Malignant Spinal Cord Compression What is Malignant Spinal















- Slides: 51
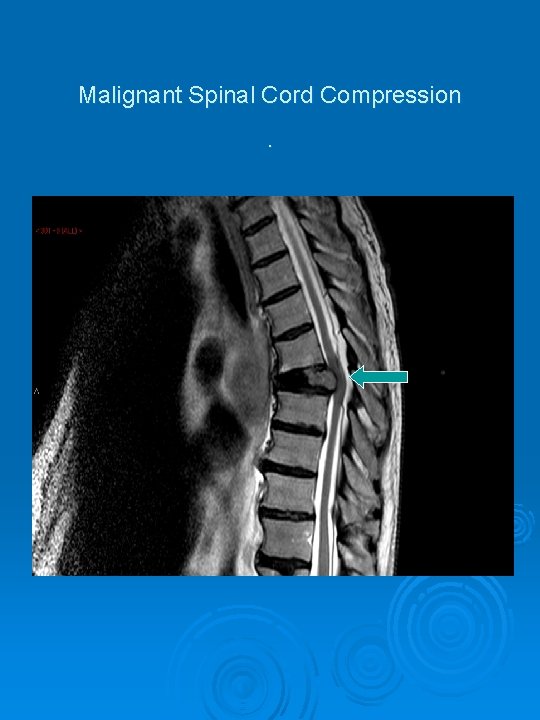
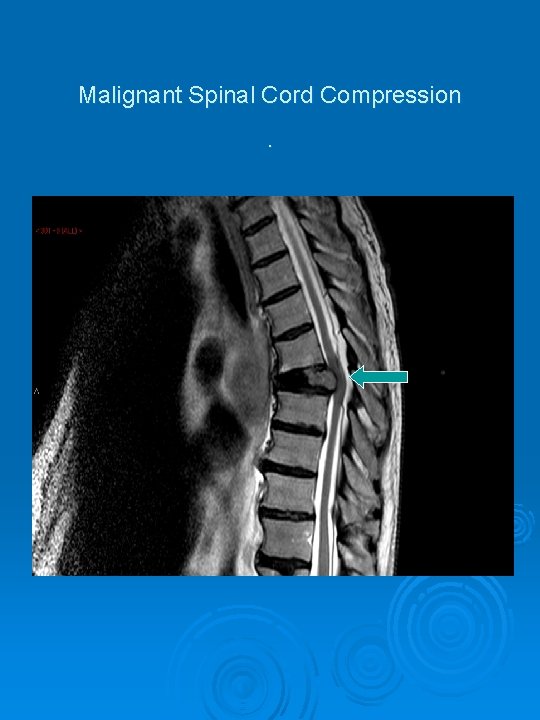
Malignant Spinal Cord Compression.
What is Malignant Spinal Cord Compression? Usually a consequence of malignant spread of a known Ca, most commonly Breast, Lung or Prostate Ca, Multiple Myeloma or Lymphoma, either to the bones of the spine – the vertebral bodies. Or to the spinal cord itself – much rarer.
NICE Guideline definition “Spinal cord or Cauda equina compression by direct pressure and/or induction of vertebral collapse or vertebral instability by metastatic spread or direct extension of malignancy that threatens or causes neurological disability. ” Nice Clinical Guideline 75 Metastatic Spinal Cord Compression November 2008
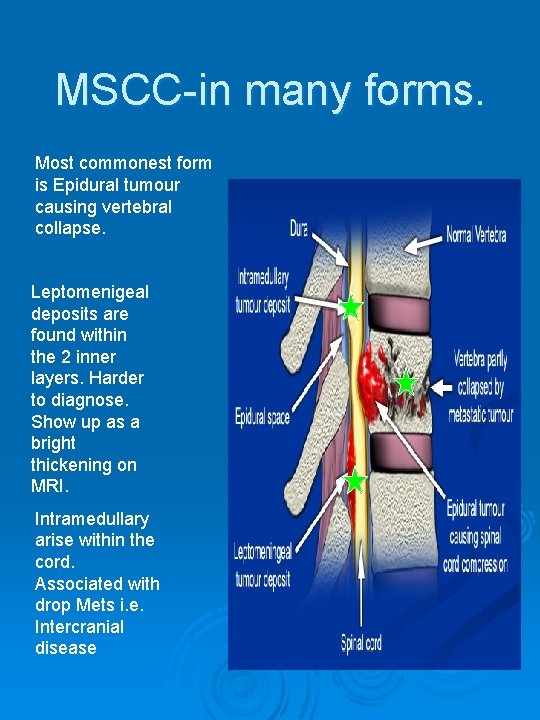
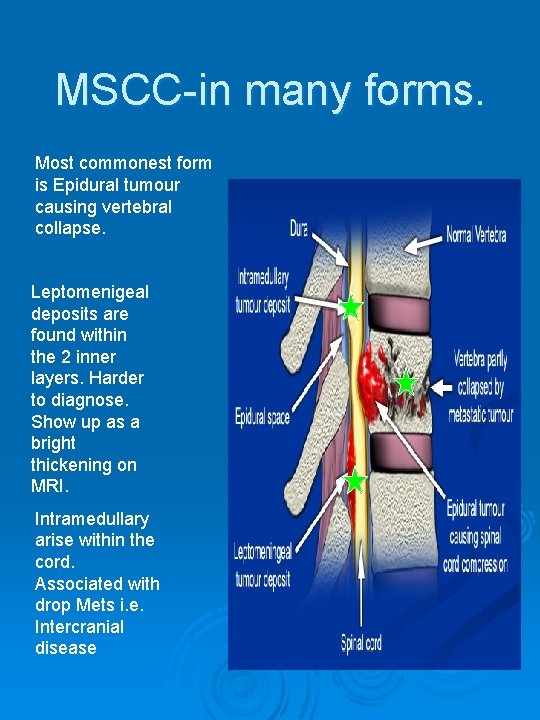
MSCC-in many forms. Most commonest form is Epidural tumour causing vertebral collapse. Leptomenigeal deposits are found within the 2 inner layers. Harder to diagnose. Show up as a bright thickening on MRI. Intramedullary arise within the cord. Associated with drop Mets i. e. Intercranial disease
What are the effects of MSCC? Paralysis from the level of the compression, if presentation is late.
“If the Presentation is late” If a suspected MSCC patient can be identified early enough, Admitted and MRI scanned swiftly, Radiotherapy planned and delivered swiftly, And the spine protected if it is UNSTABLE, All the above could mean the difference between the patient becoming paraplegic or retaining some degree of functional walking.
How does MSCC present? Patient with a known Hx of Cancer, Who develops a New Back Pain, severe in nature, which is: - worse on lying down, radicular, worse on cough, night pain. And a new difficulty walking. Much harder to diagnose if patient has an undiagnosed Ca.
The Fast Track System, (Malignant Spinal Cord Compression Co-ordinators Role) Set up May 2009, reported in Team Brief and by e-mail flyer to all Ward Managers, Objective was to improve the coordination of the admission of the patient with MSCC, With the ultimate objective of improving the outcome for the patient.
The MSCC Co-ordinator Role Voluntary Rota (alongside daily clinical duties), On call from 9 am til 5 pm Mon-Fri (then covered by on-call oncologist out of Hours), Liaises directly with on-call oncologist regarding triage/management, Co-ordinates admission/MRI/Simulation and Radiotherapy/PT and OT.
The MSCC Co-ordinators Role If a suspected MSCC patient can be identified early enough, Admitted and MRI scanned swiftly, Radiotherapy planned and delivered swiftly, And the spine protected if it is UNSTABLE, All the above could mean the difference between the patient becoming paraplegic or retaining some degree of functional walking.
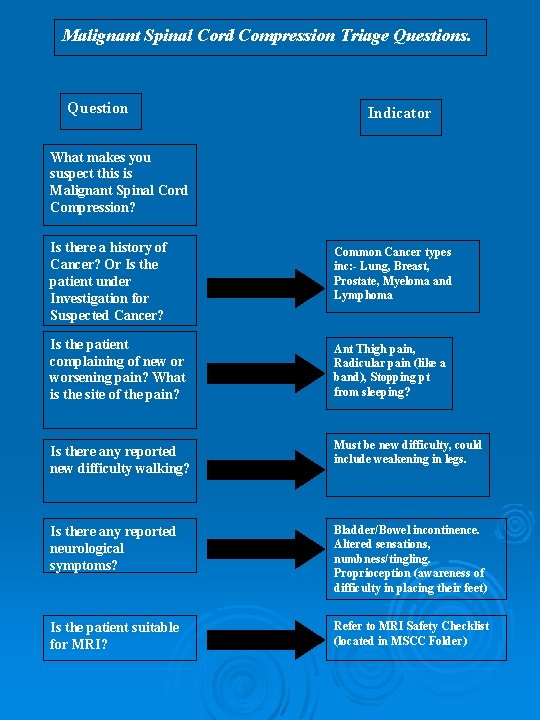
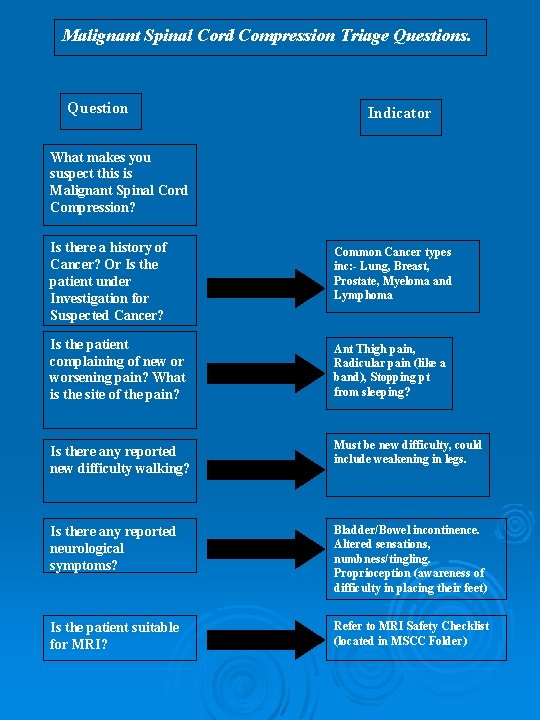
Malignant Spinal Cord Compression Triage Questions. Question Indicator What makes you suspect this is Malignant Spinal Cord Compression? Is there a history of Cancer? Or Is the patient under Investigation for Suspected Cancer? Common Cancer types inc: - Lung, Breast, Prostate, Myeloma and Lymphoma Is the patient complaining of new or worsening pain? What is the site of the pain? Ant Thigh pain, Radicular pain (like a band), Stopping pt from sleeping? Is there any reported new difficulty walking? Must be new difficulty, could include weakening in legs. Is there any reported neurological symptoms? Bladder/Bowel incontinence. Altered sensations, numbness/tingling. Proprioception (awareness of difficulty in placing their feet) Is the patient suitable for MRI? Refer to MRI Safety Checklist (located in MSCC Folder)
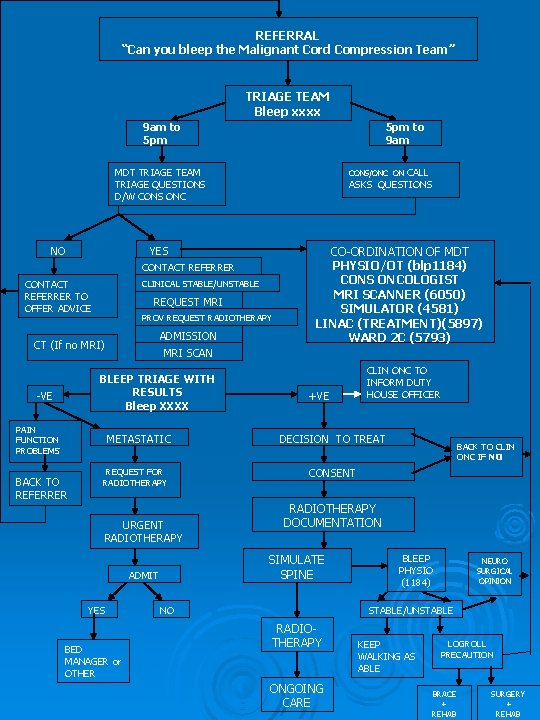
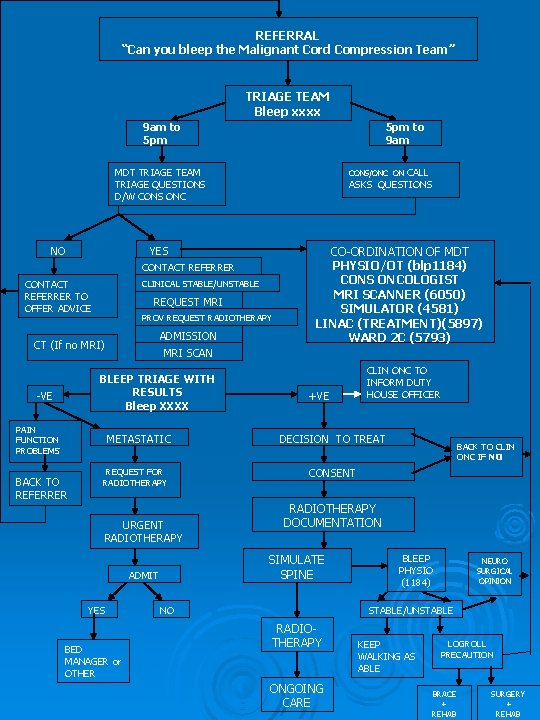
REFERRAL “Can you bleep the Malignant Cord Compression Team” TRIAGE TEAM Bleep xxxx 9 am to 5 pm to 9 am MDT TRIAGE TEAM TRIAGE QUESTIONS D/W CONS ONC NO CALL ASKS QUESTIONS CONS/ONC ON YES CONTACT REFERRER TO OFFER ADVICE CLINICAL STABLE/UNSTABLE REQUEST MRI PROV REQUEST RADIOTHERAPY ADMISSION CT (If no MRI) MRI SCAN BLEEP TRIAGE WITH RESULTS Bleep XXXX -VE PAIN FUNCTION PROBLEMS METASTATIC BACK TO REFERRER CO-ORDINATION OF MDT PHYSIO/OT (blp 1184) CONS ONCOLOGIST MRI SCANNER (6050) SIMULATOR (4581) LINAC (TREATMENT)(5897) WARD 2 C (5793) REQUEST FOR RADIOTHERAPY URGENT RADIOTHERAPY BED MANAGER or OTHER DECISION TO TREAT BACK TO CLIN ONC IF NO CONSENT RADIOTHERAPY DOCUMENTATION SIMULATE SPINE ADMIT YES +VE CLIN ONC TO INFORM DUTY HOUSE OFFICER NO BLEEP PHYSIO (1184) NEURO SURGICAL OPINION STABLE/UNSTABLE RADIOTHERAPY ONGOING CARE KEEP WALKING AS ABLE LOGROLL PRECAUTION BRACE + REHAB SURGERY + REHAB
How to contact MSCC Co-ordinator Via Switchboard: Automatic Lady
Admissions Through the pathway should be to Ward 2 C, Ideally the patient will be admitted to 2 C, because they are then under the care of an Oncology or Haematology Consultant, and 2 C Nursing Staff have an awareness of the implications of the Stable/Unstable spine status. 2 C, between hours of 9 - 5 will decant to accommodate pathway/confirmed MSCC patient if at all possible, after 8 pm decants need to be organised through the duty manager, as per hospital policy.
Admissions cont. Outwith hours of the pathway may well come in through 6 A, If a suspected cord compression is admitted during the day, not via the pathway, INFORM the pathway. Uncomfirmed Cord Compressions who come in outwith the pathway generally need to stay on their admission ward until scanned and confirmed. Uncomfirmed, but suspected Cord Compressions should be treated as UNSTABLE until proved otherwise. (NICE Guidelines 2008)
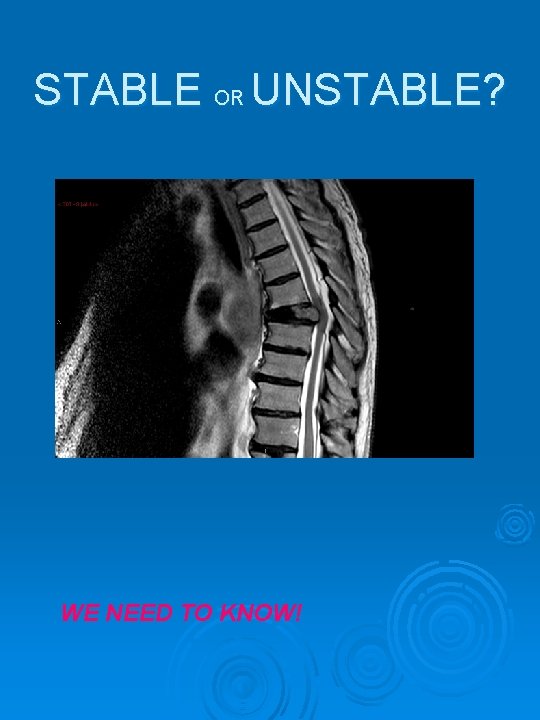
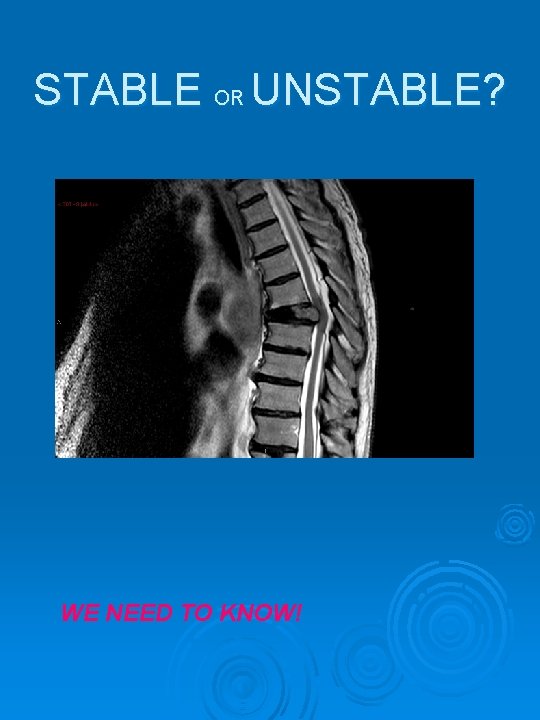
STABLE OR UNSTABLE? WE NEED TO KNOW!

‘Stable’ Vertebral Bodies Ø Cannot do any further damage to the spinal cord. Ø Patients with Stable vertebral bodies can move around as able, without any restrictions, as safety allows. Ø Can sit up in bed, in a chair, walk around if able.
‘Unstable’ Vertebral Bodies Ø Have the potential to cause further damage to the spinal cord and therefore reduce the patients function further. Ø Require to be log-rolled, and kept totally supine, one pillow allowed and cathaterised until fitted with a brace or transferred to another hospital for surgery. Ø If a brace is fitted, patient can be up to sit/walk as able when brace is on, all other times must be kept supine, on a firm mattress.



Ø Who is ‘at risk’ and incidence? Ø Early diagnosis is a priority (Evidence base) Ø Management once MSCC has occurred (Evidence base) Ø Progress re implementation
Who is at risk? Ø Stats: - General incidence 5 -10% of patients with cancer will develop MSCC, (3 -7. 4% of all patients with Ca lung, breast and prostate) Ø Professionally: GP’s would rate the condition as rare (2 -3 in GP Career) Oncology Consultants - quite common, Palliative Medics – common++, Ø Other statistics estimate that 75% of MSCC go undiagnosed, (diagnosis made at post-mortem) clinical presentation is of an elderly patient with a cancer Hx who has gone off their feet.
MSCC Facts • • • Commonest cause is blood spread (85%) Less common is direct invasion or direct deposition of tumour cells. Compression causes Oedema, Venous Congestion and demyelination. If gradual, effects can be reversible. Prolonged compression causes vascular injury resulting in Cord Infarction, this is not reversible.

MSCC Facts • • • T spine is commonest site (68%) The site of pain is not always the site of the compression 54% pts with upper T Spine compression had Lumbar pain Sensory level does not always correspond with site of compression (could be out by many dermatomes) useful in only 16% of cases Sensory level is a late indicator of cord compression
Early diagnosis is a priority Ø Refs: - Clinical Research and Audit Group Report, 2001 Ø Levak et al, Clinical Oncology, 2002, 14, 472 -480
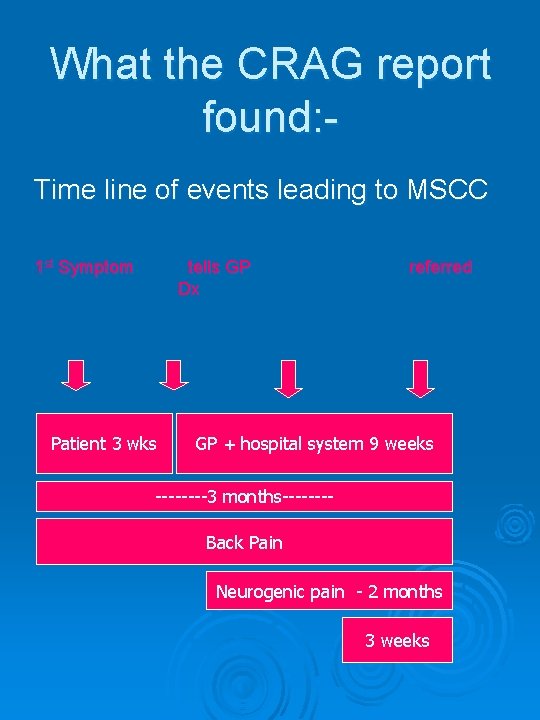
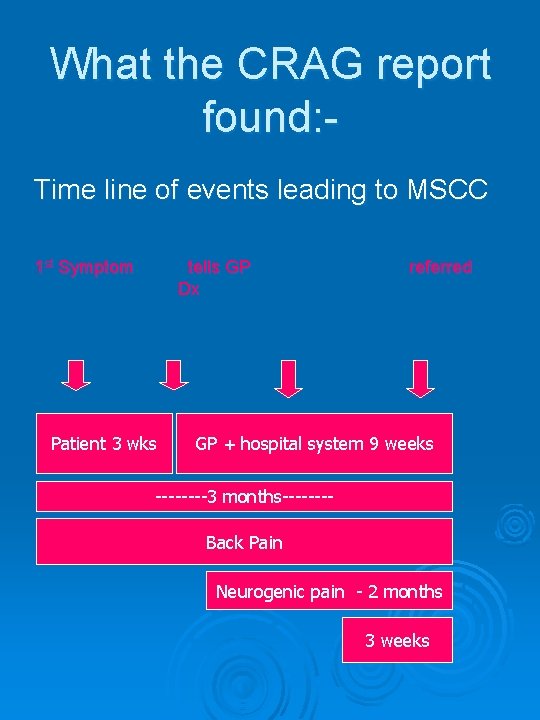
What the CRAG report found: Time line of events leading to MSCC 1 st Symptom tells GP Dx Patient 3 wks referred GP + hospital system 9 weeks ----3 months-------Back Pain Neurogenic pain - 2 months 3 weeks
FACT Ø If a patient presents with paraplegia due to MSCC it is unlikely that they will walk again. Ø The Scottish Executive Clinical Research and Audit Group study in 2001, found that 48% of their study population were unable to walk at diagnosis.
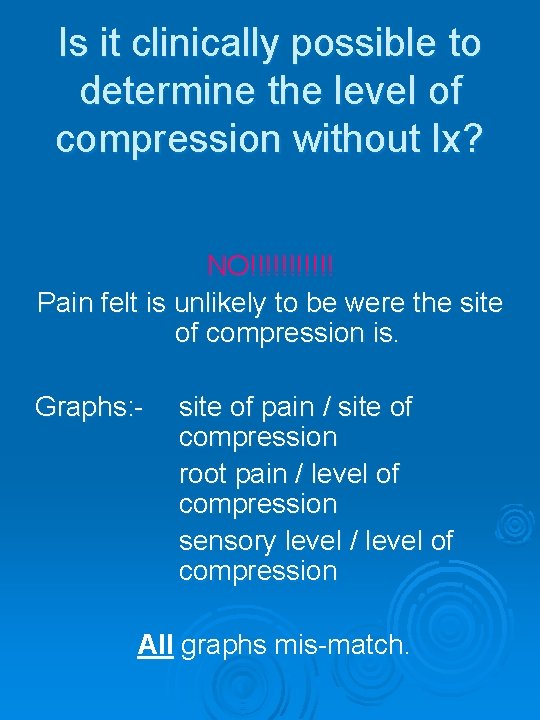
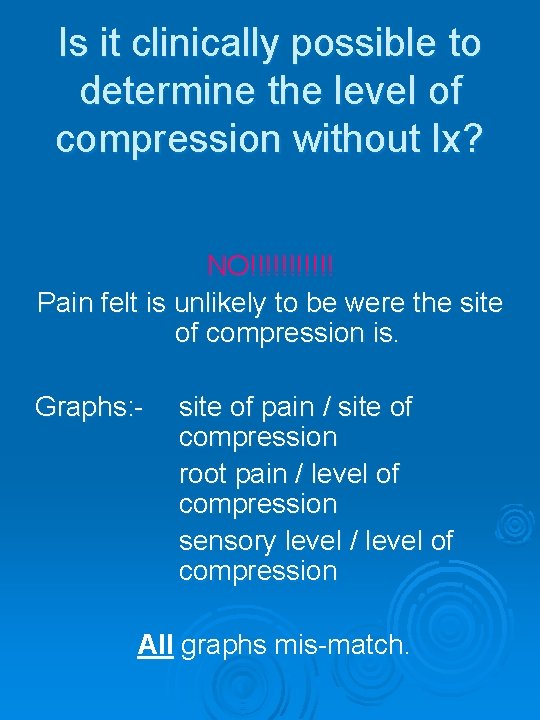
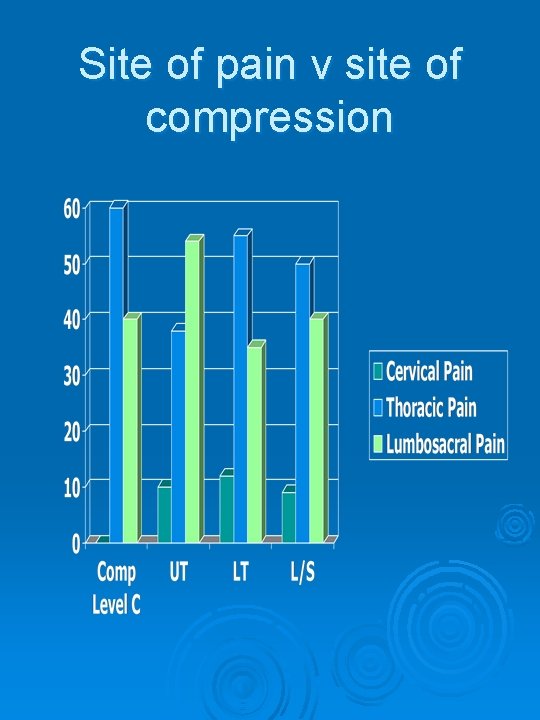
Is it clinically possible to determine the level of compression without Ix? NO!!!!!! Pain felt is unlikely to be were the site of compression is. Graphs: - site of pain / site of compression root pain / level of compression sensory level / level of compression All graphs mis-match.
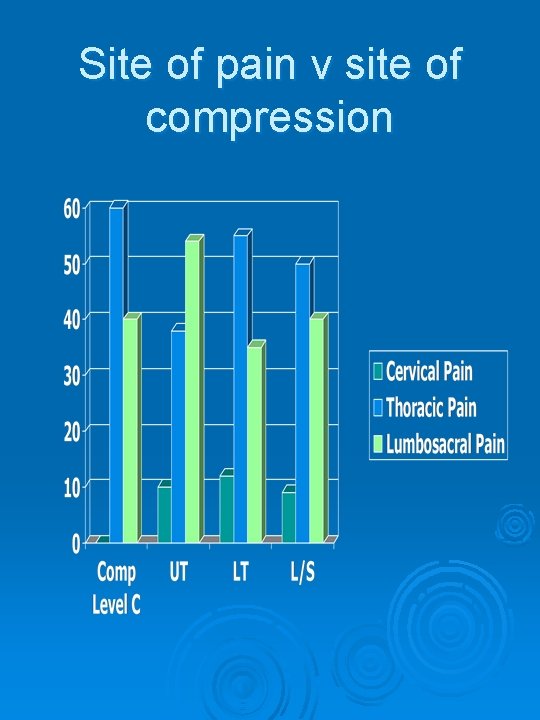
Site of pain v site of compression
The definitive test for diagnosis of MSCC Is a whole spine MRI scan CRAG Audit Results showed less than 1 in 5 plain films, and less than 1 in 5 bone scans were predictive of MSCC. Also that when x-rays were taken, most xrays were of the lumbar spine and most of the compressions were at thoracic level.
What has developed from the CRAG report? A clinician, Dr Pam Levak, spearheaded a campaign entitled ‘QED’ QUERY EPIDURAL DISEASE It took her at least 3 years but she finally realised her dream and developed a QED Hotline in Dundee in 2004. Sept 2005 Update: -In Tayside the Hotline was a victim of its own success. It was so successful that it is now no longer required as a special service, it has become “Best Practice”
What are we looking for ? Pt with known history of cancer especially lung, breast, prostate, Lymphoma and Multiple Myeloma. Who presents with new back pain, which is worse on lying down, radicular, worse on coughing, night pain.

MSCC Symptoms • • • Localised Back Pain (Progressive and latterly Severe) Sharp, Shooting, Burning are common descriptors. Nerve Root pain (Like a band around chest or sore front of thighs). Weakness in one or both legs. May be reporting unexplained falls. Neuro Symptoms. (Numb/Tingling/Proprioception) Problems passing urine/faeces. (Think of Opioids) Paralysis
Dr Levak says … Ø It is not clever to diagnose MSCC once someone has gone off their feet!!! Ø Weakness is a late sign so don’t wait for it to happen!!!!!
Message? Query Epidural Disease

Step 2 Management once MSCC has occurred: Pease, Harris and Finlay (2004) “Development and audit of a care pathway for the management of patients with suspected Malignant Spinal Cord Compression” Physiotherapy, Vol 90, No 1, Pp 27 – 34. Provides the evidence base.
Design and Implementation of a Fast Track Malignant Spinal Cord Compression Service

The Spinal Cord…a little revision! A Cylindrical structure constituting the central nervous system, extending from the Medulla to the lower border of L 1 where it then becomes the Cauda Equina or the horses tail. It is surrounded by the 3 layers called the meninges and bathed in Cerebrospinal Fluid or CSF. There are 31 pairs of spinal nerves 8 Cervical, 12 Thoracic, 5 Lumbar, 5 sacral and 1 Coccygeal. This constitutes the peripheral nervous system. Reproduced by kind permission of S. Garrett 2009 Function: allows nerve impulses to travel between brain and body

So Why Implement a Fast Track MSCC Service? Ø Ø Patients Perspective Referrers Perspective Hospital Perspective Nice Guidelines Nov 2008 Our existing ‘pathway’ was non existent! With ‘some’ work this is what we came up with!!!
Reasons for implementation Ø Existing pathway involved multiple disciplines (Largely unaware of each other)! Ø It lacked co-ordination, structure and understanding of each disciplines role in MSCC. Ø Lack of coherence. Ø Conflicting information given to patients/staff which resulted in delays in diagnosis and treatment/rehabilitation.

Patients Perspective Early Onset + Early treatment = Better QOL Improved Mobility Maintained Independence Late Treatment= None of the above and increased complication and mortality rate.
Referrers Perspective. Ø Clear, efficient and streamlined referral pathway. Ø Timely referral to correct services. Ø Advice, support and feedback via Triage Team Ø Assurance that patient will follow a consistent pathway to treatment.
NHS Perspective Ø Our objective was always to redirect resources into patient focused care. Ø Reduce inefficiency and create a better system of work. Ø Using a successful template from Tayside, tailored to meet the specific demands of Highland, structure a pathway of our own.
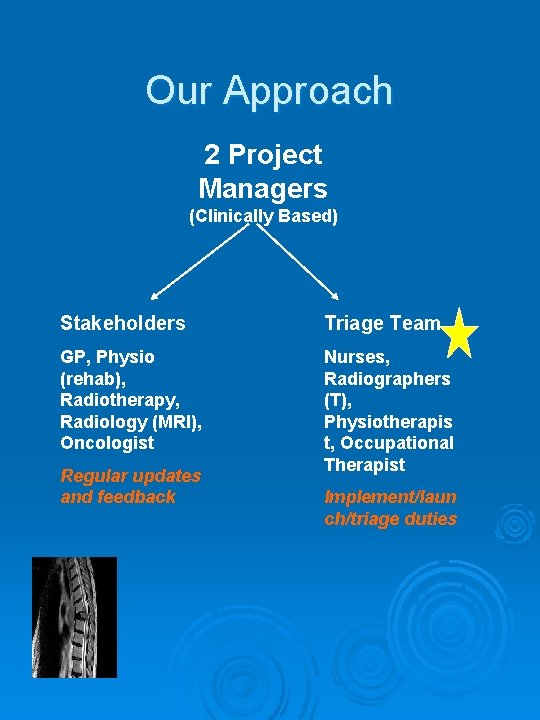
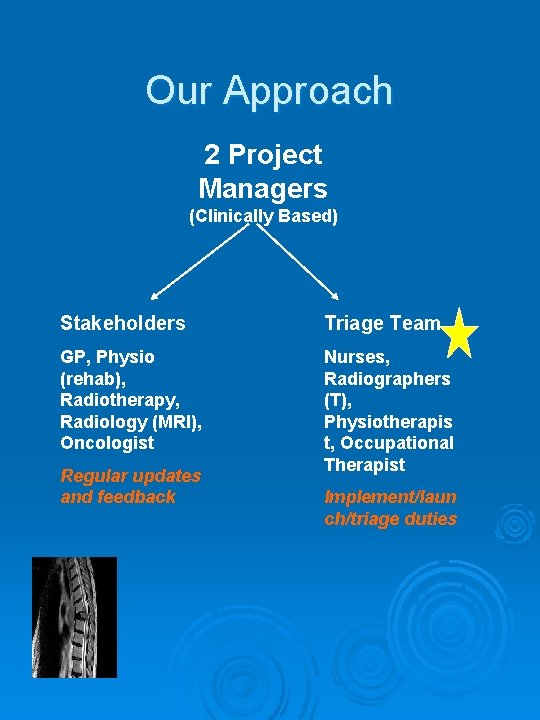
Our Approach 2 Project Managers (Clinically Based) Stakeholders Triage Team GP, Physio (rehab), Radiotherapy, Radiology (MRI), Oncologist Nurses, Radiographers (T), Physiotherapis t, Occupational Therapist Regular updates and feedback Implement/laun ch/triage duties

Our Approach Health Professionals (community) Palliative care (community) Outpatient Depts Oncology Dept awareness sessions Wards GP practices Peripheral Hospitals Start small and local to check infra structure. Once out in the ‘public domain’ its hard to control

Our Approach to Training §Triage Training 5 Staff members operating a rota system. In house Triage Training in liasion with Oncology Consultants. In depth scenario training using actual case studies with feedback from Oncology Consultants. Standardised documentation. Audit under development Why have a logo? It gives us an identity and ownership. The puzzle is a visual prompt.
The MSCC Co-ordinator Role…. what the referrer would expect. § § § Timely response and explanation of process. Taken through a series of triage questions A named point of contact. Advice and feedback. Logical approach to transfer of patient to appropriate services.

IMPORTANT What you need to know § § § If You Suspect MSCC speak to someone. Anyone can bleep the MSCC Co-ordinator. Use the correct Phraseology at switchboard. ‘Malignant Spinal Cord Co-ordinator’ If it doesn’t fit our pathway we will tell you and advise on an alternative route.

Results at 6 months Ø Number of referrals = 25 Ø Number of positive cords = 8 Ø No of Cauda Equina = 6 Ø No of patients scanned/not =5 Rx (2 allowed significant subsequent diagnosis to be made) Ø Not Scanned = 2 (seen by consultant) Ø No inappropriate referrals = 4

References P. Levak et al. Don’t wait for a sensory level – Listen to the symptoms: a prospective Audit of the Delays in Diagnosis of Malignant Cord Compression. Clin Oncol 2002: 14: 472 -480 Metastatic Spinal Cord Compression: Diagnosis and Management of Patients at risk of or with Metastatic Spinal Cord compression. Nice Clinical Guidelines Nov 2008 L Allan et al, Suspected Malignant Spinal Cord Compression – improving time to diagnosis via a ‘hotline’: a prospective audit. British Journal of Cancer 2009, 100, 1867 -1872.
Thank you. Any Questions?