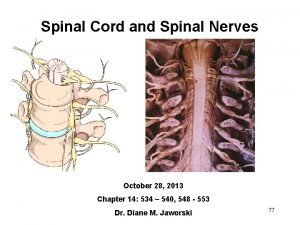
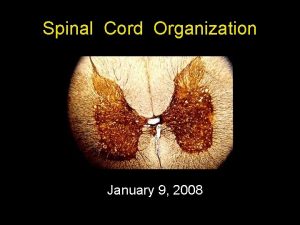
The Spinal Cord Structure of the spinal cord









- Slides: 82

The Spinal Cord Structure of the spinal cord v Tracts of the spinal cord v Spinal cord syndromes Nabeel Kouka, MD, DO, MBA www. brain 101. info
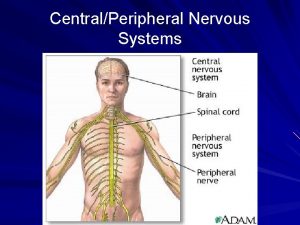
Spinal Cord - Comparable to Input-Output (IO) System of the Computer - Spinal Nerve (C 8, T 12, L 5, S 5, Cx 1) - Segmental Structure of Neural Tube Origin
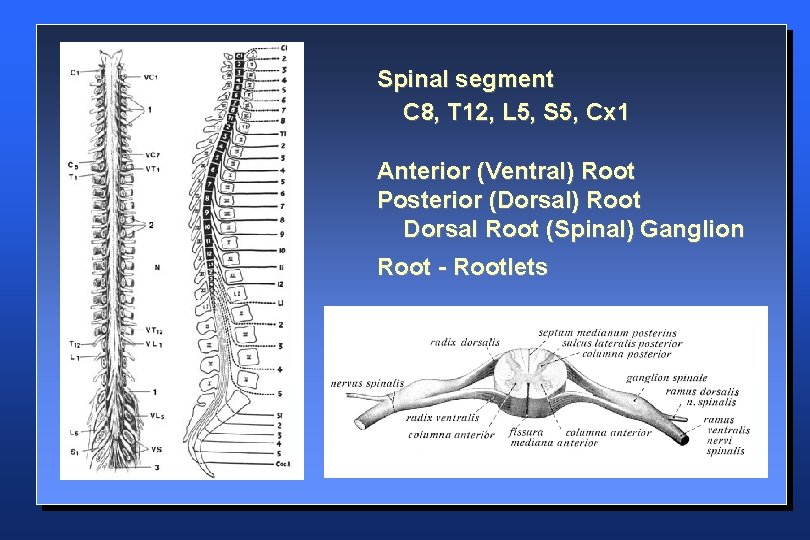
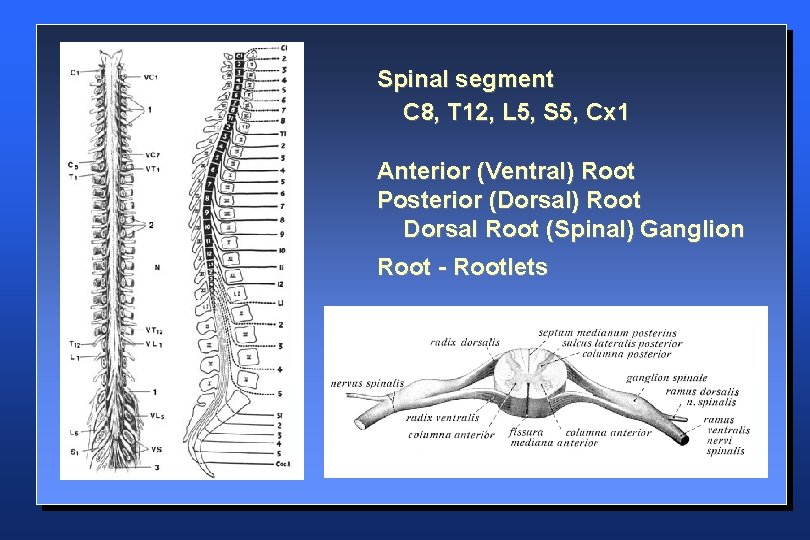
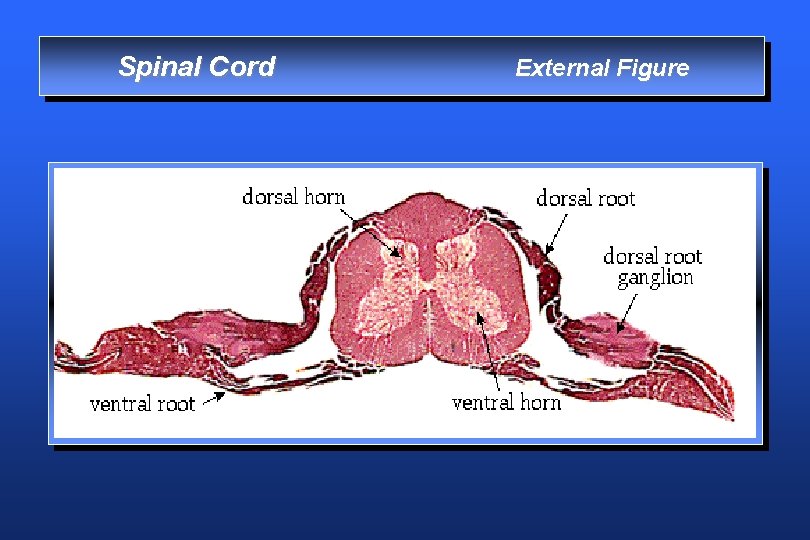
Spinal segment C 8, T 12, L 5, S 5, Cx 1 Anterior (Ventral) Root Posterior (Dorsal) Root Dorsal Root (Spinal) Ganglion Root - Rootlets
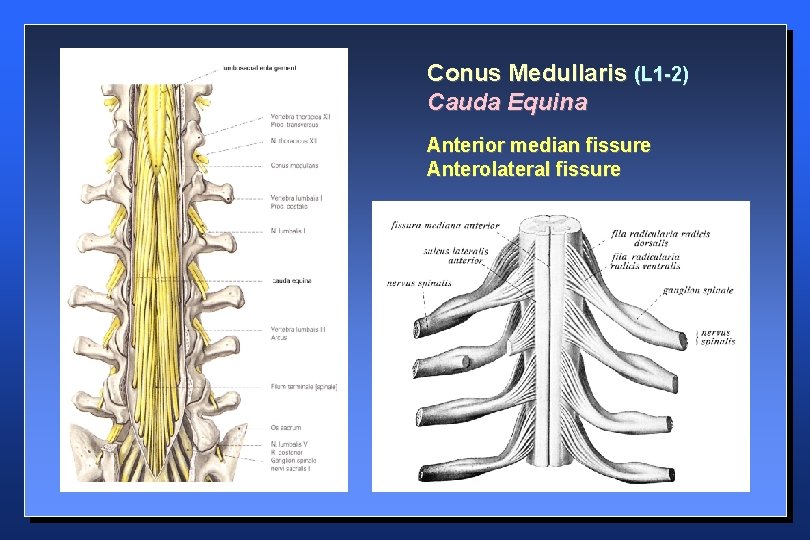
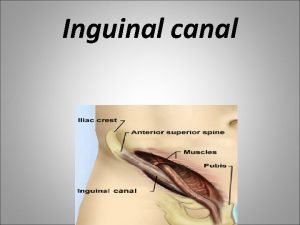
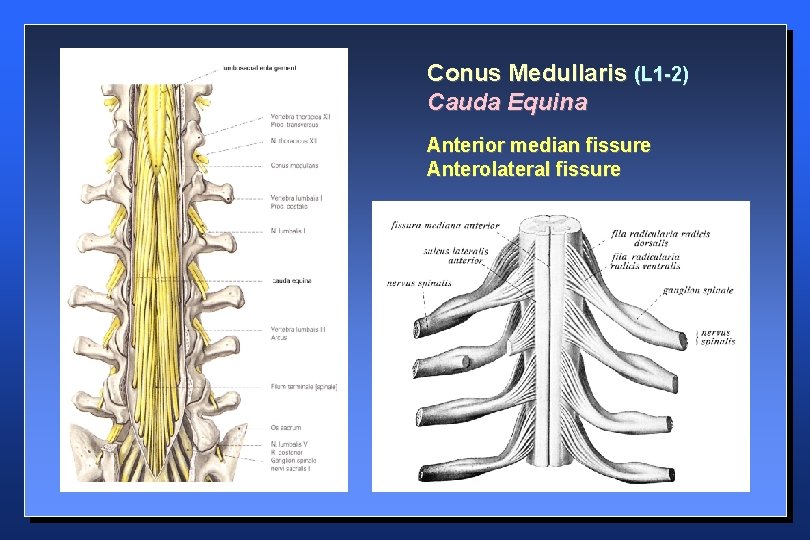
Conus Medullaris (L 1 -2) Cauda Equina Anterior median fissure Anterolateral fissure
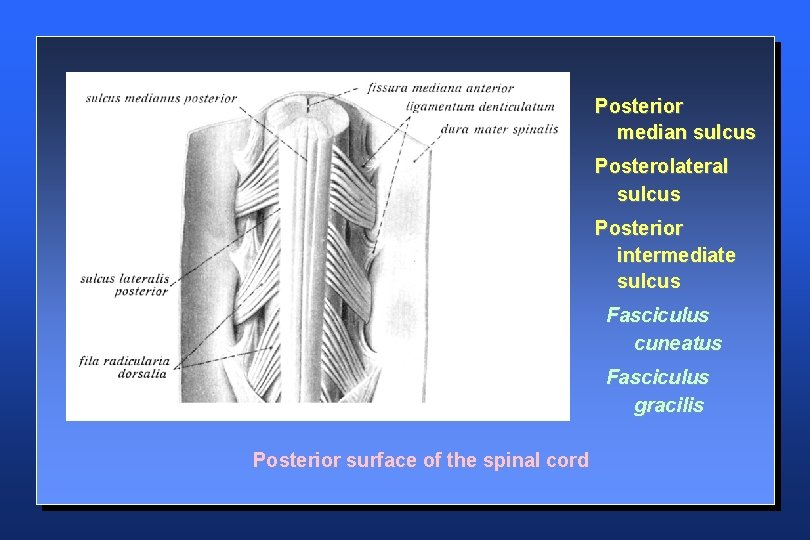
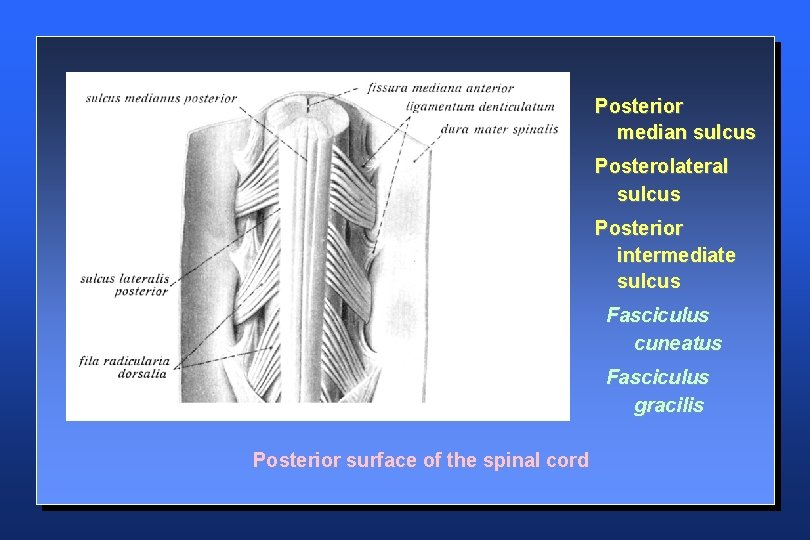
Posterior median sulcus Posterolateral sulcus Posterior intermediate sulcus Fasciculus cuneatus Fasciculus gracilis Posterior surface of the spinal cord
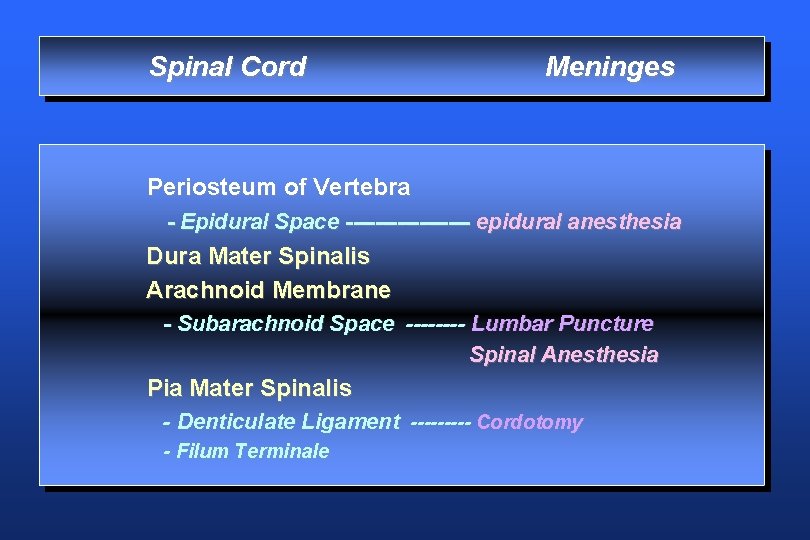
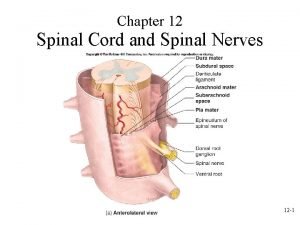
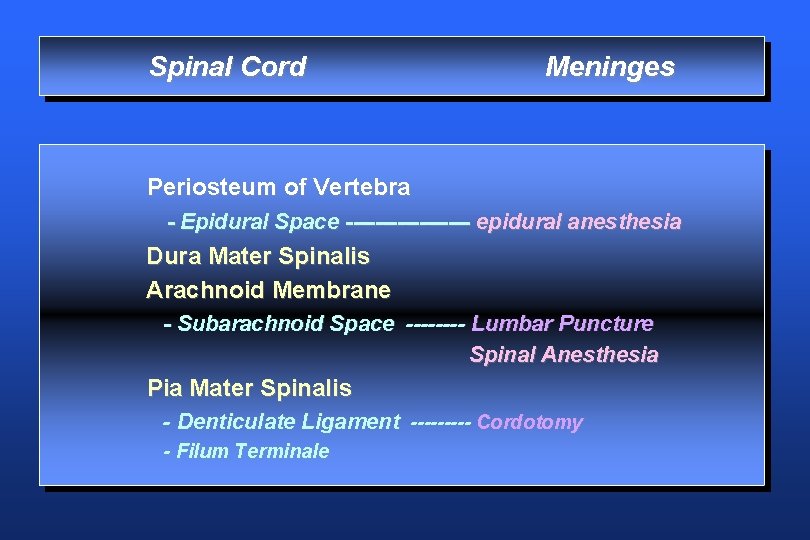
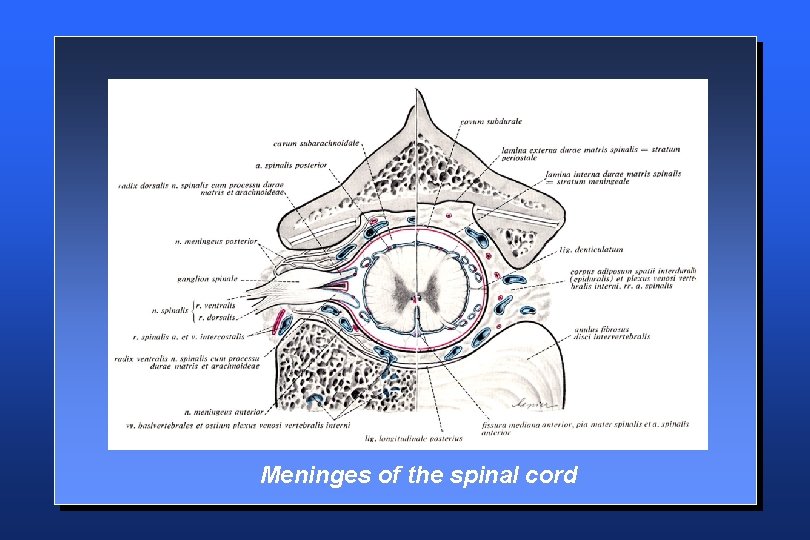
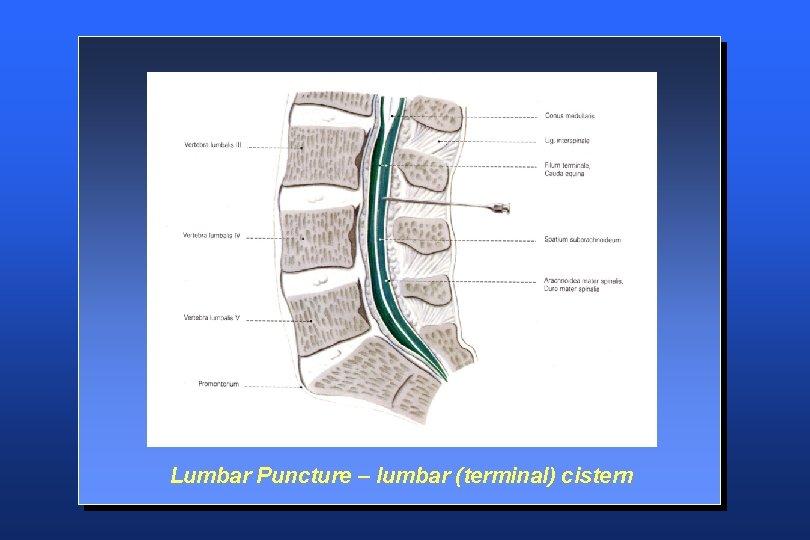
Spinal Cord Meninges Periosteum of Vertebra - Epidural Space --------- epidural anesthesia Dura Mater Spinalis Arachnoid Membrane - Subarachnoid Space ---- Lumbar Puncture Spinal Anesthesia Pia Mater Spinalis - Denticulate Ligament ----- Cordotomy - Filum Terminale
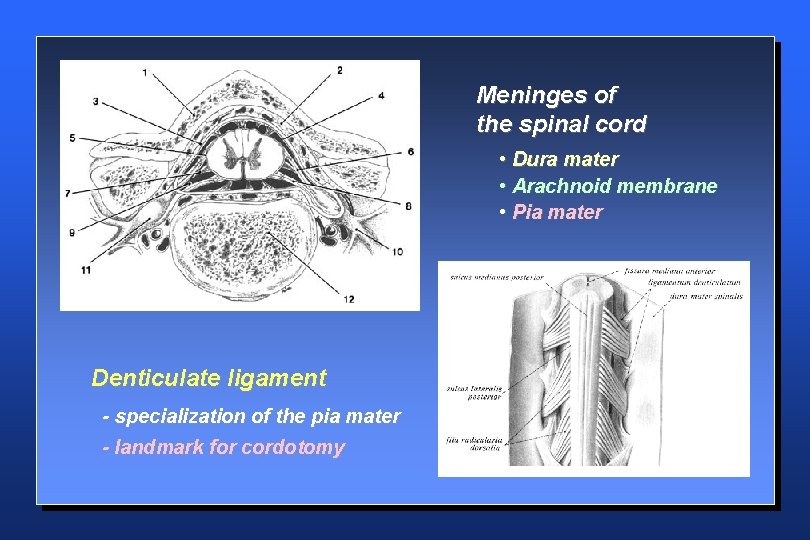
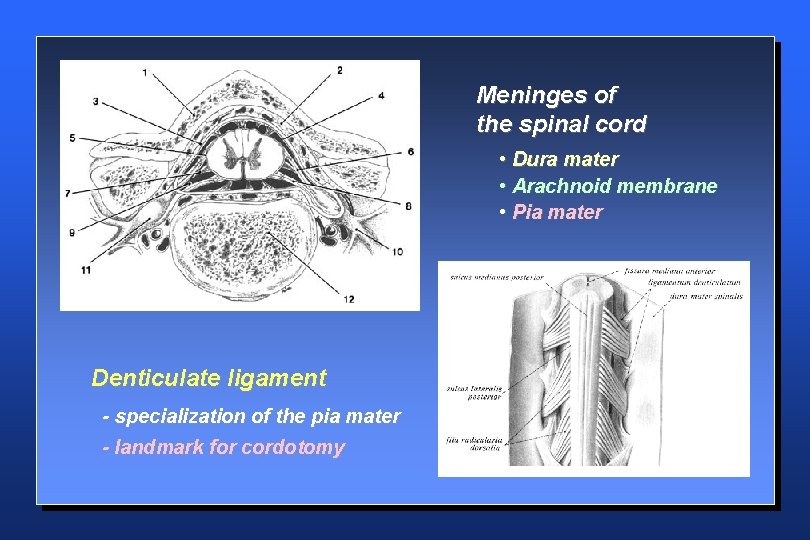
Meninges of the spinal cord • Dura mater • Arachnoid membrane • Pia mater Denticulate ligament - specialization of the pia mater - landmark for cordotomy
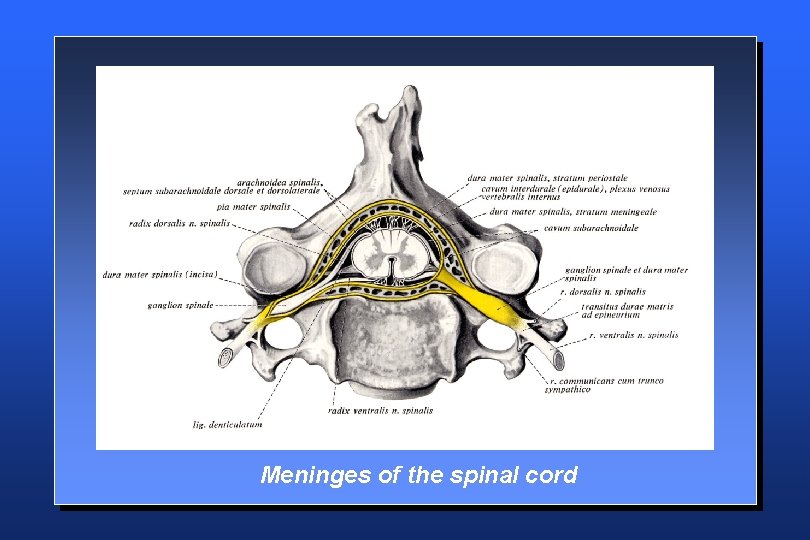
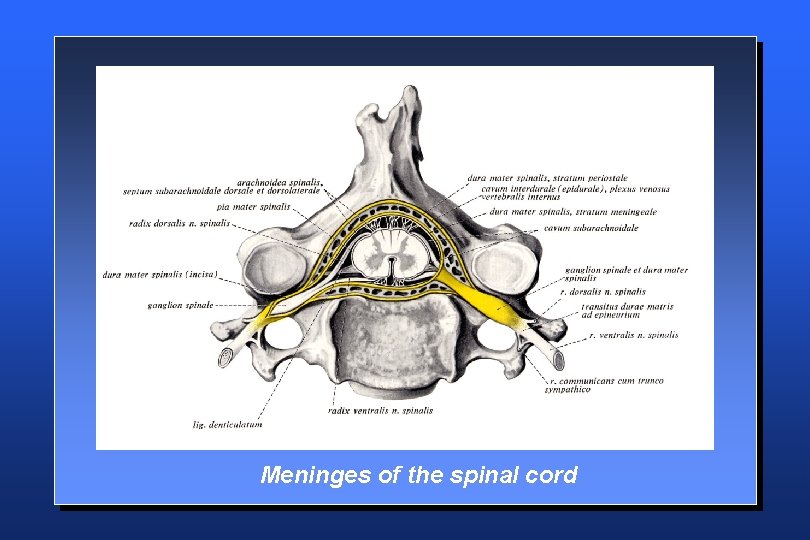
Meninges of the spinal cord
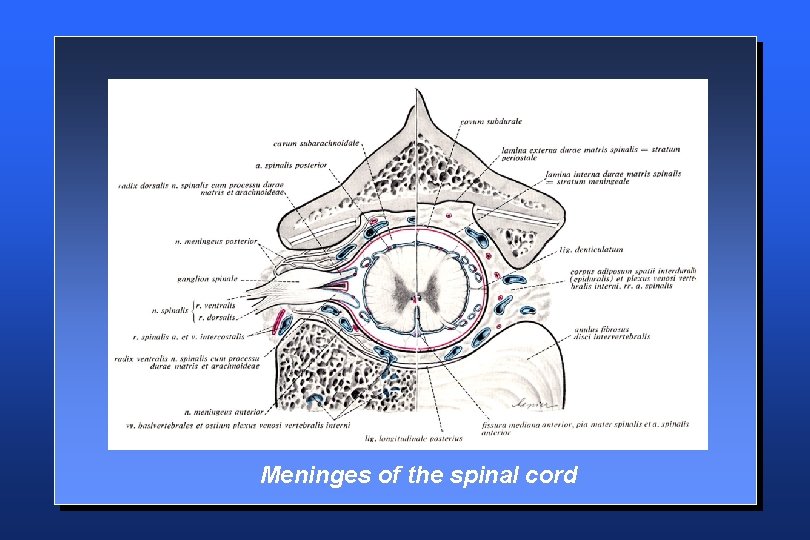
Meninges of the spinal cord
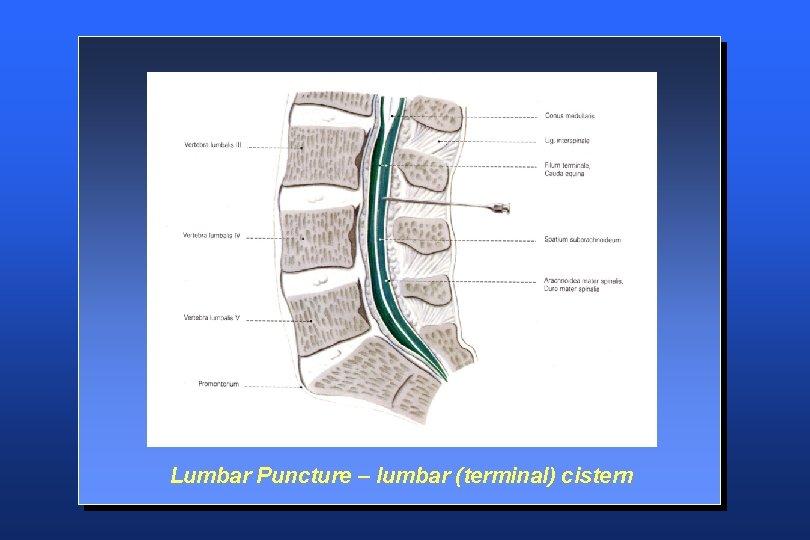
Lumbar Puncture – lumbar (terminal) cistern
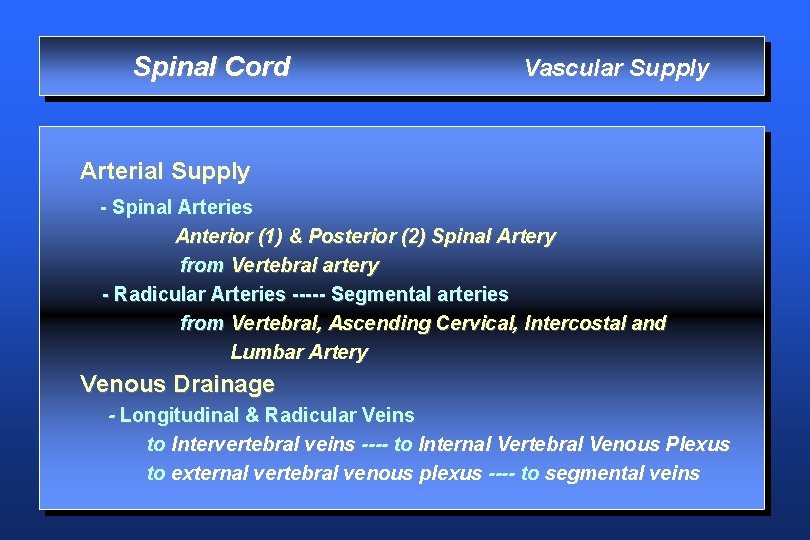
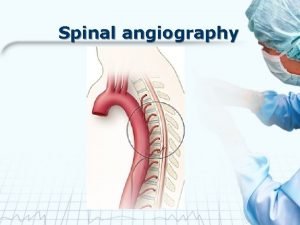
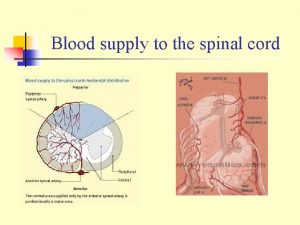
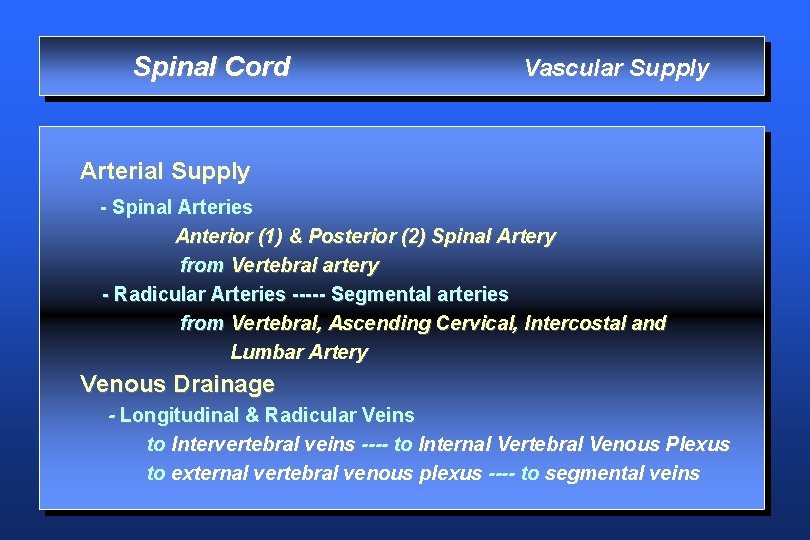
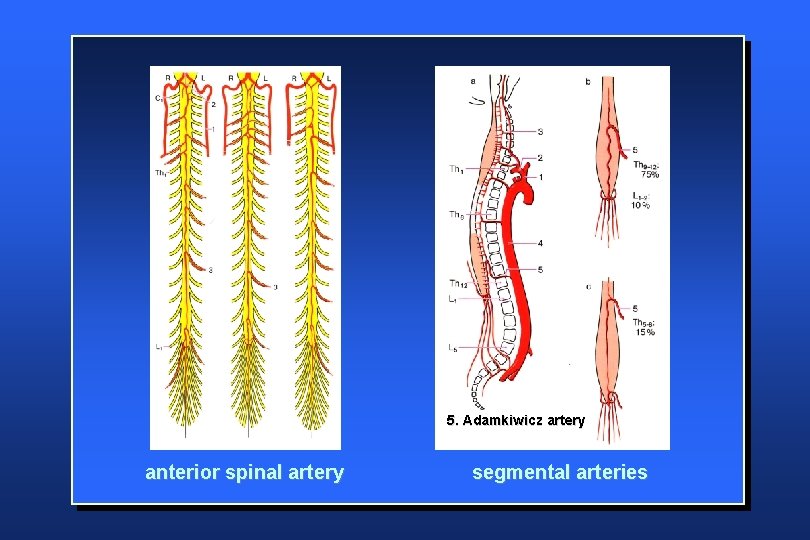
Spinal Cord Vascular Supply Arterial Supply - Spinal Arteries Anterior (1) & Posterior (2) Spinal Artery from Vertebral artery - Radicular Arteries ----- Segmental arteries from Vertebral, Ascending Cervical, Intercostal and Lumbar Artery Venous Drainage - Longitudinal & Radicular Veins to Intervertebral veins ---- to Internal Vertebral Venous Plexus to external vertebral venous plexus ---- to segmental veins
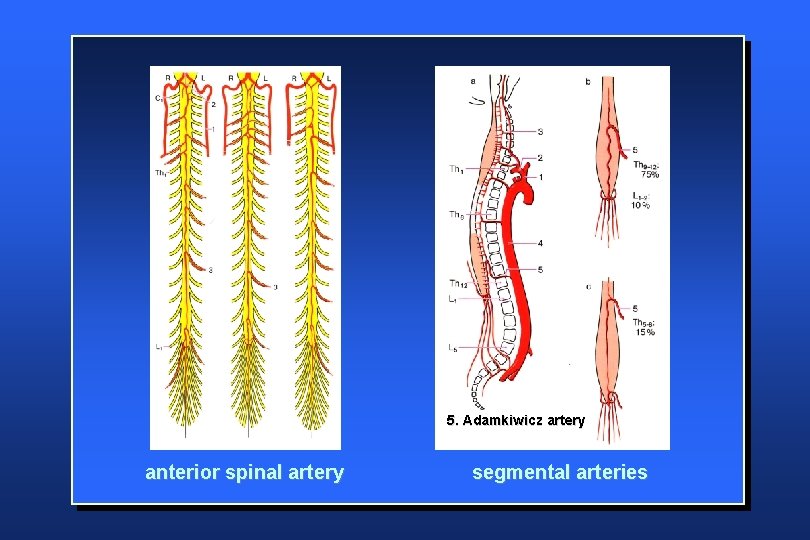
5. Adamkiwicz artery anterior spinal artery segmental arteries
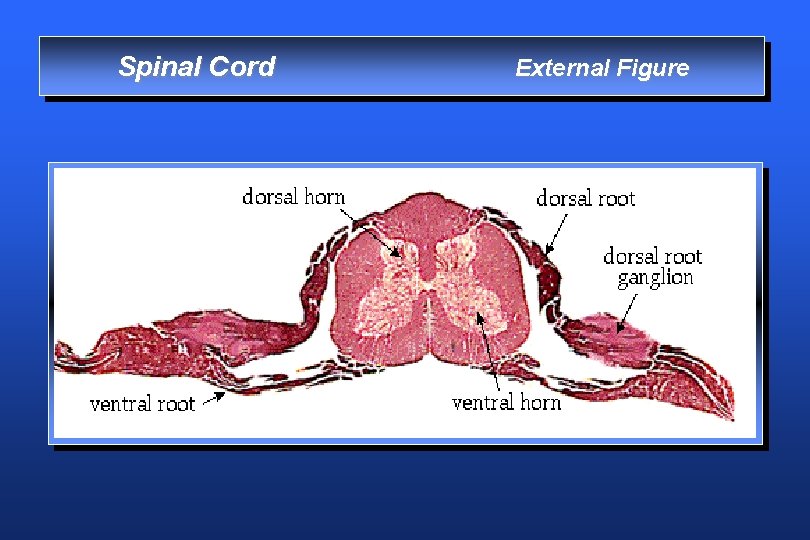
Spinal Cord External Figure
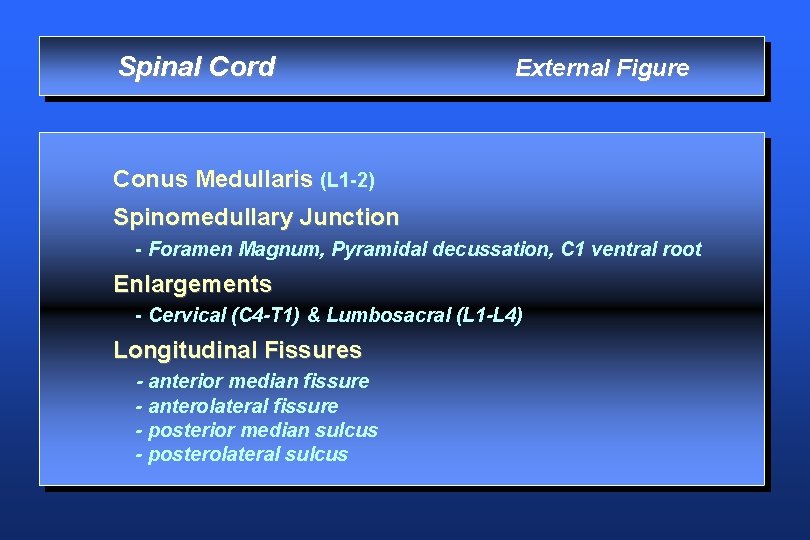
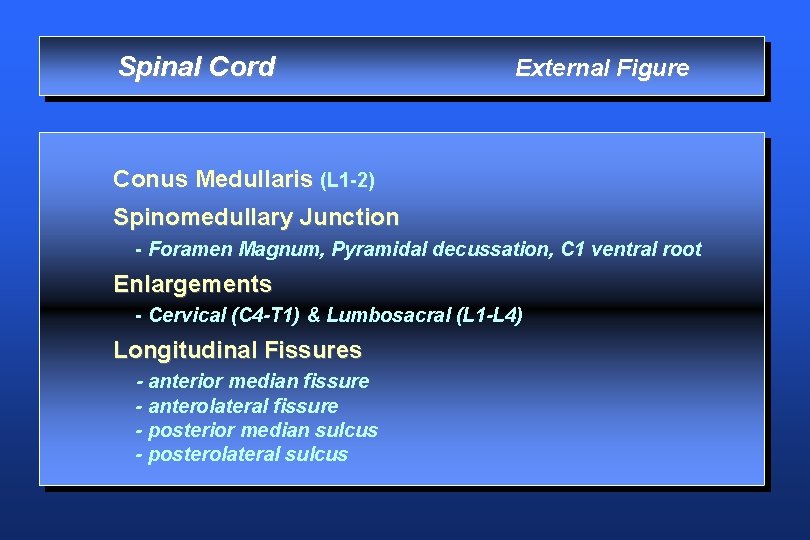
Spinal Cord External Figure Conus Medullaris (L 1 -2) Spinomedullary Junction - Foramen Magnum, Pyramidal decussation, C 1 ventral root Enlargements - Cervical (C 4 -T 1) & Lumbosacral (L 1 -L 4) Longitudinal Fissures - anterior median fissure - anterolateral fissure - posterior median sulcus - posterolateral sulcus
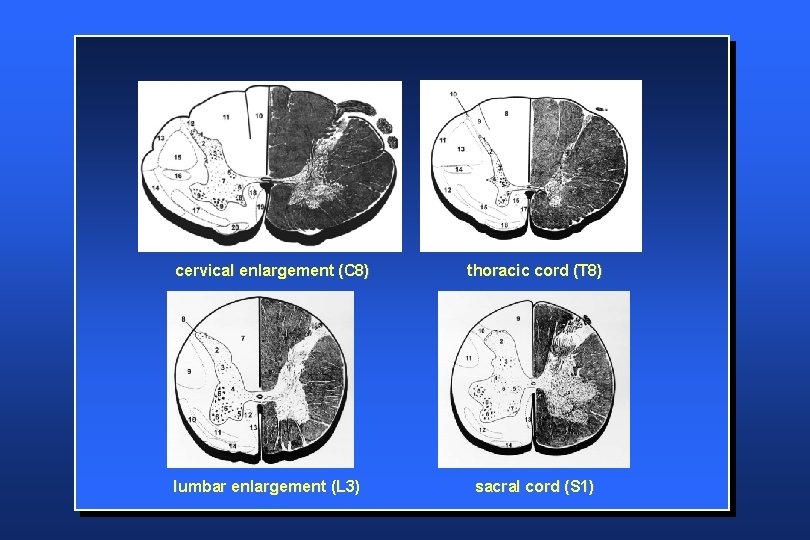
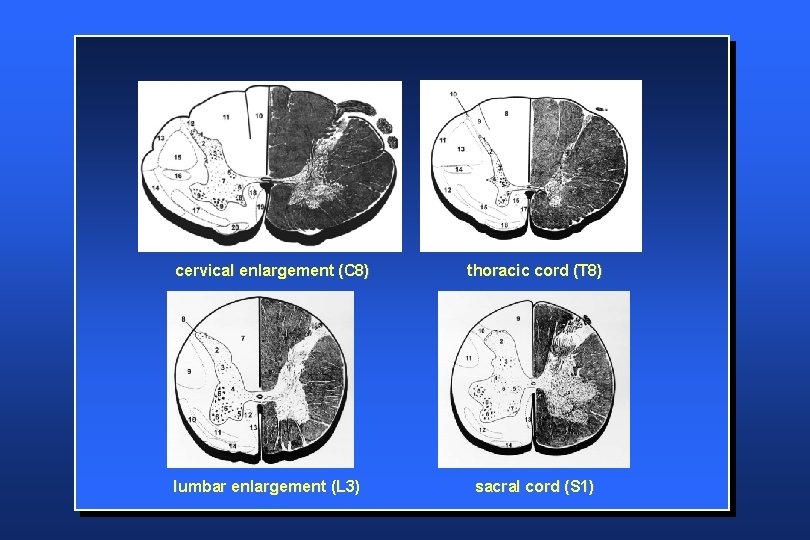
cervical enlargement (C 8) lumbar enlargement (L 3) thoracic cord (T 8) sacral cord (S 1)
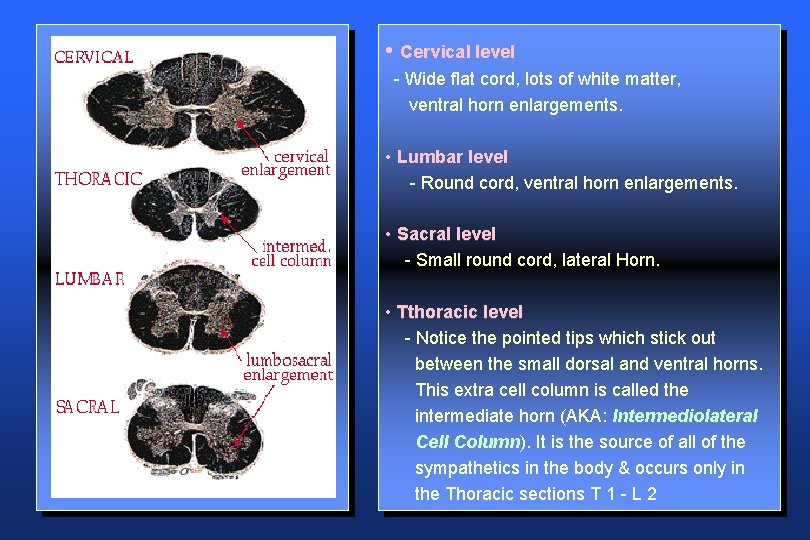
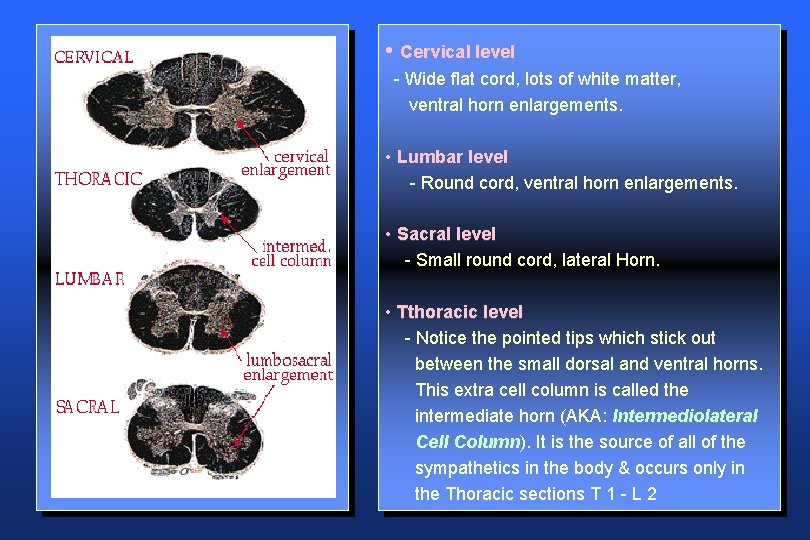
• Cervical level - Wide flat cord, lots of white matter, ventral horn enlargements. • Lumbar level - Round cord, ventral horn enlargements. • Sacral level - Small round cord, lateral Horn. • Tthoracic level - Notice the pointed tips which stick out between the small dorsal and ventral horns. This extra cell column is called the intermediate horn (AKA: Intermediolateral Cell Column). Column It is the source of all of the sympathetics in the body & occurs only in the Thoracic sections T 1 - L 2
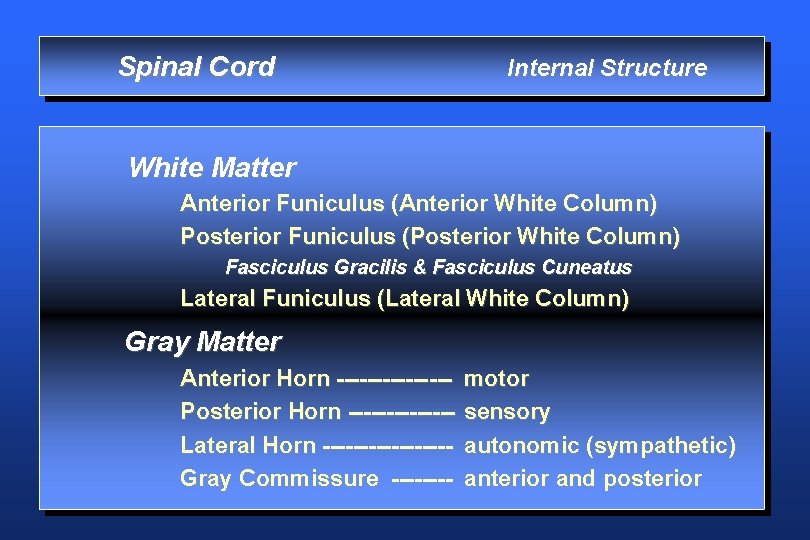
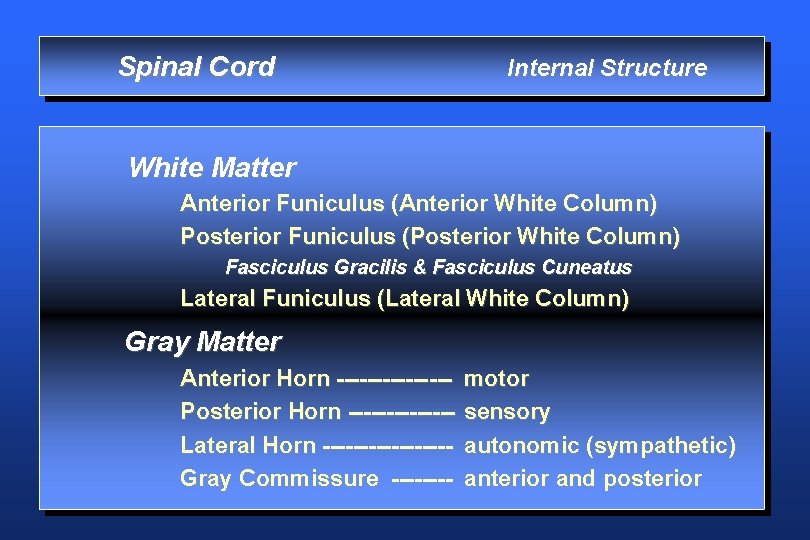
Spinal Cord Internal Structure White Matter Anterior Funiculus (Anterior White Column) Posterior Funiculus (Posterior White Column) Fasciculus Gracilis & Fasciculus Cuneatus Lateral Funiculus (Lateral White Column) Gray Matter Anterior Horn ------ --Posterior Horn -------Lateral Horn --------Gray Commissure ---- motor sensory autonomic (sympathetic) anterior and posterior
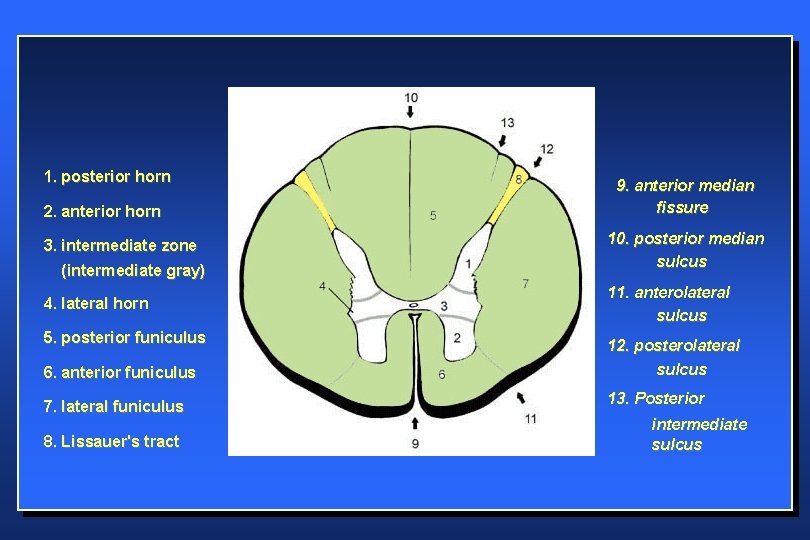
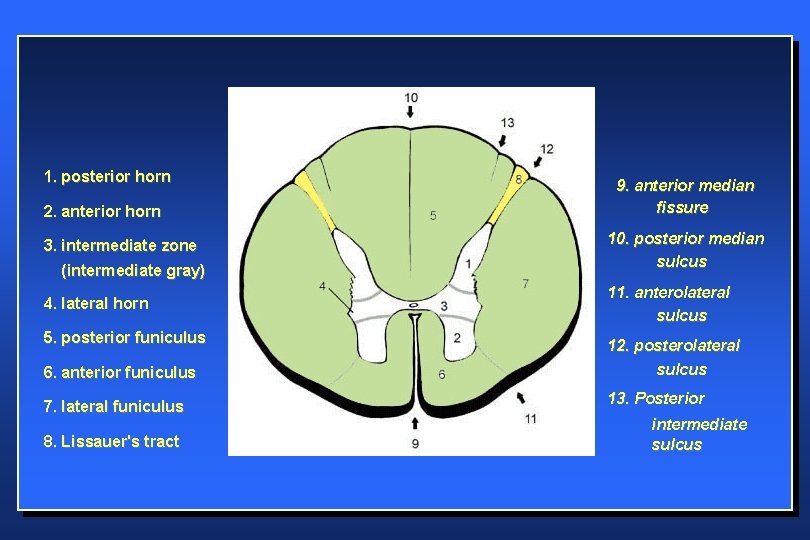
1. posterior horn 2. anterior horn 3. intermediate zone (intermediate gray) 4. lateral horn 5. posterior funiculus 6. anterior funiculus 7. lateral funiculus 8. Lissauer's tract 9. anterior median fissure 10. posterior median sulcus 11. anterolateral sulcus 12. posterolateral sulcus 13. Posterior intermediate sulcus
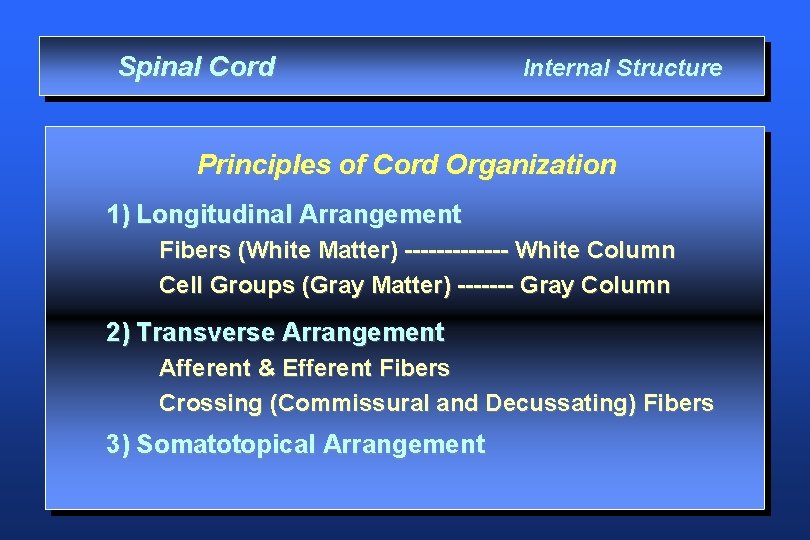
Spinal Cord Internal Structure Principles of Cord Organization 1) Longitudinal Arrangement Fibers (White Matter) ------- White Column Cell Groups (Gray Matter) ------- Gray Column 2) Transverse Arrangement Afferent & Efferent Fibers Crossing (Commissural and Decussating) Fibers 3) Somatotopical Arrangement
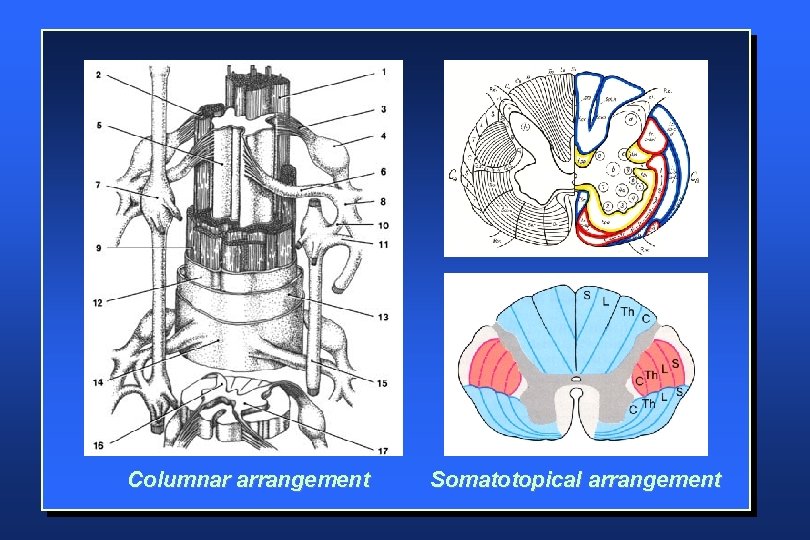
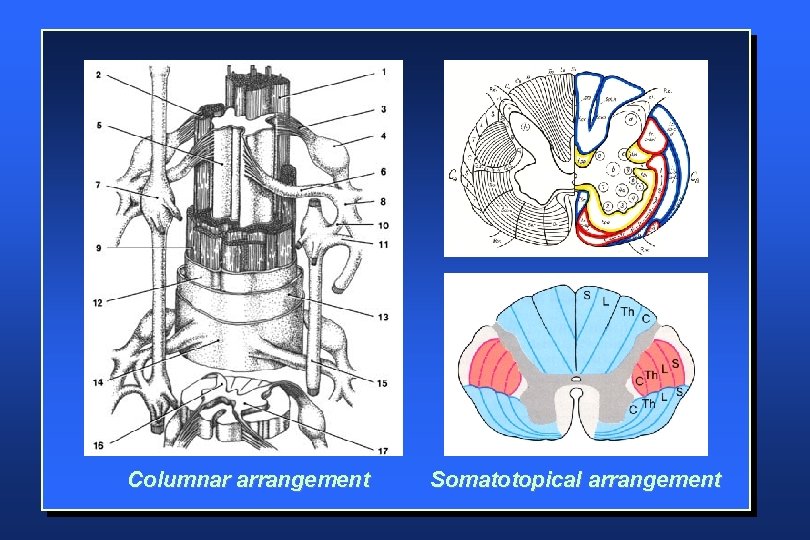
Columnar arrangement Somatotopical arrangement
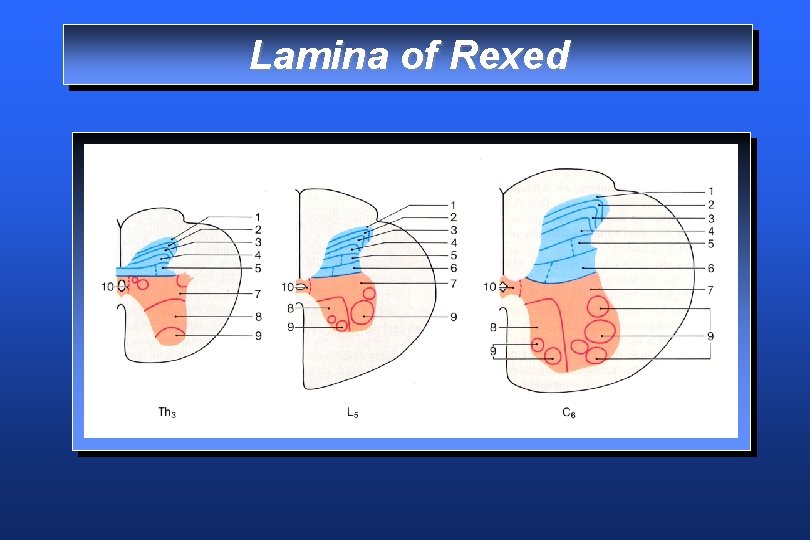
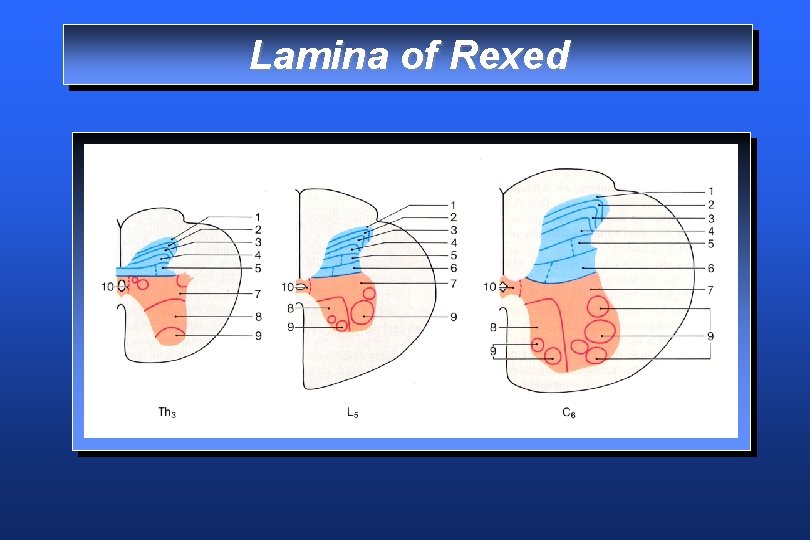
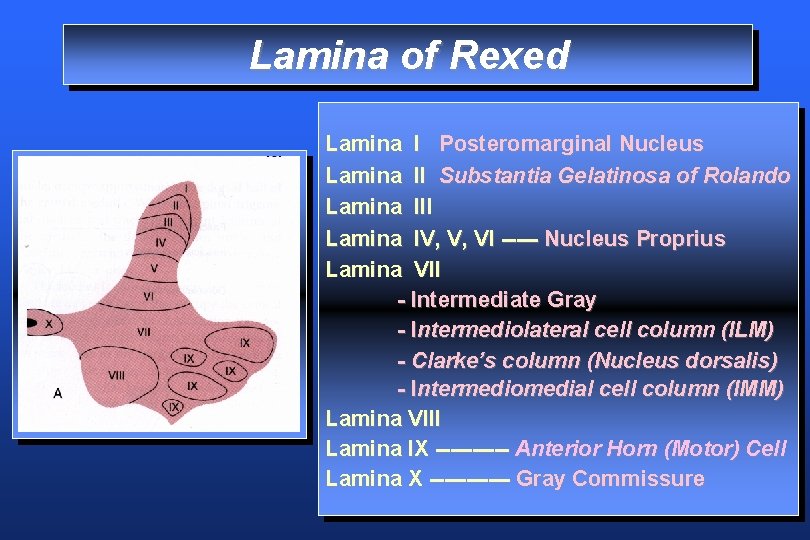
Lamina of Rexed
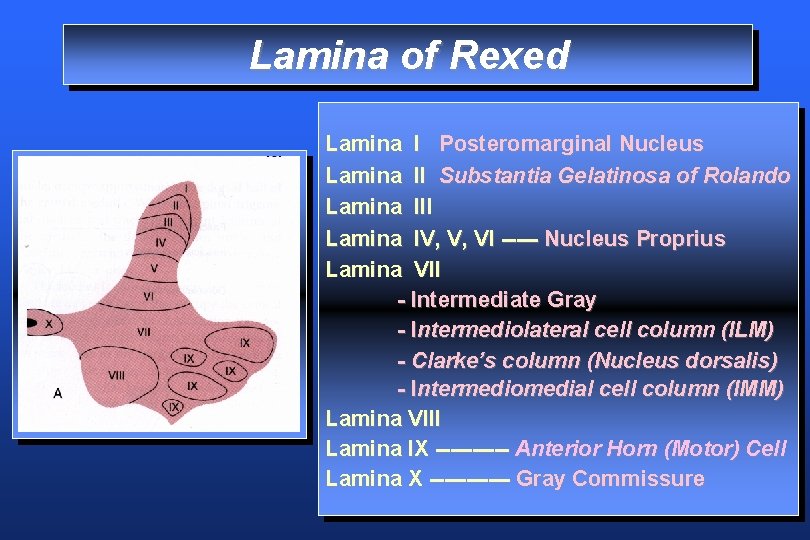
Lamina of Rexed Lamina I Posteromarginal Nucleus Lamina II Substantia Gelatinosa of Rolando Lamina III Lamina IV, V, VI ----- Nucleus Proprius Lamina VII - Intermediate Gray - Intermediolateral cell column (ILM) - Clarke’s column (Nucleus dorsalis) - Intermediomedial cell column (IMM) Lamina VIII Lamina IX ----- Anterior Horn (Motor) Cell Lamina X ------ Gray Commissure
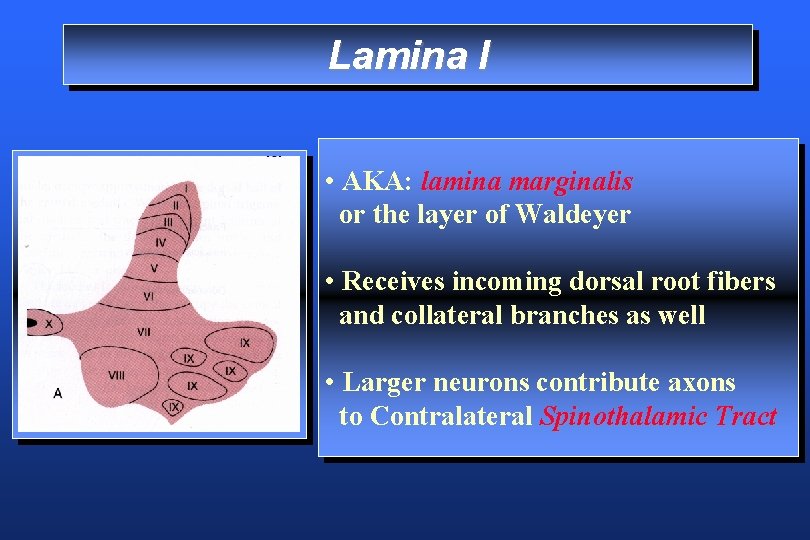
Lamina I • AKA: lamina marginalis or the layer of Waldeyer • Receives incoming dorsal root fibers and collateral branches as well • Larger neurons contribute axons to Contralateral Spinothalamic Tract
Lamina II • AKA: Substantia Gelatinosa • Involved in Pain interpretation • Receives incoming input from dorsal root axons & descending input from reticular formation of the medulla • Efferent axons travel up & down several segments to make contact with other areas of the dorsal horn
Lamina III • Contains larger, less densely packed cells than lamina II • Receives primary afferents from dorsal root fibers • Neurons considered as a part of nucleus proprius
Lamina IV • Contains a variety of cell types that have more myelin than any other lamina • Some tract cells originate here, axons cross the midline and enter the contralateral Spinothalamic Tract, Tract also sends contacts to layers II and III • Receives afferents from dorsal roots via the dorsal funiculus • At rostral end of spinal cord, laminas I-IV become continuous with the spinal trigeminal nucleus
Lamina V - VI • Origination of tract cells, cells similar to lamina IV, these tracts cells are also known as the Nucleus Proprius (e. g. spinal thalamic tract or anterolateral system; system pain and temperature, some tactile) • Receives afferent input from dorsal roots and descending fibers, most importantly Corticospinal
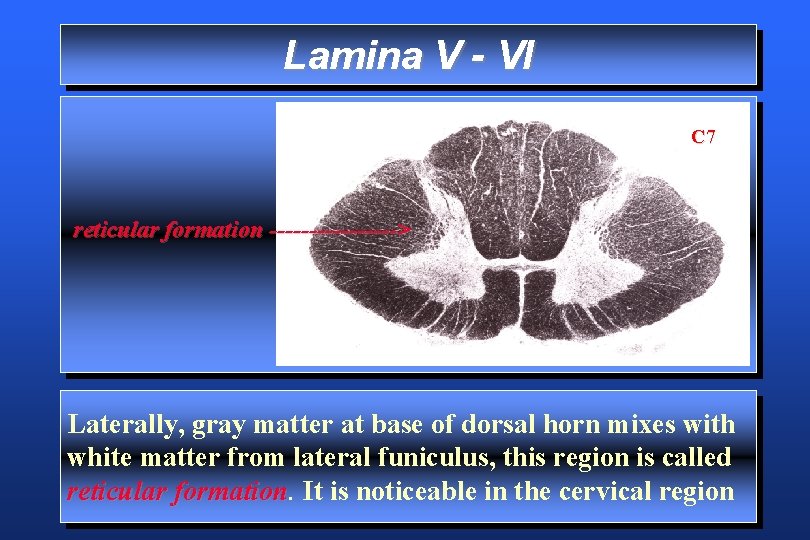
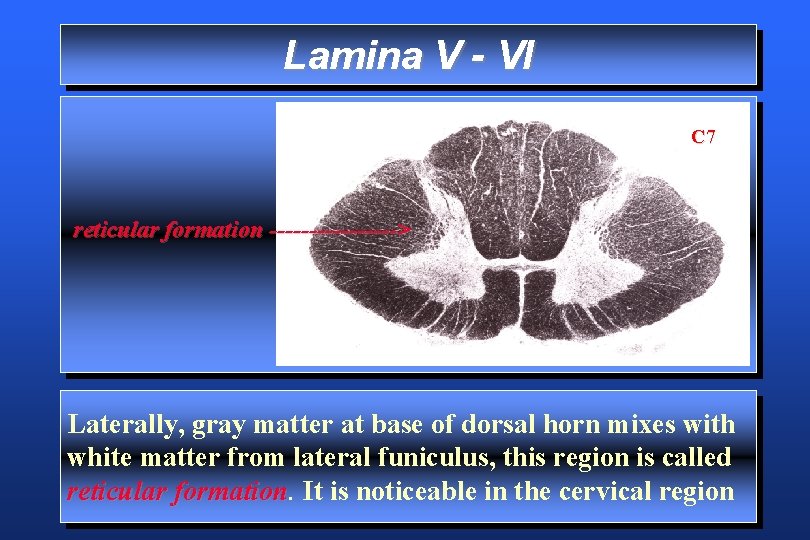
Lamina V - VI C 7 reticular formation --------> Laterally, gray matter at base of dorsal horn mixes with white matter from lateral funiculus, this region is called reticular formation It is noticeable in the cervical region
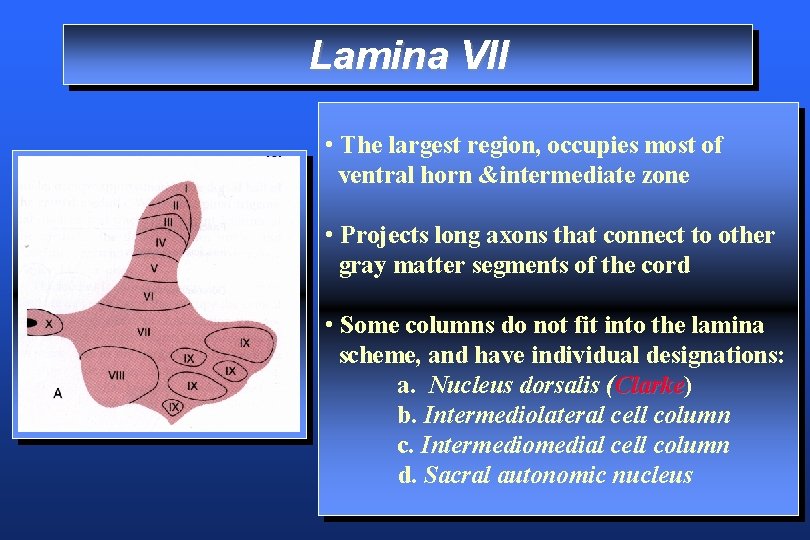
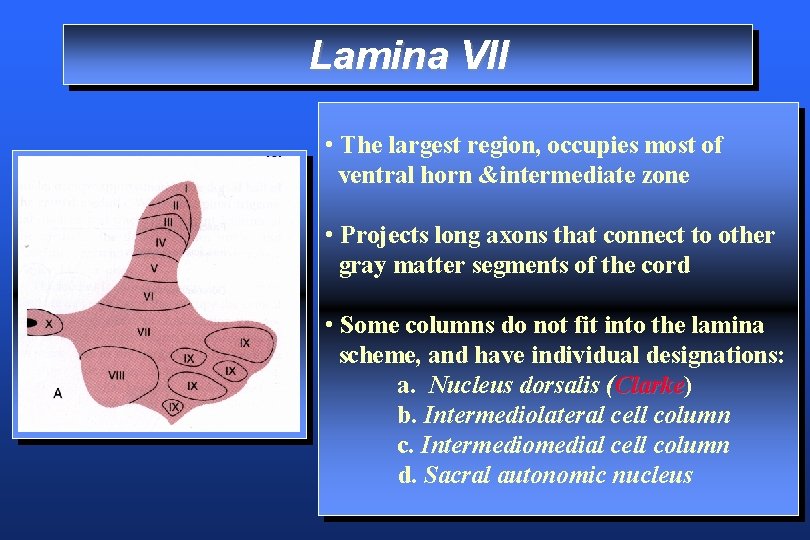
Lamina VII • The largest region, occupies most of ventral horn &intermediate zone • Projects long axons that connect to other gray matter segments of the cord • Some columns do not fit into the lamina scheme, and have individual designations: a. Nucleus dorsalis (Clarke) Clarke b. Intermediolateral cell column c. Intermediomedial cell column d. Sacral autonomic nucleus
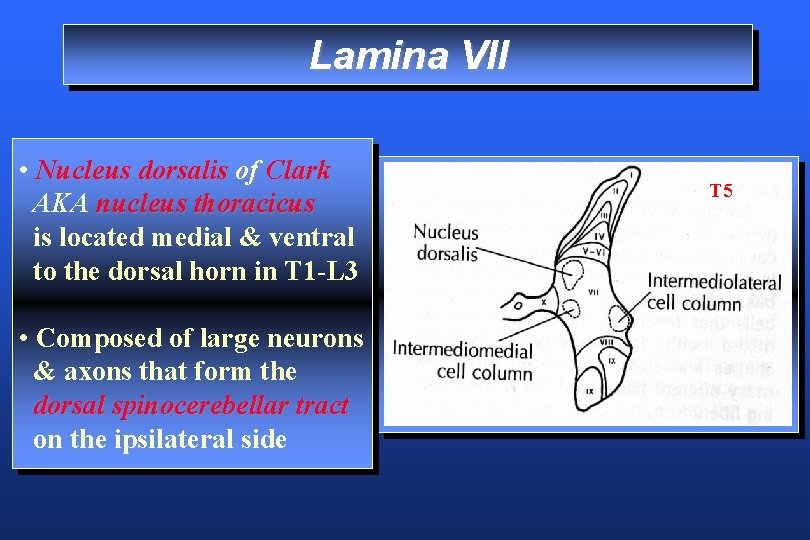
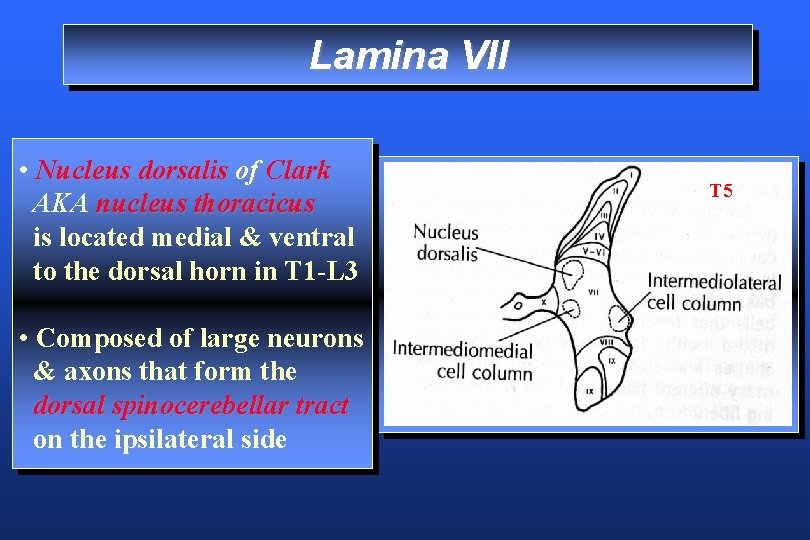
Lamina VII • Nucleus dorsalis of Clark AKA nucleus thoracicus is located medial & ventral to the dorsal horn in T 1 -L 3 • Composed of large neurons & axons that form the dorsal spinocerebellar tract on the ipsilateral side T 5
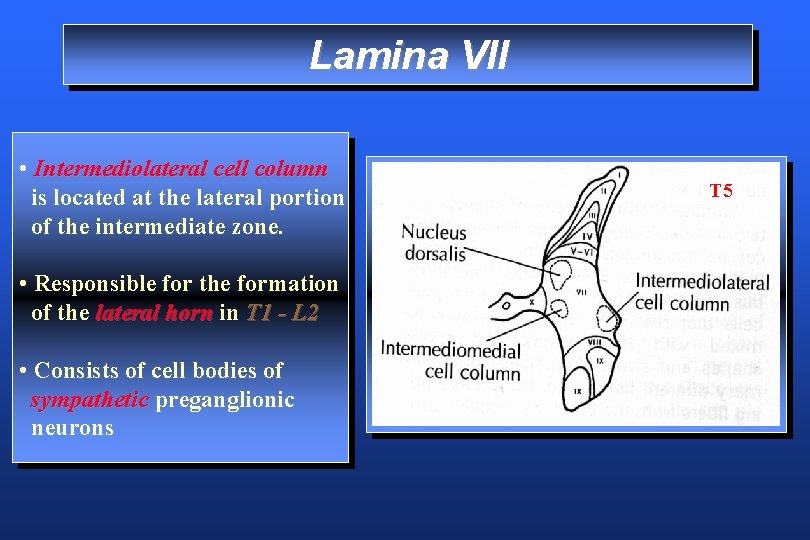
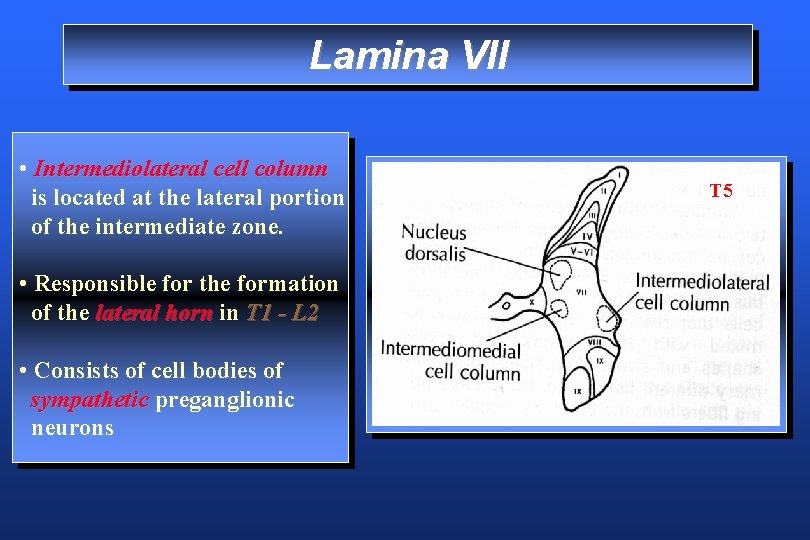
Lamina VII • Intermediolateral cell column is located at the lateral portion of the intermediate zone. • Responsible for the formation of the lateral horn in T 1 - L 2 • Consists of cell bodies of sympathetic preganglionic neurons T 5
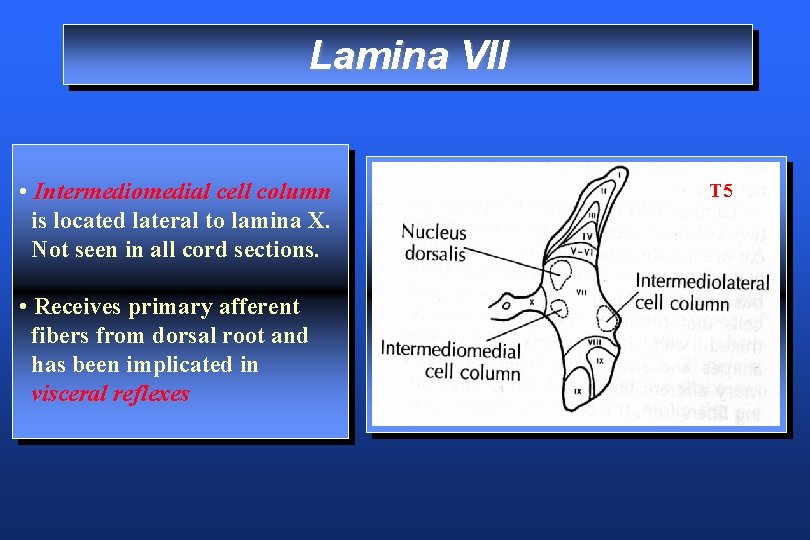
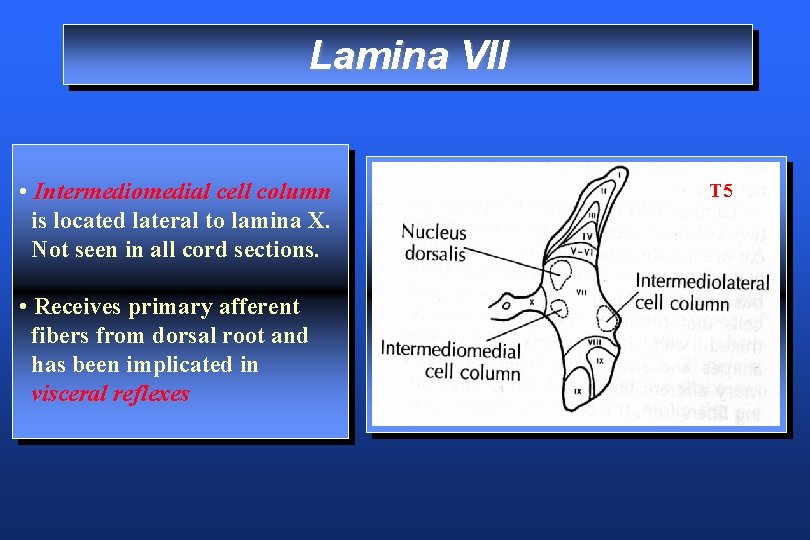
Lamina VII • Intermediomedial cell column is located lateral to lamina X. Not seen in all cord sections. • Receives primary afferent fibers from dorsal root and has been implicated in visceral reflexes T 5
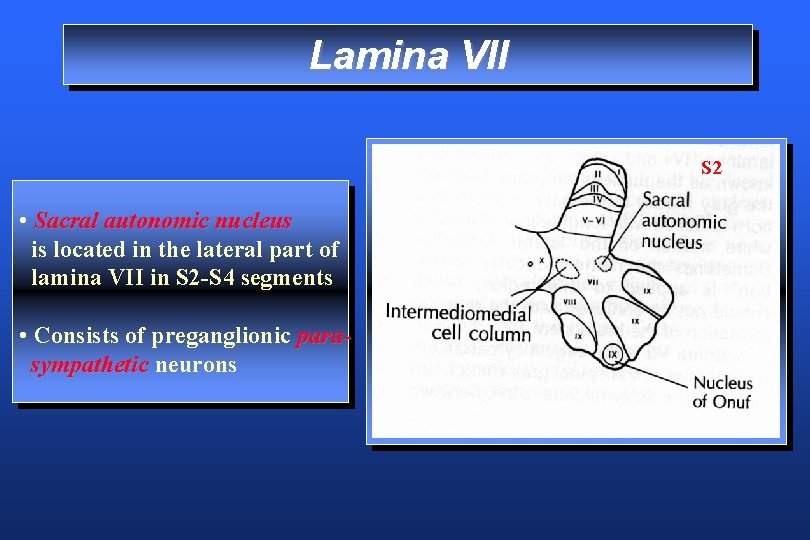
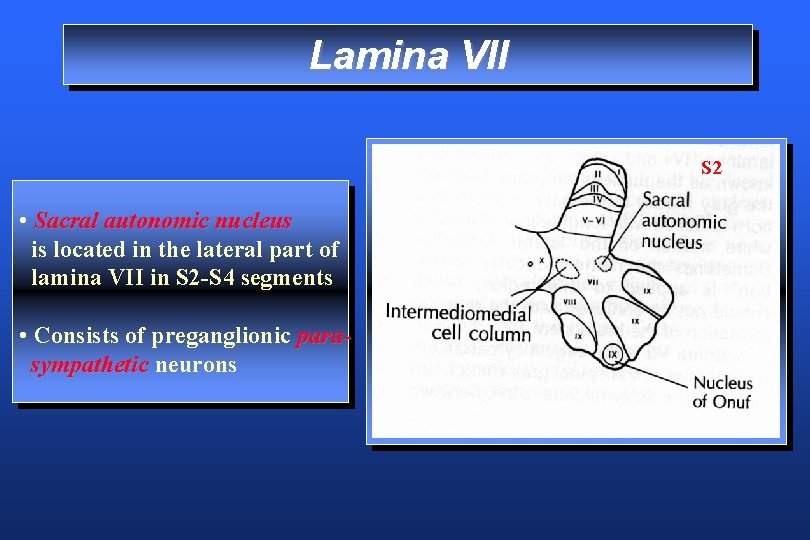
Lamina VII S 2 • Sacral autonomic nucleus is located in the lateral part of lamina VII in S 2 -S 4 segments • Consists of preganglionic parasympathetic neurons
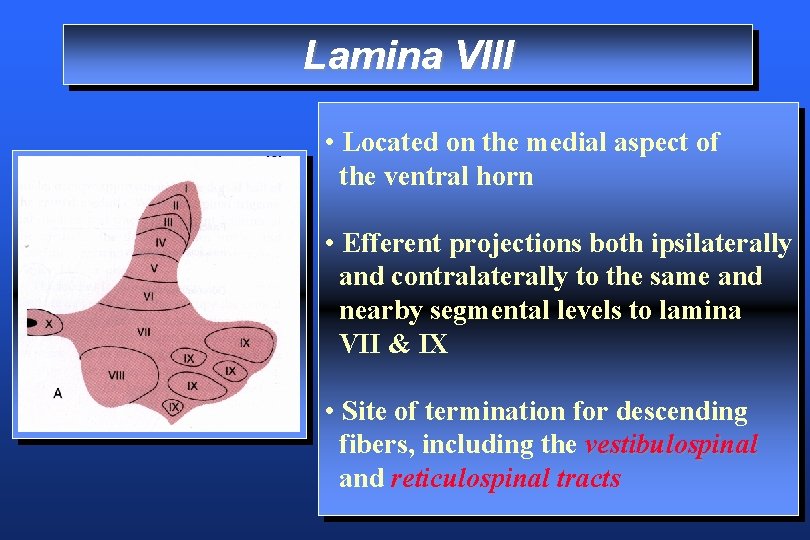
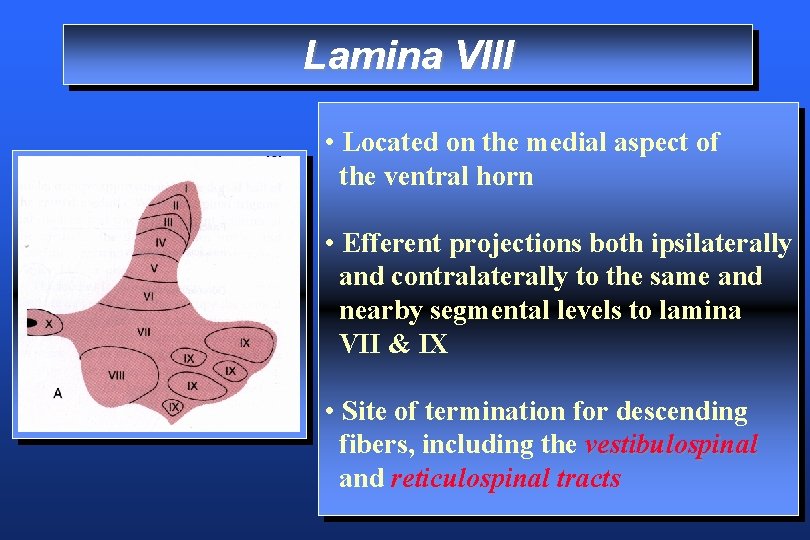
Lamina VIII • Located on the medial aspect of the ventral horn • Efferent projections both ipsilaterally and contralaterally to the same and nearby segmental levels to lamina VII & IX • Site of termination for descending fibers, including the vestibulospinal and reticulospinal tracts
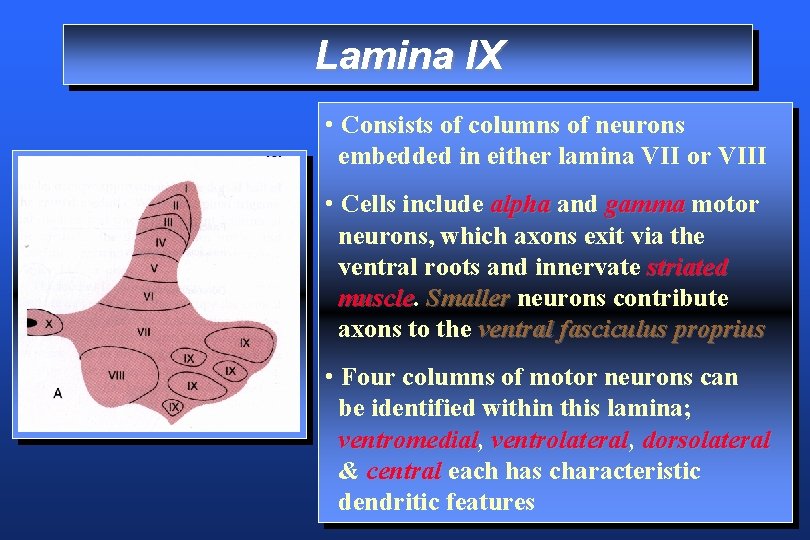
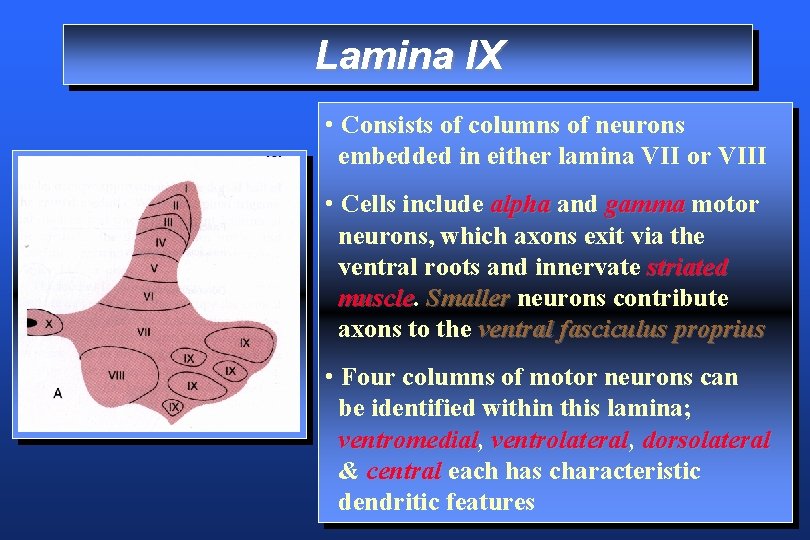
Lamina IX • Consists of columns of neurons embedded in either lamina VII or VIII • Cells include alpha and gamma motor neurons, which axons exit via the ventral roots and innervate striated muscle Smaller neurons contribute axons to the ventral fasciculus proprius • Four columns of motor neurons can be identified within this lamina; ventromedial, ventromedial ventrolateral, ventrolateral dorsolateral & central each has characteristic dendritic features
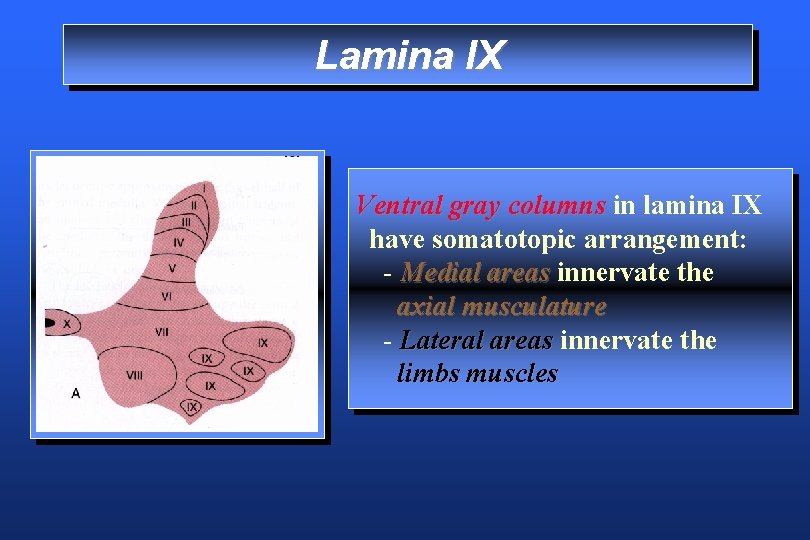
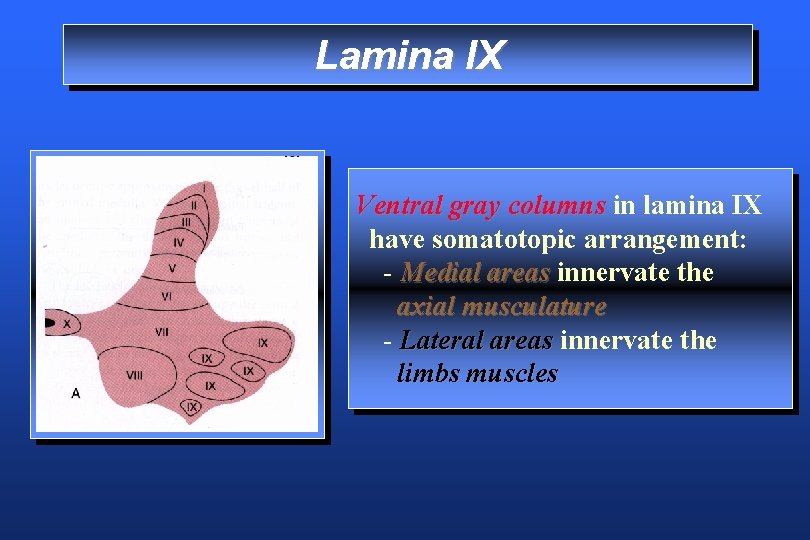
Lamina IX Ventral gray columns in lamina IX have somatotopic arrangement: - Medial areas innervate the axial musculature - Lateral areas innervate the limbs muscles
PHRENIC NUCLEUS The phrenic nucleus is located in the ventromedial area of the ventral horn in C 2 -C 5 segments. It receives bilateral innervation from the solitary nucleus of the medullary region, via solitary tract. This nucleus is responsible for the innervation of the diaphragm SPINAL ACCESSORY NUCLEUS The spinal accessory nucleus (cranial nerve XI) is located in the lateral area of vental horn in C 1 -C 5 segments. Corticospinal tract innervates this nucleus bilaterally. This nucleus is also responsible for the innervation of the trapezius & sternocleidomastoid muscles (ipsilaterally)
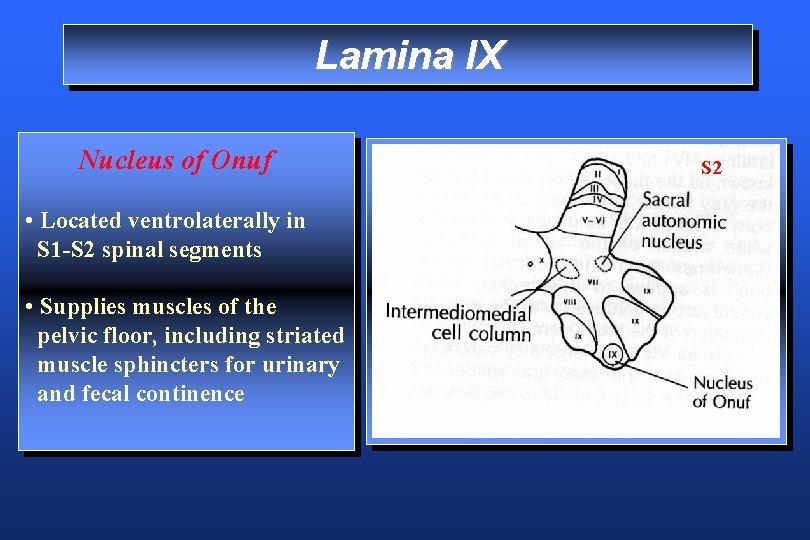
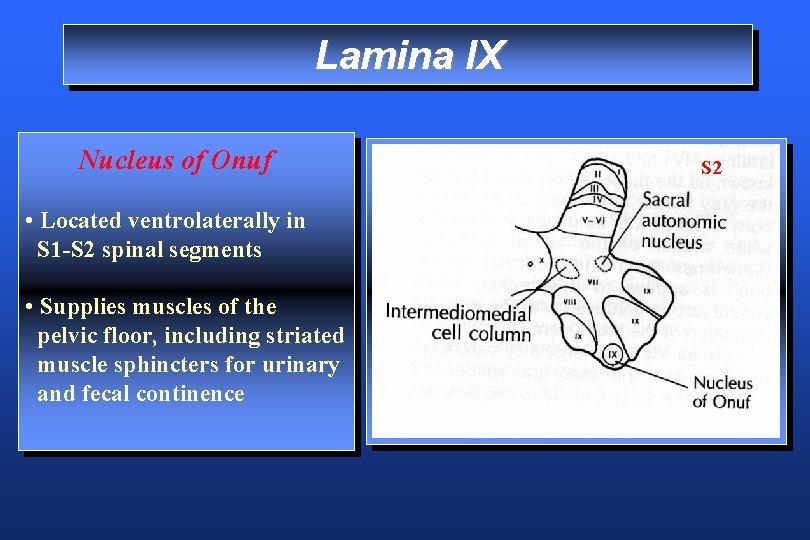
Lamina IX Nucleus of Onuf • Located ventrolaterally in S 1 -S 2 spinal segments • Supplies muscles of the pelvic floor, including striated muscle sphincters for urinary and fecal continence S 2
Lamina X • Surrounds the central canal, canal and includes the ventral gray commissure • Contains relatively small neurons, neurons radial neuroglia cells & decussating axons • Some dorsal root afferents terminate here
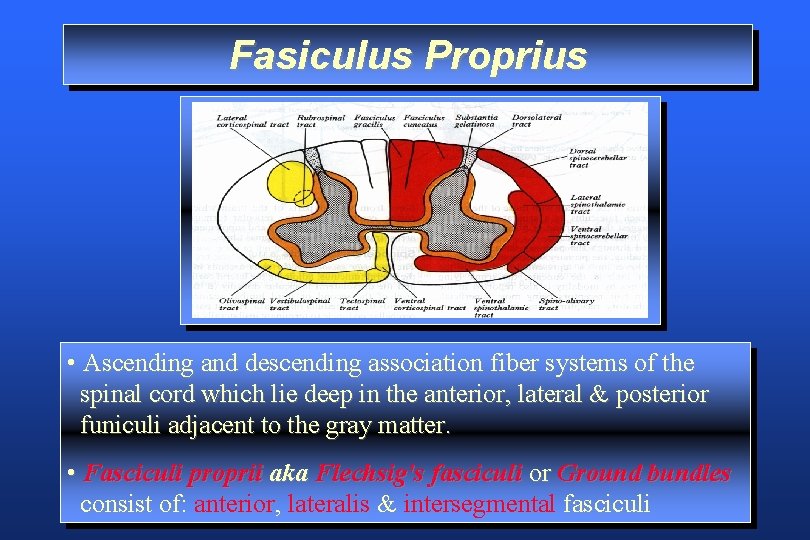
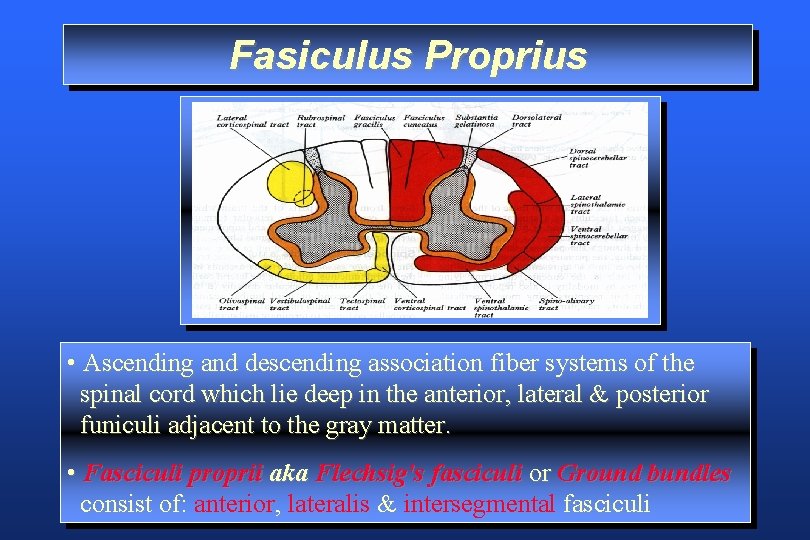
Fasiculus Proprius • Ascending and descending association fiber systems of the spinal cord which lie deep in the anterior, lateral & posterior funiculi adjacent to the gray matter. • Fasciculi proprii aka Flechsig's fasciculi or Ground bundles consist of: anterior, lateralis & intersegmental fasciculi
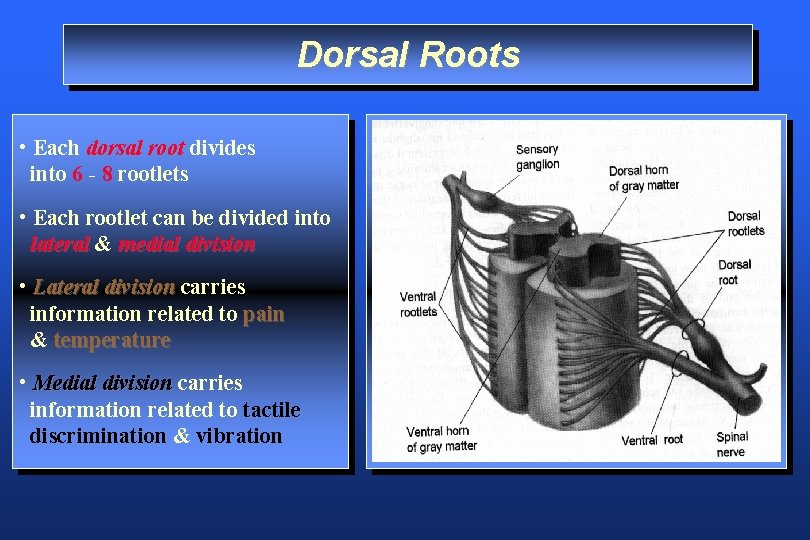
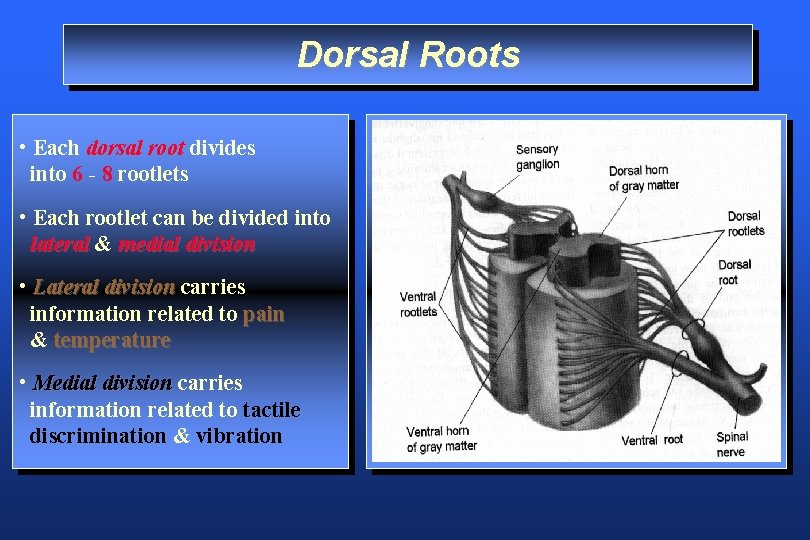
Dorsal Roots • Each dorsal root divides into 6 - 8 rootlets • Each rootlet can be divided into lateral & medial division • Lateral division carries information related to pain & temperature • Medial division carries information related to tactile discrimination & vibration
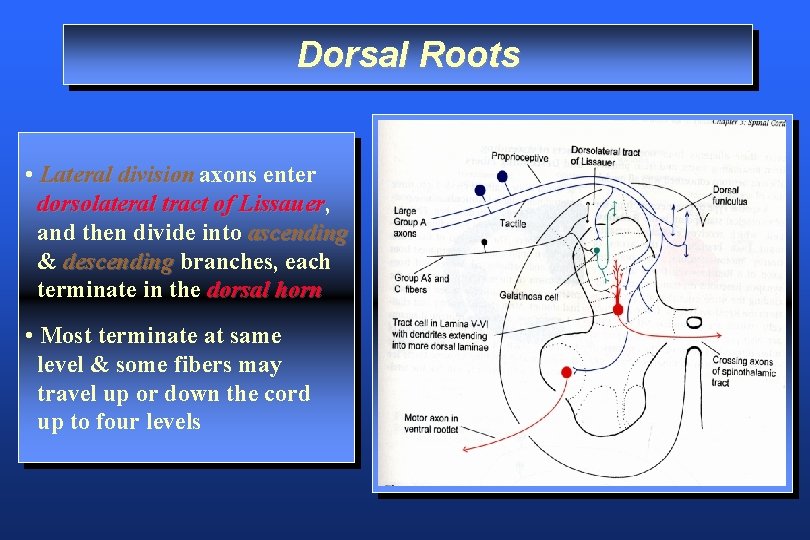
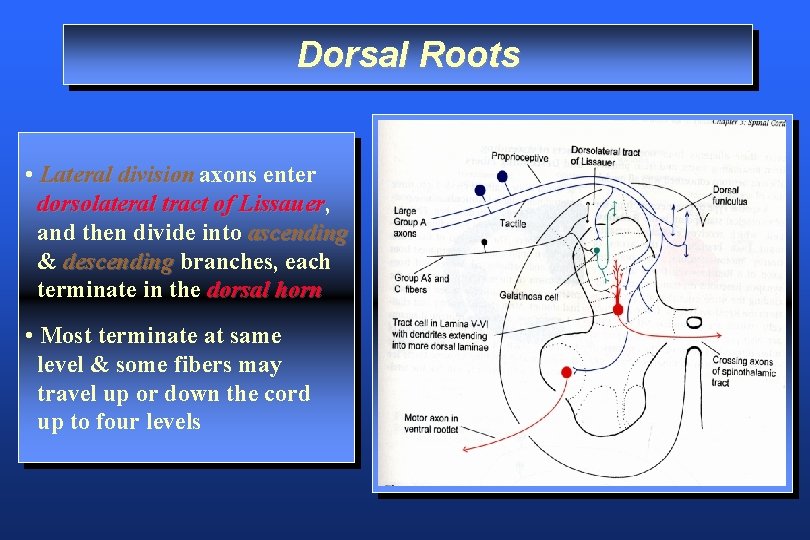
Dorsal Roots • Lateral division axons enter dorsolateral tract of Lissauer, Lissauer and then divide into ascending & descending branches, each terminate in the dorsal horn • Most terminate at same level & some fibers may travel up or down the cord up to four levels
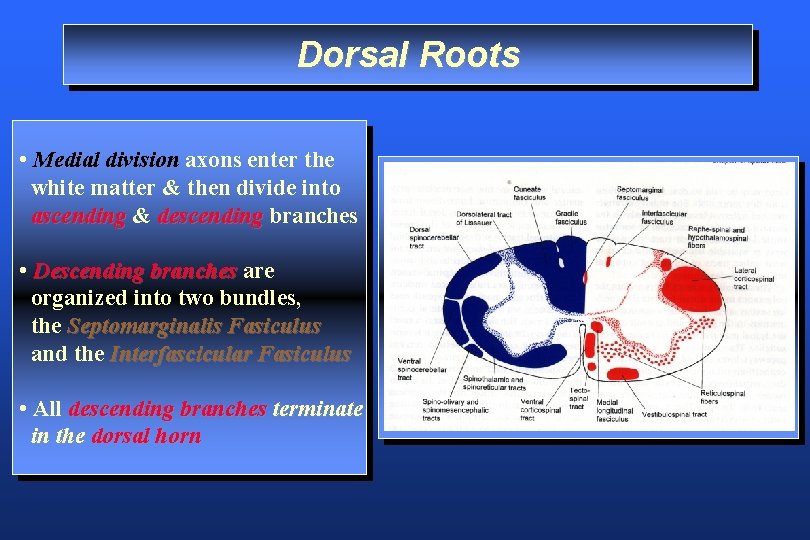
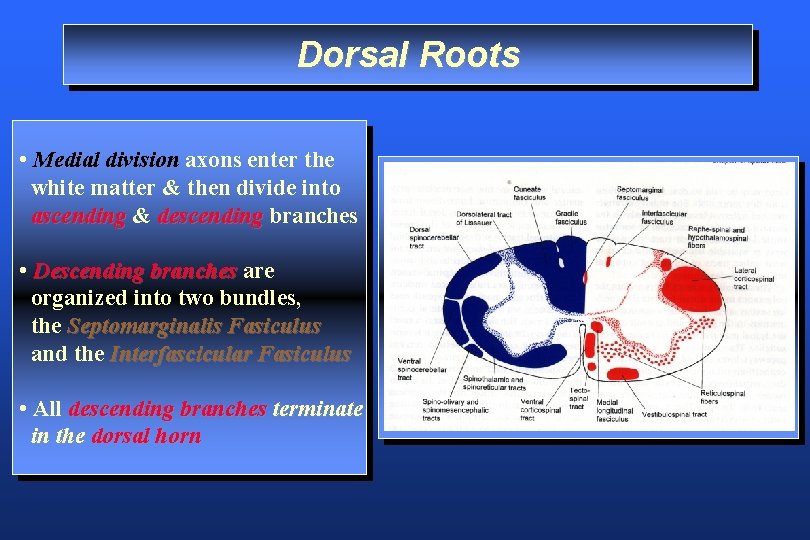
Dorsal Roots • Medial division axons enter the white matter & then divide into ascending & descending branches • Descending branches are organized into two bundles, the Septomarginalis Fasiculus and the Interfascicular Fasiculus • All descending branches terminate in the dorsal horn
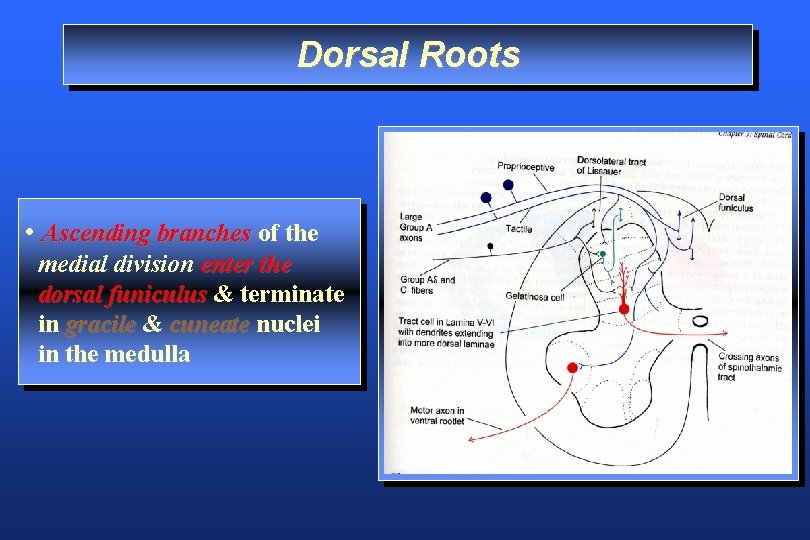
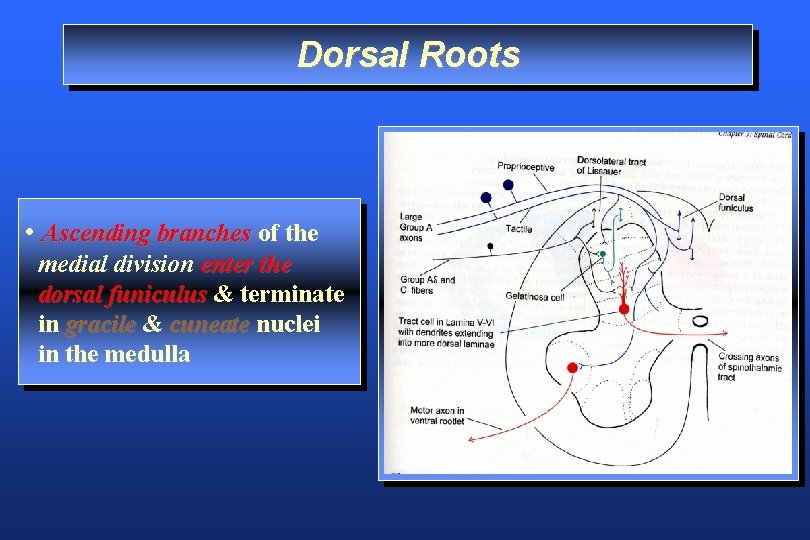
Dorsal Roots • Ascending branches of the medial division enter the dorsal funiculus & terminate in gracile & cuneate nuclei in the medulla
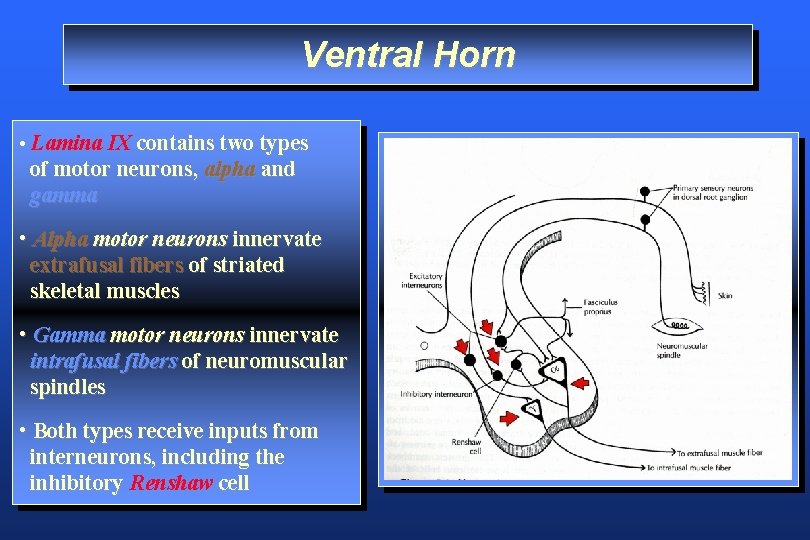
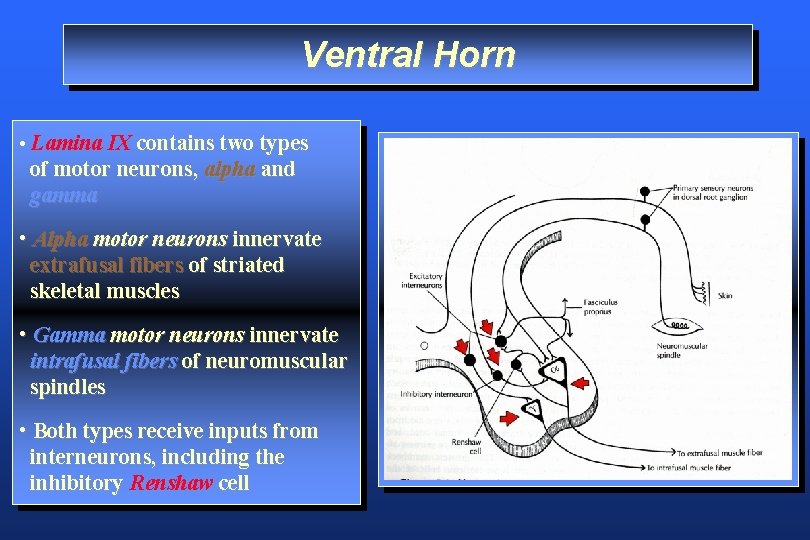
Ventral Horn • Lamina IX contains two types of motor neurons, alpha and gamma • Alpha motor neurons innervate extrafusal fibers of striated skeletal muscles • Gamma motor neurons innervate intrafusal fibers of neuromuscular spindles • Both types receive inputs from interneurons, including the inhibitory Renshaw cell

Spinal Cord Tracts
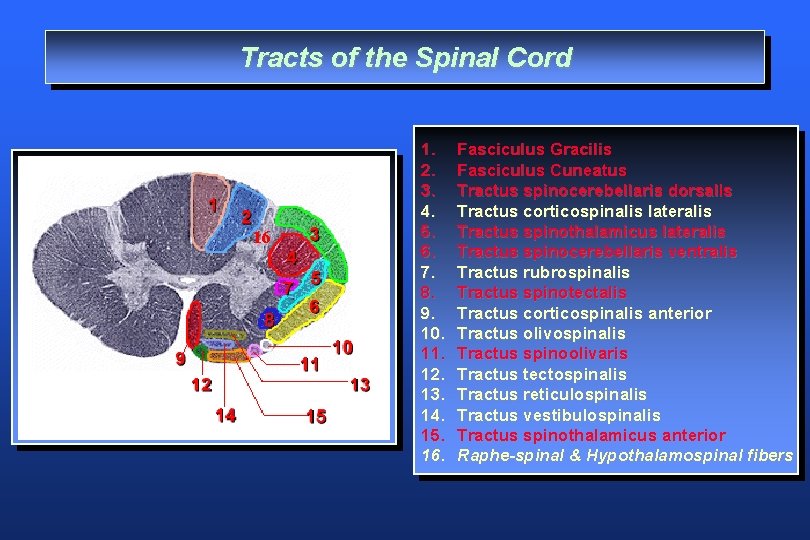
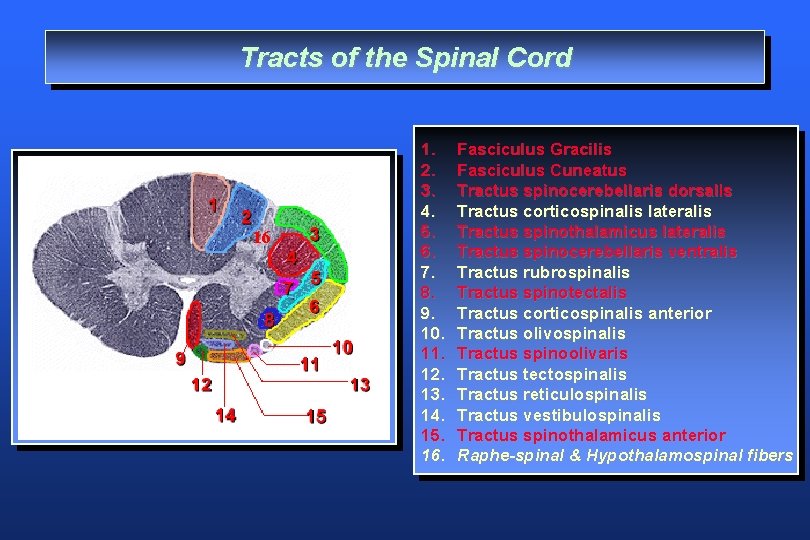
Tracts of the Spinal Cord 16 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Fasciculus Gracilis Fasciculus Cuneatus Tractus spinocerebellaris dorsalis Tractus corticospinalis lateralis Tractus spinothalamicus lateralis Tractus spinocerebellaris ventralis Tractus rubrospinalis Tractus spinotectalis Tractus corticospinalis anterior Tractus olivospinalis Tractus spinoolivaris Tractus tectospinalis Tractus reticulospinalis Tractus vestibulospinalis Tractus spinothalamicus anterior Raphe-spinal & Hypothalamospinal fibers
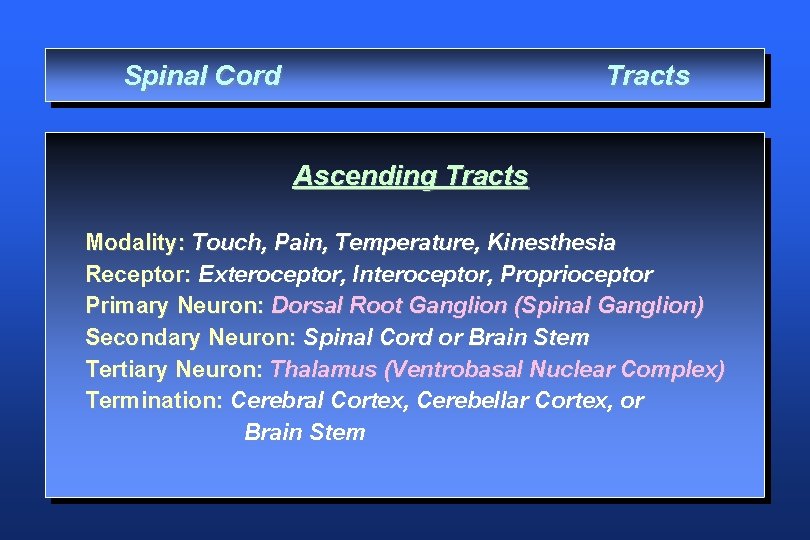
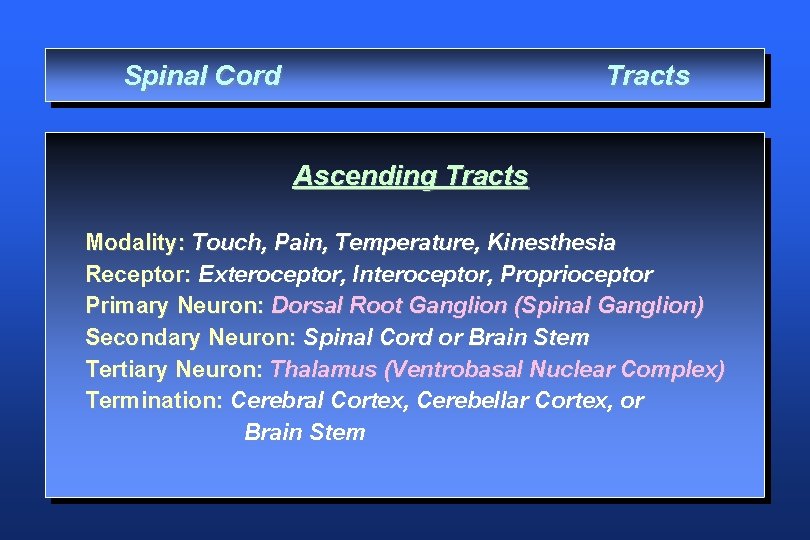
Spinal Cord Tracts Ascending Tracts Modality: Touch, Pain, Temperature, Kinesthesia Receptor: Exteroceptor, Interoceptor, Proprioceptor Primary Neuron: Dorsal Root Ganglion (Spinal Ganglion) Secondary Neuron: Spinal Cord or Brain Stem Tertiary Neuron: Thalamus (Ventrobasal Nuclear Complex) Termination: Cerebral Cortex, Cerebellar Cortex, or Brain Stem
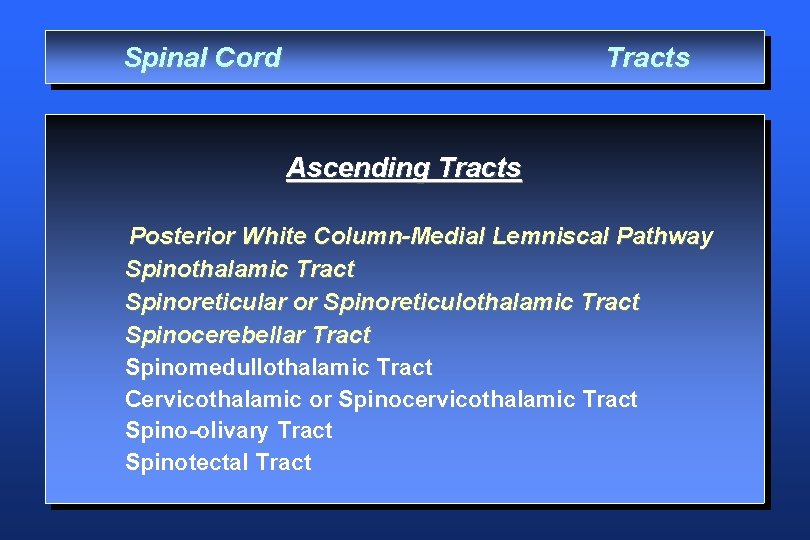
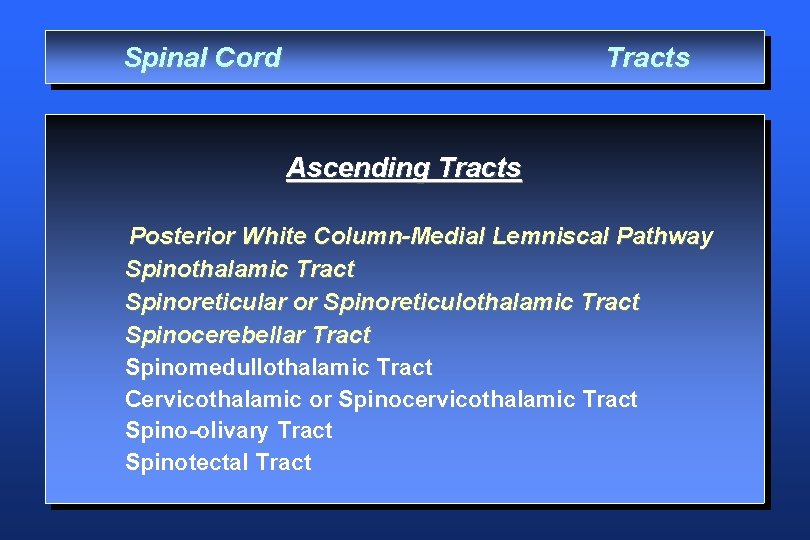
Spinal Cord Tracts Ascending Tracts Posterior White Column-Medial Lemniscal Pathway Spinothalamic Tract Spinoreticular or Spinoreticulothalamic Tract Spinocerebellar Tract Spinomedullothalamic Tract Cervicothalamic or Spinocervicothalamic Tract Spino-olivary Tract Spinotectal Tract

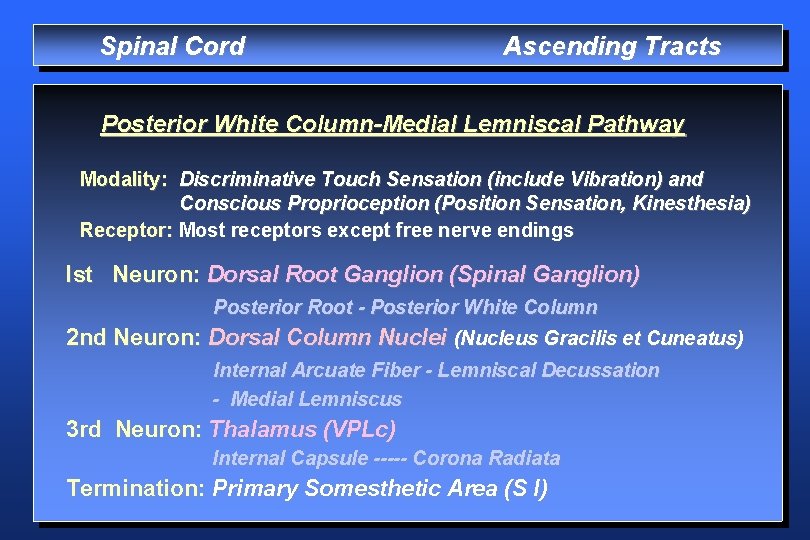
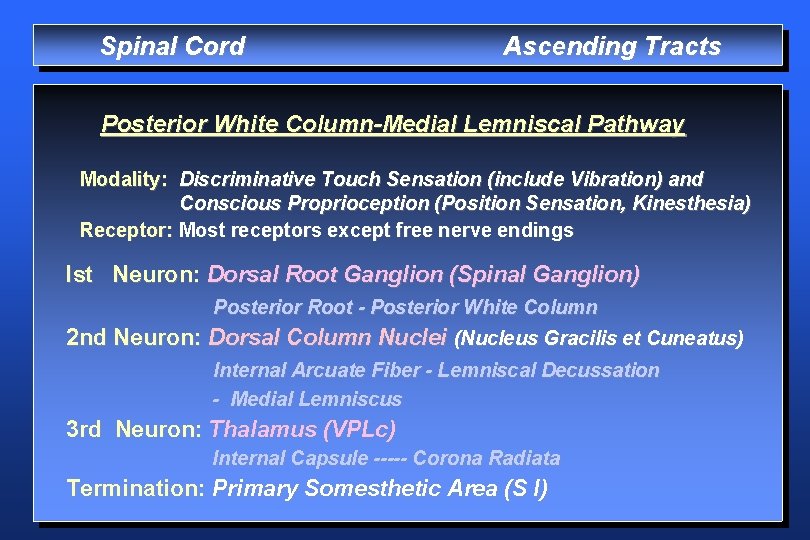
Spinal Cord Ascending Tracts Posterior White Column-Medial Lemniscal Pathway Modality: Discriminative Touch Sensation (include Vibration) and Conscious Proprioception (Position Sensation, Kinesthesia) Receptor: Most receptors except free nerve endings Ist Neuron: Dorsal Root Ganglion (Spinal Ganglion) Posterior Root - Posterior White Column 2 nd Neuron: Dorsal Column Nuclei (Nucleus Gracilis et Cuneatus) Internal Arcuate Fiber - Lemniscal Decussation - Medial Lemniscus 3 rd Neuron: Thalamus (VPLc) Internal Capsule ----- Corona Radiata Termination: Primary Somesthetic Area (S I)
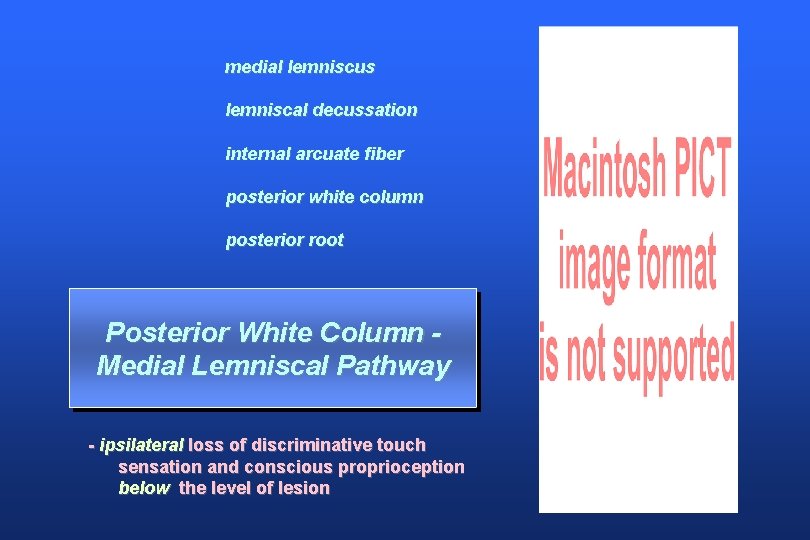
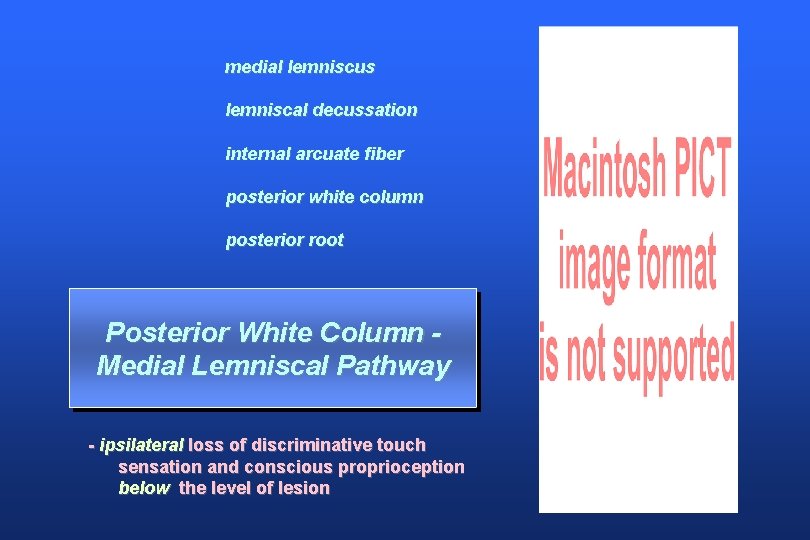
medial lemniscus lemniscal decussation internal arcuate fiber posterior white column posterior root Posterior White Column Medial Lemniscal Pathway - ipsilateral loss of discriminative touch sensation and conscious proprioception below the level of lesion
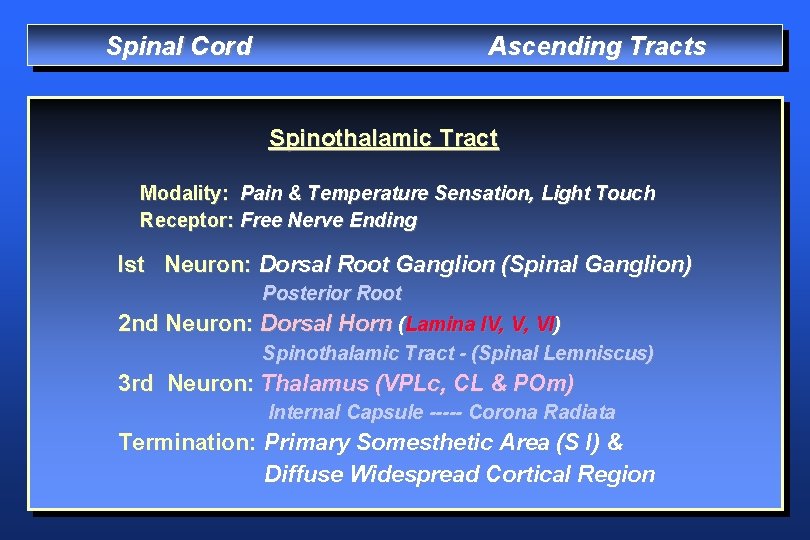
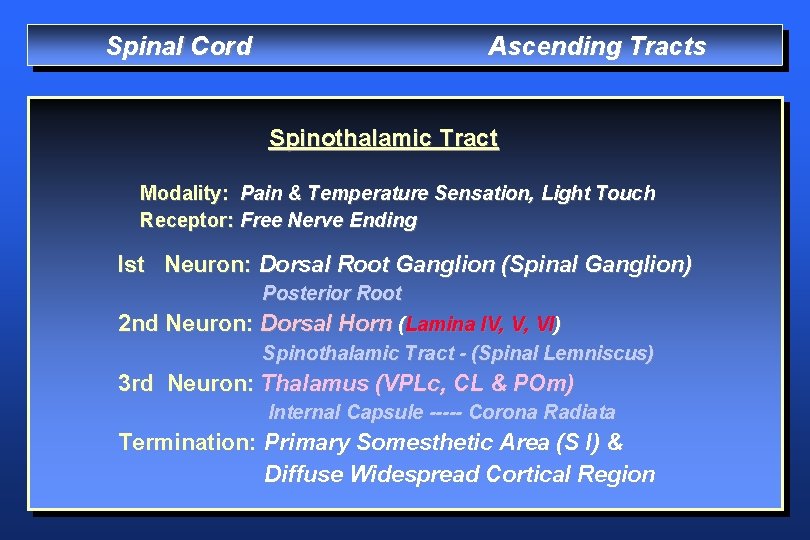
Spinal Cord Ascending Tracts Spinothalamic Tract Modality: Pain & Temperature Sensation, Light Touch Receptor: Free Nerve Ending Ist Neuron: Dorsal Root Ganglion (Spinal Ganglion) Posterior Root 2 nd Neuron: Dorsal Horn (Lamina IV, V, VI) Spinothalamic Tract - (Spinal Lemniscus) 3 rd Neuron: Thalamus (VPLc, CL & POm) Internal Capsule ----- Corona Radiata Termination: Primary Somesthetic Area (S I) & Diffuse Widespread Cortical Region
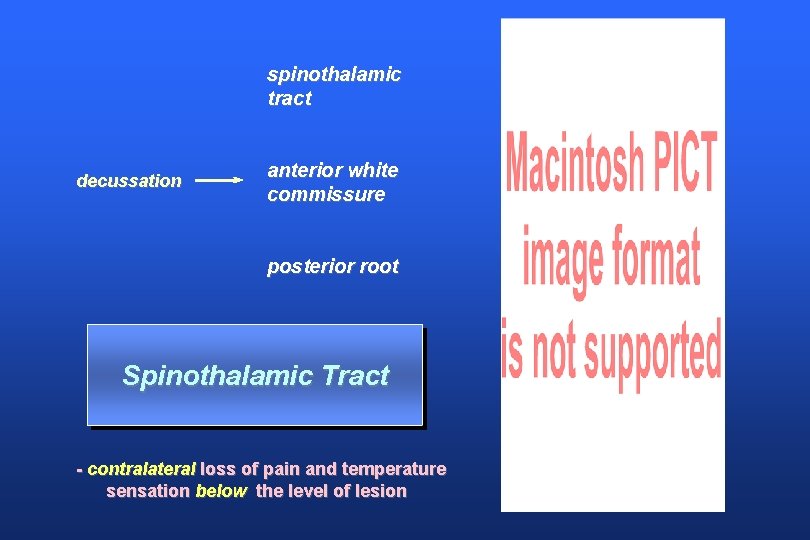
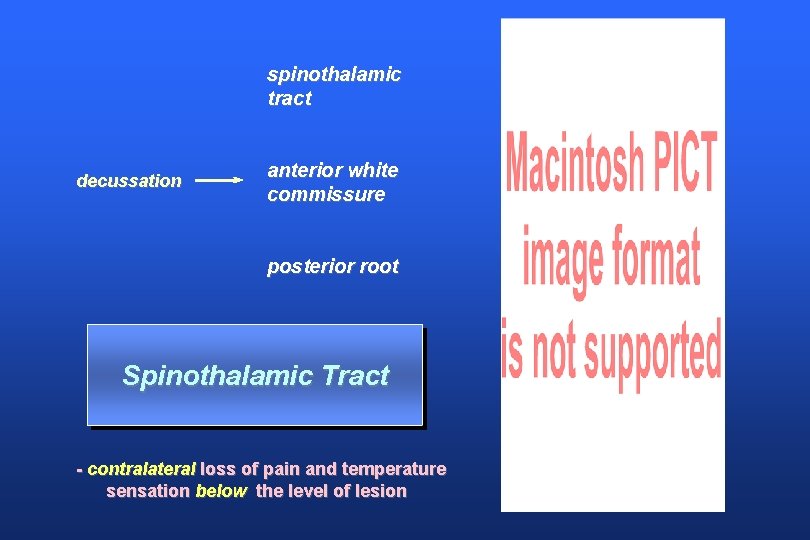
spinothalamic tract decussation anterior white commissure posterior root Spinothalamic Tract - contralateral loss of pain and temperature sensation below the level of lesion
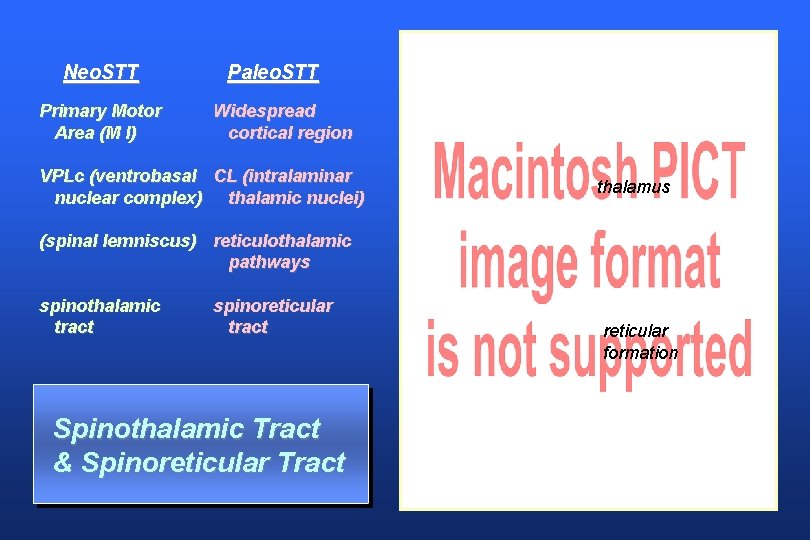
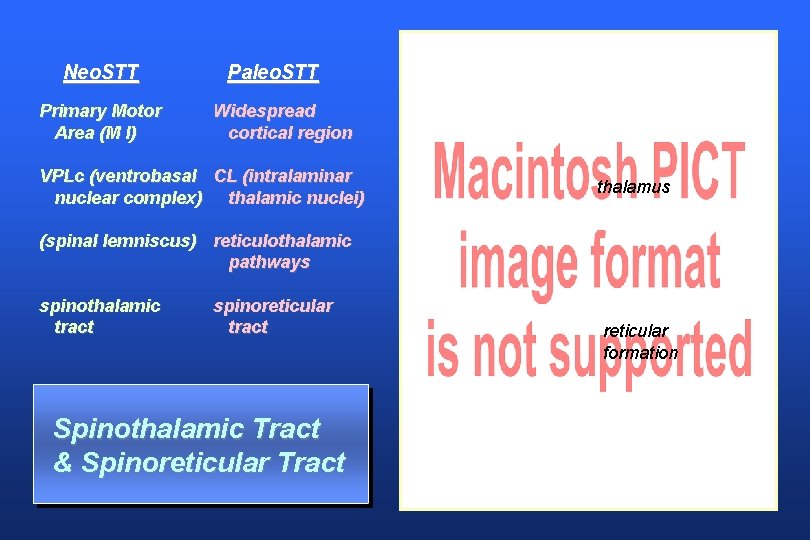
Neo. STT Primary Motor Area (M I) Paleo. STT Widespread cortical region VPLc (ventrobasal CL (intralaminar nuclear complex) thalamic nuclei) thalamus (spinal lemniscus) reticulothalamic pathways spinothalamic tract spinoreticular tract Spinothalamic Tract & Spinoreticular Tract reticular formation
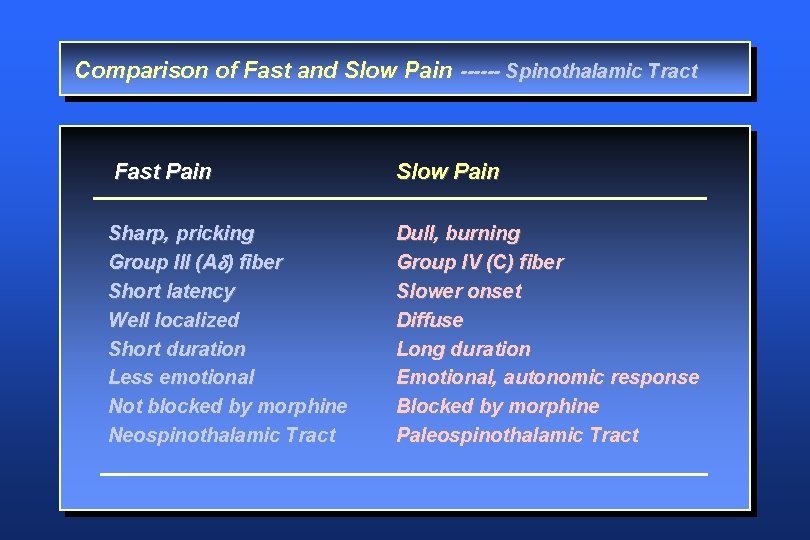
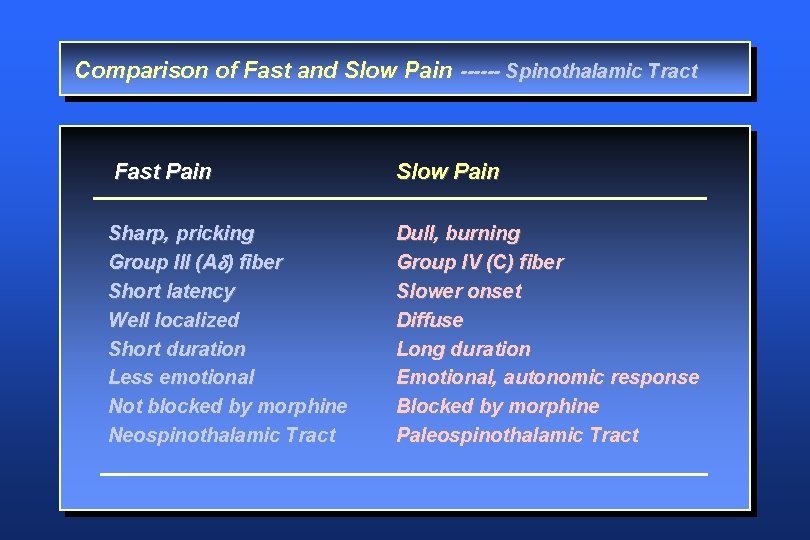
Comparison of Fast and Slow Pain ------ Spinothalamic Tract Fast Pain Sharp, pricking Group III (A ) fiber Short latency Well localized Short duration Less emotional Not blocked by morphine Neospinothalamic Tract Slow Pain Dull, burning Group IV (C) fiber Slower onset Diffuse Long duration Emotional, autonomic response Blocked by morphine Paleospinothalamic Tract
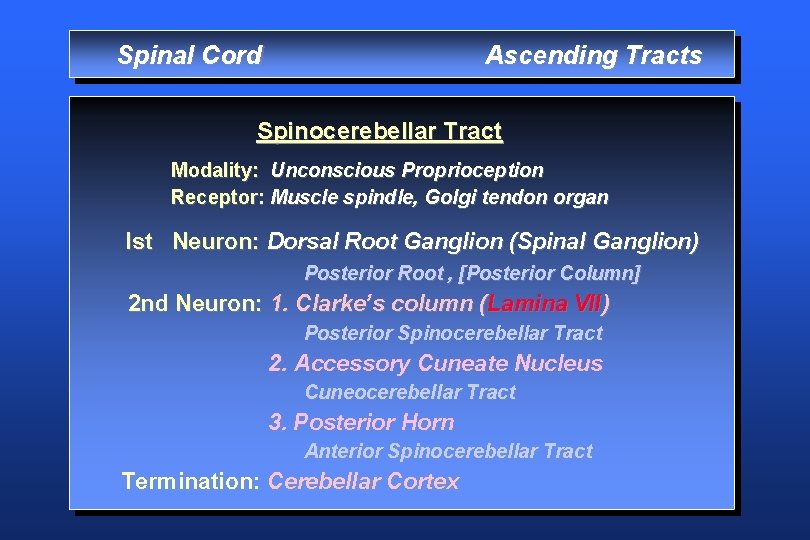
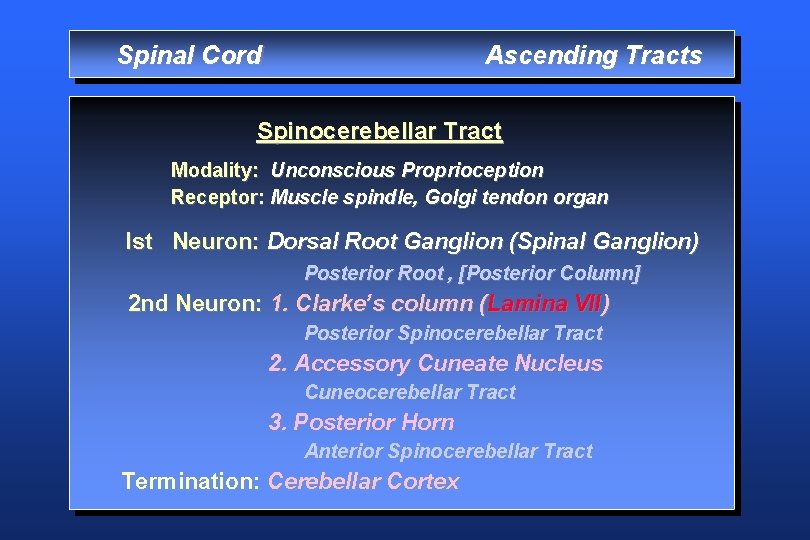
Spinal Cord Ascending Tracts Spinocerebellar Tract Modality: Unconscious Proprioception Receptor: Muscle spindle, Golgi tendon organ Ist Neuron: Dorsal Root Ganglion (Spinal Ganglion) Posterior Root , [Posterior Column] 2 nd Neuron: 1. Clarke’s column (Lamina VII) Posterior Spinocerebellar Tract 2. Accessory Cuneate Nucleus Cuneocerebellar Tract 3. Posterior Horn Anterior Spinocerebellar Tract Termination: Cerebellar Cortex
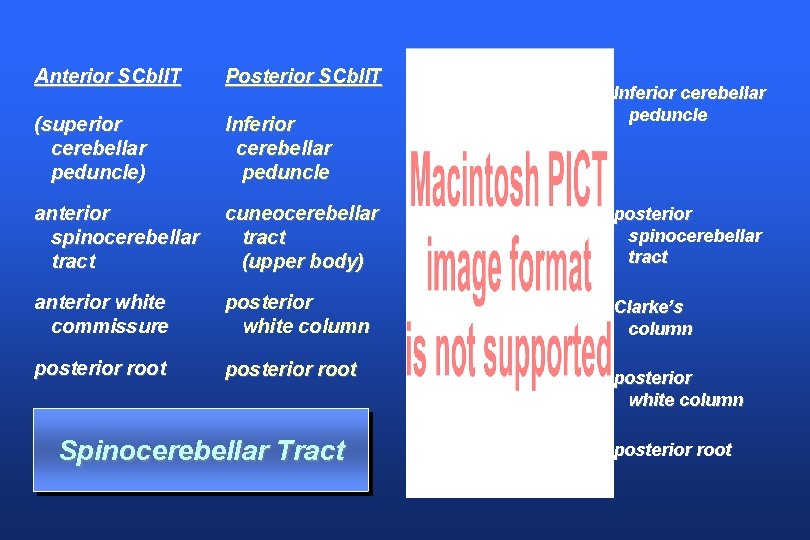
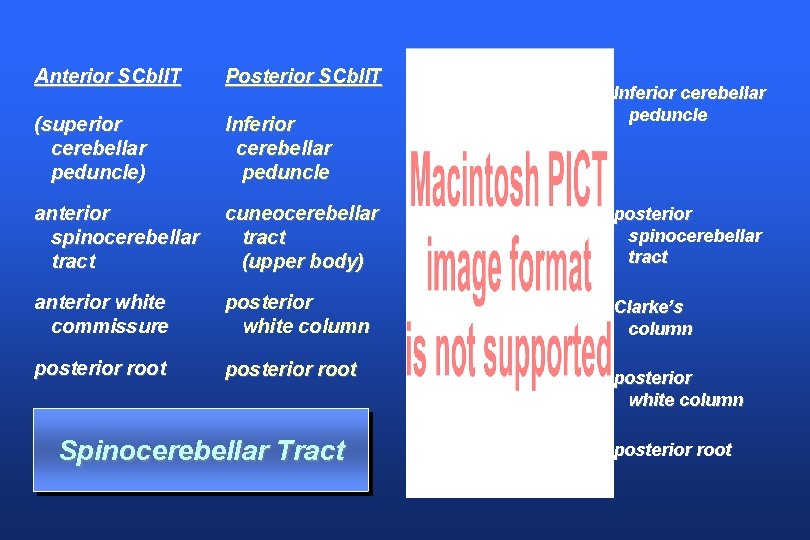
Anterior SCbll. T Posterior SCbll. T (superior cerebellar peduncle) Inferior cerebellar peduncle anterior spinocerebellar tract cuneocerebellar tract (upper body) posterior spinocerebellar tract anterior white commissure posterior white column Clarke’s column posterior root Spinocerebellar Tract Inferior cerebellar peduncle posterior white column posterior root

Spinocerebellar Tract
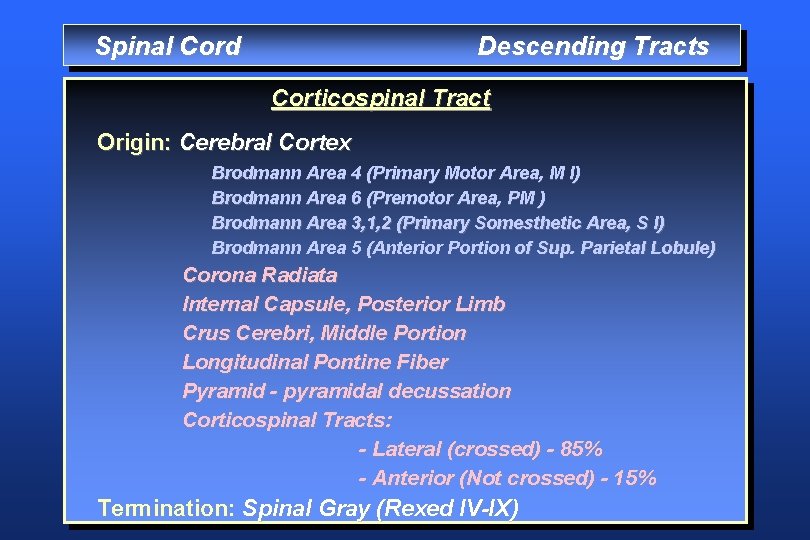
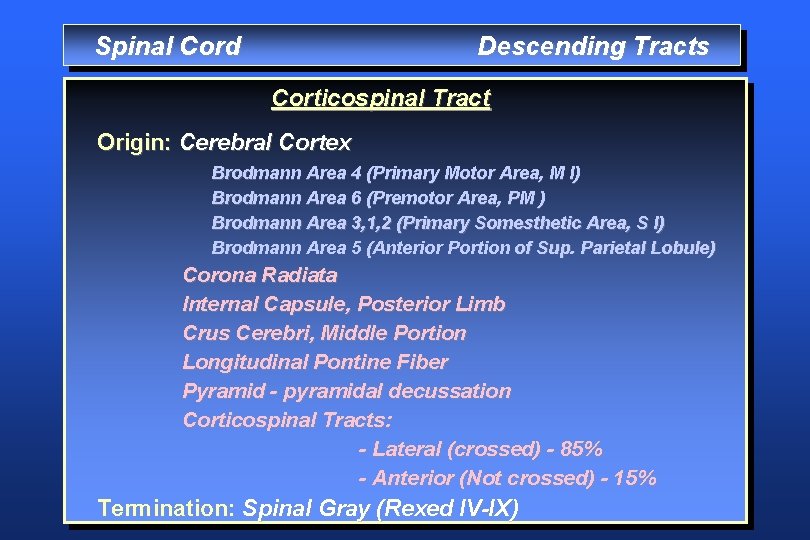
Spinal Cord Descending Tracts Corticospinal Tract Origin: Cerebral Cortex Brodmann Area 4 (Primary Motor Area, M I) Brodmann Area 6 (Premotor Area, PM ) Brodmann Area 3, 1, 2 (Primary Somesthetic Area, S I) Brodmann Area 5 (Anterior Portion of Sup. Parietal Lobule) Corona Radiata lnternal Capsule, Posterior Limb Crus Cerebri, Middle Portion Longitudinal Pontine Fiber Pyramid - pyramidal decussation Corticospinal Tracts: - Lateral (crossed) - 85% - Anterior (Not crossed) - 15% Termination: Spinal Gray (Rexed IV-IX)

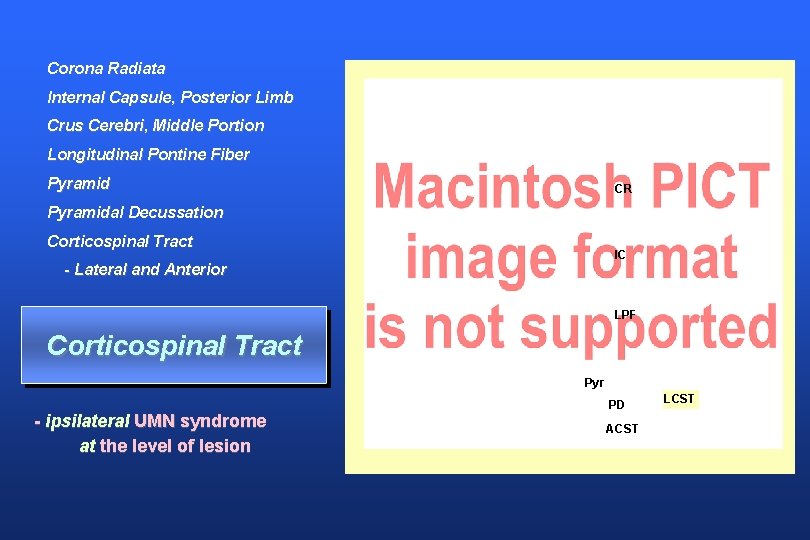
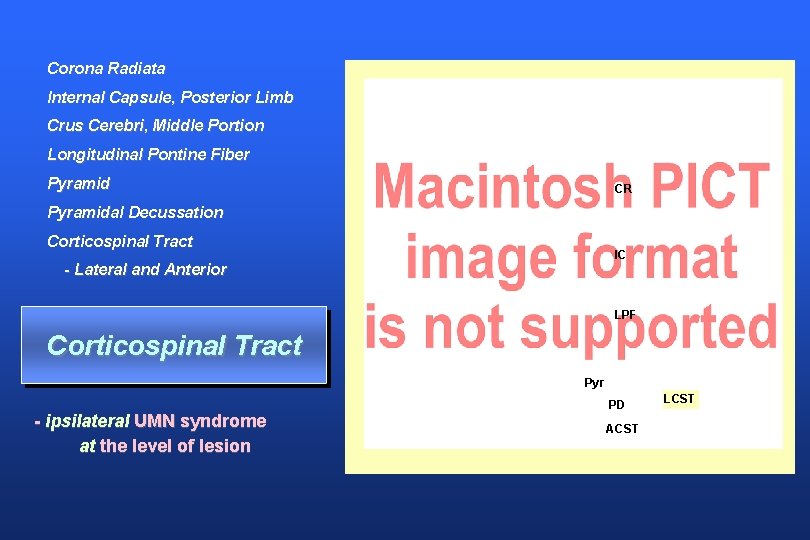
Corona Radiata lnternal Capsule, Posterior Limb Crus Cerebri, Middle Portion Longitudinal Pontine Fiber Pyramid CR Pyramidal Decussation Corticospinal Tract IC - Lateral and Anterior LPF Corticospinal Tract Pyr - ipsilateral UMN syndrome at the level of lesion PD ACST LCST
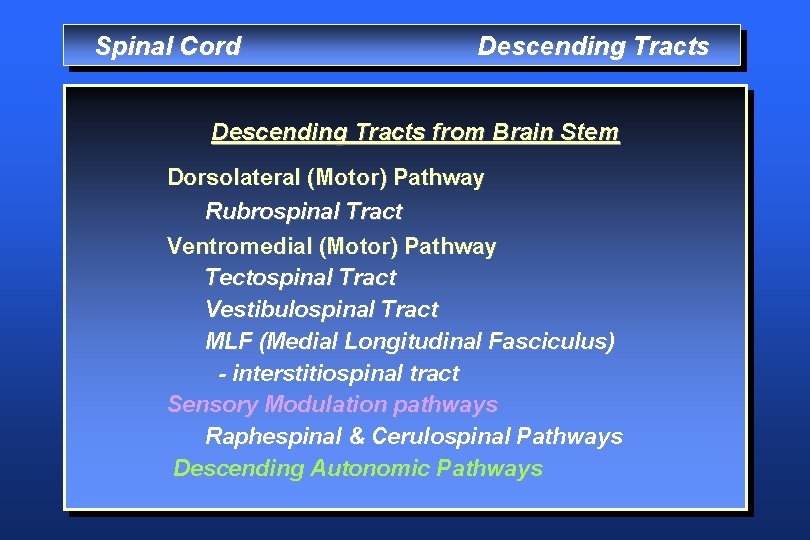
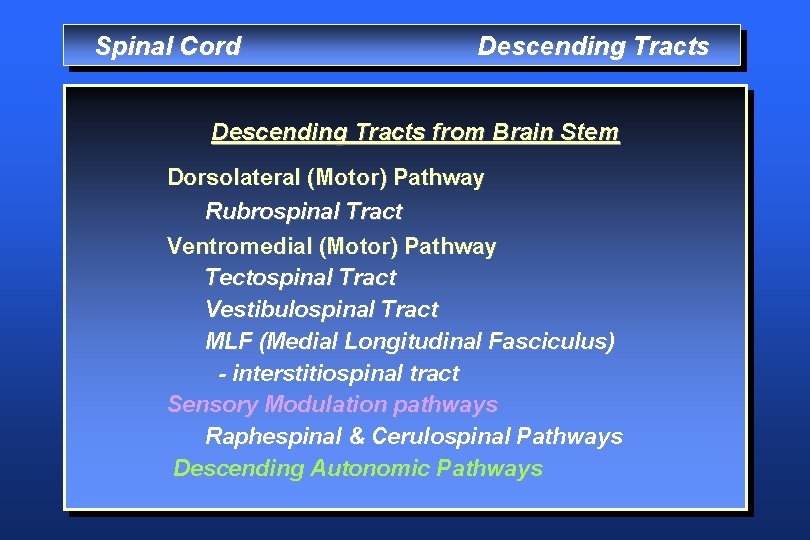
Spinal Cord Descending Tracts from Brain Stem Dorsolateral (Motor) Pathway Rubrospinal Tract Ventromedial (Motor) Pathway Tectospinal Tract Vestibulospinal Tract MLF (Medial Longitudinal Fasciculus) - interstitiospinal tract Sensory Modulation pathways Raphespinal & Cerulospinal Pathways Descending Autonomic Pathways

Spinal Cord Tracts Descending Tracts from Brain Stem ventromedial pathway dorsolateral pathway
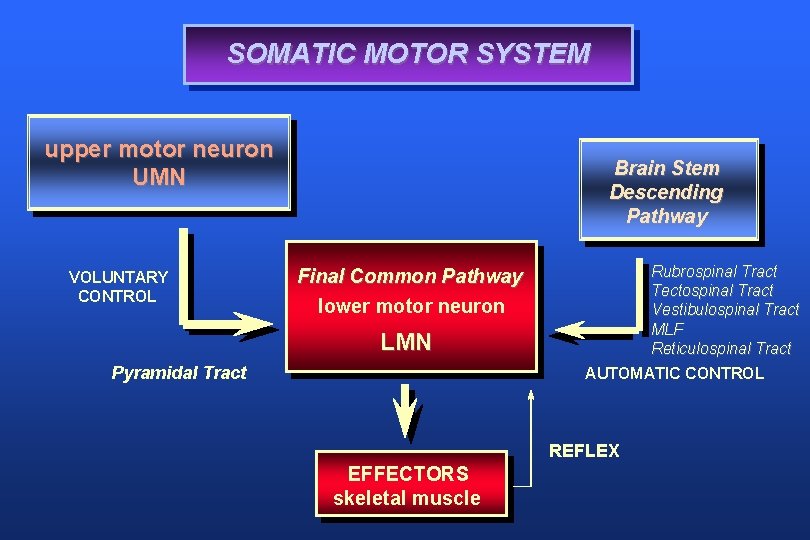
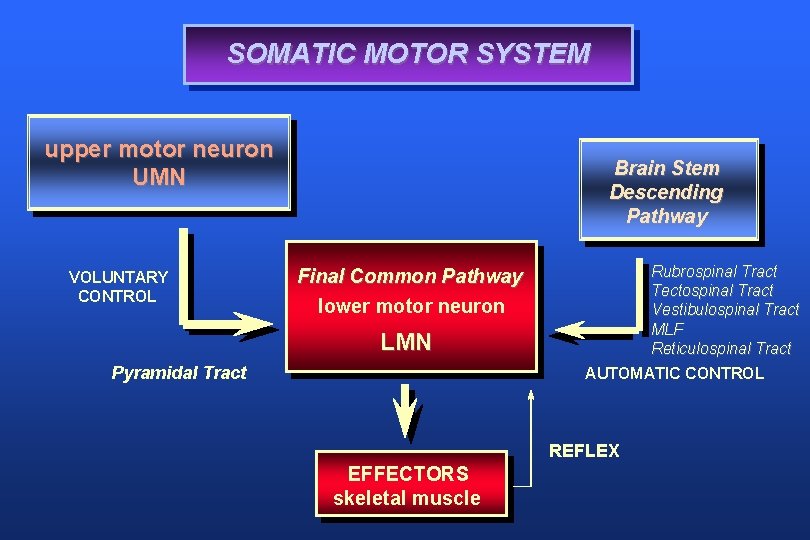
SOMATIC MOTOR SYSTEM upper motor neuron UMN VOLUNTARY CONTROL Brain Stem Descending Pathway Rubrospinal Tract Tectospinal Tract Vestibulospinal Tract MLF Reticulospinal Tract Final Common Pathway lower motor neuron LMN Pyramidal Tract AUTOMATIC CONTROL REFLEX EFFECTORS skeletal muscle
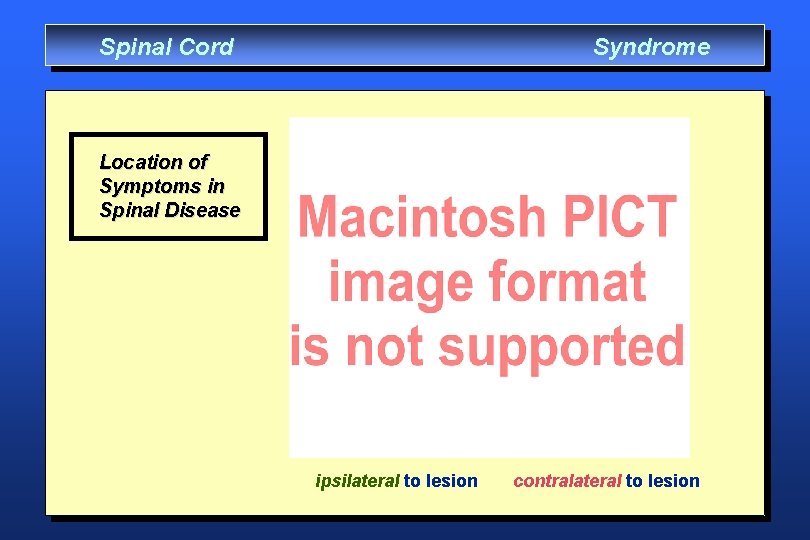
Spinal Cord Syndrome Location of Symptoms in Spinal Disease ipsilateral to lesion contralateral to lesion
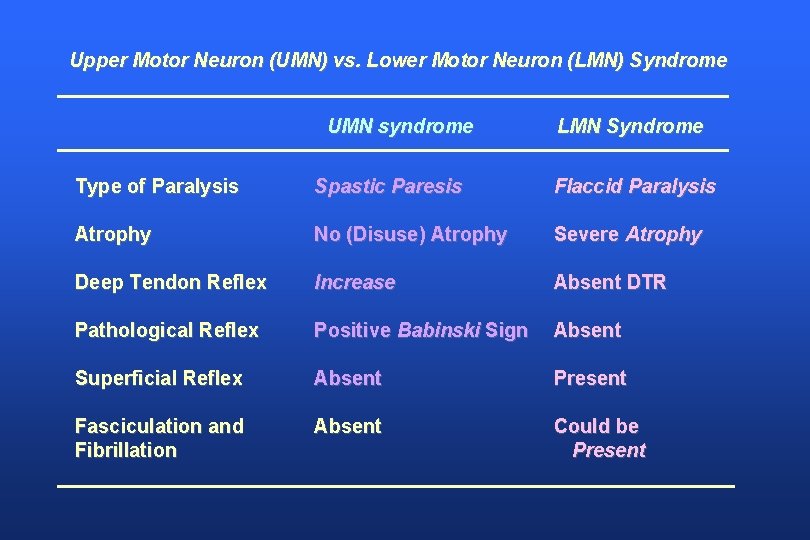
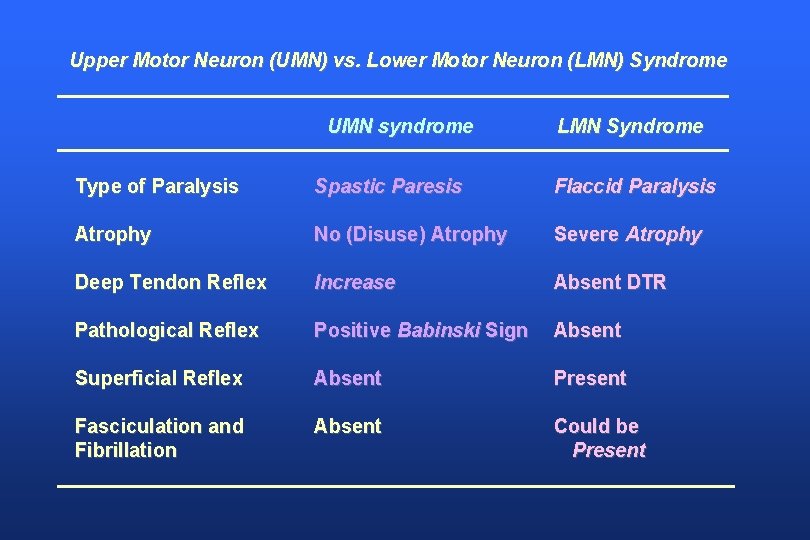
Upper Motor Neuron (UMN) vs. Lower Motor Neuron (LMN) Syndrome UMN syndrome LMN Syndrome Type of Paralysis Spastic Paresis Flaccid Paralysis Atrophy No (Disuse) Atrophy Severe Atrophy Deep Tendon Reflex Increase Absent DTR Pathological Reflex Positive Babinski Sign Absent Superficial Reflex Absent Present Fasciculation and Fibrillation Absent Could be Present
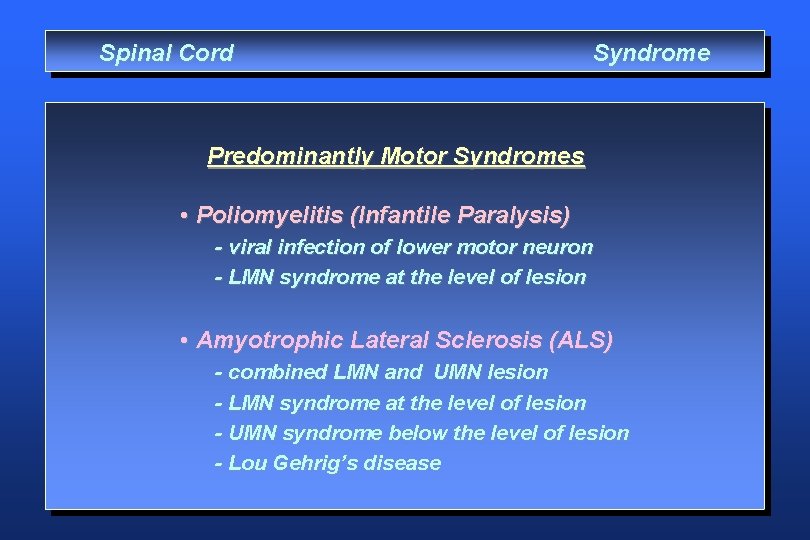
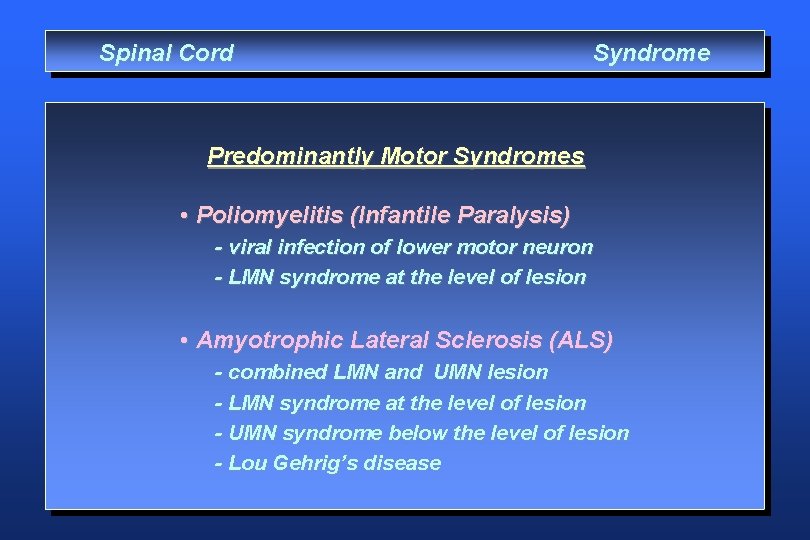
Spinal Cord Syndrome Predominantly Motor Syndromes • Poliomyelitis (Infantile Paralysis) - viral infection of lower motor neuron - LMN syndrome at the level of lesion • Amyotrophic Lateral Sclerosis (ALS) - combined LMN and UMN lesion - LMN syndrome at the level of lesion - UMN syndrome below the level of lesion - Lou Gehrig’s disease
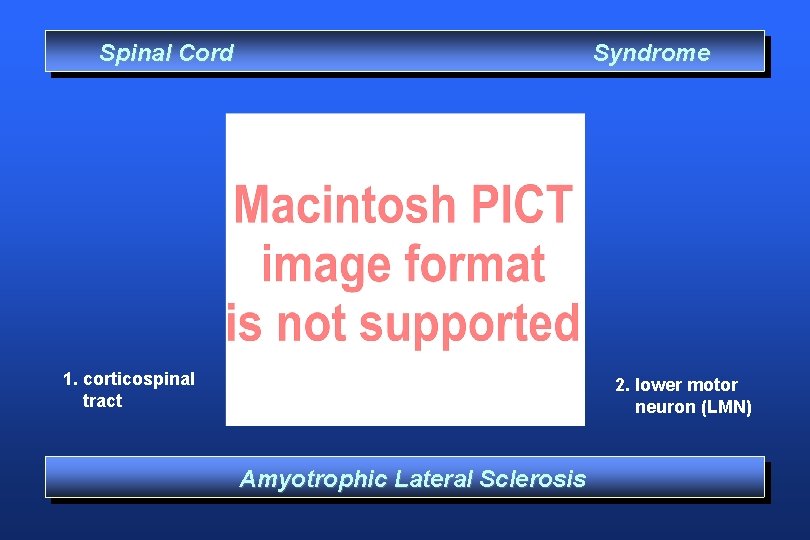
Spinal Cord Syndrome 1. corticospinal tract 2. lower motor neuron (LMN) Amyotrophic Lateral Sclerosis
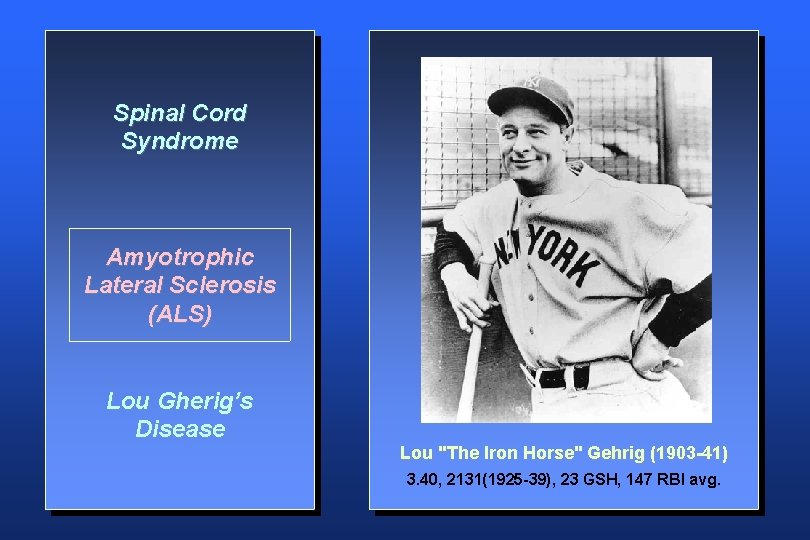
Spinal Cord Syndrome Amyotrophic Lateral Sclerosis (ALS) Lou Gherig’s Disease Lou "The Iron Horse" Gehrig (1903 -41) 3. 40, 2131(1925 -39), 23 GSH, 147 RBI avg.
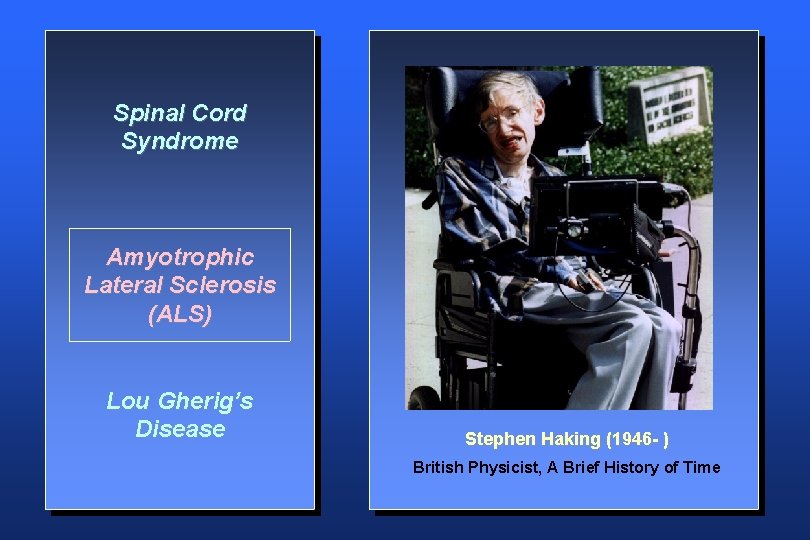
Spinal Cord Syndrome Amyotrophic Lateral Sclerosis (ALS) Lou Gherig’s Disease Stephen Haking (1946 - ) British Physicist, A Brief History of Time
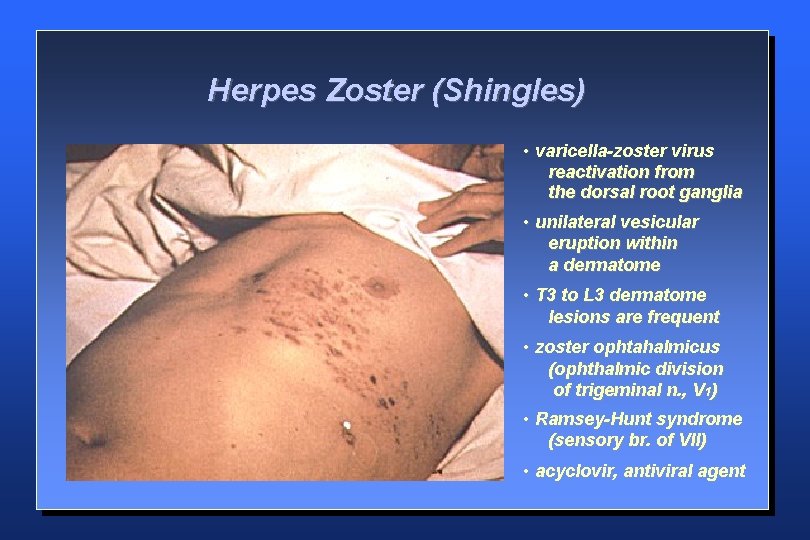
Spinal Cord Syndrome Predominantly Sensory Syndromes • Herpes Zoster - inflammatory reactions of spinal ganglion - severe pain on the dermatomes of affected ganglion • Tabes Dorsalis - common variety of neurosyphilis - posterior column and spinal posterior root lesion - loss of discriminative touch sensation and conscious proprioception below the level of lesion - posterior column ataxia - lancinating pain (a stabbing or piercing sensation) - loss of deep tendon reflex (DTR)
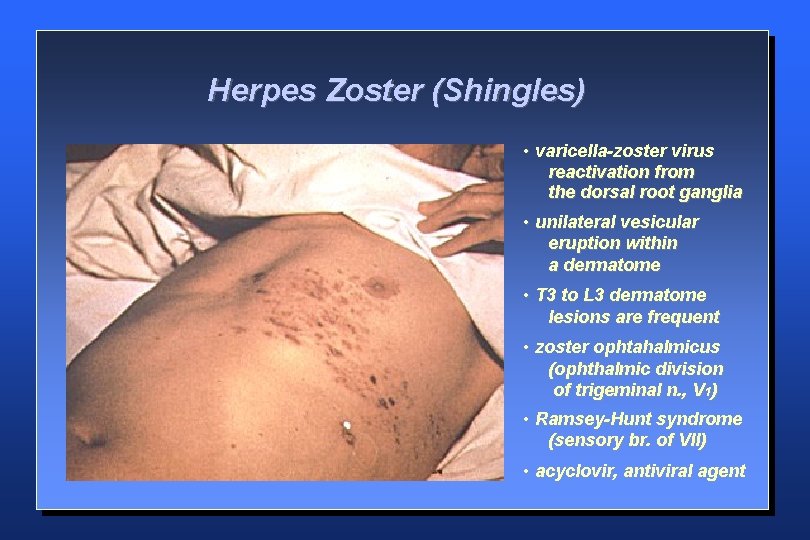
Herpes Zoster (Shingles) • varicella-zoster virus reactivation from the dorsal root ganglia • unilateral vesicular eruption within a dermatome • T 3 to L 3 dermatome lesions are frequent • zoster ophtahalmicus (ophthalmic division of trigeminal n. , V 1) • Ramsey-Hunt syndrome (sensory br. of VII) • acyclovir, antiviral agent
Spinal Cord Syndrome Sub-Acute Combined Degeneration (Combined System Disease) Lesion - posterior white column - corticospinal tract (UMN) Symptom - loss of discriminative touch sensation and conscious proprioception below the level of lesion - ipsilateral UMN syndrome below the level of lesion
Spinal Cord 1. corticospinal tract Syndrome 2. posterior white column Sub-Acute Combined Degeneration
Spinal Cord Syndrome Syringomyelia, Hematomyelia Lesion - central canal of spinal cord - gradually extended to peripheral part of the cord Symptom - initial symptom is bilateral loss of pain (compression of anterior white commissure) - variety of symptoms appear according to the lesion extended from central canal
Spinal Cord Syndrome Syringomyelia - Initial Symptoms

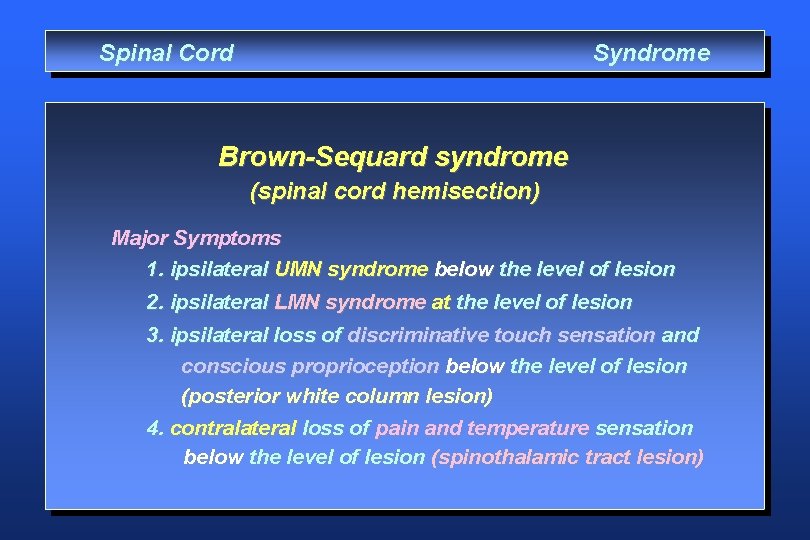
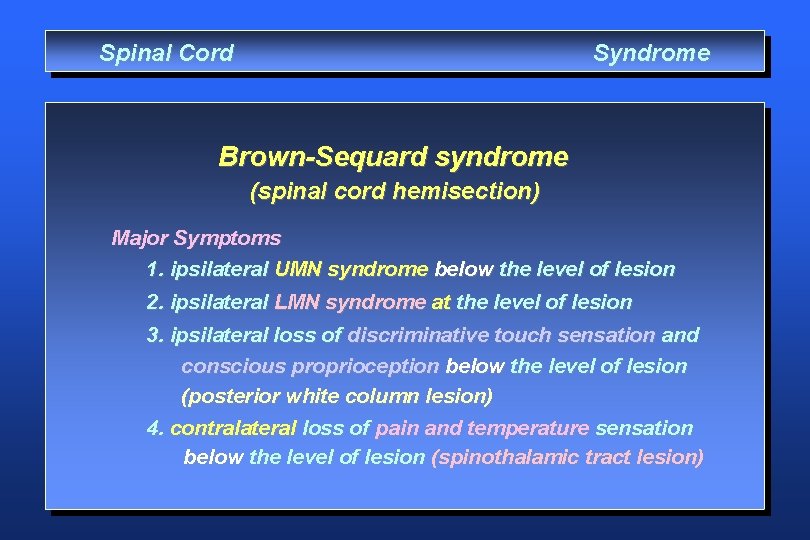
Spinal Cord Syndrome Brown-Sequard syndrome (spinal cord hemisection) Major Symptoms 1. ipsilateral UMN syndrome below the level of lesion 2. ipsilateral LMN syndrome at the level of lesion 3. ipsilateral loss of discriminative touch sensation and conscious proprioception below the level of lesion (posterior white column lesion) 4. contralateral loss of pain and temperature sensation below the level of lesion (spinothalamic tract lesion)
Spinal Cord Syndrome Brown-Sequard Syndrome (Spinal Cord Hemisection)


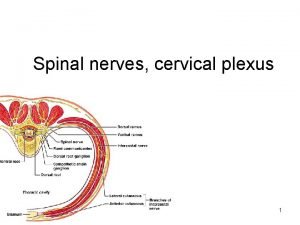
 Spinal nerves
Spinal nerves Figure 13-2 spinal nerves
Figure 13-2 spinal nerves Innervations of the brachial and lumbar enlargements
Innervations of the brachial and lumbar enlargements Spinal cord and spinal nerves exercise 15
Spinal cord and spinal nerves exercise 15 Spinal cord diagram
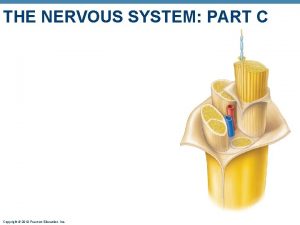
Spinal cord diagram Neuron bundle
Neuron bundle Spinal cord diagram
Spinal cord diagram Renshaw cell inhibition
Renshaw cell inhibition Spinal cord denticulate ligament
Spinal cord denticulate ligament Hypothalamus
Hypothalamus Causes of spinal cord compression
Causes of spinal cord compression Spinal cord
Spinal cord Function of the medulla oblongata
Function of the medulla oblongata Posterior medial sulcus
Posterior medial sulcus Spinal cord extends from
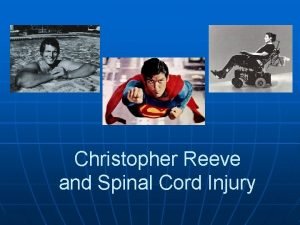
Spinal cord extends from Christopher reeve spinal cord injury level
Christopher reeve spinal cord injury level Bird air sac
Bird air sac Components of the reflex arc
Components of the reflex arc Substantia gelatinosa
Substantia gelatinosa Spinal cord organization
Spinal cord organization Spinal cord
Spinal cord Osd sindrom
Osd sindrom What is the spinal cord made of
What is the spinal cord made of Spinal arteries
Spinal arteries Trachea and spinal cord
Trachea and spinal cord Spinal cord
Spinal cord Spinal cord
Spinal cord Tissue
Tissue Morphology of spinal cord
Morphology of spinal cord Eat well live well
Eat well live well Thecal sac compression icd 10
Thecal sac compression icd 10 Intensivis
Intensivis Back hurts
Back hurts Spinal cord cross section
Spinal cord cross section Spinal cord and brain
Spinal cord and brain Mater qqn
Mater qqn Christopher reeve ventilator
Christopher reeve ventilator Spinal cord injury shoulder exercises
Spinal cord injury shoulder exercises Anconeus
Anconeus Ventral root and dorsal root
Ventral root and dorsal root Frog spleen
Frog spleen Spinal cord
Spinal cord Connective tissue layer
Connective tissue layer Spinal cord nerve anatomy
Spinal cord nerve anatomy Spine meninges
Spine meninges Division of spinal cord
Division of spinal cord Spinal cord
Spinal cord Spinal cord
Spinal cord Grey commissure
Grey commissure 31 spinal nerves
31 spinal nerves Boston scientific spinal cord stimulator
Boston scientific spinal cord stimulator Anterior median fissure
Anterior median fissure Spinal cord injury rehabilitation st. louis
Spinal cord injury rehabilitation st. louis Umbilical cord histology diagram
Umbilical cord histology diagram Medula espinal
Medula espinal Pns
Pns Spinal cord
Spinal cord Spinal cord muscles
Spinal cord muscles Indibulum
Indibulum Spinal shock symptoms
Spinal shock symptoms Neural crest cells derivatives
Neural crest cells derivatives Somi brace
Somi brace Arkus refleks
Arkus refleks Spinal cord compression nice
Spinal cord compression nice Blastocoal
Blastocoal Spinal cord spasticity
Spinal cord spasticity Nerves branching beyond the spinal cord into the body
Nerves branching beyond the spinal cord into the body Visceral reflex
Visceral reflex Vertebral landmarks
Vertebral landmarks Spinal anaesthesia structures pierced
Spinal anaesthesia structures pierced Oblique passage
Oblique passage Scrotal sac layers
Scrotal sac layers Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Thang điểm glasgow
Thang điểm glasgow Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng