Imaging of Pancreatic Cystic Lesions Dr Zaghouani H








- Slides: 30
Imaging of Pancreatic Cystic Lesions Dr Zaghouani. H, Pr Kraiem Ch Service d’imagerie Farhat Hached 5 th ARC of PAARS& 6 th annuel Meeting of PAIRS 25 -28 April Hammamet

INTRODUCTION • Incidence of pancreatic cystic lesions ranges from 1% to 25% in various studies; incidence in asymptomatic general populations is about 2. 6%. • Wide spectrum of lesions including, non neoplastic, benign, borderline, and malignant pathologies. • Radiologists play an important role in detection, characterization, and follow-up of cystic lesions of the pancreas.
Clinical Presentation • A large number of pancreatic cysts are incidentally detected during imaging work-up for an unrelated medical problem.
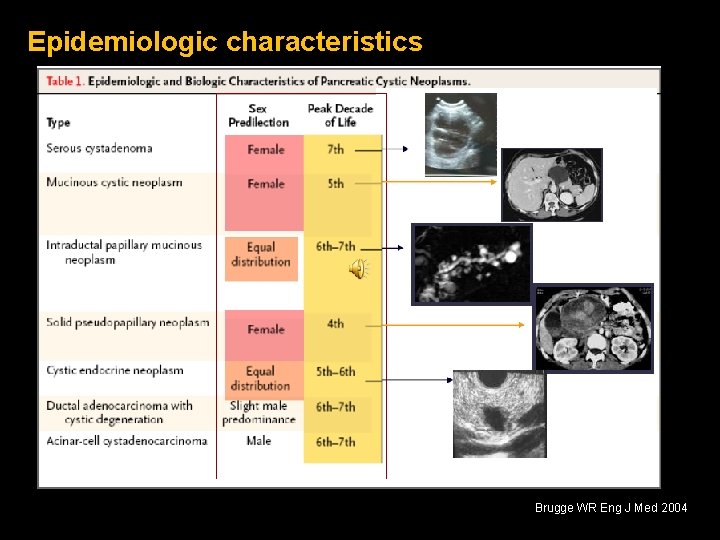
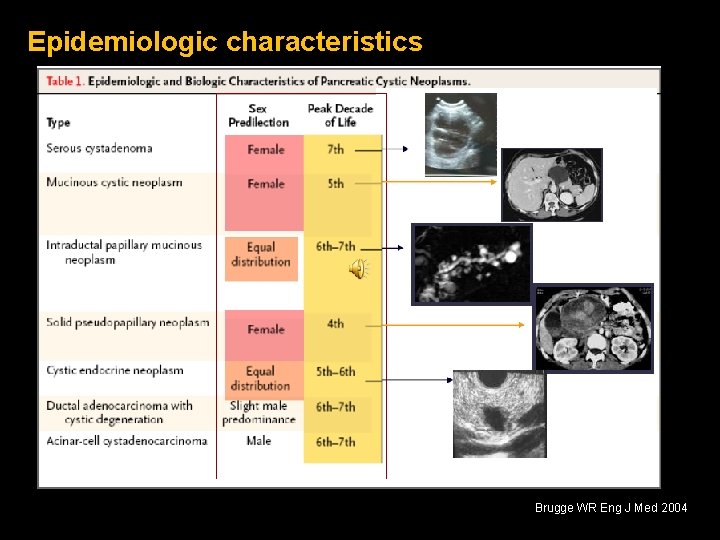
Epidemiologic characteristics Brugge WR Eng J Med 2004
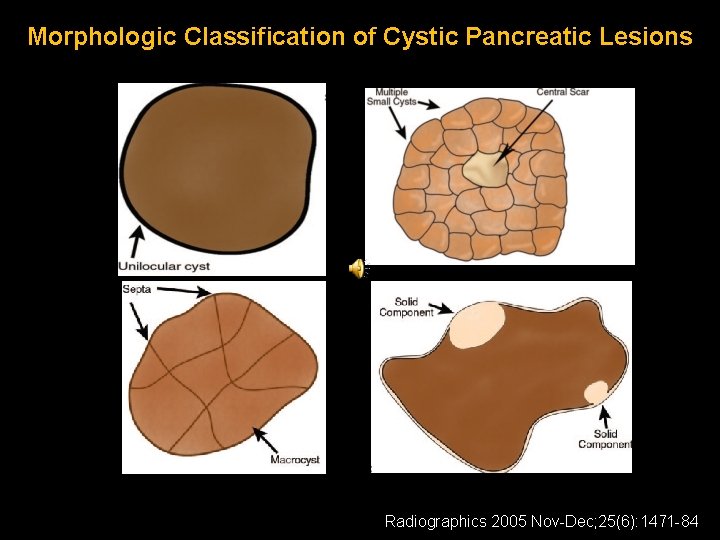
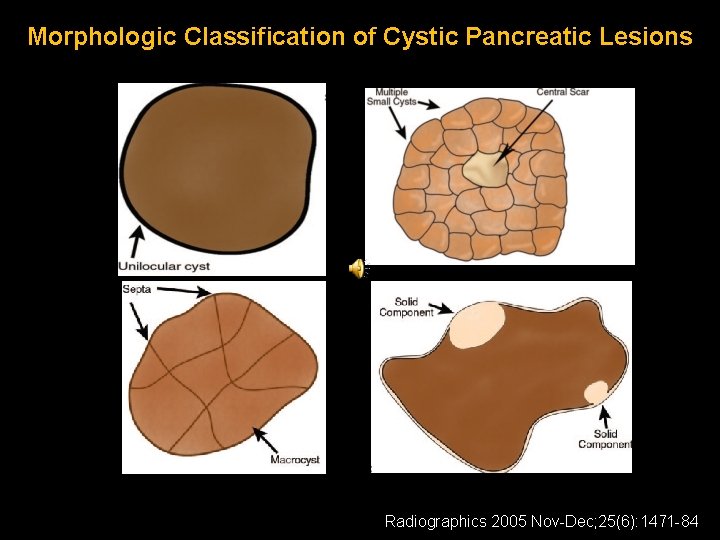
Morphologic Classification of Cystic Pancreatic Lesions Radiographics 2005 Nov-Dec; 25(6): 1471 -84
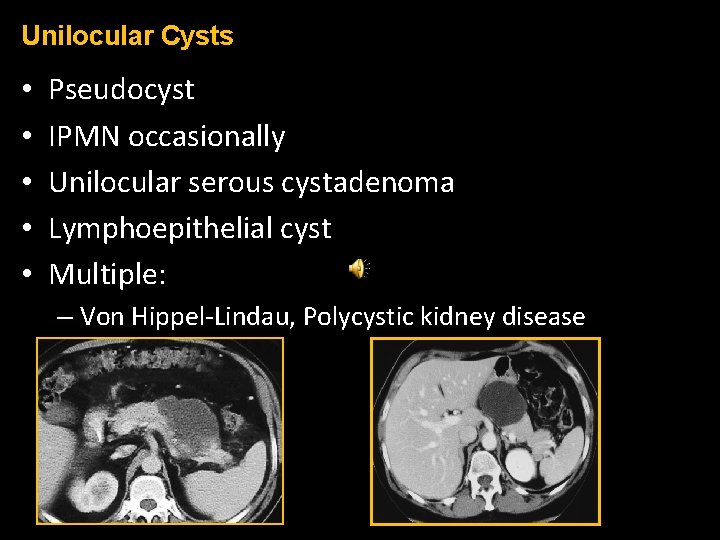
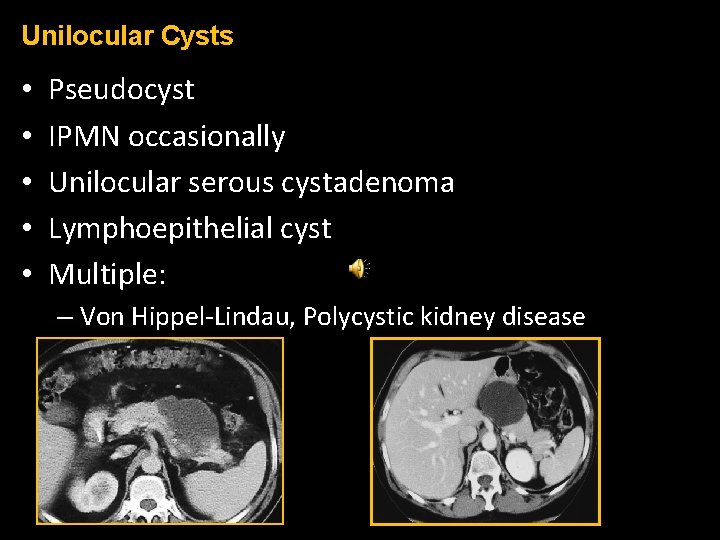
Unilocular Cysts • • • Pseudocyst IPMN occasionally Unilocular serous cystadenoma Lymphoepithelial cyst Multiple: – Von Hippel-Lindau, Polycystic kidney disease
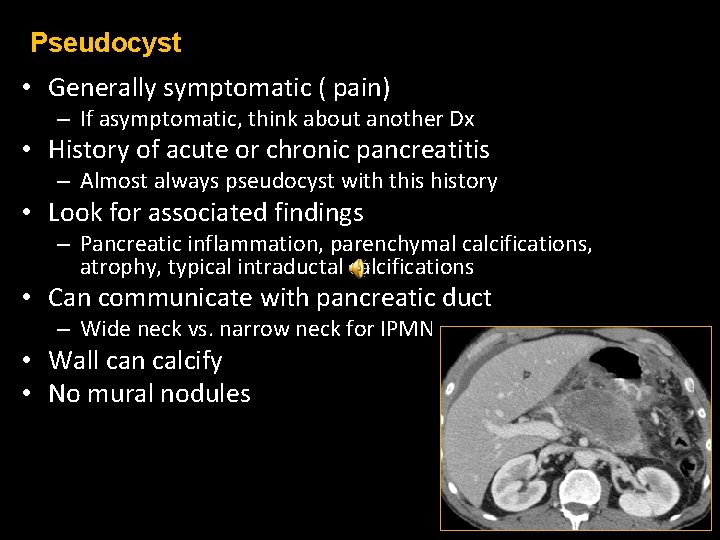
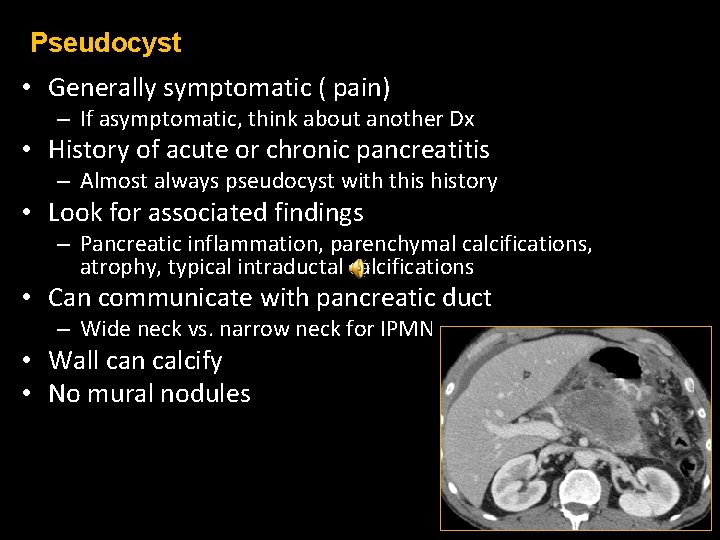
Pseudocyst • Generally symptomatic ( pain) – If asymptomatic, think about another Dx • History of acute or chronic pancreatitis – Almost always pseudocyst with this history • Look for associated findings – Pancreatic inflammation, parenchymal calcifications, atrophy, typical intraductal calcifications • Can communicate with pancreatic duct – Wide neck vs. narrow neck for IPMN • Wall can calcify • No mural nodules
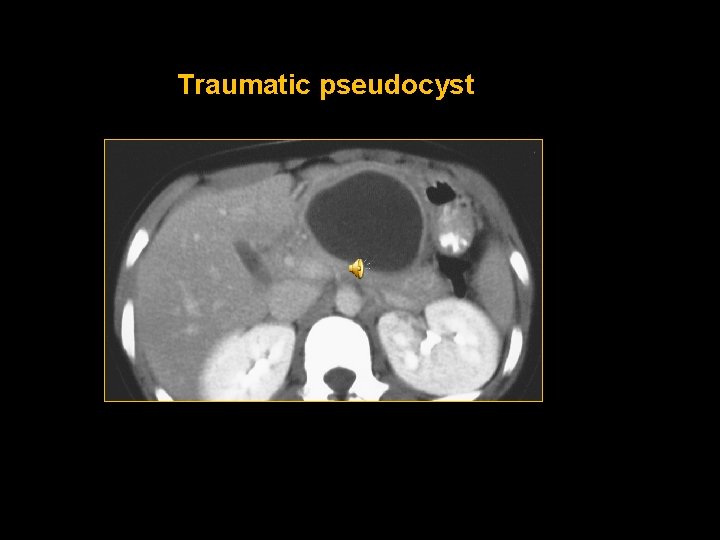
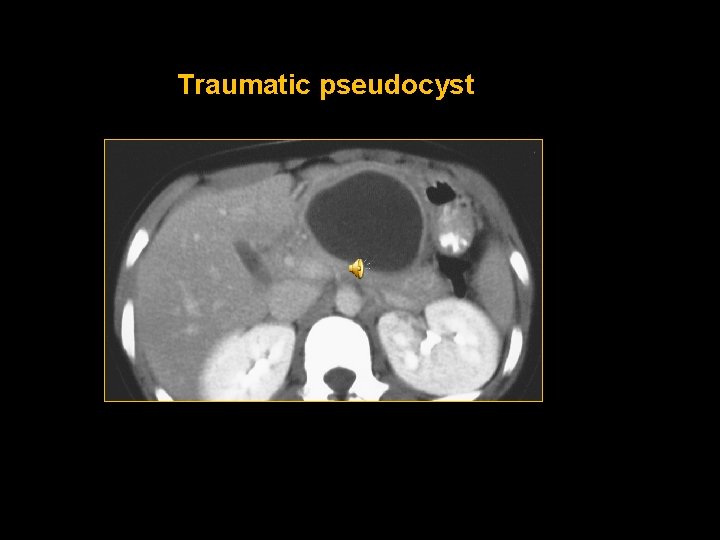
Traumatic pseudocyst
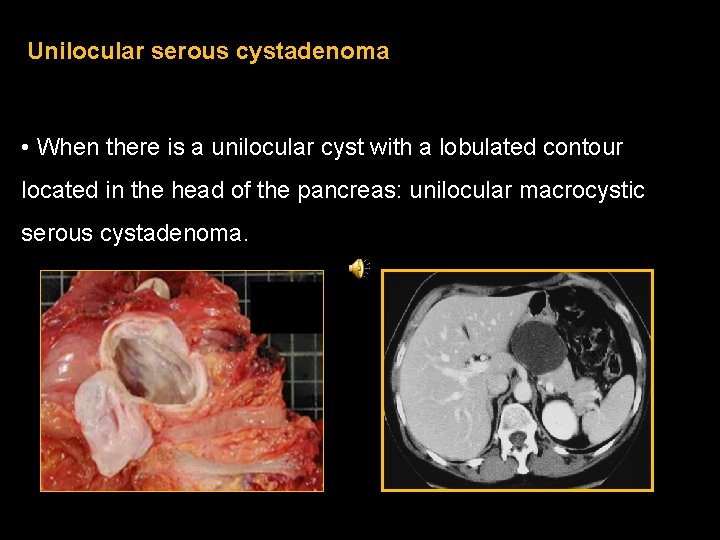
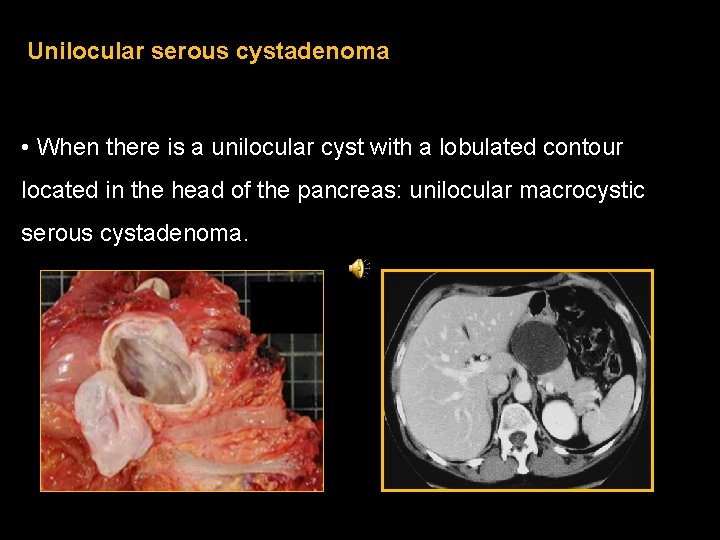
Unilocular serous cystadenoma • When there is a unilocular cyst with a lobulated contour located in the head of the pancreas: unilocular macrocystic serous cystadenoma.
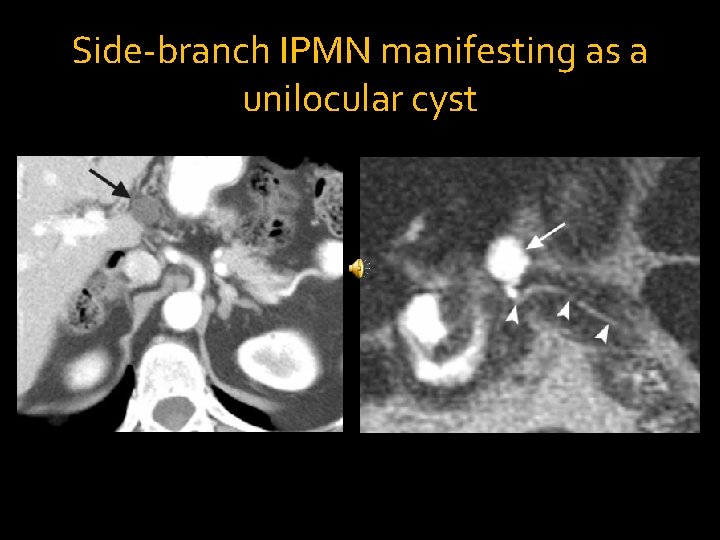
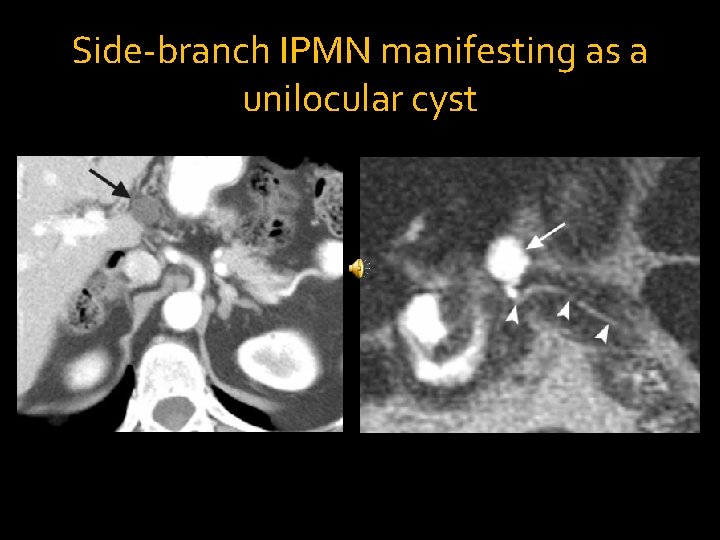
Side-branch IPMN manifesting as a unilocular cyst
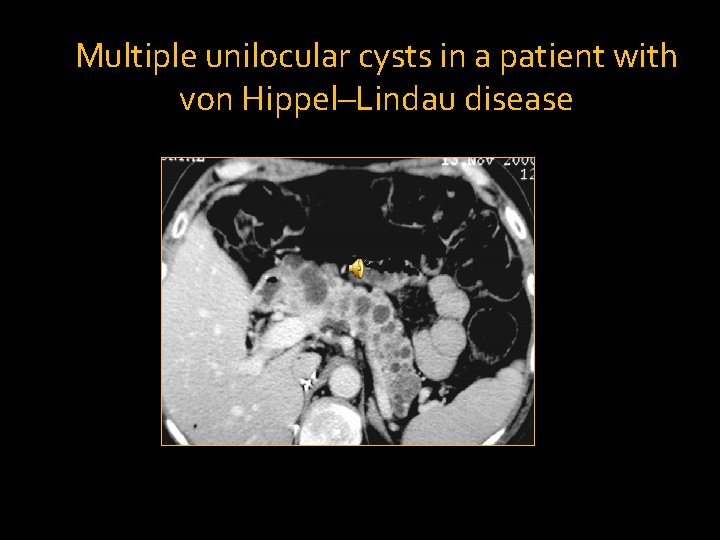
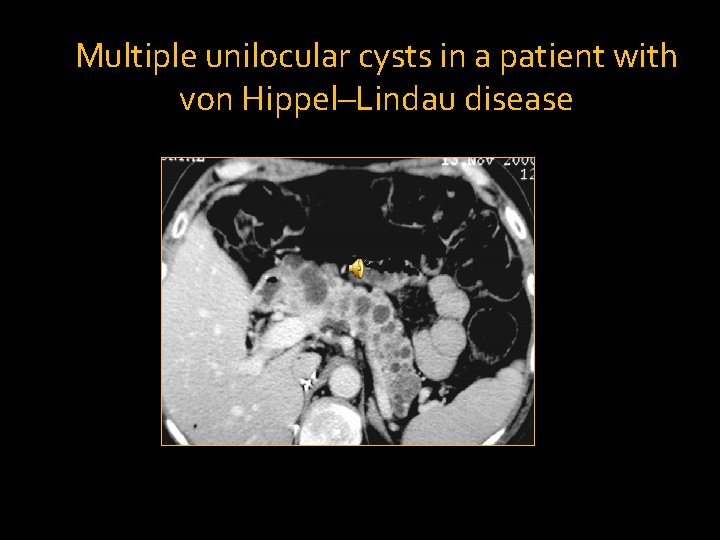
Multiple unilocular cysts in a patient with von Hippel–Lindau disease
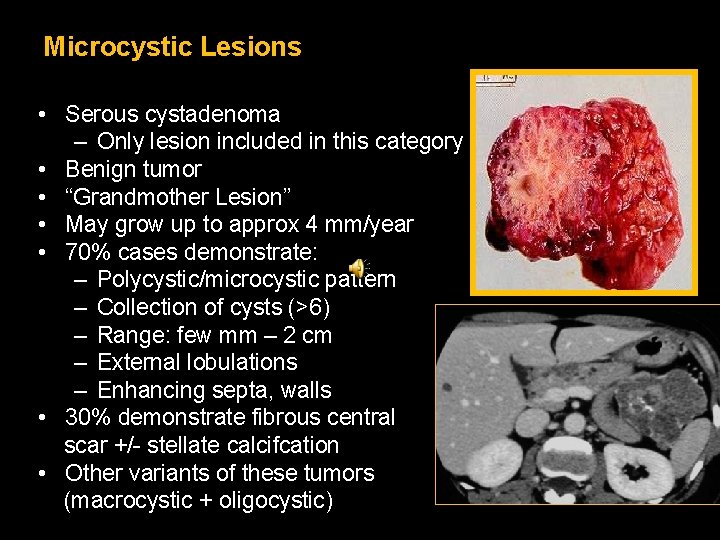
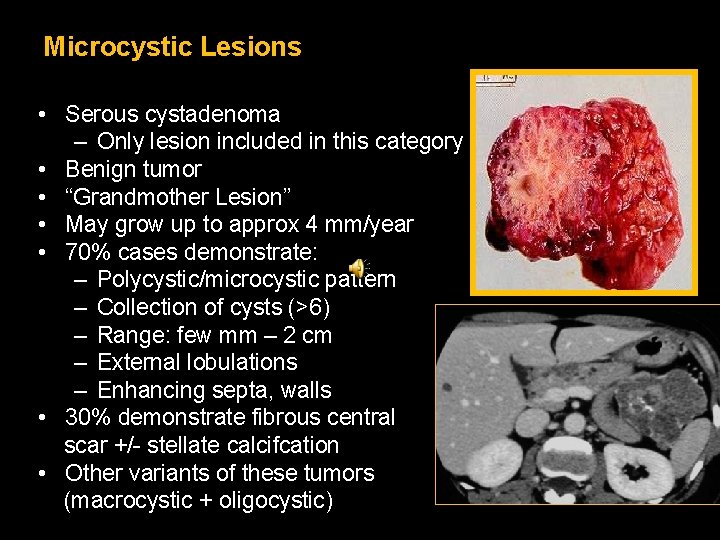
Microcystic Lesions • Serous cystadenoma – Only lesion included in this category • Benign tumor • “Grandmother Lesion” • May grow up to approx 4 mm/year • 70% cases demonstrate: – Polycystic/microcystic pattern – Collection of cysts (>6) – Range: few mm – 2 cm – External lobulations – Enhancing septa, walls • 30% demonstrate fibrous central scar +/- stellate calcifcation • Other variants of these tumors (macrocystic + oligocystic)

Serous cystadenoma: MRI
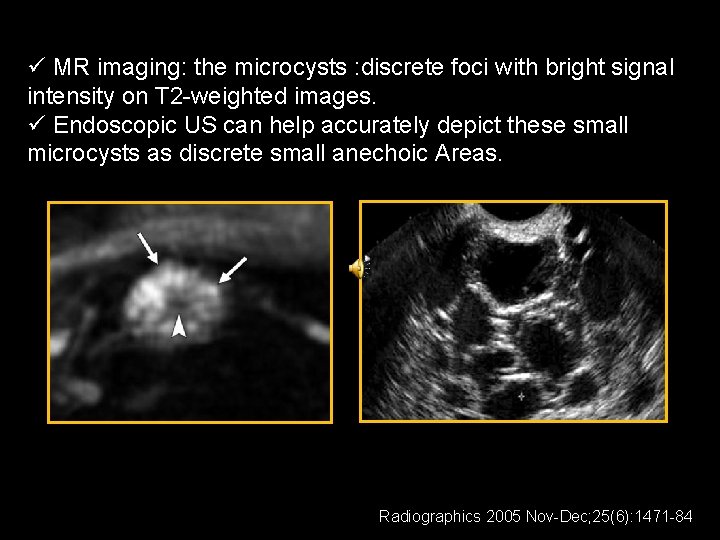
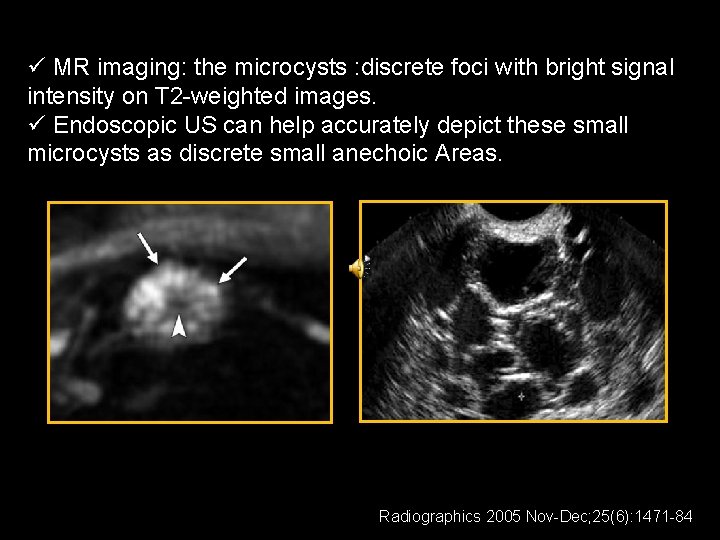
ü MR imaging: the microcysts : discrete foci with bright signal intensity on T 2 -weighted images. ü Endoscopic US can help accurately depict these small microcysts as discrete small anechoic Areas. Radiographics 2005 Nov-Dec; 25(6): 1471 -84

Macrocystic Lesions • Mucinous cystic neoplasms • Intraductal Papillary Mucinous Neoplasm (IPMN)
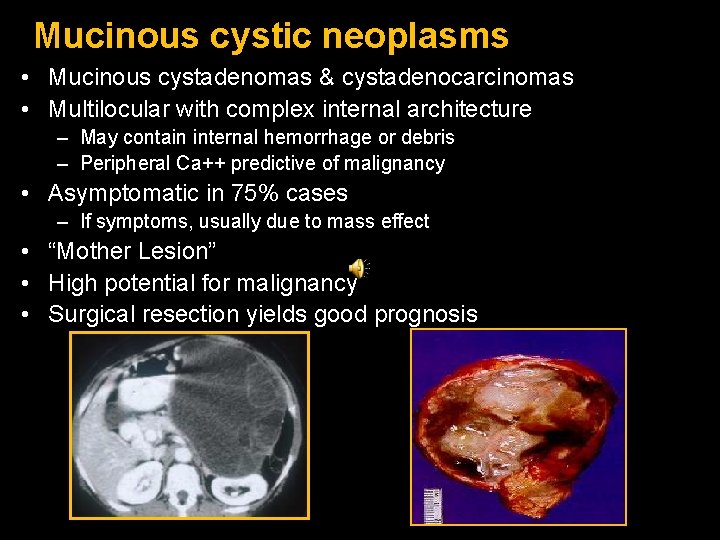
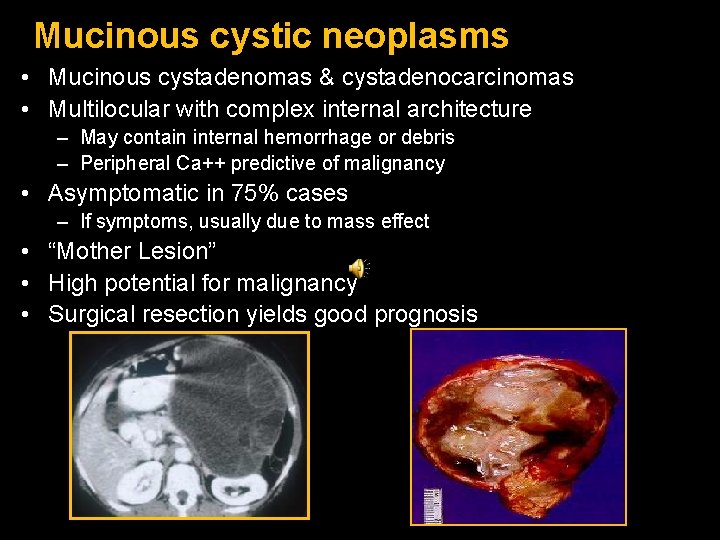
Mucinous cystic neoplasms • Mucinous cystadenomas & cystadenocarcinomas • Multilocular with complex internal architecture – May contain internal hemorrhage or debris – Peripheral Ca++ predictive of malignancy • Asymptomatic in 75% cases – If symptoms, usually due to mass effect • “Mother Lesion” • High potential for malignancy • Surgical resection yields good prognosis
• Mucinous cystic neoplasms (mucinous cystadenomas) predominantly: - involve the body and tail of the pancreas - they do not communicate with the pancreatic duct, they can cause partial pancreatic ductal obstruction.

Intraductal Papillary Mucinous Neoplasm (IPMN) • IPMNs classified : main duct, branch duct (side-branch), or mixed IPMNs, • Main duct IPMN is a morphologically distinct entity and cannot be included in the discussion of pancreatic cysts.
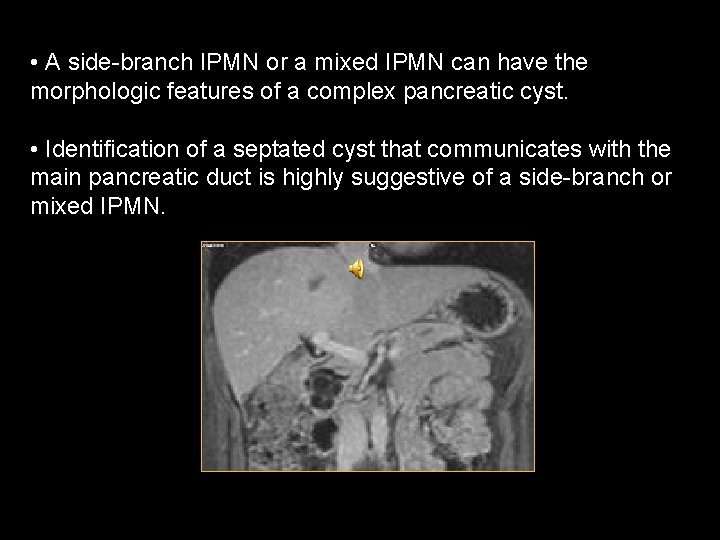
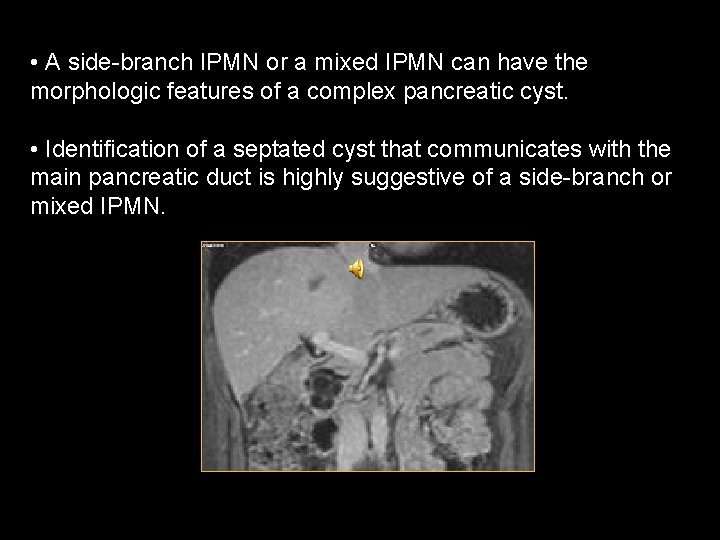
• A side-branch IPMN or a mixed IPMN can have the morphologic features of a complex pancreatic cyst. • Identification of a septated cyst that communicates with the main pancreatic duct is highly suggestive of a side-branch or mixed IPMN.
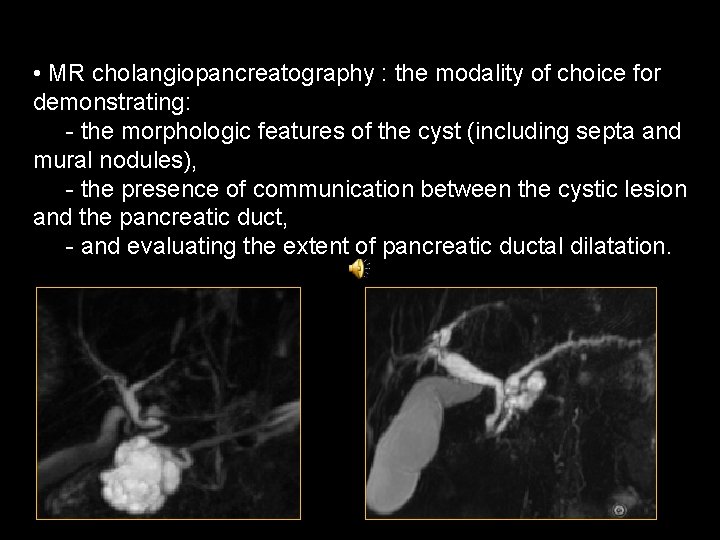
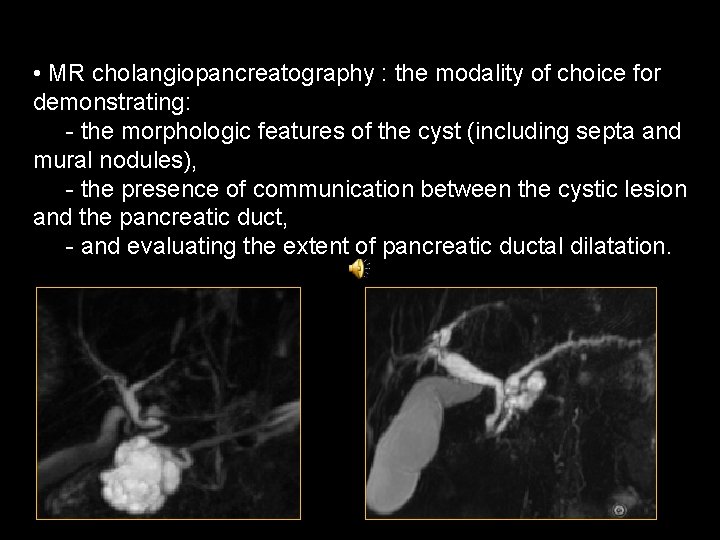
• MR cholangiopancreatography : the modality of choice for demonstrating: - the morphologic features of the cyst (including septa and mural nodules), - the presence of communication between the cystic lesion and the pancreatic duct, - and evaluating the extent of pancreatic ductal dilatation.

• The occurrence of malignancy is significantly higher in main duct and mixed IPMNs than in side-branch IPMNs. • In cases of side-branch IPMN with; - septated pancreatic cysts more than 3 cm in diameter - MDP> 7 mm - mural nodules have a high malignant potential
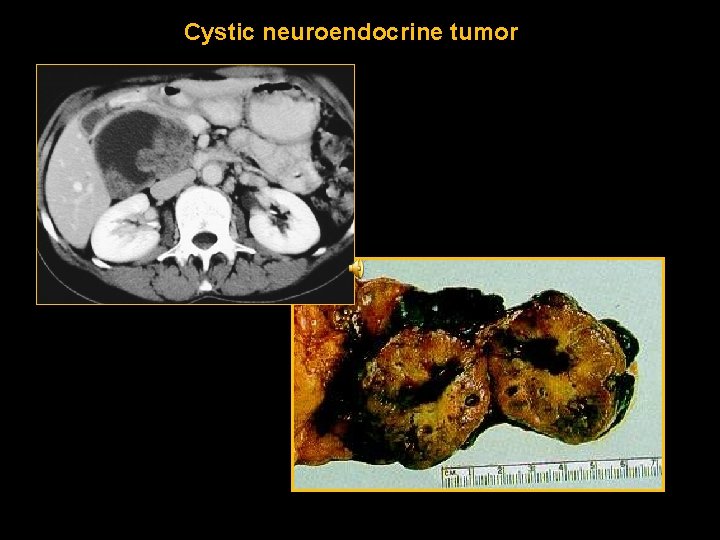
Other uncommon tumors (macrocystic lesions) include non functioning neuroendocrine tumors and rare congenital malformations such as lymphangiomas.

Cysts with a Solid Component • Unilocular or multilocular • True cystic tumors or solid pancreatic neoplasms with cystic component/degeneration • Wide DDx – Mucinous cystic neoplasms – IPMNs – Islet cell tumor – Solid pseudopapillary tumor (SPEN) – Adenocarcinoma – Metastasis • All malignant or have a high malignant potential • Surgical management
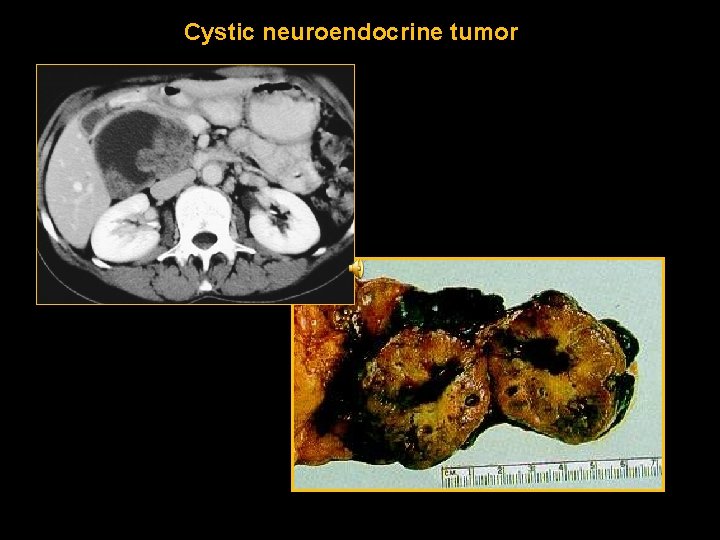
Cystic neuroendocrine tumor

Management Pancreatic cystic lesions: Classification Kloppel et al. WHO Classification. 2000

Management Pancreatic cystic lesions: Predictors of Malignancy Verbesy et al. Sur Clin N Am. 2010.
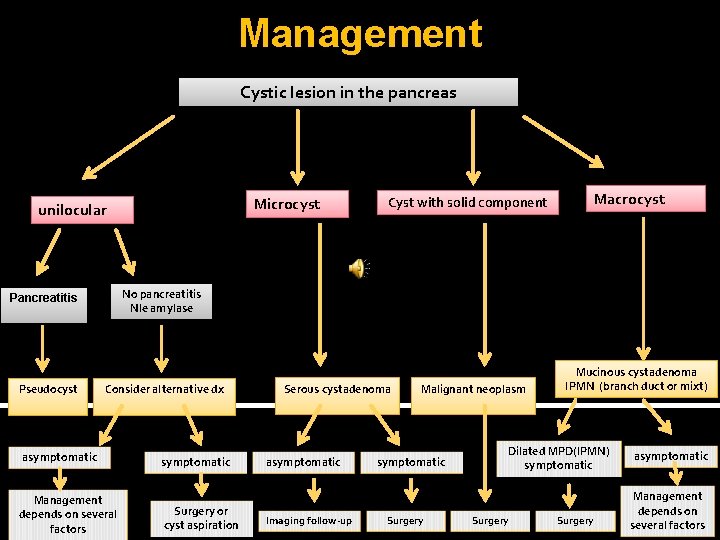
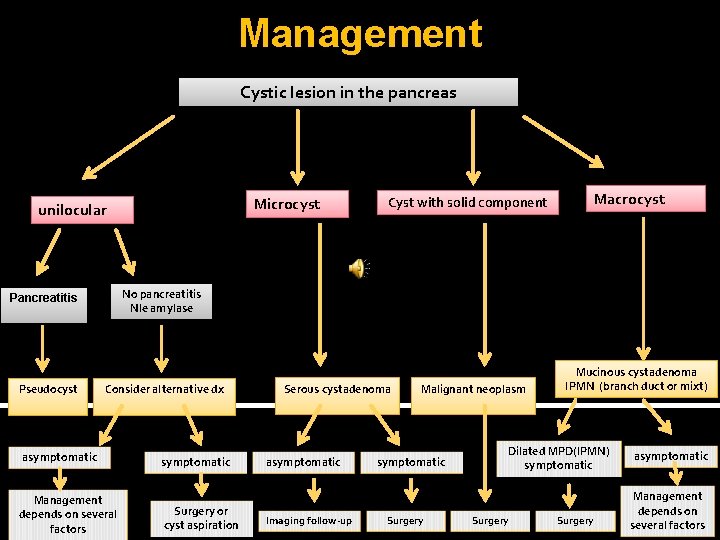
Management Cystic lesion in the pancreas Microcyst unilocular Macrocyst No pancreatitis Nle amylase Pancreatitis Pseudocyst Cyst with solid component Consider alternative dx asymptomatic Management depends on several factors symptomatic Surgery or cyst aspiration Serous cystadenoma asymptomatic Imaging follow-up Malignant neoplasm symptomatic Surgery Mucinous cystadenoma IPMN (branch duct or mixt) Dilated MPD(IPMN) symptomatic Surgery asymptomatic Management depends on several factors
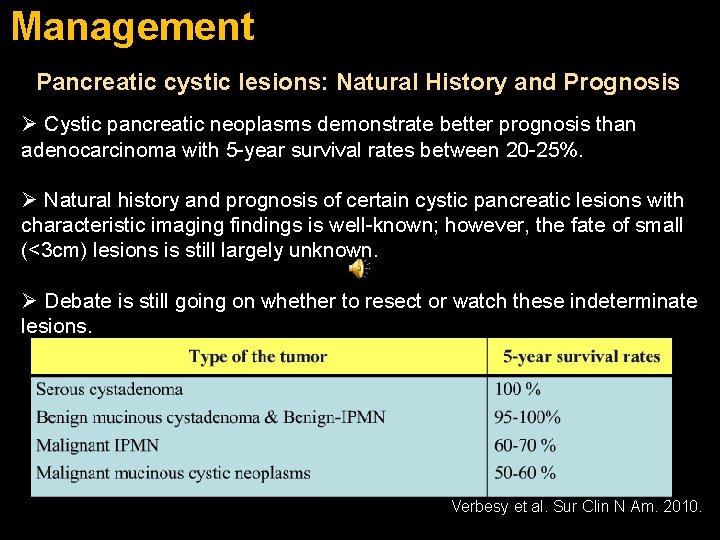
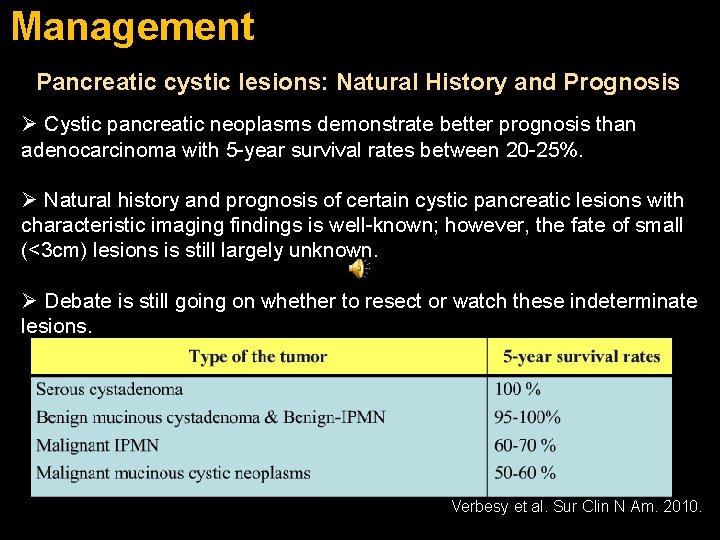
Management Pancreatic cystic lesions: Natural History and Prognosis Ø Cystic pancreatic neoplasms demonstrate better prognosis than adenocarcinoma with 5 -year survival rates between 20 -25%. Ø Natural history and prognosis of certain cystic pancreatic lesions with characteristic imaging findings is well-known; however, the fate of small (<3 cm) lesions is still largely unknown. Ø Debate is still going on whether to resect or watch these indeterminate lesions. Verbesy et al. Sur Clin N Am. 2010.
Follow-up • No consensus • 6 month intervals for 1 st year • Annual imaging for 3 years
TAKE HOME MESSAGES • Age & Gender – “Daughter Lesion”: SPEN – “Mother Lesion”: Mucinous cystic – “Grandmother Lesion”: Serous cystadenoma • Location – Head/neck for serous & side branch IMPN – Body/tail for mucinous cystic neoplasm • Calcification – Peripheral in mucinous cystic – Central in serous cystadenoma • Mural Nodularity (enhancement = neoplasm) • Duct communication (narrow neck) favors IPMN
 Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Frc control system
Frc control system Prognosis of cystic fibrosis
Prognosis of cystic fibrosis Cystic fibrosis irt
Cystic fibrosis irt Mechanisms of evolution
Mechanisms of evolution Pancreas anatomy cadaver
Pancreas anatomy cadaver Charcot triangle
Charcot triangle Organic acidemia
Organic acidemia How to show fraternal twins on a pedigree
How to show fraternal twins on a pedigree Cystic fibrosis mendelian inheritance
Cystic fibrosis mendelian inheritance Cystic fibrosis male infertility
Cystic fibrosis male infertility Cystic fibrosis transmembrane conductance regulator
Cystic fibrosis transmembrane conductance regulator Subcostal retractions
Subcostal retractions Cftr
Cftr Cystic fibrosis pedigree chart
Cystic fibrosis pedigree chart Autosomal recessive cystic fibrosis
Autosomal recessive cystic fibrosis Bdhhg
Bdhhg Cystic fibrosis life expectancy
Cystic fibrosis life expectancy Horseshoe tear
Horseshoe tear Oral cholecystogram
Oral cholecystogram Cystic fibrosis transmembrane conductance regulator
Cystic fibrosis transmembrane conductance regulator Crms cf
Crms cf Sexlinked traits examples
Sexlinked traits examples Adam nash (savior sibling)
Adam nash (savior sibling) Periradicular tissues
Periradicular tissues Olneys lesions
Olneys lesions Nature lésions
Nature lésions Lésions
Lésions Chapter 17 oral pathology short answer questions
Chapter 17 oral pathology short answer questions Describing skin lesions
Describing skin lesions Med
Med