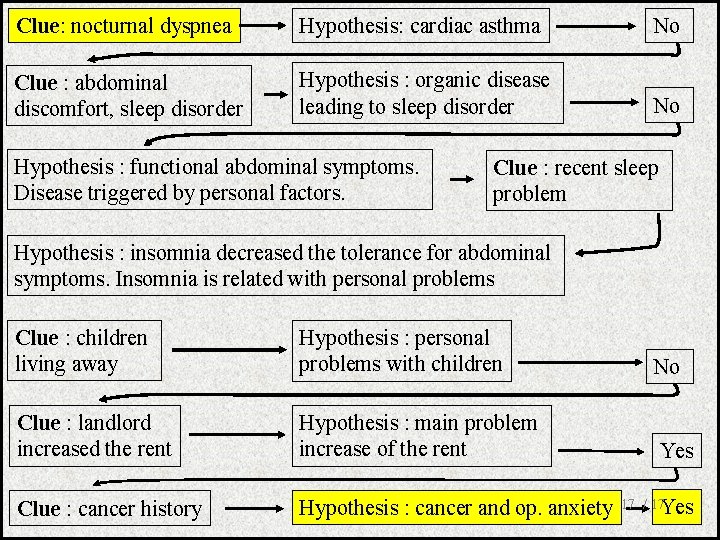
Clue: nocturnal dyspnea Hypothesis: cardiac asthma No Clue : abdominal discomfort, sleep disorder Hypothesis : organic disease leading to sleep disorder No Hypothesis : functional abdominal symptoms. Disease triggered by personal factors. Clue : recent sleep problem Hypothesis : insomnia decreased the tolerance for abdominal symptoms. Insomnia is related with personal problems Clue : children living away Hypothesis : personal problems with children No Clue : landlord increased the rent Hypothesis : main problem increase of the rent Yes Clue : cancer history Hypothesis : cancer and op. anxiety 17 / 17 Yes
 Paradigm shift teacher-centered to student-centered
Paradigm shift teacher-centered to student-centered Patient centered medical home conference
Patient centered medical home conference Qsen patient centered care examples
Qsen patient centered care examples Patient centered medical home
Patient centered medical home Patient centered primary care collaborative
Patient centered primary care collaborative Patient centered primary care collaborative
Patient centered primary care collaborative Patient centered care
Patient centered care Principles of family medicine
Principles of family medicine Dr riaz qureshi
Dr riaz qureshi Strategies of family centered care
Strategies of family centered care Family centered care definition
Family centered care definition Learner centered psychological principles
Learner centered psychological principles What are the three principles of user-centered design?
What are the three principles of user-centered design? Patient 2 patient
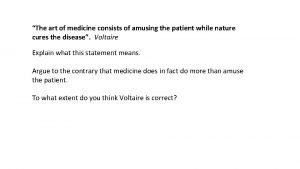
Patient 2 patient The art of medicine is amusing the patient
The art of medicine is amusing the patient Which type of drug are distributed by the envelope method
Which type of drug are distributed by the envelope method Patient family
Patient family Types of family in community medicine
Types of family in community medicine