PREMALIGNANT LESION OF ORAL CAVITY AND ESOPHAGUS Prof






















- Slides: 83
PREMALIGNANT LESION OF ORAL CAVITY AND ESOPHAGUS Prof Mandira Sharma
Benign Mucosal Lesions of the Oral Cavity
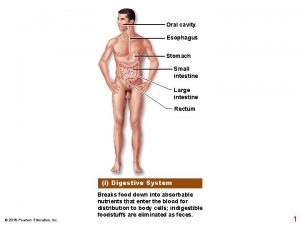
Infections of the Oral Cavity � � � Bacteria, spirochetes, viruses, fungi, and parasites are normal in the oral cavity and are usually harmless. The following terms are used to describe localized inflammation of the oral cavity: Cheilitis (lips) Gingivitis (gum) Glossitis (tongue) Stomatitis (oral mucosa)
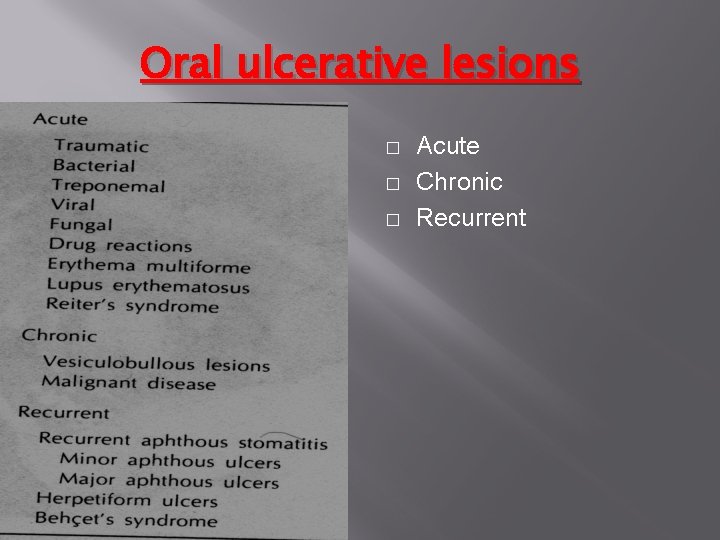
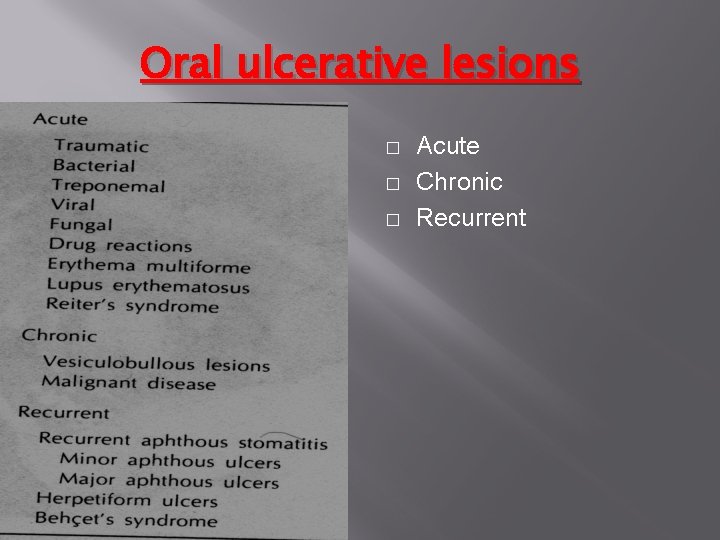
Oral ulcerative lesions � � � Acute Chronic Recurrent
Bacterial and Fungal Infections Commonly Affect the Oral Cavity � APHTHOUS STOMATITIS : Aphthous stomatitis is a common disease characterized by painful, recurrent, solitary or multiple, small ulcers of oral mucosa. � ACUTE NECROTIZING ULCERATIVE GINGIVITIS � LUDWIG ANGINA: Ludwig angina is a rapidly spreading cellulites � CANDIDIASIS: Also termed thrush or moniliasis, candidiasis is caused by Candida albicans � HERPES SIMPLEX VIRUS TYPE 1 (HSV-1) HUMAN PAPILLOMAVIRUS (HPV): EPSTEIN-BARR VIRUS (EBV) � OTHER VIRAL INFECTIONS: Coxsackie � � virus causes herpangina, an acute vesicular oropharyngitis.

Oral candidiasis. White plaques coat mucous membranes of the oral cavity.

Preneoplastic or Epithelial Precursor Lesions: � � � Premalignant lesions include leukoplakia, Erythroplakia, speckled leukoplakia. The terms reflecting the presence of a white, red, or mixed white/red lesion, respectively. Leukoplakia is an asymptomatic white lesion on the surface of a mucous membrane.
Preneoplastic or Epithelial Precursor Lesions: � � Some of these lesions undergo transformation to squamous cell carcinoma. As a preneoplastic lesion, the causes of leukoplakia are diverse and include use of tobacco products, alcoholism, and local irritation.
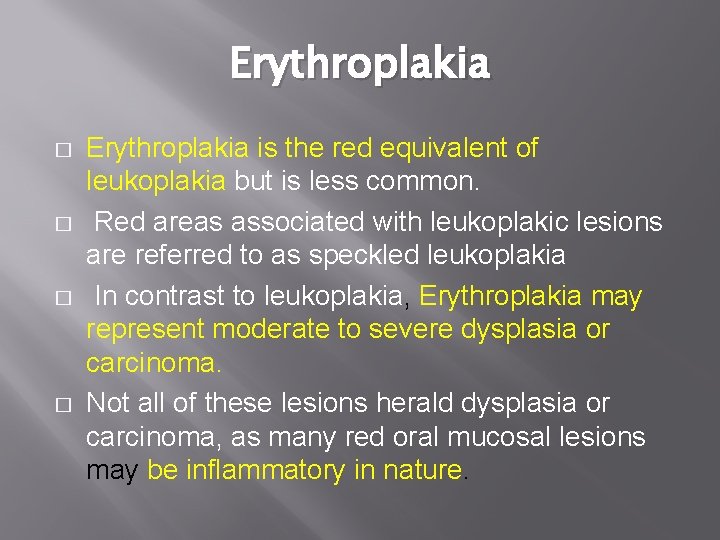
Erythroplakia � � Erythroplakia is the red equivalent of leukoplakia but is less common. Red areas associated with leukoplakic lesions are referred to as speckled leukoplakia In contrast to leukoplakia, Erythroplakia may represent moderate to severe dysplasia or carcinoma. Not all of these lesions herald dysplasia or carcinoma, as many red oral mucosal lesions may be inflammatory in nature.
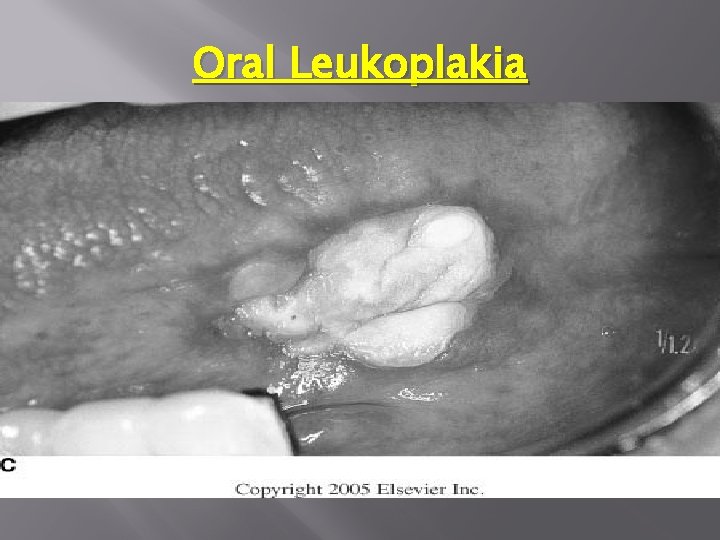
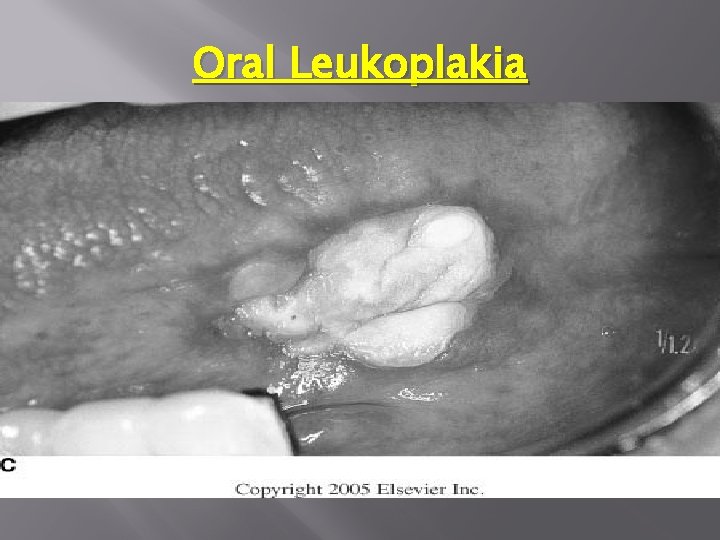
Oral Leukoplakia
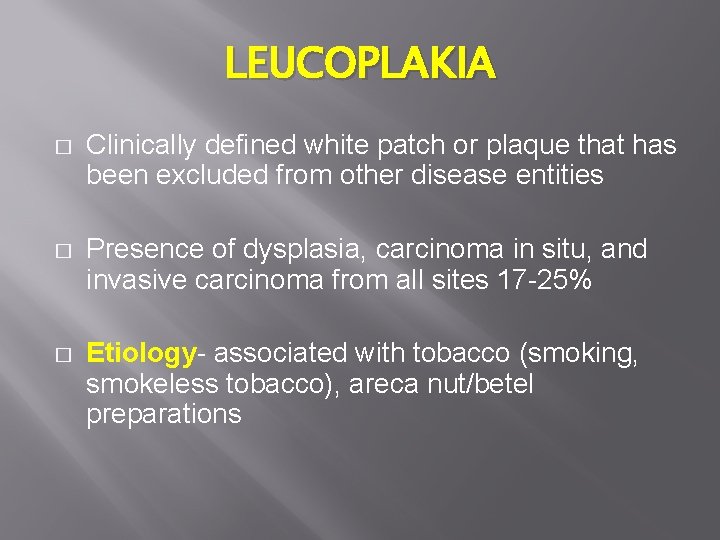
LEUCOPLAKIA � Clinically defined white patch or plaque that has been excluded from other disease entities � Presence of dysplasia, carcinoma in situ, and invasive carcinoma from all sites 17 -25% � Etiology- associated with tobacco (smoking, smokeless tobacco), areca nut/betel preparations

LEUCOPLAKIA � May be macular, slightly elevated, ulcerative, erosive, speckled, nodular, or verrucous � Clinical shift in appearance from homogenous to heterogeneous, speckled, or nodular, a rebiopsy is mandatory � Correlation between increasing levels of dysplasia and increases in regional heterogeneity or speckled quality
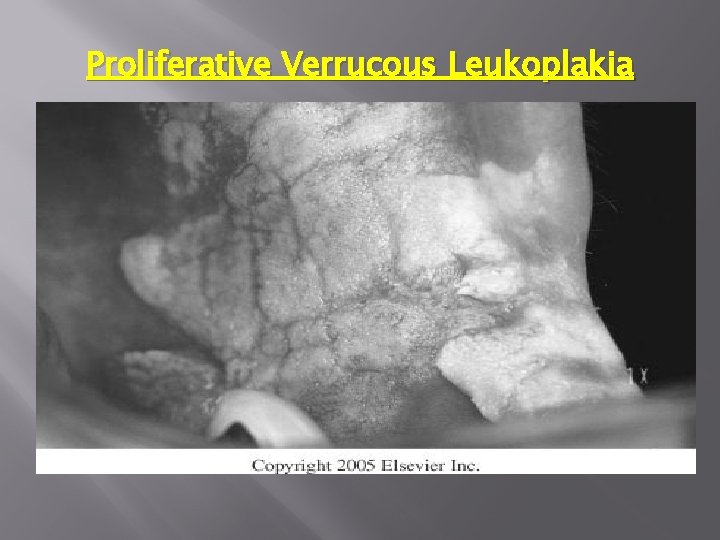
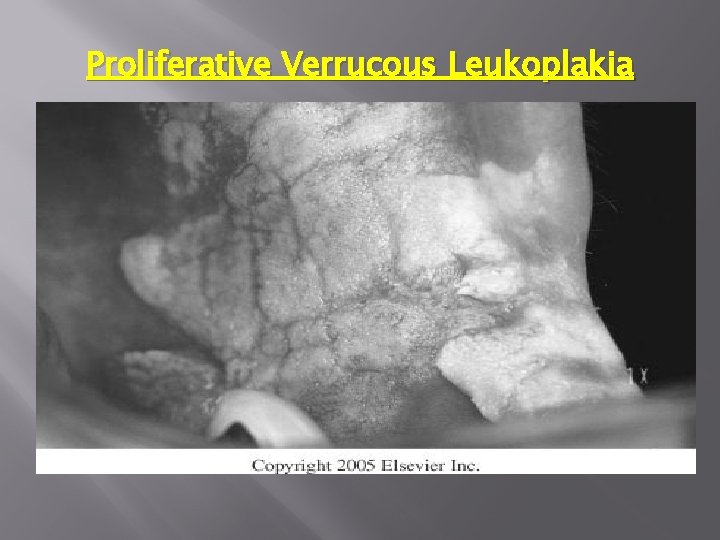
Proliferative Verrucous Leukoplakia
VERRUCOUS LEUCOPLAKIA � � Uncommon variant of leukoplakia Multifocal, occurring more in women, and in those without the usual risk factors Evolution from a thin, flat white patch to leathery, then papillary to verrucous Development of squamous cell CA in over 70% of cases

LEUCOPLAKIA Site of Leukoplakia � � � Risk of dysplasia/carcinoma higher with floor of mouth, Ventro lateral tongue, retro molar trig one, soft palate than with other oral sites
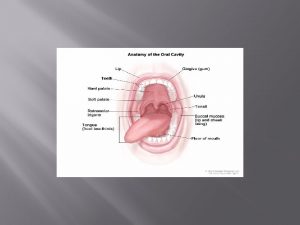
TONGUE The tongue is a mobile muscular organ can assume a variety of shapes and positions. The tongue is partly in the oral cavity and partly in the pharynx. At rest it occupies essentially all the oral cavity proper.
Tongue The main functions: Forming words during speaking Squeezing food into the pharynx when swallowing Other functions: Taste deglutition articulation oral cleaning
Conditions of the TONGUE � Congenital abnormities � Glossitis � Ulceration of the tongue � Neoplasms of the tongue
Congenital abnormalities � Aglossia � Bifid tongue � Ankyloglossia (tongue tie) � Congenital furrowing � Macroglossia (e. g. , idiots, cretins and lymphangiomas) � Lingual thyroid
(Tongue tie) � Commonly Congenital in origin and due to short frenulum linguae. It is common cause of speech defect. � The tongue is bent down to the floor of the mouth and its movements are impaired.

Tumors of Tongue NEOPLASM OF TONGUE

Tumors Of Tongue Benign Tumors � Haemangioma � Papilloma � Lymphangioma � Lipoma � Neurofibroma � Osteoma � Juvenile fibrous Carcinoma (sq. cell carcinoma) of the tongue
CA Tongue Cancer of the tongue common in male around the age of 50 years (50 -70 years) predisposing causes: � Chronic irritation by smoking, sepsis, spices and spirits (alcohol). � Pre-cancerous lesions which include syphilis, ch. superficial glossitis, dental ulcers and papilloma. � Poor oral hygiene and mal-nutrition. � Betel chewing.
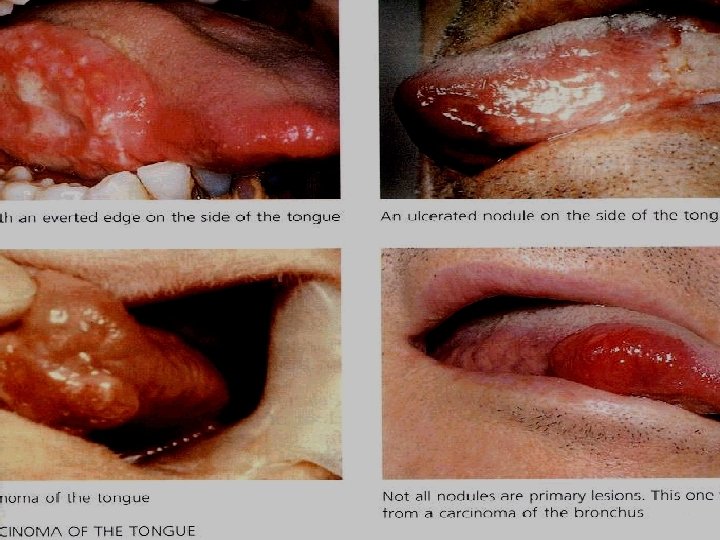
SITE� Two-thirds of the tongue cancer arise in the ant. 2/3 rd and 1/3 rd in the posterior part. � The commonest sites are the sides of the ant. 2/3 rd of the tongue. � Posterior tumors are much more to be in the midline.

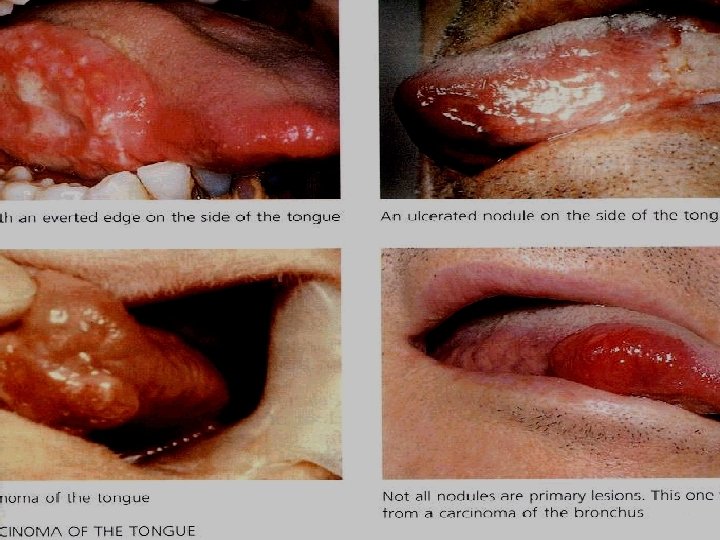
GROSS� The tumor usually occurs as malignant ulcer. � Less often it take, the form of hard sub mucous nodule or deep fissure. � Rarely it occurs as diffuse hard infiltration of whole tongue. (wooden tongue)

Histology The tumor is carcinoma. . usually Squamous cell
Spread of carcinoma of the TONGUE � Local (direct to the floor of the mouth, gums and pharynx). � Lymphatic spread. � Blood spread (very rare)

The patient may seek advice because of mass or ulcer in the tongue. � Profuse salvation and foul breathing � Severe haemorrhage � Fixation of the tongue (ankyloglossia) � Alteration of the voice � Lump of glands in the neck � Dysphagia � PAIN
PROGNOSIS � For patient with LN negative with tumors in the ant. 2/3 rd there is 50%, 5 years survival. � For patient with posterior 1/3 rd of the tongue with negative LN 20 -25%, 5 years survival.
General Concepts - Neoplasia � Named after the type of cell they derived from � Grade is based on differentiation � Well-differentiated - appears very similar to nonneoplastic tissue � Moderately differentiated - retains some resemblance to the cell of origin � Poorly differentiated - difficult to tell histological the cell of origin, may have to perform special stains � Stage is based on extent of invasion and metastases
ESOPHAGUS Pathology of the Esophagus
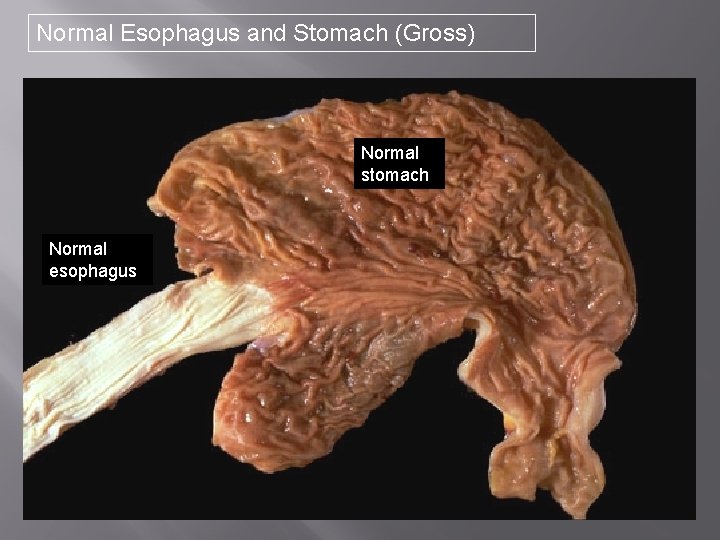
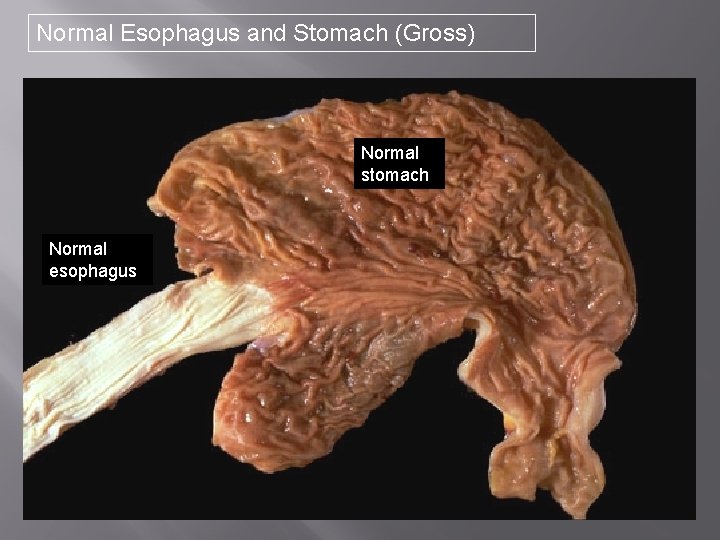
Normal Esophagus and Stomach (Gross) Normal stomach Normal esophagus
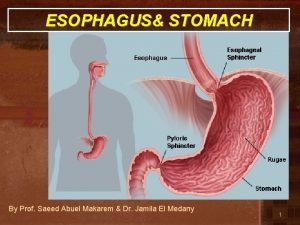
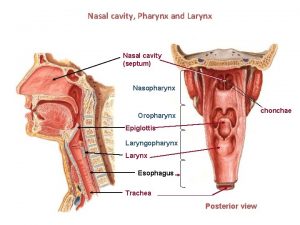
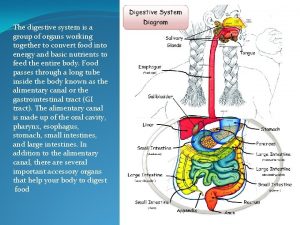
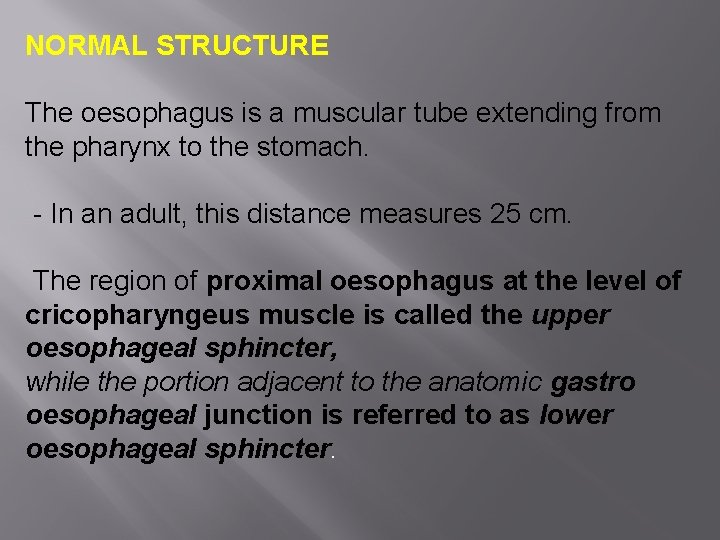
NORMAL STRUCTURE The oesophagus is a muscular tube extending from the pharynx to the stomach. - In an adult, this distance measures 25 cm. The region of proximal oesophagus at the level of cricopharyngeus muscle is called the upper oesophageal sphincter, while the portion adjacent to the anatomic gastro oesophageal junction is referred to as lower oesophageal sphincter.

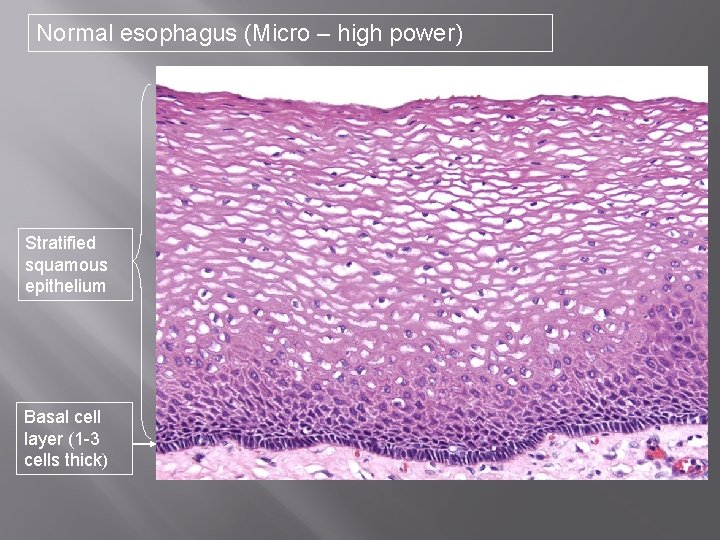
Normal Esophagus (Microscopic) Squamous Epithelium Muscularis mucosa Submucosa Muscular Wall (muscularis propria)
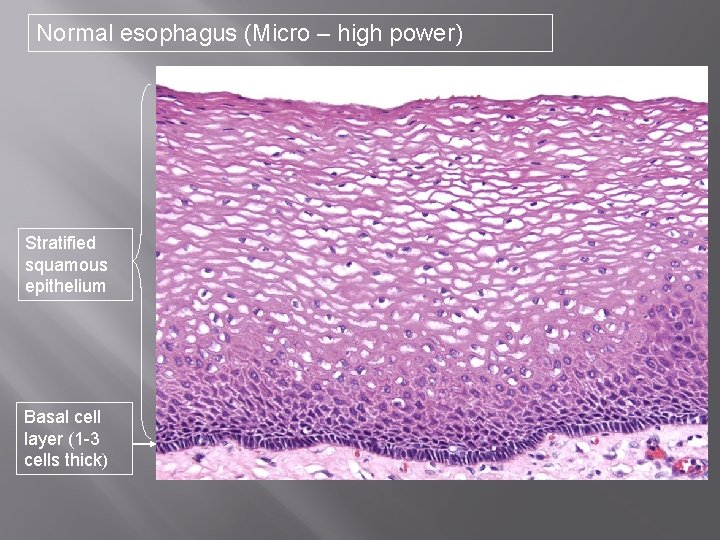
Normal esophagus (Micro – high power) Stratified squamous epithelium Basal cell layer (1 -3 cells thick)
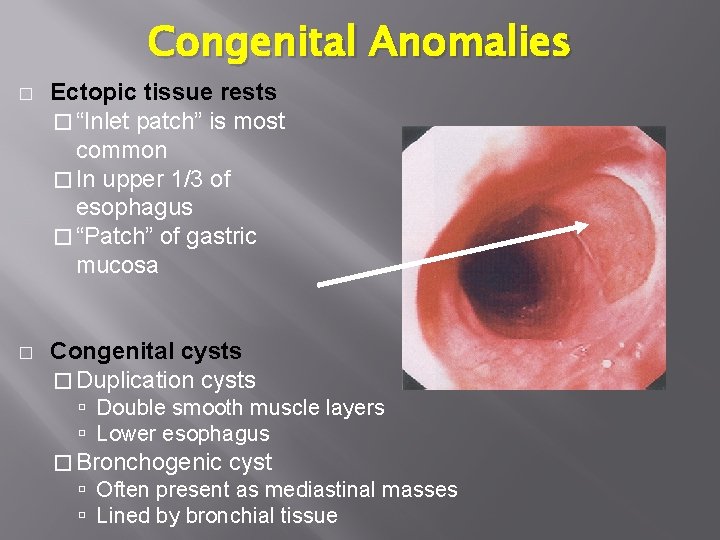
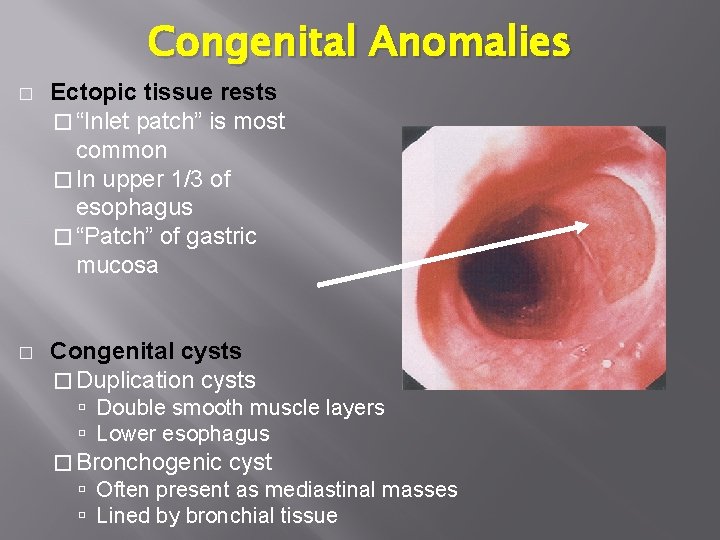
Congenital Anomalies � Ectopic tissue rests � “Inlet patch” is most common � In upper 1/3 of esophagus � “Patch” of gastric mucosa � Congenital cysts � Duplication cysts Double smooth muscle layers Lower esophagus � Bronchogenic cyst Often present as mediastinal masses Lined by bronchial tissue
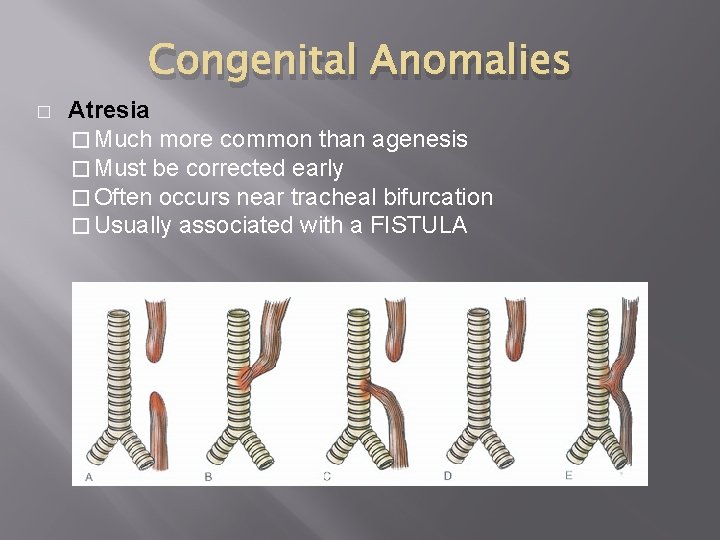
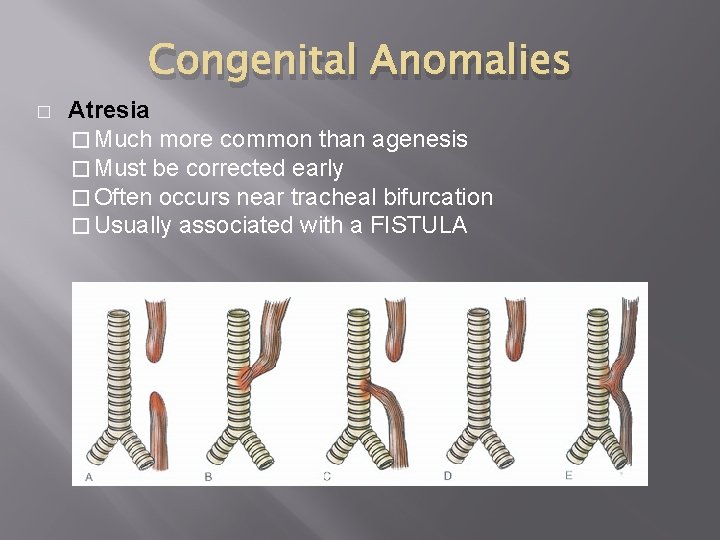
Congenital Anomalies � Atresia � Much more common than agenesis � Must be corrected early � Often occurs near tracheal bifurcation � Usually associated with a FISTULA
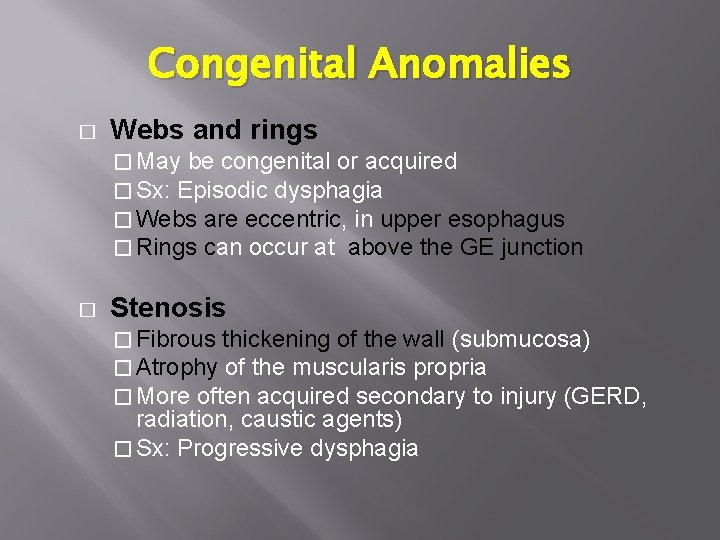
Congenital Anomalies � Webs and rings � May be congenital or acquired � Sx: Episodic dysphagia � Webs are eccentric, in upper esophagus � Rings can occur at above the GE junction � Stenosis � Fibrous thickening of the wall (submucosa) � Atrophy of the muscularis propria � More often acquired secondary to injury (GERD, radiation, caustic agents) � Sx: Progressive dysphagia
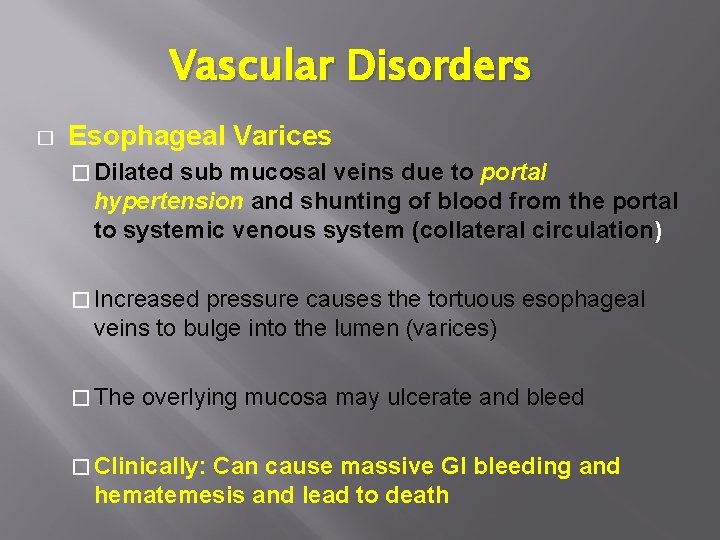
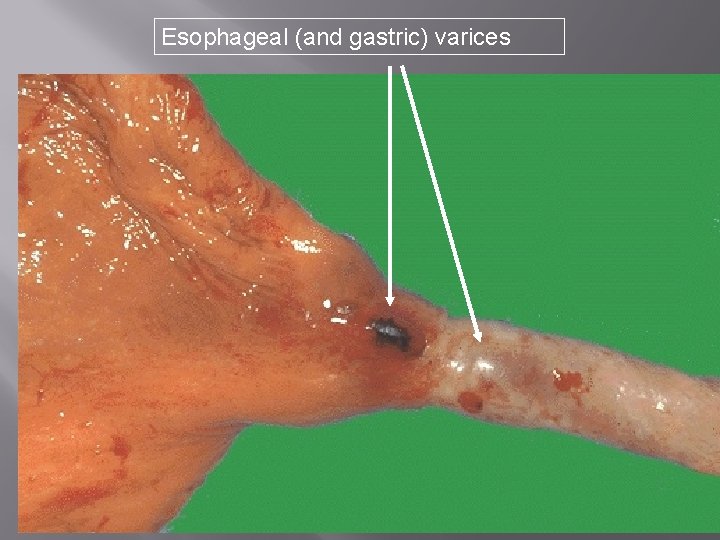
Vascular Disorders � Esophageal Varices � Dilated sub mucosal veins due to portal hypertension and shunting of blood from the portal to systemic venous system (collateral circulation) � Increased pressure causes the tortuous esophageal veins to bulge into the lumen (varices) � The overlying mucosa may ulcerate and bleed � Clinically: Can cause massive GI bleeding and hematemesis and lead to death
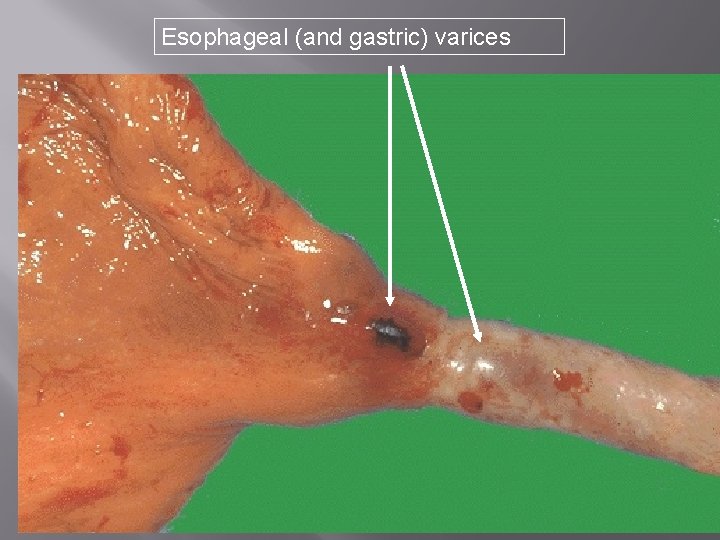
Esophageal (and gastric) varices

Esophagitis � � � “Inflammation of the esophageal mucosa” Clinical Features: Retrosternal pain and dysphagia Causes: � Reactive � Infectious – Candida, Herpes � Toxic – Pill Ulcer, Alkali or Acid � Ingestion The General Pathologic Feature: �Inflammatory cells (eosinophils, neutrophils or lymphocytes) within the epithelium and lamina propria
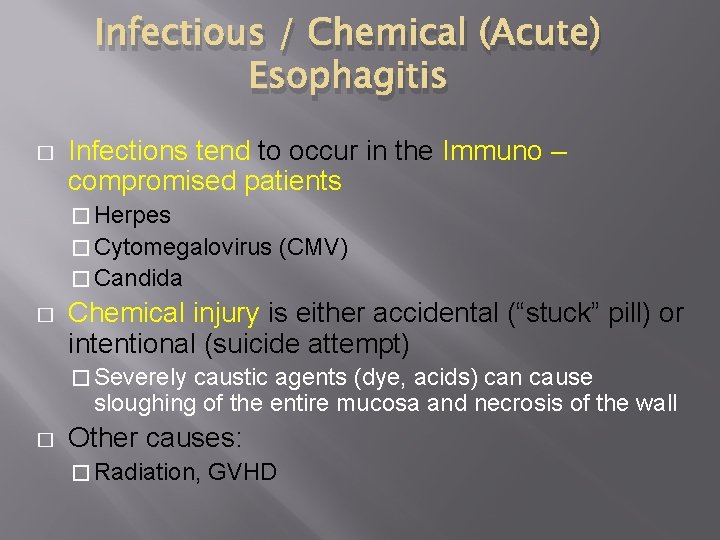
Infectious / Chemical (Acute) Esophagitis � Infections tend to occur in the Immuno – compromised patients � Herpes � Cytomegalovirus (CMV) � Candida � Chemical injury is either accidental (“stuck” pill) or intentional (suicide attempt) � Severely caustic agents (dye, acids) can cause sloughing of the entire mucosa and necrosis of the wall � Other causes: � Radiation, GVHD
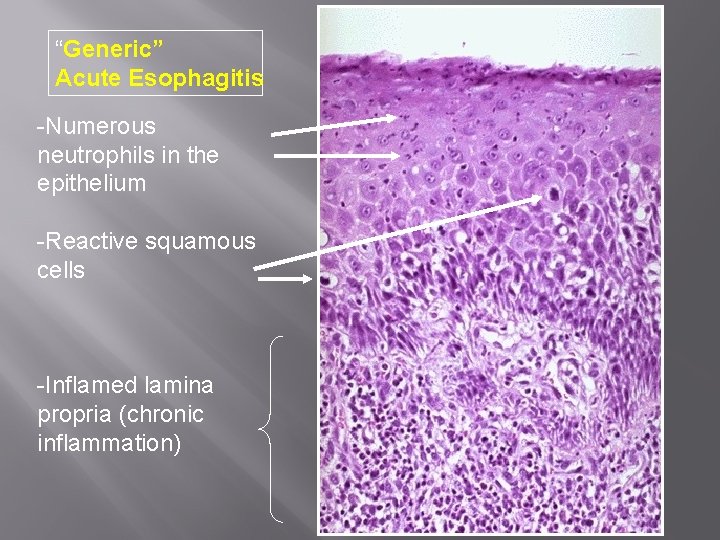
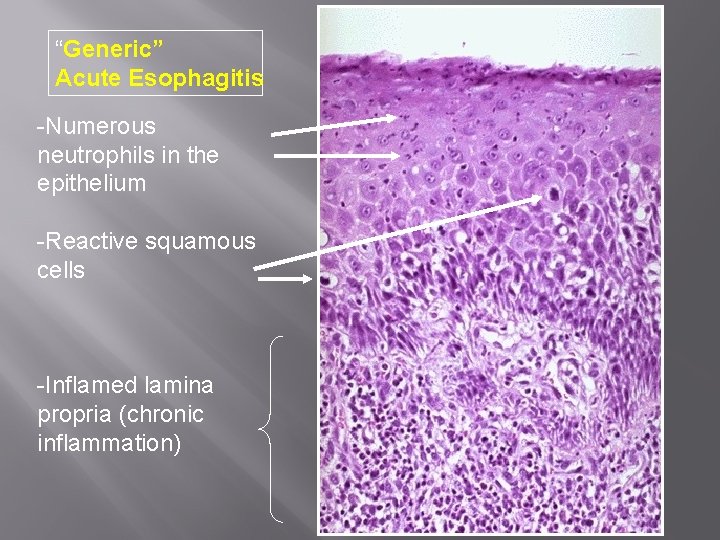
“Generic” Acute Esophagitis -Numerous neutrophils in the epithelium -Reactive squamous cells -Inflamed lamina propria (chronic inflammation)
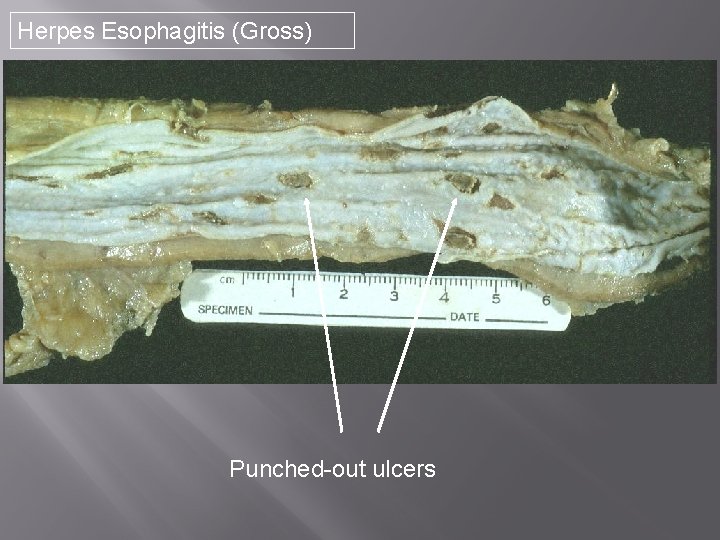
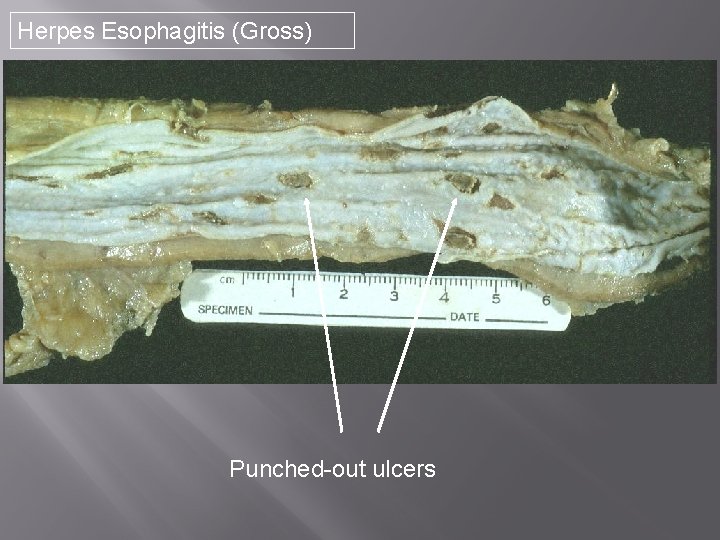
Herpes Esophagitis (Gross) Punched-out ulcers

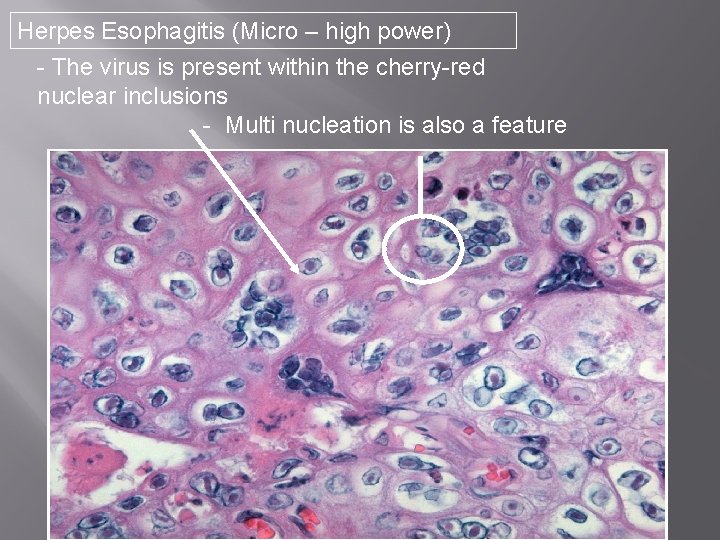
Herpes Esophagitis (Micro) (See next slide) Edge of ulcer
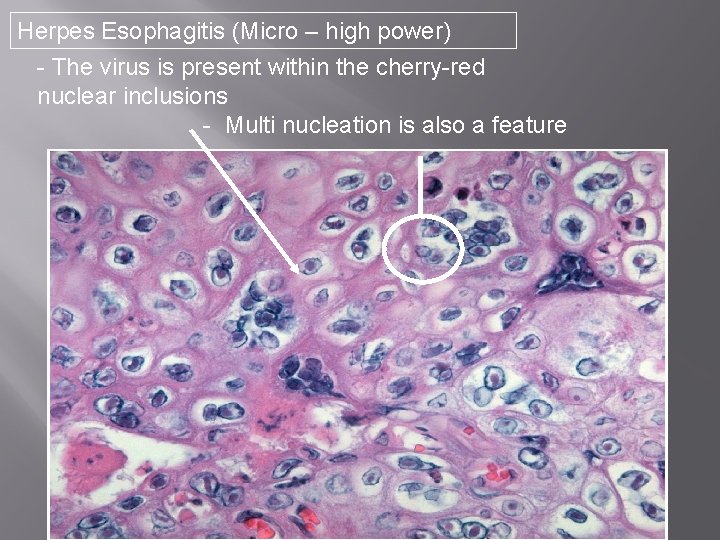
Herpes Esophagitis (Micro – high power) - The virus is present within the cherry-red nuclear inclusions - Multi nucleation is also a feature

Eosinophilic Esophagitis � � � “Increased intraepithelial eosinophils in the esophagus” First described in children; incidence appears to be increasing in adults (especially in young men) Etiology & Pathogenesis: � Unknown; � may be related to food or airborne allergies Symptoms: � Longstanding dysphagia with solid foods � Food impaction � GERD Sx without improvement on therapy
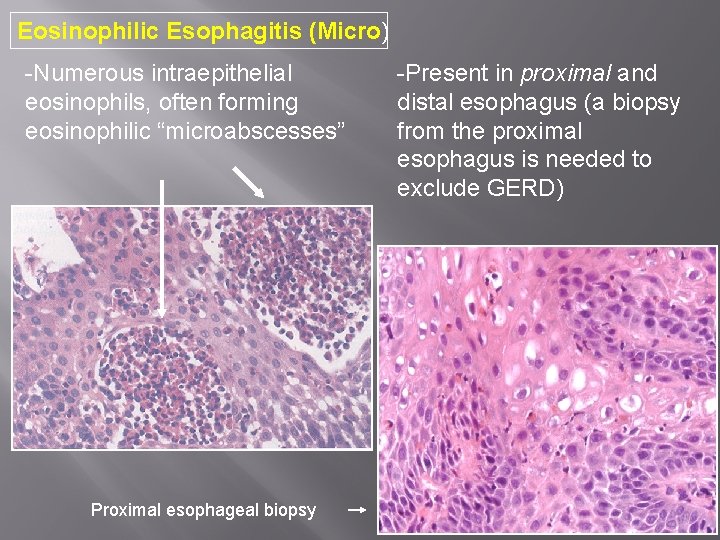
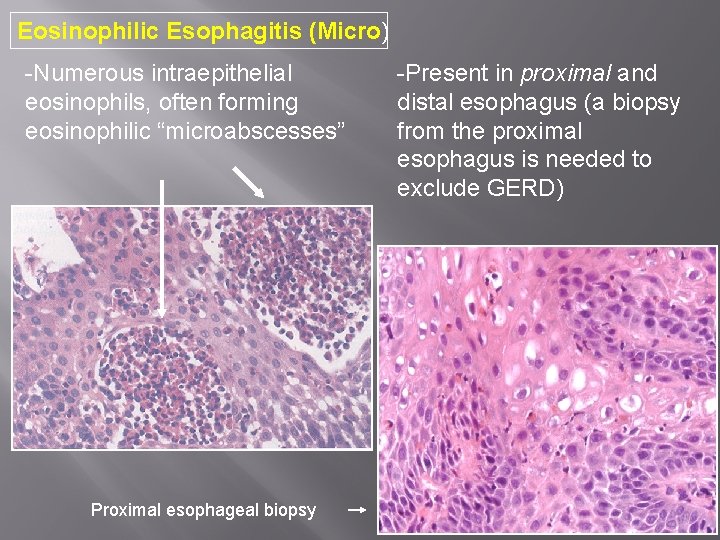
Eosinophilic Esophagitis (Micro) -Numerous intraepithelial eosinophils, often forming eosinophilic “microabscesses” Proximal esophageal biopsy -Present in proximal and distal esophagus (a biopsy from the proximal esophagus is needed to exclude GERD)
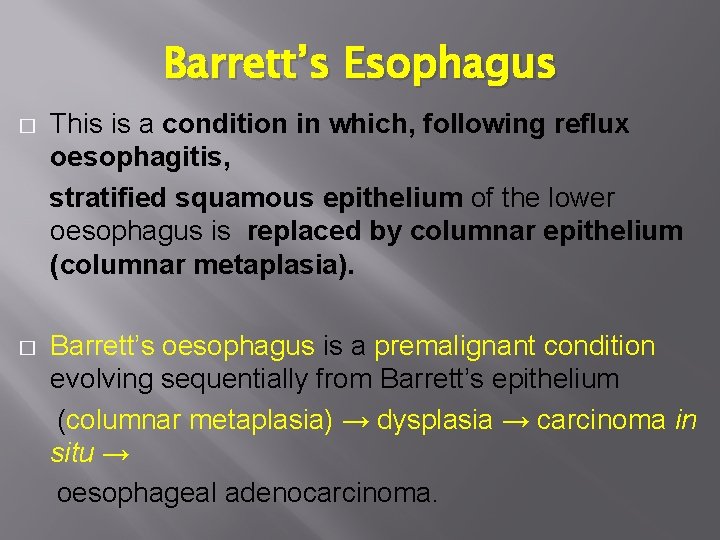
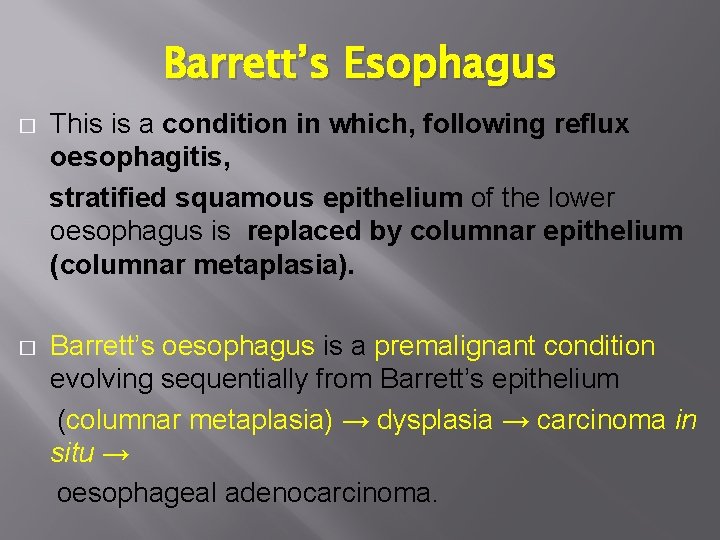
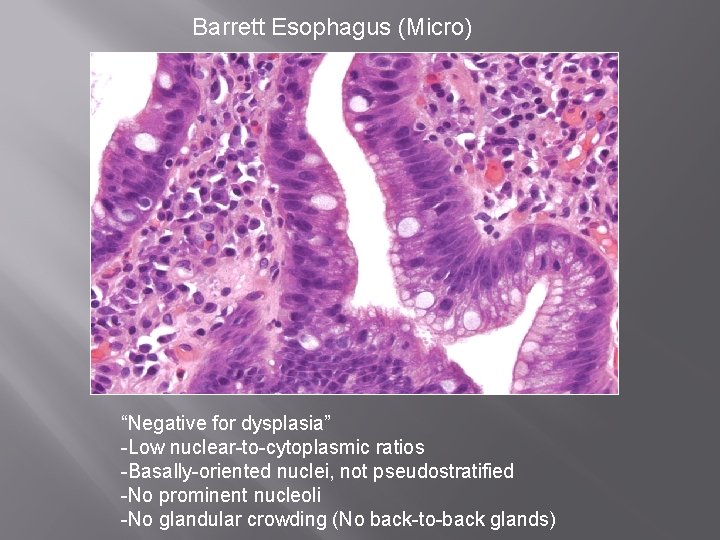
Barrett’s Esophagus � This is a condition in which, following reflux oesophagitis, stratified squamous epithelium of the lower oesophagus is replaced by columnar epithelium (columnar metaplasia). � Barrett’s oesophagus is a premalignant condition evolving sequentially from Barrett’s epithelium (columnar metaplasia) → dysplasia → carcinoma in situ → oesophageal adenocarcinoma.

Barrett’s Esophagus � Single most important risk factor for esophageal adenocarcinoma �Patients with >3 cm of Barrett mucosa have a 30 x 40 x increased risk of developing cancer � A complication of longstanding GERD �Chronic mucosal injury causes the squamous mucosa to change into intestinal-type mucosa with goblet cells (“intestinal metaplasia” / “specialized metaplasia”)
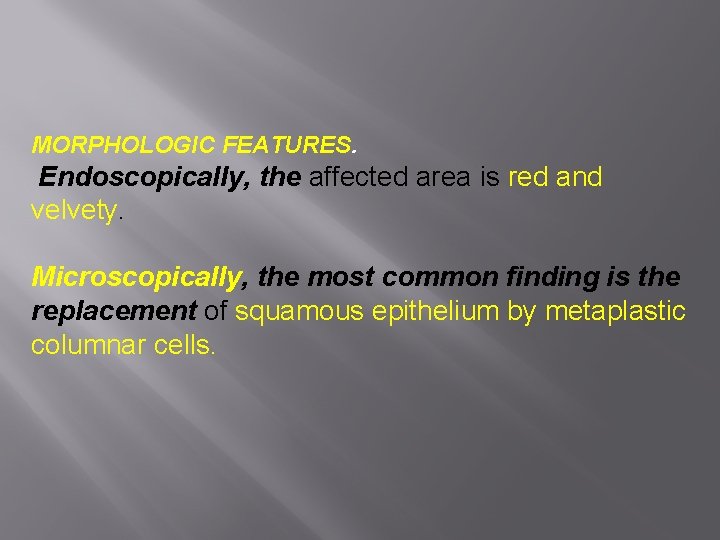
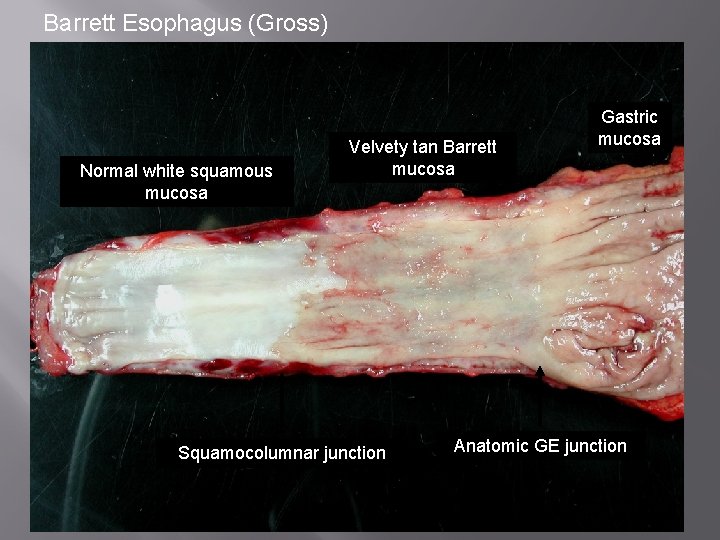
MORPHOLOGIC FEATURES. Endoscopically, the affected area is red and velvety. Microscopically, the most common finding is the replacement of squamous epithelium by metaplastic columnar cells.
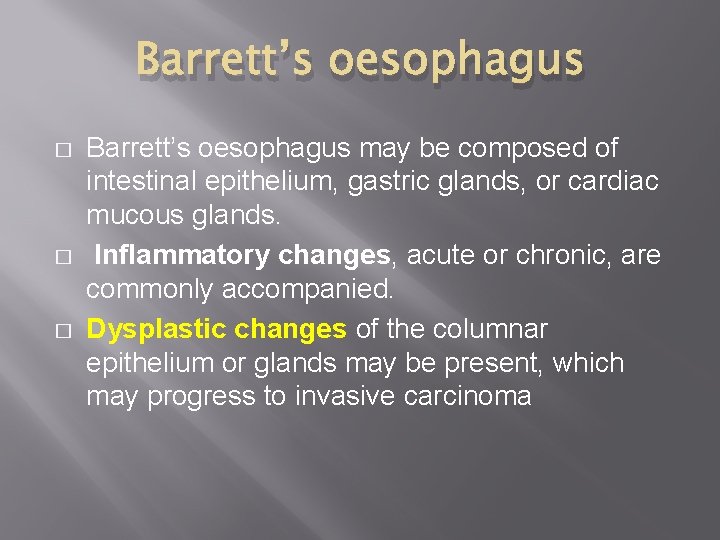
Barrett’s oesophagus � � � Barrett’s oesophagus may be composed of intestinal epithelium, gastric glands, or cardiac mucous glands. Inflammatory changes, acute or chronic, are commonly accompanied. Dysplastic changes of the columnar epithelium or glands may be present, which may progress to invasive carcinoma
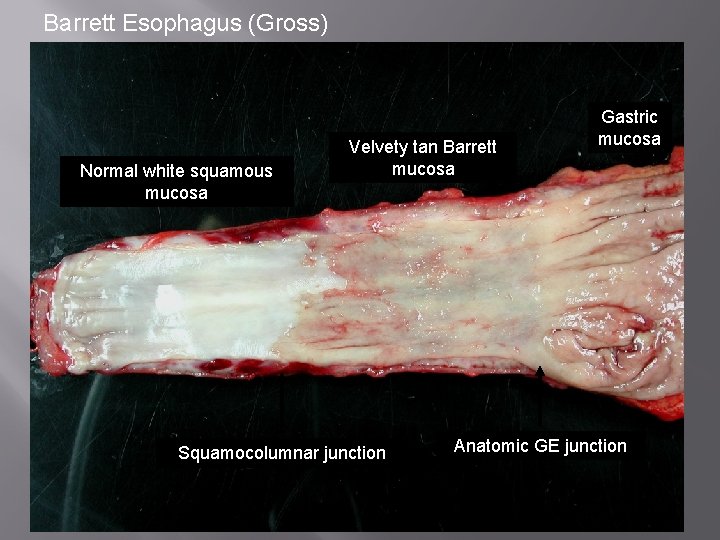
Barrett Esophagus (Gross) Normal white squamous mucosa Velvety tan Barrett mucosa Squamocolumnar junction Gastric mucosa Anatomic GE junction
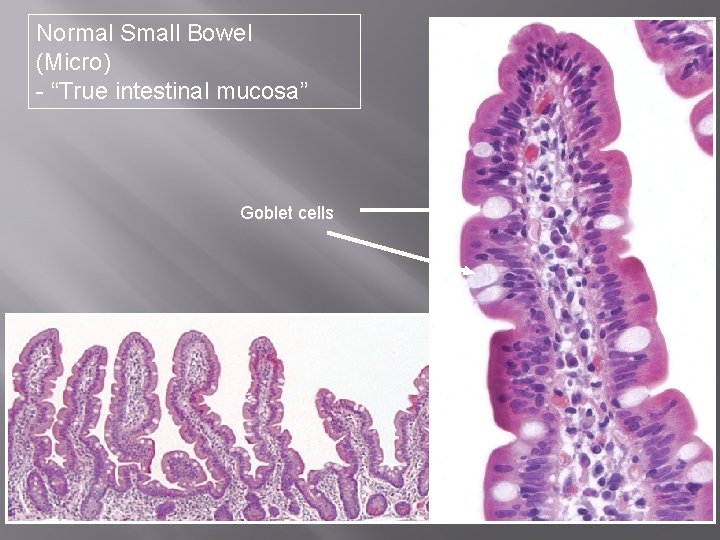
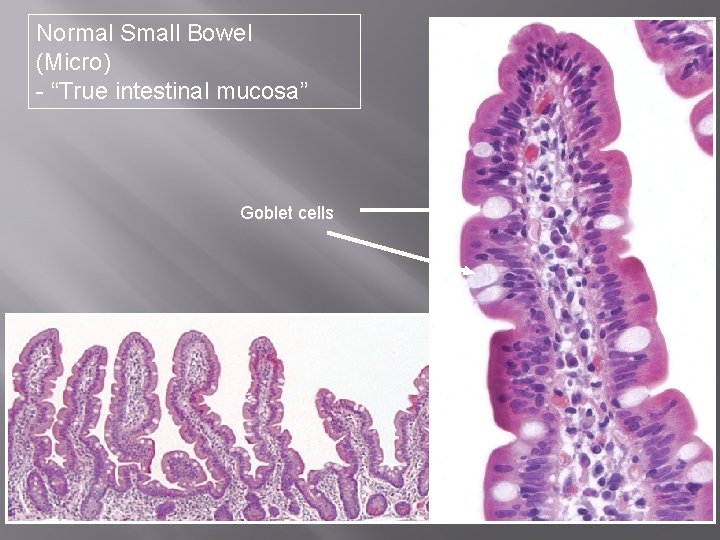
Normal Small Bowel (Micro) - “True intestinal mucosa” Goblet cells

Barrett’s Esophagus (Micro) Squamous mucosa Glandular mucosa with goblet cells
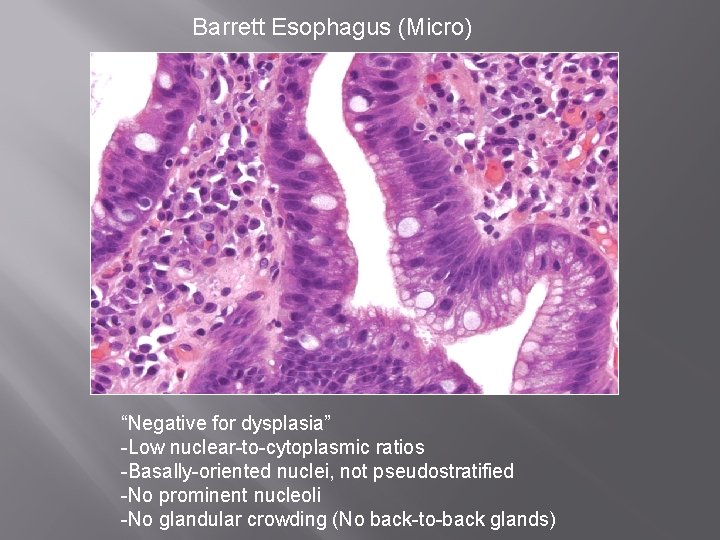
Barrett Esophagus (Micro) “Negative for dysplasia” -Low nuclear-to-cytoplasmic ratios -Basally-oriented nuclei, not pseudostratified -No prominent nucleoli -No glandular crowding (No back-to-back glands)

Barrett Esophagus w/High Grade Dysplasia - High nuclear-to-cytoplasmic ratios - Loss of nuclear polarity with pseudostratification - Loss of goblet cells - Glandular crowding (back-to-back or cribriforming glands)

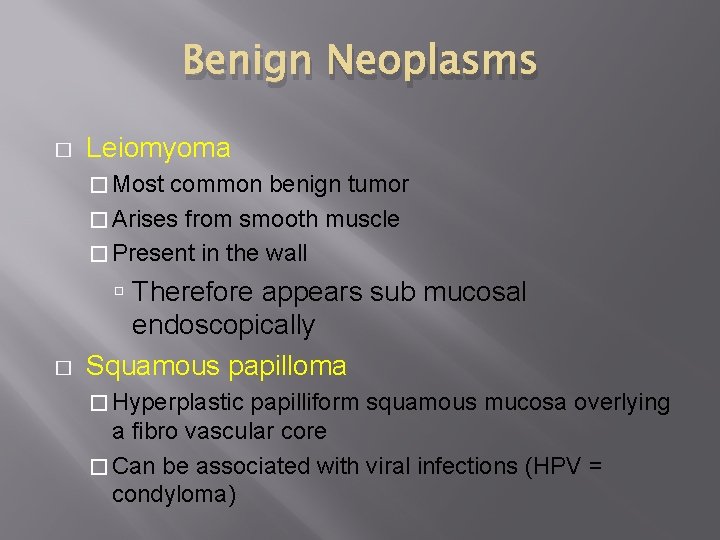
NEOPLASMS � Tumors of the esophagus may be derived from �squamous epithelium (squamous cell carcinoma) �glandular epithelium (adenocarcinoma) �the muscular wall (leiomyoma)
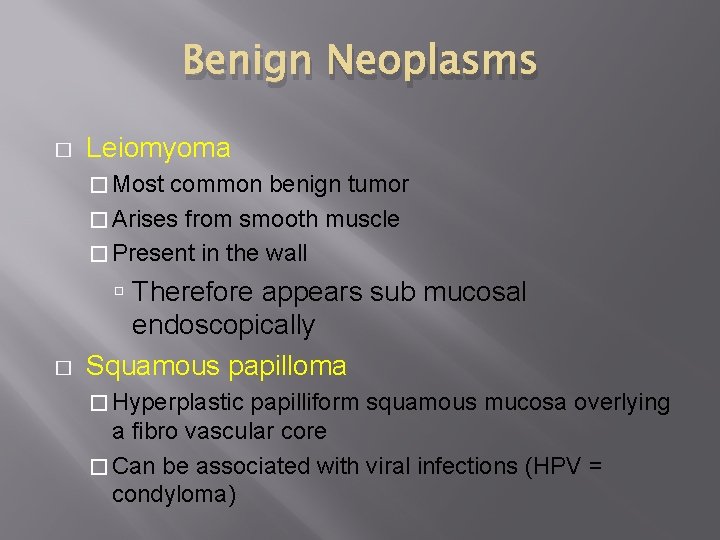
Benign Neoplasms � Leiomyoma � Most common benign tumor � Arises from smooth muscle � Present in the wall � Therefore appears sub mucosal endoscopically Squamous papilloma � Hyperplastic papilliform squamous mucosa overlying a fibro vascular core � Can be associated with viral infections (HPV = condyloma)

Malignant Neoplasms - Squamous Cell Carcinoma � � � � Most common esophageal cancer Incidence: 5 -7/100, 000 M>F 2: 1 to 20: 1 Peak age 50 -60 yrs Mutations in the p 53 gene are common Can involve upper (20%), mid (50%) and lower (30%) esophagus Associations: � Alcohol and tobacco (US, Europe) � Carcinogens in food (China, S. Africa)
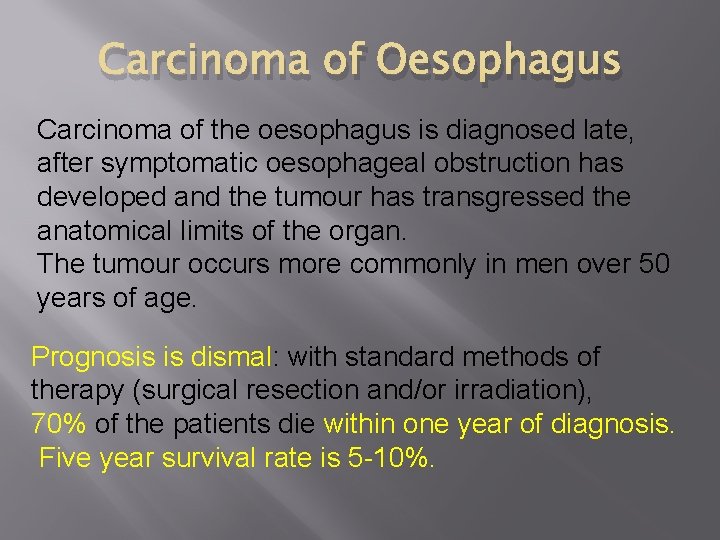
Carcinoma of Oesophagus Carcinoma of the oesophagus is diagnosed late, after symptomatic oesophageal obstruction has developed and the tumour has transgressed the anatomical limits of the organ. The tumour occurs more commonly in men over 50 years of age. Prognosis is dismal: with standard methods of therapy (surgical resection and/or irradiation), 70% of the patients die within one year of diagnosis. Five year survival rate is 5 -10%.

ETIOLOGY. Although exact etiology of carcinoma of the oesophagus is not known, a number of conditions and factors have been implicated as under: 1. Diet and personal habits: i) Heavy smoking ii) Alcohol consumption iii) Intake of foods contaminated with fungus iv) Nutritional deficiency of vitamins and trace elements. 2. Oesophageal disorders: i) Oesophagitis (especially Barrett’s oesophagus in adenocarcinoma) ii) Achalasia iii) Hiatus hernia iv) Diverticula v) Plummer-Vinson syndrome.
3. Other factors: i) Race—more common in the Chinese and Japanese than in Western races; more frequent in blacks than whites. ii) Family history—association with tylosis iii) Genetic factors—predisposition with coeliac disease, epidermolysis bullosa, tylosis. iv) HPV infection—is the recent addition in etiologic factors. At molecular level, abnormality of p 53 tumour suppressor gene has been found associated with a number of above risk factors, notably with consumption of tobacco and alcohol, and in cases having proven Barrett’s oesophagus.
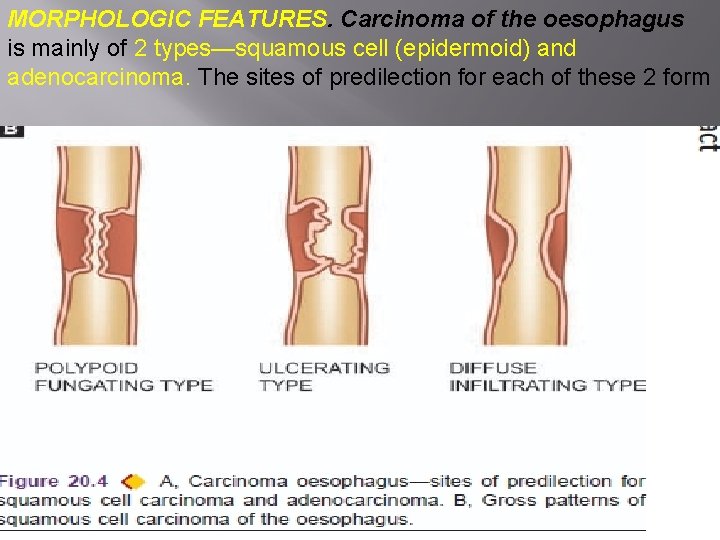
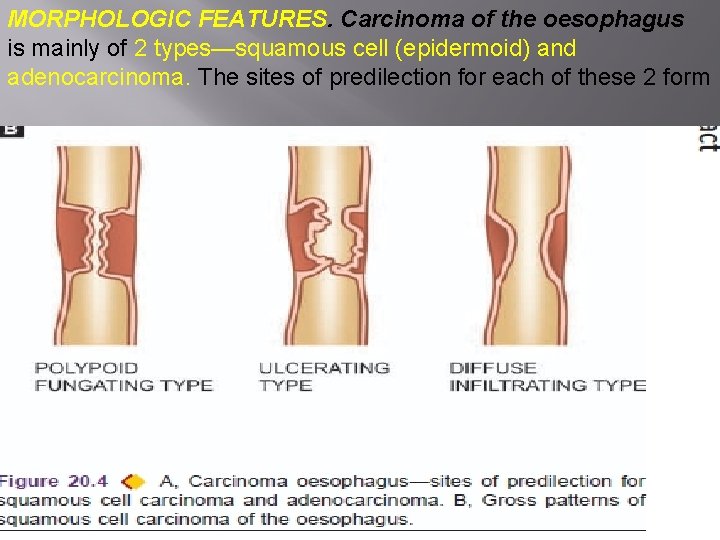
MORPHOLOGIC FEATURES. Carcinoma of the oesophagus is mainly of 2 types—squamous cell (epidermoid) and adenocarcinoma. The sites of predilection for each of these 2 form
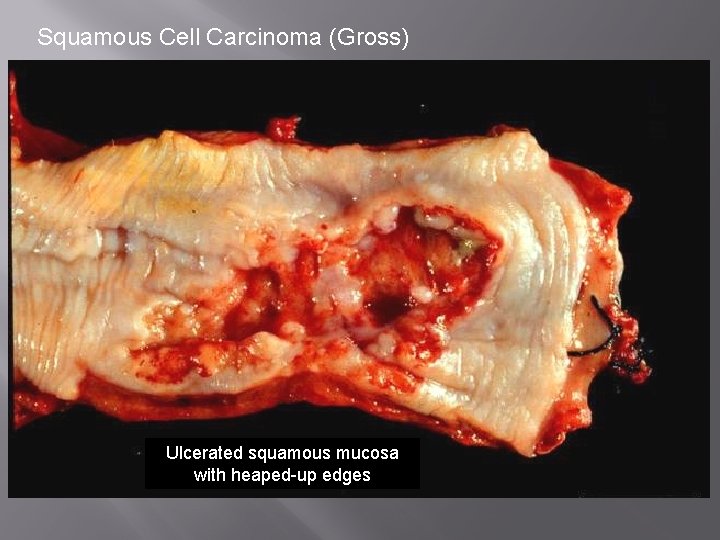
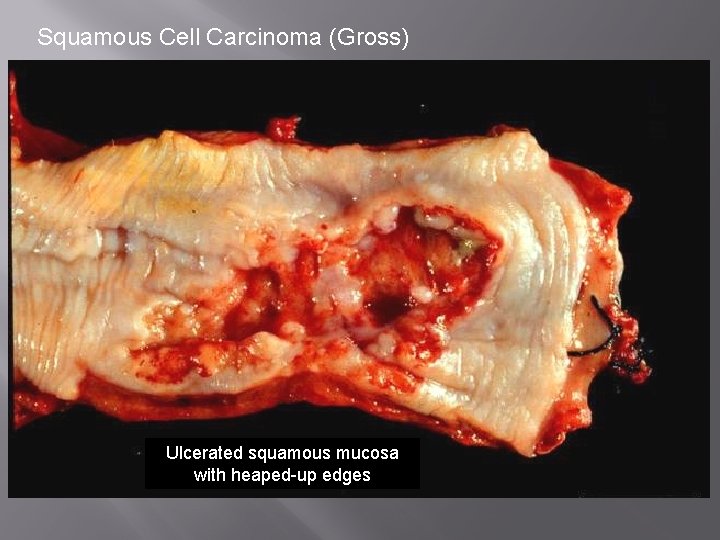
Squamous Cell Carcinoma (Gross) Ulcerated squamous mucosa with heaped-up edges
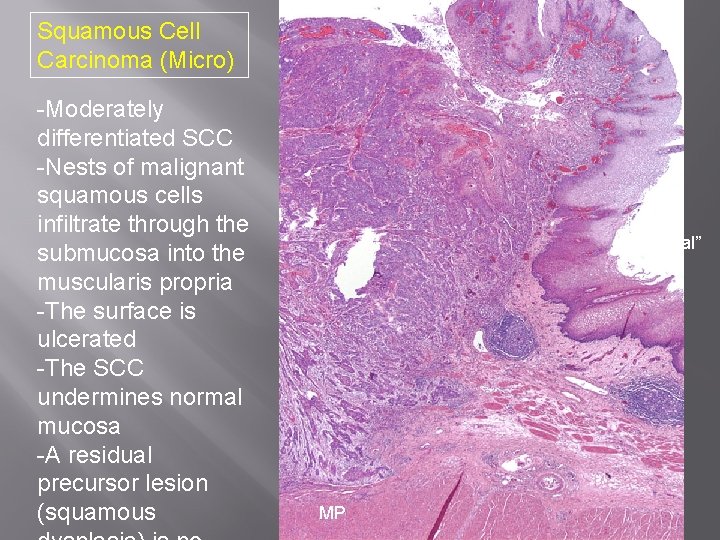
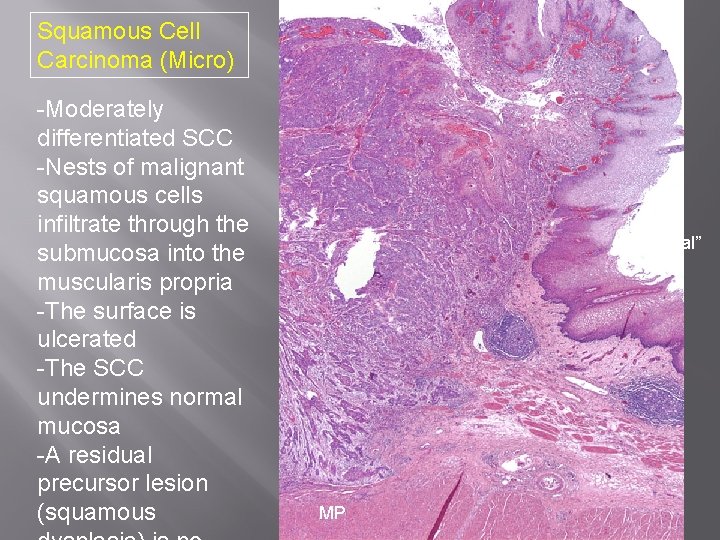
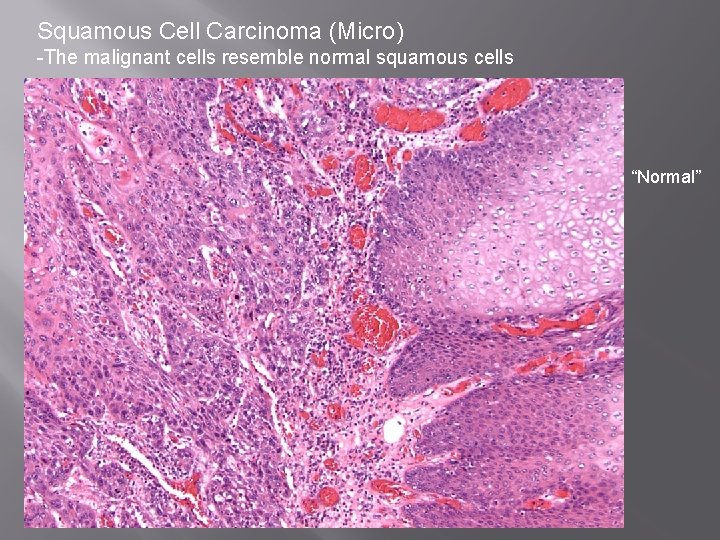
Squamous Cell Carcinoma (Micro) -Moderately differentiated SCC -Nests of malignant squamous cells infiltrate through the submucosa into the muscularis propria -The surface is ulcerated -The SCC undermines normal mucosa -A residual precursor lesion (squamous “Normal” MP
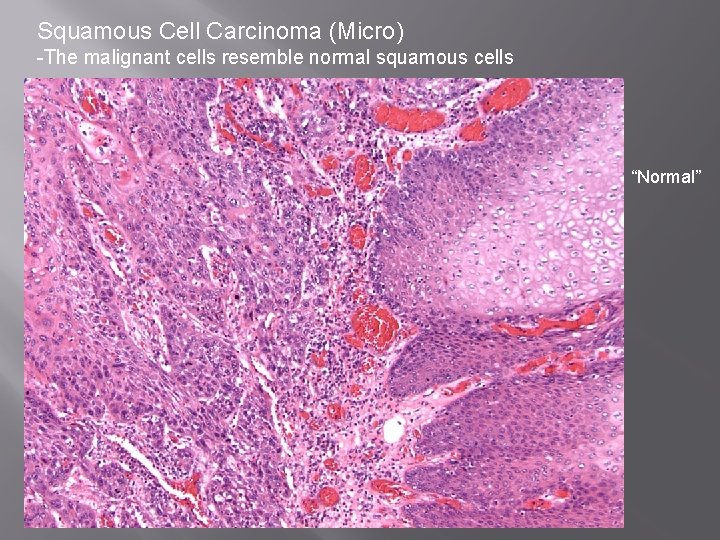
Squamous Cell Carcinoma (Micro) -The malignant cells resemble normal squamous cells “Normal”
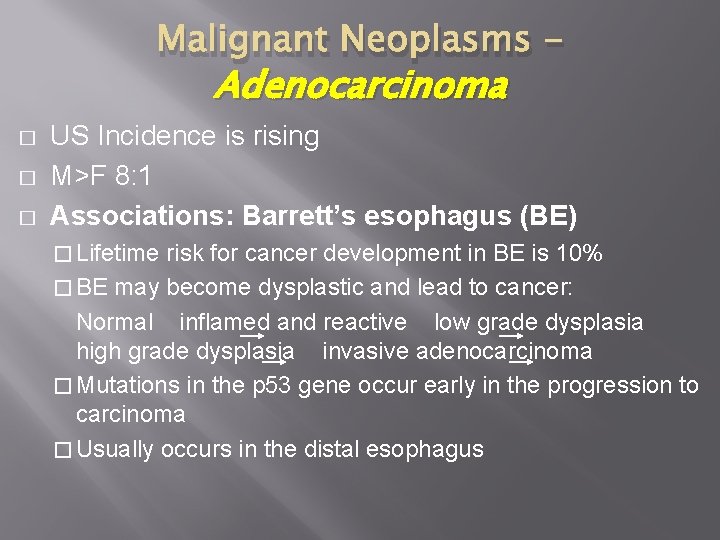
Malignant Neoplasms - Adenocarcinoma � � � US Incidence is rising M>F 8: 1 Associations: Barrett’s esophagus (BE) � Lifetime risk for cancer development in BE is 10% � BE may become dysplastic and lead to cancer: Normal inflamed and reactive low grade dysplasia high grade dysplasia invasive adenocarcinoma � Mutations in the p 53 gene occur early in the progression to carcinoma � Usually occurs in the distal esophagus
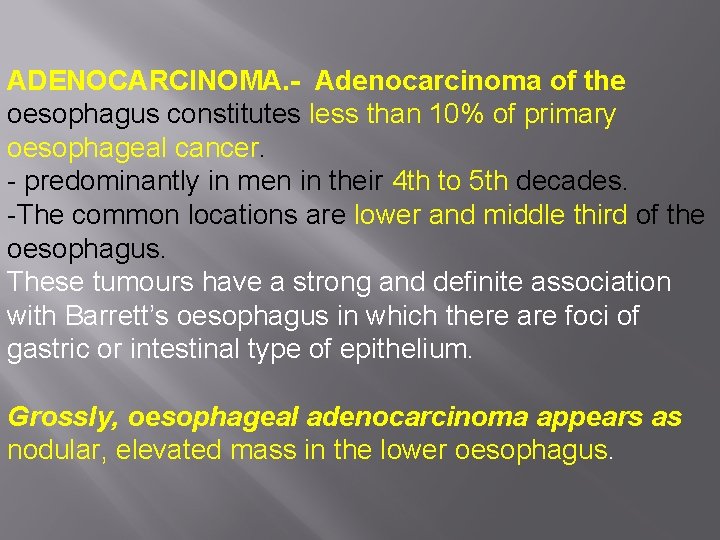
ADENOCARCINOMA. - Adenocarcinoma of the oesophagus constitutes less than 10% of primary oesophageal cancer. - predominantly in men in their 4 th to 5 th decades. -The common locations are lower and middle third of the oesophagus. These tumours have a strong and definite association with Barrett’s oesophagus in which there are foci of gastric or intestinal type of epithelium. Grossly, oesophageal adenocarcinoma appears as nodular, elevated mass in the lower oesophagus.

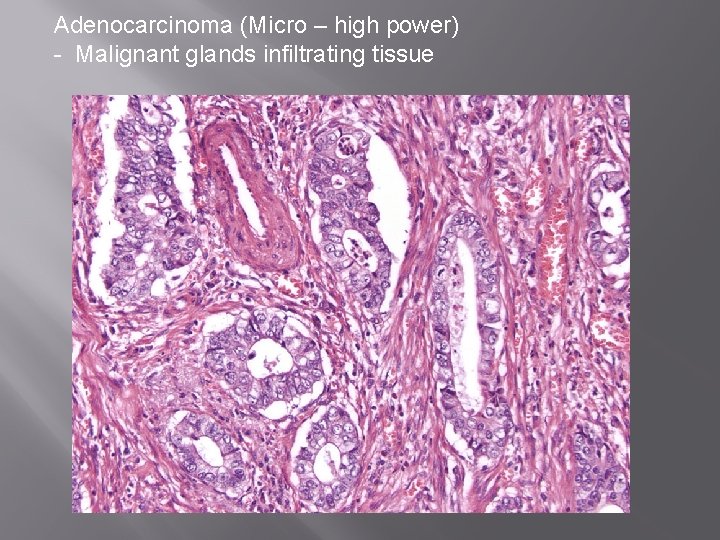
Microscopically, adenocarcinoma of the oesophagus can have 3 patterns: i) Intestinal type—is the adenocarcinoma with a pattern similar to that seen in adenocarcinoma of intestine or stomach. ii) Adenosquamous type—is the pattern in which there is an irregular admixture of adenocarcinoma and squamous cell carcinoma. iii) Adenoid cystic type—is an uncommon variety and is akin to similar growth in salivary gland i. e. a cribriform appearance in an epithelial tumour.
adenocarcinoma � � Adenocarcinoma of the oesophagus must be distinguished from adenocarcinoma of the gastric cardia. This is done by identifying normal oesophageal mucosa on distal as well as proximal margin of the tumour.

Adenocarcinoma (Gross) Gastric mucosa Barrett mucosa Ulcerated mass at the GEJ with heaped-up edges
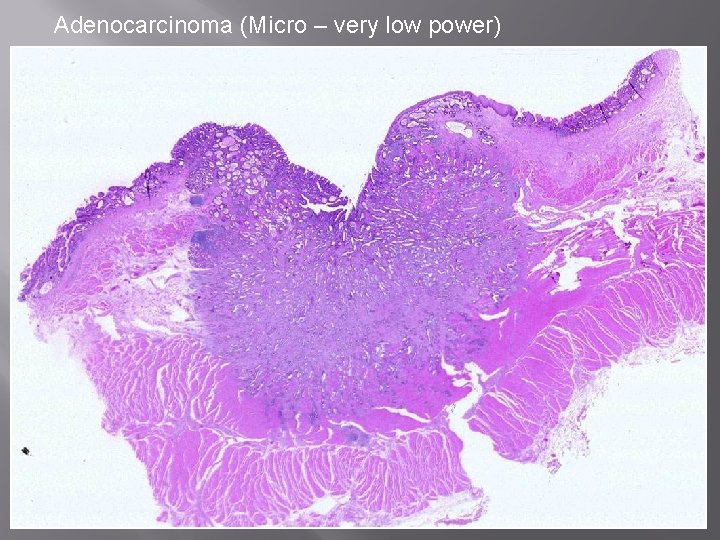
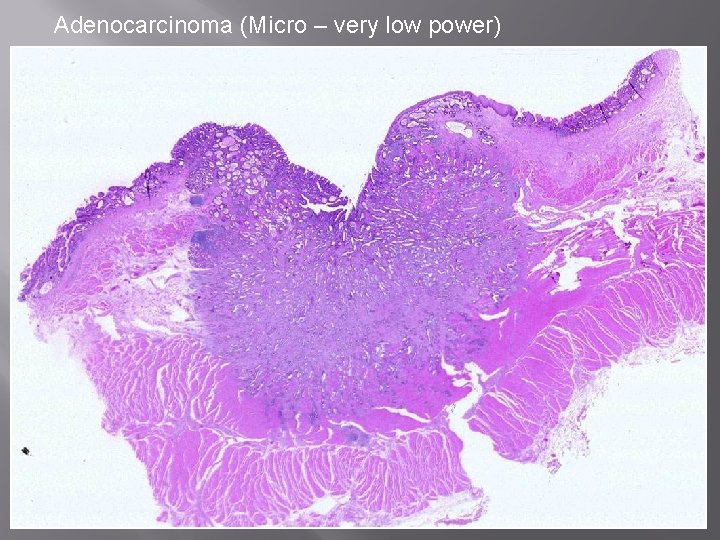
Adenocarcinoma (Micro – very low power)

Adenocarcinoma (Micro – low power) “Normal” -Moderately differentiated adenocarcinoma -Malignant glandular structures infiltrate into submucosa -The surface is ulcerated -A residual precursor lesion (BE with dyspalsia) is no longer present MP
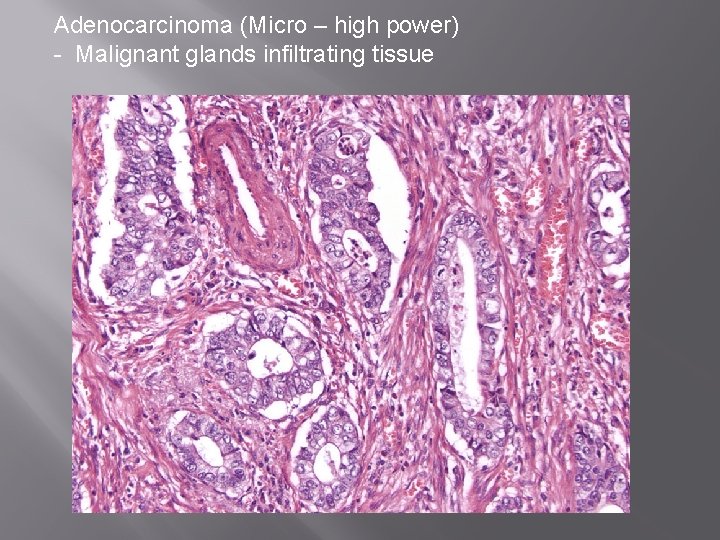
Adenocarcinoma (Micro – high power) - Malignant glands infiltrating tissue
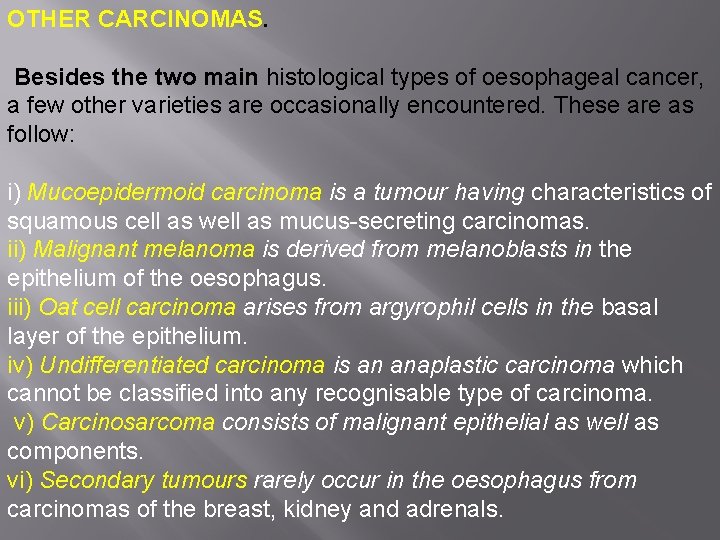
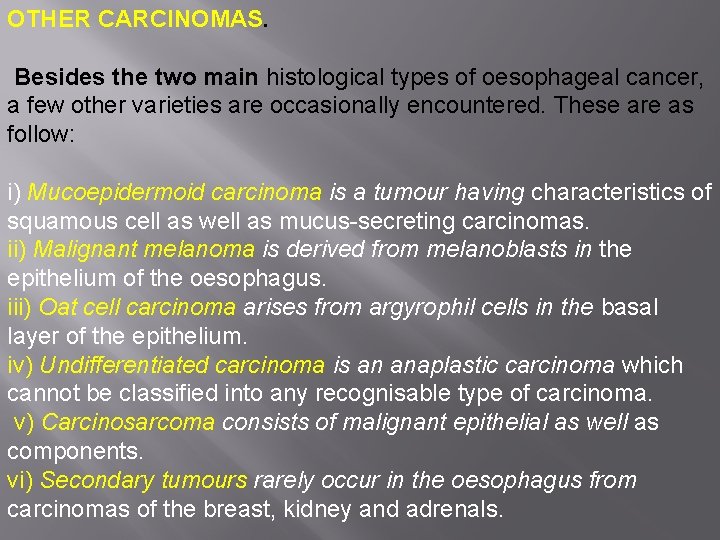
OTHER CARCINOMAS. Besides the two main histological types of oesophageal cancer, a few other varieties are occasionally encountered. These are as follow: i) Mucoepidermoid carcinoma is a tumour having characteristics of squamous cell as well as mucus-secreting carcinomas. ii) Malignant melanoma is derived from melanoblasts in the epithelium of the oesophagus. iii) Oat cell carcinoma arises from argyrophil cells in the basal layer of the epithelium. iv) Undifferentiated carcinoma is an anaplastic carcinoma which cannot be classified into any recognisable type of carcinoma. v) Carcinosarcoma consists of malignant epithelial as well as components. vi) Secondary tumours rarely occur in the oesophagus from carcinomas of the breast, kidney and adrenals.
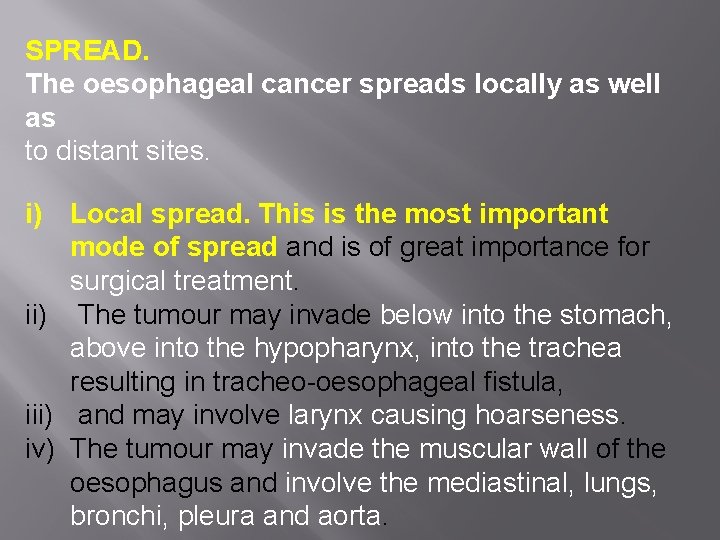
SPREAD. The oesophageal cancer spreads locally as well as to distant sites. i) Local spread. This is the most important mode of spread and is of great importance for surgical treatment. ii) The tumour may invade below into the stomach, above into the hypopharynx, into the trachea resulting in tracheo-oesophageal fistula, iii) and may involve larynx causing hoarseness. iv) The tumour may invade the muscular wall of the oesophagus and involve the mediastinal, lungs, bronchi, pleura and aorta.
ii) Lymphatic spread- may lead to multiple satellite nodules away from the main tumour. Besides, the lymphatic spread may result in metastases to the cervical, para-oesophageal, tracheobronchial and subdiaphragmatic lymph nodes. iii) Haematogenous spread. Blood-borne metastases from the oesophageal cancer are rare, probably because the death occurs early due to invasion of important structures by other modes of spread Metastatic deposits by haematogenous route can occur in the lungs, liver and Adrenal
THE END
 Thoracic membranes and cavities
Thoracic membranes and cavities Epidermoid carcinoma
Epidermoid carcinoma Syphilitic glossitis premalignant
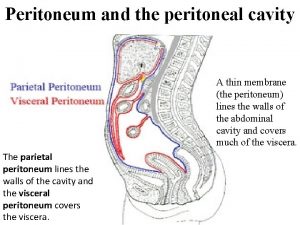
Syphilitic glossitis premalignant Ventral body cavity
Ventral body cavity The abdominal cavity is to the thoracic cavity
The abdominal cavity is to the thoracic cavity Parietal peritoneum
Parietal peritoneum Lesser sac boundaries
Lesser sac boundaries Pyloric orifice function
Pyloric orifice function Landmarks of the face and oral cavity
Landmarks of the face and oral cavity Palatine aponeurosis
Palatine aponeurosis Classification of white lesions of oral cavity
Classification of white lesions of oral cavity Larynx function in digestive system
Larynx function in digestive system Incisive papilla
Incisive papilla Throat paints are liquid preparation
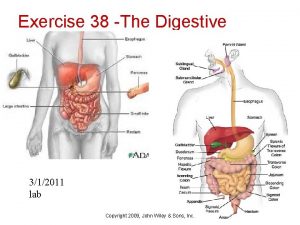
Throat paints are liquid preparation Exercise 38 review sheet art-labeling activity 1 (1 of 2)
Exercise 38 review sheet art-labeling activity 1 (1 of 2) Normal flora of oral cavity
Normal flora of oral cavity Sialedinitis
Sialedinitis Gastroesophageal junction histology
Gastroesophageal junction histology Cural
Cural Esophagus function
Esophagus function Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Mouth esophagus stomach intestines
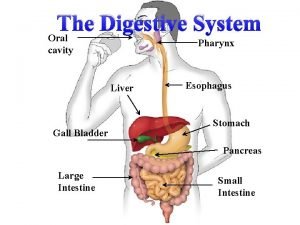
Mouth esophagus stomach intestines Tubular part of stomach
Tubular part of stomach Squid genus
Squid genus Dr haris manzoor qadri
Dr haris manzoor qadri Enterochromaffin like cells
Enterochromaffin like cells Upper third esophagus
Upper third esophagus Esophageal constrictions level
Esophageal constrictions level Peristaltic contraction
Peristaltic contraction Prograde dilatation with bougies
Prograde dilatation with bougies Nutcracker esophagus
Nutcracker esophagus Rugae in stomach
Rugae in stomach Parts of stomach
Parts of stomach Pharyngeal opening of auditory tube
Pharyngeal opening of auditory tube Chronic laryngitis classification
Chronic laryngitis classification Esophagus
Esophagus Layers of the pharynx
Layers of the pharynx Arthrlgia
Arthrlgia Figure 24-12 the stomach
Figure 24-12 the stomach Barrett's esophagus
Barrett's esophagus Pvt tim hall
Pvt tim hall Cardiac orifice
Cardiac orifice Esophagus cadaver
Esophagus cadaver Histological structure of oesophagus
Histological structure of oesophagus Vitelline duct
Vitelline duct Esophagus
Esophagus Esophagus frog function
Esophagus frog function Esophagus stomach small intestine large intestine
Esophagus stomach small intestine large intestine Heterogeneous hypoechoic lesion in liver
Heterogeneous hypoechoic lesion in liver Spinothalamic pathway
Spinothalamic pathway Ascending tracts
Ascending tracts Internal capsule homunculus
Internal capsule homunculus Pprf mlf pathway
Pprf mlf pathway Fractura monteggia y galeazzi
Fractura monteggia y galeazzi Paraplrgia
Paraplrgia Lateral geniculate nucleus lesion
Lateral geniculate nucleus lesion Lesions of vagus nerve
Lesions of vagus nerve Hyperechoic lesion in liver
Hyperechoic lesion in liver Pie on the floor visual field defect
Pie on the floor visual field defect Prostatakreft symptomer
Prostatakreft symptomer Signos duros y blandos de lesion vascular
Signos duros y blandos de lesion vascular Signos duros y blandos de lesion vascular
Signos duros y blandos de lesion vascular Citolítico
Citolítico Archicerebellum
Archicerebellum Lesion subepicardica
Lesion subepicardica Ejemplos hiperplasia
Ejemplos hiperplasia Molusco contagioso lesion elemental
Molusco contagioso lesion elemental Nerve supply of face
Nerve supply of face Vcolesterol
Vcolesterol Infarto subendocardico
Infarto subendocardico Shahab vahdat
Shahab vahdat Endo perio lesion
Endo perio lesion Territoires ecg
Territoires ecg Dont touch lesions
Dont touch lesions N
N Felipe morera oftalmologo
Felipe morera oftalmologo Febs letters
Febs letters Objetivo de diptongos y hiatos
Objetivo de diptongos y hiatos Diagrama de wallace
Diagrama de wallace Menisco
Menisco Radiopaco y radiolucido
Radiopaco y radiolucido Nurografia
Nurografia Oftalmlogo
Oftalmlogo Lésion en verre dépoli
Lésion en verre dépoli