Hypertension Definition the force exerted by the blood
Hypertension Ø Definition: the force exerted by the blood against the walls of the bleed vessels ØAdequate to maintain tissue perfusion during activity and rest ØArterial blood pressure: primary function of cardiac output and systemic vascular resistance
Hypertension Arterial BP = Cardiac Output (CO) x Systemic vascular resistance (SVR) Cardiac Output = stroke volume x beats per min Systemic vascular resistance = force opposing the movement of blood within the blood vessels What is the effect on BP if SVR increased
Hypertension Mechanisms that Regulate BP Ø Sympathetic Nervous System Ø Vascular Endothelium Ø Renal System Ø Endocrine System
Hypertension Mechanisms that Regulate BP Ø Sympathetic Nervous System (SNS) – norepinephrine released from sympathetic nerve endings - to receptors alpha 1, alpha 2, beta 1 & beta 2 ØReacts within seconds ØIncreases Heart Rate - chronotropic ØIncreased cardiac contractility - inotropic ØProduces widespread vasoconstriction in peripheral arterioles
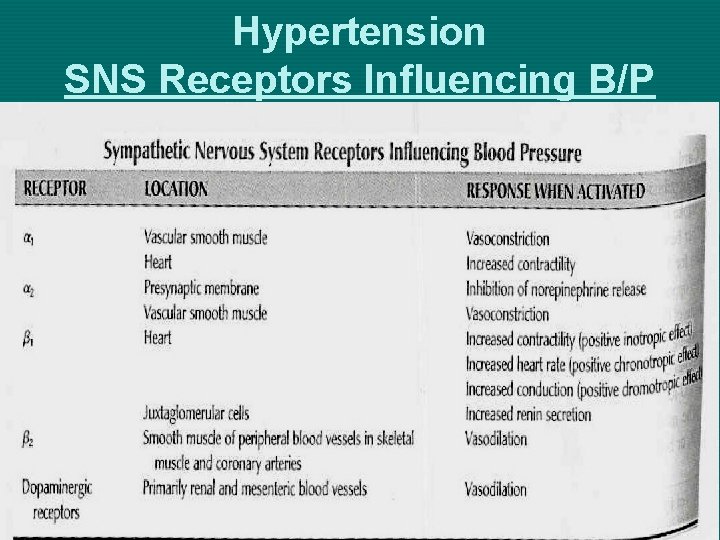
Hypertension SNS Receptors Influencing B/P
Hypertension Mechanisms that Regulate BP Ø Sympathetic Nervous System (SNS)– ØSympathetic Vasomotor Center – located in the medulla – interacts with many areas of the brain to maintain BP within normal range under various conditions ØExercise – changes to meet oxygen demand ØPostural Changes – peripheral vasoconstriction
Hypertension Mechanisms that Regulate BP Ø Sympathetic Nervous System (SNS) – ØBaroreceptors: specialized nerve cells the carotid arteries and the aortic arch ØSensitive to BP changes: ØIncrease: Inhibits SNS – peripheral vessel dilation. Decreased heart rate, and decreased contractility of the heart + increased parasympathetic activity (vagus nerve) decreased heart rate ØDecrease: Activates SNS – peripheral vessel constriction, increased heart rate, and
Hypertension Mechanisms that Regulate BP Ø Vascular Endothelium ØSingle cell layer that lines the blood vessels ØProduce vasoactive substances: ØEDRF Endothelium-derive relaxing factor – Ø Helps maintain low arterial tone at rest Ø Inhibits growth of the smooth muscle layer Ø Inhibits platelet aggregation ØVasodilation – prostacyclin ØEndothelin (ET) potent vasoconstrictor Endothelial dysfunction may contribute to atherosclerosis & primary hypertension
Hypertension Mechanisms that Regulate BP Ø Renal System ØControl Na+ excretion & extracellular fluid volume ØRenal - Renin-angiotensin-aldosterone ØRenin converts angiotensinogen to angiotensin I ØAngiotensin-converting enzyme (ACE) converts I into angiotsensin II ØImmediate: Vasoconstrictor – increased systemic vascular resistance ØProlonged: Stimulates the adrenal cortex to secret Aldosterone – Na+ and Water retention ØRenal Medulla - Prostaglandins - vasodilator
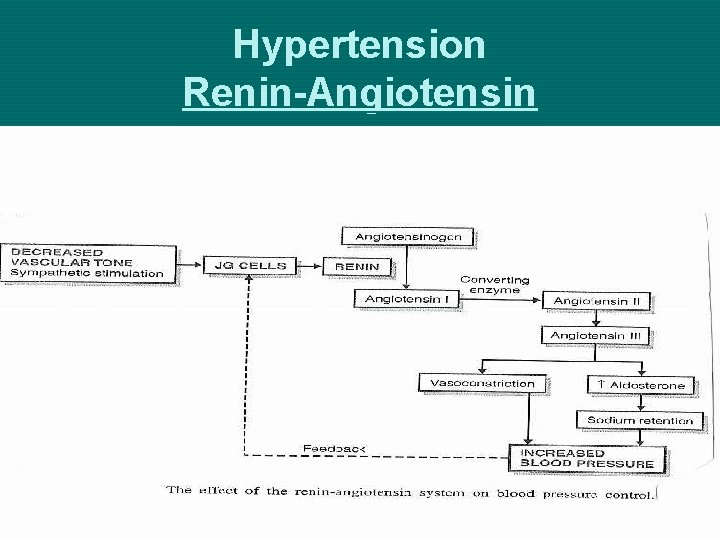
Hypertension Renin-Angiotensin
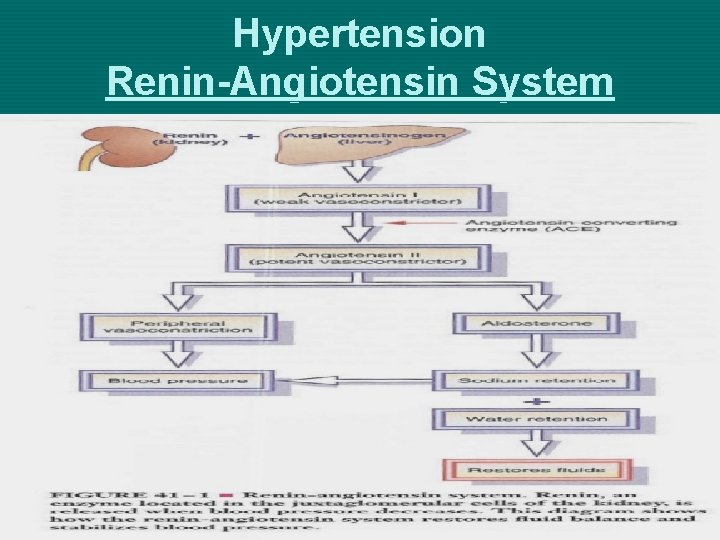
Hypertension Renin-Angiotensin System
Hypertension Mechanisms that Regulate BP Ø Endocrine System ØStimulates the SNS with ØEpinephrine – increases HR and contractility ØActivates B 2 -adrenergic receptors in peripheral arterioles of skeletal muscle = vasodilation ØActivates A 1 -adrenergic receptors in peripheral arterioles of skin and kidneys = vasoconstiction ØAdrenal Cortex – Aldosterone – stimulates kidneys to retain Na+ ØIncreased Na+ stimulates posterior pituitary – ADH – reabsorbs ECF/water
Hypertension Aldosterone Mechanism • Increased Aldosterone = • Increases sodium reabsorption = • Increases water reabsorption = • Increases blood volume = • Increases cardiac output
Hypertension Mechanisms that Regulate BP Ø Regulatory mechanisms in the health person function in response to the demands on the body Ø When Hypertension develops, one or more of these mechanisms are defective Ø Sympathetic Nervous System Ø Vascular Endothelium Ø Renal System Ø Endocrine System
Secondary Hypertension Pathophysiology Ø Specific cause of hypertension can be identified Ø 5+% of adult hypertension Ø Causes: Ø Coarctation or congenital narrowing of the aorta Ø Renal disease – renal artery disease / parenchymal Ø Endocrine disorders: Pheochromocytoma, Cushing Syndrome, Hyperaldosteronism Ø Neurology disorders – brain tumors / head injury Ø Sleep apnea Ø Medications – sympathetic stimulants
Hypertension Pathophysiology Ø Primary (Essential) Hypertension: ØElevated BP without an identified cause ØAccounts for 95% of all cases of hypertension ØCause – unknown ØContributing Factors: Increased SNS activity, overproduction of Na+ retaining hormones & vasoconstrictors, increased Na+ intake ØRisk Factors: Modifiable
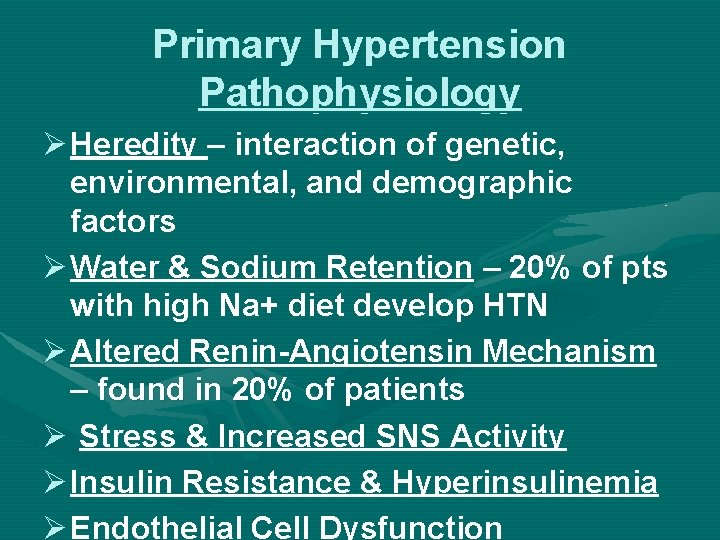
Primary Hypertension Pathophysiology Ø Heredity – interaction of genetic, environmental, and demographic factors Ø Water & Sodium Retention – 20% of pts with high Na+ diet develop HTN Ø Altered Renin-Angiotensin Mechanism – found in 20% of patients Ø Stress & Increased SNS Activity Ø Insulin Resistance & Hyperinsulinemia Ø Endothelial Cell Dysfunction
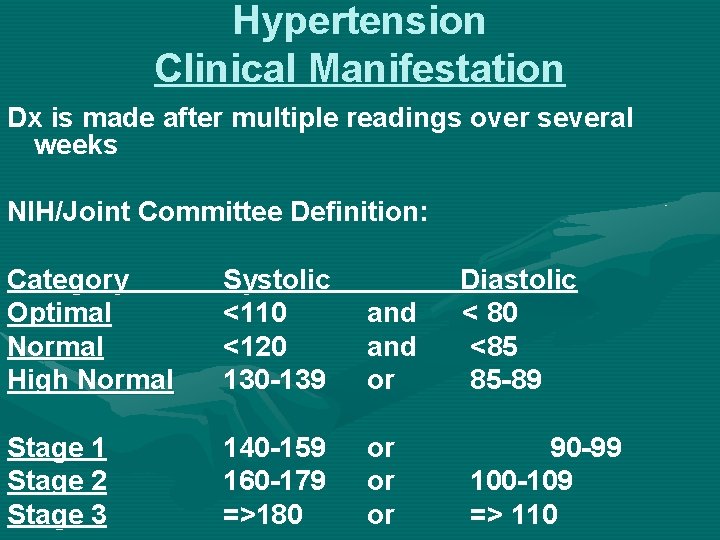
Hypertension Clinical Manifestation Dx is made after multiple readings over several weeks NIH/Joint Committee Definition: Category Optimal Normal High Normal Systolic <110 <120 130 -139 and or Stage 1 Stage 2 Stage 3 140 -159 160 -179 =>180 or or or Diastolic < 80 <85 85 -89 90 -99 100 -109 => 110

Primary Hypertension Risk Factors Ø Age Ø Alcohol Ø Cigarette Smoking Ø Diabetes Mellitus Ø Elevated serum lipids Ø Excess Na+ in diet Ø Gender Ø Family History Ø Obesity Ø Ethnicity Ø Sedentary Lifestyle Ø Socioeconomic Ø Stress
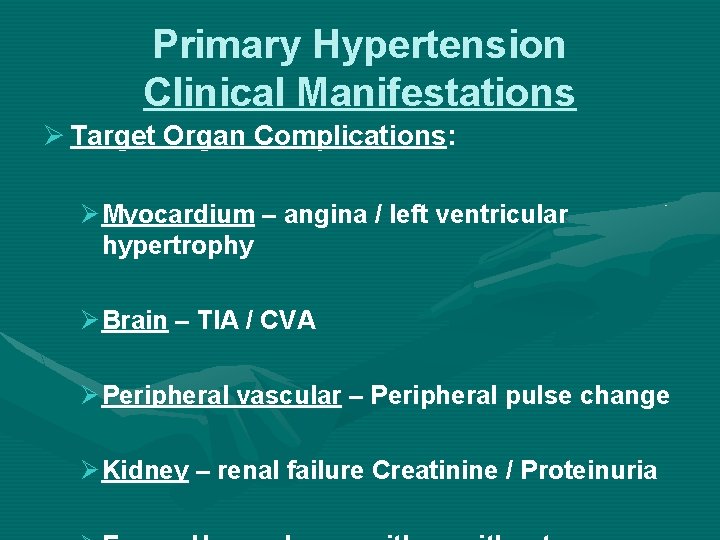
Primary Hypertension Clinical Manifestations Ø Target Organ Complications: Ø Myocardium – angina / left ventricular hypertrophy Ø Brain – TIA / CVA Ø Peripheral vascular – Peripheral pulse change Ø Kidney – renal failure Creatinine / Proteinuria
Primary Hypertension Clinical Manifestations Ø “Silent Killer” – asymptomatic and insidious Ø Severe HTN – fatigue, reduced activity tolerance, dyspnea, dizziness, palpitations, angina
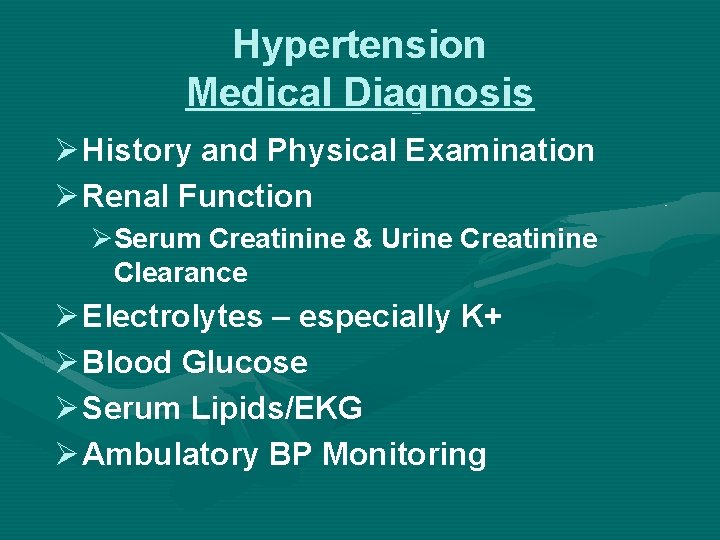
Hypertension Medical Diagnosis Ø History and Physical Examination Ø Renal Function ØSerum Creatinine & Urine Creatinine Clearance Ø Electrolytes – especially K+ Ø Blood Glucose Ø Serum Lipids/EKG Ø Ambulatory BP Monitoring
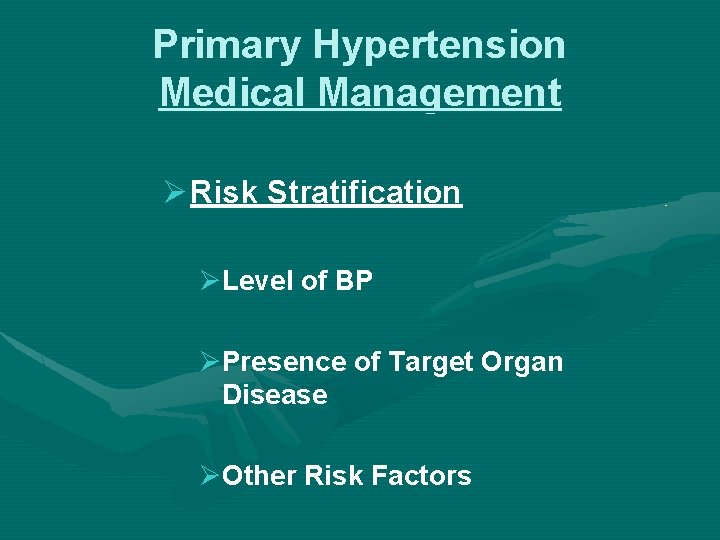
Primary Hypertension Medical Management Ø Risk Stratification ØLevel of BP ØPresence of Target Organ Disease ØOther Risk Factors
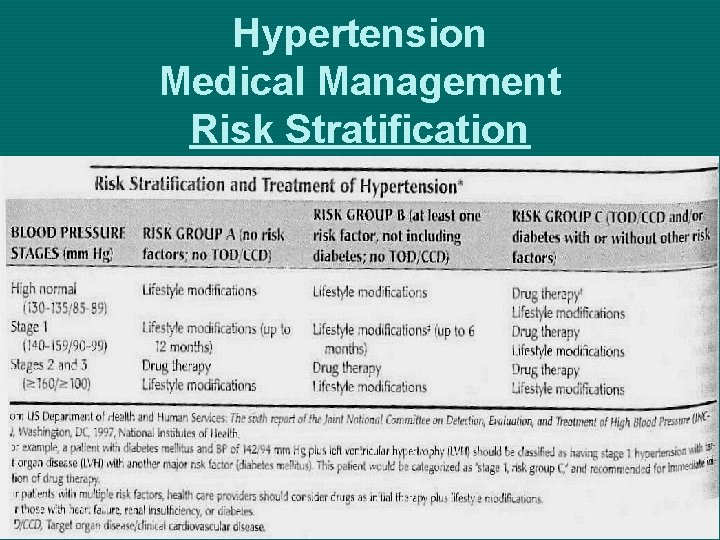
Hypertension Medical Management Risk Stratification

Primary Hypertension Medical Management Ø Lifestyle modification Ø Nutritional therapy Ø Alcohol consumption Ø Physical activity Ø Tobacco avoidance Ø Stress management Ø Drug Therapy
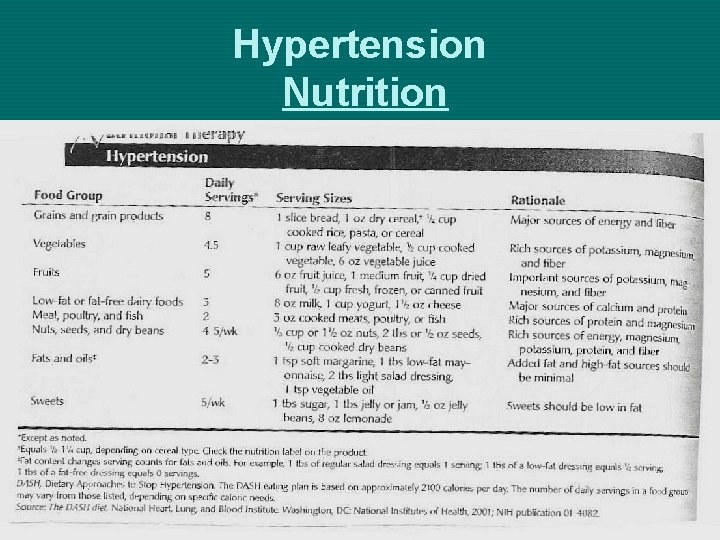
Hypertension Nutrition
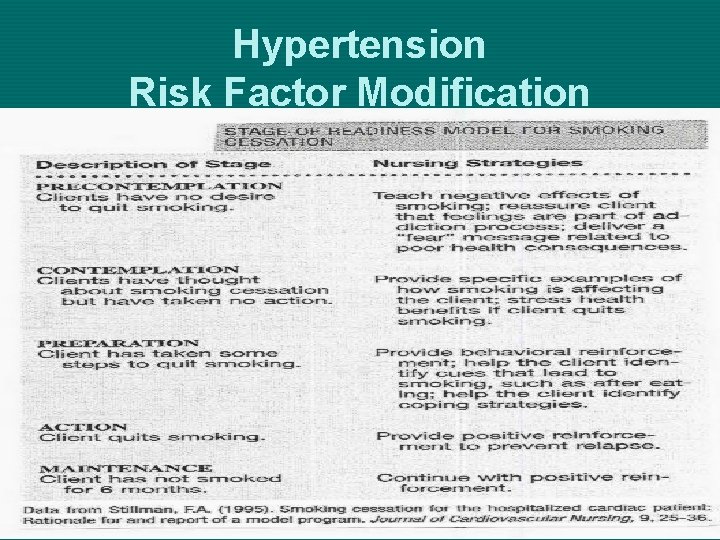
Hypertension Risk Factor Modification
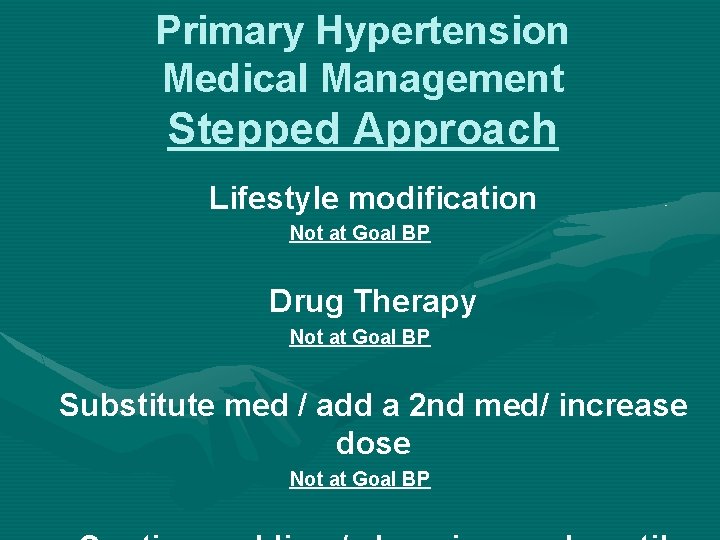
Primary Hypertension Medical Management Stepped Approach Lifestyle modification Not at Goal BP Drug Therapy Not at Goal BP Substitute med / add a 2 nd med/ increase dose Not at Goal BP
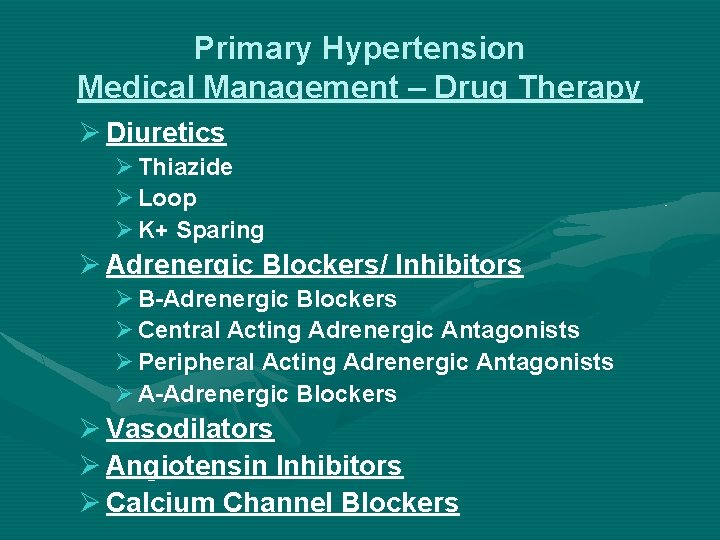
Primary Hypertension Medical Management – Drug Therapy Ø Diuretics Ø Thiazide Ø Loop Ø K+ Sparing Ø Adrenergic Blockers/ Inhibitors Ø B-Adrenergic Blockers Ø Central Acting Adrenergic Antagonists Ø Peripheral Acting Adrenergic Antagonists Ø A-Adrenergic Blockers Ø Vasodilators Ø Angiotensin Inhibitors Ø Calcium Channel Blockers
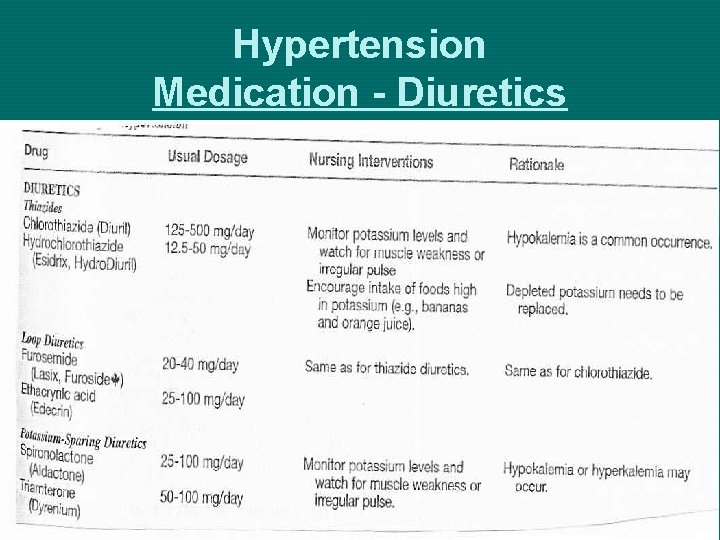
Hypertension Medication - Diuretics
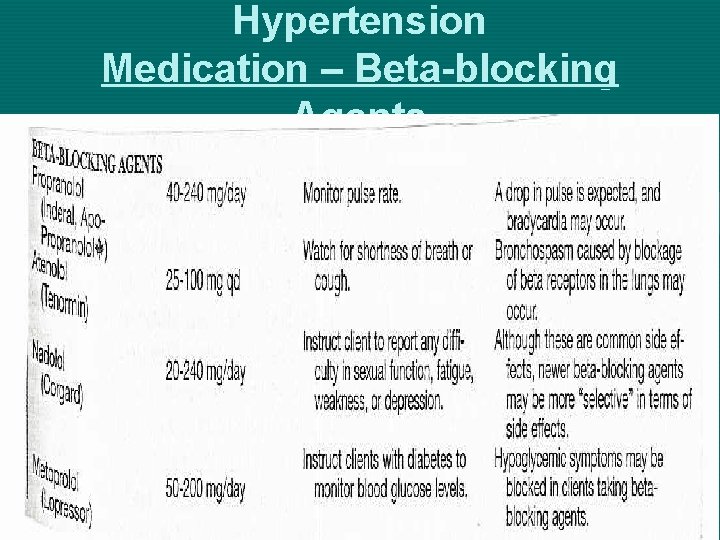
Hypertension Medication – Beta-blocking Agents

Hypertension Medication Calcium Channel Blockers

Hypertension Medication Alpha Agonists & Vasodilators

Hypertension Antihypertensive Drug Therapy
Primary Hypertension Lack of Responsiveness to Therapy Ø Nonadherence to Therapy Ø Drug-Related Causes Ø Associated conditions Ø Secondary Hypertension Ø Volume overload
Primary Hypertension Hypertensive Crisis Ø Definition: Severe & abrupt elevation of BP with diastolic > 120 -130 mm Hg. Ø Causes: ØNonadherence, renovascular changes, preeclampsia, Pheochromocytoma, Rebound from abruptly stopping beta blockers, head injury, necrotizing vasculitis, acute aortic dissection Ø Hypertensive Encephalopathy: Øheadache, N/V, confusion, obtunded, stuporous, seizures, blurred vision, transient blindness
Primary Hypertension Nursing Diagnoses Assess: Cardiovascular status; adherence to therapy; family interaction; risk factor modification? Nsg Action: Supportive & reality-based; Administer meds; referrals; diagnostic preps; ask questions; supportive care during hospitalization for acute crisis Pt/Family Education: Medications; risk factor modification; Community support
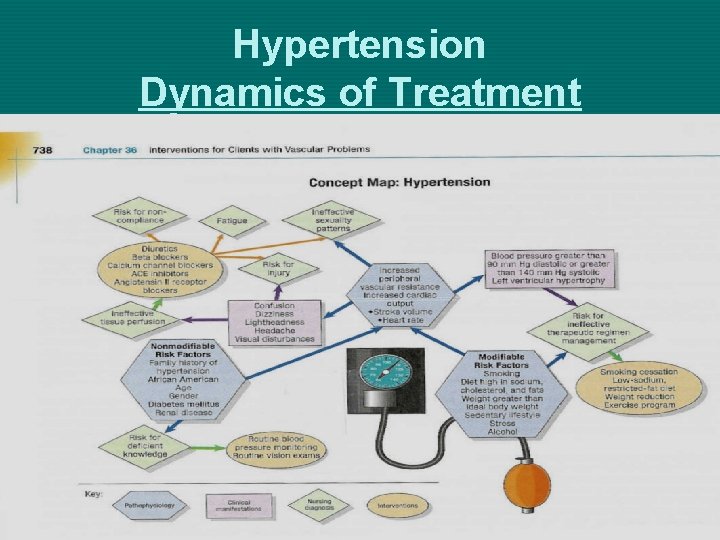
Hypertension Dynamics of Treatment
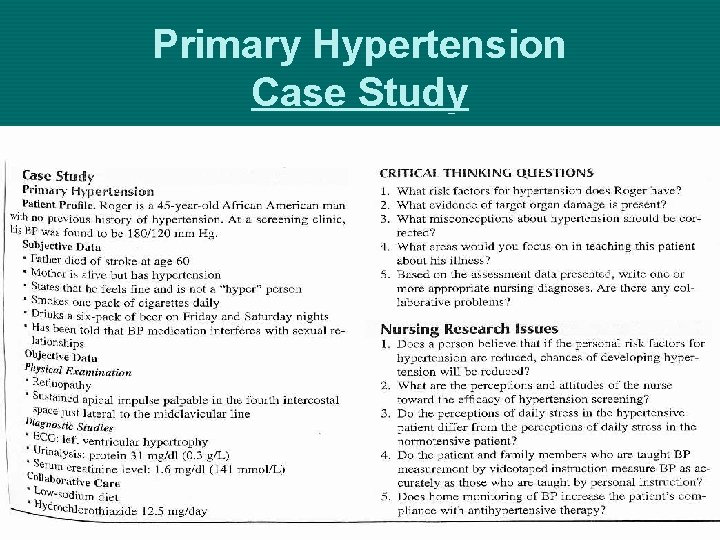
Primary Hypertension Case Study
- Slides: 39