Differential diagnosis Pancreatic arteriovenous malformation Pancreatic AVMS are
- Slides: 16
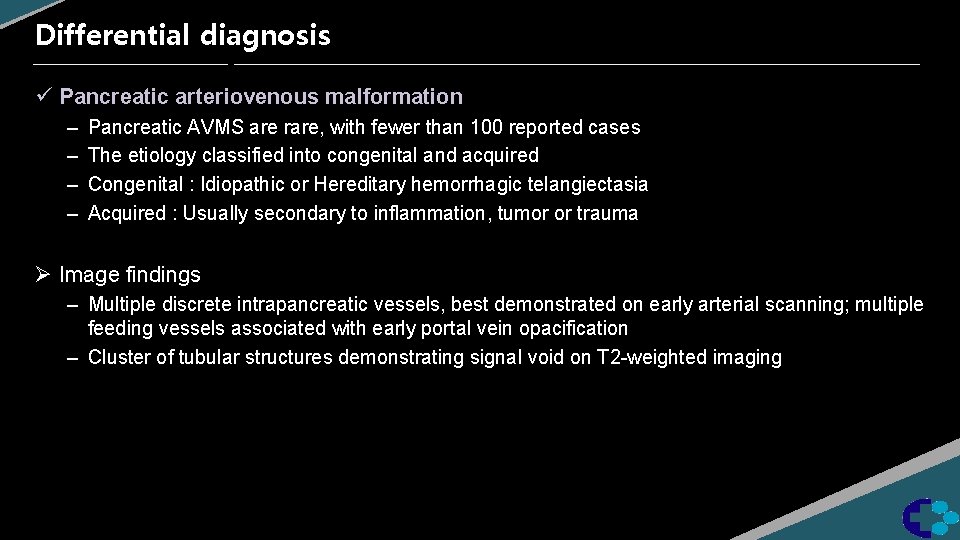
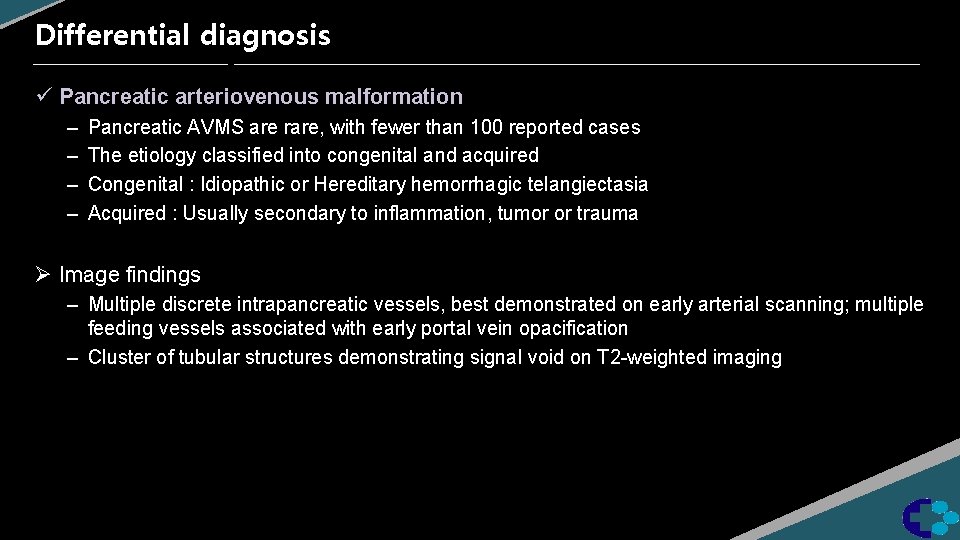
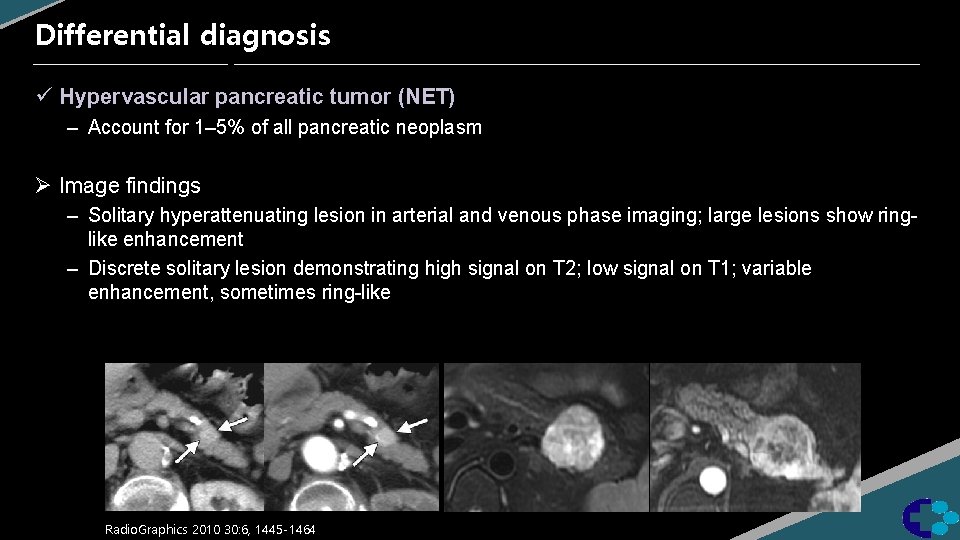
Differential diagnosis ü Pancreatic arteriovenous malformation – – Pancreatic AVMS are rare, with fewer than 100 reported cases The etiology classified into congenital and acquired Congenital : Idiopathic or Hereditary hemorrhagic telangiectasia Acquired : Usually secondary to inflammation, tumor or trauma Ø Image findings – Multiple discrete intrapancreatic vessels, best demonstrated on early arterial scanning; multiple feeding vessels associated with early portal vein opacification – Cluster of tubular structures demonstrating signal void on T 2 -weighted imaging
J Korean Soc Radiol 2010; 62: 257 -261
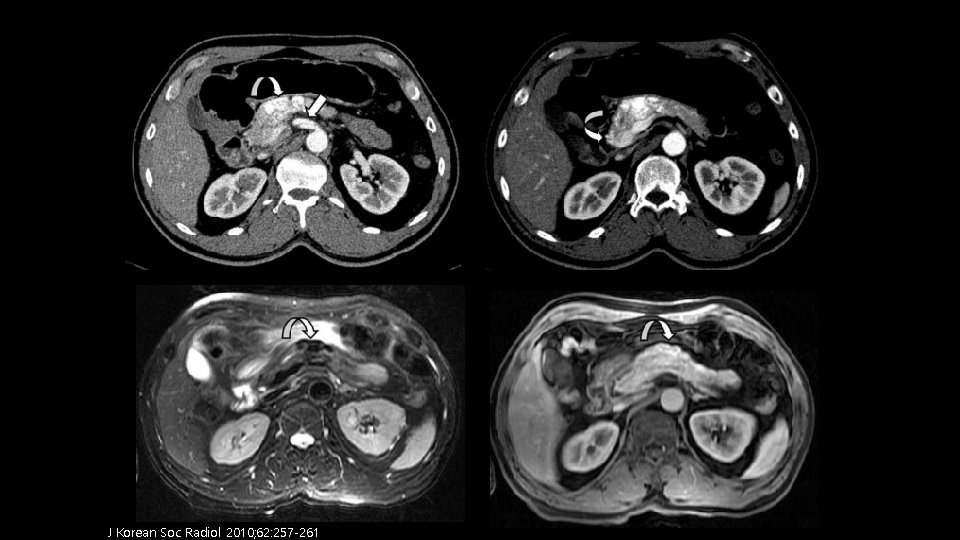
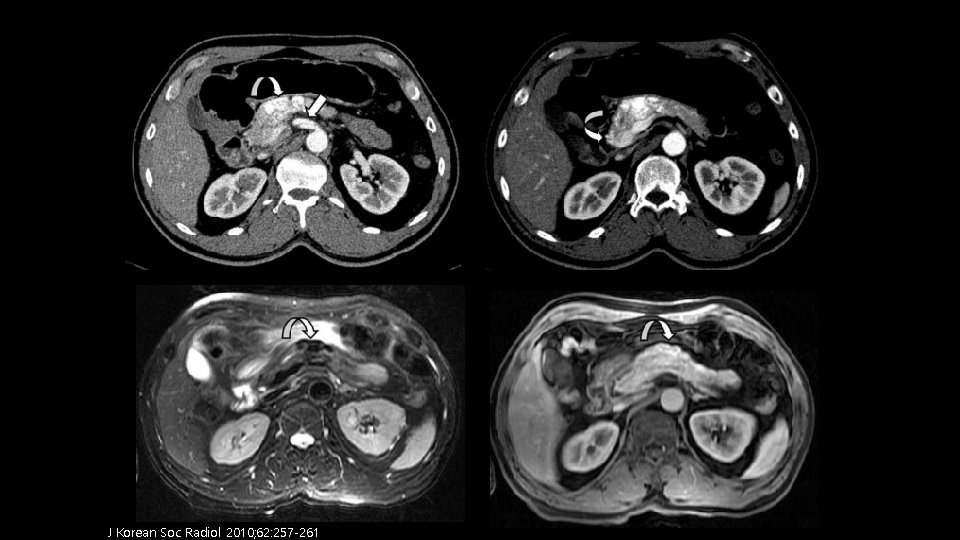
Differential diagnosis ü Hypervascular metastases – Commonly seen with renal cell carcinoma and melanoma Ø Image findings – Solitary or multiple discrete masses with peripheral or homogeneous enhancement – Solitary or multiple discrete masses with variable signal intensity; peripheral or homogeneous enhancement Clin Imaging. 2004 Sep-Oct; 28(5): 349 -52.
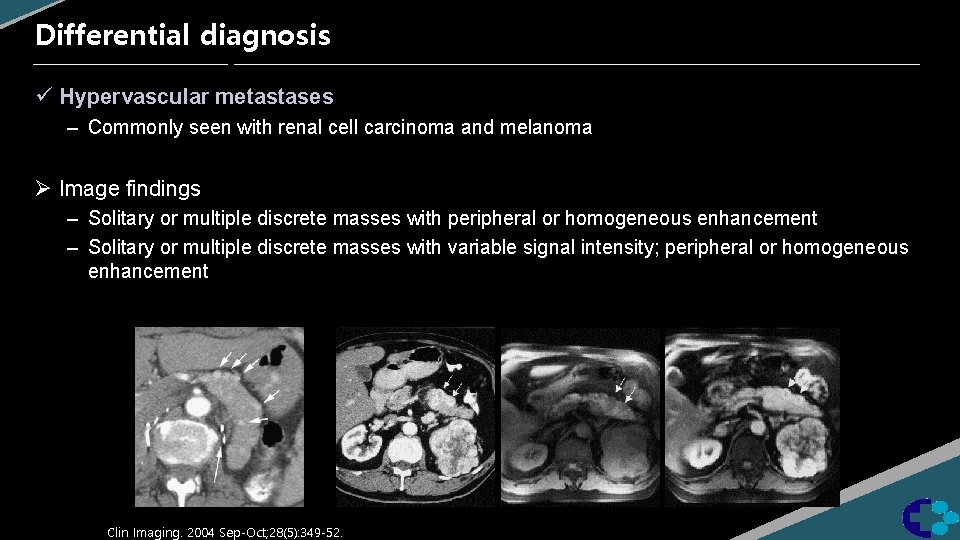
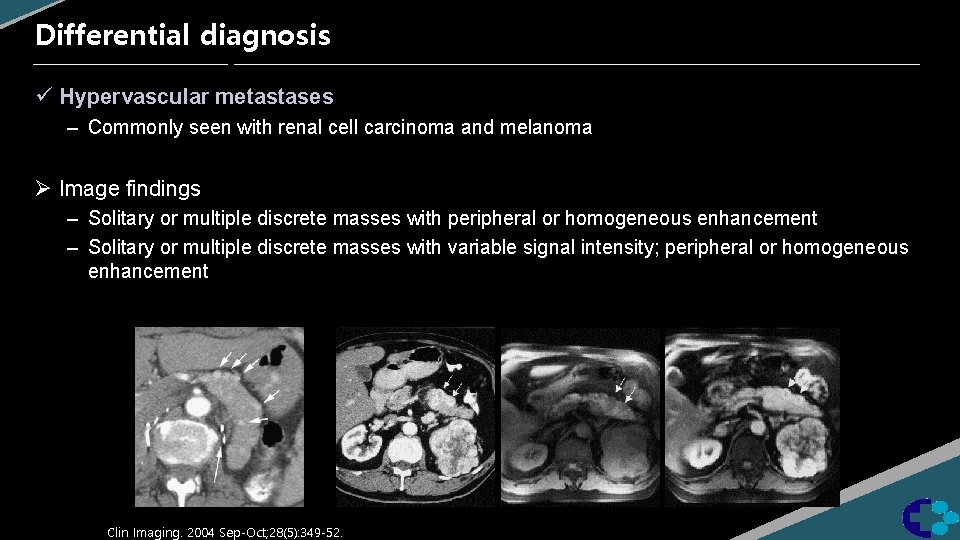
Differential diagnosis ü Hypervascular pancreatic tumor (NET) – Account for 1– 5% of all pancreatic neoplasm Ø Image findings – Solitary hyperattenuating lesion in arterial and venous phase imaging; large lesions show ringlike enhancement – Discrete solitary lesion demonstrating high signal on T 2; low signal on T 1; variable enhancement, sometimes ring-like Radio. Graphics 2010 30: 6, 1445 -1464
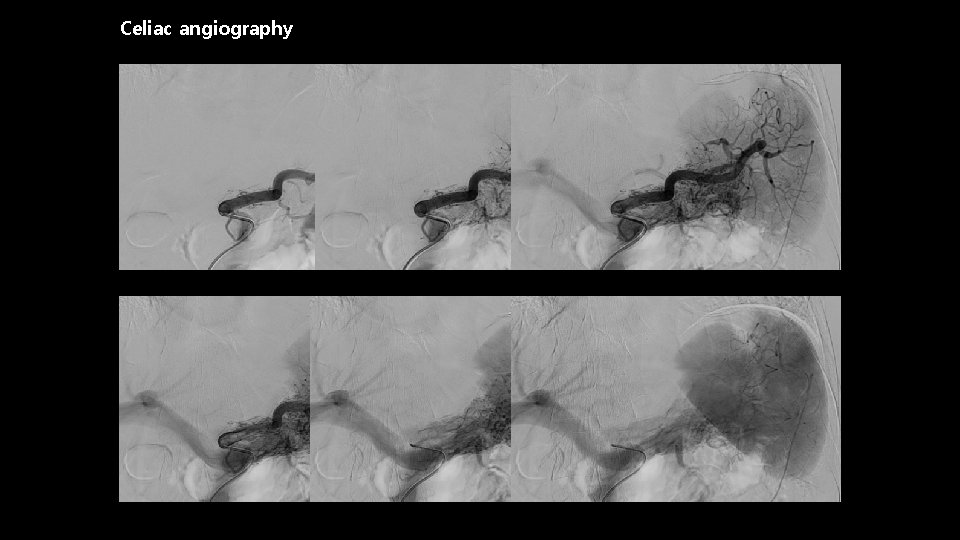
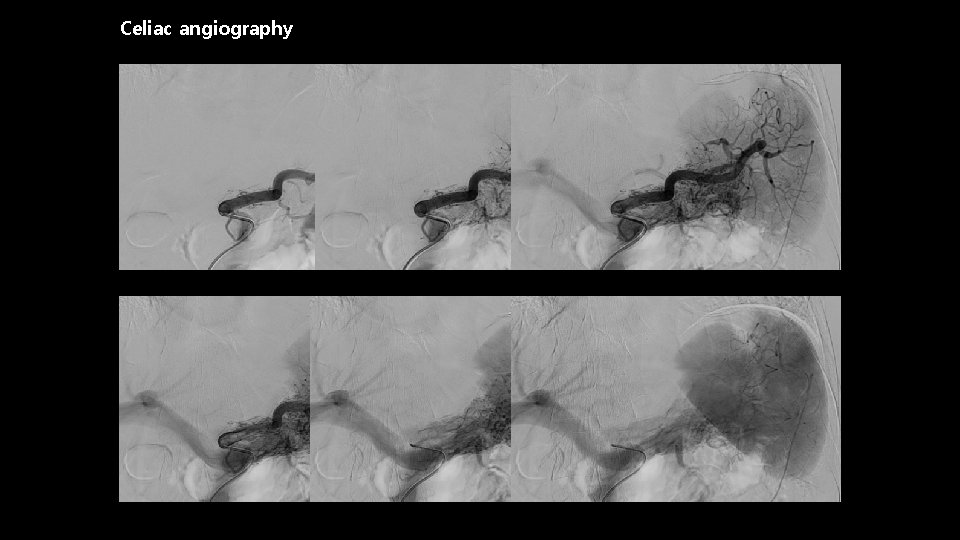
Celiac angiography
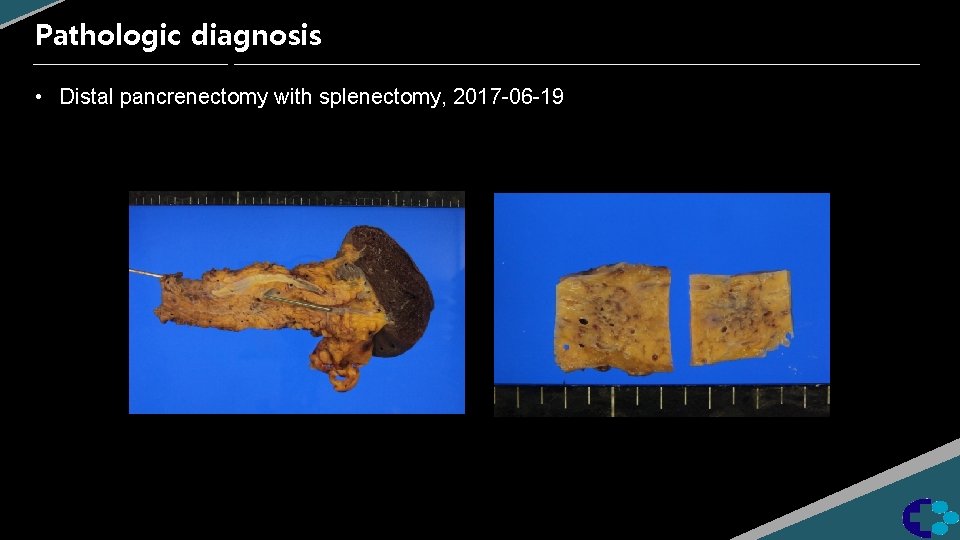
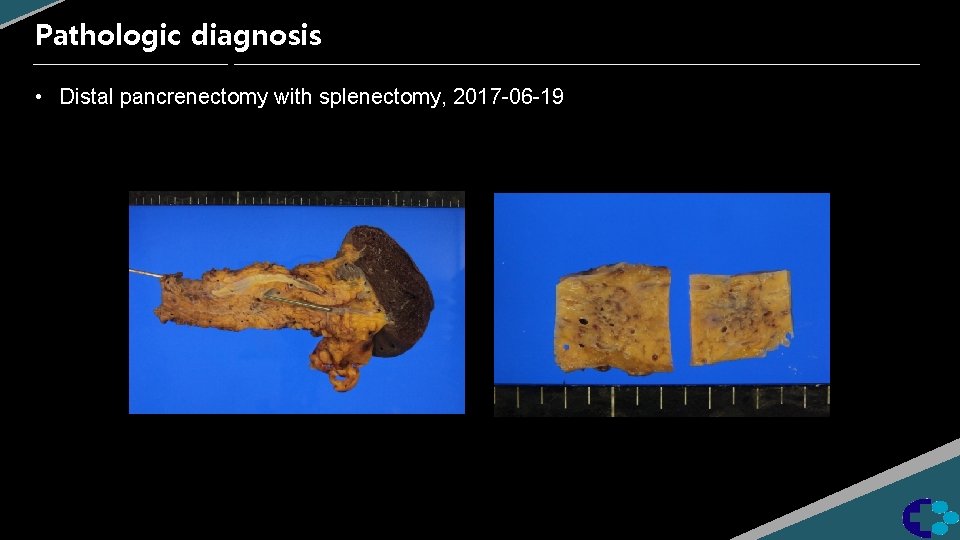
Pathologic diagnosis • Distal pancrenectomy with splenectomy, 2017 -06 -19
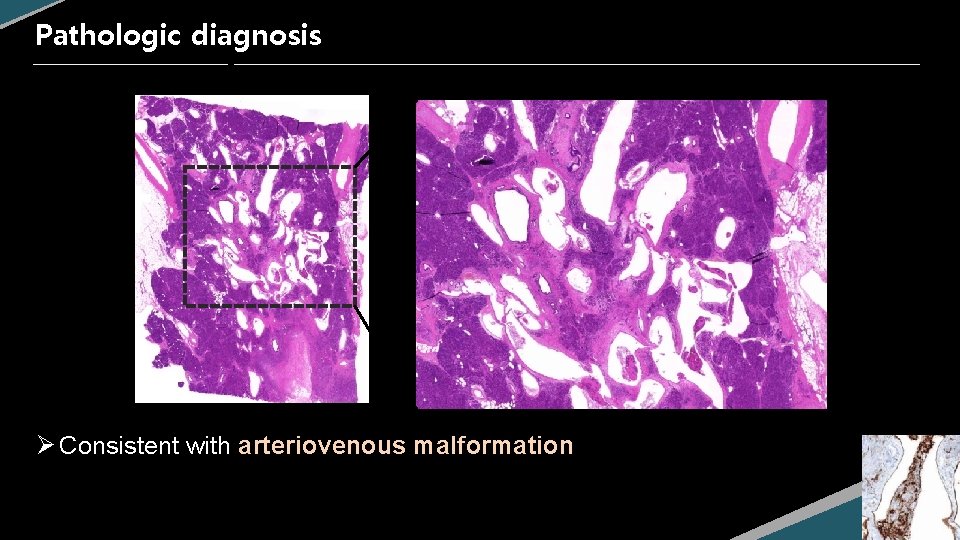
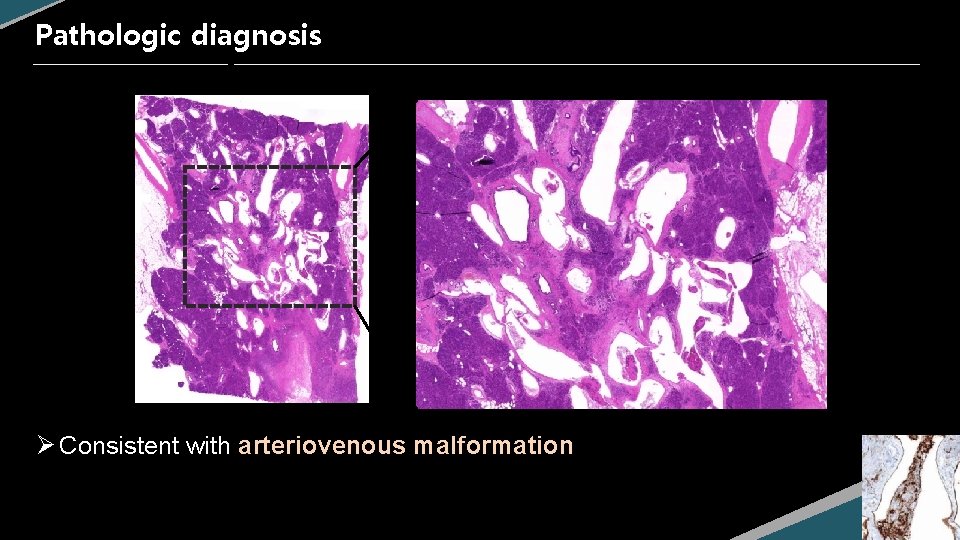
Pathologic diagnosis Ø Consistent with arteriovenous malformation
Review Pancreas AVM
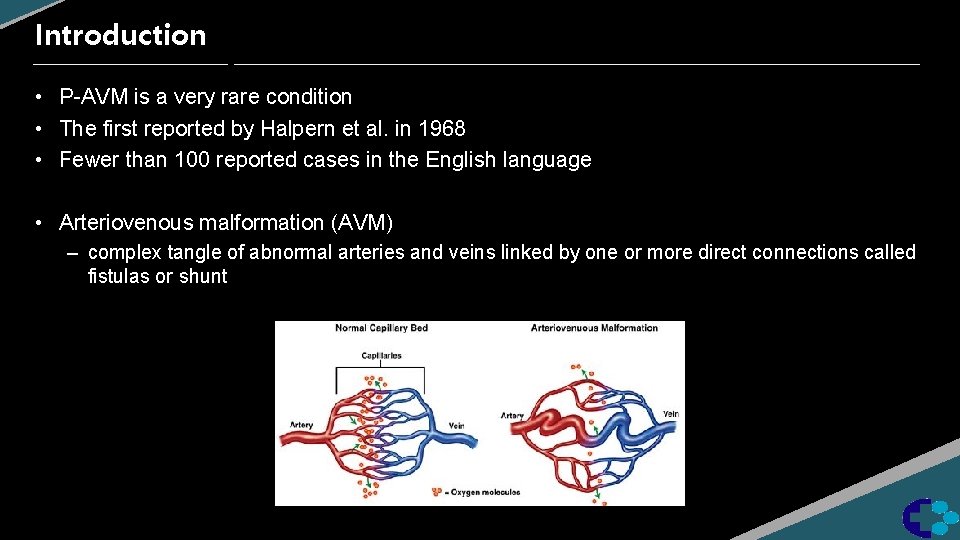
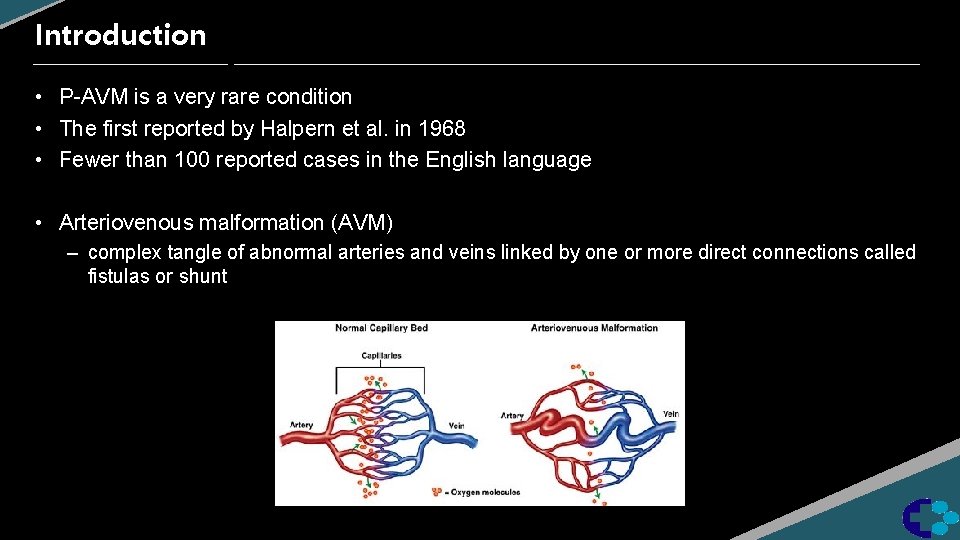
Introduction • P-AVM is a very rare condition • The first reported by Halpern et al. in 1968 • Fewer than 100 reported cases in the English language • Arteriovenous malformation (AVM) – complex tangle of abnormal arteries and veins linked by one or more direct connections called fistulas or shunt
Etiology • Gender : Strong male predilection (88%) • Age : 7 mos - 73 yrs, predominantly 50– 60 years old • Risk factors : HHT, trauma, surgery, inflammation, tumor • Classified into congenital and acquired – Congenital type ; 90% • 15% of Hereditary hemorrhagic telangiectasia – (= Osler–Weber–Rendu syndrome) – AD multiorgan vascular dysplasia, characterized by multiple AVMs – Acquired type; 10% • usually secondary to inflammation, tumor or trauma
Clinical manifestations • Frequently associated with abdominal pain and gastrointestinal bleeding • Steal syndrome may cause abdominal pain – Shunting of blood away from the mesenteric circulation through the AVM • Mechanism of gastrointestinal bleeding into the following five types 1) 2) 3) 4) 5) bleeding from esophagogastric varices secondary to portal hypertension bleeding from the AVM to the pancreatic duct bleeding from the AVM to the bile duct bleeding from intestinal mucosa in contact with the AVM bleeding from a duodenal ulcer associated with the AVM
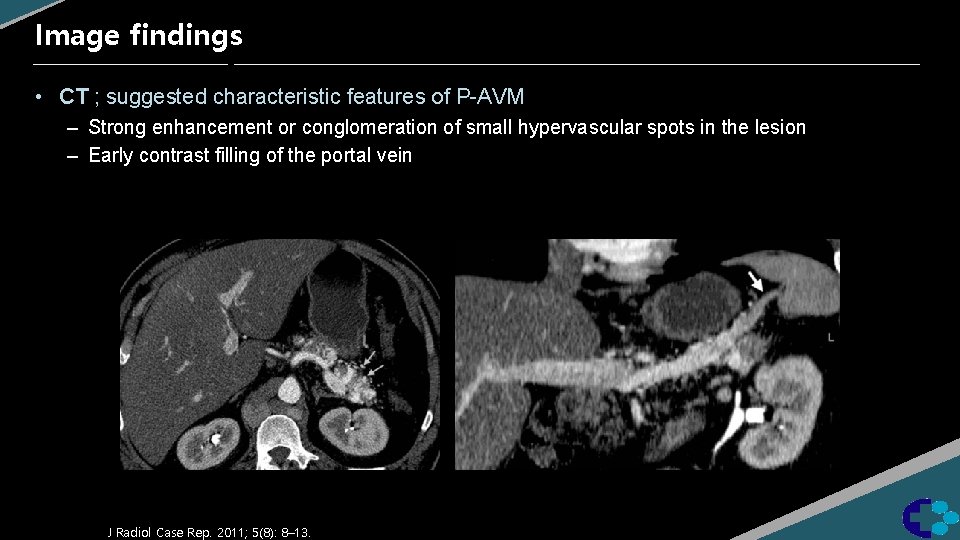
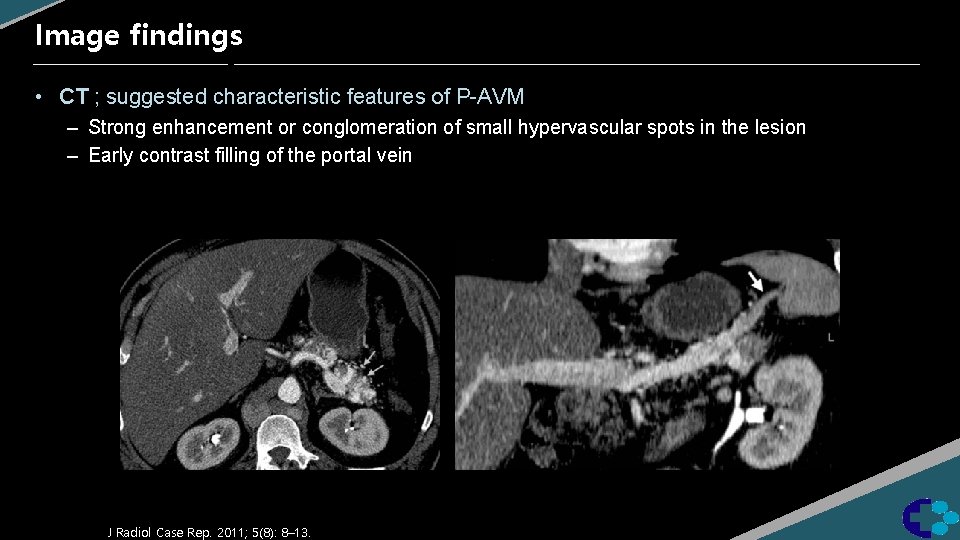
Image findings • CT ; suggested characteristic features of P-AVM – Strong enhancement or conglomeration of small hypervascular spots in the lesion – Early contrast filling of the portal vein J Radiol Case Rep. 2011; 5(8): 8– 13.
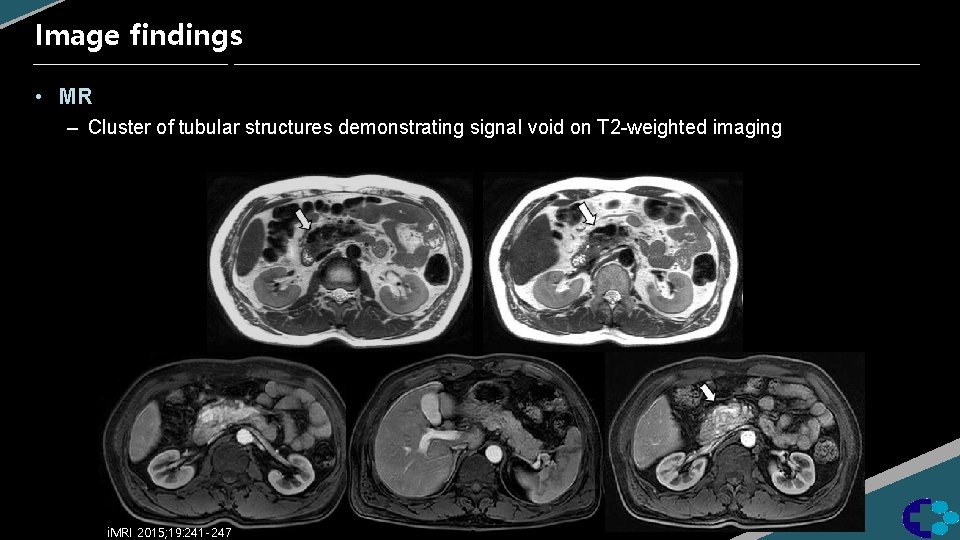
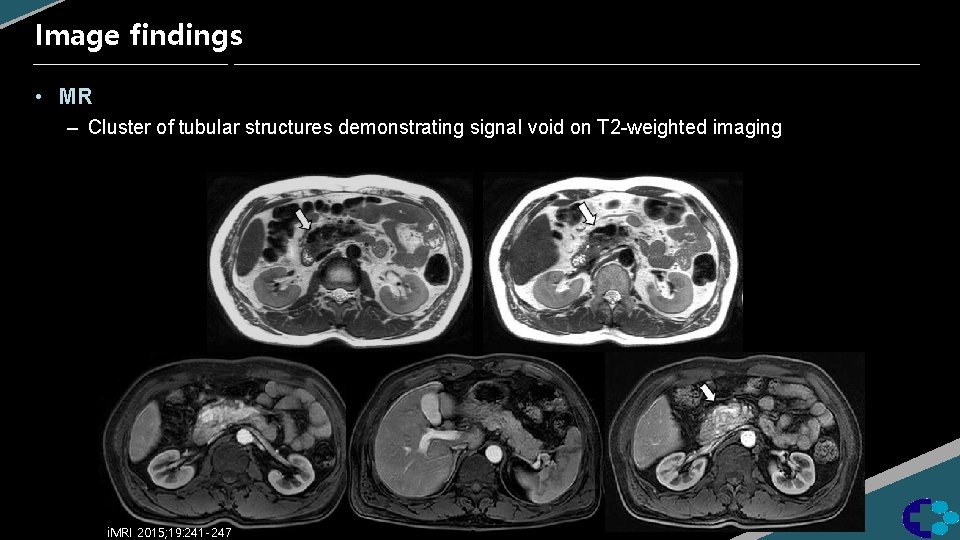
Image findings • MR – Cluster of tubular structures demonstrating signal void on T 2 -weighted imaging i. MRI 2015; 19: 241 -247
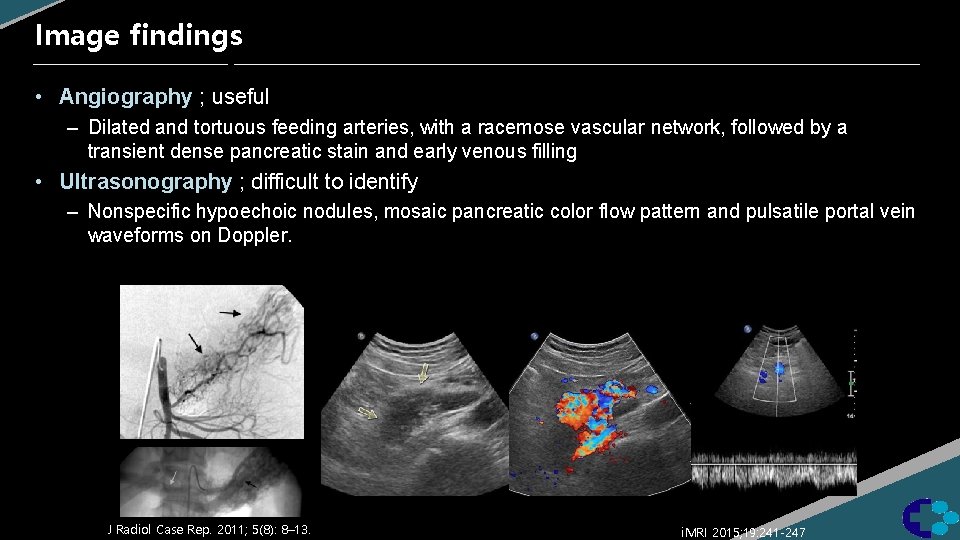
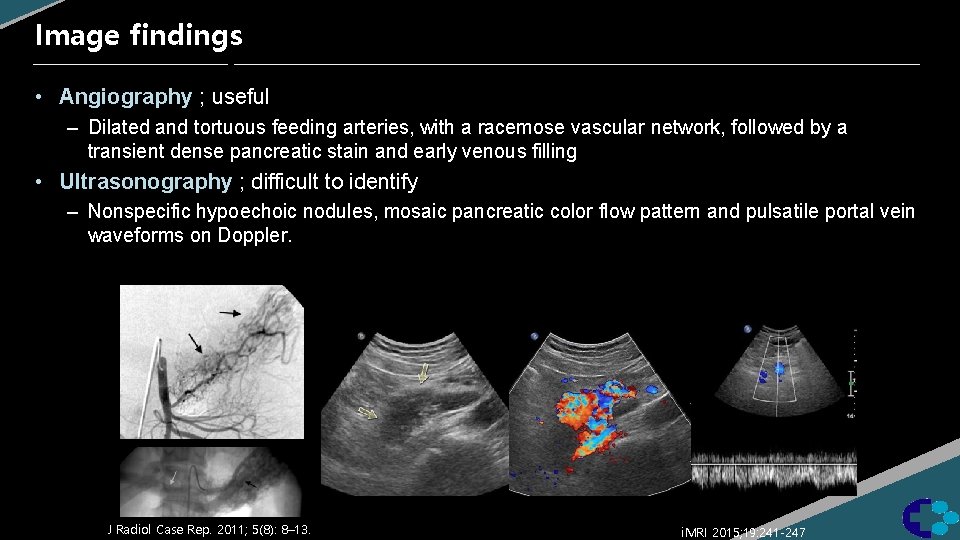
Image findings • Angiography ; useful – Dilated and tortuous feeding arteries, with a racemose vascular network, followed by a transient dense pancreatic stain and early venous filling • Ultrasonography ; difficult to identify – Nonspecific hypoechoic nodules, mosaic pancreatic color flow pattern and pulsatile portal vein waveforms on Doppler. J Radiol Case Rep. 2011; 5(8): 8– 13. i. MRI 2015; 19: 241 -247
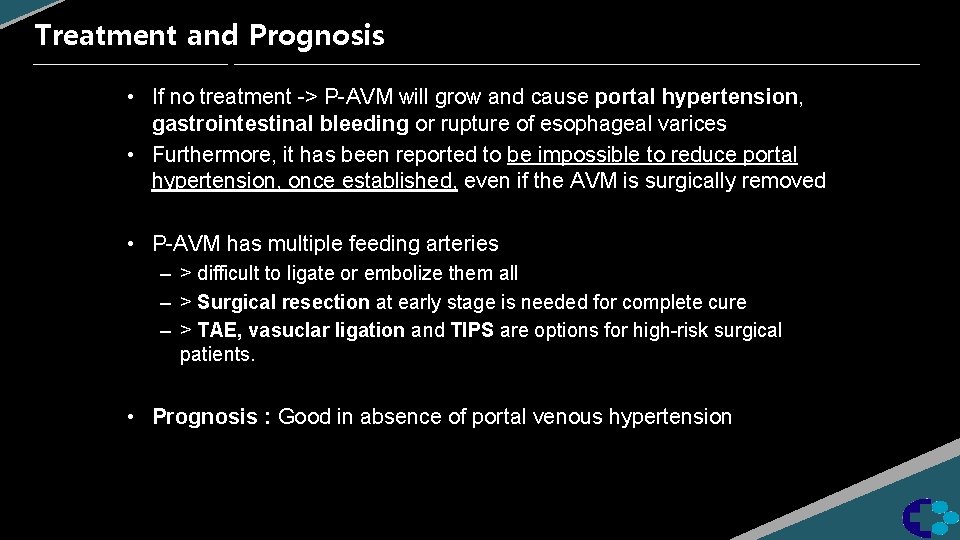
Treatment and Prognosis • If no treatment -> P-AVM will grow and cause portal hypertension, gastrointestinal bleeding or rupture of esophageal varices • Furthermore, it has been reported to be impossible to reduce portal hypertension, once established, even if the AVM is surgically removed • P-AVM has multiple feeding arteries – > difficult to ligate or embolize them all – > Surgical resection at early stage is needed for complete cure – > TAE, vasuclar ligation and TIPS are options for high-risk surgical patients. • Prognosis : Good in absence of portal venous hypertension
References • • J Korean Soc Radiol 2010; 62: 257 -261 Clin Imaging. 2004 Sep-Oct; 28(5): 349 -52. Radio. Graphics 2010 30: 6, 1445 -1464 i. MRI 2015; 19: 241 -247 J Radiol Case Rep. 2011; 5(8): 8– 13. Int J Angiol. 2008 Winter; 17(4): 211– 213. Case Rep Gastroenterol. 2014 Jan-Apr; 8(1): 26– 31. ECR 2012; C-1070
 Hemangioma arteriovenous malformation
Hemangioma arteriovenous malformation Insidan region jh
Insidan region jh Continuous arteriovenous hemofiltration
Continuous arteriovenous hemofiltration Arteriovenous nicking
Arteriovenous nicking Continuous arteriovenous hemofiltration
Continuous arteriovenous hemofiltration Pied bot
Pied bot Chiari malformation usmle
Chiari malformation usmle Wingspread classification of anorectal malformation
Wingspread classification of anorectal malformation Psarp procedure steps
Psarp procedure steps Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing process and critical thinking
Nursing process and critical thinking Ongoing planning in nursing process
Ongoing planning in nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Pernicious anemia symptoms
Pernicious anemia symptoms Ohio state lymphedema
Ohio state lymphedema Pitting vs non pitting edema
Pitting vs non pitting edema