WHITE AND RED LESIONS A white appearance of












- Slides: 33

WHITE AND RED LESIONS
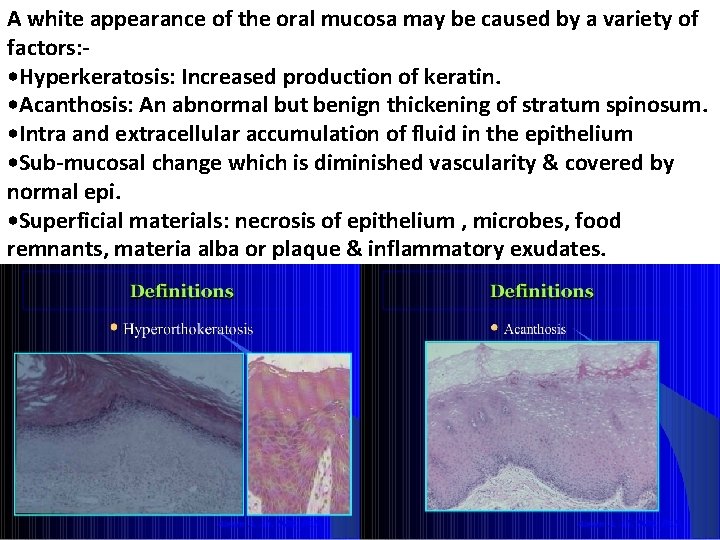
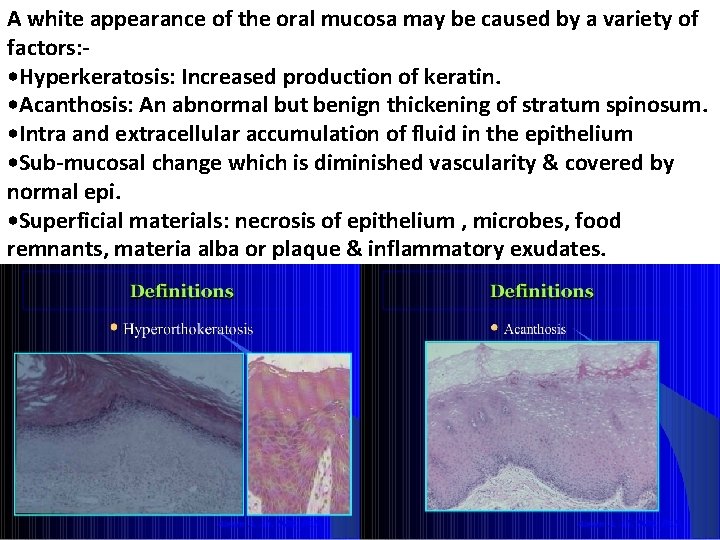
A white appearance of the oral mucosa may be caused by a variety of factors: • Hyperkeratosis: Increased production of keratin. • Acanthosis: An abnormal but benign thickening of stratum spinosum. • Intra and extracellular accumulation of fluid in the epithelium • Sub-mucosal change which is diminished vascularity & covered by normal epi. • Superficial materials: necrosis of epithelium , microbes, food remnants, materia alba or plaque & inflammatory exudates.








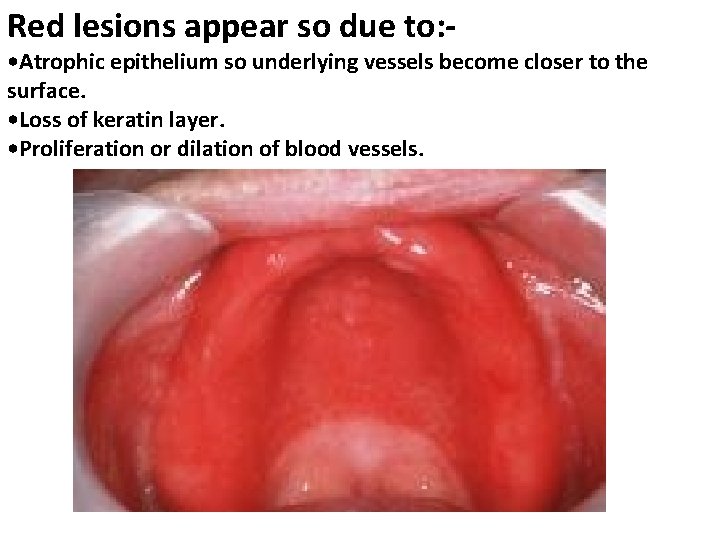
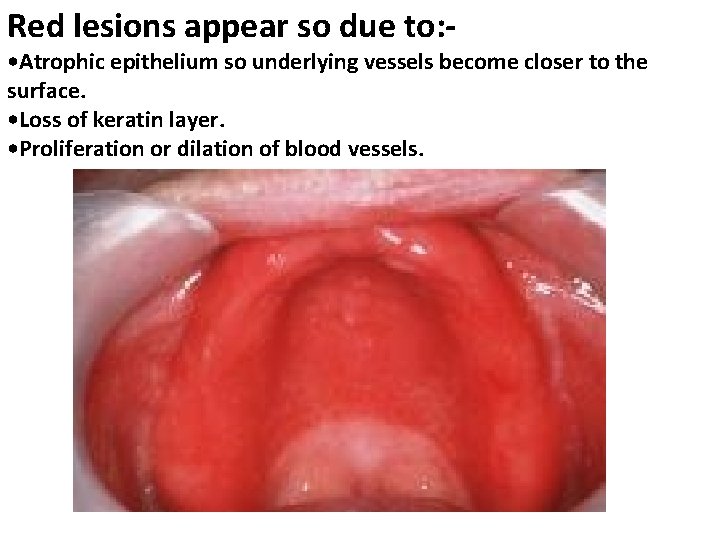
Red lesions appear so due to: - • Atrophic epithelium so underlying vessels become closer to the surface. • Loss of keratin layer. • Proliferation or dilation of blood vessels.
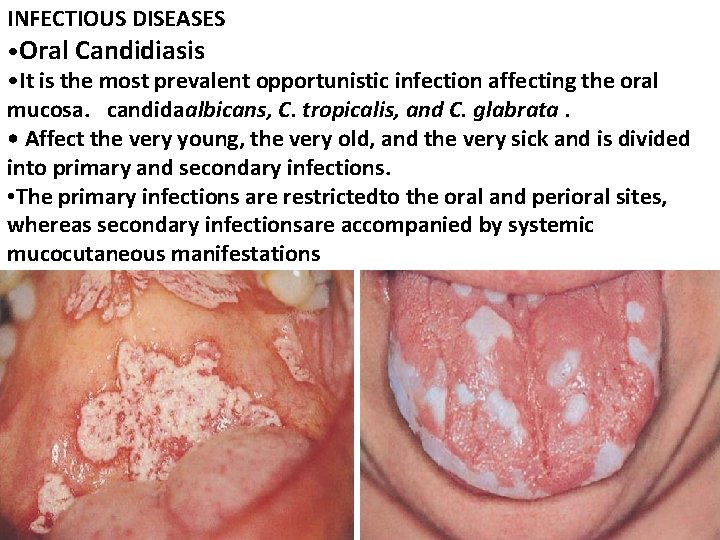
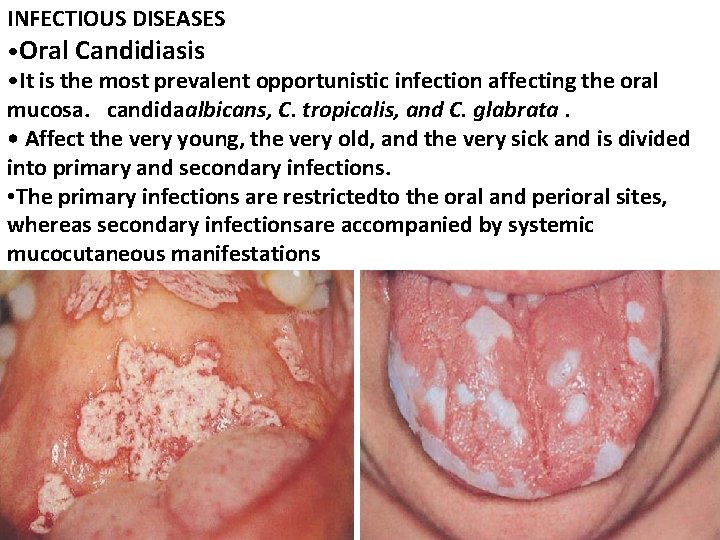
INFECTIOUS DISEASES • Oral Candidiasis • It is the most prevalent opportunistic infection affecting the oral mucosa. candidaalbicans, C. tropicalis, and C. glabrata. • Affect the very young, the very old, and the very sick and is divided into primary and secondary infections. • The primary infections are restrictedto the oral and perioral sites, whereas secondary infectionsare accompanied by systemic mucocutaneous manifestations
Oral hairy leukoplakia(OHL) • Caused by an infection with Epstein-Barr virus (EBV) secondary to immunosuppression. • Its mostly seen in patients with HIV disease then other states of immune deficiencies, • Rarely, individuals with a normal immunesystem may present with OHL.
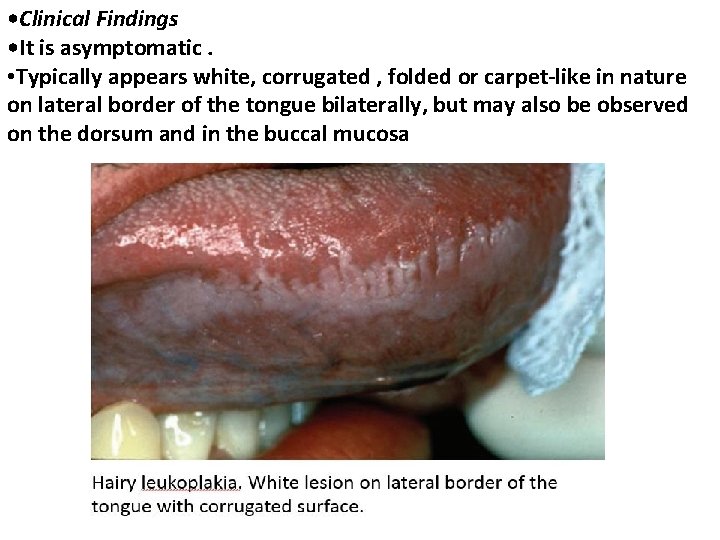
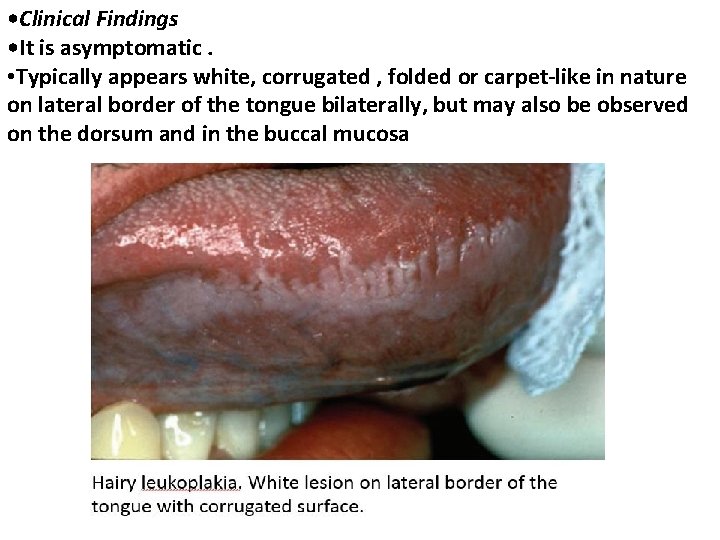
• Clinical Findings • It is asymptomatic. • Typically appears white, corrugated , folded or carpet-like in nature on lateral border of the tongue bilaterally, but may also be observed on the dorsum and in the buccal mucosa
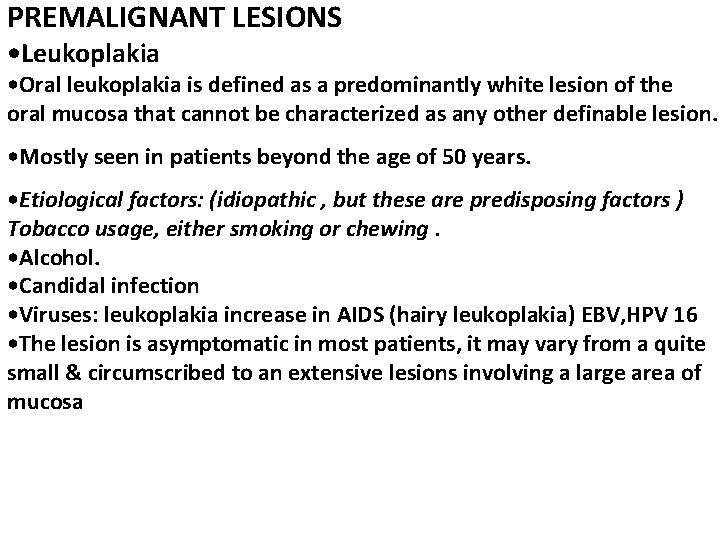
PREMALIGNANT LESIONS • Leukoplakia • Oral leukoplakia is defined as a predominantly white lesion of the oral mucosa that cannot be characterized as any other definable lesion. • Mostly seen in patients beyond the age of 50 years. • Etiological factors: (idiopathic , but these are predisposing factors ) Tobacco usage, either smoking or chewing. • Alcohol. • Candidal infection • Viruses: leukoplakia increase in AIDS (hairy leukoplakia) EBV, HPV 16 • The lesion is asymptomatic in most patients, it may vary from a quite small & circumscribed to an extensive lesions involving a large area of mucosa
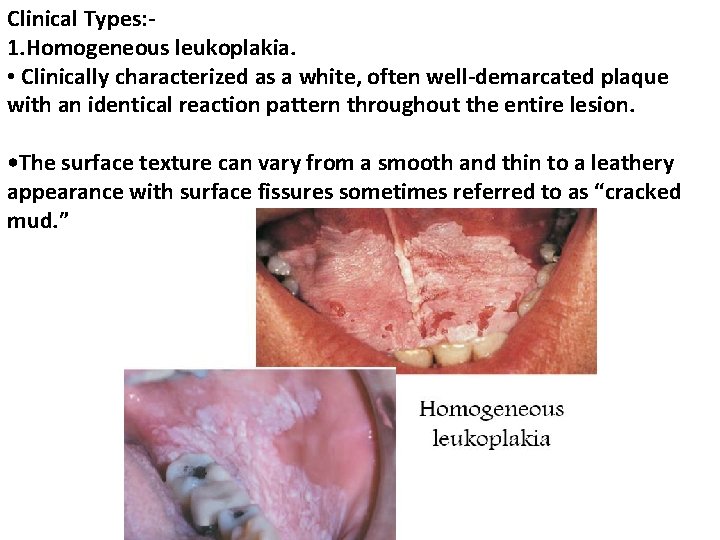
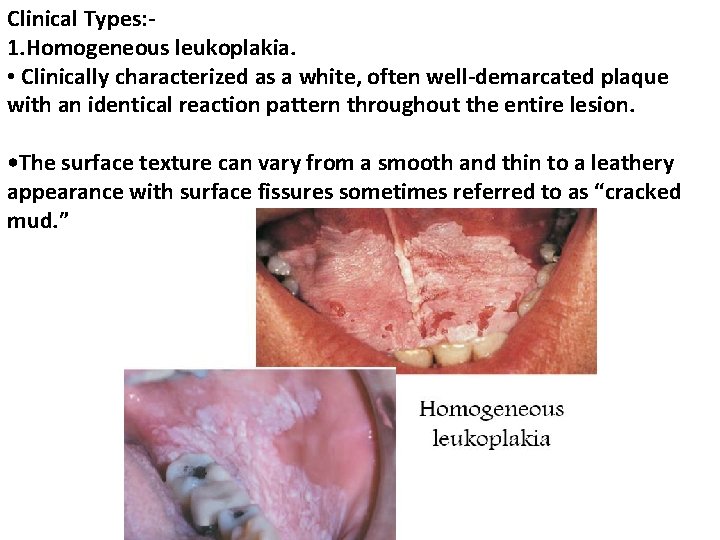
Clinical Types: 1. Homogeneous leukoplakia. • Clinically characterized as a white, often well-demarcated plaque with an identical reaction pattern throughout the entire lesion. • The surface texture can vary from a smooth and thin to a leathery appearance with surface fissures sometimes referred to as “cracked mud. ”
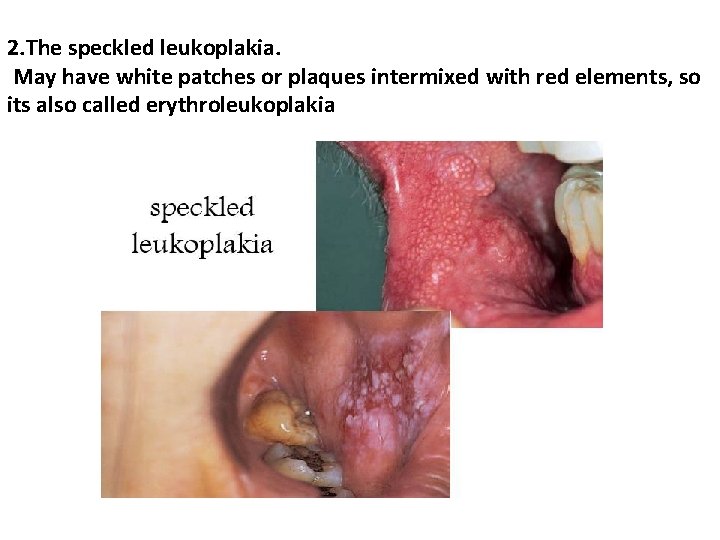
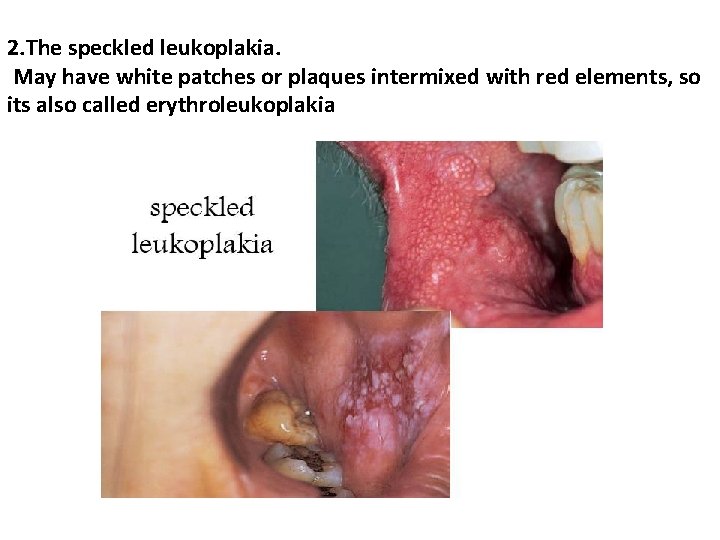
2. The speckled leukoplakia. May have white patches or plaques intermixed with red elements, so its also called erythroleukoplakia
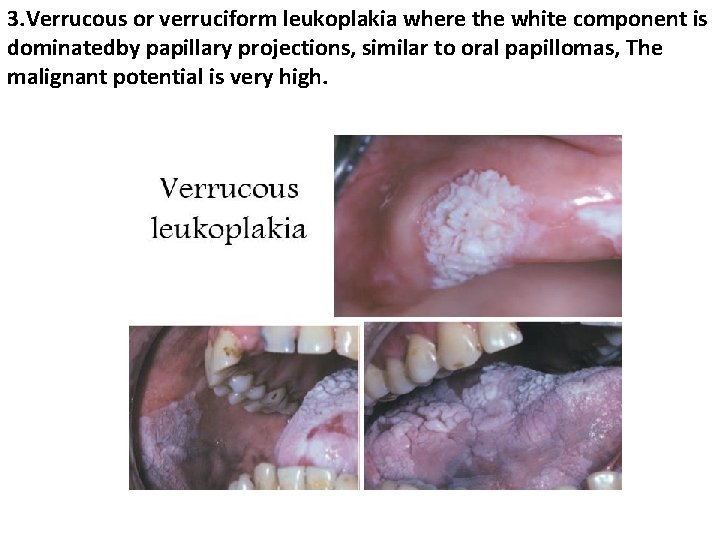
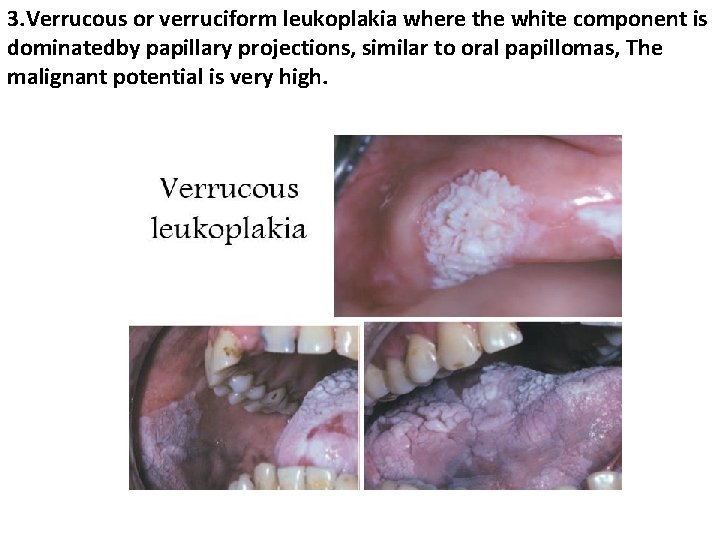
3. Verrucous or verruciform leukoplakia where the white component is dominatedby papillary projections, similar to oral papillomas, The malignant potential is very high.
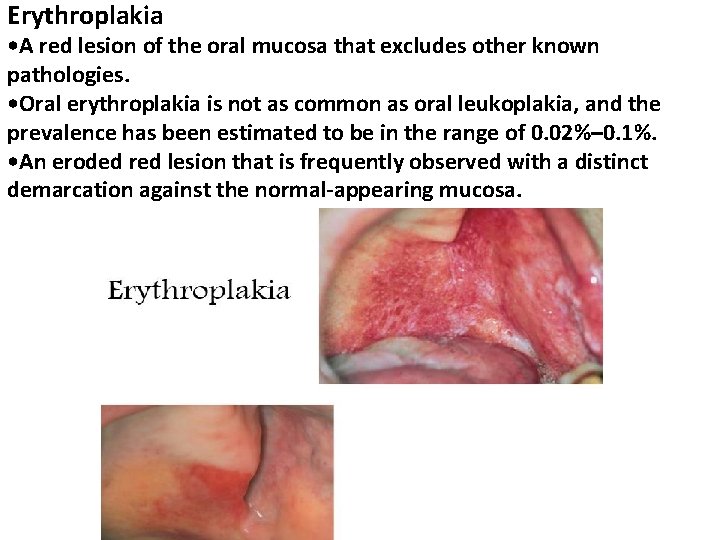
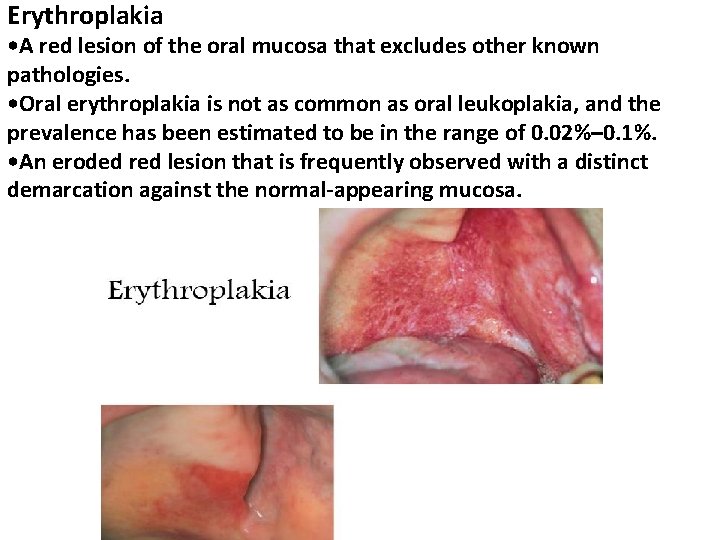
Erythroplakia • A red lesion of the oral mucosa that excludes other known pathologies. • Oral erythroplakia is not as common as oral leukoplakia, and the prevalence has been estimated to be in the range of 0. 02%– 0. 1%. • An eroded red lesion that is frequently observed with a distinct demarcation against the normal-appearing mucosa.
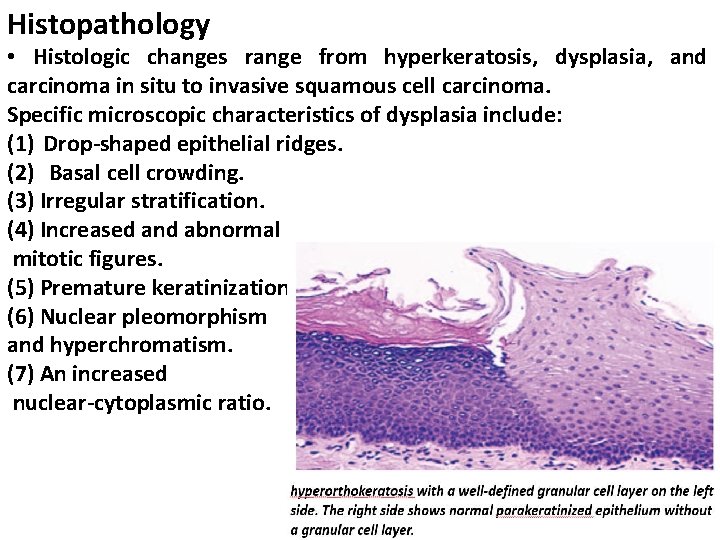
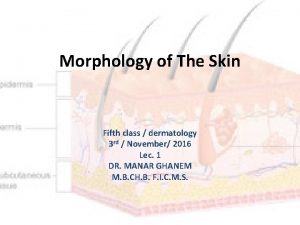
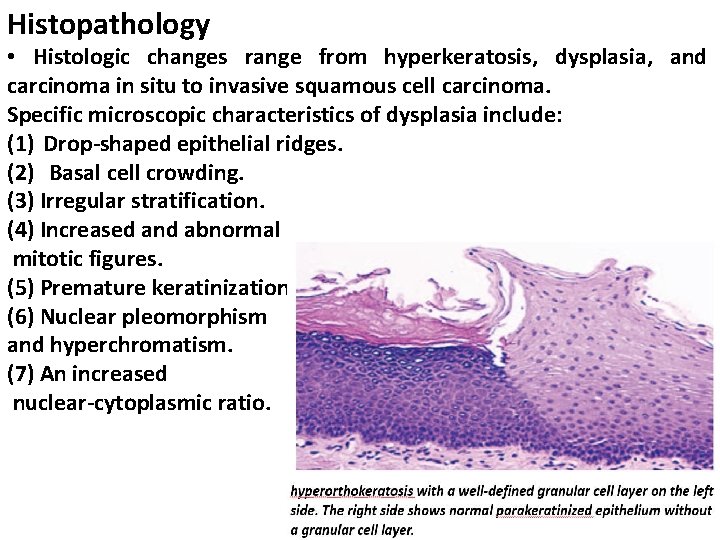
Histopathology • Histologic changes range from hyperkeratosis, dysplasia, and carcinoma in situ to invasive squamous cell carcinoma. Specific microscopic characteristics of dysplasia include: (1) Drop-shaped epithelial ridges. (2) Basal cell crowding. (3) Irregular stratification. (4) Increased and abnormal mitotic figures. (5) Premature keratinization. (6) Nuclear pleomorphism and hyperchromatism. (7) An increased nuclear-cytoplasmic ratio.

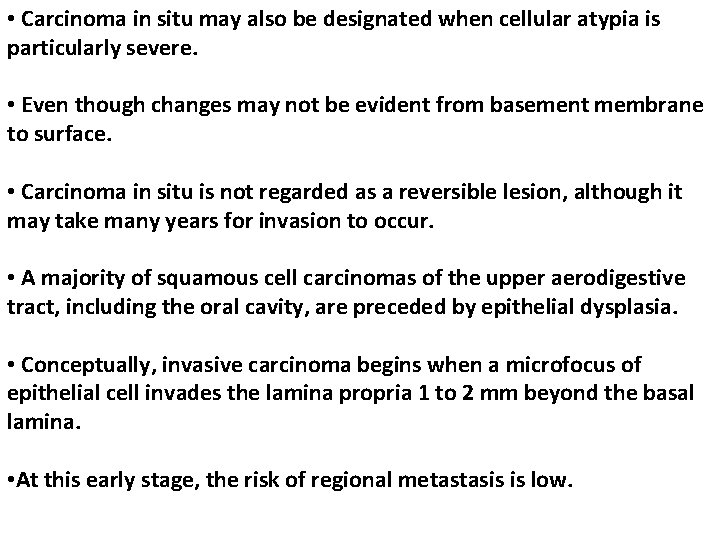
• Carcinoma in situ may also be designated when cellular atypia is particularly severe. • Even though changes may not be evident from basement membrane to surface. • Carcinoma in situ is not regarded as a reversible lesion, although it may take many years for invasion to occur. • A majority of squamous cell carcinomas of the upper aerodigestive tract, including the oral cavity, are preceded by epithelial dysplasia. • Conceptually, invasive carcinoma begins when a microfocus of epithelial cell invades the lamina propria 1 to 2 mm beyond the basal lamina. • At this early stage, the risk of regional metastasis is low.

Treatment and Prognosis: • In the absence of dysplastic or atypical epithelial changes, periodic examination and rebiopsy of new suspicious areas of leukoplakia are recommended. • If a lesion is mildly dysplastic, some clinical judgment should be exercised in patient management. Removal of mildly dysplastic lesions is in the patient’s best interest if no causative factor is apparent and the lesion is small. • If considerable morbidity would result because of the lesion’s size or location, follow-up surveillance is acceptable, provided the degree of epithelial dysplasia is mild. • Surgical excision and other physical forms of ablation are the currently preferred treatment modalities.
IMMUNOPATHOLOGIC DISEASES -Lichenoid Reactions • Lichenoid reactions represent a family of lesions with different etiologies and with a common clinical and histologic appearance. • Oral lichenoid reactions include the following disorders: • Oral lichen planus. • Lichenoid contact reactions. • Lichenoid drug eruptions. • Lichenoid reactions of graft-versus-host disease (GVHD).
Oral lichen planus • It is a chronic inflammatory disease of skin & mucous membrane. • It mainly affects patients of middle age or over, especially women. • It is relatively common and if untreated can persist for many years. • Etiology and Pathogensis • The etiology of OLP is not known, but recently it has become evident that the immune system has a primary role in the development of this disease through T-lymphocyte cytotoxicity directed against antigens expressed by the basal cell layer.
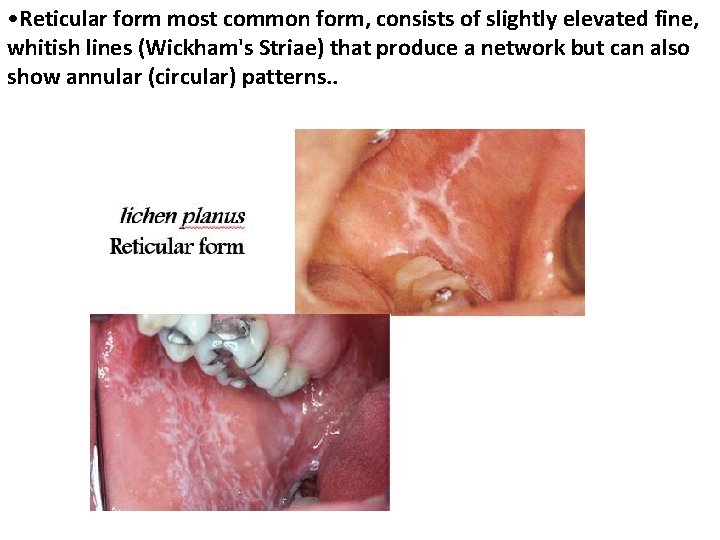
This inflammatory process may be triggered by: 1. Stress. 2. Hepatitis C virus. 3. Systemic disease like diabetes mellitus and rheumatoid arthritis. Clinical types 1. Reticular type 2. Papular type 3. Plaque-like type 4. Bullous 5. Erythematous type 6. Ulcerative type
• The most frequently affected areas are the buccal mucosa particularly posteriorly but the lesions may spread forward almost to the commissures. • The next most common site is the tongue, the lip, palate & gingiva. • The lesions are very often symmetrical, but in some cases are more prominent on one side than another. • Malignant transformation less than 1% it has been suggested and the ulcerative from more likely to undergo such change.
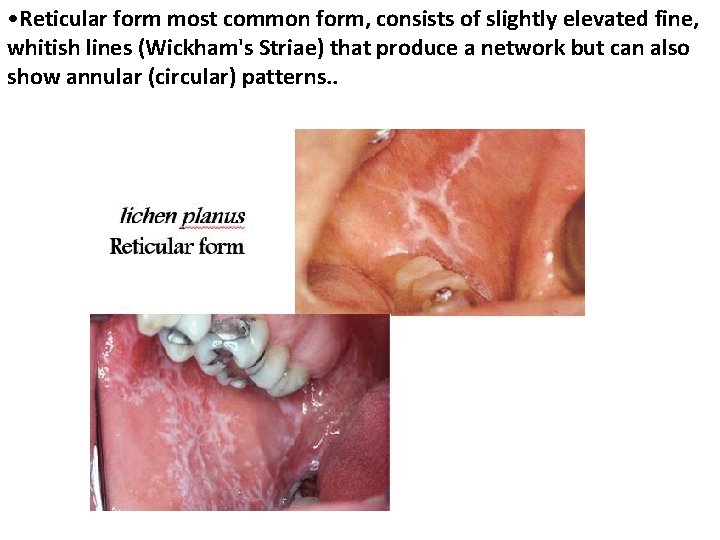
• Reticular form most common form, consists of slightly elevated fine, whitish lines (Wickham's Striae) that produce a network but can also show annular (circular) patterns. .
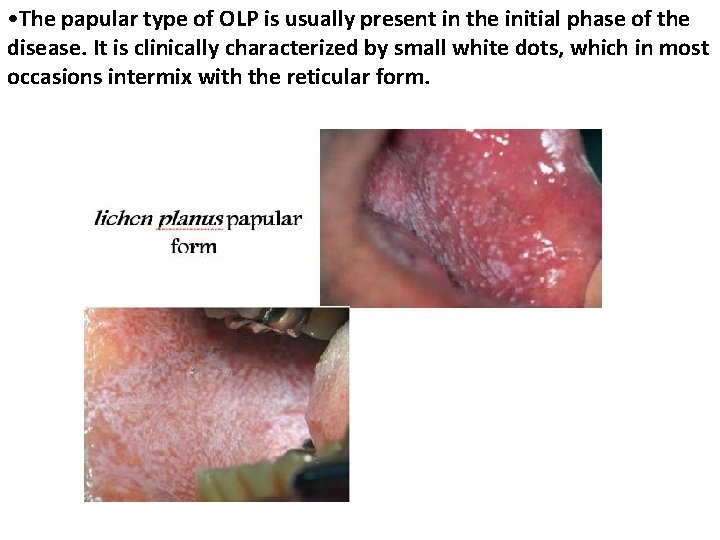
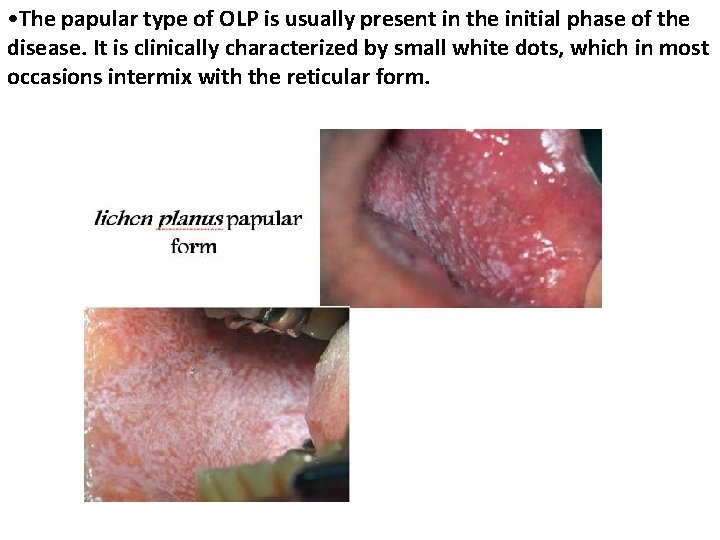
• The papular type of OLP is usually present in the initial phase of the disease. It is clinically characterized by small white dots, which in most occasions intermix with the reticular form.
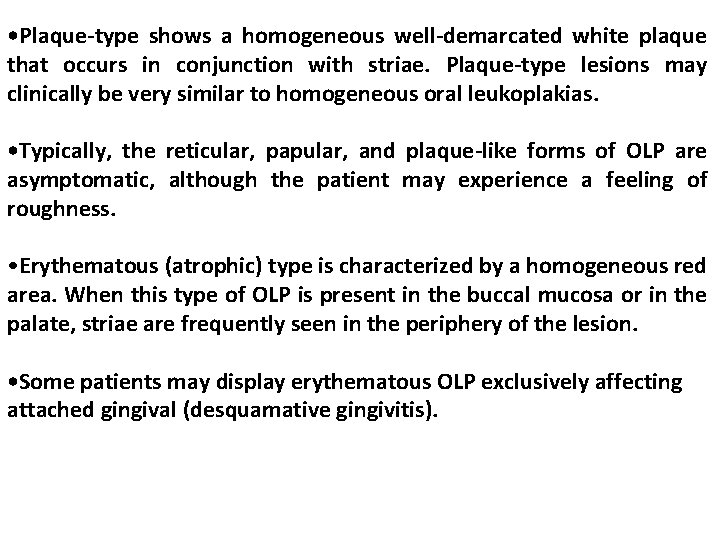
• Plaque-type shows a homogeneous well-demarcated white plaque that occurs in conjunction with striae. Plaque-type lesions may clinically be very similar to homogeneous oral leukoplakias. • Typically, the reticular, papular, and plaque-like forms of OLP are asymptomatic, although the patient may experience a feeling of roughness. • Erythematous (atrophic) type is characterized by a homogeneous red area. When this type of OLP is present in the buccal mucosa or in the palate, striae are frequently seen in the periphery of the lesion. • Some patients may display erythematous OLP exclusively affecting attached gingival (desquamative gingivitis).

desquamative gingivitis
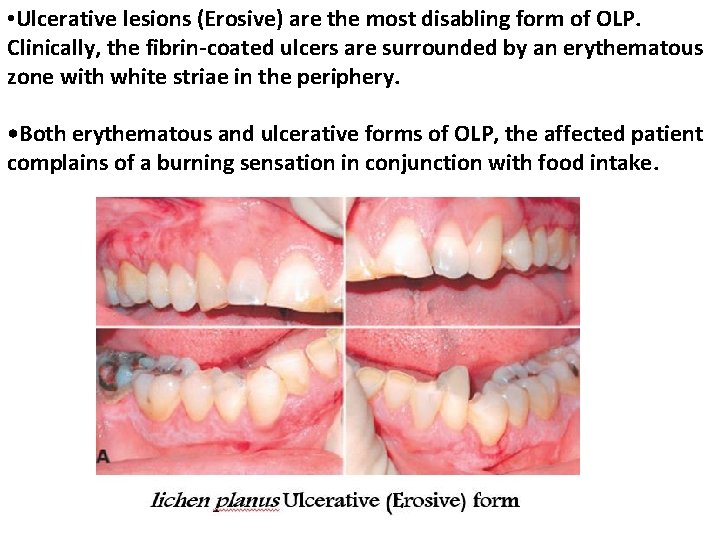
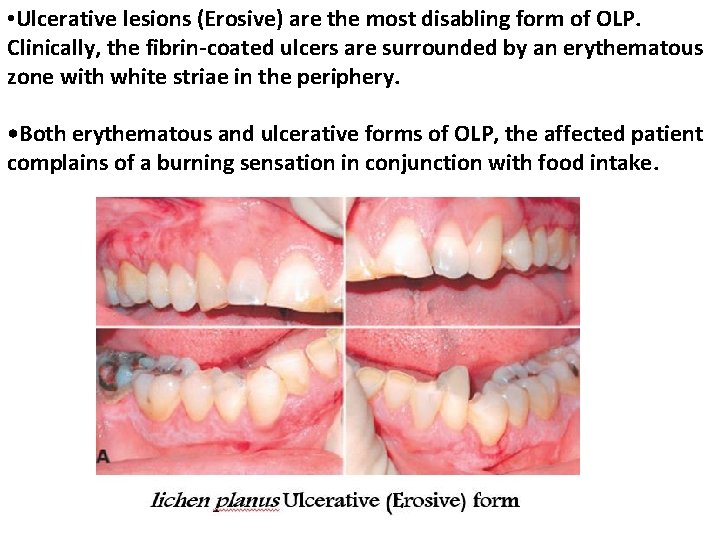
• Ulcerative lesions (Erosive) are the most disabling form of OLP. Clinically, the fibrin-coated ulcers are surrounded by an erythematous zone with white striae in the periphery. • Both erythematous and ulcerative forms of OLP, the affected patient complains of a burning sensation in conjunction with food intake.
 White appearance
White appearance Scattered white matter lesions
Scattered white matter lesions Site:slidetodoc.com
Site:slidetodoc.com Site:slidetodoc.com
Site:slidetodoc.com Orange green blue
Orange green blue Pustule
Pustule Optic tract lesions
Optic tract lesions Pyramidal tract vs extrapyramidal tract
Pyramidal tract vs extrapyramidal tract Describing skin lesions
Describing skin lesions Epidermoid carcinoma
Epidermoid carcinoma Olneys lesions
Olneys lesions Pyramidal vs extrapyramidal
Pyramidal vs extrapyramidal Caries on lingual surfaces of maxillary incisors
Caries on lingual surfaces of maxillary incisors Nature lésions
Nature lésions Dont touch lesion
Dont touch lesion Vagus nerve lesion
Vagus nerve lesion Oral pathology
Oral pathology Pr��ca projektov�� mana����r
Pr��ca projektov�� mana����r Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Definition of periradicular disease
Definition of periradicular disease Med
Med Eye lesions
Eye lesions Lésions
Lésions Vesiculobullous lesions
Vesiculobullous lesions A red red rose
A red red rose Both artists use exaggeration to emphasize
Both artists use exaggeration to emphasize Red white and blue chair
Red white and blue chair The yellow colour of asean flag symbolizes
The yellow colour of asean flag symbolizes Red blood cells and white blood cells difference
Red blood cells and white blood cells difference Lymph tissue fluid
Lymph tissue fluid Red white and blue tortilla chips
Red white and blue tortilla chips Red eyed female and white eyed male
Red eyed female and white eyed male Hydrostatic equilibrium
Hydrostatic equilibrium Aksum had access to the red sea blue nile and white nile
Aksum had access to the red sea blue nile and white nile