Skin lesions Encountered in approximately 15 of patients








- Slides: 24
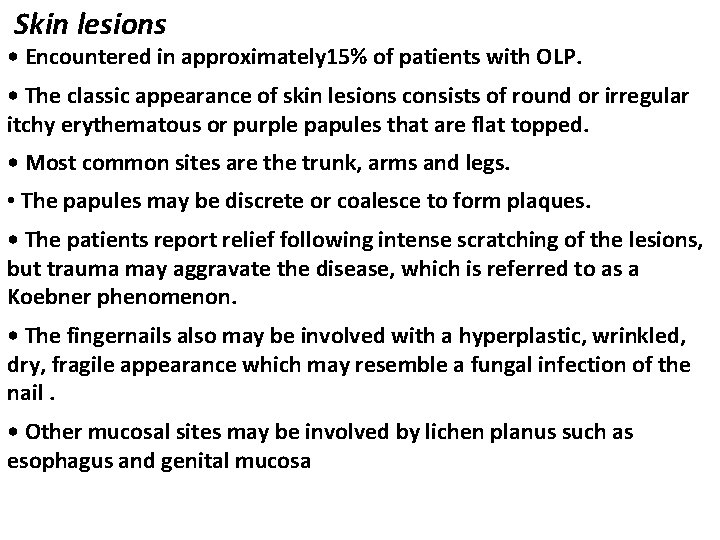
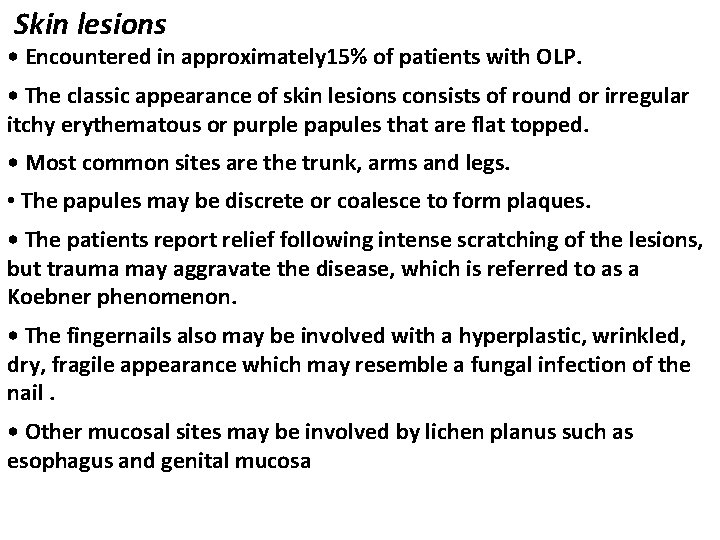
Skin lesions • Encountered in approximately 15% of patients with OLP. • The classic appearance of skin lesions consists of round or irregular itchy erythematous or purple papules that are flat topped. • Most common sites are the trunk, arms and legs. • The papules may be discrete or coalesce to form plaques. • The patients report relief following intense scratching of the lesions, but trauma may aggravate the disease, which is referred to as a Koebner phenomenon. • The fingernails also may be involved with a hyperplastic, wrinkled, dry, fragile appearance which may resemble a fungal infection of the nail. • Other mucosal sites may be involved by lichen planus such as esophagus and genital mucosa
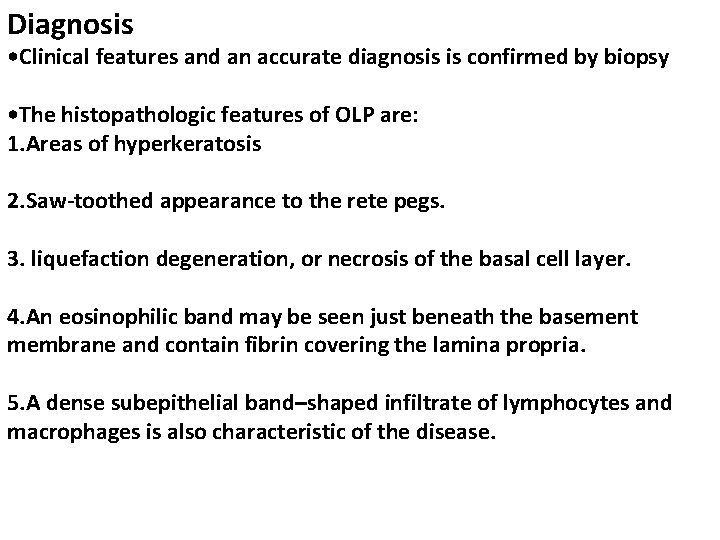
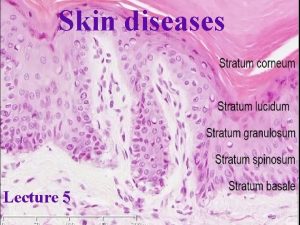
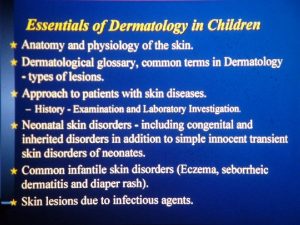
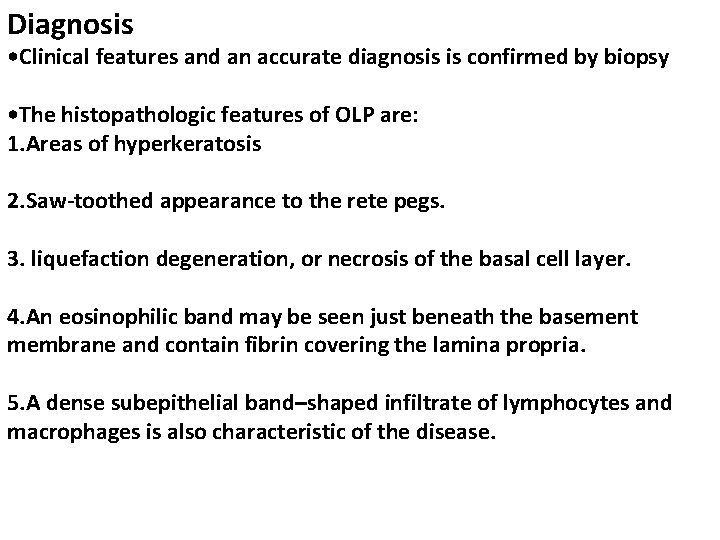
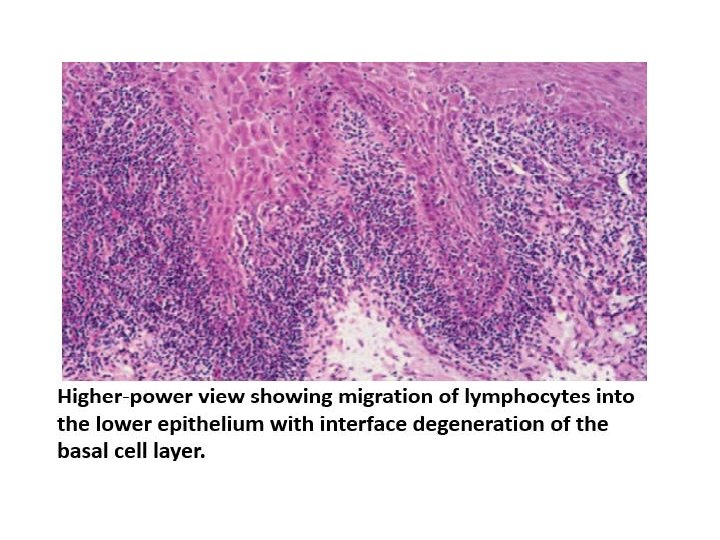
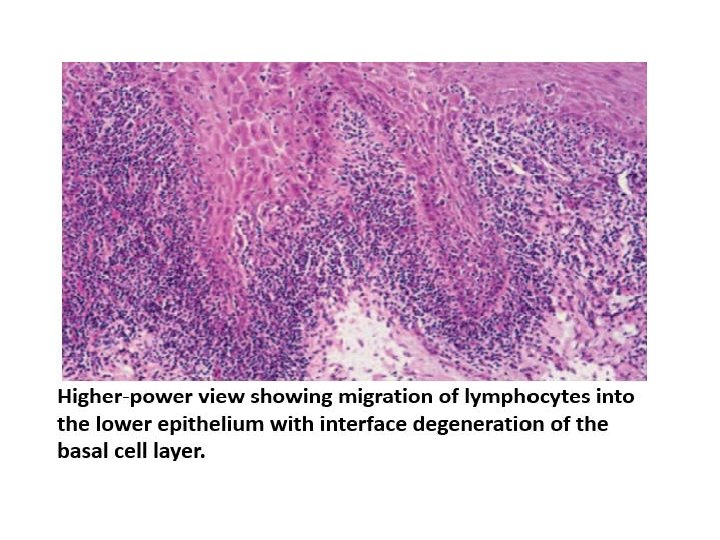
Diagnosis • Clinical features and an accurate diagnosis is confirmed by biopsy • The histopathologic features of OLP are: 1. Areas of hyperkeratosis 2. Saw-toothed appearance to the rete pegs. 3. liquefaction degeneration, or necrosis of the basal cell layer. 4. An eosinophilic band may be seen just beneath the basement membrane and contain fibrin covering the lamina propria. 5. A dense subepithelial band–shaped infiltrate of lymphocytes and macrophages is also characteristic of the disease.
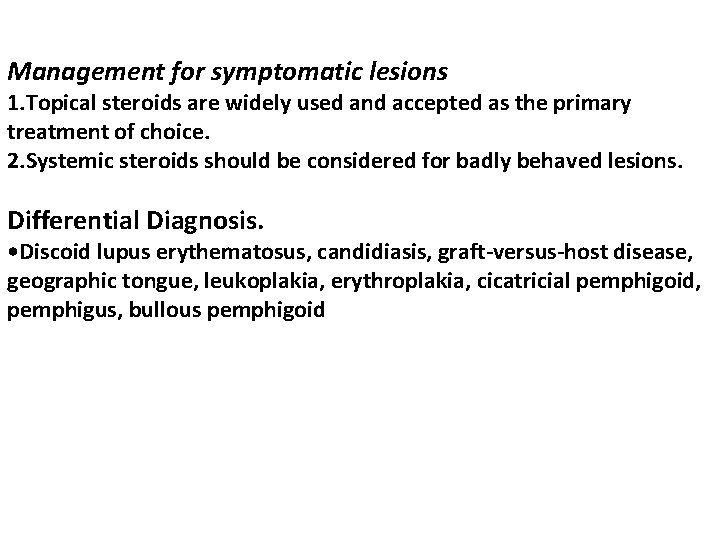
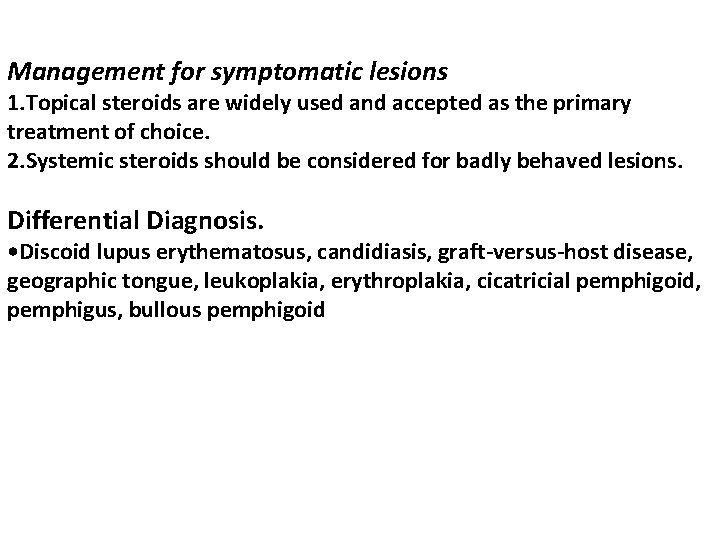
Management for symptomatic lesions 1. Topical steroids are widely used and accepted as the primary treatment of choice. 2. Systemic steroids should be considered for badly behaved lesions. Differential Diagnosis. • Discoid lupus erythematosus, candidiasis, graft-versus-host disease, geographic tongue, leukoplakia, erythroplakia, cicatricial pemphigoid, pemphigus, bullous pemphigoid

Drug-Induced Lichenoid Reactions • May occur as a reaction to a wide range of drugs which includes penicillin, NSAID, and sulfonamides. • This lesion have identical clinical and histological appearance to L. P. but lichenoid reactions are predominantly unilateral and present with an ulcerative reaction pattern.
Management • Discontinuance of the drug and symptomatic treatment with topical steroids are often sufficient. • The patient should be properly educated about the responsible drug. • Lichenoid reactions of graft-versus-host disease (GVHD) • Lichenoid eruptions on skin & mucosa may also be seen as part of a graft-versus-host reaction, for example; in patients who have received bone marrow transplants.
ALLERGIC REACTIONS Lichenoid Contact Reactions(LCR) A type of delayed hypersensitivity reaction to constituents derived from dental materials, predominantly amalgam fillings. Clinically LCRs display the same reaction patterns as seen in OLP, that is, reticulum, papules, plaque, erythema, and ulcers. The most apparent clinical difference between OLP and LCR is the extension of the lesions. The majority of LCRs are confined to sites that are regularly in contact with dental materials, such as the buccal mucosa and the border of the tongue.

Management Replacement of dental materials in direct contact with LCR will result in cure or considerable improvement in most of the cases. Reactions to Dentifrice and Chlorhexidine • Delayed hypersensitivity reactions to tooth pastes and mouth washes have been reported. • The compounds responsible for the allergic reactions may include flavor additives such as cinnamon or preservatives. • These flavoring constituents may also be used in chewing gum and produce similar forms of gingivostomatitis. • The clinical manifestations include red edematous gingiva, which may include both ulcerations and white lesions. • Similar lesions may involve other sites, such as the labial, buccal, and tongue
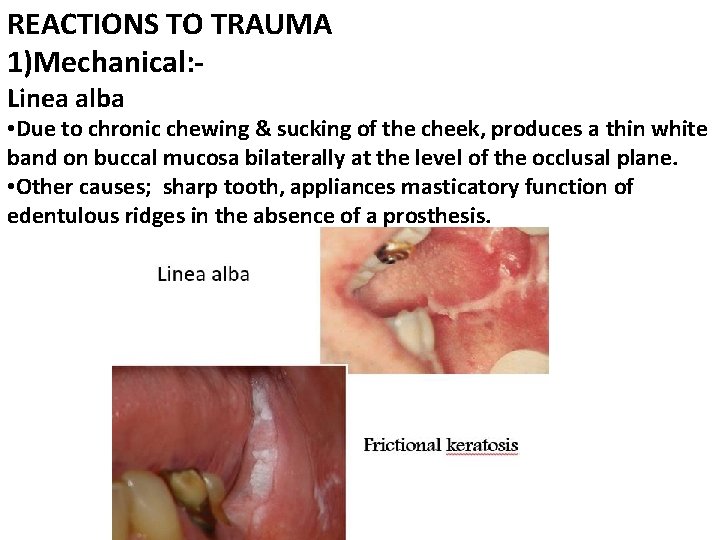
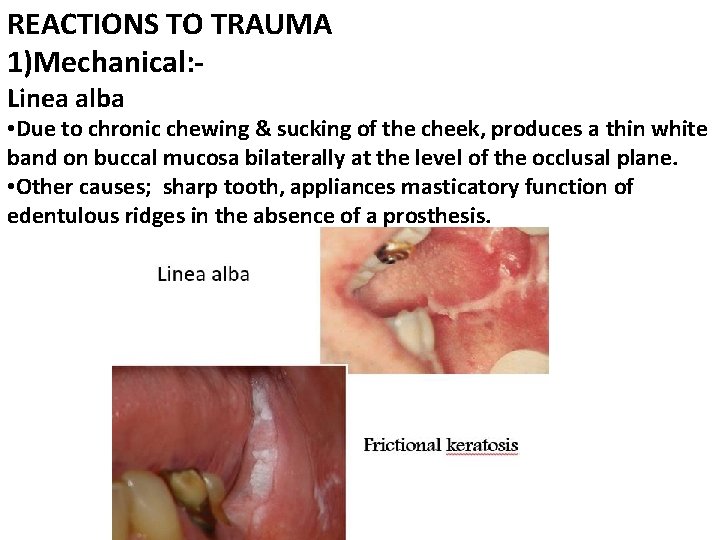
REACTIONS TO TRAUMA 1)Mechanical: Linea alba • Due to chronic chewing & sucking of the cheek, produces a thin white band on buccal mucosa bilaterally at the level of the occlusal plane. • Other causes; sharp tooth, appliances masticatory function of edentulous ridges in the absence of a prosthesis.

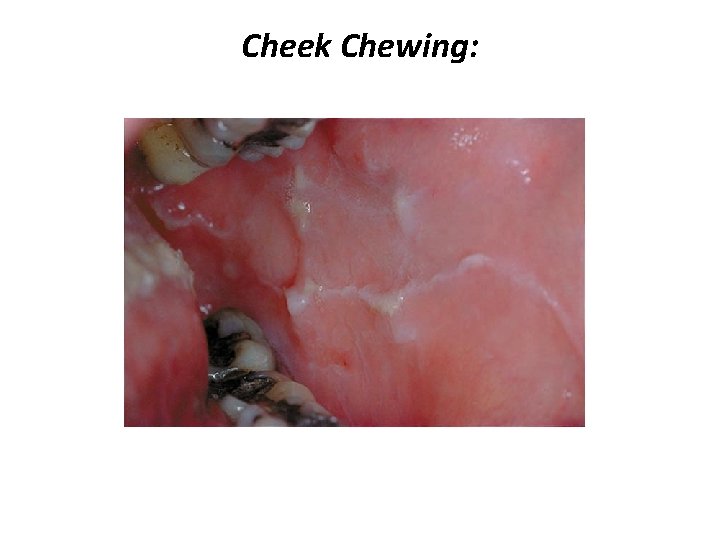
Frictional keratosis The oral mucosa react to friction in one of two ways; • An acute frictional response leads to a blister and ulceration. • While a chronic frictional response leads to epithelial thickening and hyperkeratinization. • Irritants such as sharp tooth , cheek biting & prolonged wearing of often ill-fitting dentures by time become dense and white and show a roughened surface.
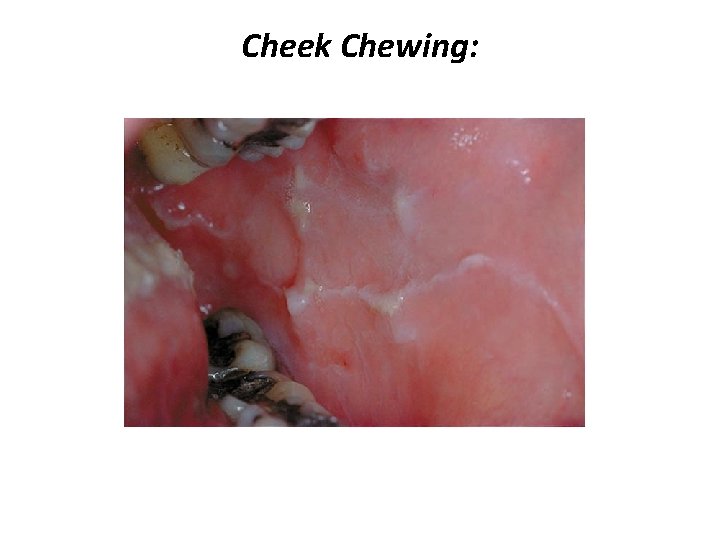
Cheek Chewing:


Reactive and Inflammatory White Lesions: Frictional Keratosis
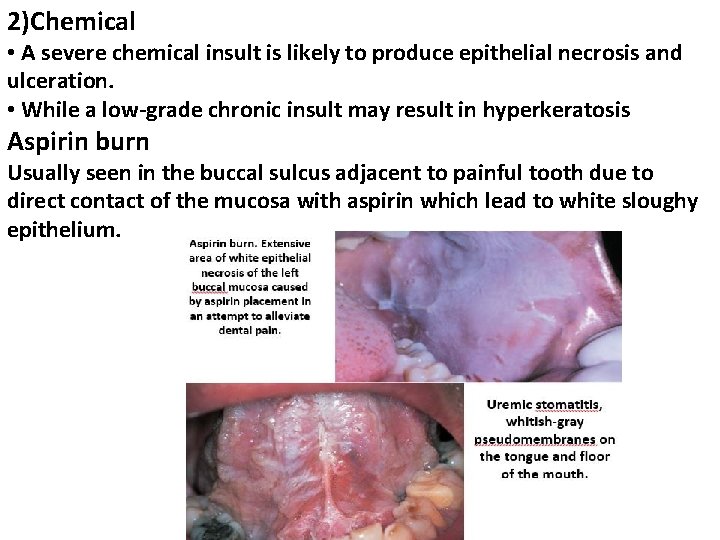
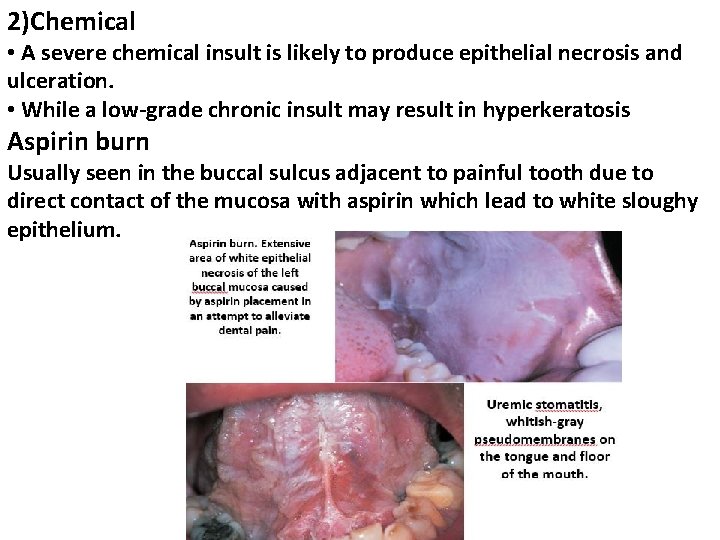
2)Chemical • A severe chemical insult is likely to produce epithelial necrosis and ulceration. • While a low-grade chronic insult may result in hyperkeratosis Aspirin burn Usually seen in the buccal sulcus adjacent to painful tooth due to direct contact of the mucosa with aspirin which lead to white sloughy epithelium.

Chemical Injuries of the Oral Mucosa:
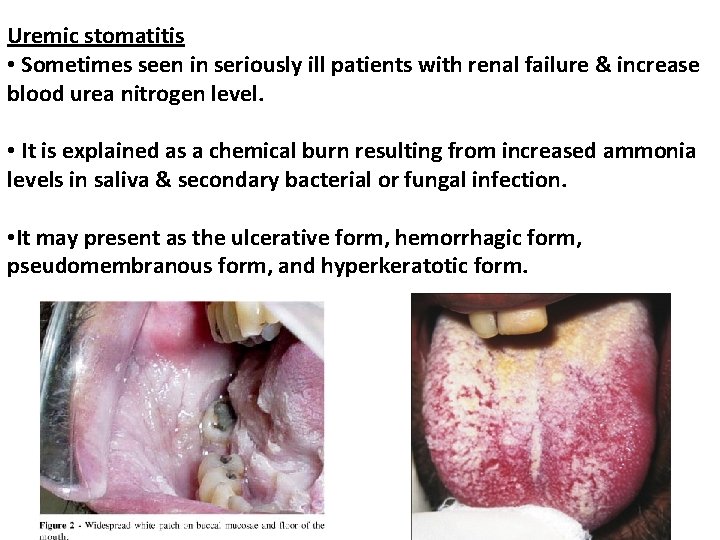
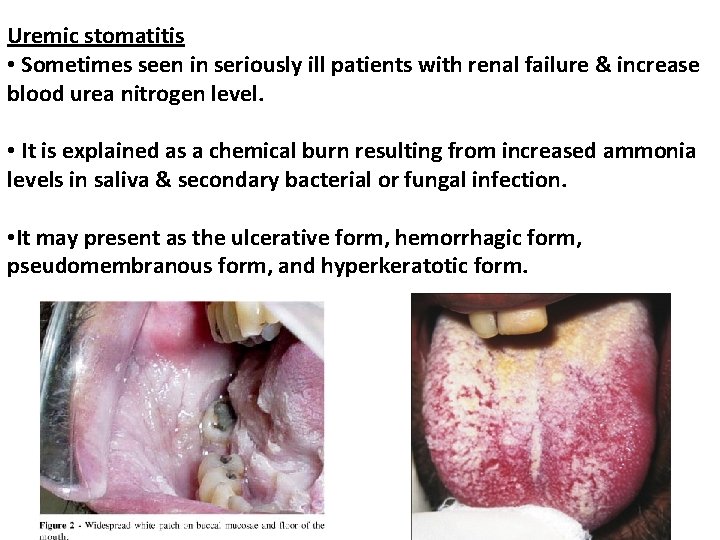
Uremic stomatitis • Sometimes seen in seriously ill patients with renal failure & increase blood urea nitrogen level. • It is explained as a chemical burn resulting from increased ammonia levels in saliva & secondary bacterial or fungal infection. • It may present as the ulcerative form, hemorrhagic form, pseudomembranous form, and hyperkeratotic form.
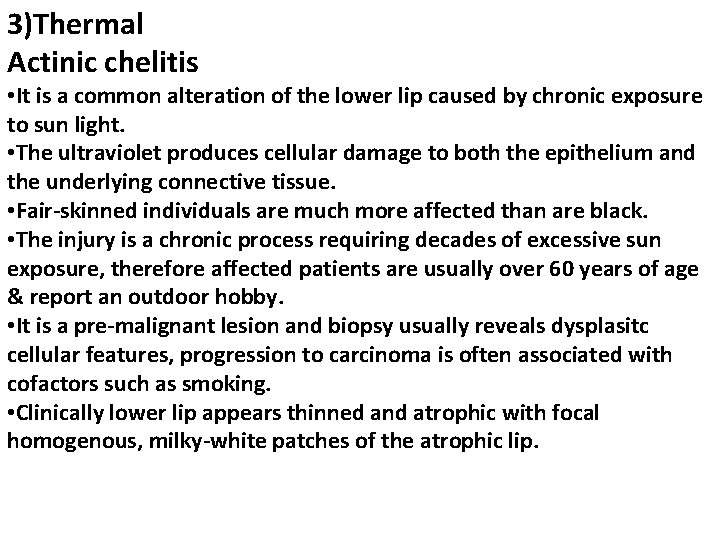
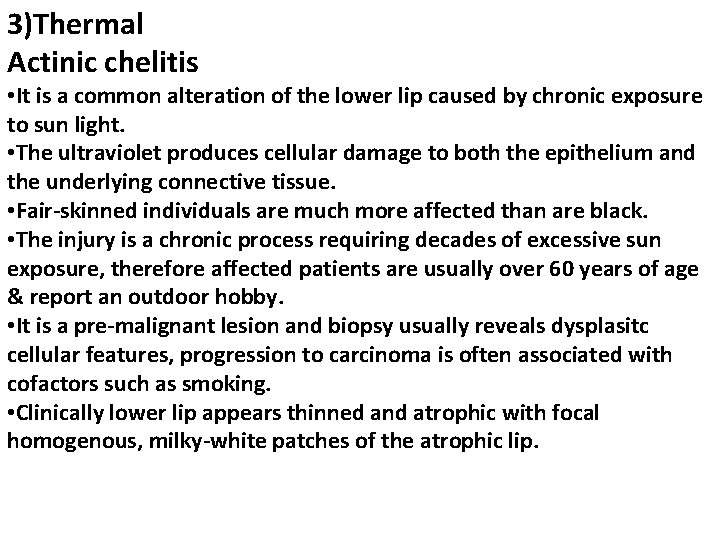
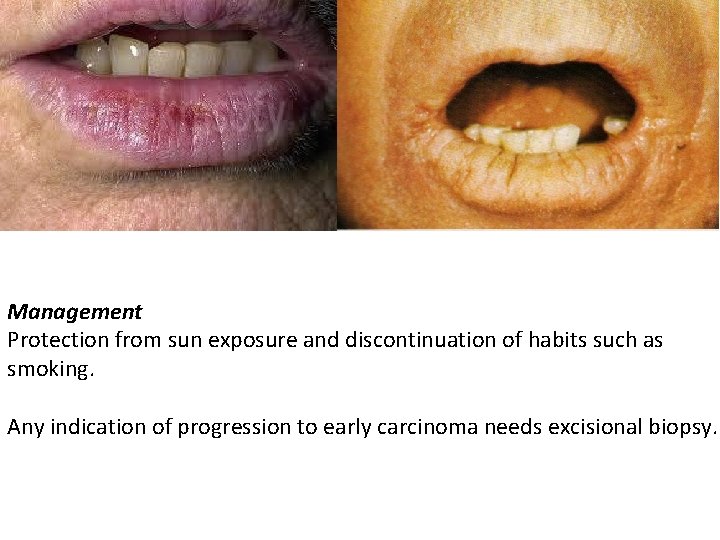
3)Thermal Actinic chelitis • It is a common alteration of the lower lip caused by chronic exposure to sun light. • The ultraviolet produces cellular damage to both the epithelium and the underlying connective tissue. • Fair-skinned individuals are much more affected than are black. • The injury is a chronic process requiring decades of excessive sun exposure, therefore affected patients are usually over 60 years of age & report an outdoor hobby. • It is a pre-malignant lesion and biopsy usually reveals dysplasitc cellular features, progression to carcinoma is often associated with cofactors such as smoking. • Clinically lower lip appears thinned and atrophic with focal homogenous, milky-white patches of the atrophic lip.
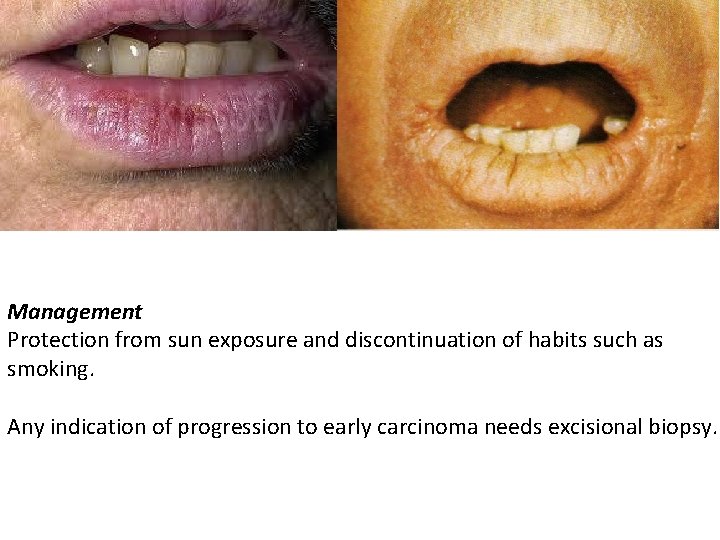
Management Protection from sun exposure and discontinuation of habits such as smoking. Any indication of progression to early carcinoma needs excisional biopsy.
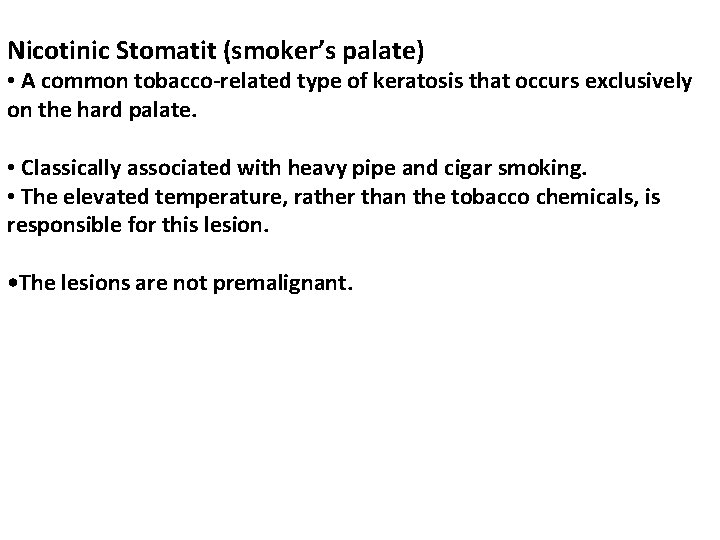
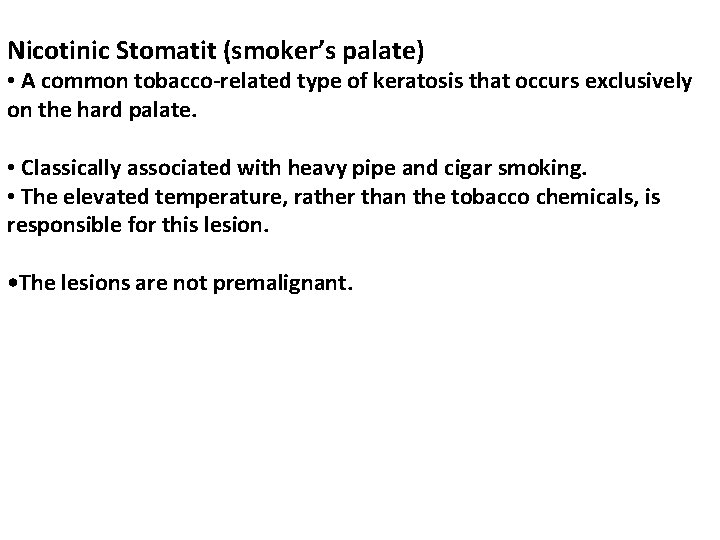
Nicotinic Stomatit (smoker’s palate) • A common tobacco-related type of keratosis that occurs exclusively on the hard palate. • Classically associated with heavy pipe and cigar smoking. • The elevated temperature, rather than the tobacco chemicals, is responsible for this lesion. • The lesions are not premalignant.

Clinically, • The palatal mucosa initially responds to the high temperature with redness. • Later, it becomes wrinkled and takes on a diffusely grayish-white color, with numerous micronodules with characteristic punctate red centers, which represent the inflamed and dilated orifices of the minor salivary gland ducts. Treatment Cessation of smoking
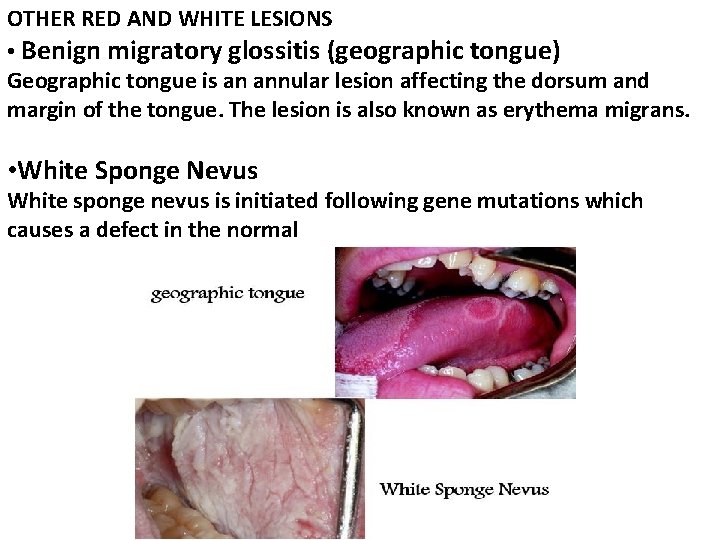
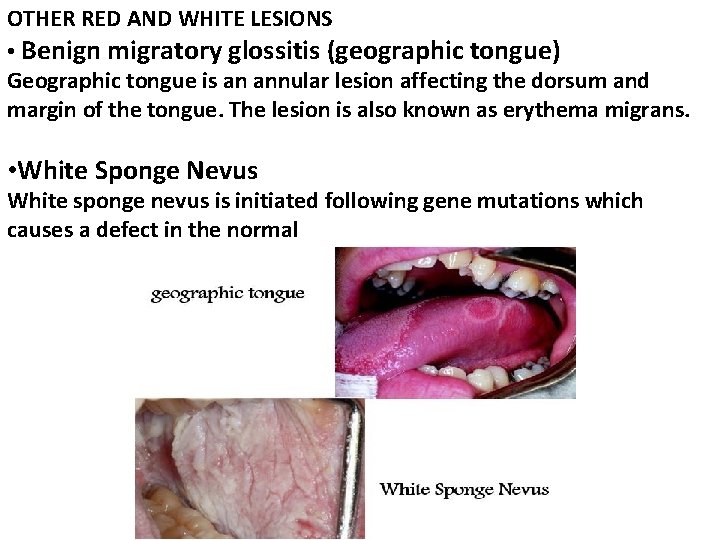
OTHER RED AND WHITE LESIONS • Benign migratory glossitis (geographic tongue) Geographic tongue is an annular lesion affecting the dorsum and margin of the tongue. The lesion is also known as erythema migrans. • White Sponge Nevus White sponge nevus is initiated following gene mutations which causes a defect in the normal
• Leukodema It is a diffuse, translucent , milky whiteness thickening (folded appearance), may in fact represent a variation of the normal appearance rather than a disease • Fordyce granules Heterotopic collections of sebaceous glands in the buccal mucosa, and vermilion border of the lip. • Hairy Tongue

Leukoedema
 Dermatology morphology
Dermatology morphology Describing skin lesions
Describing skin lesions Example of divided powder
Example of divided powder Thin skin vs thick skin
Thin skin vs thick skin Milady chapter 23
Milady chapter 23 Thick skin
Thick skin Site:slidetodoc.com
Site:slidetodoc.com Chapter 17 oral pathology
Chapter 17 oral pathology Epidermoid carcinoma
Epidermoid carcinoma Periradicular disease definition
Periradicular disease definition Amiante
Amiante Lésions
Lésions Projektov�� mana����r
Projektov�� mana����r Olneys lesions
Olneys lesions Eye lesions
Eye lesions White appearance
White appearance Vesiculobullous lesions
Vesiculobullous lesions Components of visual pathway
Components of visual pathway Scattered white matter lesions
Scattered white matter lesions Difference between pyramidal and extrapyramidal tract
Difference between pyramidal and extrapyramidal tract Convergence insufficiency athens
Convergence insufficiency athens Lesion to vagus nerve
Lesion to vagus nerve Dont touch lesion
Dont touch lesion Clinical features of burns
Clinical features of burns Pyramidal vs extrapyramidal lesions
Pyramidal vs extrapyramidal lesions