Lymph Nodes Examination Examination of the Lymphatic System




- Slides: 105
Lymph Nodes Examination
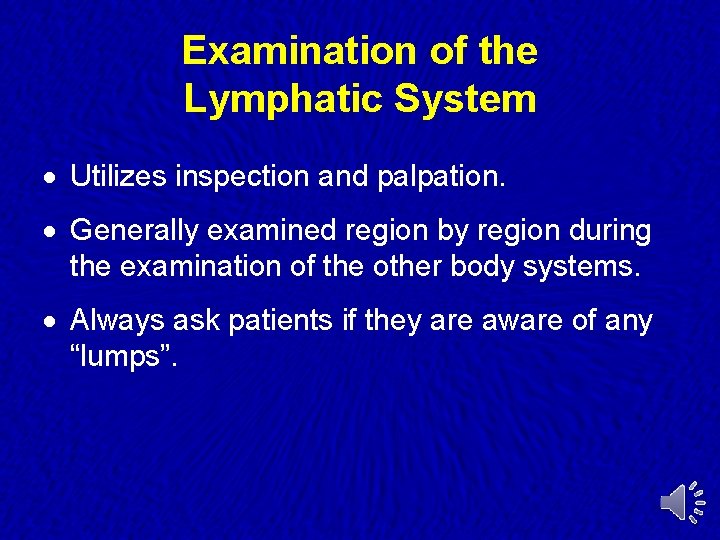
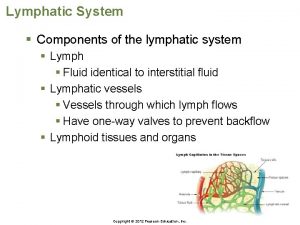
Examination of the Lymphatic System · Utilizes inspection and palpation. · Generally examined region by region during the examination of the other body systems. · Always ask patients if they are aware of any “lumps”.
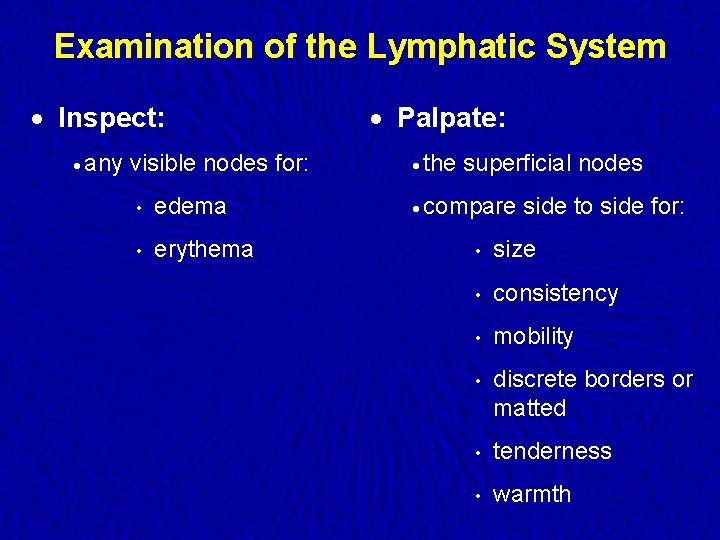
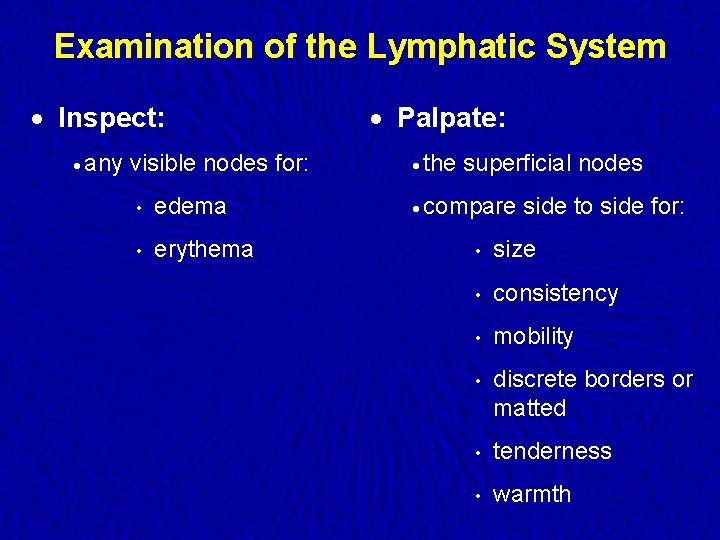
Examination of the Lymphatic System · Inspect: · Palpate: · any · the visible nodes for: • edema • erythema superficial nodes · compare side to side for: • size • consistency • mobility • discrete borders or matted • tenderness • warmth
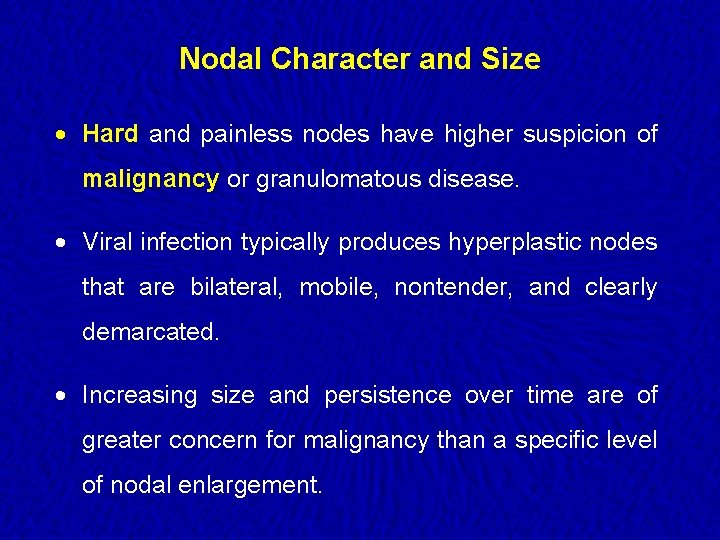
Nodal Character and Size · Hard and painless nodes have higher suspicion of malignancy or granulomatous disease. · Viral infection typically produces hyperplastic nodes that are bilateral, mobile, nontender, and clearly demarcated. · Increasing size and persistence over time are of greater concern for malignancy than a specific level of nodal enlargement.
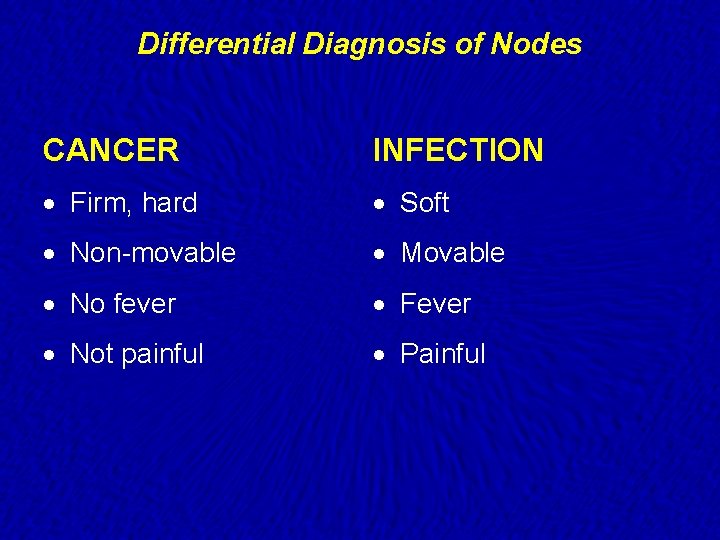
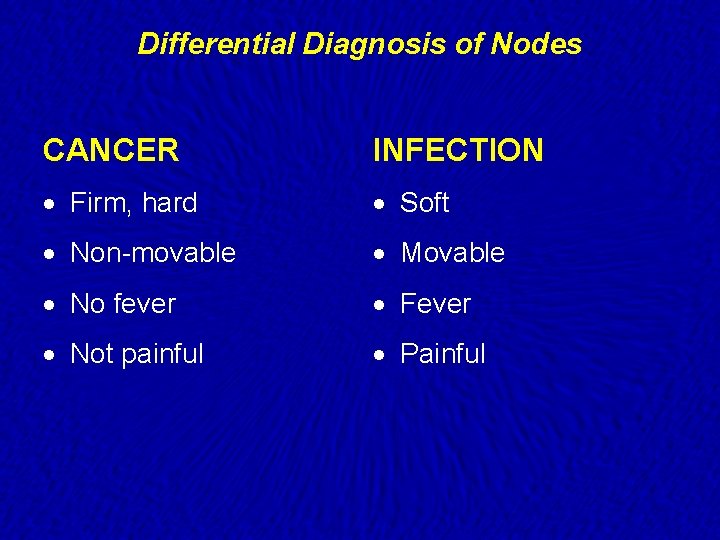
Differential Diagnosis of Nodes CANCER INFECTION · Firm, hard · Soft · Non-movable · Movable · No fever · Fever · Not painful · Painful
Examination of the Lymphatic System · If an enlarged lymph node is found, examine: ·P Primary site ·A All associated nodes ·L Liver ·S Spleen
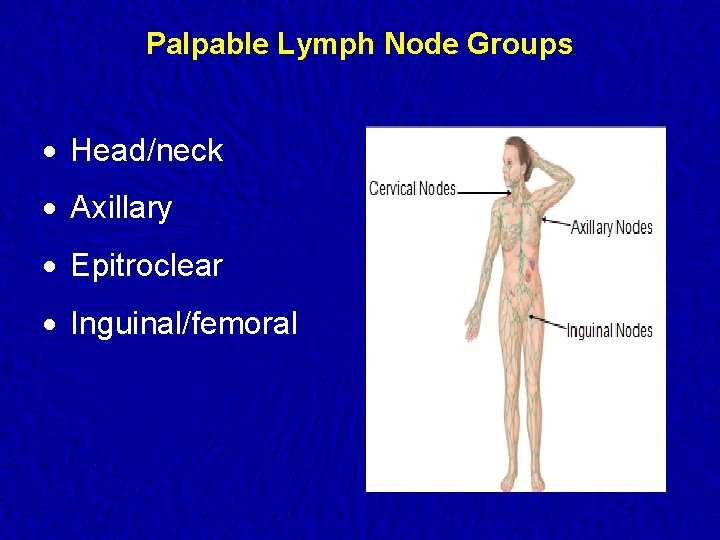
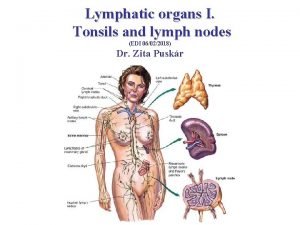
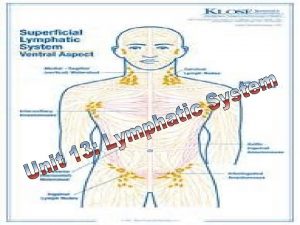
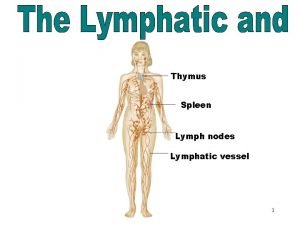
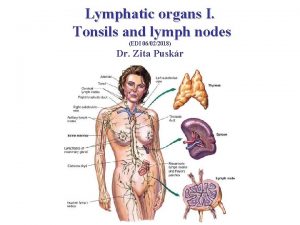
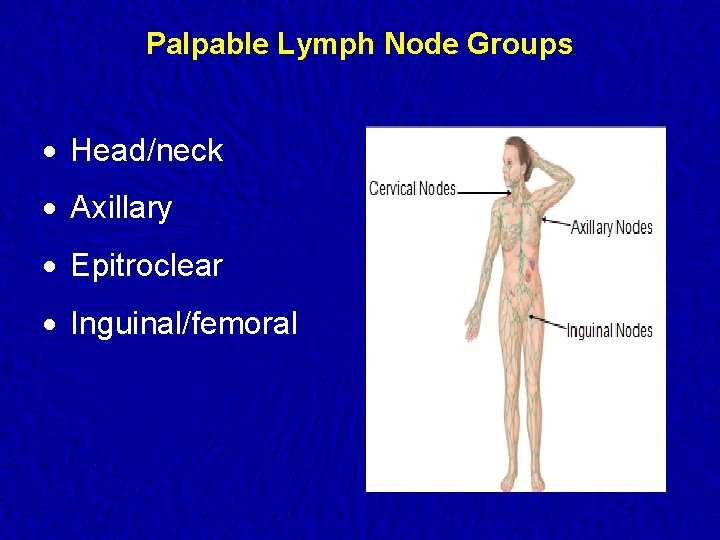
Palpable Lymph Node Groups · Head/neck · Axillary · Epitroclear · Inguinal/femoral
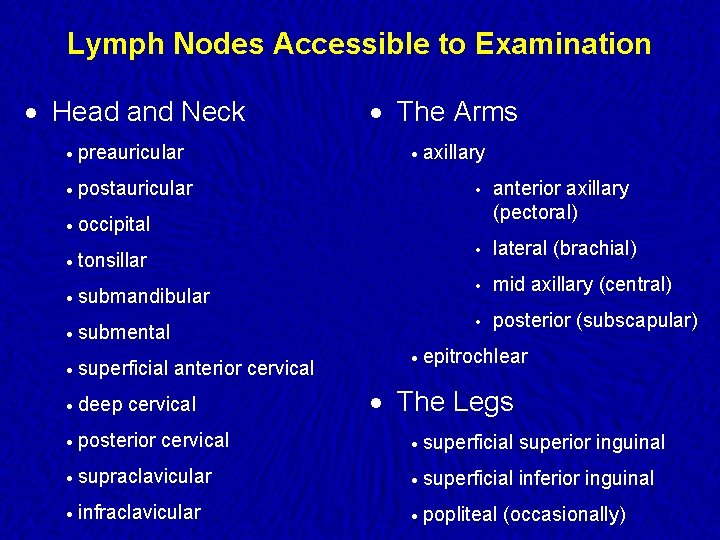
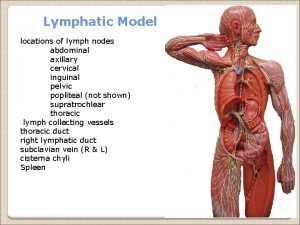
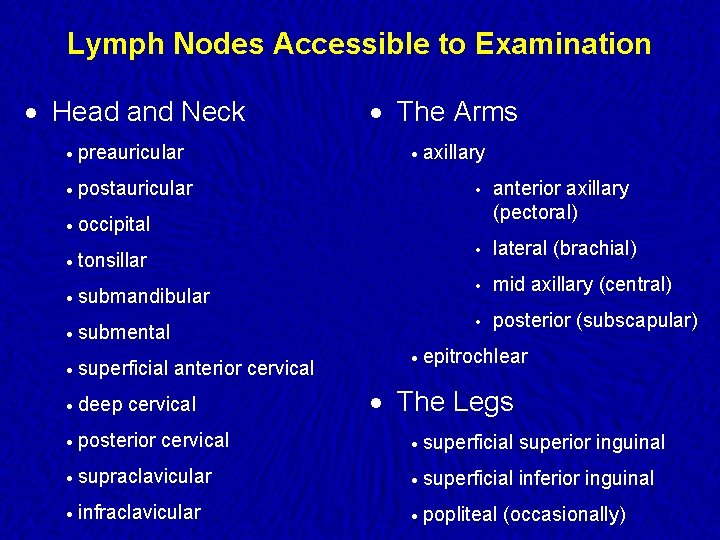
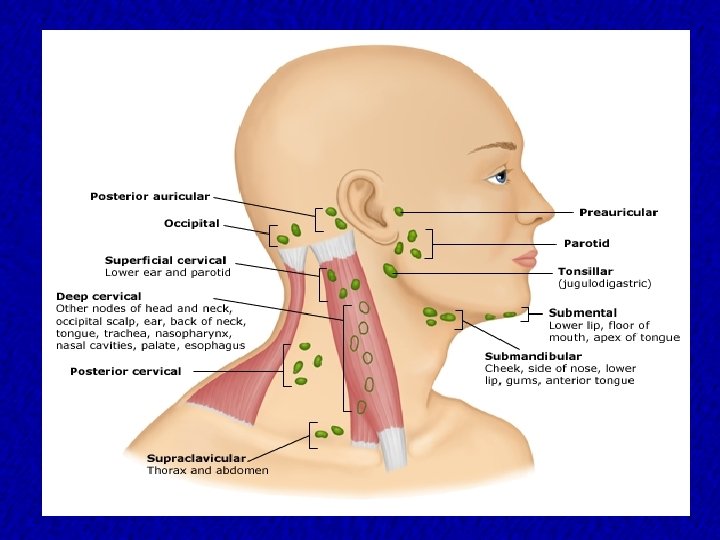
Lymph Nodes Accessible to Examination · Head and Neck · preauricular · postauricular · The Arms · axillary • anterior axillary (pectoral) • lateral (brachial) • mid axillary (central) • posterior (subscapular) · occipital · tonsillar · submandibular · submental · superficial · deep anterior cervical · posterior cervical · epitrochlear · The Legs · superficial superior inguinal · supraclavicular · superficial inferior inguinal · infraclavicular · popliteal (occasionally)
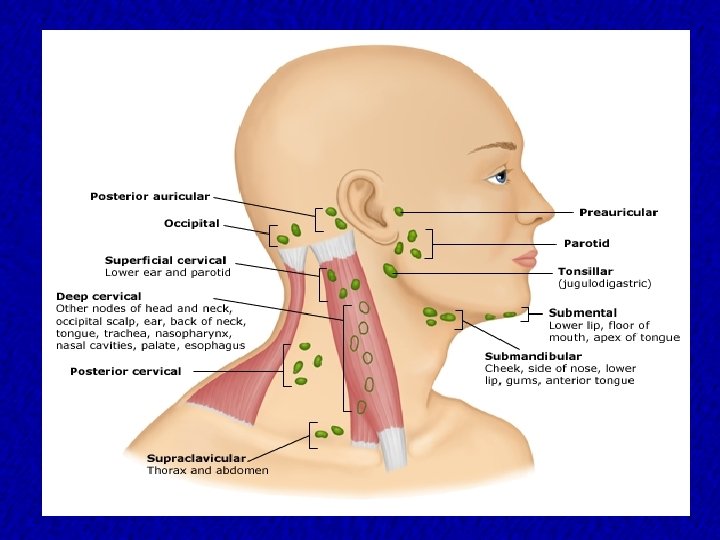
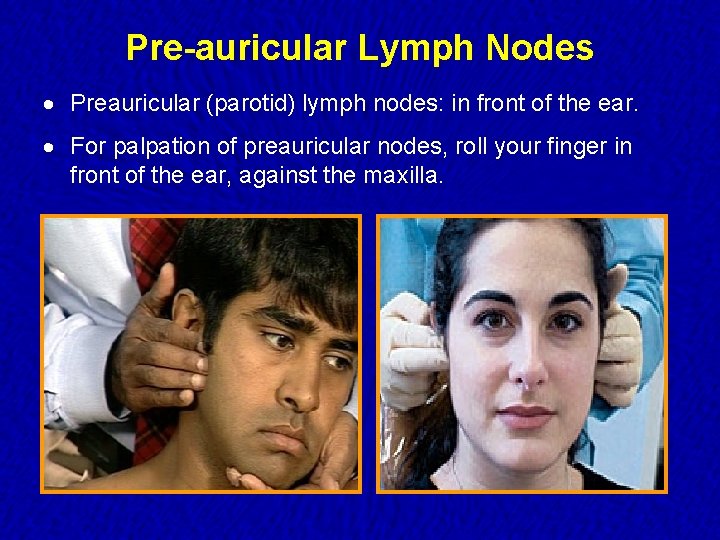
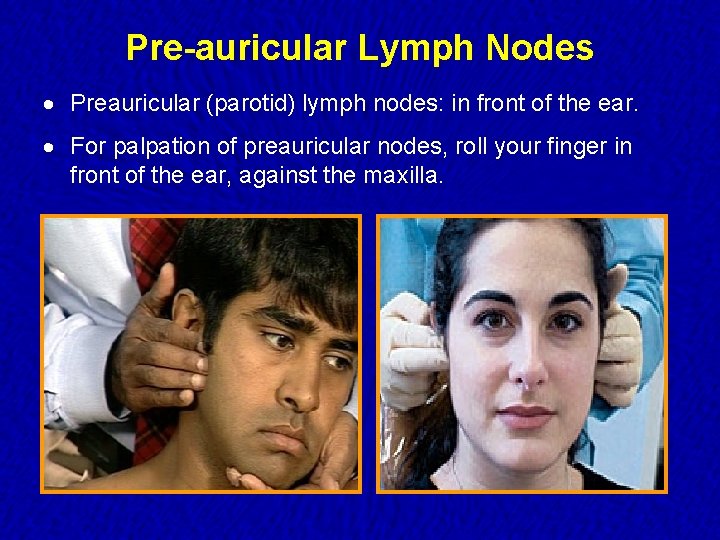
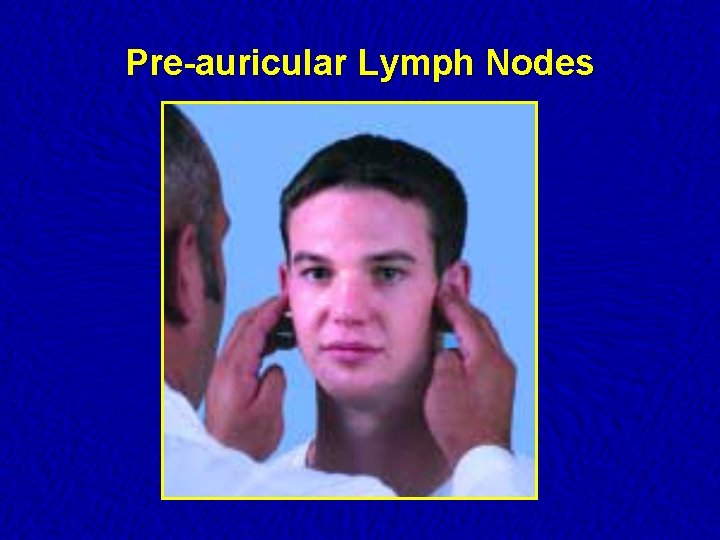
Pre-auricular Lymph Nodes · Preauricular (parotid) lymph nodes: in front of the ear. · For palpation of preauricular nodes, roll your finger in front of the ear, against the maxilla.
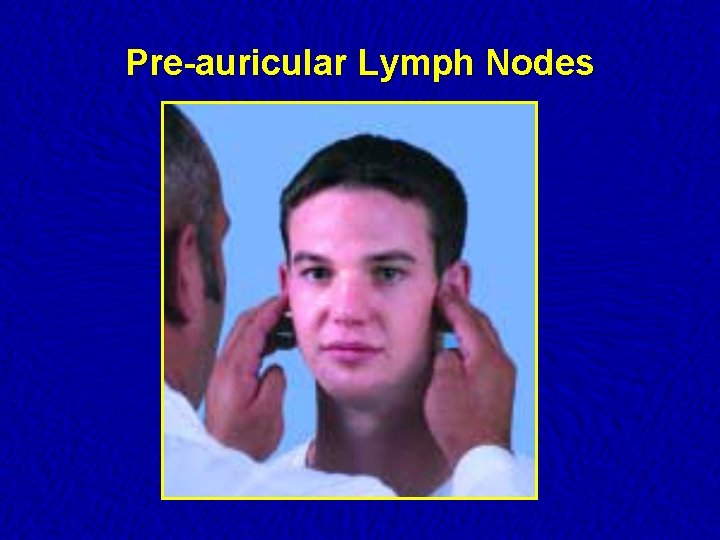
Pre-auricular Lymph Nodes
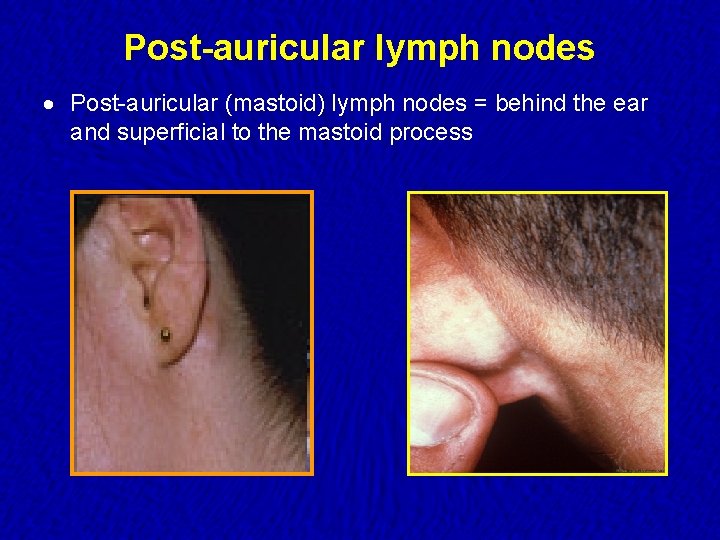
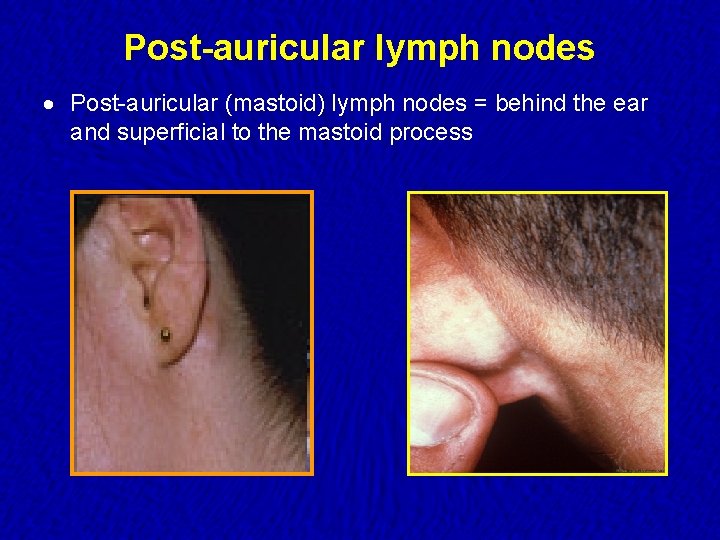
Post-auricular lymph nodes · Post-auricular (mastoid) lymph nodes = behind the ear and superficial to the mastoid process
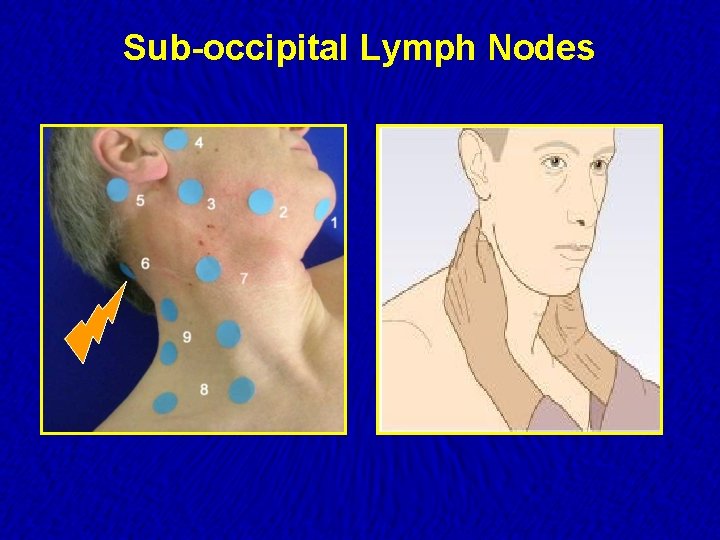
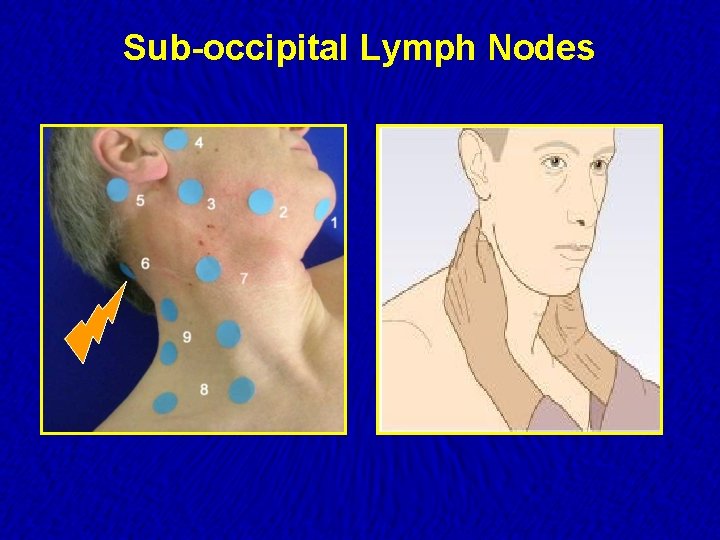
Sub-occipital Lymph Nodes
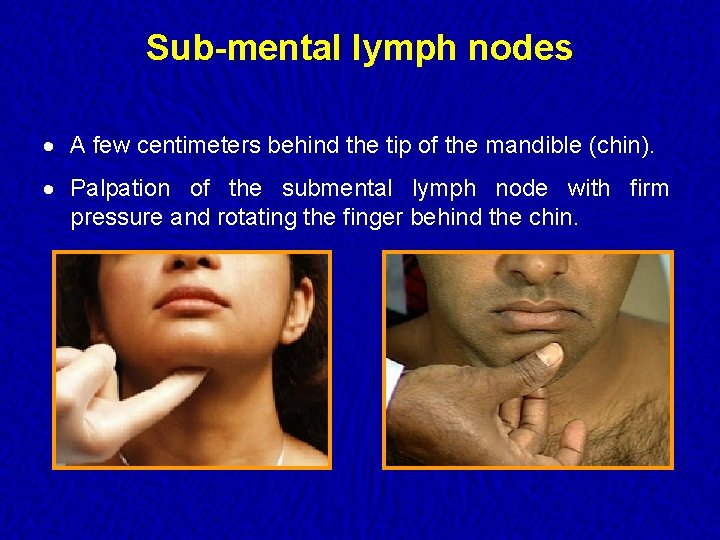
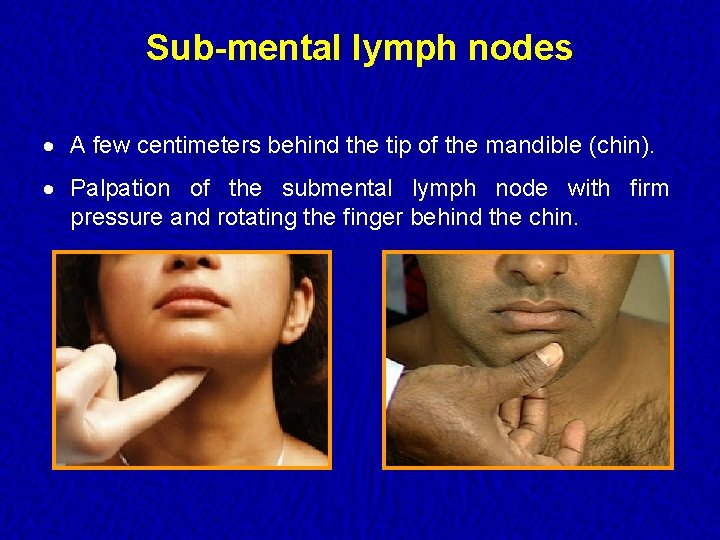
Sub-mental lymph nodes · A few centimeters behind the tip of the mandible (chin). · Palpation of the submental lymph node with firm pressure and rotating the finger behind the chin.
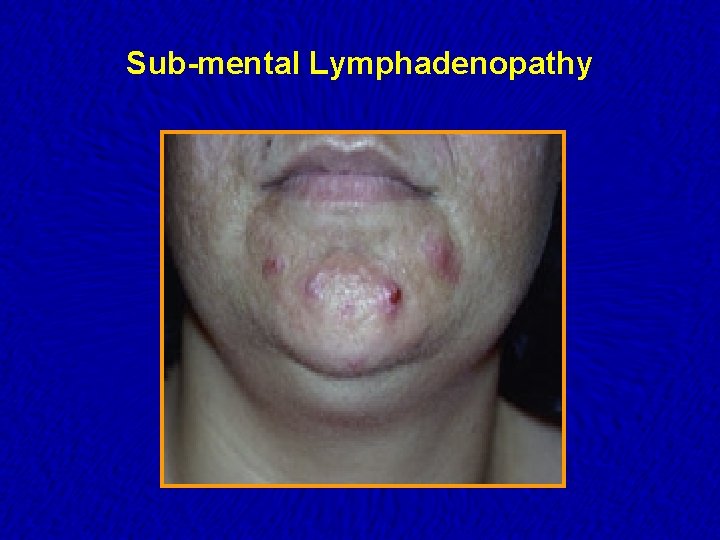
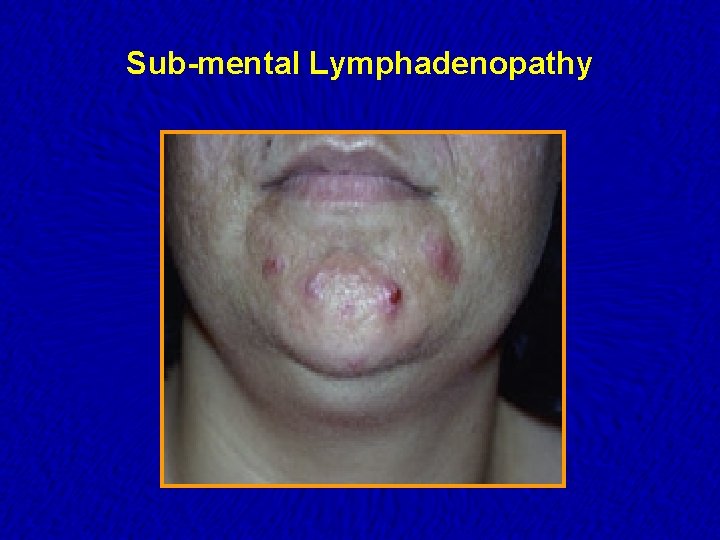
Sub-mental Lymphadenopathy
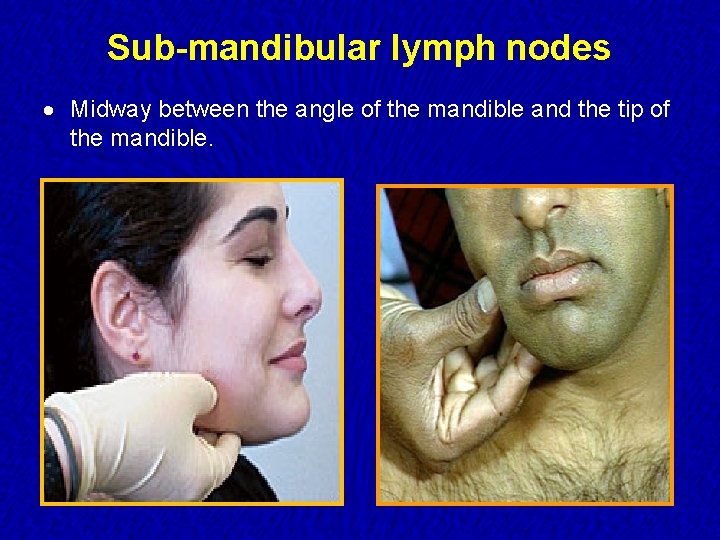
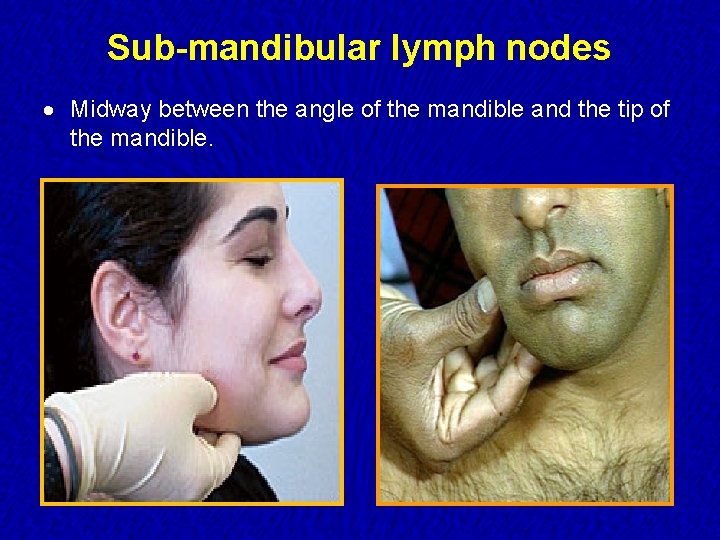
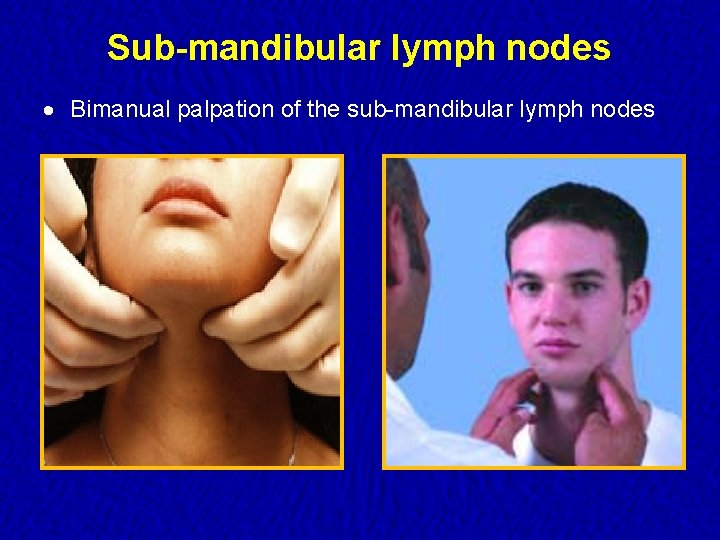
Sub-mandibular lymph nodes · Midway between the angle of the mandible and the tip of the mandible.
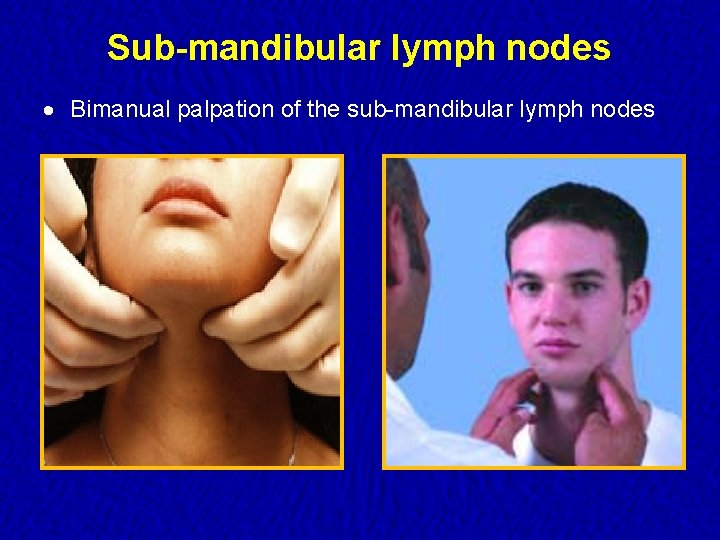
Sub-mandibular lymph nodes · Bimanual palpation of the sub-mandibular lymph nodes
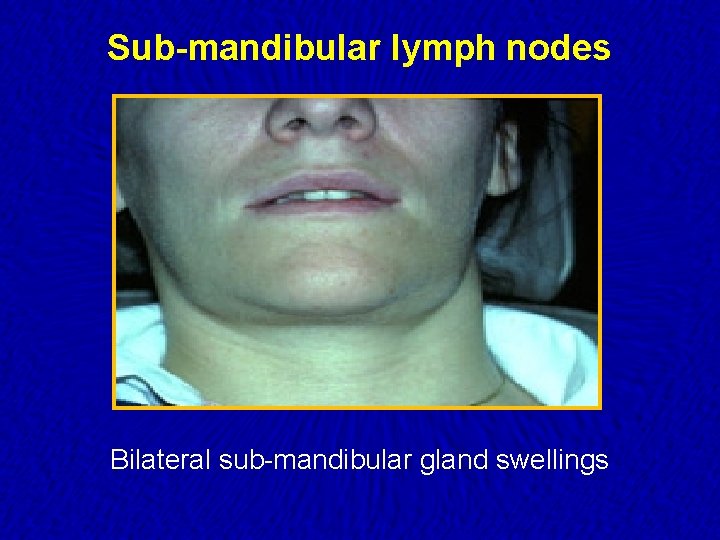
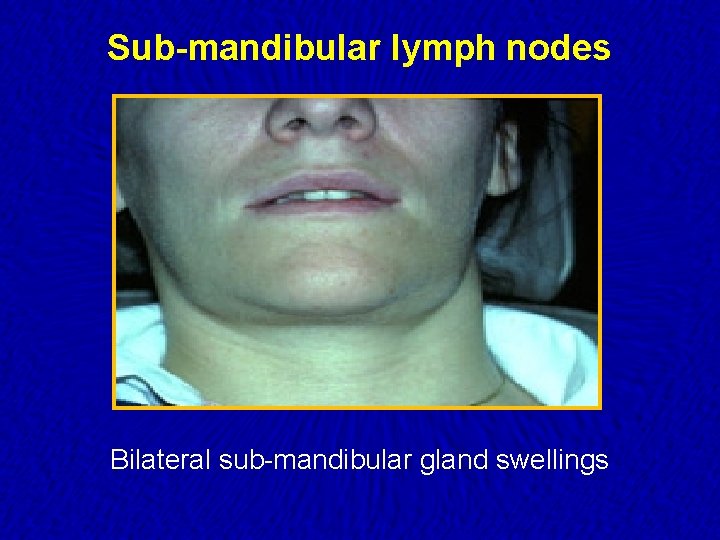
Sub-mandibular lymph nodes Bilateral sub-mandibular gland swellings
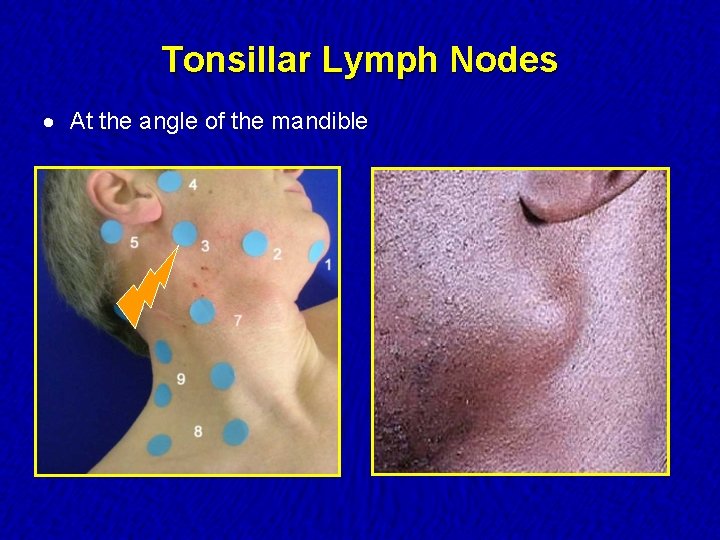
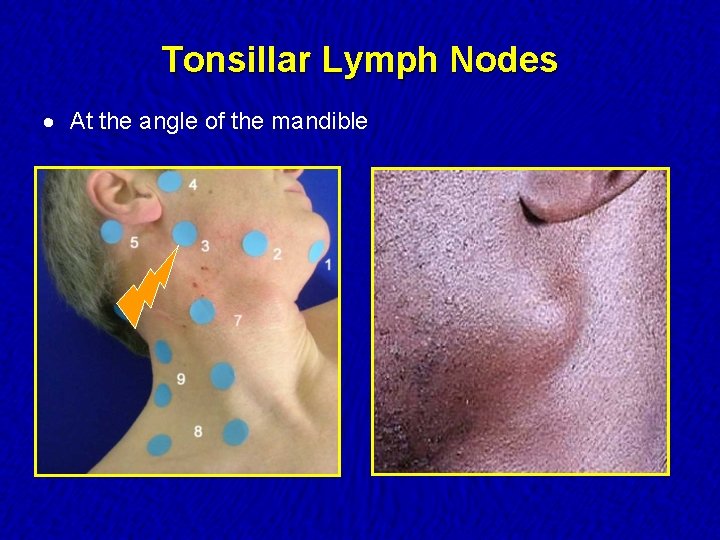
Tonsillar Lymph Nodes · At the angle of the mandible
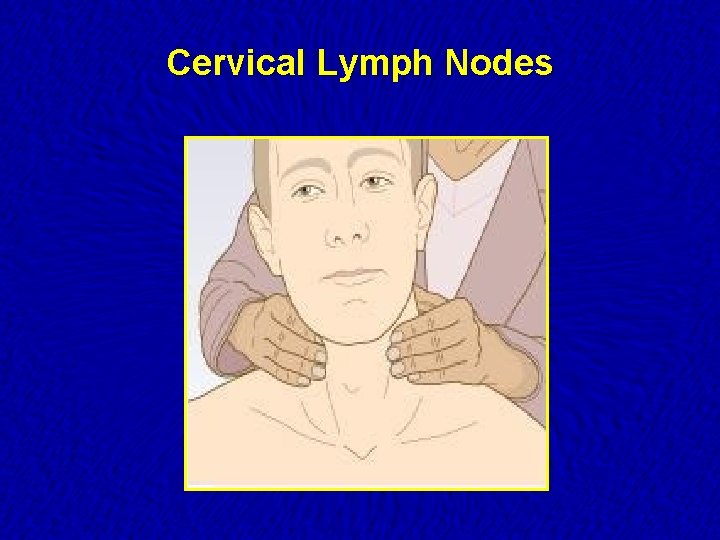
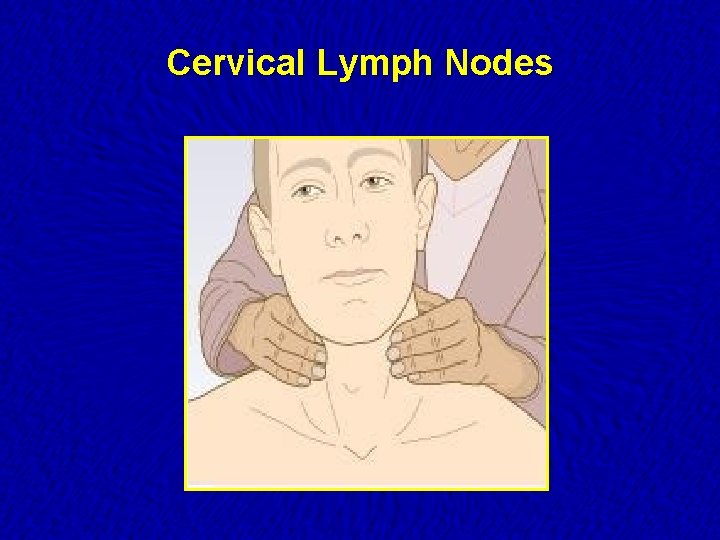
Cervical Lymph Nodes
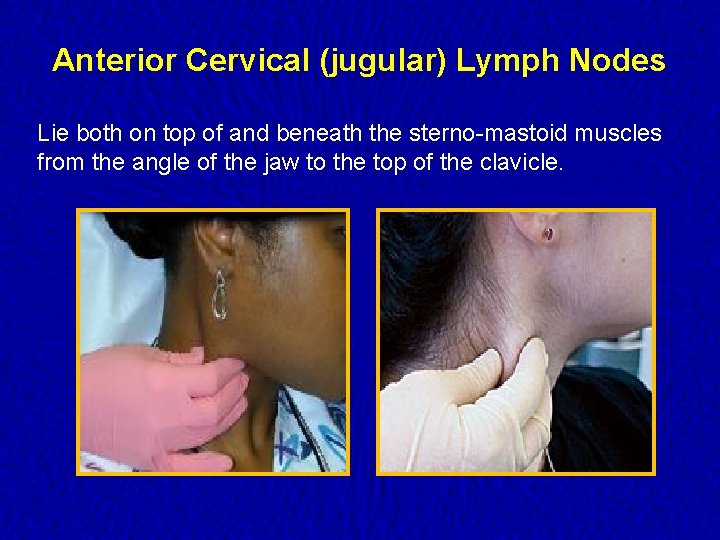
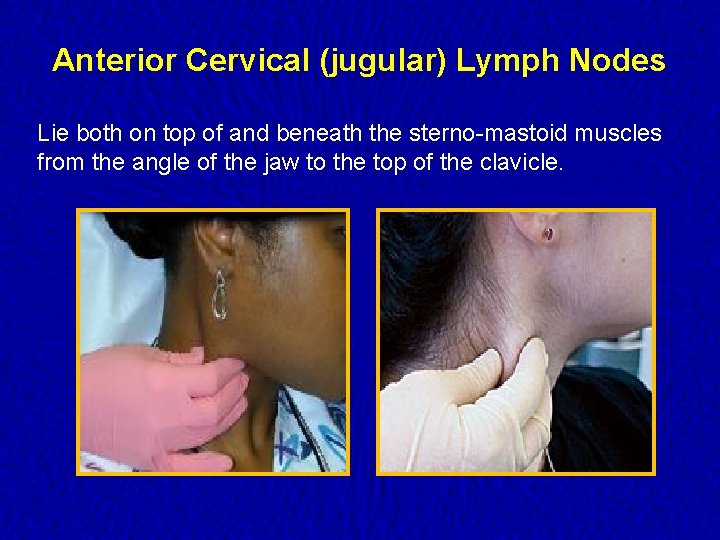
Anterior Cervical (jugular) Lymph Nodes Lie both on top of and beneath the sterno-mastoid muscles from the angle of the jaw to the top of the clavicle.
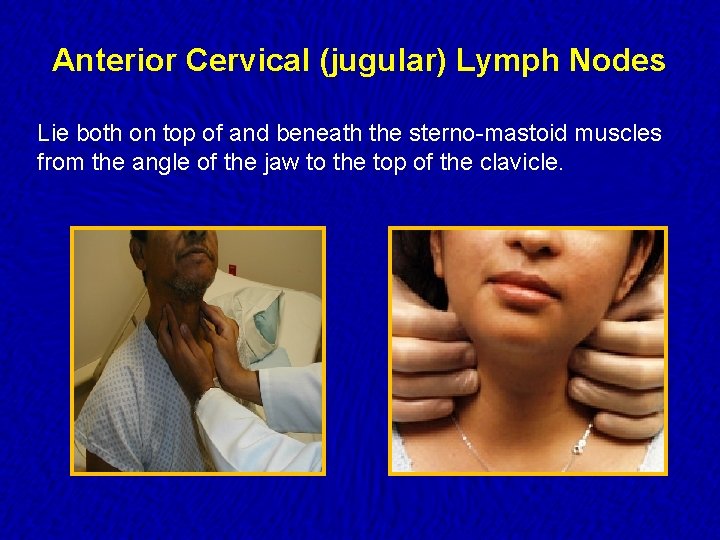
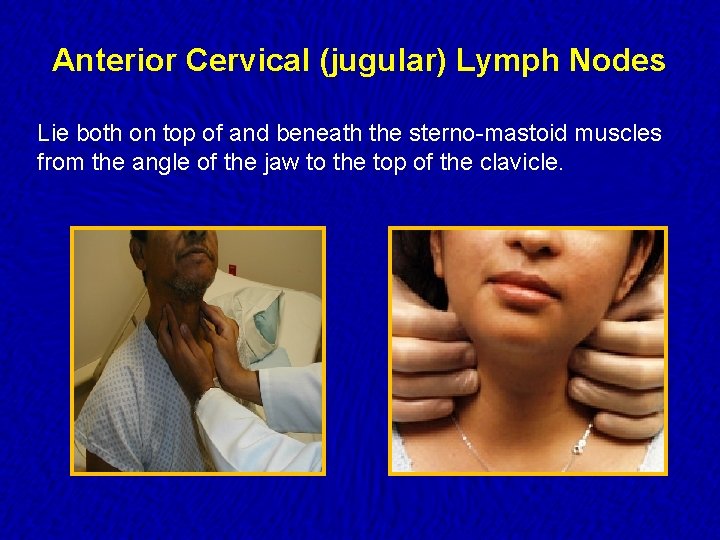
Anterior Cervical (jugular) Lymph Nodes Lie both on top of and beneath the sterno-mastoid muscles from the angle of the jaw to the top of the clavicle.
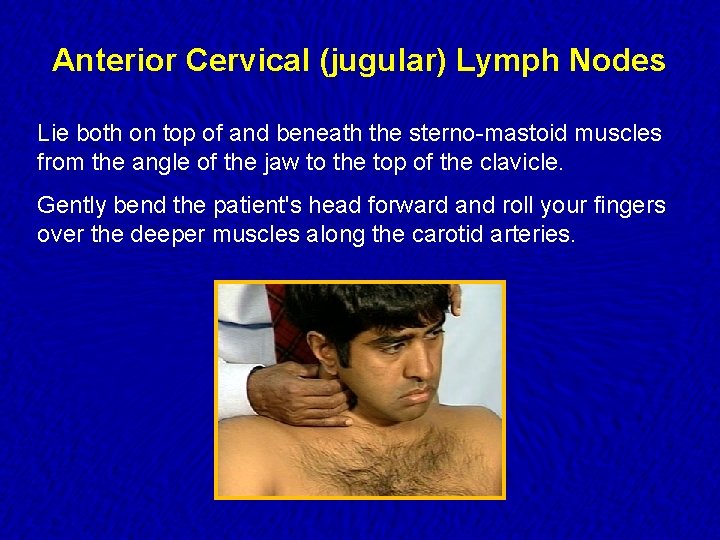
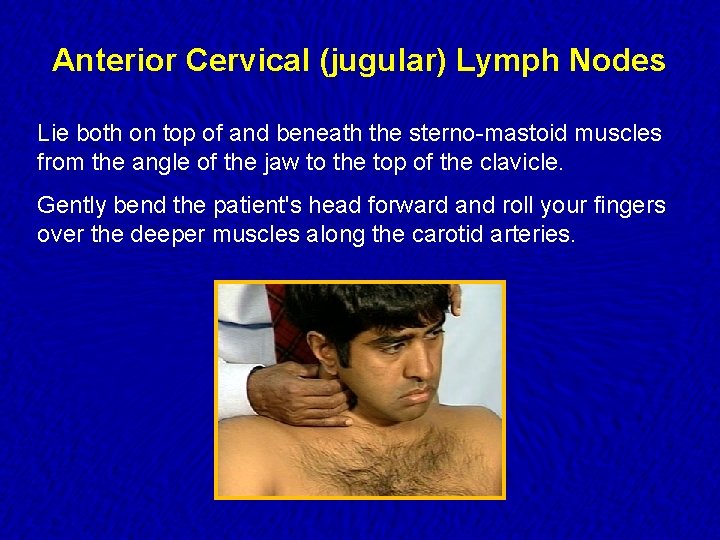
Anterior Cervical (jugular) Lymph Nodes Lie both on top of and beneath the sterno-mastoid muscles from the angle of the jaw to the top of the clavicle. Gently bend the patient's head forward and roll your fingers over the deeper muscles along the carotid arteries.
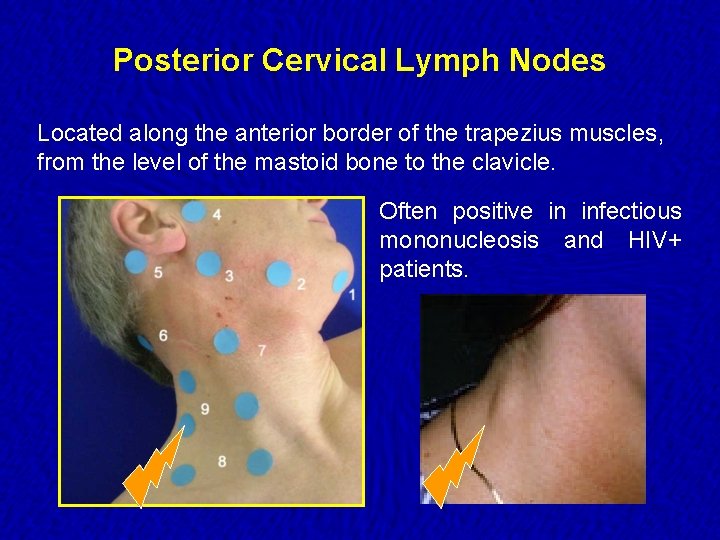
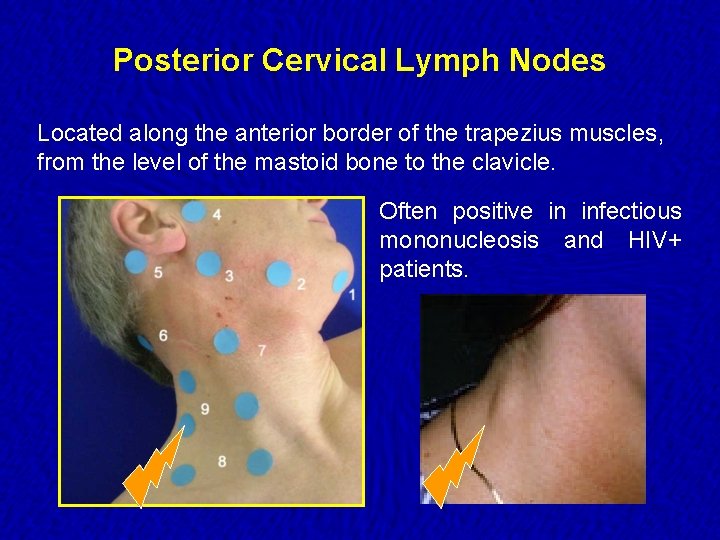
Posterior Cervical Lymph Nodes Located along the anterior border of the trapezius muscles, from the level of the mastoid bone to the clavicle. Often positive in infectious mononucleosis and HIV+ patients.
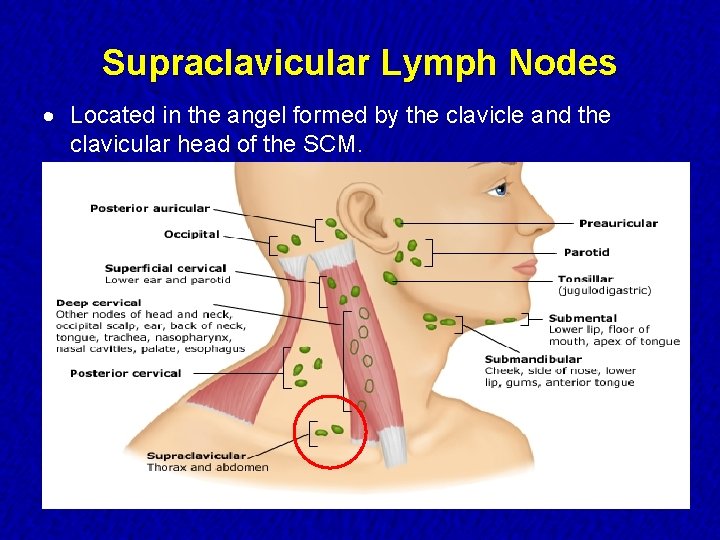
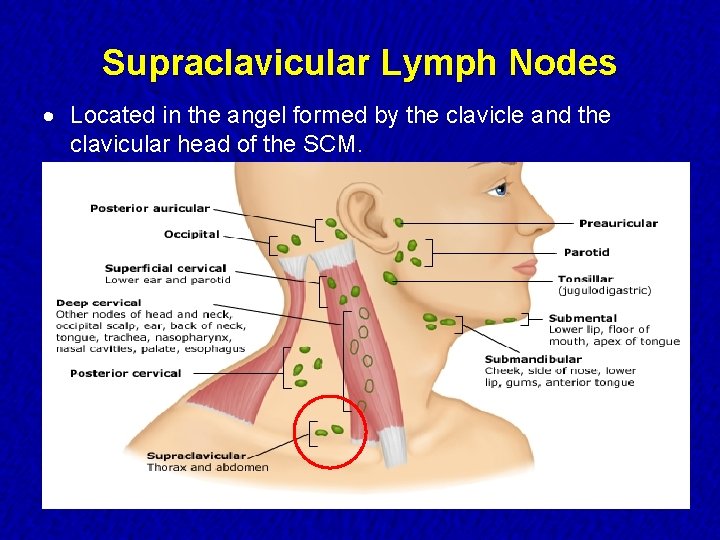
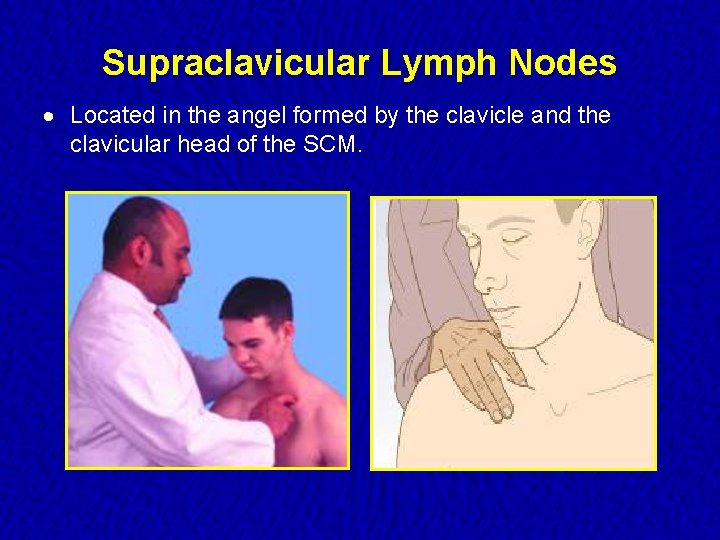
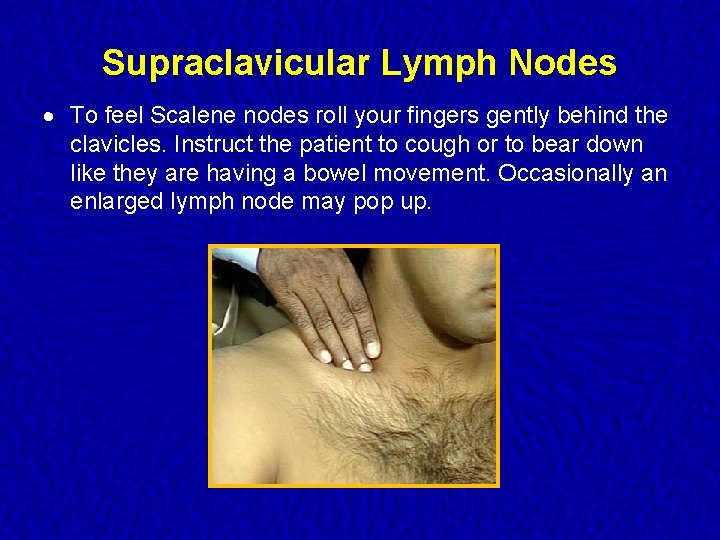
Supraclavicular Lymph Nodes · Located in the angel formed by the clavicle and the clavicular head of the SCM.
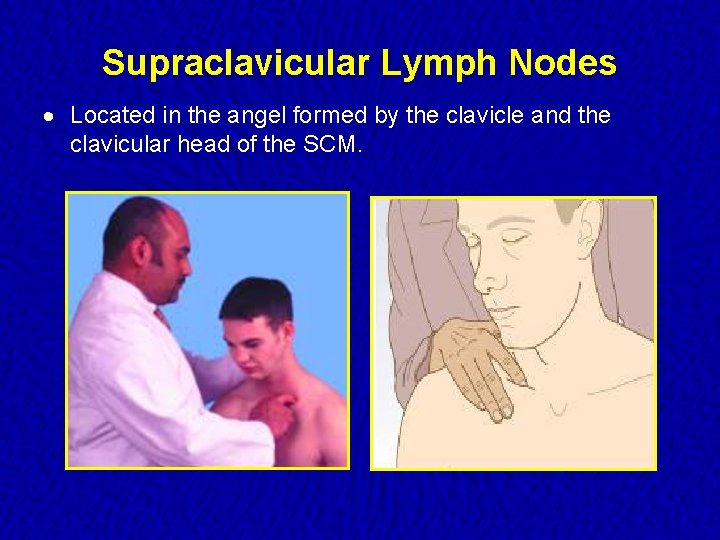
Supraclavicular Lymph Nodes · Located in the angel formed by the clavicle and the clavicular head of the SCM.
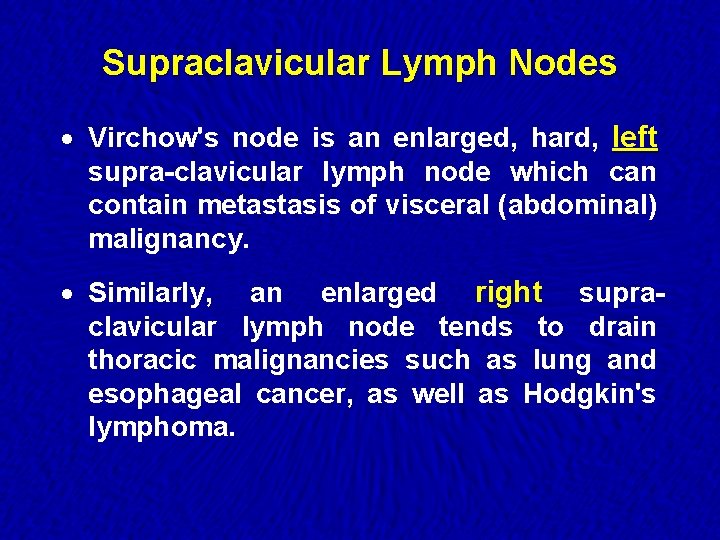
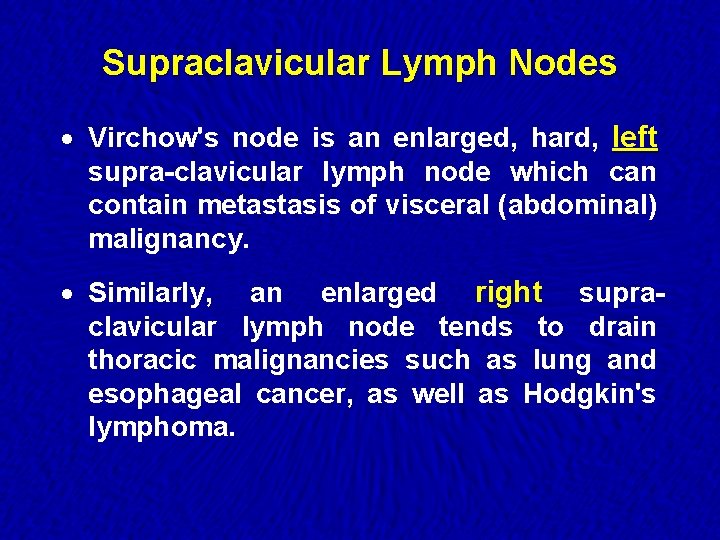
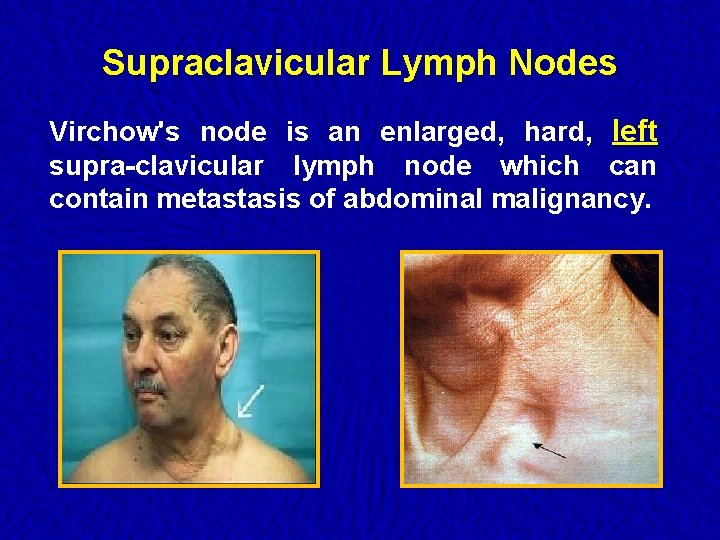
Supraclavicular Lymph Nodes · Virchow's node is an enlarged, hard, left supra-clavicular lymph node which can contain metastasis of visceral (abdominal) malignancy. · Similarly, an enlarged right supraclavicular lymph node tends to drain thoracic malignancies such as lung and esophageal cancer, as well as Hodgkin's lymphoma.
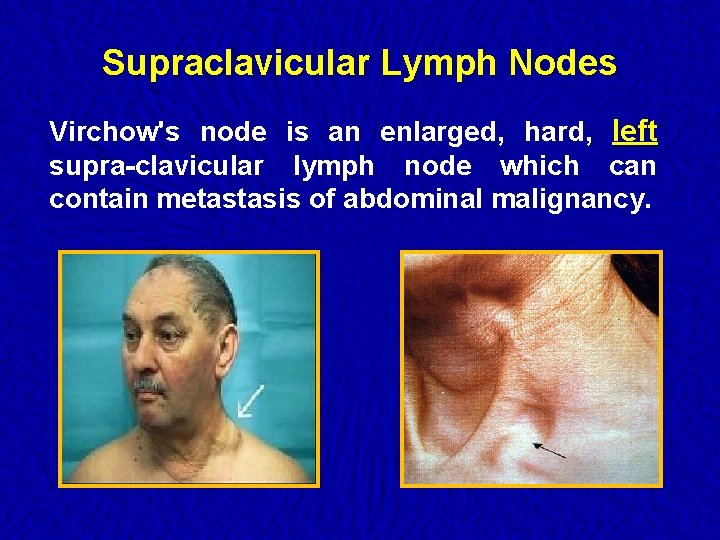
Supraclavicular Lymph Nodes Virchow's node is an enlarged, hard, left supra-clavicular lymph node which can contain metastasis of abdominal malignancy.
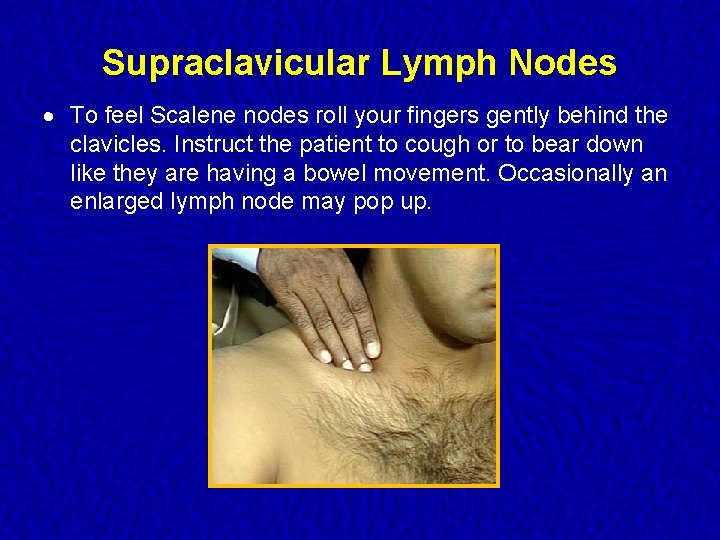
Supraclavicular Lymph Nodes · To feel Scalene nodes roll your fingers gently behind the clavicles. Instruct the patient to cough or to bear down like they are having a bowel movement. Occasionally an enlarged lymph node may pop up.
Head and Neck Lymphadenopathy · Infection is the most common cause. · Infected lymph nodes: Firm, tender, enlarged and warm. Inflammation can spread to the overlying skin, causing redness. · Supra-clavicular nodes are the most likely to be malignant and should always be investigated, even in children. · Malignant lymph nodes: Firm, non-tender, fixed and increase in size over time.
Examination of Lymph Nodes · Small, mobile, discrete, nontender nodes are common and termed shotty · Nodes are abnormal if greater than 1 cm and/or present greater than one month · Hard nodes suggest malignancy · Tender nodes suggest infection · Rubbery nodes suggest lymphoma
Age Related Variations Infants and Children · Commonly find small, discreet, firm, movable nodes in occipital, postauricular, cervical and inguinal chains. . . ü should not be warm or tender ü shape usually ovoid or globular ü often · May referred to as “shotty nodes” find enlarged postauricular and occipital nodes in children < 2 years old
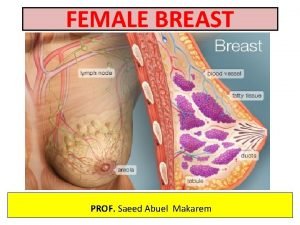
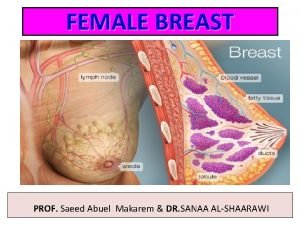
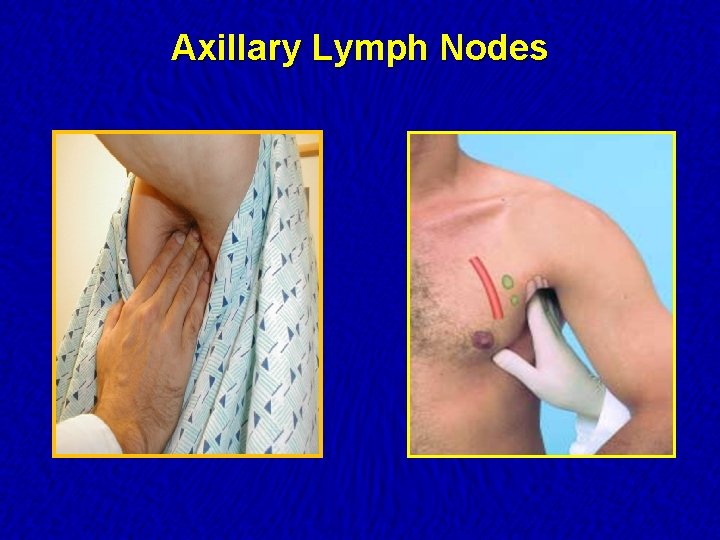
Axillary Lymph Nodes
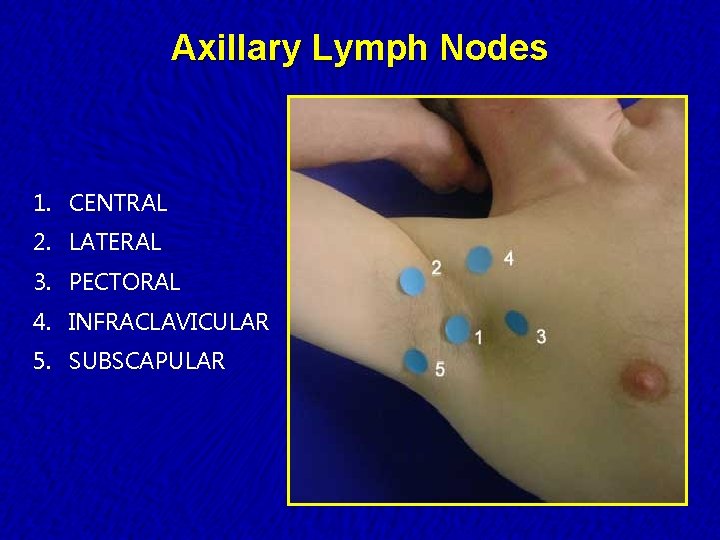
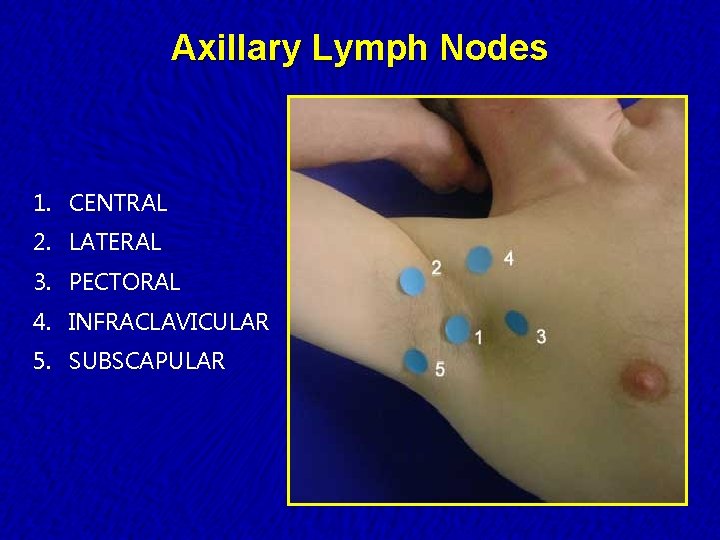
Axillary Lymph Nodes 1. CENTRAL 2. LATERAL 3. PECTORAL 4. INFRACLAVICULAR 5. SUBSCAPULAR
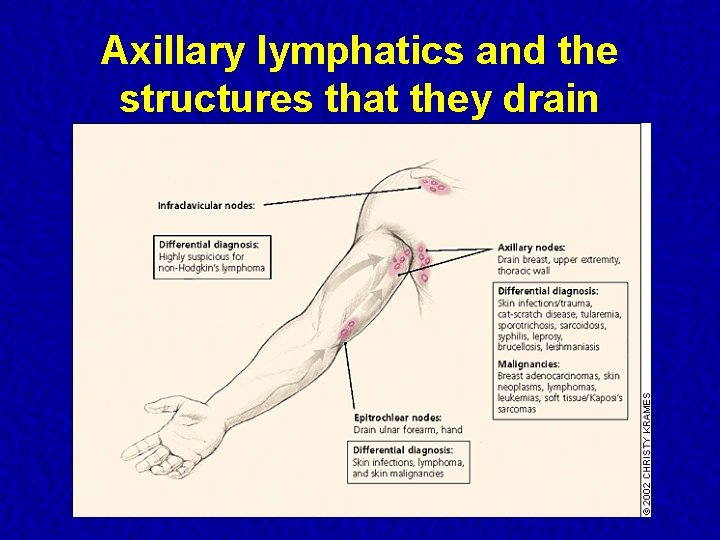
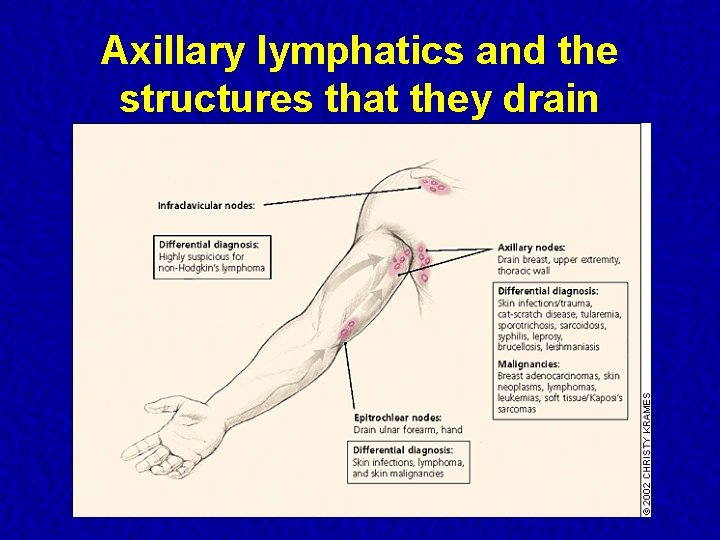
Axillary lymphatics and the structures that they drain
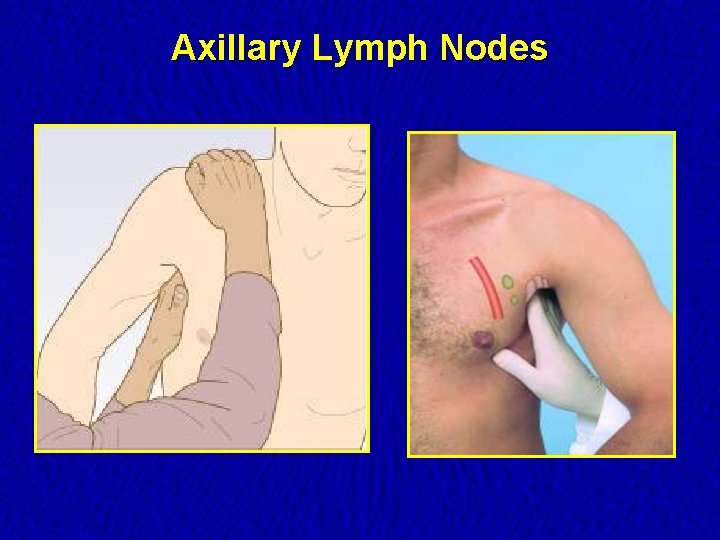
Axillary Lymph Nodes
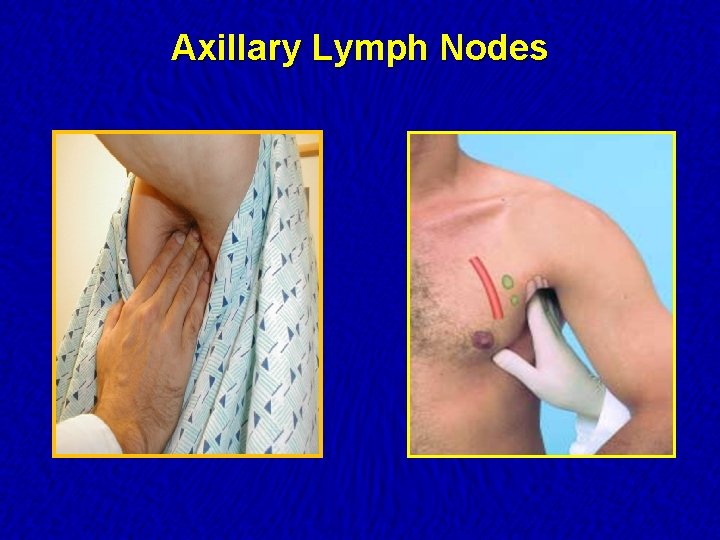
Axillary Lymph Nodes
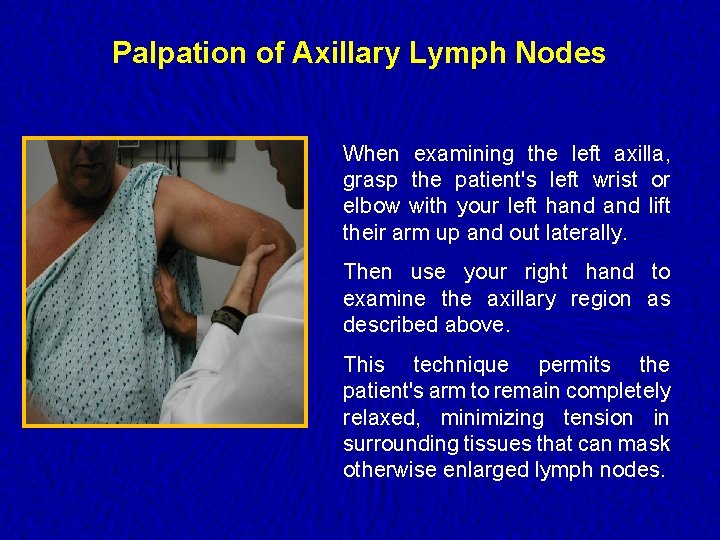
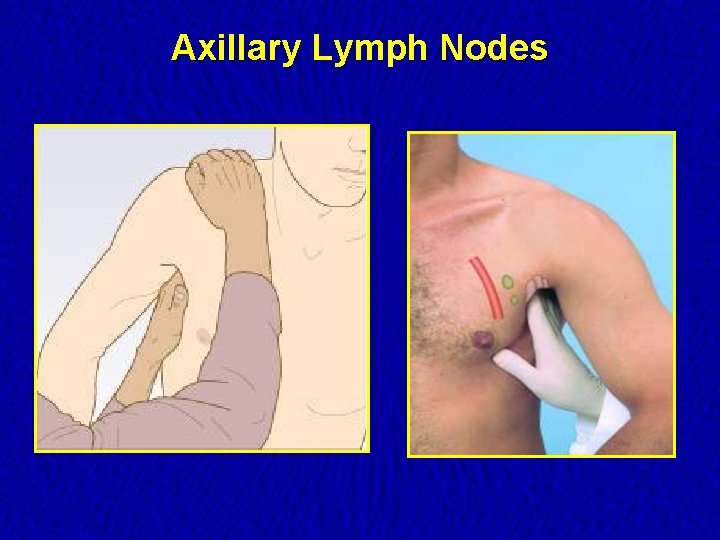
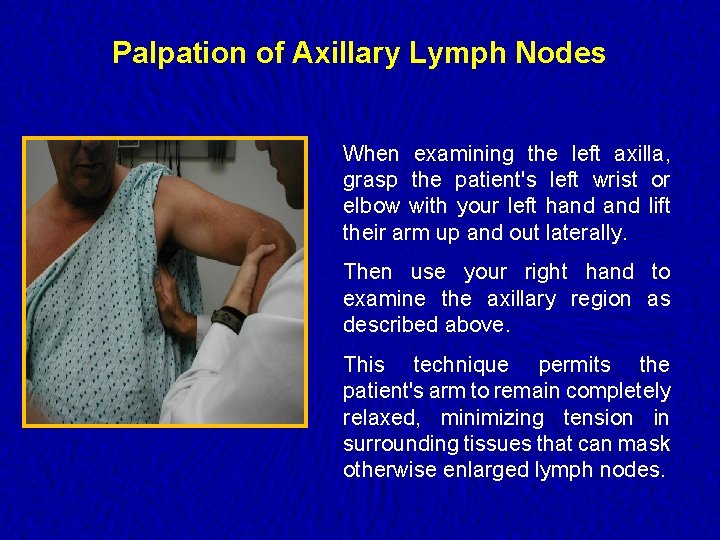
Palpation of Axillary Lymph Nodes When examining the left axilla, grasp the patient's left wrist or elbow with your left hand lift their arm up and out laterally. Then use your right hand to examine the axillary region as described above. This technique permits the patient's arm to remain completely relaxed, minimizing tension in surrounding tissues that can mask otherwise enlarged lymph nodes.
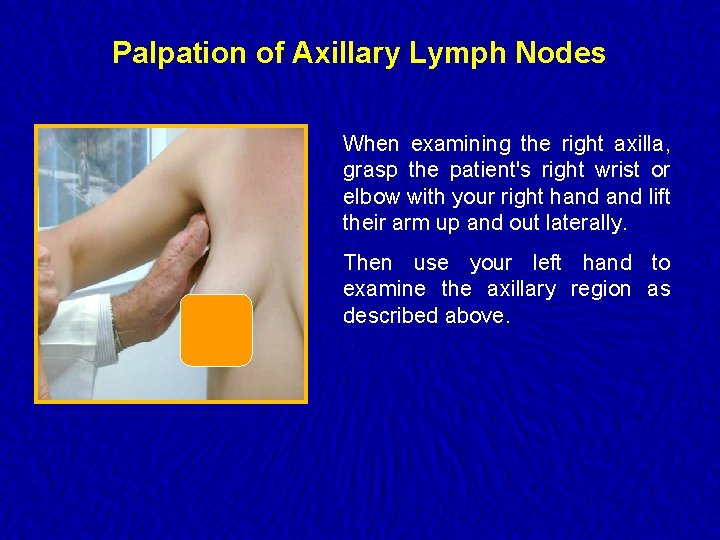
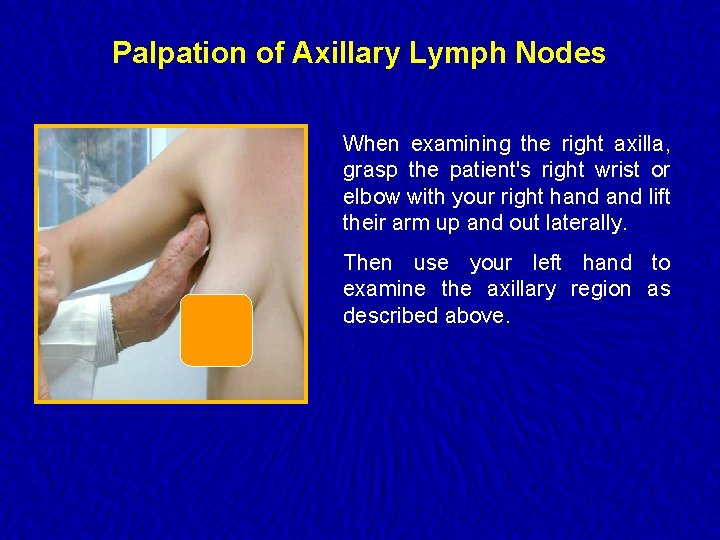
Palpation of Axillary Lymph Nodes When examining the right axilla, grasp the patient's right wrist or elbow with your right hand lift their arm up and out laterally. Then use your left hand to examine the axillary region as described above.
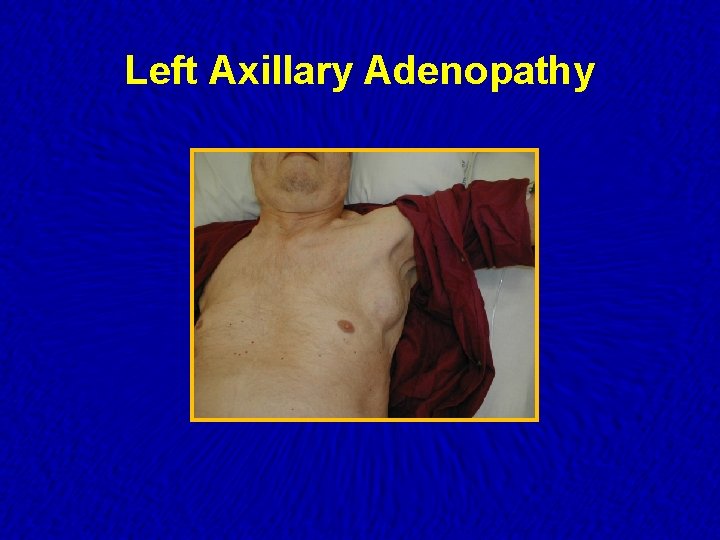
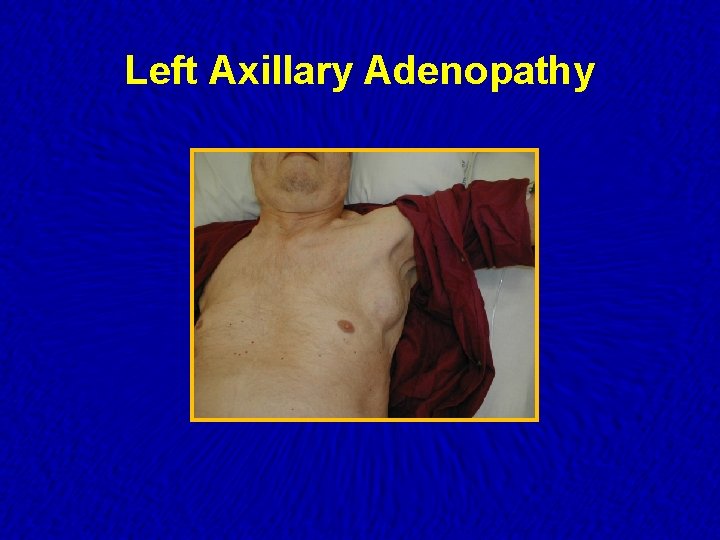
Left Axillary Adenopathy
Axillary Lymphadenopathy · Most of cases are nonspecific or reactive to local injury/infection in etiology. · Persistent lymphadenopathy is less commonly found in the axillary nodes than in the inguinal chain. · Breast adenocarcinoma often metastasis initially to the anterior and central axillary nodes, which may be palpable before discovery of the primary tumor.
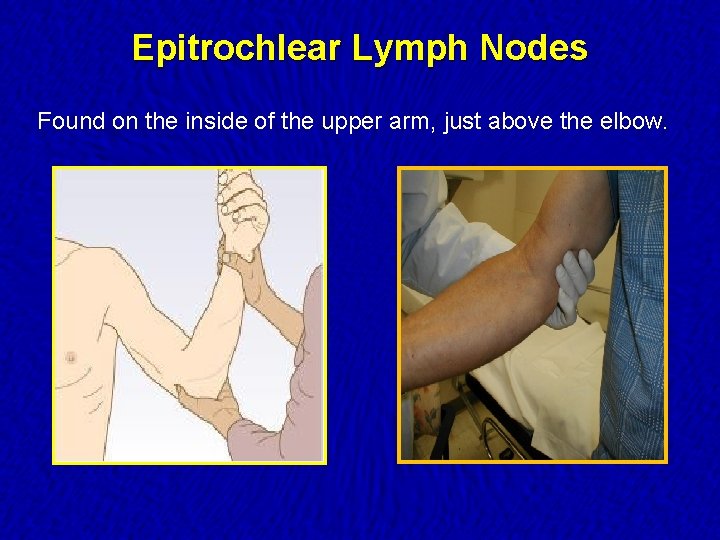
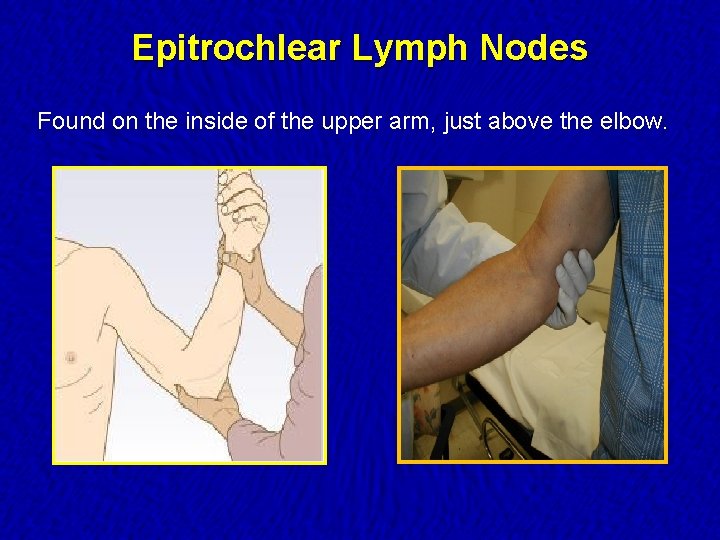
Epitrochlear Lymph Nodes Found on the inside of the upper arm, just above the elbow.
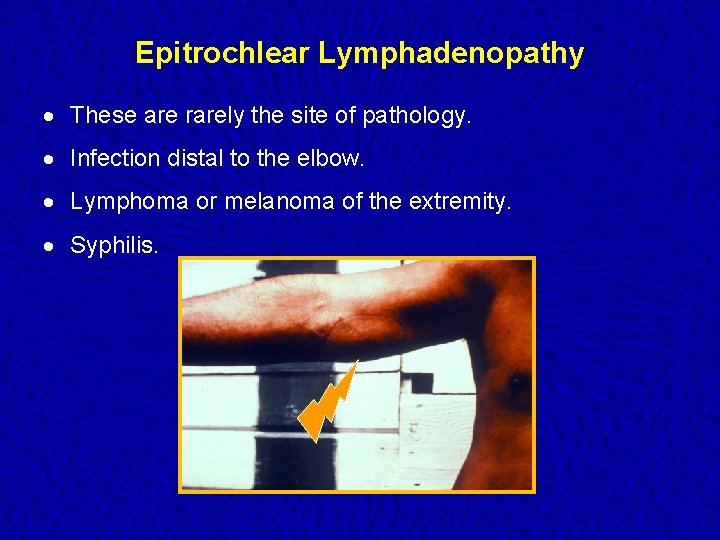
Epitrochlear Lymphadenopathy · These are rarely the site of pathology. · Infection distal to the elbow. · Lymphoma or melanoma of the extremity. · Syphilis.
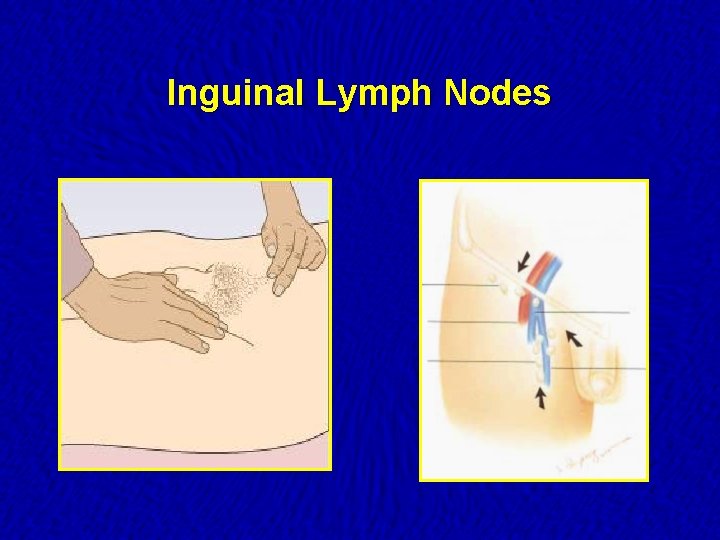
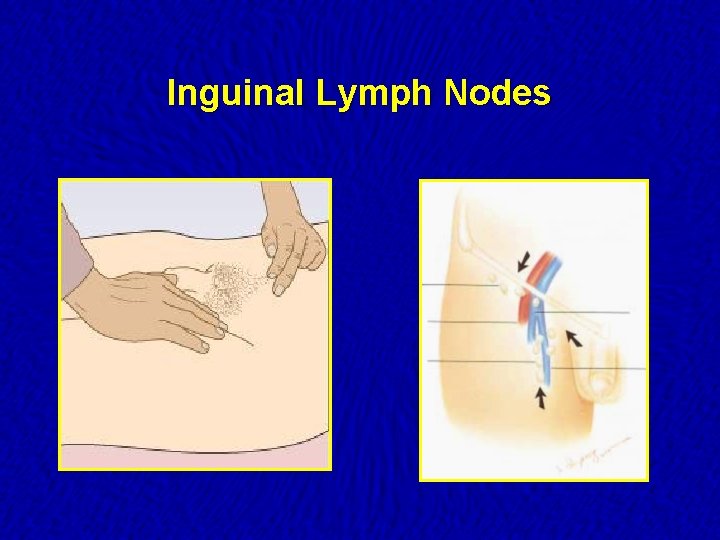
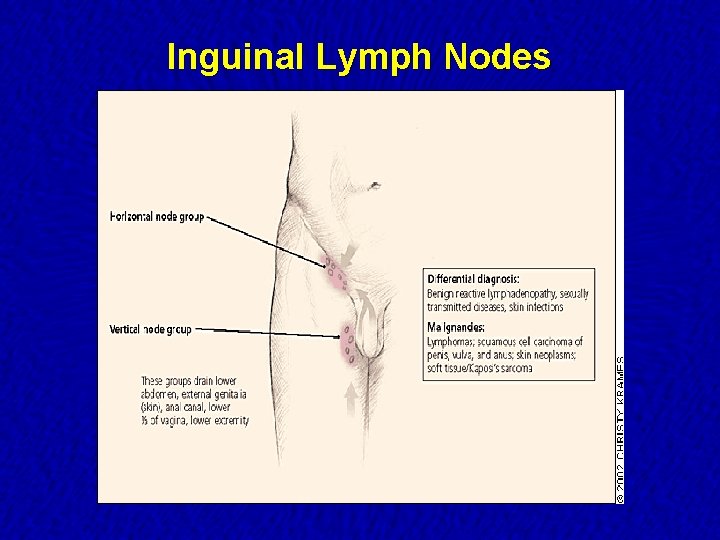
Inguinal Lymph Nodes
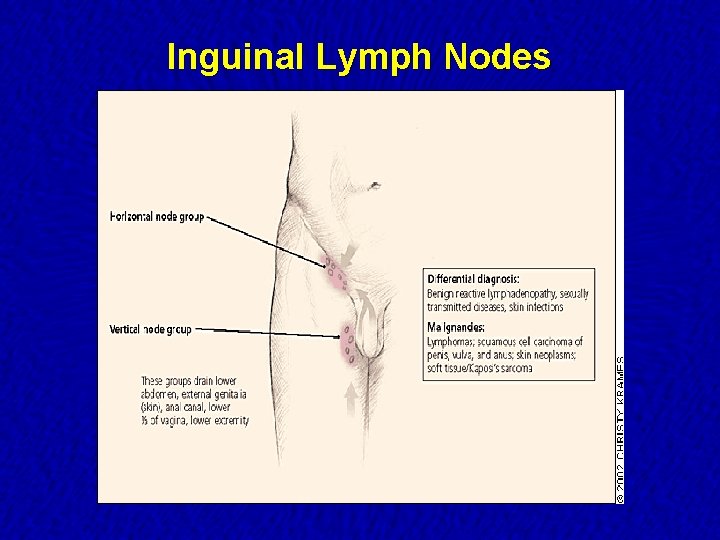
Inguinal Lymph Nodes
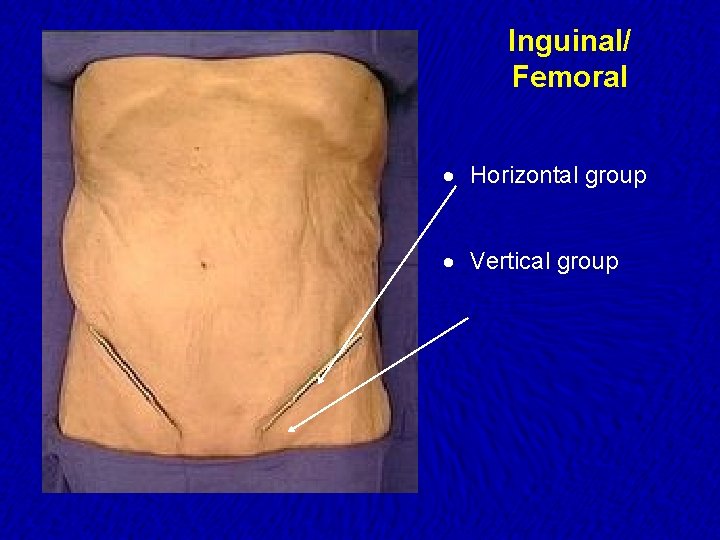
Inguinal/ Femoral · Horizontal group · Vertical group
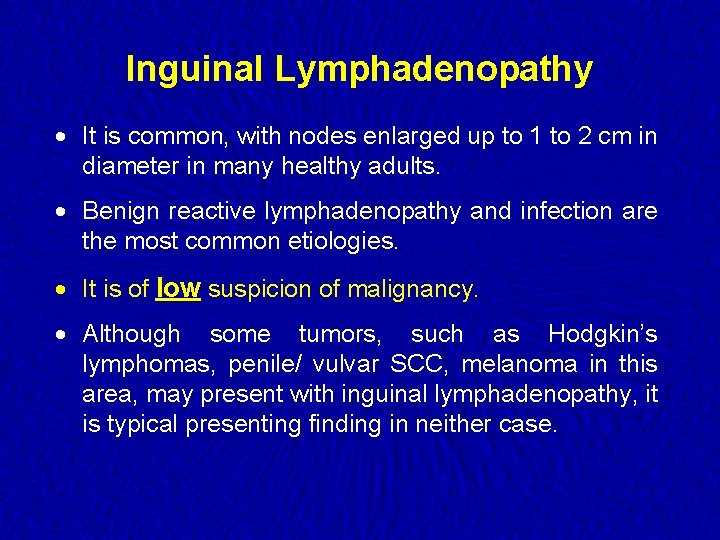
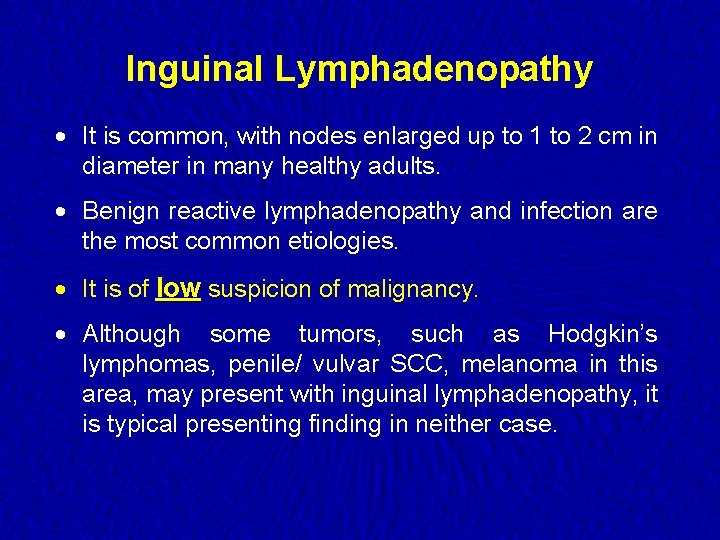
Inguinal Lymphadenopathy · It is common, with nodes enlarged up to 1 to 2 cm in diameter in many healthy adults. · Benign reactive lymphadenopathy and infection are the most common etiologies. · It is of low suspicion of malignancy. · Although some tumors, such as Hodgkin’s lymphomas, penile/ vulvar SCC, melanoma in this area, may present with inguinal lymphadenopathy, it is typical presenting finding in neither case.
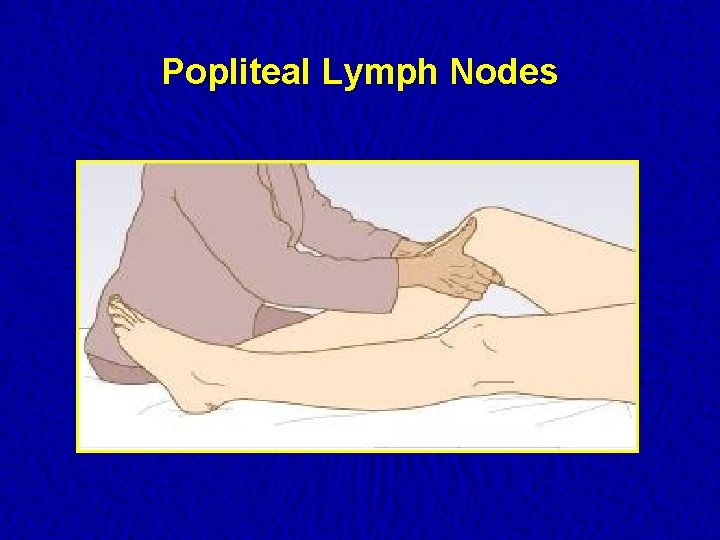
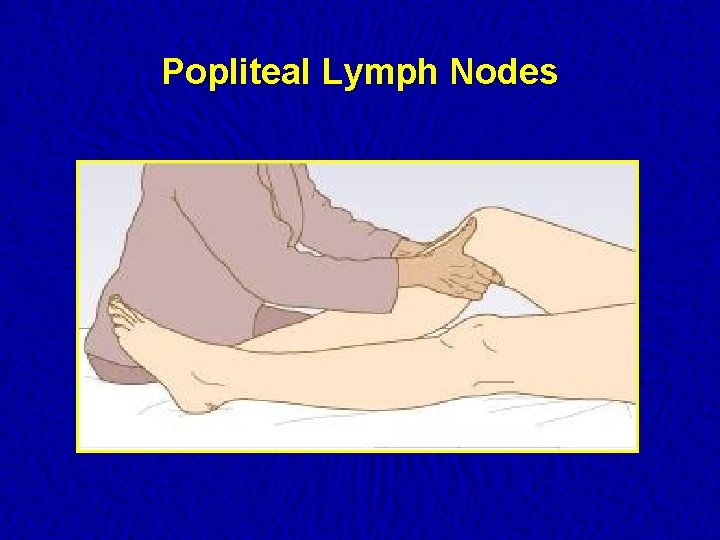
Popliteal Lymph Nodes
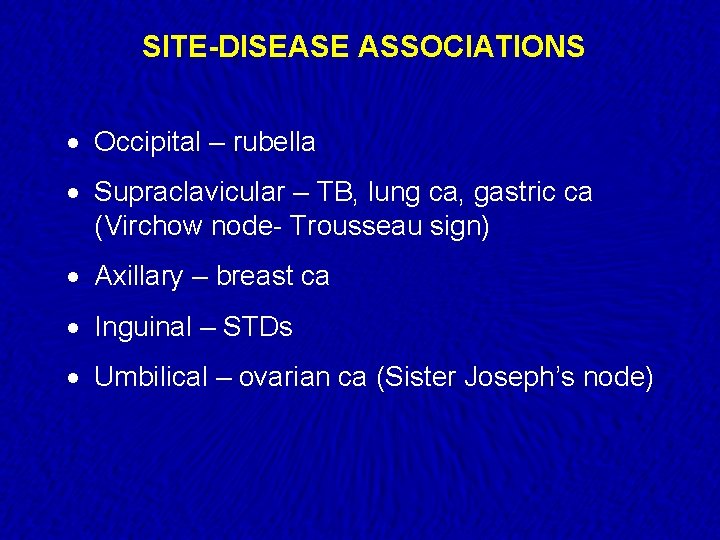
SITE-DISEASE ASSOCIATIONS · Occipital – rubella · Supraclavicular – TB, lung ca, gastric ca (Virchow node- Trousseau sign) · Axillary – breast ca · Inguinal – STDs · Umbilical – ovarian ca (Sister Joseph’s node)
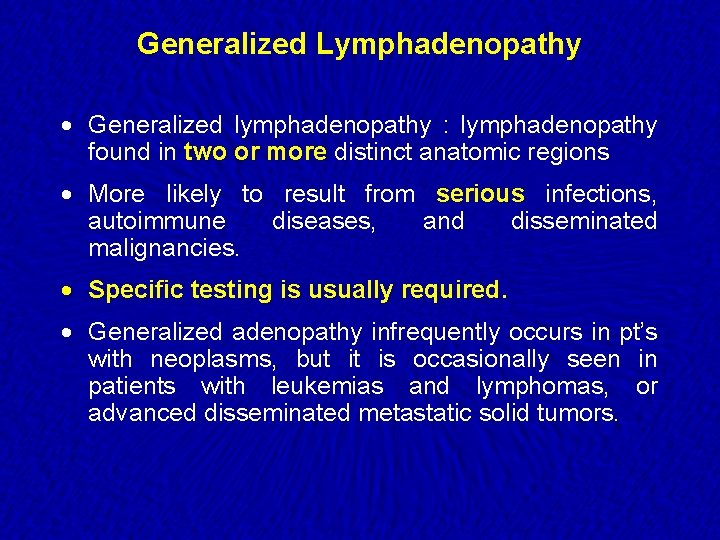
Generalized Lymphadenopathy · Generalized lymphadenopathy : lymphadenopathy found in two or more distinct anatomic regions · More likely to result from serious infections, autoimmune diseases, and disseminated malignancies. · Specific testing is usually required. · Generalized adenopathy infrequently occurs in pt’s with neoplasms, but it is occasionally seen in patients with leukemias and lymphomas, or advanced disseminated metastatic solid tumors.
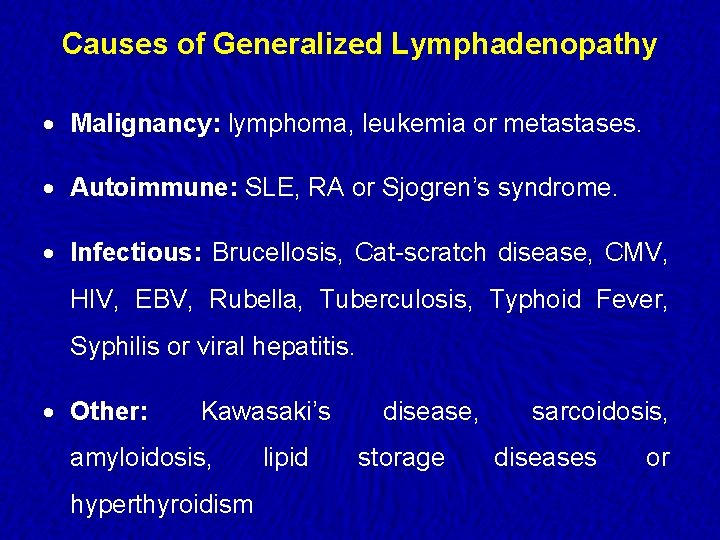
Causes of Generalized Lymphadenopathy · Malignancy: lymphoma, leukemia or metastases. · Autoimmune: SLE, RA or Sjogren’s syndrome. · Infectious: Brucellosis, Cat-scratch disease, CMV, HIV, EBV, Rubella, Tuberculosis, Typhoid Fever, Syphilis or viral hepatitis. · Other: Kawasaki’s amyloidosis, hyperthyroidism lipid disease, storage sarcoidosis, diseases or
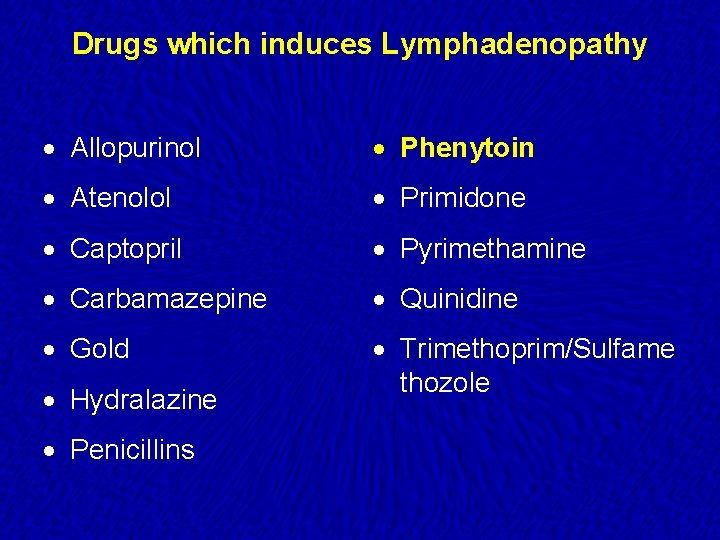
Drugs which induces Lymphadenopathy · Allopurinol · Phenytoin · Atenolol · Primidone · Captopril · Pyrimethamine · Carbamazepine · Quinidine · Gold · Trimethoprim/Sulfame thozole · Hydralazine · Penicillins
Tuberculosis lymphadenopathy · Cervical nodes most commonly involved · Usual course of lymph node disease is as follows: Firm, discrete nodes fluctuant nodes matted together skin breakdown, abscesses, chronic sinuses healing and scarring
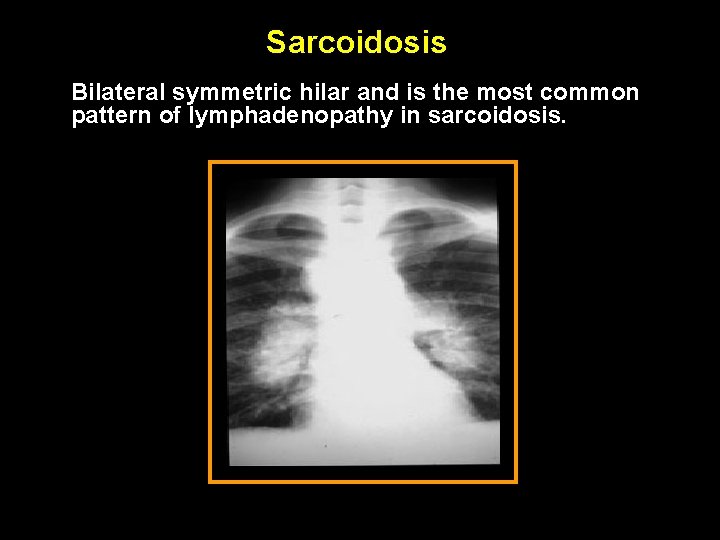
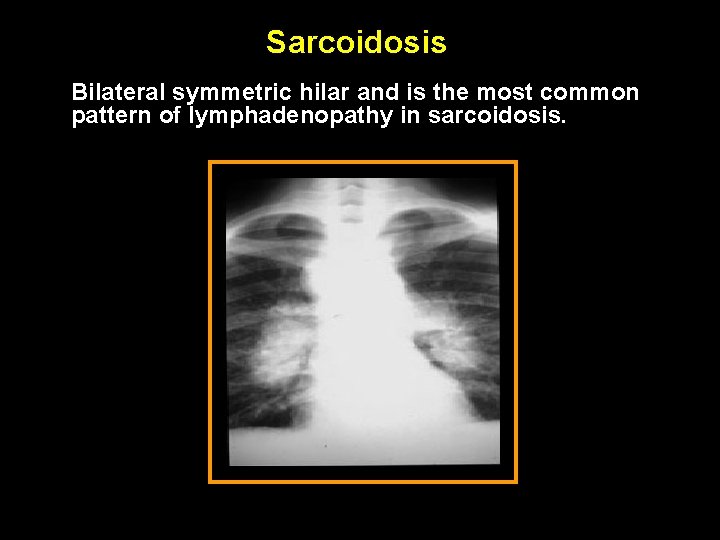
Sarcoidosis Bilateral symmetric hilar and is the most common pattern of lymphadenopathy in sarcoidosis.
When to worry? · Age · Characteristics of the node · Location of the node · Clinical setting associated with lymphadenopathy
Age · Children/young adults – more likely to respond to minor stimuli with lymphoid hyperplasia · Lymph nodes in patients less than the age of 30 are clinically benign in 80% of cases whereas in patients over the age of 50 only 40% are benign
Characteristics of the node · Consistency – Hard/Firm vs Soft/Shotty. · Mobile vs Fixed · Tender vs Painless · Clearly demarcated · Duration and Rate of Growth: Nodes lasting less than 2 weeks or greater than one year with no progression of size have a low likelihood of being neoplastic.
Location of the node · Supra-clavicular lymphadenopathy o Highest risk of malignancy o Right sided node – cancer in mediastinum, lungs, esophagus o Left sided node (Virchow’s) – testes, ovaries, kidneys, pancreas, stomach, gallbladder or prostate · Cervical nodes: up to 56% of young adults have adenopathy on clinical exam · Inguinal adenopathy: common and often benign. · Para-umbilical node (Sister Joseph’s): Abdominal or pelvic neoplasm · Epitroclear nodes: Unlikely to be reactive
Lower limbs Edema
Agenda · Definition. · Patho-physiology of edema. · Distribution of the excess fluid. · Classification & causes of edema. · How to examine for subcutaneous edema? · How to investigate? · Principles of therapy.
Definition · Physiologically Increase in the volume of the interstitial fluid. · Clinically Tissue swelling due to increase in the volume of the interstitial fluid. · The expansion takes several liters before overt manifestations of edema (i. e. weight gain of several kg).
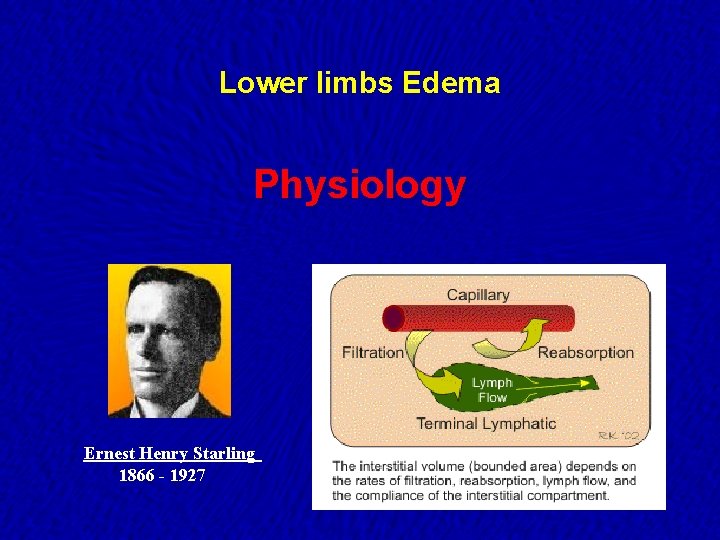
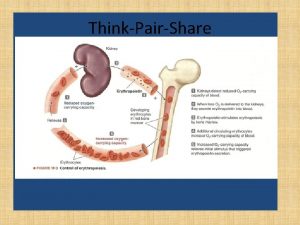
Lower limbs Edema Physiology Ernest Henry Starling 1866 - 1927
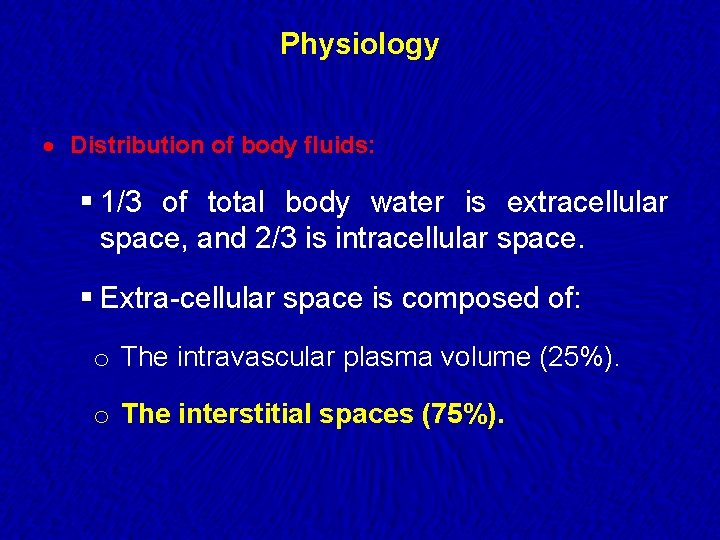
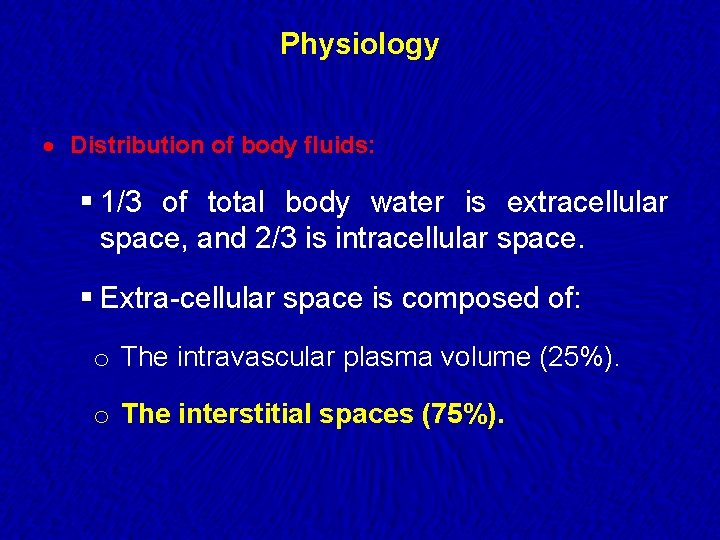
Physiology · Distribution of body fluids: § 1/3 of total body water is extracellular space, and 2/3 is intracellular space. § Extra-cellular space is composed of: o The intravascular plasma volume (25%). o The interstitial spaces (75%).
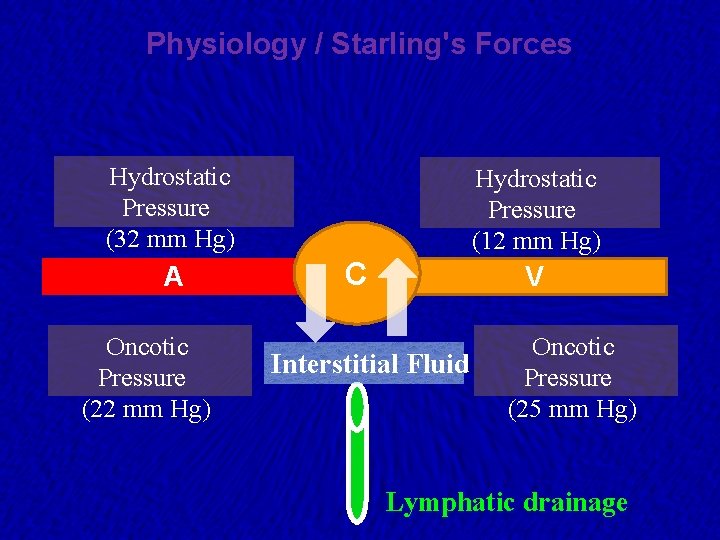
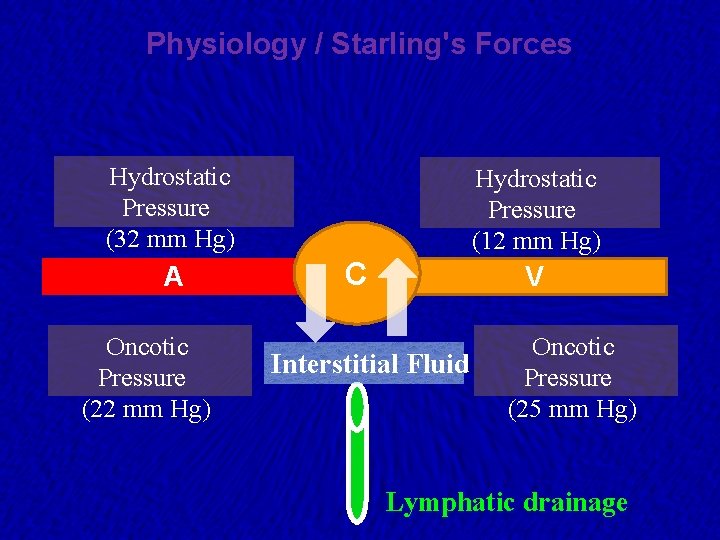
Physiology / Starling's Forces Hydrostatic Pressure (32 mm Hg) A Oncotic Pressure (22 mm Hg) Hydrostatic Pressure (12 mm Hg) C V Interstitial Fluid Oncotic Pressure (25 mm Hg) Lymphatic drainage
Oncotic Pressure · Osmotic pressure created by plasma protein molecules that are impermeable across the capillary membrane.
Patho-physiology · ↑Capillary hydrostatic pressure. · ↓Plasma oncotic pressure (attracting force). ü Dependent on circulating albumin. · ↑ Capillary permeability. · ↓ Lymphatic drainage.
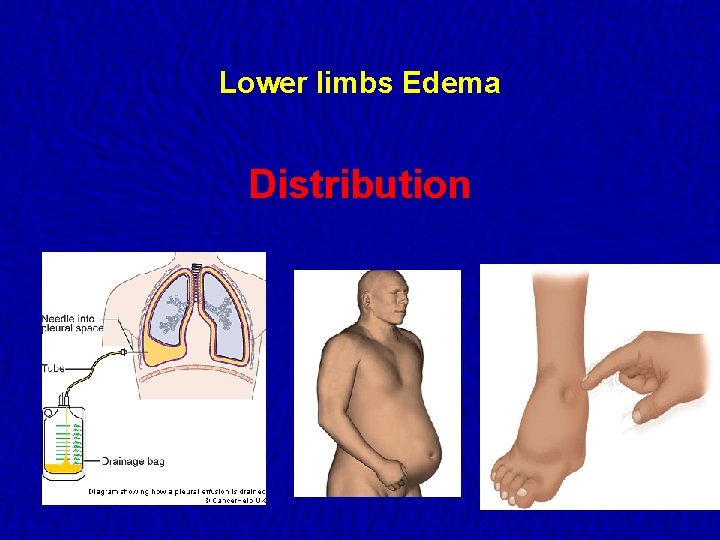
Lower limbs Edema Distribution
Distribution · Sub-cutenous edema: § Edema of lower limb ankles first affected. § Sacrum If patient is confined to bed. § Face puffy eye lids in the early morning. · Effusion of serosal cavities: § Pleural effusion. § Pericardial effusion. § Ascites. · Organ specific: § Brain: Cerebral edema. § Lung: pulmonary edema.
Generalized Edema · Distribution of subcutaneous edema: § When edema is generalized its distribution of generalized edema is determined by gravity: · If the patient is ambulant: edema is found in the ankles. · If the patient lies flat; it may involve the sacrum, face and the hands. · An early feature of generalized edema is tightening of rings in the fingers. § Massive generalized edema is called anasarca.
Lower limbs Edema Classification / Causes
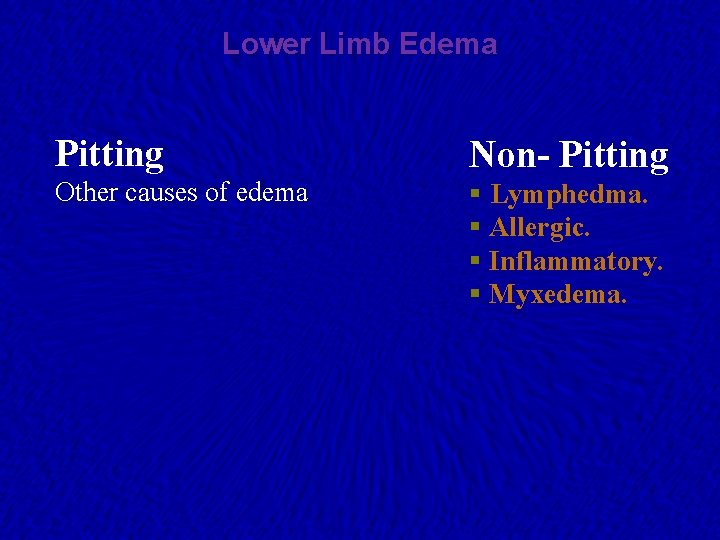
Lower Limb Edema Pitting Non- Pitting Other causes of edema § Lymphedma. § Allergic. § Inflammatory. § Myxedema.
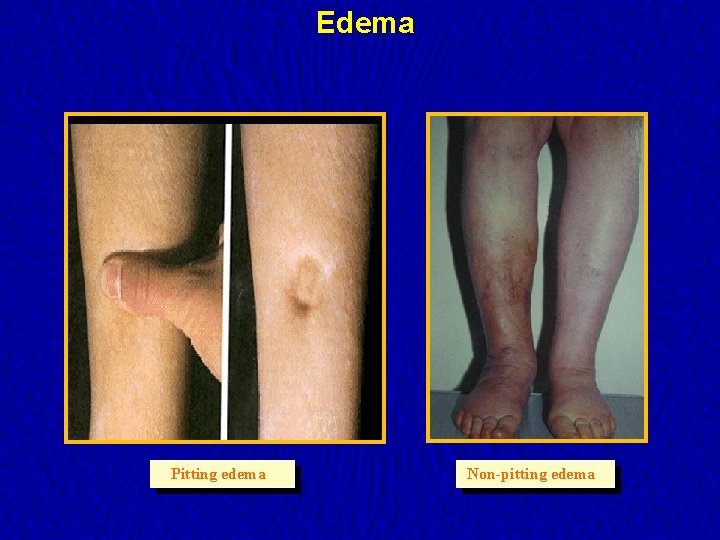
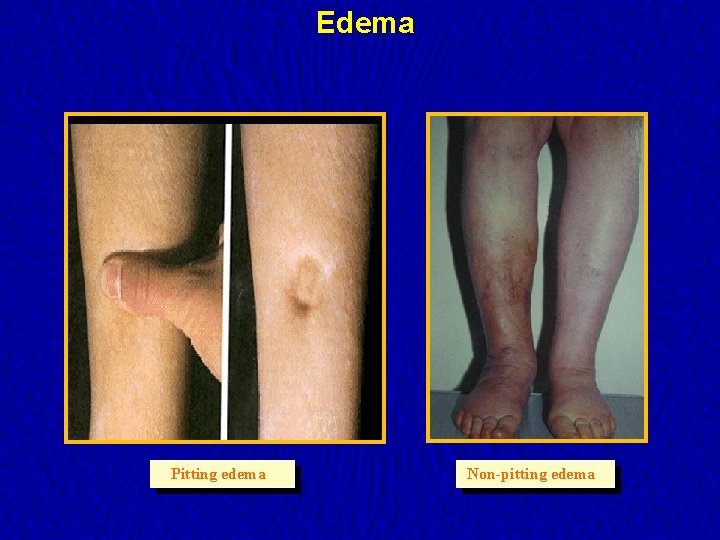
Edema Pitting edema Non-pitting edema
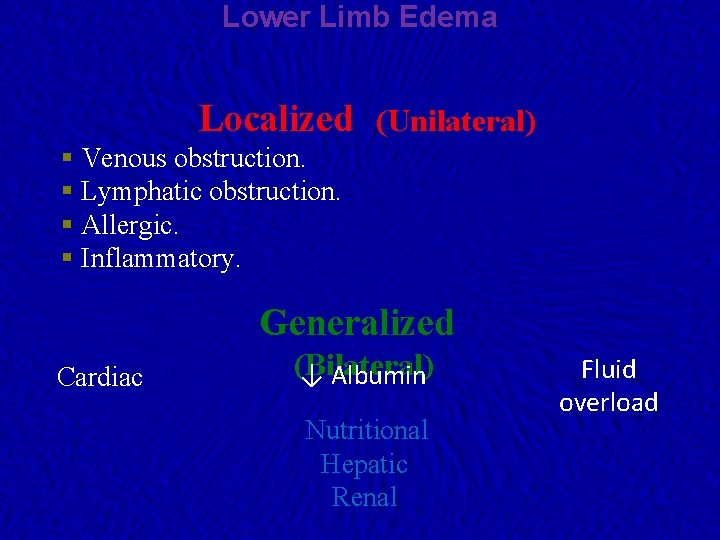
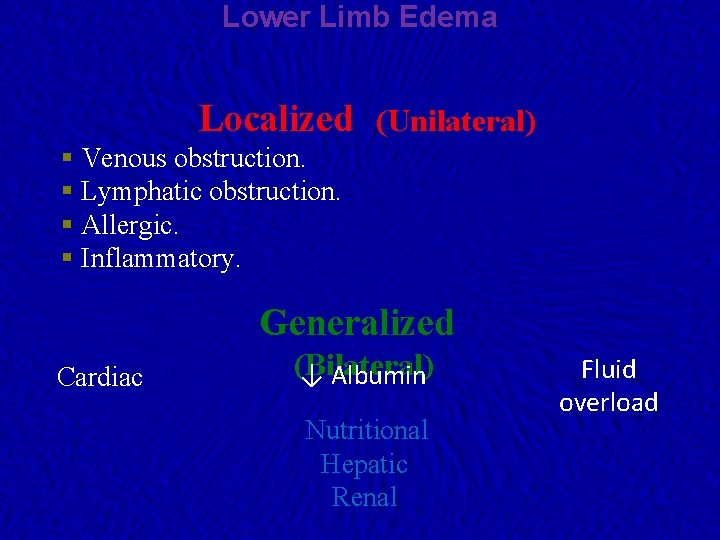
Lower Limb Edema Localized (Unilateral) § Venous obstruction. § Lymphatic obstruction. § Allergic. § Inflammatory. Generalized Cardiac (Bilateral) ↓ Albumin Nutritional Hepatic Renal Fluid overload
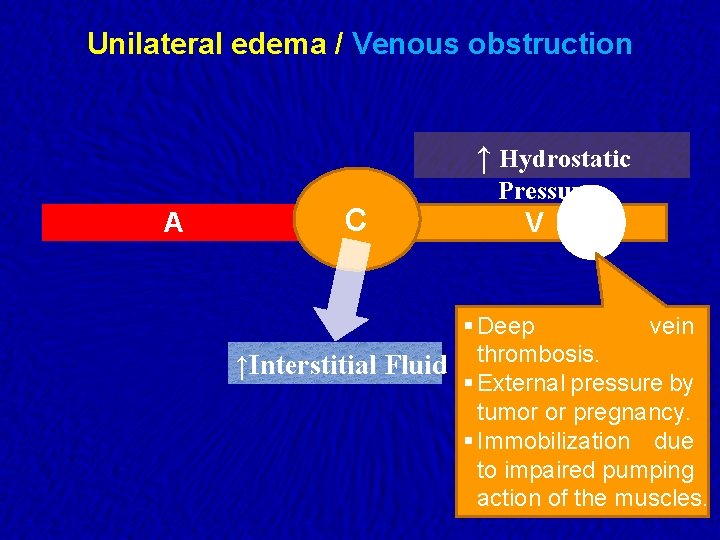
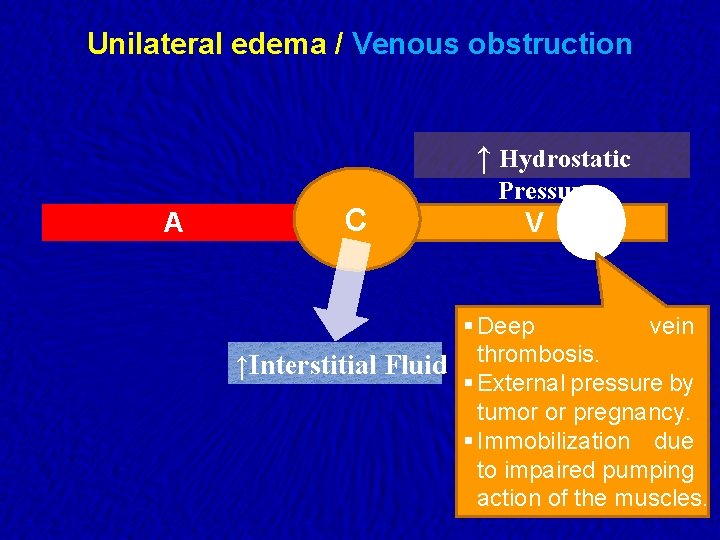
Unilateral edema / Venous obstruction ↑ Hydrostatic A C Pressure V § Deep vein ↑Interstitial Fluid thrombosis. § External pressure by tumor or pregnancy. § Immobilization due to impaired pumping action of the muscles.
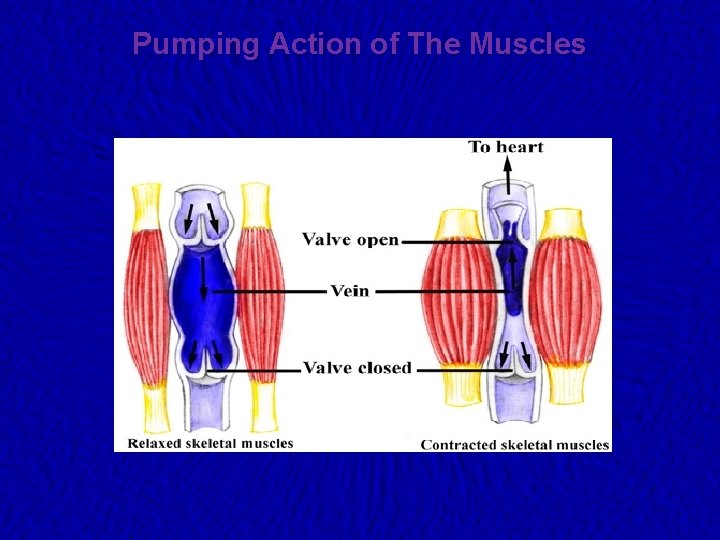
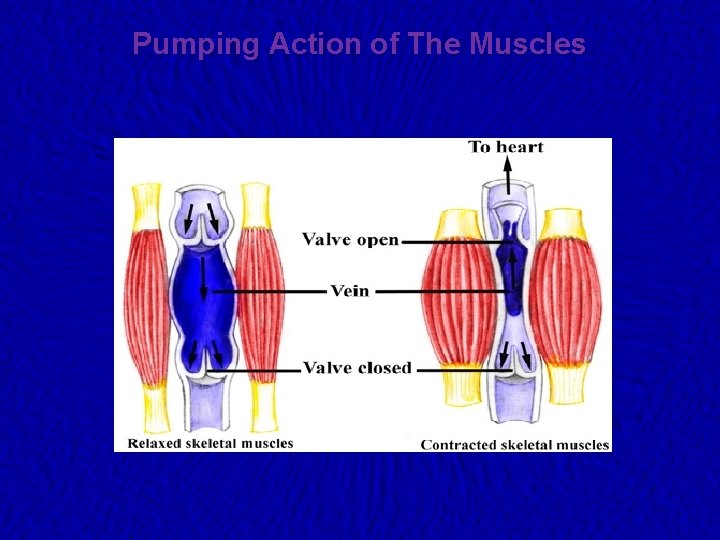
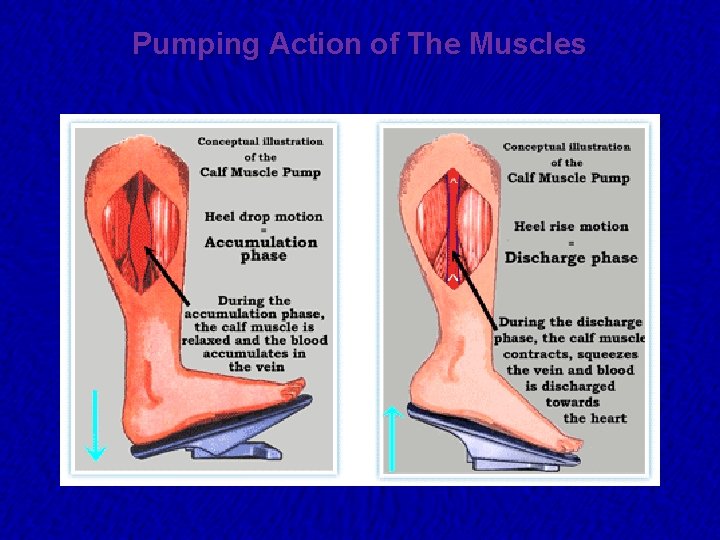
Pumping Action of The Muscles
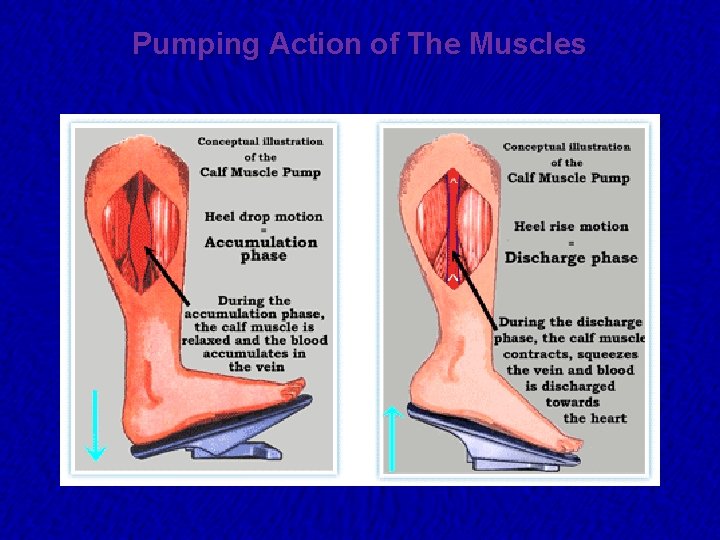
Pumping Action of The Muscles
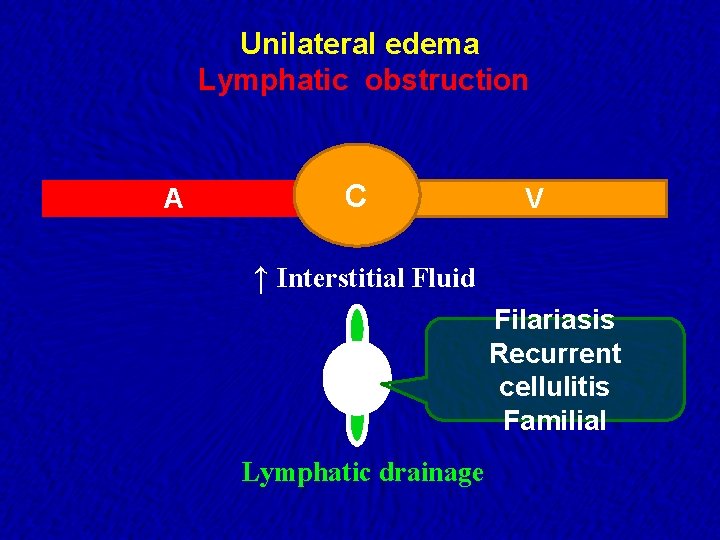
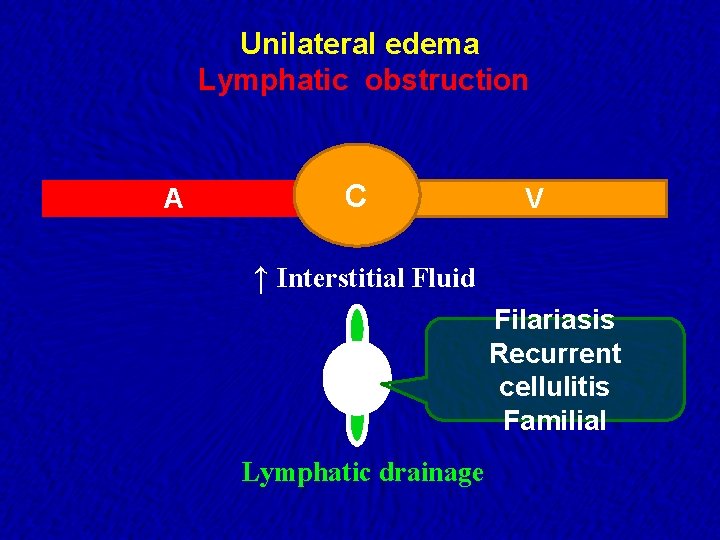
Unilateral edema Lymphatic obstruction A C V ↑ Interstitial Fluid Filariasis Recurrent cellulitis Familial Lymphatic drainage
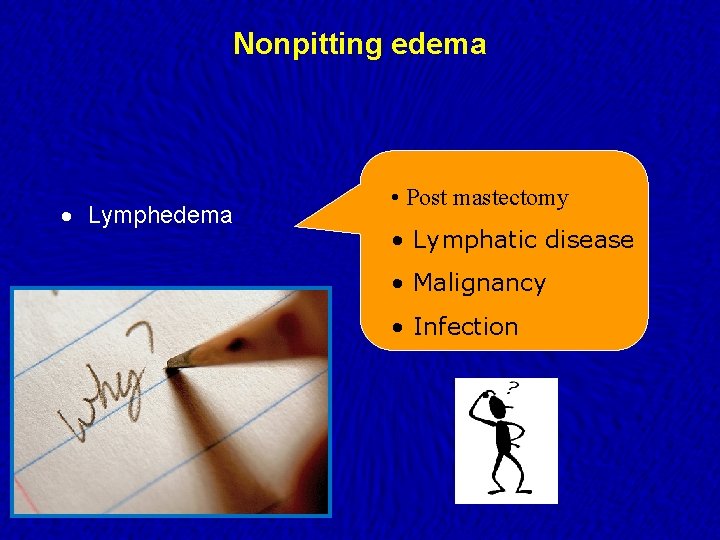
Nonpitting edema · Lymphedema • Post mastectomy • Lymphatic disease • Malignancy • Infection
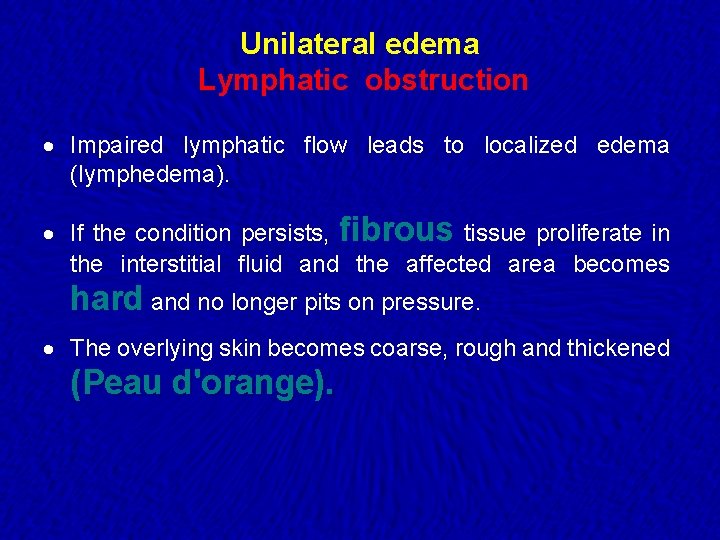
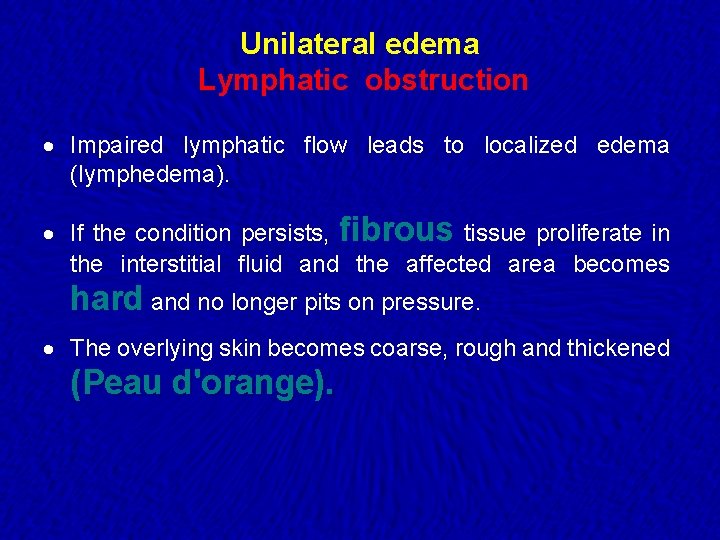
Unilateral edema Lymphatic obstruction · Impaired lymphatic flow leads to localized edema (lymphedema). · If the condition persists, fibrous tissue proliferate in the interstitial fluid and the affected area becomes hard and no longer pits on pressure. · The overlying skin becomes coarse, rough and thickened (Peau d'orange).

Lymphedema
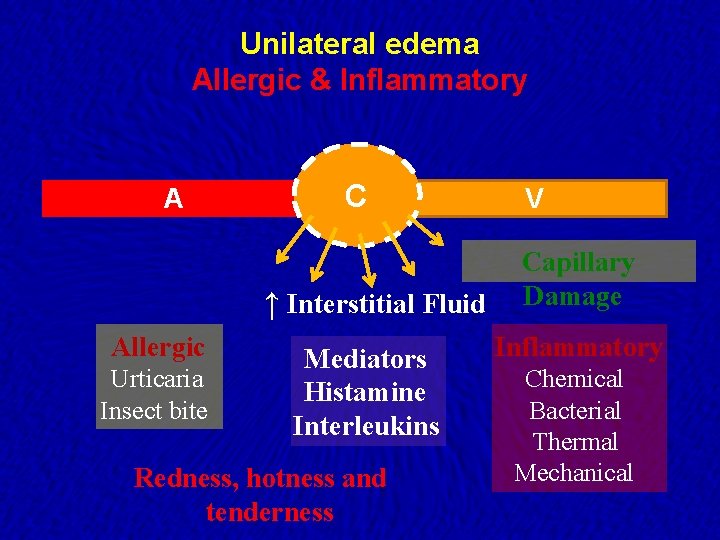
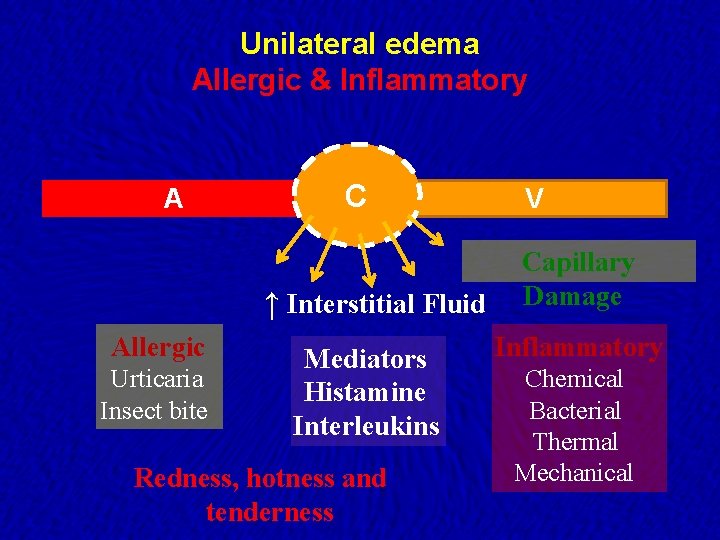
Unilateral edema Allergic & Inflammatory A C ↑ Interstitial Fluid Allergic Urticaria Insect bite Mediators Histamine Interleukins Redness, hotness and tenderness V Capillary Damage Inflammatory Chemical Bacterial Thermal Mechanical
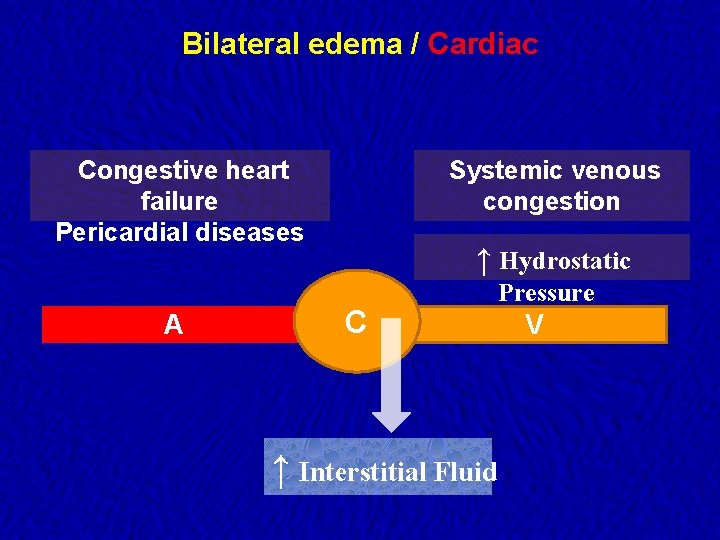
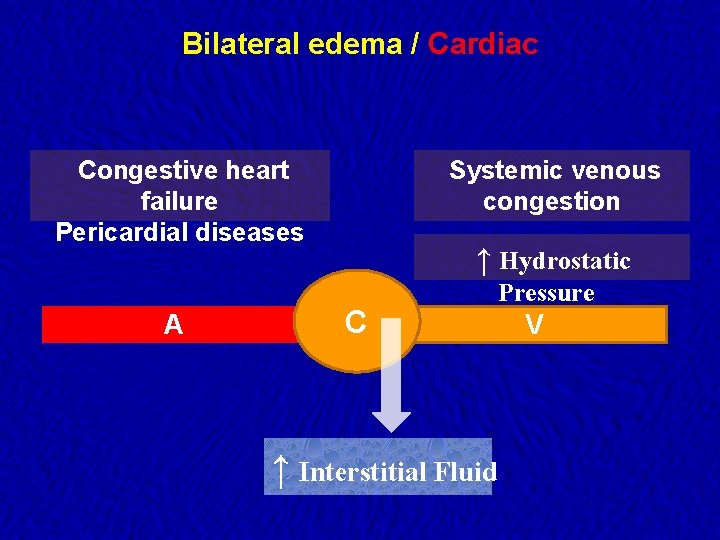
Bilateral edema / Cardiac Congestive heart failure Pericardial diseases A Systemic venous congestion ↑ Hydrostatic C ↑ Interstitial Fluid Pressure V
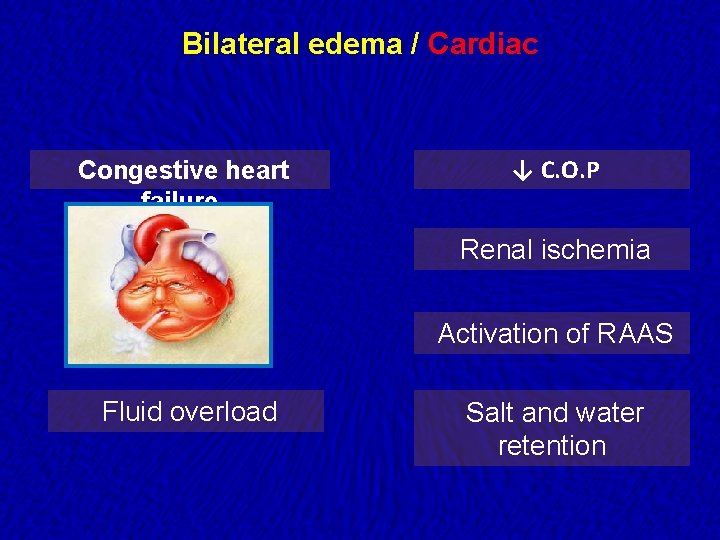
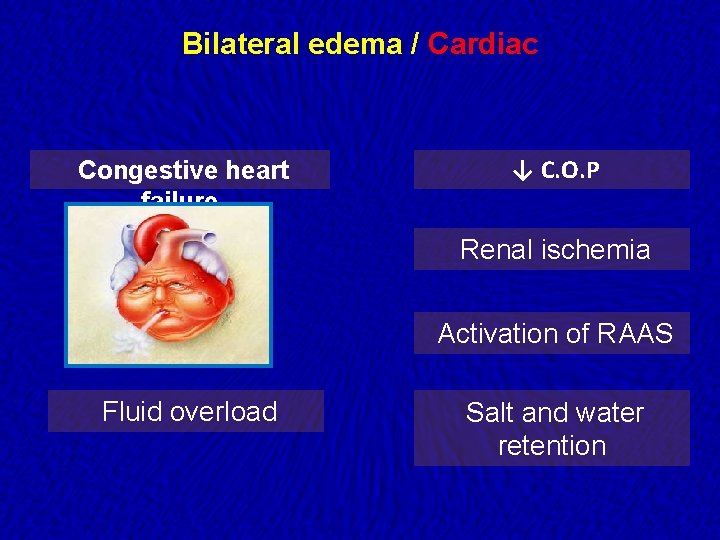
Bilateral edema / Cardiac Congestive heart failure ↓ C. O. P Renal ischemia Activation of RAAS Fluid overload Salt and water retention
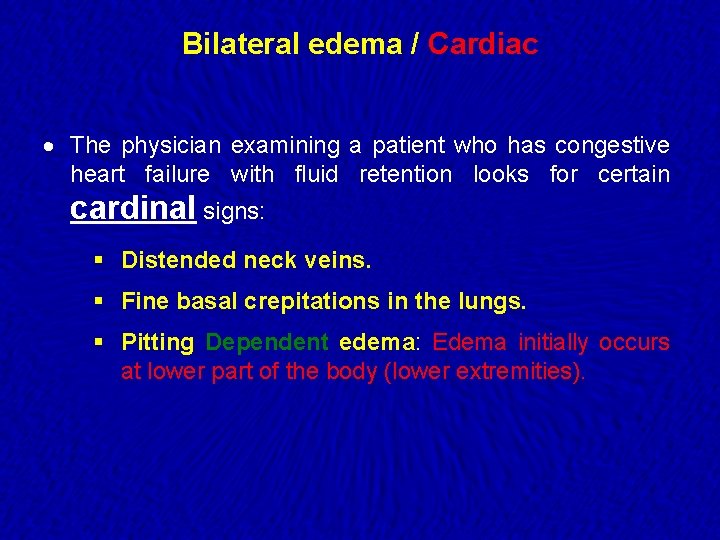
Bilateral edema / Cardiac · The physician examining a patient who has congestive heart failure with fluid retention looks for certain cardinal signs: § Distended neck veins. § Fine basal crepitations in the lungs. § Pitting Dependent edema: Edema initially occurs at lower part of the body (lower extremities).
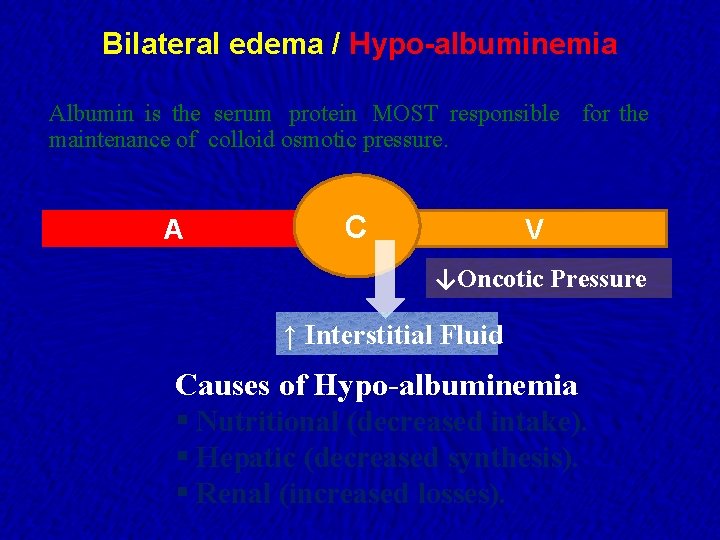
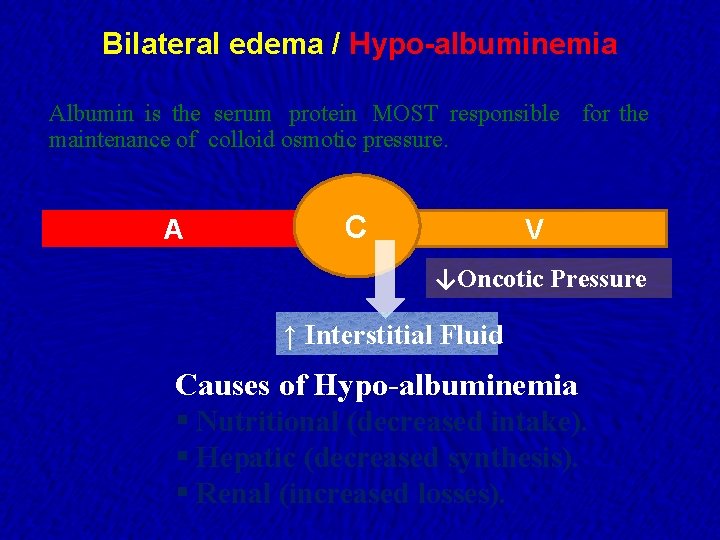
Bilateral edema / Hypo-albuminemia Albumin is the serum protein MOST responsible for the maintenance of colloid osmotic pressure. A C V ↓Oncotic Pressure ↑ Interstitial Fluid Causes of Hypo-albuminemia § Nutritional (decreased intake). § Hepatic (decreased synthesis). § Renal (increased losses).
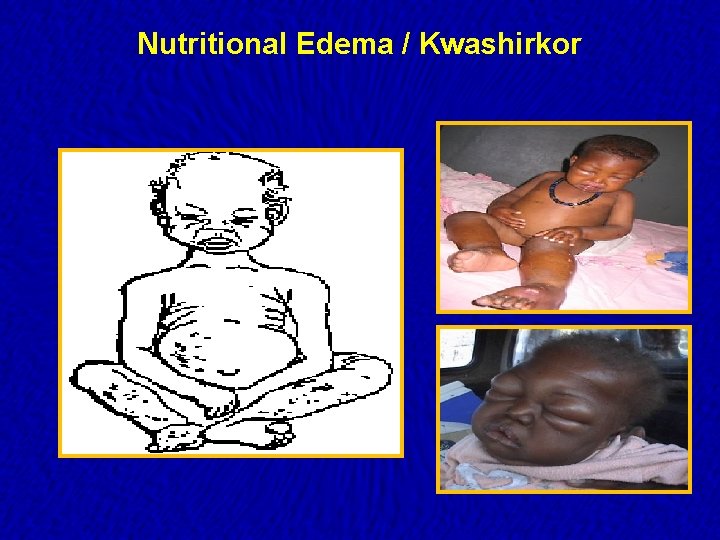
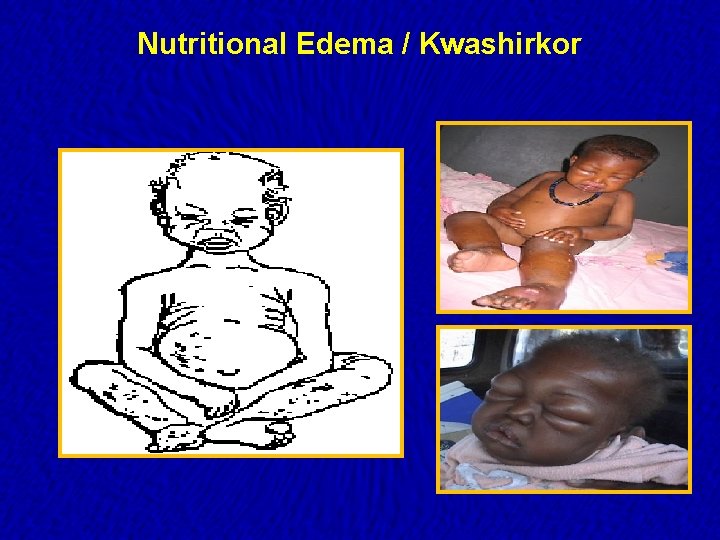
Nutritional Edema / Kwashirkor
Bilateral edema / Hepatic · Mechanism of edema in liver cirrhosis: § Hypo-albuminemia. § Salt and water retention due to impaired destruction of aldosterone and ADH. § ↑ nitric oxide systemic vasodilatation decreased effective plasma volume renal iscemia activation of the RAAS system salt and water retension.
Bilateral edema / Renal · Mechanism of edema in renal diseases: § Hypo-albuminemia due to increased losses in the urine as in nephrotic syndrome. § Salt and water retention as in cases of nephritic syndrome due to decreased renal capacity to excrete sodium.
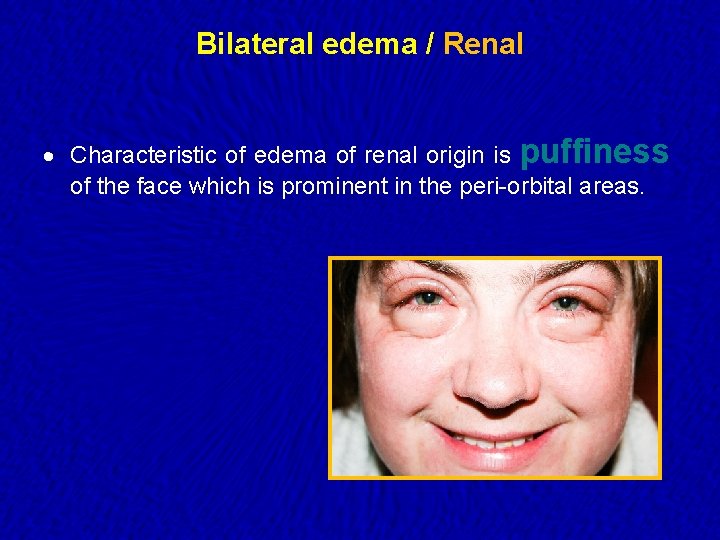
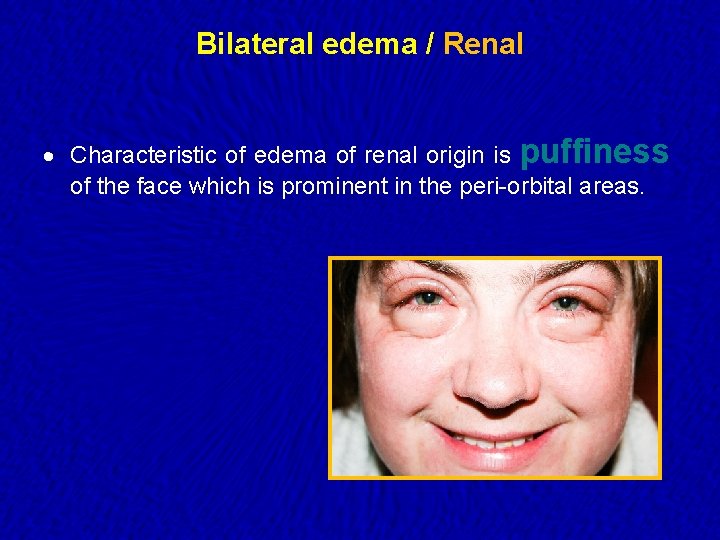
Bilateral edema / Renal · Characteristic of edema of renal origin is puffiness of the face which is prominent in the peri-orbital areas.
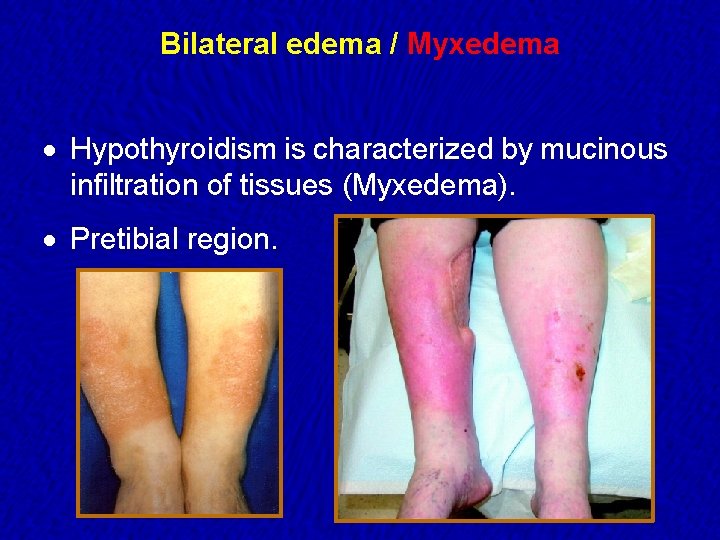
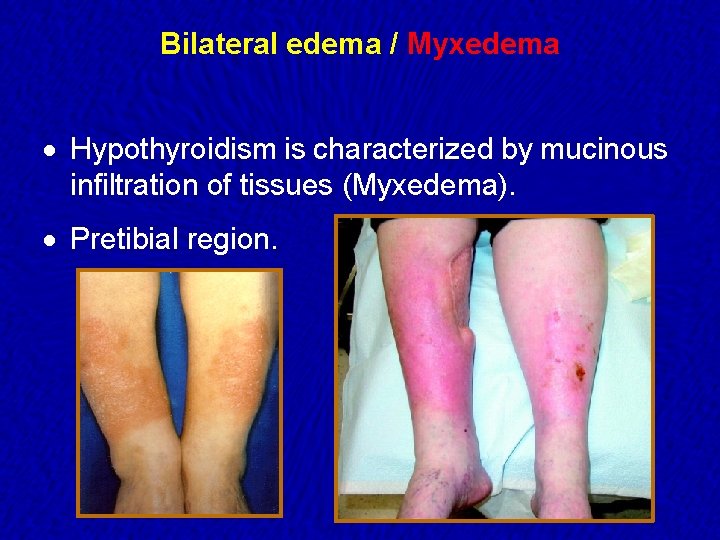
Bilateral edema / Myxedema · Hypothyroidism is characterized by mucinous infiltration of tissues (Myxedema). · Pretibial region.

Bilateral edema / Iatrogenic · Ca channel blockers. · Excess intra-venous fluids. · Corticosteroids. · Pioglitazone.
Premenstrual edema · Retention of water and increase in weight which occurs during or preceding menstruation. · The etiology is poorly understood. · The edema tends to be generalized, and resolves during a diuresis that occurs with the onset of menses.
Generalized edema / Idiopathic · Exclusive in women (usually Young & obese). · Periodic episodes of edema (unrelated to menstrual cycle). · Fluctuate in severity. · Aggravated by hot weather.
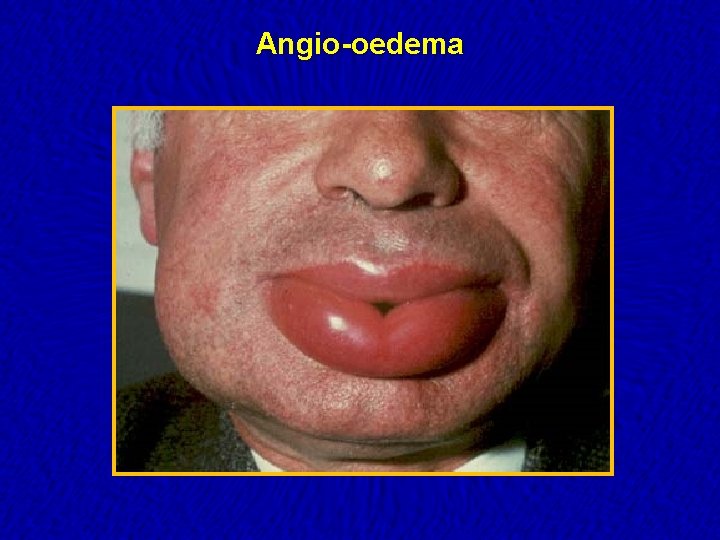
Angio-oedema · Specific form of allergic edema affecting the face, lips and mouth. · Swelling may develop rapidly and may be life-threatening if the upper airway is involved.
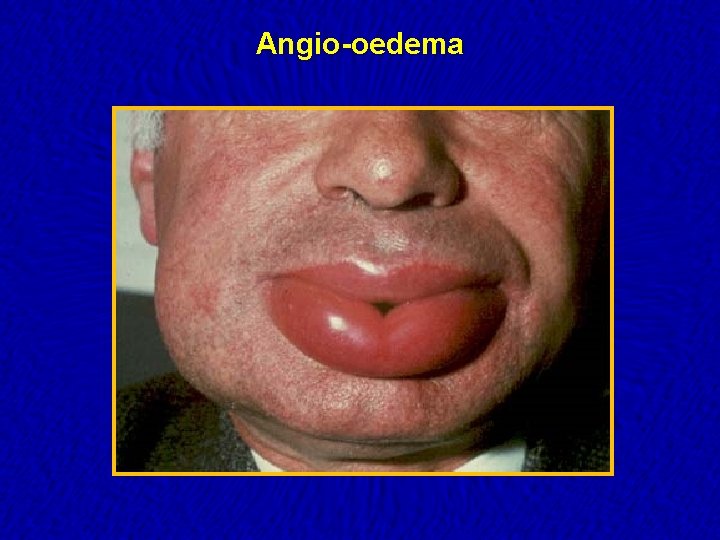
Angio-oedema
Lower limbs Edema How to examine?
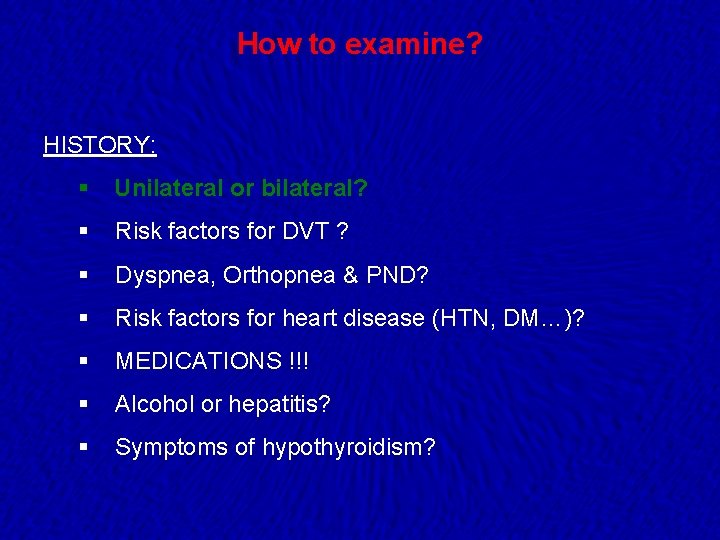
How to examine? HISTORY: § Unilateral or bilateral? § Risk factors for DVT ? § Dyspnea, Orthopnea & PND? § Risk factors for heart disease (HTN, DM…)? § MEDICATIONS !!! § Alcohol or hepatitis? § Symptoms of hypothyroidism?
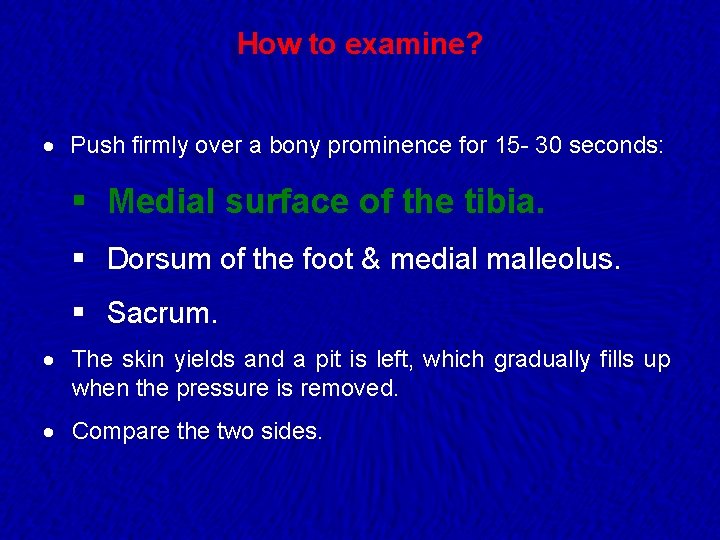
How to examine? · Push firmly over a bony prominence for 15 - 30 seconds: § Medial surface of the tibia. § Dorsum of the foot & medial malleolus. § Sacrum. · The skin yields and a pit is left, which gradually fills up when the pressure is removed. · Compare the two sides.
How to examine? Comment: · Location. · Symmetry. · Pitting or non-pitting appearance. · Severity (the four-point scale). · Tenderness. · Associated skin changes.
Physical examination · Jugular veins ? · Ascites ? · Stigmata of chronic liver disease ? · Physical findings of heart failure ?
Lower limbs Edema How to investigate?

How to investigate? · Chemistry panel and urinalysis to evaluate renal and liver function. · Albumin levels. · TSH / Free T 4. · ECG , chest radiograph or Echocardiography. · Abdominal U/S.
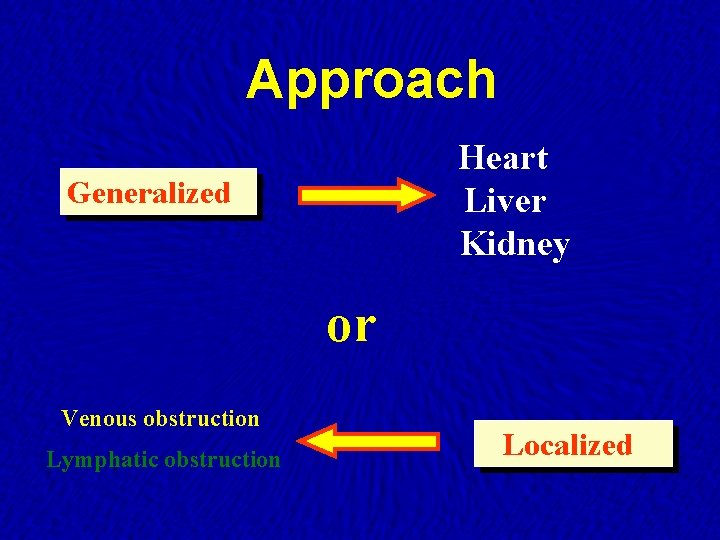
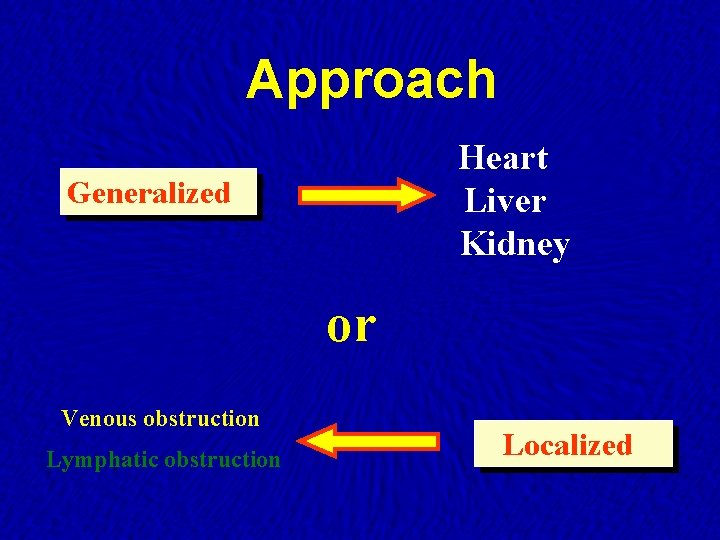
Approach Heart Liver Kidney Generalized or Venous obstruction Lymphatic obstruction Localized
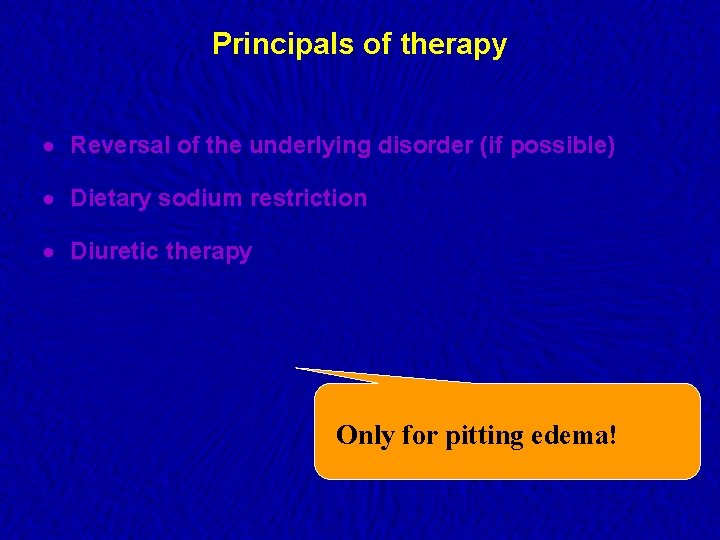
Principals of therapy · Reversal of the underlying disorder (if possible) · Dietary sodium restriction · Diuretic therapy Only for pitting edema!

Thank You
 Lymph tends to stall inside lymph nodes. this is due to
Lymph tends to stall inside lymph nodes. this is due to Lymph tends to stall inside lymph nodes
Lymph tends to stall inside lymph nodes Oobean
Oobean 5 groups of axillary lymph nodes
5 groups of axillary lymph nodes Scapula lymph nodes
Scapula lymph nodes Lymphatic drainage of lower limb
Lymphatic drainage of lower limb Middle mediastinum: contents mnemonic
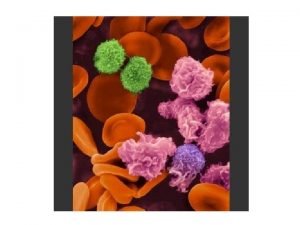
Middle mediastinum: contents mnemonic Composition of lymph
Composition of lymph Lymph nodes in forearm
Lymph nodes in forearm Lymph nodes: “filters of the blood”
Lymph nodes: “filters of the blood” Lymph nodes: “filters of the blood”
Lymph nodes: “filters of the blood” Walls of axilla
Walls of axilla Deep cervical lymph nodes drainage
Deep cervical lymph nodes drainage Left lymphatic duct
Left lymphatic duct Pitting vs nonpitting edema
Pitting vs nonpitting edema Lymph nodes function
Lymph nodes function Abdominal wall arteries
Abdominal wall arteries Ascending colon mesentery
Ascending colon mesentery Foot lymph nodes
Foot lymph nodes Gluteal ligaments
Gluteal ligaments Orbital lymph nodes
Orbital lymph nodes Blood supply of the breast
Blood supply of the breast 5 groups of axillary lymph nodes
5 groups of axillary lymph nodes 5 groups of axillary lymph nodes
5 groups of axillary lymph nodes Submental lymph nodes location
Submental lymph nodes location Supromedial
Supromedial Mycoplasma pneumoniae
Mycoplasma pneumoniae Posterior cervical lymph nodes
Posterior cervical lymph nodes Lymph formation
Lymph formation Infrahyoid region
Infrahyoid region Carotid artery hold
Carotid artery hold Epitrochlear lymph node
Epitrochlear lymph node Lymph nodes swelling in stomach
Lymph nodes swelling in stomach System
System Lymphatic system vs endocrine system
Lymphatic system vs endocrine system Lymphatic and urinary system
Lymphatic and urinary system What are the function of lymphatic system
What are the function of lymphatic system Chapter 12 the lymphatic system and body defenses
Chapter 12 the lymphatic system and body defenses Functions of the lymphatic system
Functions of the lymphatic system Cardiovascular/lymphatic system it's totally tubular
Cardiovascular/lymphatic system it's totally tubular Largest lymphoid organ
Largest lymphoid organ Lymphatic system
Lymphatic system Main components of lymphatic system
Main components of lymphatic system Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Integumentary interactions with other systems
Integumentary interactions with other systems Hemic and lymphatic
Hemic and lymphatic Organization of the lymphatic system
Organization of the lymphatic system Lymphatic system organs
Lymphatic system organs Dho7
Dho7 Lingual tonsil
Lingual tonsil Chapter 13 lymphatic system and immunity
Chapter 13 lymphatic system and immunity Exercise 38 review & practice sheet: lymphatic system.
Exercise 38 review & practice sheet: lymphatic system. Chapter 7:9 lymphatic system
Chapter 7:9 lymphatic system Flaplike minivalve
Flaplike minivalve Short tube that receives purified lymph
Short tube that receives purified lymph Types of lymphatic system
Types of lymphatic system Chapter 12 the lymphatic system and body defenses
Chapter 12 the lymphatic system and body defenses Photo of lymphatic system
Photo of lymphatic system Components of lymphatic system
Components of lymphatic system Interesting facts about the lymphatic system
Interesting facts about the lymphatic system Lymphatic vs immune system
Lymphatic vs immune system Lymph return
Lymph return Is the thyroid gland part of the lymphatic system
Is the thyroid gland part of the lymphatic system Function of skeletal muscle
Function of skeletal muscle Lymphatic system picture
Lymphatic system picture Flow chart of lymphatic system
Flow chart of lymphatic system Lymphatic system function
Lymphatic system function Lymph composition
Lymph composition Chapter 12 the lymphatic system and body defenses
Chapter 12 the lymphatic system and body defenses Chapter 16 lymphatic system and immunity
Chapter 16 lymphatic system and immunity Anatomy and physiology chapter 7
Anatomy and physiology chapter 7 Lymph system function
Lymph system function Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Chụp tư thế worms-breton
Chụp tư thế worms-breton Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ 101012 bằng
101012 bằng Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Bảng số nguyên tố
Bảng số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết