Vulval Vaginal lesions VIP Vulval Vaginal lesions DR




- Slides: 25

Vulval & Vaginal lesions VIP ﺭﺍﺋﺪ ﻋﻠﻲ : ﻋﻤﻞ
Vulval & Vaginal lesions DR Omar Abu-Azzam
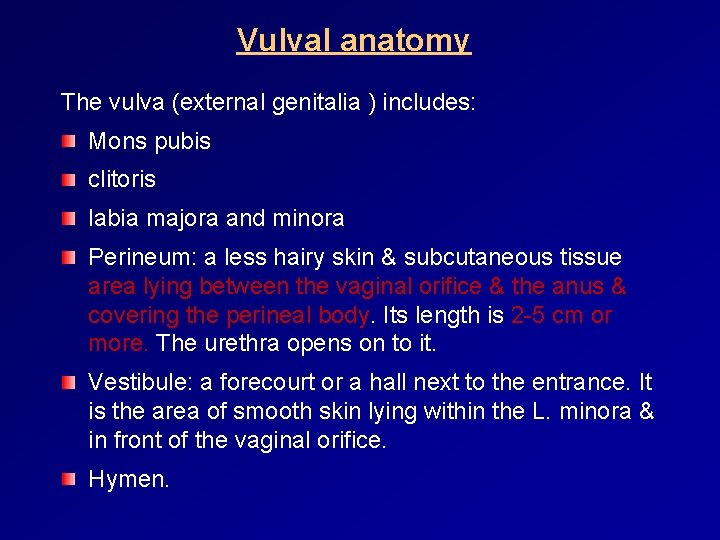
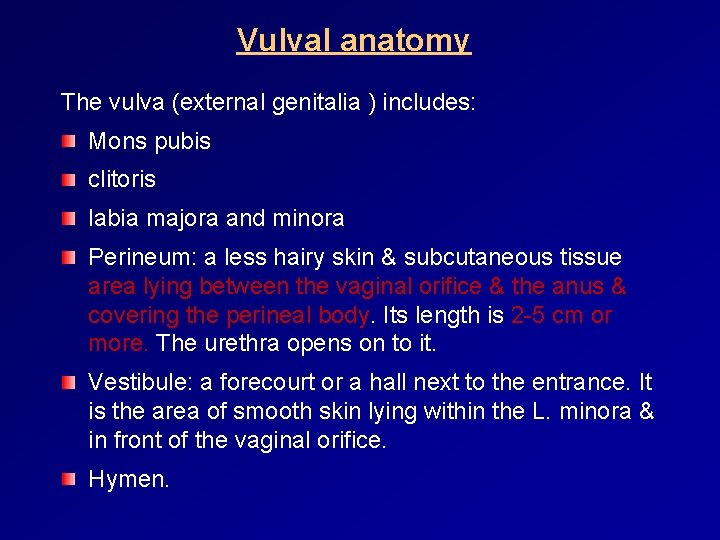
Vulval anatomy The vulva (external genitalia ) includes: Mons pubis clitoris labia majora and minora Perineum: a less hairy skin & subcutaneous tissue area lying between the vaginal orifice & the anus & covering the perineal body. Its length is 2 -5 cm or more. The urethra opens on to it. Vestibule: a forecourt or a hall next to the entrance. It is the area of smooth skin lying within the L. minora & in front of the vaginal orifice. Hymen.
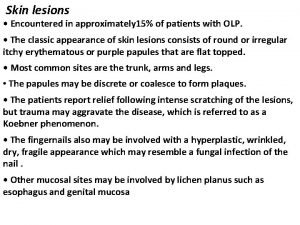
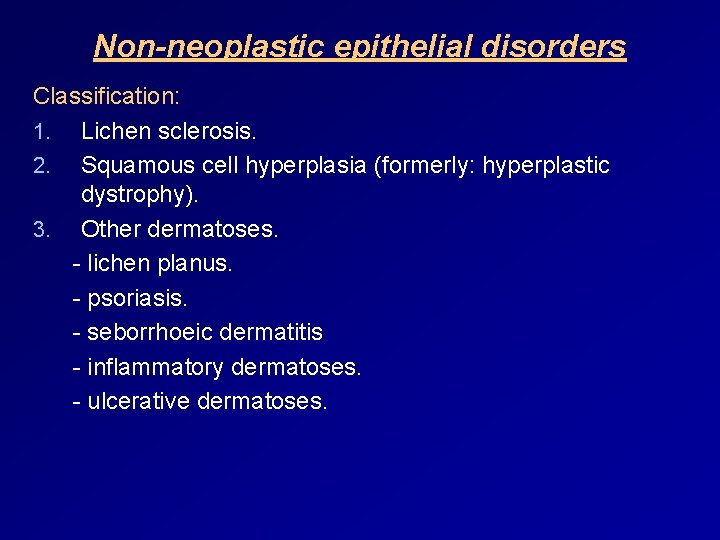
Non-neoplastic epithelial disorders Classification: 1. Lichen sclerosis. 2. Squamous cell hyperplasia (formerly: hyperplastic dystrophy). 3. Other dermatoses. - lichen planus. - psoriasis. - seborrhoeic dermatitis - inflammatory dermatoses. - ulcerative dermatoses.
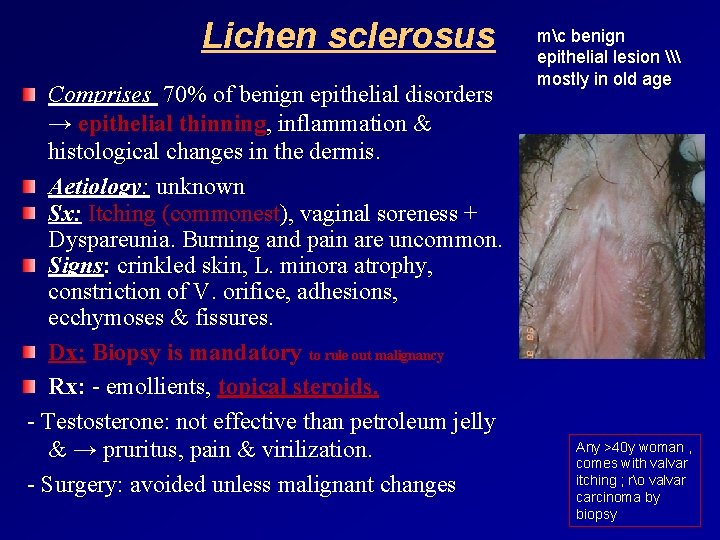
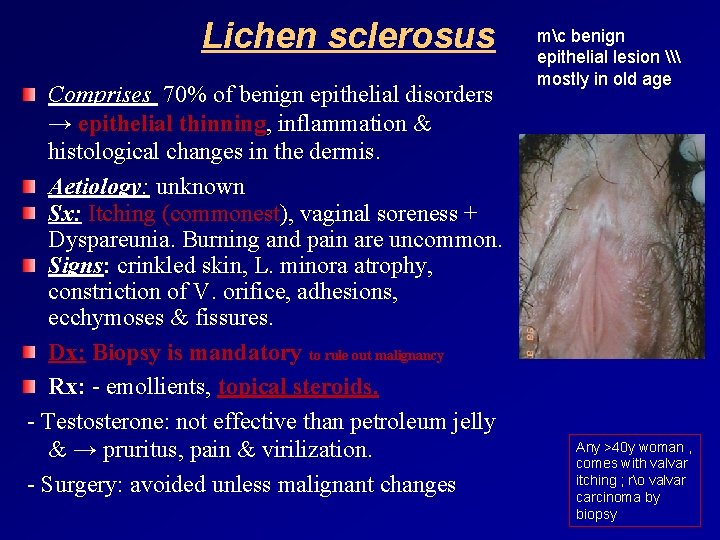
Lichen sclerosus Comprises 70% of benign epithelial disorders → epithelial thinning, inflammation & histological changes in the dermis. Aetiology: unknown Sx: Itching (commonest), vaginal soreness + Dyspareunia. Burning and pain are uncommon. Signs: crinkled skin, L. minora atrophy, constriction of V. orifice, adhesions, ecchymoses & fissures. Dx: Biopsy is mandatory to rule out malignancy Rx: - emollients, topical steroids. - Testosterone: not effective than petroleum jelly & → pruritus, pain & virilization. - Surgery: avoided unless malignant changes mc benign epithelial lesion \ mostly in old age Any >40 y woman , comes with valvar itching ; ro valvar carcinoma by biopsy
Squamous cell hyperplasia Df: thickened skin with white hyperkeratotic patches, excoriation & fissures. Histo: hyperkeratosis, cellular epithelial proliferation with normal maturation & inflammatory response in the dermis (lymphatic & plasma cell infiltration). Aetiology: repetitive surface irritation & trauma from irritants that causing scratching & rubbing. RX: topical steroid Any >40 y woman , comes with valvar itching ; ro valvar carcinoma by biopsy
Benign Vulval lumps Bartholin’s cyst. Epidermal inclusion cyst. Skene’s duct cyst. Congenital mucous cysts: arise from mesonephric ducts remnants. Cyst of the canal of Nuck: can give rise to hydrocele in labia maqjora. Sebaceous cyst. Papillomatosis (solid). Fibroma (solid). Lipoma (solid). Condylomata (solid). v Cysts are either congenital or arise from obstructed glands. v Manifestations arise from the cysts (cosmotic) or from infection.
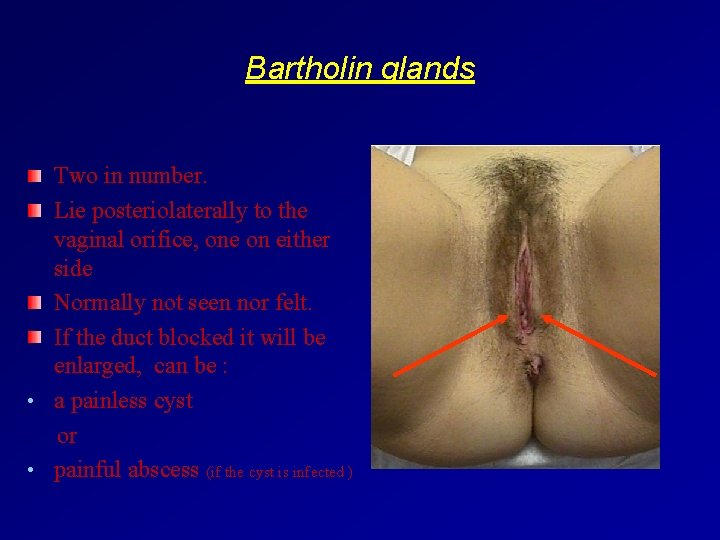
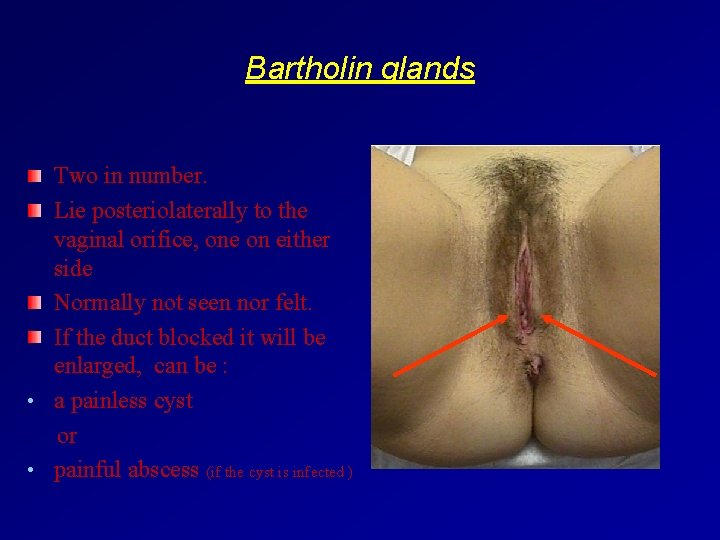
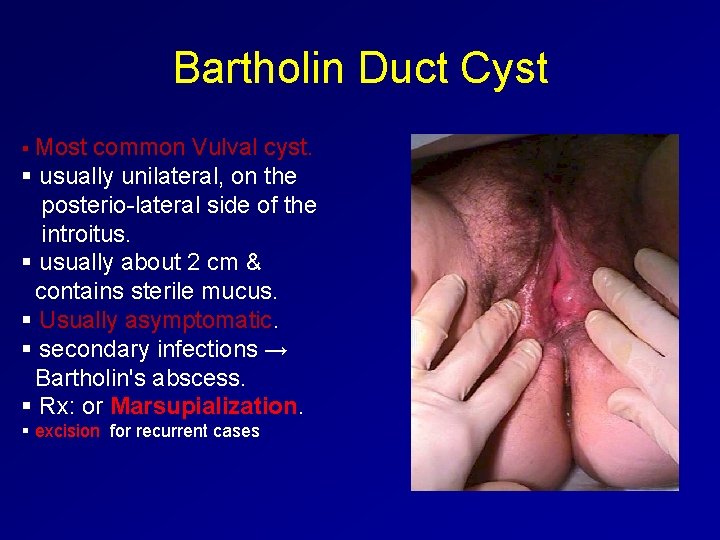
Bartholin glands Two in number. Lie posteriolaterally to the vaginal orifice, one on either side Normally not seen nor felt. If the duct blocked it will be enlarged, can be : • a painless cyst or • painful abscess (if the cyst is infected )
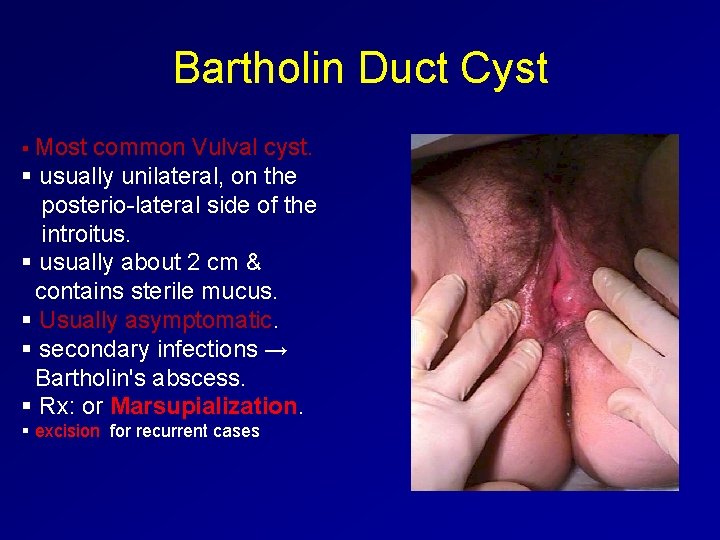
Bartholin Duct Cyst § Most common Vulval cyst. § usually unilateral, on the posterio-lateral side of the introitus. § usually about 2 cm & contains sterile mucus. § Usually asymptomatic. § secondary infections → Bartholin's abscess. § Rx: or Marsupialization. § excision for recurrent cases
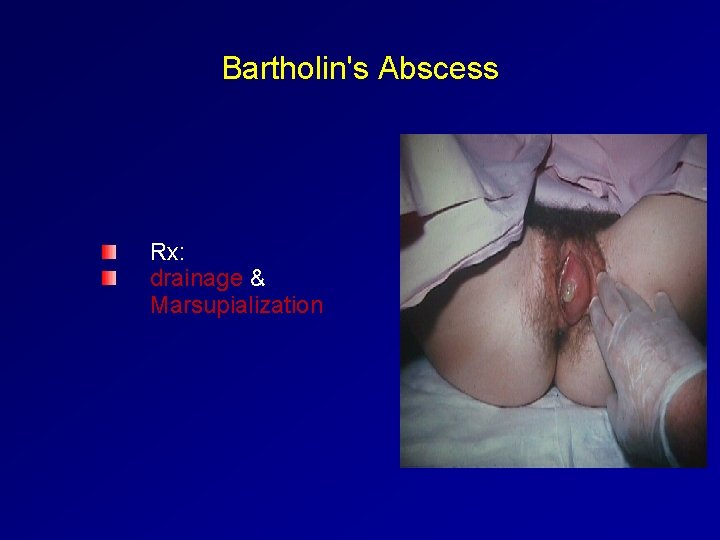
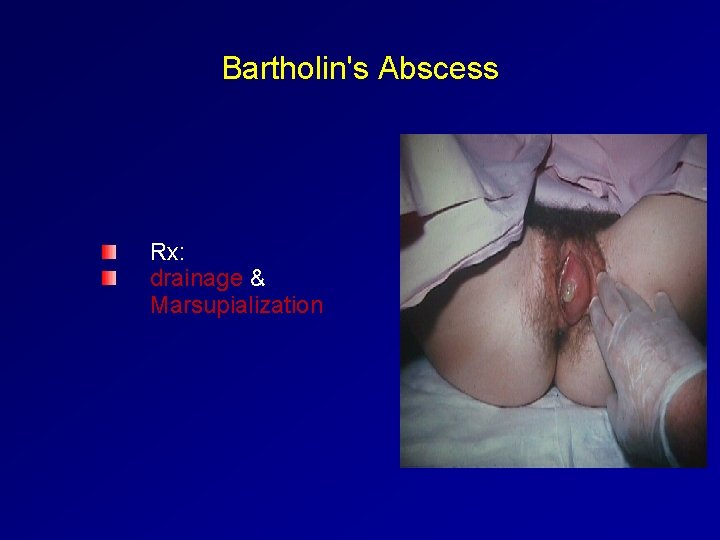
Bartholin's Abscess Rx: drainage & Marsupialization
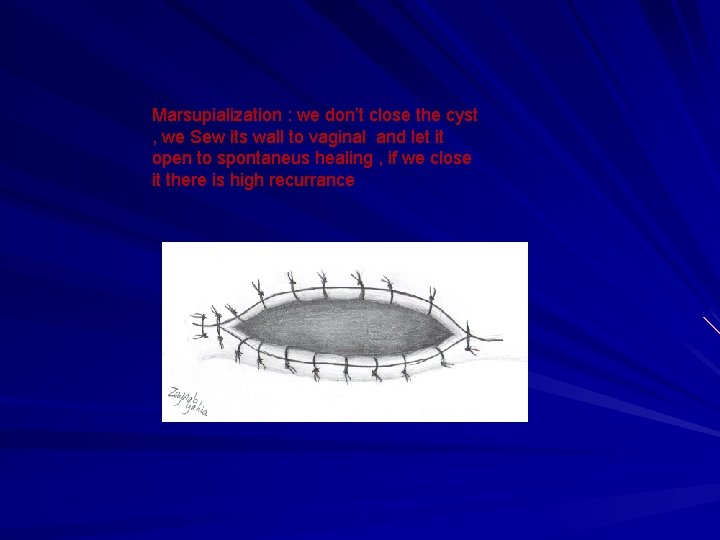
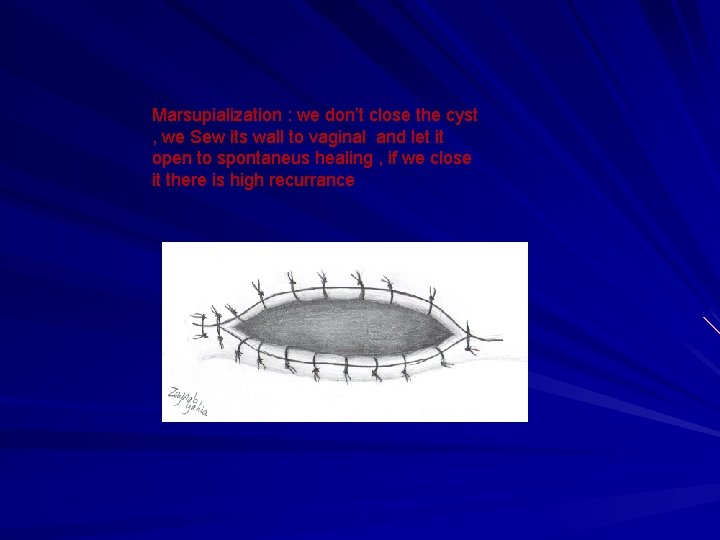
Marsupialization : we don’t close the cyst , we Sew its wall to vaginal and let it open to spontaneus healing , if we close it there is high recurrance
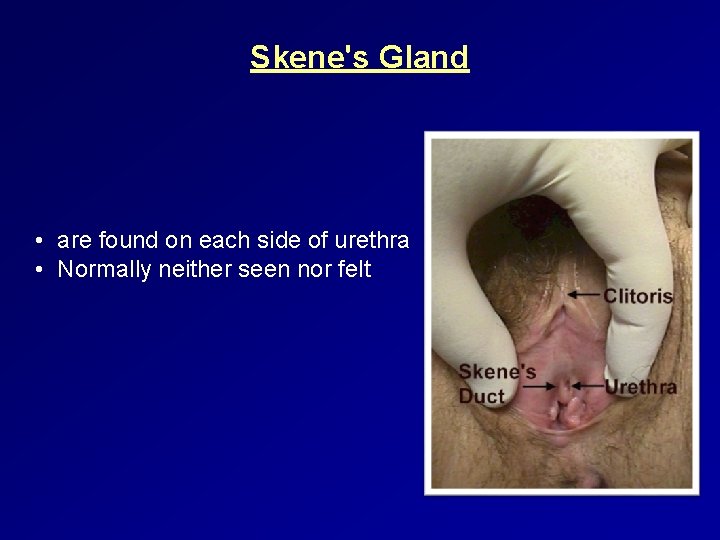
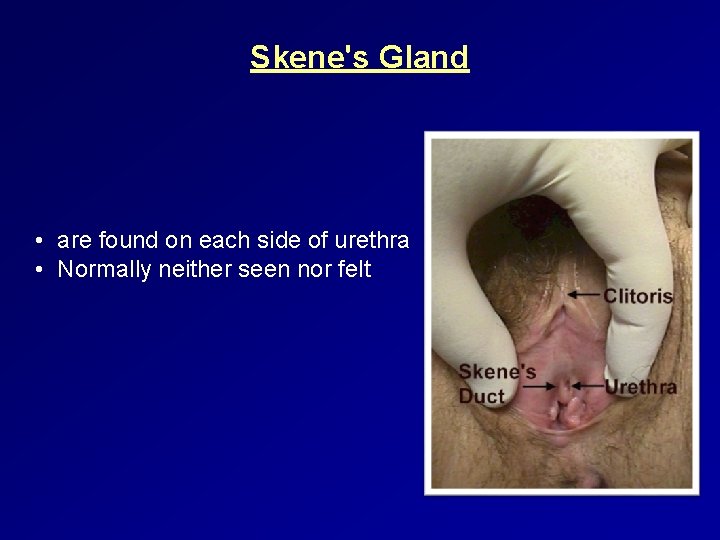
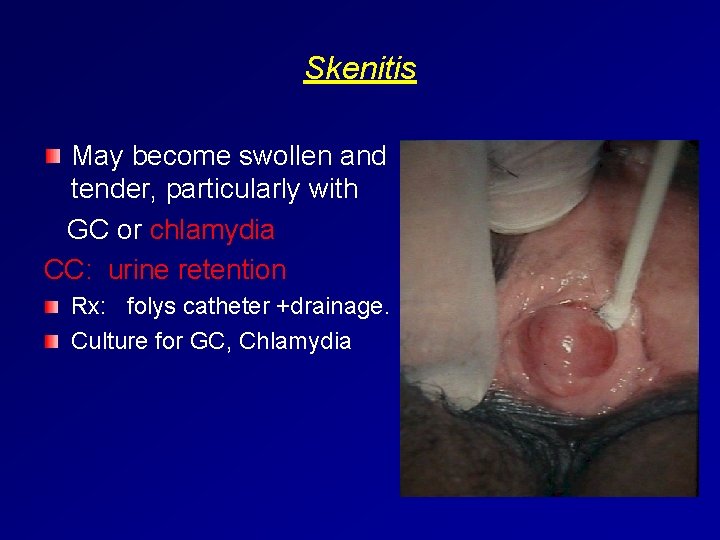
Skene's Gland • are found on each side of urethra • Normally neither seen nor felt
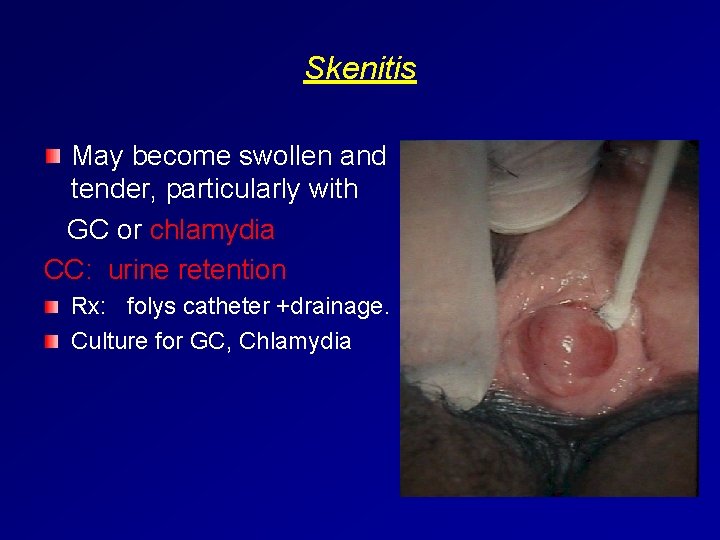
Skenitis May become swollen and tender, particularly with GC or chlamydia CC: urine retention Rx: folys catheter +drainage. Culture for GC, Chlamydia
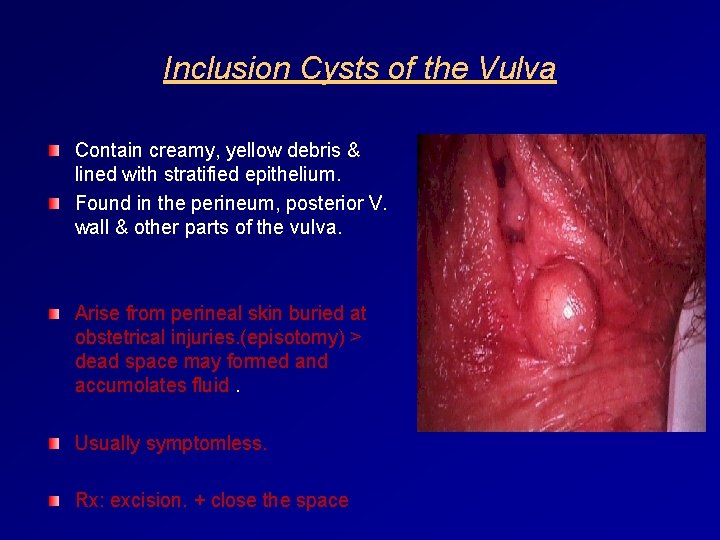
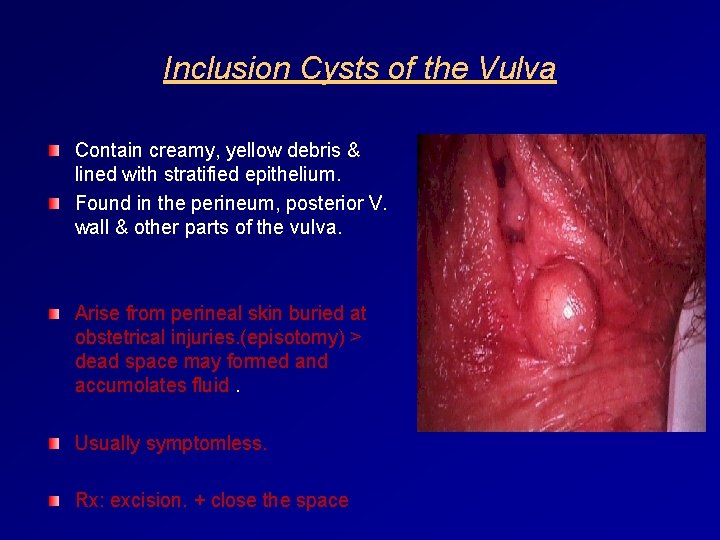
Inclusion Cysts of the Vulva Contain creamy, yellow debris & lined with stratified epithelium. Found in the perineum, posterior V. wall & other parts of the vulva. Arise from perineal skin buried at obstetrical injuries. (episotomy) > dead space may formed and accumolates fluid. Usually symptomless. Rx: excision. + close the space

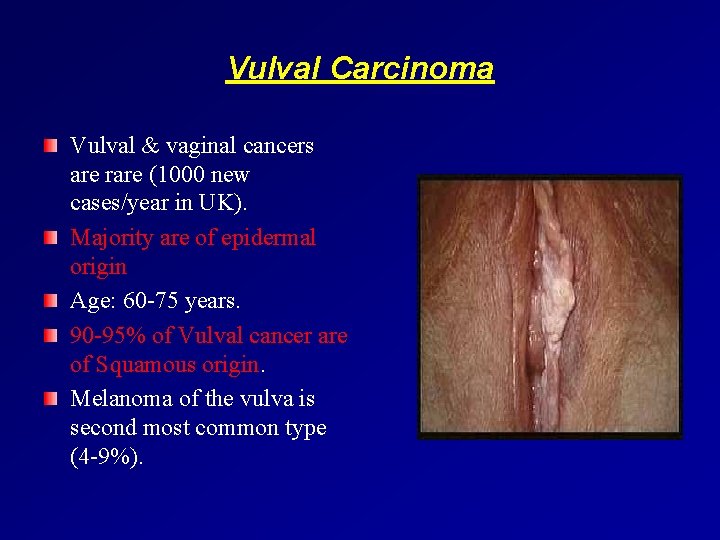
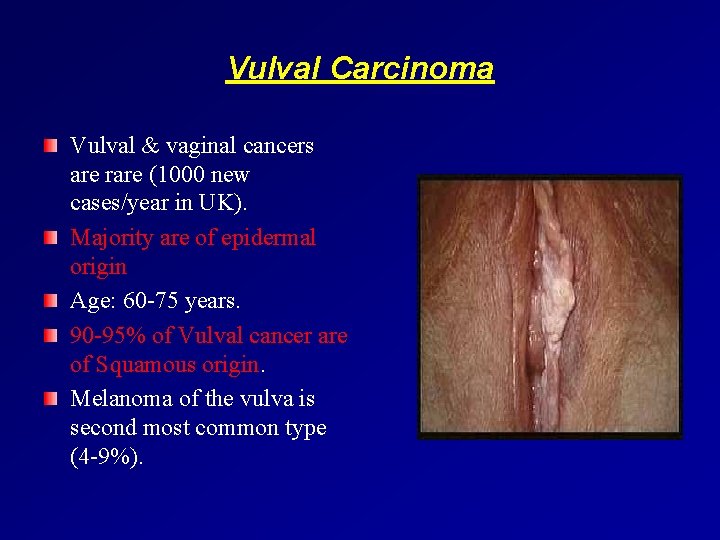
Vulval Carcinoma Vulval & vaginal cancers are rare (1000 new cases/year in UK). Majority are of epidermal origin Age: 60 -75 years. 90 -95% of Vulval cancer are of Squamous origin. Melanoma of the vulva is second most common type (4 -9%).

Aetiology Vulval dermatomes (lichen sclerosis): a common Vulval inflammatory dermatosis (HPV 16 & 33) affecting older women with ↑chance of malignant progression. Vulval Intraepithelial Neoplasia (VIN) : 80% will lead to invasive cancer at 10 years if not treated & 7 -8% if treated. VIN 3 is a pre-invasive condition. Human papilloma virus (HPV): associated with 30% of Vulval cancer & with 80 -90% of Vulval cancer in women less than 50 years of age. Smoking: co-factor of HPV & VIN development. v VIN affects mainly L. minora & perineum.
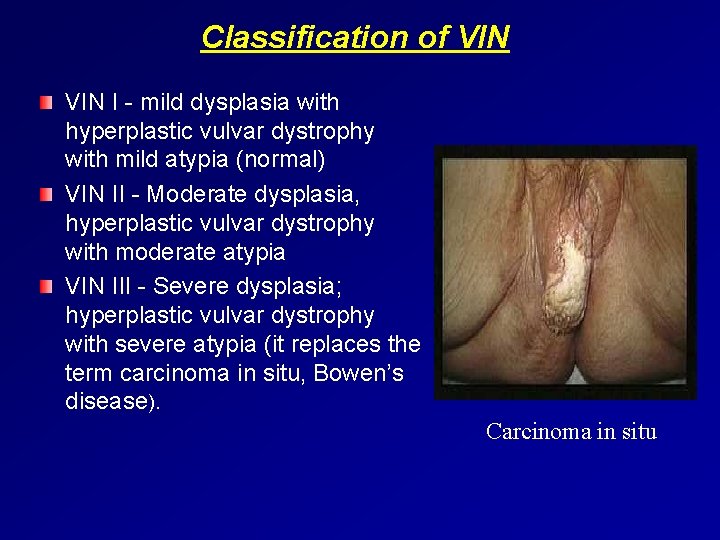
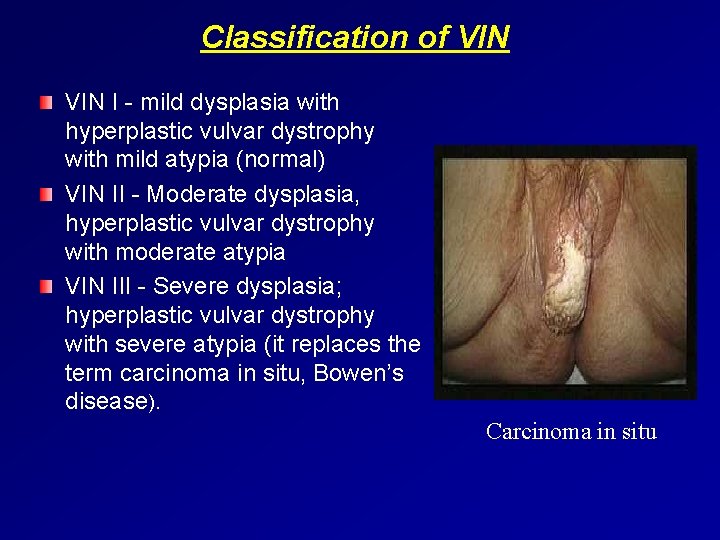
Classification of VIN I - mild dysplasia with hyperplastic vulvar dystrophy with mild atypia (normal) VIN II - Moderate dysplasia, hyperplastic vulvar dystrophy with moderate atypia VIN III - Severe dysplasia; hyperplastic vulvar dystrophy with severe atypia (it replaces the term carcinoma in situ, Bowen’s disease). Carcinoma in situ
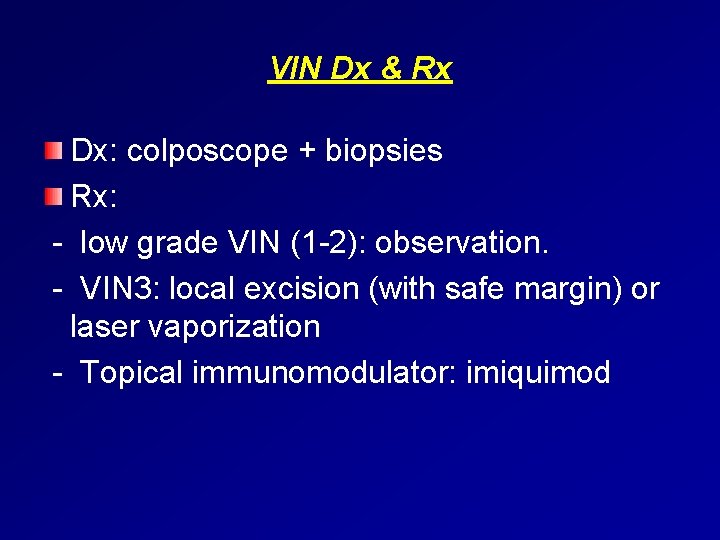
VIN Dx & Rx Dx: colposcope + biopsies Rx: - low grade VIN (1 -2): observation. - VIN 3: local excision (with safe margin) or laser vaporization - Topical immunomodulator: imiquimod
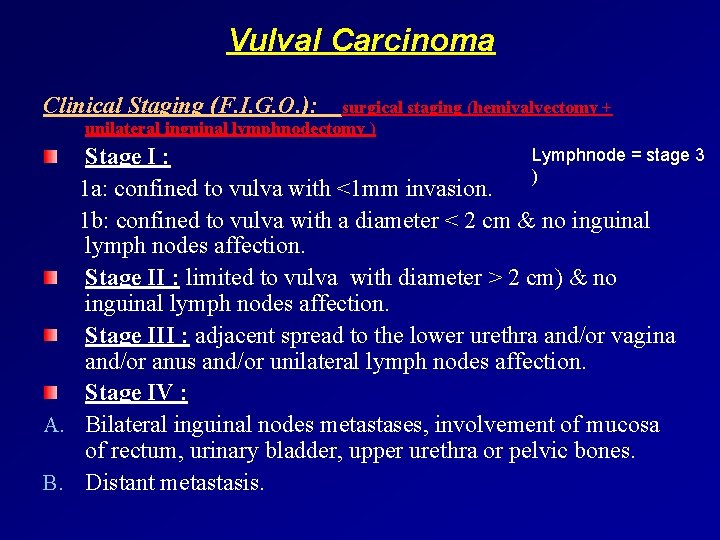
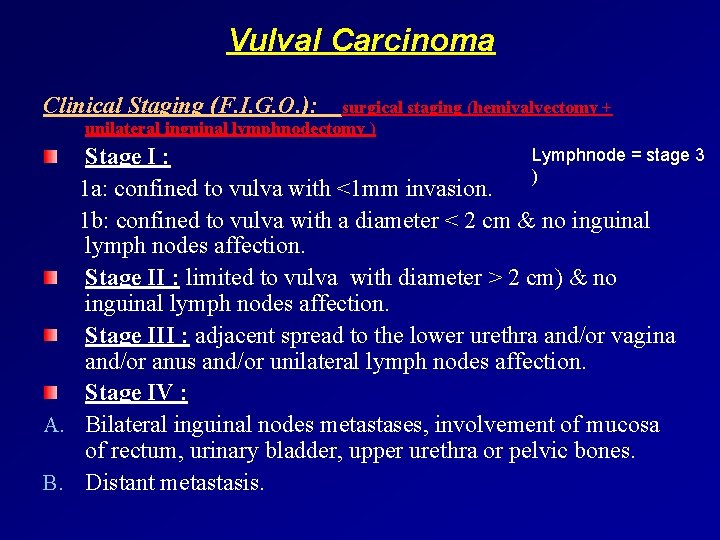
Vulval Carcinoma Clinical Staging (F. I. G. O. ): surgical staging (hemivalvectomy + unilateral inguinal lymphnodectomy ) Lymphnode = stage 3 Stage I : ) 1 a: confined to vulva with <1 mm invasion. 1 b: confined to vulva with a diameter < 2 cm & no inguinal lymph nodes affection. Stage II : limited to vulva with diameter > 2 cm) & no inguinal lymph nodes affection. Stage III : adjacent spread to the lower urethra and/or vagina and/or anus and/or unilateral lymph nodes affection. Stage IV : A. Bilateral inguinal nodes metastases, involvement of mucosa of rectum, urinary bladder, upper urethra or pelvic bones. B. Distant metastasis.
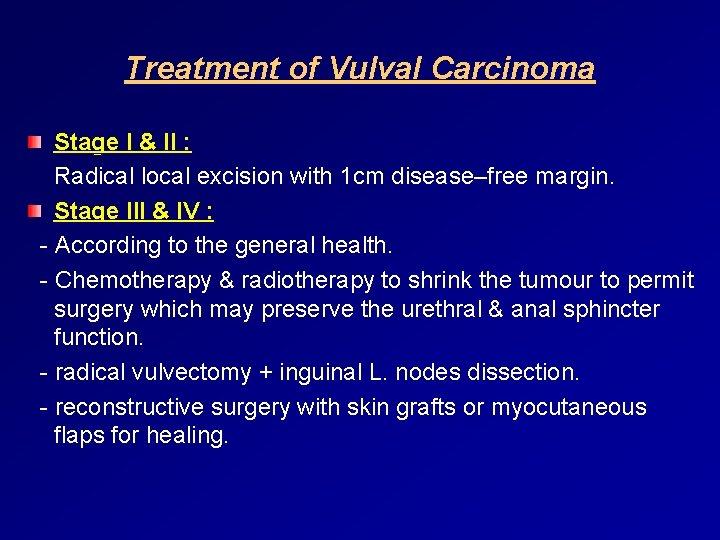
Treatment of Vulval Carcinoma Stage I & II : Radical local excision with 1 cm disease–free margin. Stage III & IV : - According to the general health. - Chemotherapy & radiotherapy to shrink the tumour to permit surgery which may preserve the urethral & anal sphincter function. - radical vulvectomy + inguinal L. nodes dissection. - reconstructive surgery with skin grafts or myocutaneous flaps for healing.

Vaginal Intraepithelial Neoplasia (Va. IN) Extremely uncommon (150 times < CIN). 70% associated with CIN (extension of the transformation zone into the vaginal fornices). Predisposing factors: similar to those of CIN (HPV), but the age of Va. IN is higher than CIN, diethylstilboesterol in utero (metaplastic transformation into the vagina), previous history of CIN), radiotherapy of CA cervix. Va. IN is graded 1 -3 but is less invasive than CIN: - Va. IN 1: mild dysplasia. - Va. IN 2: moderate dysplasia. - Va. IN 3: severe dysplasia. Dx: V. smear, colposcopy, biopsy (even after hysterectomy). Rx: low grade: observation. high grade: excision, 5 fluoroyracil, diathermy. Alternatively, Radiotherapy.
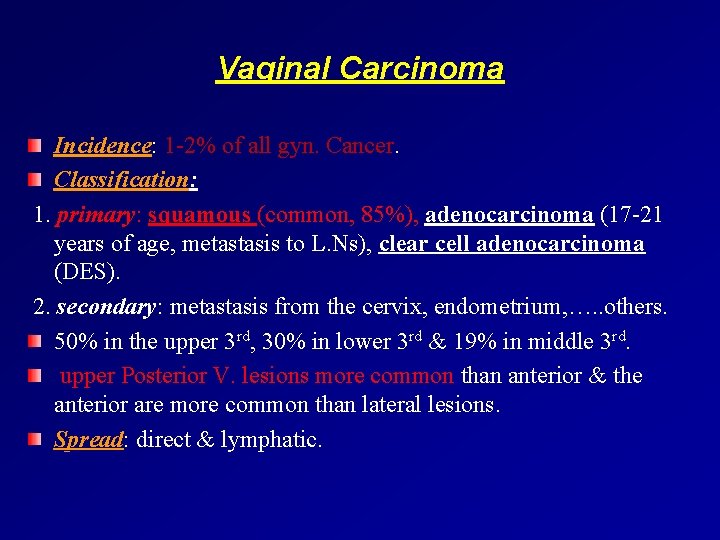
Vaginal Carcinoma Incidence: 1 -2% of all gyn. Cancer. Classification: 1. primary: squamous (common, 85%), adenocarcinoma (17 -21 years of age, metastasis to L. Ns), clear cell adenocarcinoma (DES). 2. secondary: metastasis from the cervix, endometrium, …. . others. 50% in the upper 3 rd, 30% in lower 3 rd & 19% in middle 3 rd. upper Posterior V. lesions more common than anterior & the anterior are more common than lateral lesions. Spread: direct & lymphatic.
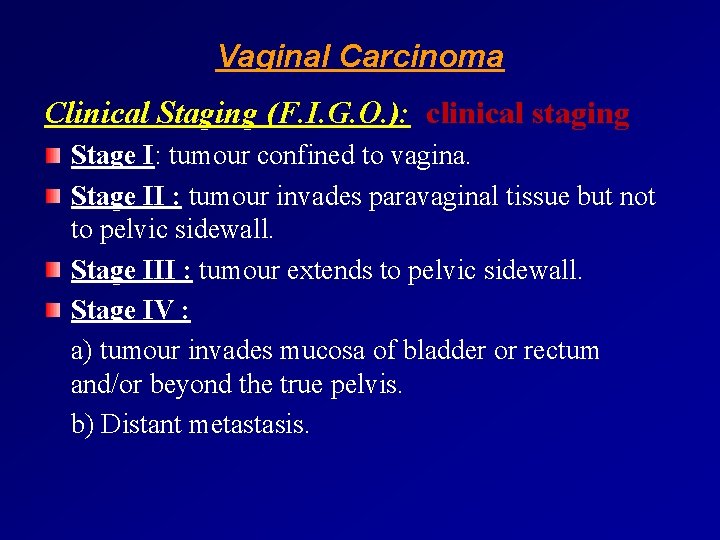
Vaginal Carcinoma Clinical Staging (F. I. G. O. ): clinical staging Stage I: tumour confined to vagina. Stage II : tumour invades paravaginal tissue but not to pelvic sidewall. Stage III : tumour extends to pelvic sidewall. Stage IV : a) tumour invades mucosa of bladder or rectum and/or beyond the true pelvis. b) Distant metastasis.
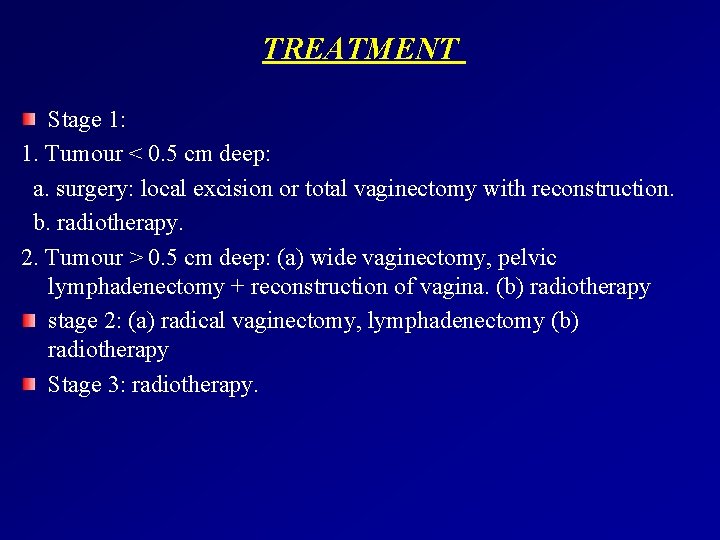
TREATMENT Stage 1: 1. Tumour < 0. 5 cm deep: a. surgery: local excision or total vaginectomy with reconstruction. b. radiotherapy. 2. Tumour > 0. 5 cm deep: (a) wide vaginectomy, pelvic lymphadenectomy + reconstruction of vagina. (b) radiotherapy stage 2: (a) radical vaginectomy, lymphadenectomy (b) radiotherapy Stage 3: radiotherapy.
 Describing skin lesions
Describing skin lesions Apical periodontitis
Apical periodontitis It projektov�� mana����r pr��ca
It projektov�� mana����r pr��ca Rubrospinal tract
Rubrospinal tract Lésions
Lésions Dont touch lesion
Dont touch lesion Esophagus
Esophagus Scattered white matter lesions
Scattered white matter lesions Visual fields
Visual fields Mount classification of dental caries
Mount classification of dental caries Pie on the floor visual field defect
Pie on the floor visual field defect Vesiculobullous lesions
Vesiculobullous lesions Vagus nerve lesion
Vagus nerve lesion Pustule
Pustule Eye lesions
Eye lesions Amiante
Amiante Extrapyramidal vs pyramidal
Extrapyramidal vs pyramidal Clinical features of burns
Clinical features of burns Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Oral pathology
Oral pathology Olneys lesions
Olneys lesions White lesions
White lesions White lesions
White lesions Hymen
Hymen Clue cells
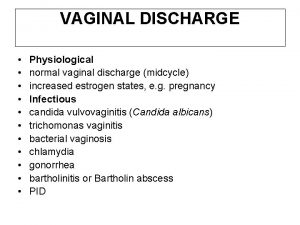
Clue cells Jonction squamo cylindrique
Jonction squamo cylindrique