MY RETINAL DETACHMENT NOW I SEE NOW I














- Slides: 56
MY RETINAL DETACHMENT: NOW I SEE, NOW I DON’T William D. Townsend, OD, FAAO Advanced Eye Care, Canyon, TX Adjunct Professor, UHCO
To Dwight and Lil Linton

21 April 2008: Canyon, Texas During clinic, I initially note a few small floaters that I had never noticed before No flashes of light No vision changes I mentioned this to my extern, Juan Menjivar, who wants to dilate me and examine my peripheral retinas I decline; it was a busy week Ø My mother was in the hospital- almost died Ø We had a bank stockholders meeting Ø I had to get ready to speak in Canada Ø I knew there wasn’t a problem: I am bullet proof
Frederickton, New Brunswick 26 April 2008 Life is Great! I am speaking to the New Brunswick Association of Optometrists Lectures are going great The audience is very interactive It is a perfect spring day in a beautiful, historic Canadian city I get to hang out with my friend, Dr. Diana Shechtman who is speaking on retina Things could not be better!
26 April 2008 I start off the day in the gym with a 7 am workout Next, I work on today’s lecture to finalize the content and add new information As I work, I notice a small dark spot in my OD lower temporal field What the heck, I plunge on
Thirty Five Years Earlier…. Hit in the right eye with a tennis ball Within a year, I noted my vision in that eye was not as quite as bright Over the years, the trend continued Why? A progressive traumatic NS cataract 10 May 2007, successful cataract surgery with implantation of Alcon Toric IOL Ø BVA without correction = 20/15
Back to New Brunswick I tell Diana about my “spot” and express concern; she calls me a hypochondriac 1: 00 pm- I start my lecture, “Pain Management” As I speak, I note that the grey spot is rapidly expanding upward reducing my field in the inferior field. I run into things as I deliver the lecture
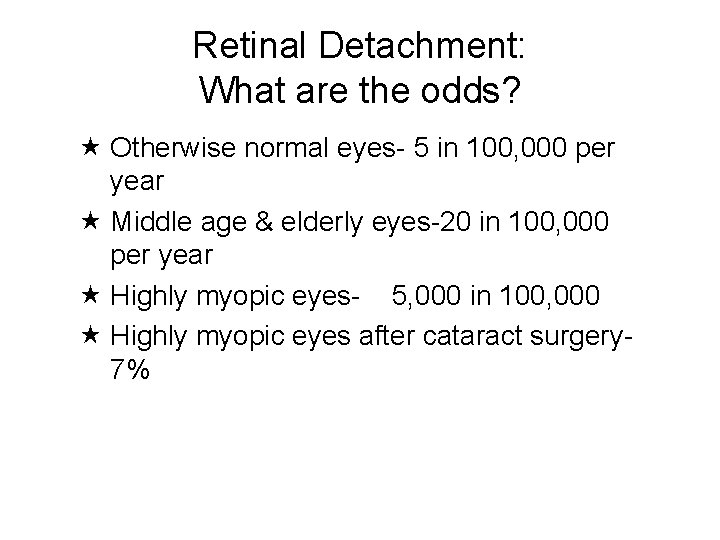
Retinal Detachment: What are the odds? Otherwise normal eyes- 5 in 100, 000 per year Middle age & elderly eyes-20 in 100, 000 per year Highly myopic eyes- 5, 000 in 100, 000 Highly myopic eyes after cataract surgery 7%
Why do we need to understand the vitreous - retina relationship ? The majority of retinal detachments are rhegmatogenous (tear-induced). Virtually all retinal tears are caused by interaction between vitreous and retina. Anatomical variations in the vitreous-retinal relationship often lead to retinal tears
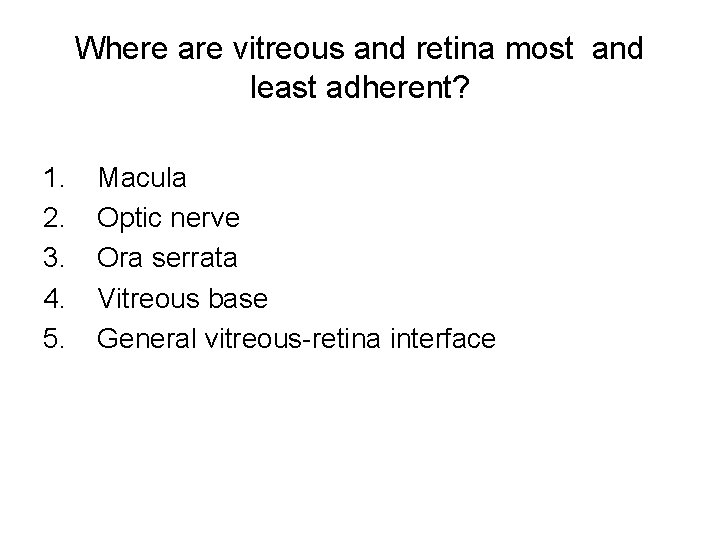
Where are vitreous and retina most and least adherent? 1. 2. 3. 4. 5. Macula Optic nerve Ora serrata Vitreous base General vitreous-retina interface
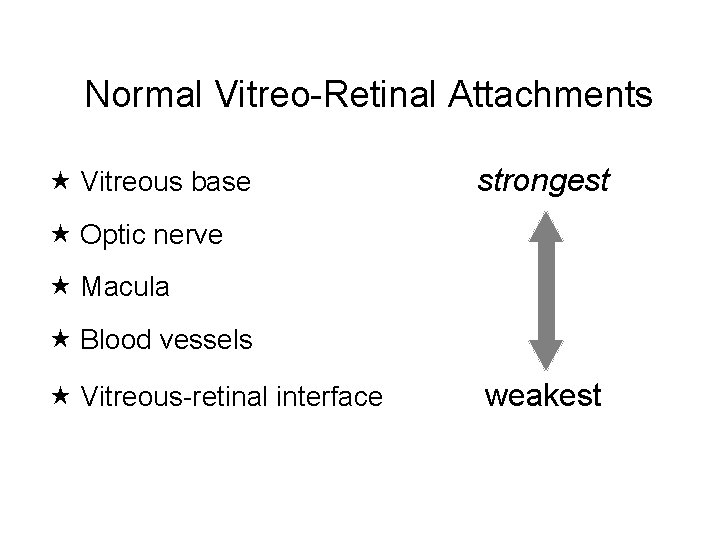
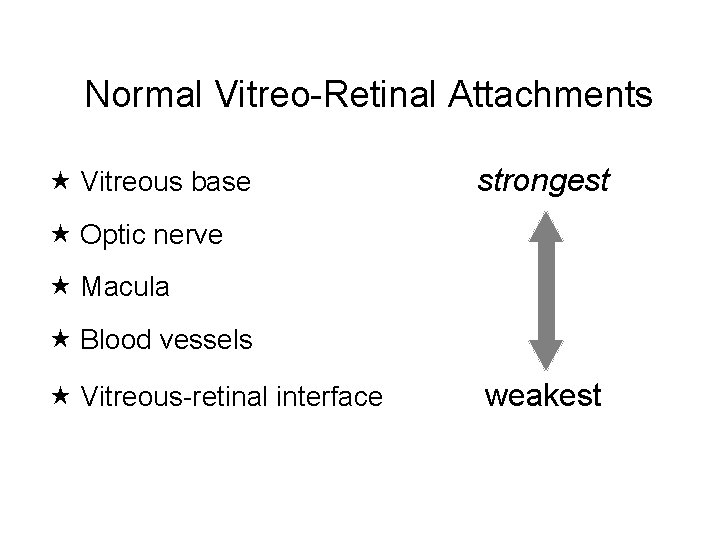
Normal Vitreo-Retinal Attachments Vitreous base strongest Optic nerve Macula Blood vessels Vitreous-retinal interface weakest
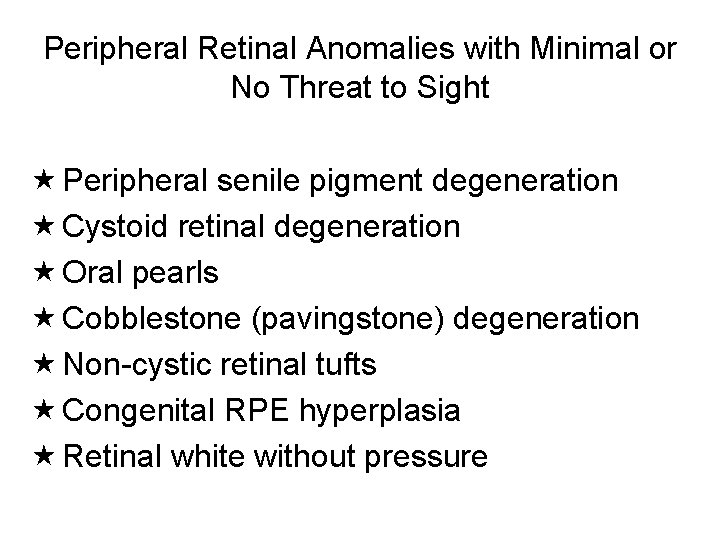
Peripheral Retinal Anomalies with Minimal or No Threat to Sight Peripheral senile pigment degeneration Cystoid retinal degeneration Oral pearls Cobblestone (pavingstone) degeneration Non-cystic retinal tufts Congenital RPE hyperplasia Retinal white without pressure
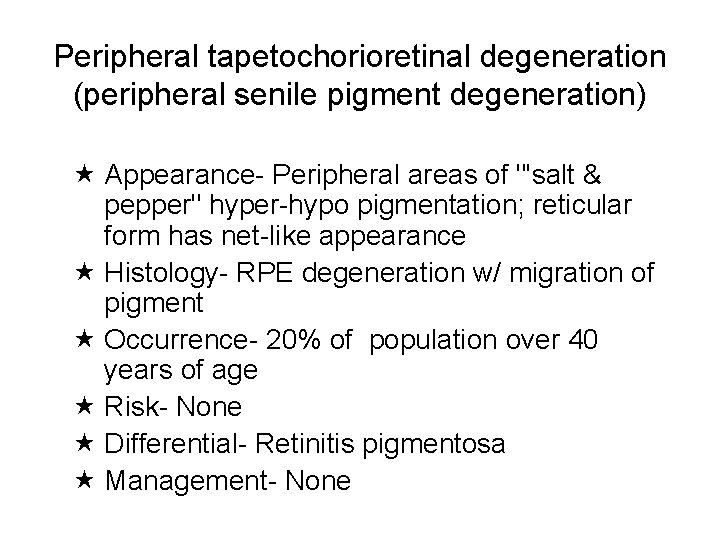
Peripheral tapetochorioretinal degeneration (peripheral senile pigment degeneration) Appearance- Peripheral areas of "'salt & pepper" hyper-hypo pigmentation; reticular form has net-like appearance Histology- RPE degeneration w/ migration of pigment Occurrence- 20% of population over 40 years of age Risk- None Differential- Retinitis pigmentosa Management- None
Peripheral Chorioretinal Atrophy (Pavingstone Degeneration) Occurrence- 27% of adult autopsy eyes, bilateral 38% of cases, increases w/ age, inferior location most common, high myopes Risk- In retinal detachment, retina may tear at border of lesion Differential- Chorioretinal scars Mgt- None

Retinal Tufts: General Information Degenerated glial tissue Vitreous traction invariably present Risk for tear depends on ØLocation ØSize ØDegree of traction present Cystic: occur posterior to vitreous base Non-cystic: occur within vitreous base
Non-cystic Retinal Tufts Appearance- small, thin projections of tissue that appear as grey-white dots close to ora Histology- composed of altered retinal tissue, degenerated glial tissue; base diameter usually less than. 1 mm Occurrence- 72% of adults and bilateral in 50% of cases; vast majority are intrabasal Risk- low to none - small size and intrabasal location Differential- none Management- none; rarely, small benign holes are noted at their base
Retinal Pigment Epithelium Hypertrophy Appearance- flat, round pigmented lesions, usually black or dark grey, distinct borders Size- varies from small to several disc diameters. May have a surrounding area of decreased pigmentation (halo). Histology- congenital hypertrophy of RPE; cells have larger than normal melanin granules; . Occurrence- unknown; unilateral in 85% of cases Risk- none Differential- nevus, melanoma Management- rule out traction as in cystic tufts, otherwise none

Retinal Pigment Epithelium Hyperplasia Appearance- flat, round pigmented lesions, usually black or dark grey, distinct borders Size- varies from small to several disc diameters. Histology- acquired (hyperplasia) increased number of RPE cells Ø May occur at site of vitreoretinal traction Unknown- unilateral in 85% of cases Risk- none Differential- nevus, melanoma, assess for vitreoretinal traction
Peripheral Retinal Anomalies with Moderate Threat to Sight Enclosed ora bays Meridional folds Cystic retinal tufts Zonular traction tufts Acquired peripheral retinoschisis ØTypical ØReticular Atrophic retinal holes Operculated retinal breaks Lattice retinal degeneration
Cystic Retinal Tufts Appearance- grey nodules of varying size, usually extrabasal Histology- degenerated, proliferated cystic tissue with some degree of vitreous traction 0. 1 to 1 mm diam. Occurrence- 6% of patients Risk- varies depending on source Ø Byer: 10% of all retinal detachment caused by CRT Ø Foos: CRT cause 82% of opercula, 97% of tears Management: scleral indentation, patient education, yearly DFE Ø Do not underestimate the potential damage!
Operculated Retinal Holes Appearance- Usually round, occasionally elongated red areas in peripheral retina, ØOften w/ cuff of subretinal fluid and subclinical detachment (30%) ØOpercula are almost universally seen in adjacent vitreous ØPigment surround common Histology- Full thickness break in retina. Caused by traction on CRT, or area of abnormal vitreoretinal traction
Operculated Retinal Holes Occurrence- 13. 4% of retinal breaks, increased in frequency w/ age, most common extrabasal; 80% associated w/ PVD. Ø Large operculated breaks associated w/ lattice degeneration & PVD are rare. Ø Reportedly associated w/ WWP & WWOP Risk- Slight, increases w/ size Differential- Atrophic hole, retinal hemorrhage, flap tear Management- If old, asymptomatic, patient education, yearly DFE Ø If fresh, or symptomatic, patient education, 6 week DFE. Ø If subclinical detachment > 2 dd, refer.

Acquired Peripheral Retinoschisis Occurs in two forms, typical and reticular Caused by splitting of sensory retina Found in 4% of general population & 7% of population over 40 years of age Round or ovoid in shape, Always associated w/ cystoid degeneration; advanced stage of same process Bullous lesions more prone to progression or detachment Causes absolute scotoma

Peripheral Retinoschisis Typical Appearance- Round or ovoid shape w/ inner & outer layers separated by fluid. ØDetails of choroidal vasculature are obscured ØWhite dots on inner surface (70%) of lesions. ØInner layer smooth, has white dots on inner surface (70% of lesions) ØOuter layer has moth-eaten, pockmarked appearance. Inner or outer layer holes occasionally seen.
Peripheral Retinoschisis Typical Histology- Splitting of neurosensory retina in region of outer plexiform layer Ø Inner layer is relatively thick & smooth in appearance. Supporting elements or pillars between layers at margins of lesions. Occurrence- found in. 69% of eyes, Ø Bilateral in 33%-64% of cases, most common inferior temporal quadrant (70%-82%), Ø some studies indicate more prevalent in hyperopes. Ø Always associated w/ cystoid degeneration; increases w/ age
Peripheral Retinoschisis Reticular Appearance- Round or ovoid shape w/ inner & outer layers separated by fluid. ØDetails of choroidal vasculature are obscured; inner layer thinner than in typical form. ØWhite dots and an arborizing pattern of white lines in inner layer; outer layer has moth-eaten, pockmarked appearance. ØInner or outer layer hole more common.
Peripheral Retinoschisis Reticular Histology- Splitting of neurosensory retina in region of internal limiting membrane; inner layer is relatively thin & smooth in appearance. Supporting elements or pillars between layers at margins of lesions. Occurrence- 0. 95% of eyes, bilateral in 15. 8% of cases: found in 1. 62% of patients. Ø Most common in inferior temporal quadrant; vast majority of lesions in temporal quadrants. Ø Outer layer holes in 22. 7% of eyes. ; increases w/ age

Peripheral Retinoschisis Reticular Risk Ø More prone to progress past equator than typical form Ø More prone to cause retinal detachment, especially when outer layer holes are present Ø Greatest risk is when outer and inner layer holes co-exist in same lesion

Atrophic Peripheral Retinal Holes Appearance- small (<. 5 dd) round red areas in peripheral retina, often w/ surrounding cuff of fluid and subclinical detachment Histology- full thickness break in retina. Occurrence- 76% of all retinal breaks, occur in 2. 4%of eyes, 4% of cases, 76% found w/in lattice lesions, associated w/ meridional folds, ZTT, CRT; increased in myopes, 80% have associated subclinical detachment

Atrophic Peripheral Retinal Holes Risk- minimal; 7% lead to clinical detachment Differential- tractional tear, retinal hemorrhage; scleral depression Management- document, yearly DFE, refer if clinical detachment > 2 dd noted
Horseshoe or Flap Tears Appearance- red, U-shaped lesion w/ "horse running toward the posterior pole” Ø Cystic retinal tuft may be seen at end of flap; 25% < 1/4 dd in size Histology- full thickness retinal break w/ attached flap of retina having traction from vitreous on apex of the flap Occurrence- 10% of all retinal breaks Ø Frequently symptomatic due to traction. Ø Often found at posterior border of lattice, scars, CRT, enclosed ora bays, chorioretinal scars Ø 81% occur in individuals over 40 years of age 50% in superior nasal quadrant.
Horseshoe or Flap Tears Risk - moderate to high because of the continuing presence of traction. Differential- atrophic hole, operculated tear, hemorrhage Management- Small (< 1/4 dd) and asymptomatic: patient education & 4 week DFE, Larger (> 1/4 dd) or symptomatic, especially if superior, or Hx detachment fellow eye: refer
Lattice Retinal Degeneration Appearance ØVaries widely; usually parallels the ora ØWhite lines- 12%-15% ØAtrophic holes- 18%-43% ØPigment- 83% ØWhite spots- 80% Histology- thinned area of peripheral retina with overlying lacunae of liquified vitreous, vitreous traction on margins, especially posterior

Lattice Retinal Degeneration Occurrence: 8%-11% of individuals ØIncreased in myopic eyes ØMost common @ 12 o’clock & 6 o’clock Risk Ø 0. 5% chance for detachment Ø 30% of all detachments associated with lattice ØGreatest risk is large horseshoe tears
Lattice Retinal Degeneration Differential: pavingstone, retinal dialysis, scleral indentation is essential Management: Ø Observe w/ annual DFE Ø Educate on signs & symptoms Ø Refer if breaks at margin are discovered Ø Examine parents, siblings
Health Care in New Brunswick My macula is still on, but the detachment is progressing quickly In New Brunswick and neighboring Nova Scotia - one surgical retinologist He is out of the country on vacation My options Ø Fly home- it will take too long Ø Get across the border to US health care With Lil and Dwight at the helm, I head fo the border
On the road again Our local retinal specialist back in Texas, Dr. Eddie Ysasaga arranges for me to see a retinal specialist in Portland, Maine the next morning Dr. Lil Linton and her husband Dwight drive me 300 miles to Portland while I lie face down in the back seat Portland retinal surgeon Dr. Fred Miller has made reservations for us at the La Quinta across the street from his office
What was going through my head? Sometimes ignorance is bliss Ø Macula on detachments have much better prognosistherefore an ocular emergency Ø I could tell from my vision that the detachment was getting close to fixation Ø I knew exactly what was happening Fear- what will I do if I lose my vision Second guessing- I should have let Juan dilate me I am going to go through this without the physical presence of family or friends I pray a lot

27 April 2008 7: 00 am- Dr. Fred Miller is waiting at his office- he has already contacted the surgery center & has people in place He confirms the diagnosis and we discuss surgical options Ø We decide to go with a vitrectomy, cryo, and air bubble- partly at my insistence He personally drives me to the center and we prep for surgery
27 April 2008 9: 00 am- I am ready for surgery and we head for the OR Ø I get and IV and some Versed Ø I am awake, but “happy”
In the OR Dr. Miller inserts ports through my pars plana, and performs a vitrectomy. He fills my eye with air and cryos the area around the flap tear He then performs a retinotomy to allow fluid under my retina to escape They close. I can see nothing with my right eye Now the waiting begins- I go back to the La Quinta and sleep
28 April 2008 After a night of sleeping with my head elevated, I awake, walk across the street to Dr. Miller’s office The initial findings; CF @ 2 feet, BUT if I hold a near card close to my eye I can see 20/30 I celebrate with pizza! My daughter Erin flies in- she will drive me 2300 miles back to Canyon, Texas
Why Not Fly? The pressure inside a commercial aircraft is roughly equivalent to an altitude of 6000 feet Rapid decline in air pressure causes the air bubble to expand causing high IOP, pain, vision loss Even going over a mountain has the same effects only more gradual The air bubble usually lasts @ 1 week
29 April 2008 Final check up with Dr. Miller looks good. My retina is flat, no infection. We hit the road Along the way, I begin to watch the bubble recede- I can read signs in my upper field. 1 May 2008 we arrive in Canyon The local retinal surgeon examines me the following day and is concerned Ø He tells me to be still and limit activity
6 May 2008 I am back at work on a limited schedule 2: 00 pm- as I examine my patient, I note a grey spot in my superior field and it makes me nervousØ It is déjà vu from the opposite direction 2: 30 pm- Dr. Janet Townsend informs me that now my right inferior retina is beginning to detach The retinal specialist confirms her findings and we schedule surgery for the next day
Why did it detach again? Pavingstone degeneration is common in high myopes It is innocuous unless the individual has a retinal detachment Pavingstone then becomes a potential site for multiple tears to occur I had seven tears This time the bottom half of my retina is detached
7 May 2008 (My Birthday) 7: 00 am- this time the procedure will be much more invasive Dr. Antonio Aragon inserts ports through the pars plana He fills my eye with air 83% air and 17% C 3 F 8, (octafluoropropane) the longest residing gas used in retinal surgery. Ø Other options include air and SF 6
Filling in for Vitreous Air- Cheap, only good in certain cases Ø Short residence time (@ 1 week) Ø May not be adequate for some cases u. Require longer tamponade SF 6 (sulfur hexafluoride) Ø Medium residence time (@ 2 -3 weeks) C 3 F 8 (octafluoropropane) Ø Long residence time (@ 6 -8 weeks) Longer duration reduces likelihood of failure, redetachment
Happy Birthday Dr. Aragon positions a silicone band around my peripheral retina and tightens it to bring it in contact with RPE He then lasers the areas around the tears and closes; we are finished! I am now to lie face down for the next ten days This is no way to spend your birthday!
The next ten days The initial post op report is good- I can see some print if I hold it close I wear a shield at all times, only removing it to instill Vigamox, Omnipred, and Nevanac Ten days later, I can only see hand motion and my eye hurts, but I can discontinue positioning face down

Three weeks later I am back at work, but can only see with one eye. Any procedure that requires binocular vision goes to my associates The bubble is regressing and I can see in my superior field Dr. Aragon is concerned; my eye is very inflamed The drops continue

Three months post op The gas bubble is gone I am now myopic, but with correction I am 20/20 But Ø My eye is still inflamed, with significant cells and flare Ø My pressures are going up because I use steroids every other hour. I now know what it is like to need steroids, but to be a steroid responder
5 months post op My inflammation still persists, but is beginning to decrease I am on three meds for IOP, but my pressure spikes as high as 51 mm Hg I see halos around lights I get discouraged We increase the Nevanac and taper the steroid

6 months post op I am finally off all steroids There is no flare, shaking my head results in an amazing display of cells Leukocytes still reside in my anterior chamber blocking outflow. I take my meds; the IOP is < 30 mm Hg OCT of my nerve looks good I continue Combigan Q 12 hours & Azopt Q 8 hours

Today Moderate NS OS Pseudophakia OD with 20/20+ vision No inflammation No medications I am blessed!
Conclusion I appreciate vision more than ever before I appreciate what we as optometrists do more than ever Know the risk factors for retinal tears & detachment Know how to recognize and manage peripheral retinal conditions that pose a risk of retinal tears, detachment Take good care of your own eyes THANK YOU
 Hemophtalmus
Hemophtalmus Padded tongue blade
Padded tongue blade Anterior hyaloid membrane
Anterior hyaloid membrane Autism nursing diagnosis
Autism nursing diagnosis Impaired swallowing nursing diagnosis
Impaired swallowing nursing diagnosis Retinal detachment
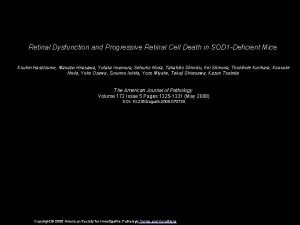
Retinal detachment Retinal detachment presentation
Retinal detachment presentation Now i see it now you don't
Now i see it now you don't Color constancy ap psychology
Color constancy ap psychology Retinal vessels
Retinal vessels Pragnanz ilkesi
Pragnanz ilkesi Monocular depth cues interposition
Monocular depth cues interposition Retinal disparity definition psychology
Retinal disparity definition psychology Phi phenomenon
Phi phenomenon Paroxysmal hemicrania
Paroxysmal hemicrania Vergensi
Vergensi Cystic retinal tuft
Cystic retinal tuft Retinal disparity psychology
Retinal disparity psychology Optic nerve histology
Optic nerve histology Storied and non storied cell types
Storied and non storied cell types Retinal ganglion
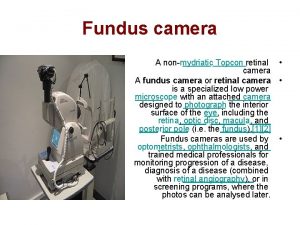
Retinal ganglion Topcon retinal camera
Topcon retinal camera Depth perception ap psychology
Depth perception ap psychology Retinopexy
Retinopexy Screenless display technology documentation
Screenless display technology documentation Lesson 7 now you see it the copper cycle answer key
Lesson 7 now you see it the copper cycle answer key All these pieces broken and scattered
All these pieces broken and scattered Modal verbs
Modal verbs I once was blind but now i see
I once was blind but now i see Modal passive
Modal passive Eye can see clearly now
Eye can see clearly now Vitrous detachment
Vitrous detachment Attachment issues
Attachment issues Rule of detachment logic
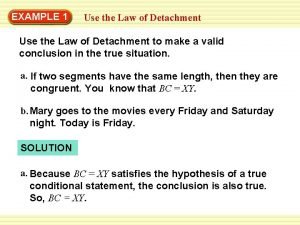
Rule of detachment logic Posterior vitreous detachment
Posterior vitreous detachment Mastering detatchment
Mastering detatchment Care welfare safety and security
Care welfare safety and security Cpi defensive behavior
Cpi defensive behavior Law of detachment example
Law of detachment example Trailblazer personality type
Trailblazer personality type Qualities of atticus finch
Qualities of atticus finch Law of detachment geometry
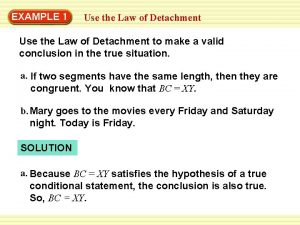
Law of detachment geometry Rule of detachment logic
Rule of detachment logic Deductive reasoning
Deductive reasoning Detachment stylistic device
Detachment stylistic device Tuesdays with morrie the curriculum
Tuesdays with morrie the curriculum Detachment transportation and deposition
Detachment transportation and deposition Law of detachment
Law of detachment Detachment of planners
Detachment of planners Law of detachment example
Law of detachment example Crisis development model integrated experience
Crisis development model integrated experience Lhi army number
Lhi army number See judge act framework
See judge act framework Hello in lithuanian
Hello in lithuanian Future continuous.
Future continuous. What do you see
What do you see Tigers
Tigers