Practical dementia assessment Walking with the patient through
- Slides: 36
Practical dementia assessment Walking with the patient through the memory clinic process With tangents into theory Dr Ross Dunne
Learning objectives • To know the subtypes of dementia – And to know the red flags for each • To understand the clinical assessment • To understand the use of neuroimaging • To understand the use of pen and paper tests
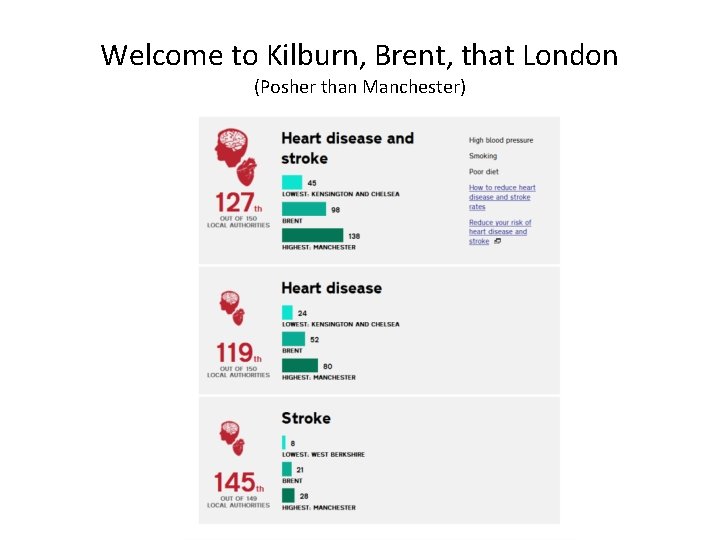
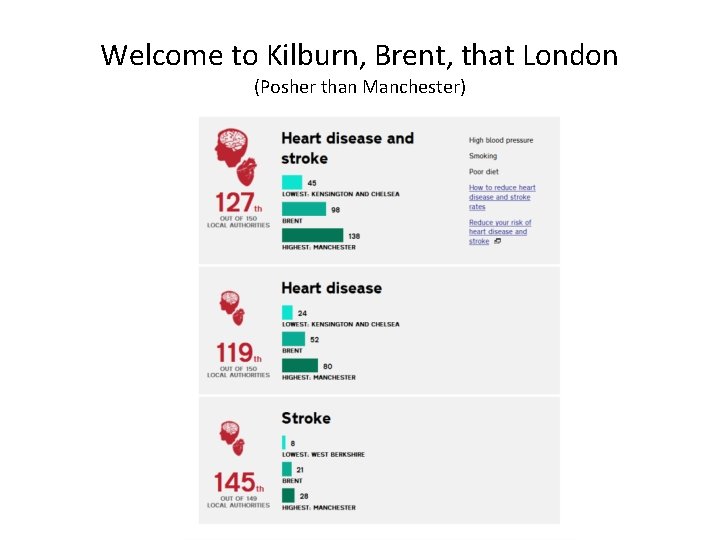
Welcome to Kilburn, Brent, that London (Posher than Manchester)
Meet Maria • 77 year old Irish lady with the following medical history – Osteoarthritis – COPD – Childhood TB – Ex smoker (30 py) – Never drinker
Meet Maria • Attends with her daughter • Maria does not think anything is wrong but has been cajoled into being there • Daughter reports Maria has become gradually and progressively more forgetful over 12 months. • Family only realised when son in California came home for Christmas and mentioned how “bad” mum was. • When they really thought about it, they noticed some changes as early as 18 months ago.
Meet Maria • Maria, says they’re fussing over nothing • “Just my age” doctor • Doesn’t recognise that she has forgotten appointments, times, dates. • Doesn’t recognise that she has difficulty with the washing machine • Does recognise some frustration with names but “I have twenty grandchildren doctor”.
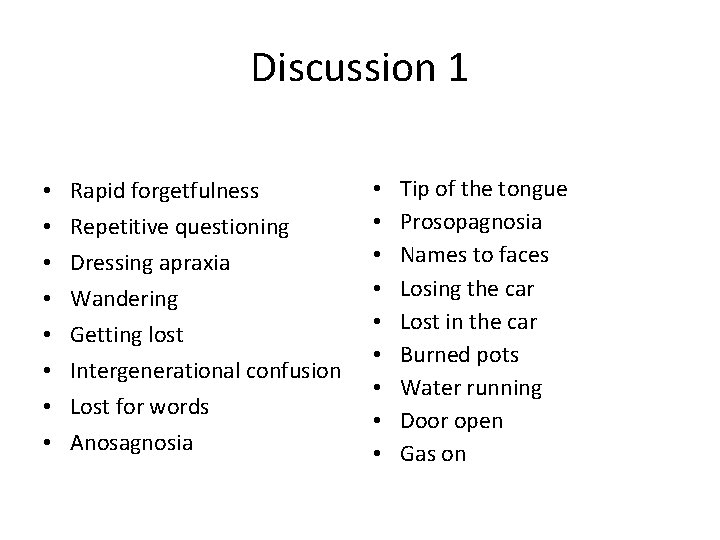
Discussion 1 • What would you ask about?
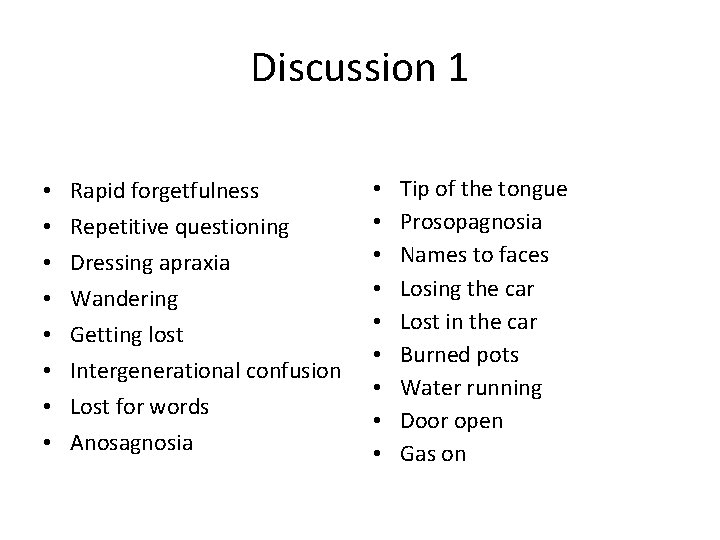
Discussion 1 • • Rapid forgetfulness Repetitive questioning Dressing apraxia Wandering Getting lost Intergenerational confusion Lost for words Anosagnosia • • • Tip of the tongue Prosopagnosia Names to faces Losing the car Lost in the car Burned pots Water running Door open Gas on
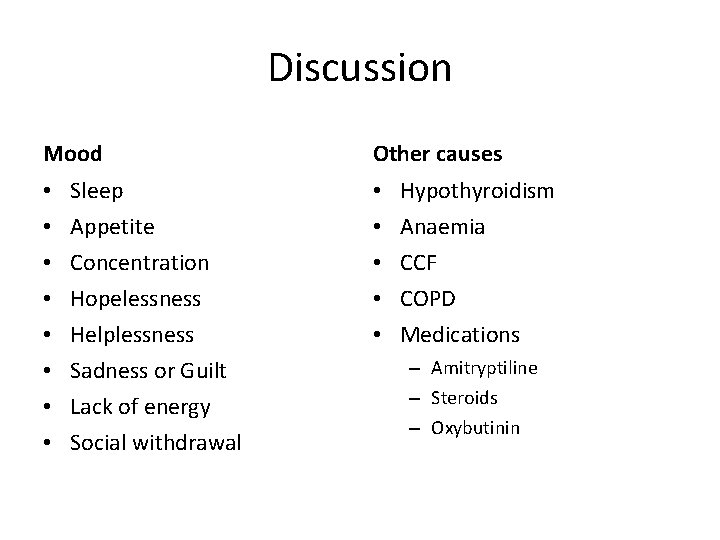
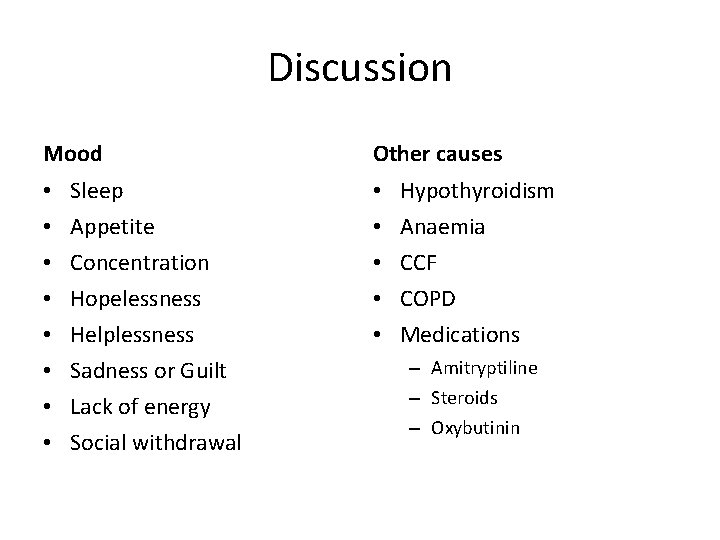
Discussion Mood • • Sleep Appetite Concentration Hopelessness Helplessness Sadness or Guilt Lack of energy Social withdrawal Other causes • • • Hypothyroidism Anaemia CCF COPD Medications – Amitryptiline – Steroids – Oxybutinin
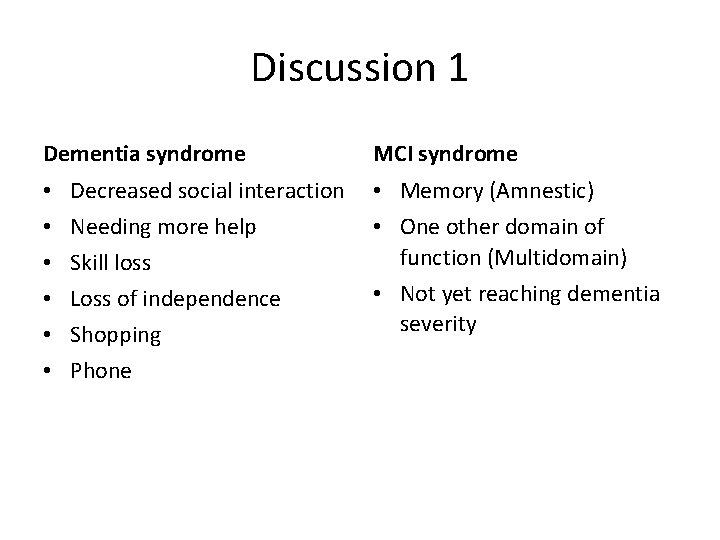
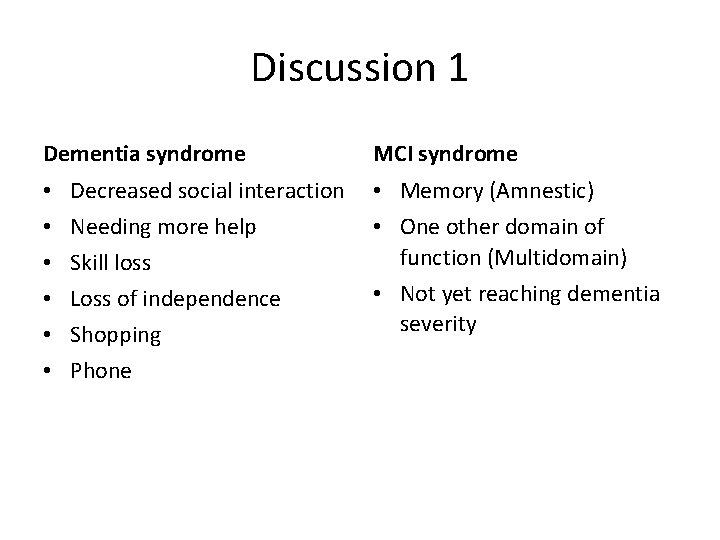
Discussion 1 Dementia syndrome • • • Decreased social interaction Needing more help Skill loss Loss of independence Shopping Phone MCI syndrome • Memory (Amnestic) • One other domain of function (Multidomain) • Not yet reaching dementia severity
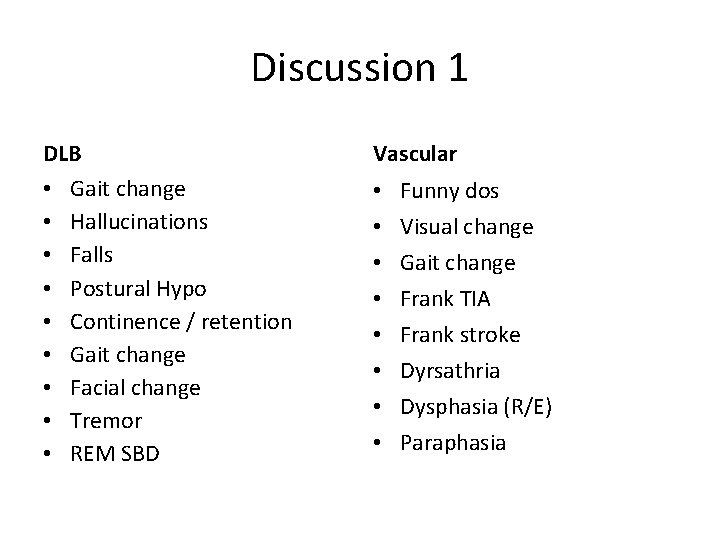
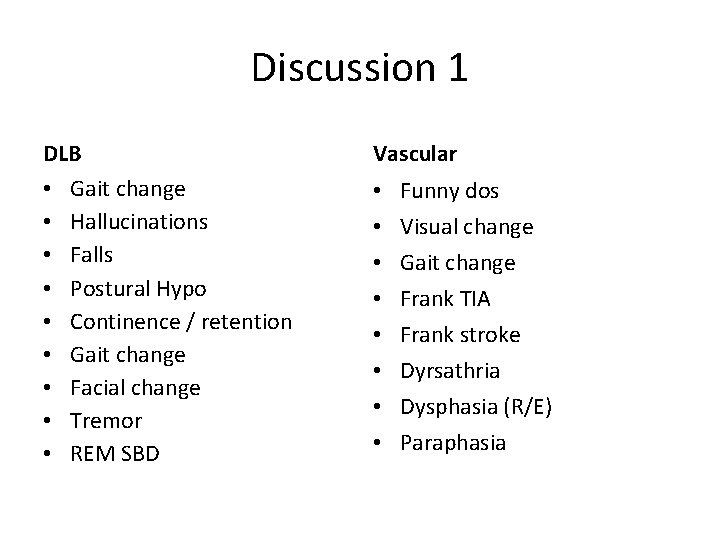
Discussion 1 DLB • Gait change • Hallucinations • Falls • Postural Hypo • Continence / retention • Gait change • Facial change • Tremor • REM SBD Vascular • • Funny dos Visual change Gait change Frank TIA Frank stroke Dyrsathria Dysphasia (R/E) Paraphasia
Alzheimer Disease
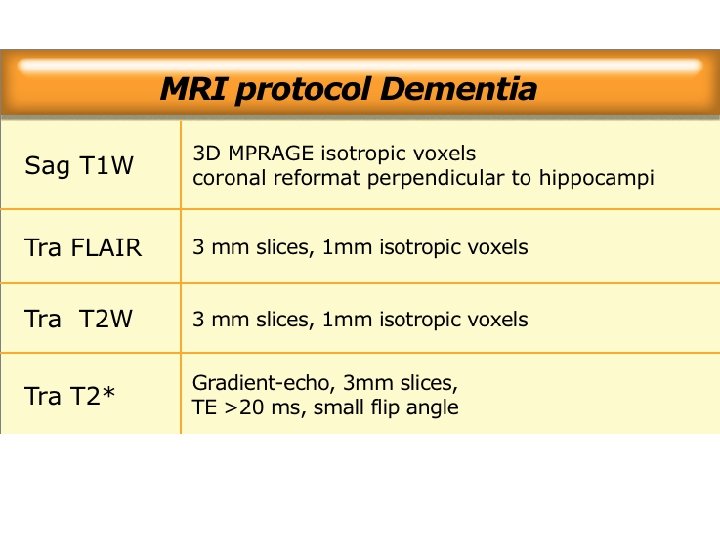
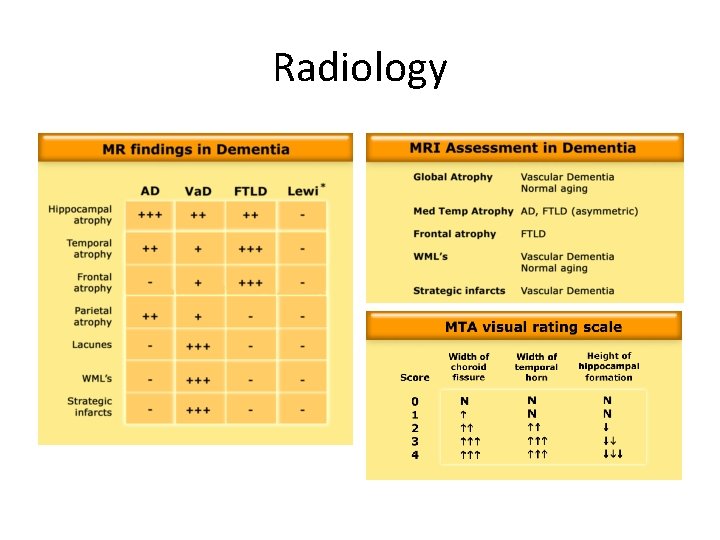
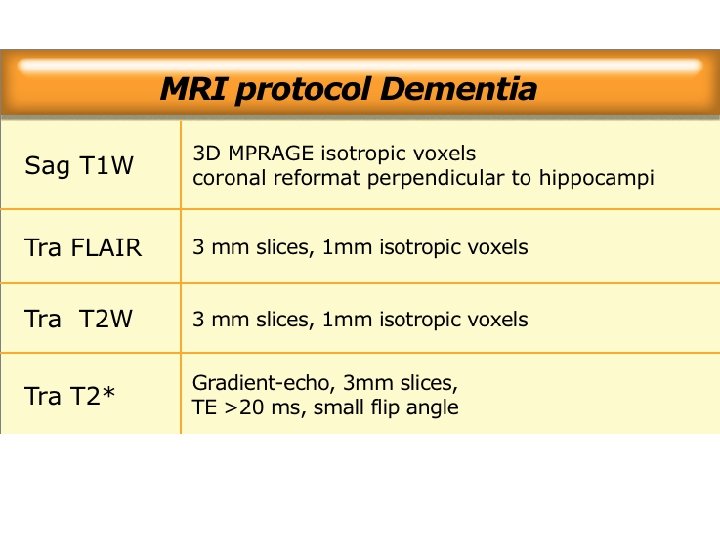
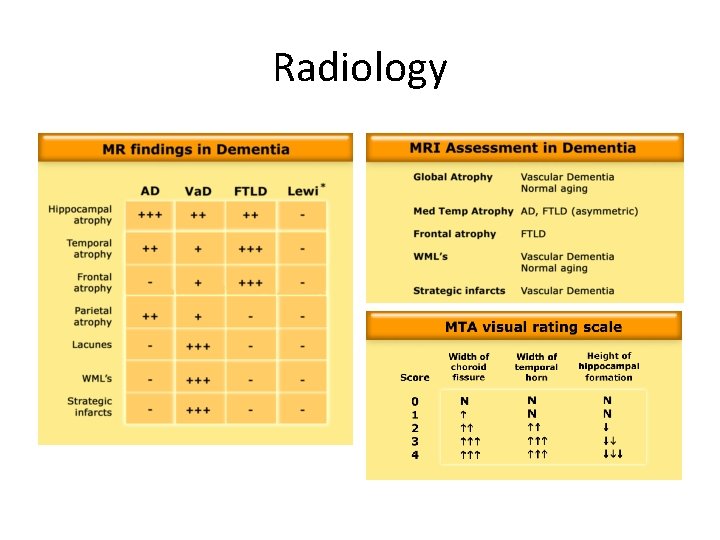
Radiology
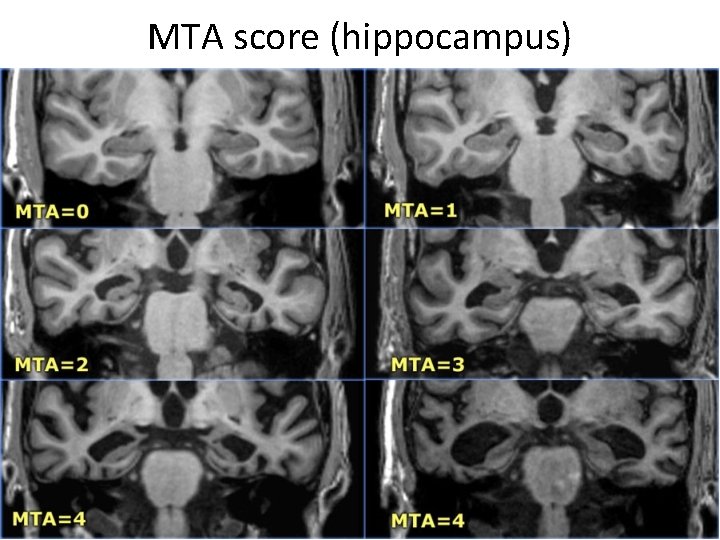
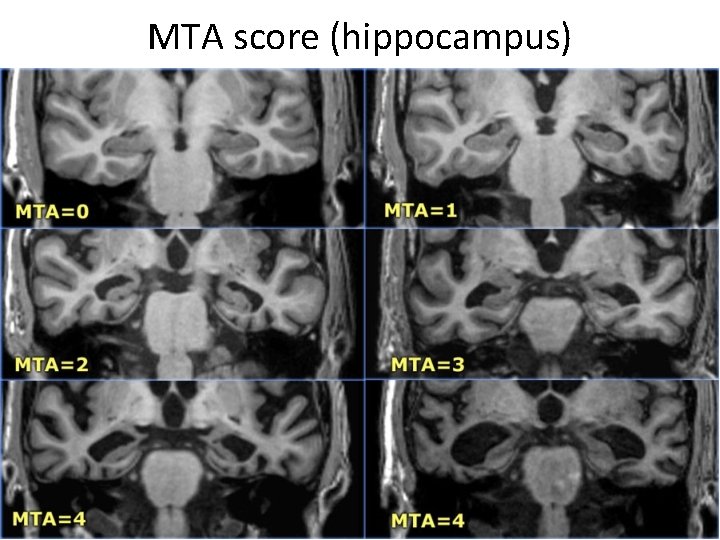
MTA score (hippocampus)
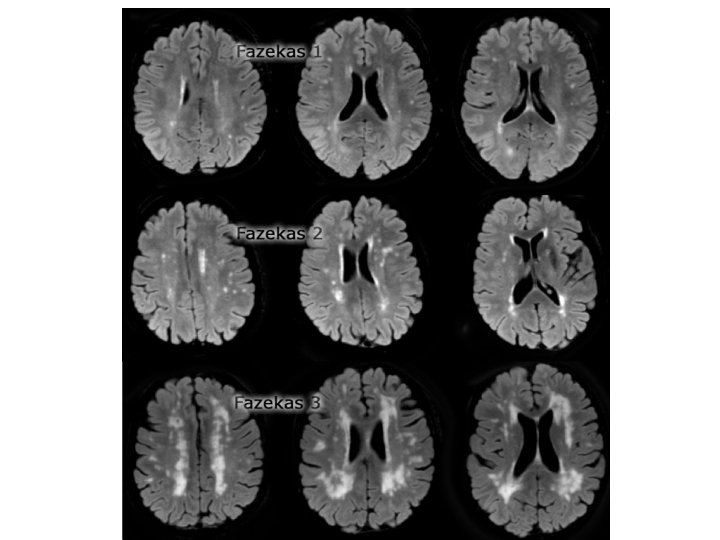
• Fazekas 1 is considered normal in the elderly. Fazekas 2 and 3 are pathologic, but may be seen in normally functioning individuals. They are however, at high risk for disability. • In 600 normally functioning elderly people the Fazekas score predicted disability within one year (table). In the Fazekas 3 group 25% was disabled within one year • Three year follow-up shows that severe white matter changes independently and strongly predict rapid global functional decline.
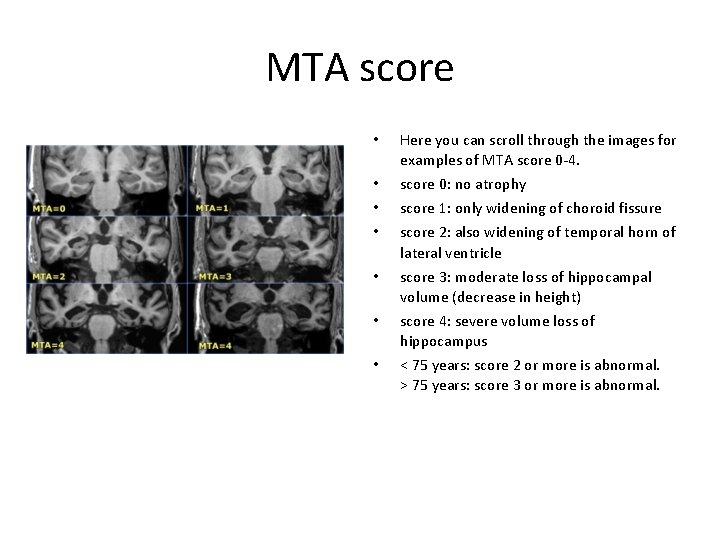
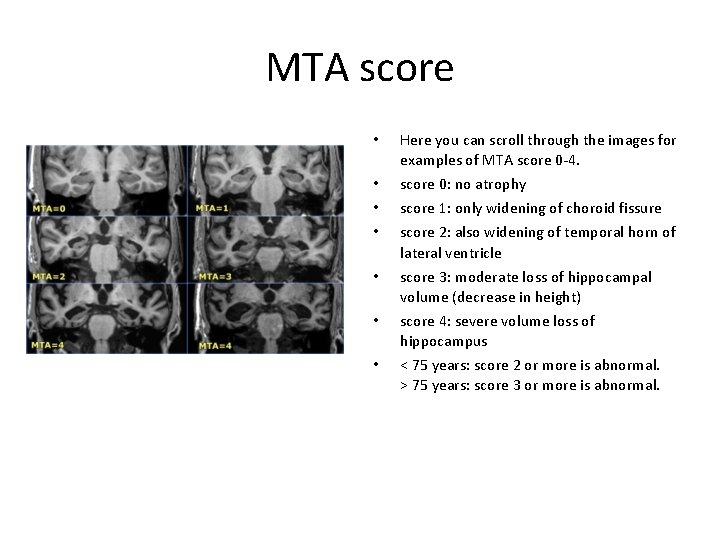
MTA score • • Here you can scroll through the images for examples of MTA score 0 -4. score 0: no atrophy score 1: only widening of choroid fissure score 2: also widening of temporal horn of lateral ventricle score 3: moderate loss of hippocampal volume (decrease in height) score 4: severe volume loss of hippocampus < 75 years: score 2 or more is abnormal. > 75 years: score 3 or more is abnormal.
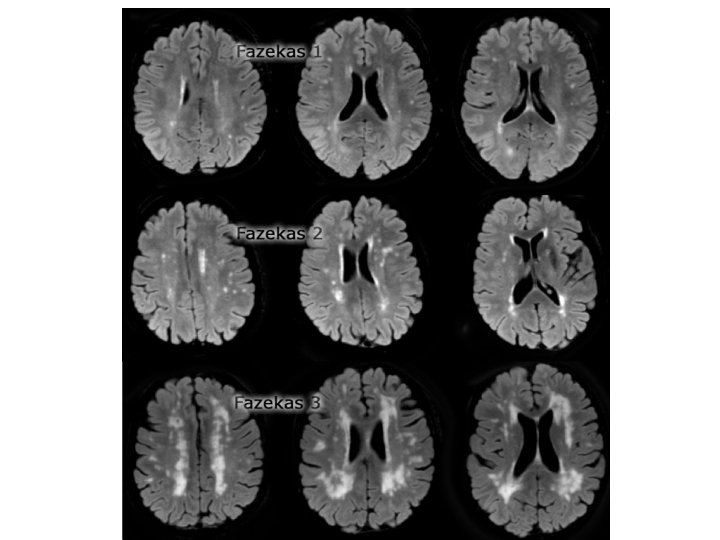
Fazekas score
Neuropsychology • The art of triangulating pathology in the brain using pen and paper tasks which examine overlapping functions. • Visuospatial • Memory • Attention & Concentration • Language – Naming – Semantics
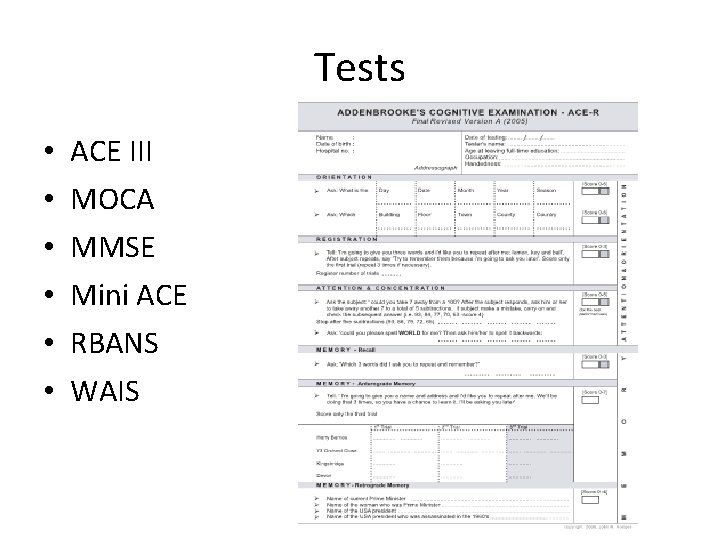
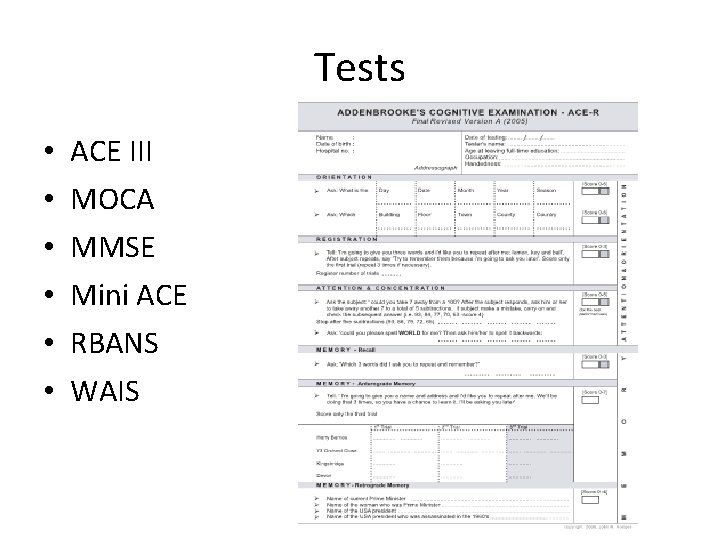
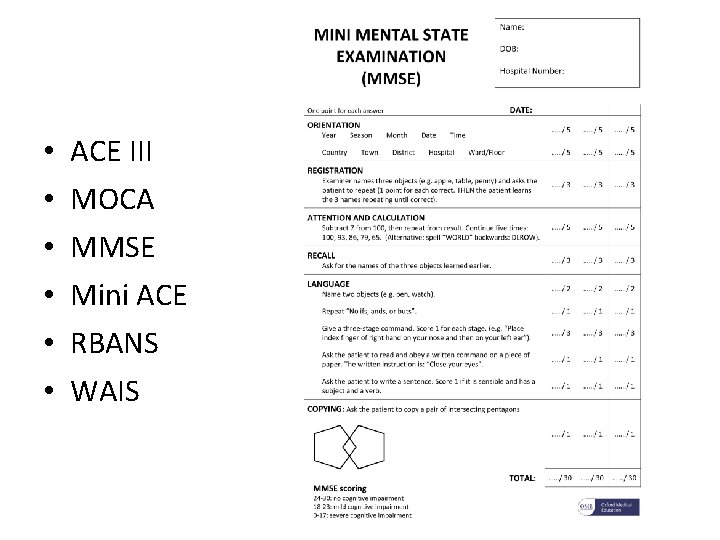
Tests • • • ACE III MOCA MMSE Mini ACE RBANS WAIS
Tests • • • ACE III MOCA MMSE Mini ACE RBANS WAIS
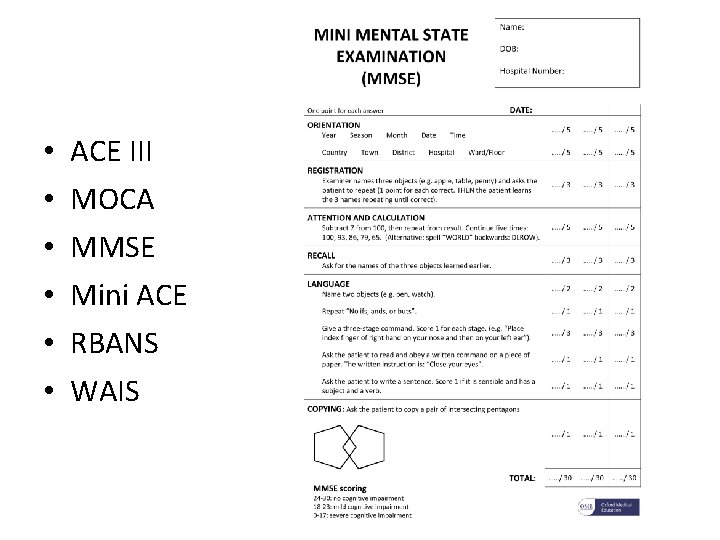
Tests • • • ACE III MOCA MMSE Mini ACE RBANS WAIS
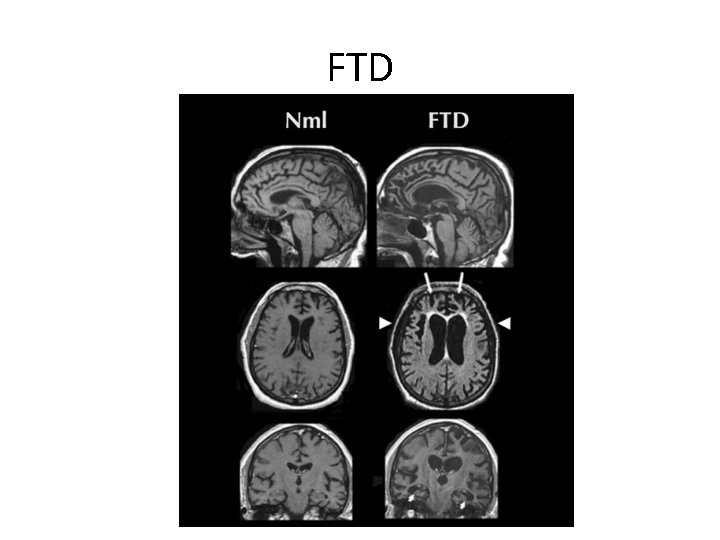
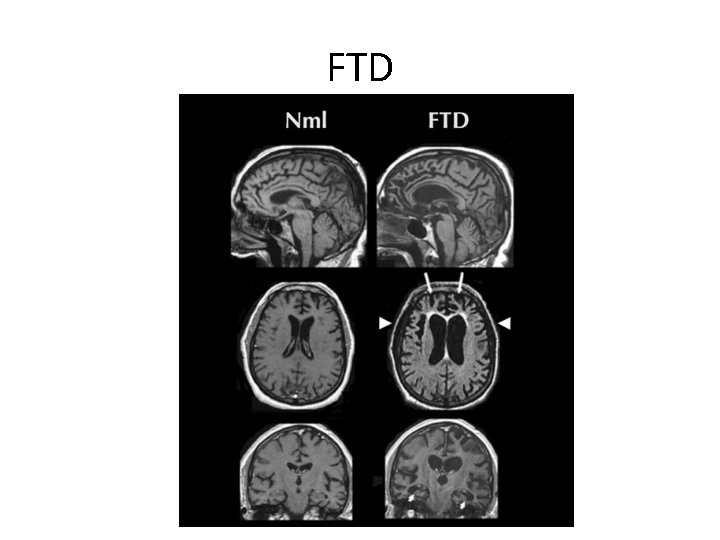
FTD
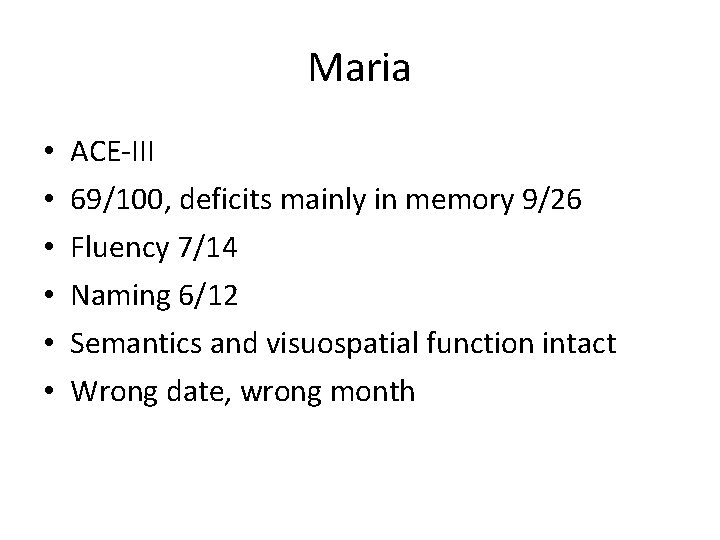
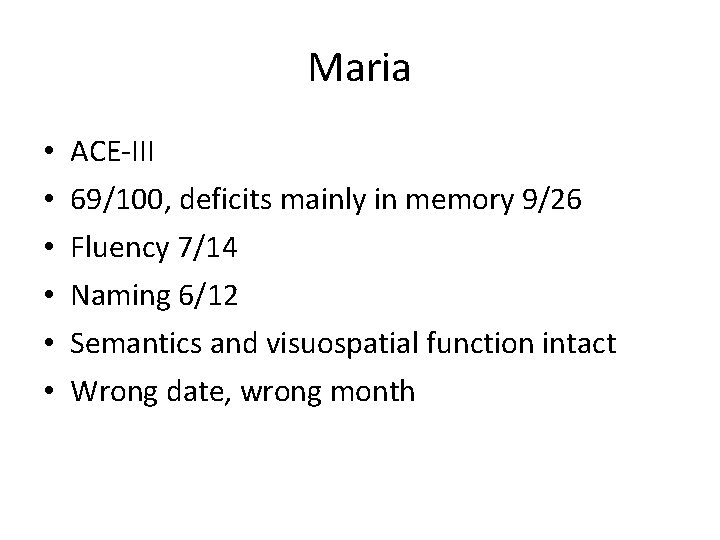
Maria • • • ACE-III 69/100, deficits mainly in memory 9/26 Fluency 7/14 Naming 6/12 Semantics and visuospatial function intact Wrong date, wrong month
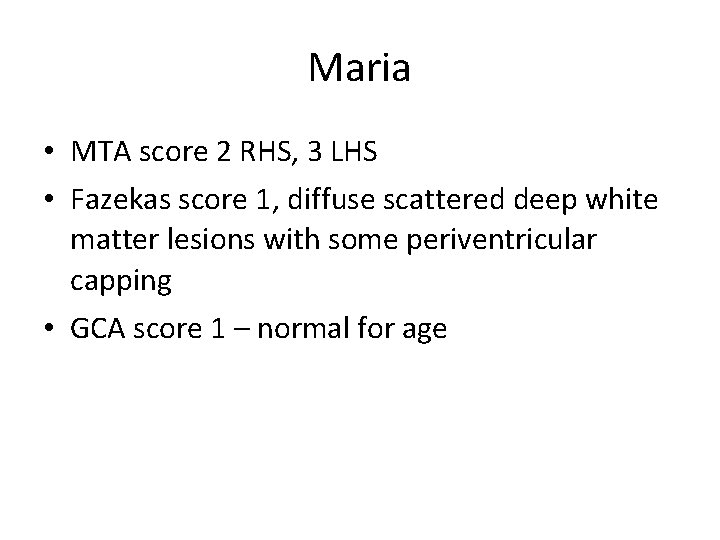
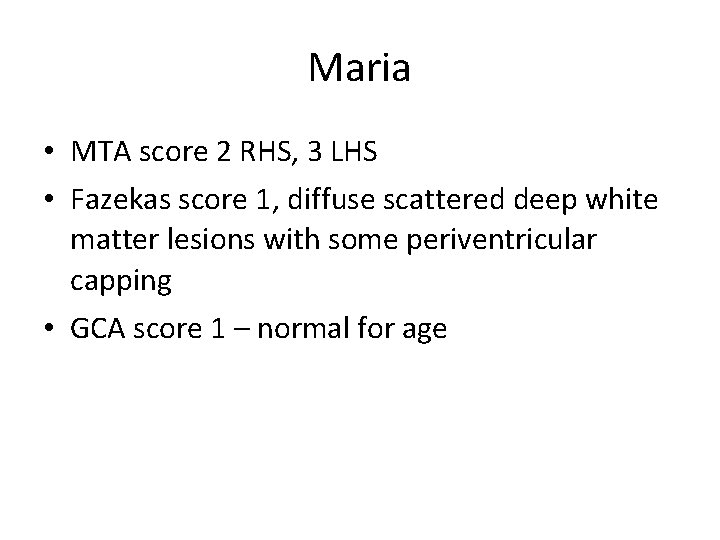
Maria • MTA score 2 RHS, 3 LHS • Fazekas score 1, diffuse scattered deep white matter lesions with some periventricular capping • GCA score 1 – normal for age
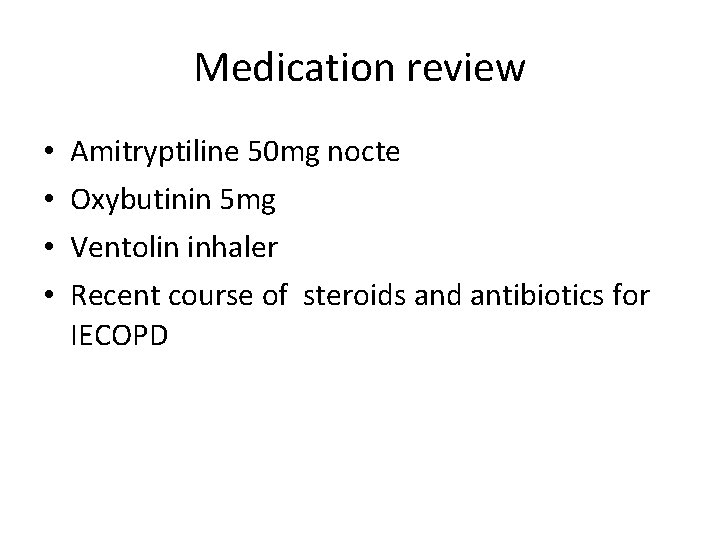
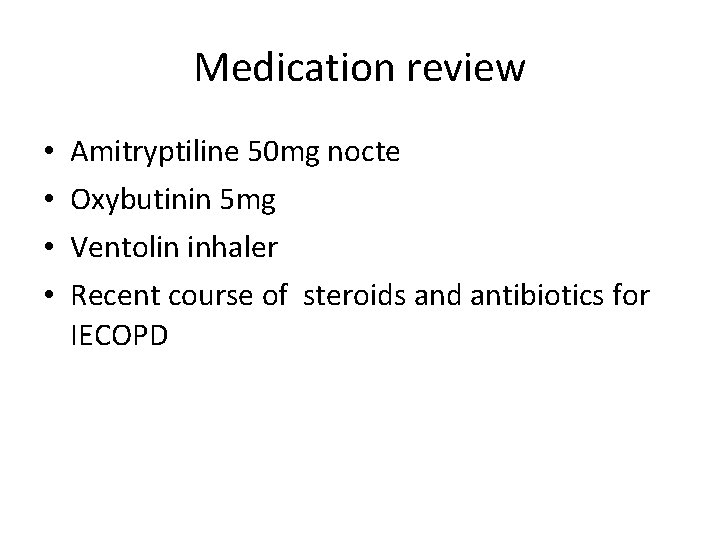
Medication review • • Amitryptiline 50 mg nocte Oxybutinin 5 mg Ventolin inhaler Recent course of steroids and antibiotics for IECOPD
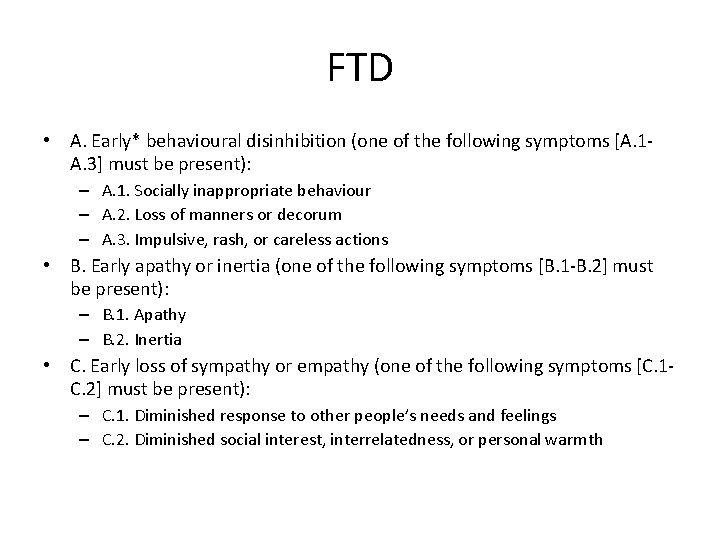
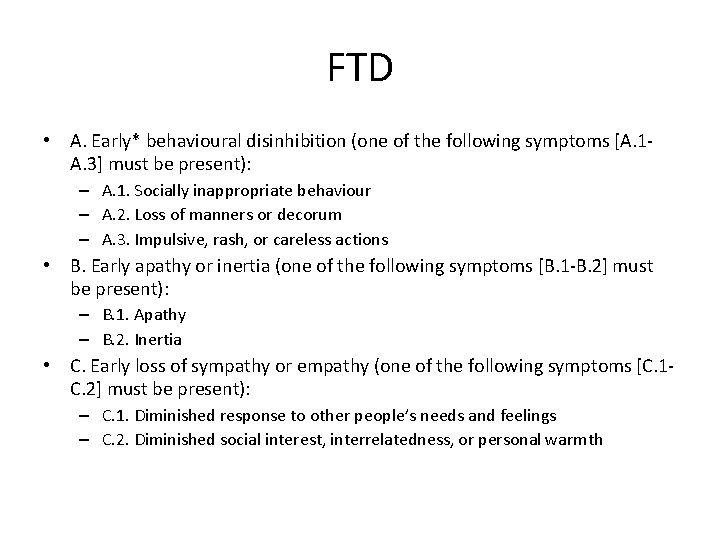
FTD • A. Early* behavioural disinhibition (one of the following symptoms [A. 1 A. 3] must be present): – A. 1. Socially inappropriate behaviour – A. 2. Loss of manners or decorum – A. 3. Impulsive, rash, or careless actions • B. Early apathy or inertia (one of the following symptoms [B. 1 -B. 2] must be present): – B. 1. Apathy – B. 2. Inertia • C. Early loss of sympathy or empathy (one of the following symptoms [C. 1 C. 2] must be present): – C. 1. Diminished response to other people’s needs and feelings – C. 2. Diminished social interest, interrelatedness, or personal warmth
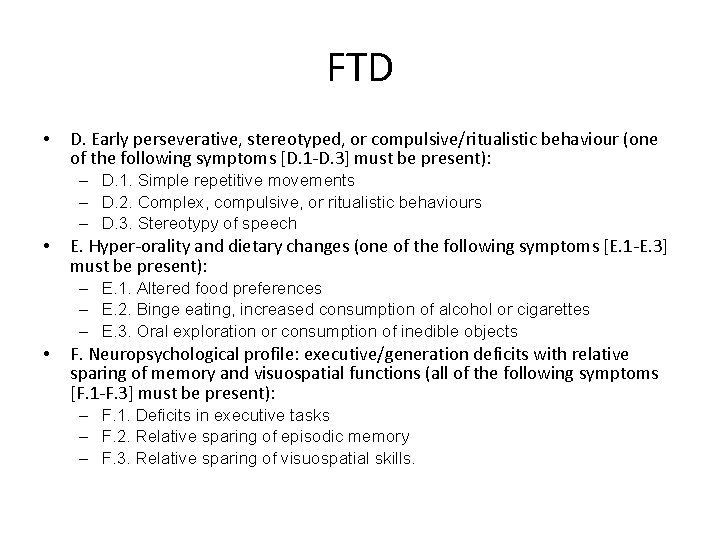
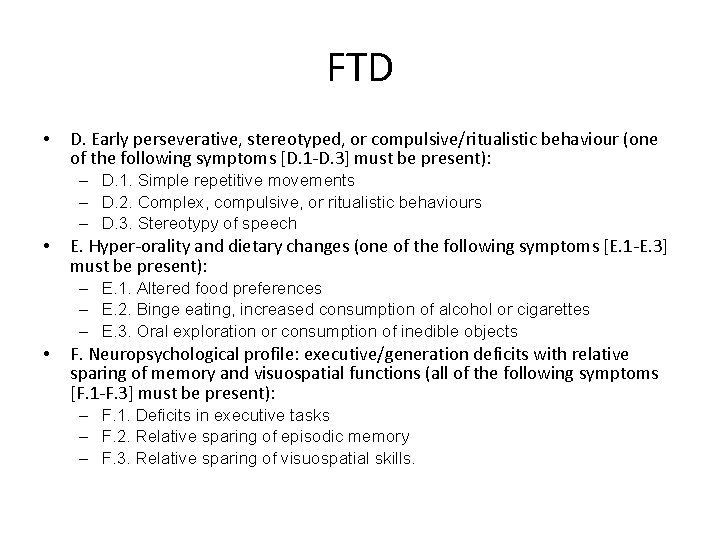
FTD • D. Early perseverative, stereotyped, or compulsive/ritualistic behaviour (one of the following symptoms [D. 1 -D. 3] must be present): – D. 1. Simple repetitive movements – D. 2. Complex, compulsive, or ritualistic behaviours – D. 3. Stereotypy of speech • E. Hyper-orality and dietary changes (one of the following symptoms [E. 1 -E. 3] must be present): – E. 1. Altered food preferences – E. 2. Binge eating, increased consumption of alcohol or cigarettes – E. 3. Oral exploration or consumption of inedible objects • F. Neuropsychological profile: executive/generation deficits with relative sparing of memory and visuospatial functions (all of the following symptoms [F. 1 -F. 3] must be present): – F. 1. Deficits in executive tasks – F. 2. Relative sparing of episodic memory – F. 3. Relative sparing of visuospatial skills.
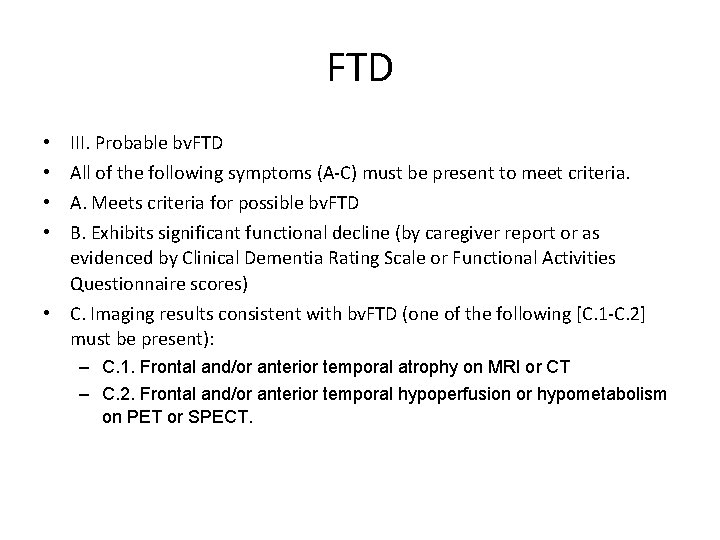
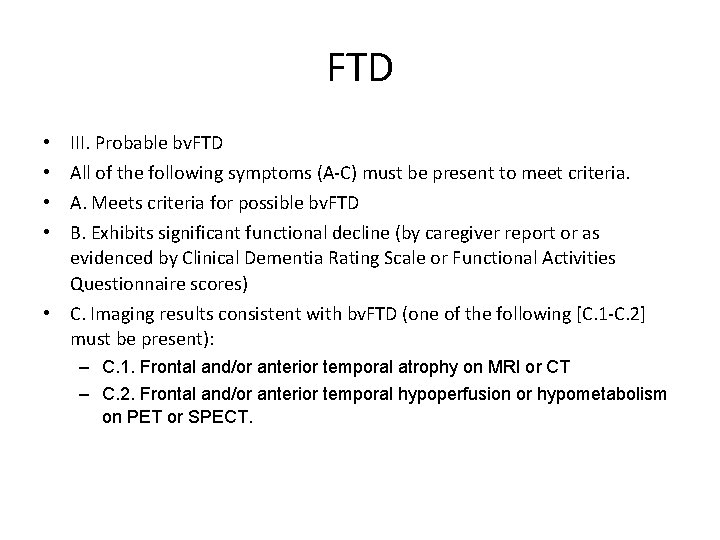
FTD • • III. Probable bv. FTD All of the following symptoms (A-C) must be present to meet criteria. A. Meets criteria for possible bv. FTD B. Exhibits significant functional decline (by caregiver report or as evidenced by Clinical Dementia Rating Scale or Functional Activities Questionnaire scores) • C. Imaging results consistent with bv. FTD (one of the following [C. 1 -C. 2] must be present): – C. 1. Frontal and/or anterior temporal atrophy on MRI or CT – C. 2. Frontal and/or anterior temporal hypoperfusion or hypometabolism on PET or SPECT.
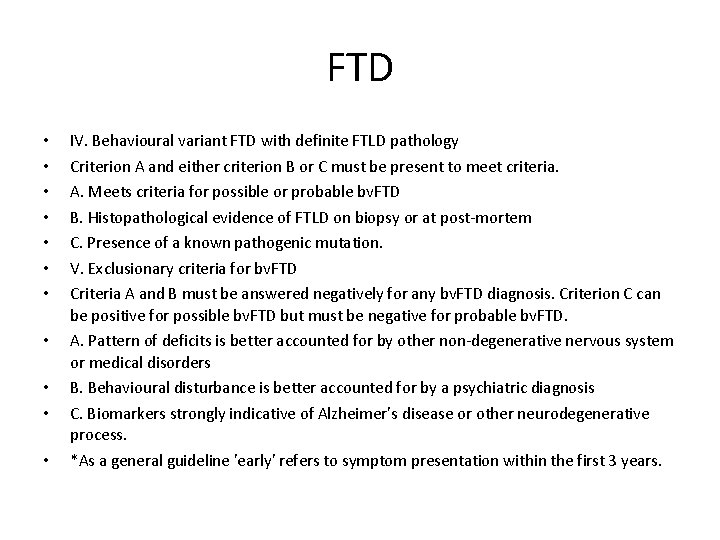
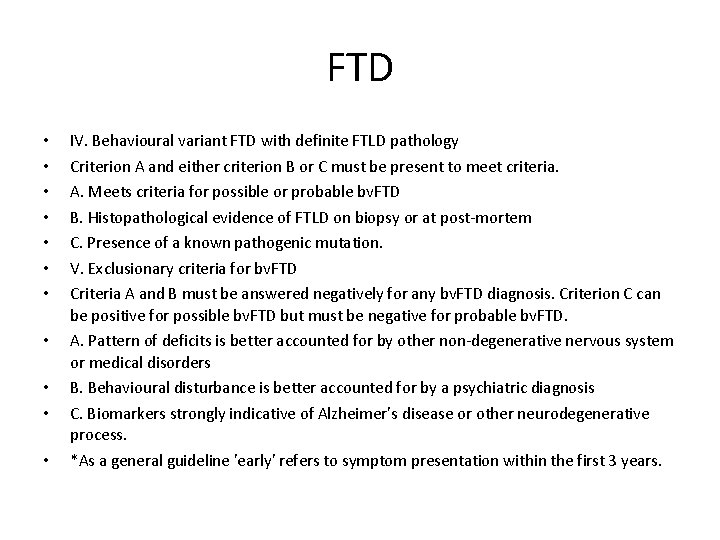
FTD • • • IV. Behavioural variant FTD with definite FTLD pathology Criterion A and either criterion B or C must be present to meet criteria. A. Meets criteria for possible or probable bv. FTD B. Histopathological evidence of FTLD on biopsy or at post-mortem C. Presence of a known pathogenic mutation. V. Exclusionary criteria for bv. FTD Criteria A and B must be answered negatively for any bv. FTD diagnosis. Criterion C can be positive for possible bv. FTD but must be negative for probable bv. FTD. A. Pattern of deficits is better accounted for by other non-degenerative nervous system or medical disorders B. Behavioural disturbance is better accounted for by a psychiatric diagnosis C. Biomarkers strongly indicative of Alzheimer’s disease or other neurodegenerative process. *As a general guideline 'early' refers to symptom presentation within the first 3 years.
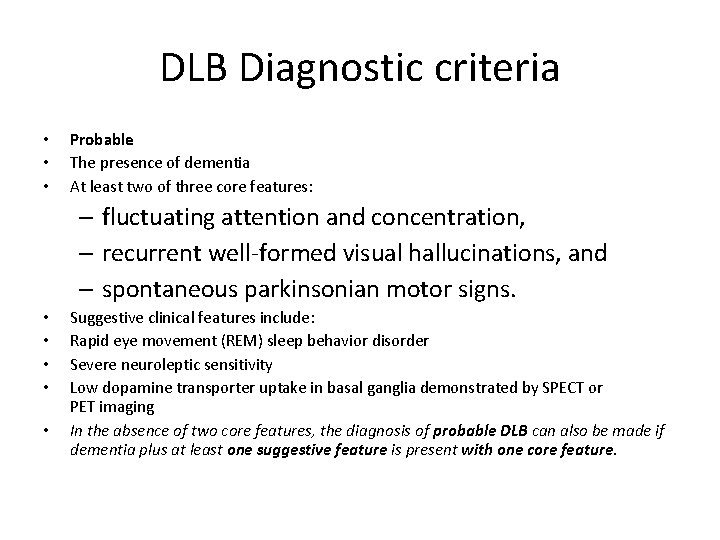
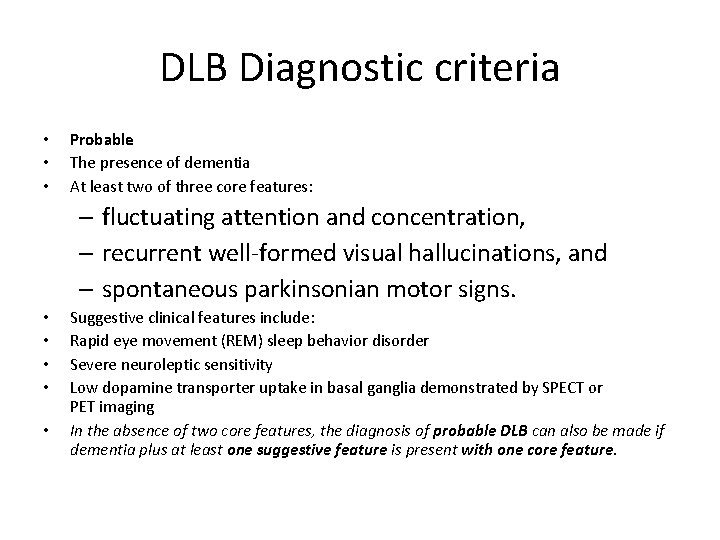
DLB Diagnostic criteria • • • Probable The presence of dementia At least two of three core features: – fluctuating attention and concentration, – recurrent well-formed visual hallucinations, and – spontaneous parkinsonian motor signs. • • • Suggestive clinical features include: Rapid eye movement (REM) sleep behavior disorder Severe neuroleptic sensitivity Low dopamine transporter uptake in basal ganglia demonstrated by SPECT or PET imaging In the absence of two core features, the diagnosis of probable DLB can also be made if dementia plus at least one suggestive feature is present with one core feature.
DLB • Possible DLB can be diagnosed with the presence of dementia plus one core or suggestive feature. • Supportive clinical features include repeated falls, syncope, a transient loss of consciousness, severe autonomic dysfunction, depression, systematized delusions, or hallucinations in other sensory and perceptual modalities. While these features may support the clinical diagnosis, they lack diagnostic specificity and can be seen in other neurodegenerative disorders. • These criteria have a sensitivity of 83% (17% clinical false negative rate) and a specificity of 95% (clinical false positive rate of only 5%) for the presence of neocortical Lewy bodies (LBs) at autopsy, the current diagnostic gold standard.
Va. D Criteria • • I. The criteria for the clinical diagnosis of probable vascular dementia include all of the following: Dementia – deficits should be severe enough to interfere with activities of daily living not due to physical effects of stroke alone. Exclusion criteria: cases with disturbance of consciousness, delirium, psychosis, severe aphasia, or major sensorimotor impairment precluding neuropsychological testing. • Cerebrovascular disease – defined by the presence of focal signs on neurologic examination, such as hemiparesis, lower facial weakness, Babinski sign, sensory deficit, hemianopia, and dysarthria consistent with stroke (with or without history of stroke), – MRI : multiple large vessel infarcts or a single strategically placed infarct as well as multiple basal ganglia and white matter lacunes, or extensive periventricular white matter lesions, or combinations thereof. • A relationship between the above two disorders, manifested or inferred by the presence of one or more of the following: (a) onset of dementia within 3 months following a recognized stroke; (b) abrupt deterioration in cognitive functions; or fluctuating, stepwise progression of cognitive deficits.
FTD • Behavioural variant – Apathetic – Disinhibited • Language variant(s) – Semantic – Agrammatic – PNFA
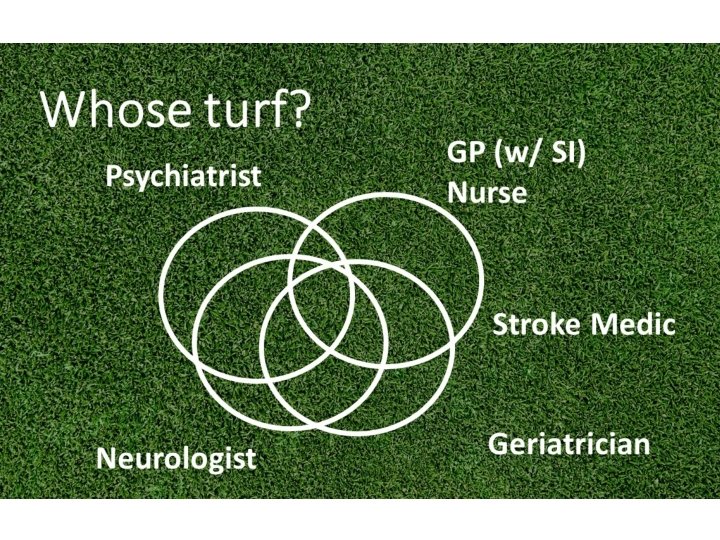
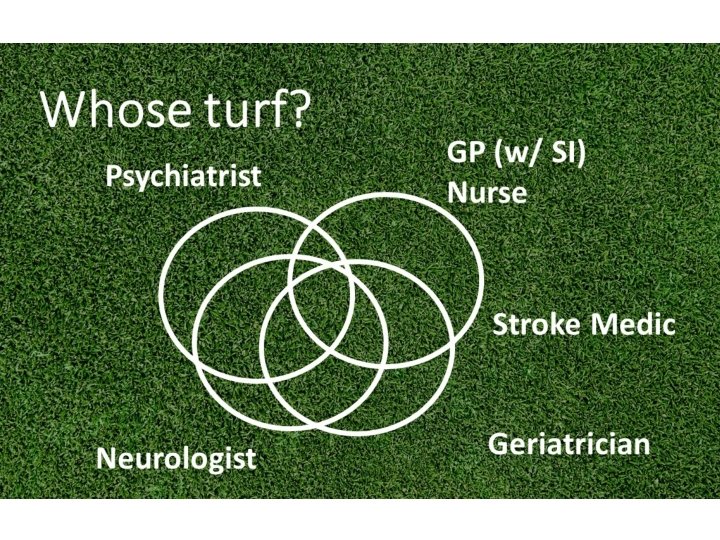
MDT • • Occupational therapy Dementia adviser Pharmacist CPN Physio GP Neurology • Roles?