Neuroleptic Malignant Syndrome Recognition Risk factors and Management





- Slides: 13
Neuroleptic Malignant Syndrome Recognition, Risk factors and Management Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
Pathophysiology N Relative lack of dopamine – dopamine receptor blockade – inadequate dopamine production Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
Pathophysiology N Supporting evidence – neuroleptic drugs block dopamine receptors – occurs with other dopamine blocking drugs – occurs on sudden withdrawal of antiparkinsonian therapy – responds to dopamine agonists Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital

Clinical features N Essential – recent or current therapy with dopamine blocking drug neuroleptic l other drug eg metoclopramide l – recently stopped a dopamine agonist eg L -dopa Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital

Clinical features N Major (all within 24 h) – fever > 37. 5 o. C (no other cause) – autonomic dysfunction – extrapyramidal features Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
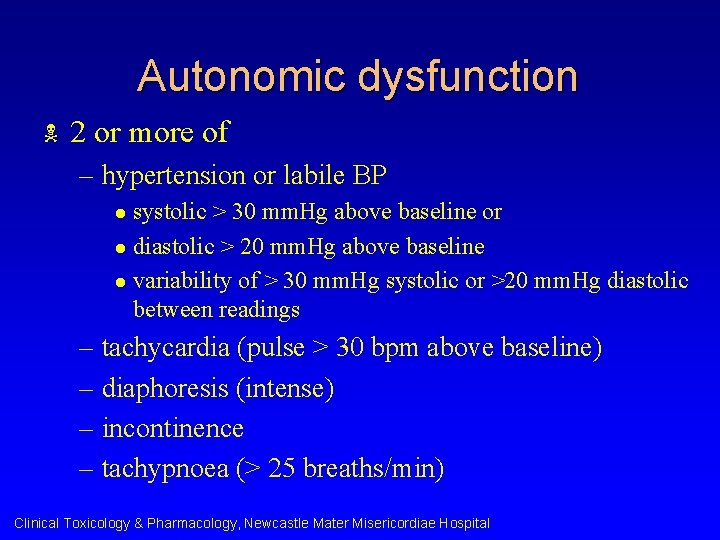
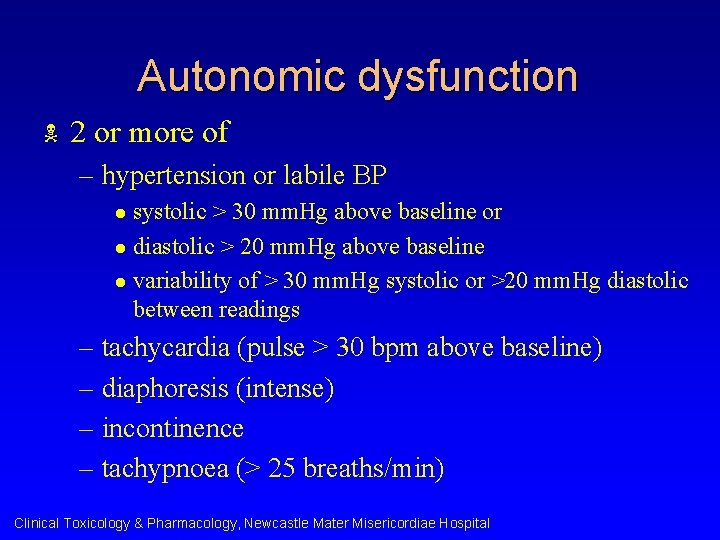
Autonomic dysfunction N 2 or more of – hypertension or labile BP systolic > 30 mm. Hg above baseline or l diastolic > 20 mm. Hg above baseline l variability of > 30 mm. Hg systolic or >20 mm. Hg diastolic between readings l – tachycardia (pulse > 30 bpm above baseline) – diaphoresis (intense) – incontinence – tachypnoea (> 25 breaths/min) Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
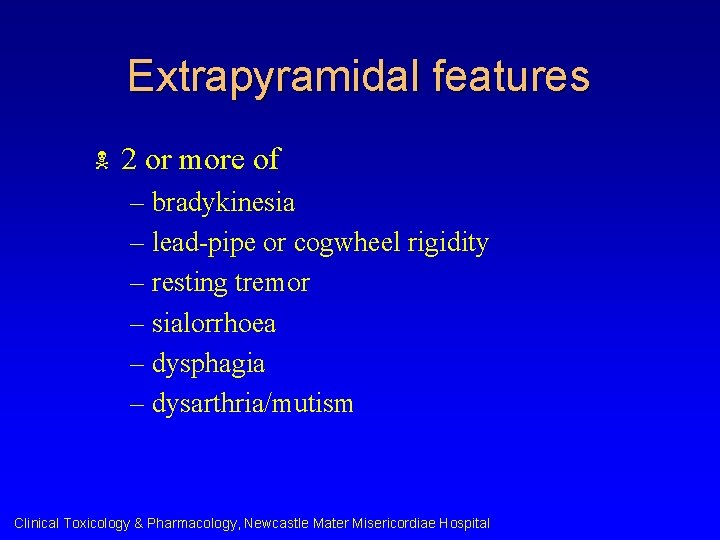
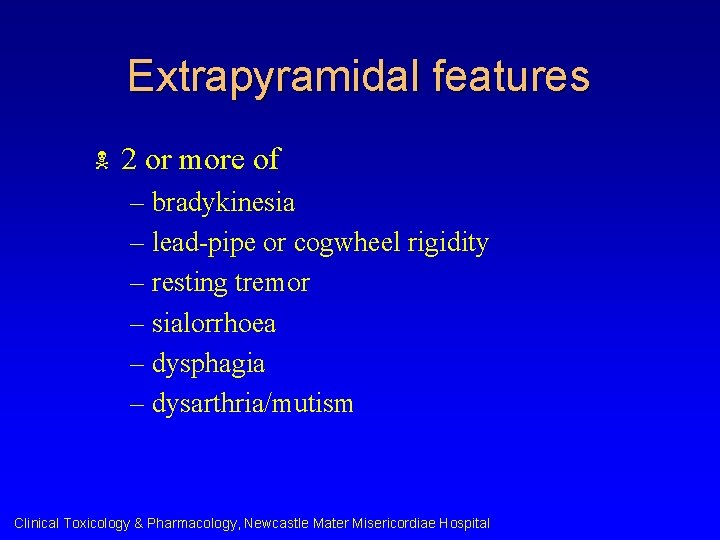
Extrapyramidal features N 2 or more of – bradykinesia – lead-pipe or cogwheel rigidity – resting tremor – sialorrhoea – dysphagia – dysarthria/mutism Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
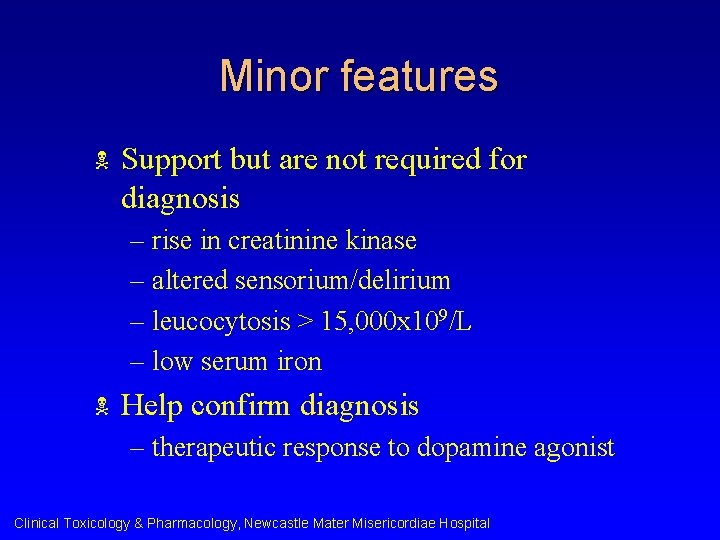
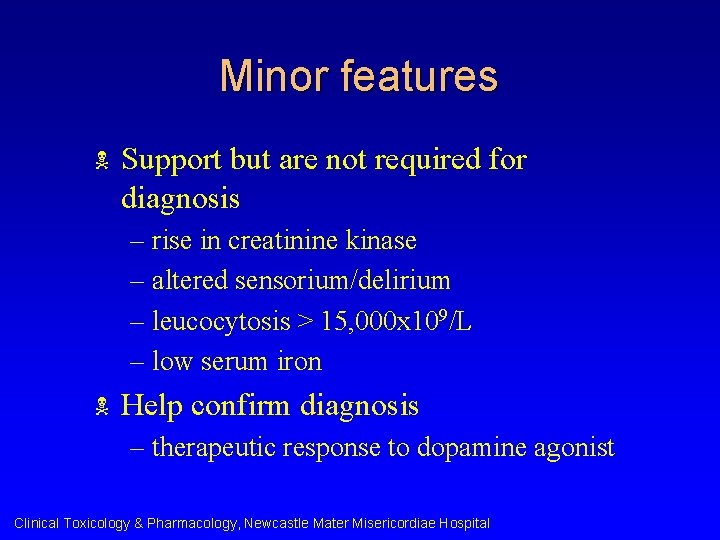
Minor features N Support but are not required for diagnosis – rise in creatinine kinase – altered sensorium/delirium – leucocytosis > 15, 000 x 109/L – low serum iron N Help confirm diagnosis – therapeutic response to dopamine agonist Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
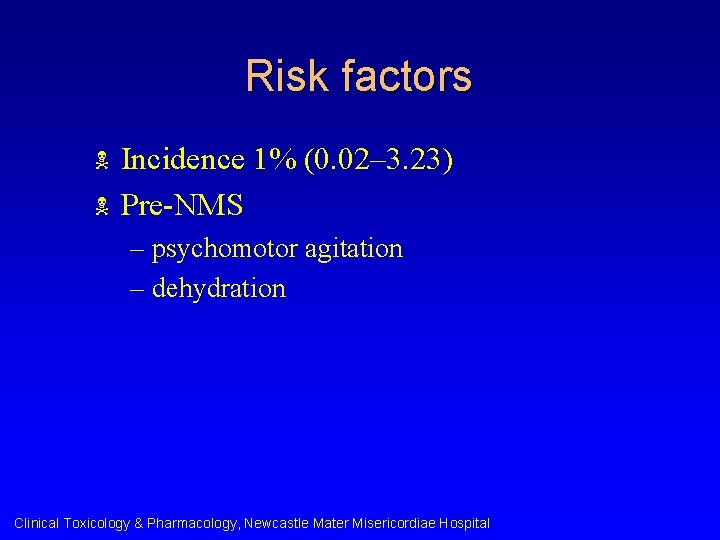
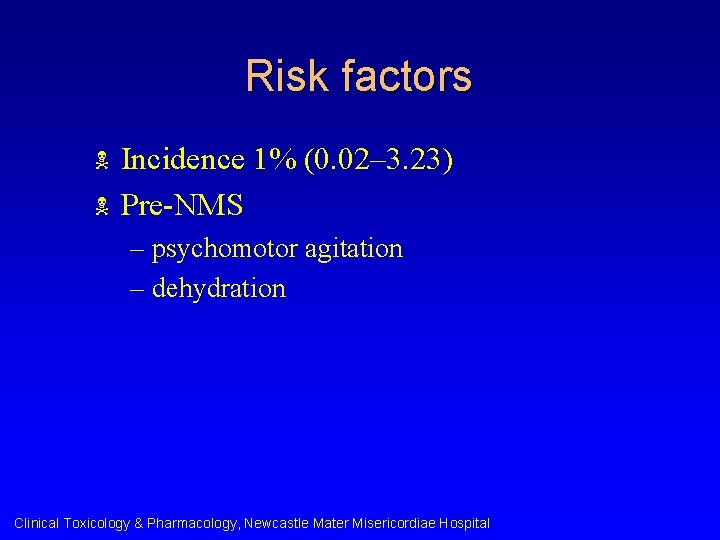
Risk factors N N Incidence 1% (0. 02– 3. 23) Pre-NMS – psychomotor agitation – dehydration Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital

Risk factors N Related to treatment – neuroleptic dose in first 24 h > 600 mg of chlorpromazine – maximum dose in any 24 h > 600 mg of chlorpromazine – required restraint or seclusion N Associated – past ECT Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
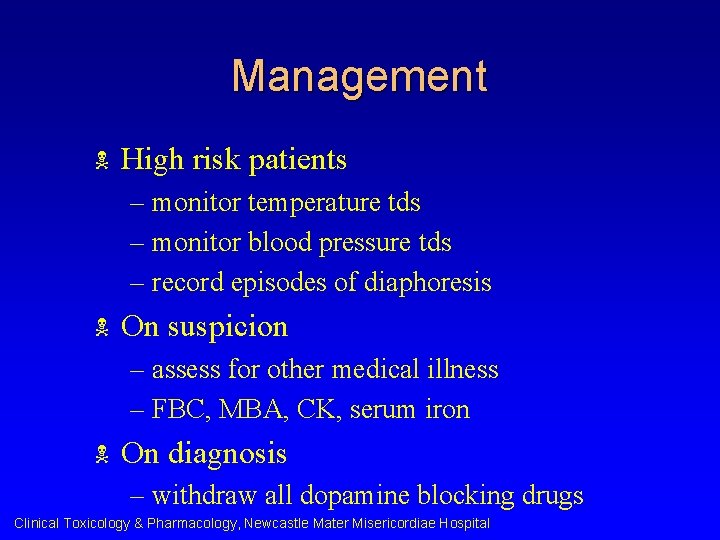
Management N High risk patients – monitor temperature tds – monitor blood pressure tds – record episodes of diaphoresis N On suspicion – assess for other medical illness – FBC, MBA, CK, serum iron N On diagnosis – withdraw all dopamine blocking drugs Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital

Drug therapy N Bromocriptine – 2. 5 mg q 8 h up to 5 mg q 4 h – continue for 7– 10 days after resolution then taper over 1– 2 weeks (except depot preparations) N Dantrolene – 2– 3 mg/kg – extreme rigidity, very high fever (> 40 o. C), unable to tolerate oral treatment Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital

Otherapy N Benzodiazepines – to control agitation/delirium N ECT – refractory to adequate trial of dopamine agonist/supportive care – after resolution of acute features remain catatonic or l develop ECT-responsive psychotic features l – suspected acute lethal catatonia Clinical Toxicology & Pharmacology, Newcastle Mater Misericordiae Hospital
 Malignant neuroleptic syndrome
Malignant neuroleptic syndrome Neuroleptic malignant syndrome
Neuroleptic malignant syndrome Nursing care plan for schizophrenia pdf
Nursing care plan for schizophrenia pdf Stratum basale
Stratum basale Neurolyptics
Neurolyptics Neurolyptics
Neurolyptics Hyperosmolar hyponatremia
Hyperosmolar hyponatremia Osmotic demyelination syndrome risk factors
Osmotic demyelination syndrome risk factors Cataractectomy
Cataractectomy Market risk assessment
Market risk assessment Malignant and benign tumors
Malignant and benign tumors Adenocarcinoma
Adenocarcinoma Cachexia
Cachexia Benign vs malignant
Benign vs malignant