The Management of Malignant Spinal Cord Compression Dr







- Slides: 26

The Management of Malignant Spinal Cord Compression Dr H. K. Lord Consultant Clinical Oncologist

Aim – ambulatory patients
Introduction u 2 -5% of cancer patients have an episode of SCC u Commoner in myeloma, prostate, lung and breast cancer (15 -20%) u Initial presentation in 8% cancer patients, sometimes of unknown primary u 10% of patients diagnosed with SCC may have a second episode
Presentation u Depends u Radicular on level (77% in T spine) (1) back pain in 85 -95% u Worsened by lying flat, weight bearing, coughing and sneezing, relieved by sitting 1. Levack P, Graham J, Collie D, Grant R, Kidd J, Kunkler I, Gibson A, Hurman D, Mc. Millan N, Rampling R, Slider L, Statham P, Summers D (2001) A prospective audit of the diagnosis, management and outcome of malignant spinal cord compression. Clinical Resource and Audit Group (CRAG) 97/08
Presentation u Motor weakness u Sensory disturbance u Sphincter disturbance u However localisation of pain poorly correlates with site of disease – 16%

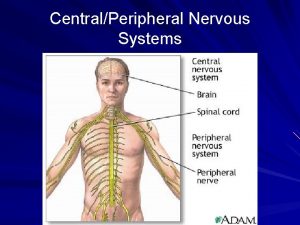
Aetiology 3 routes: u Vertebral mets invading the epidural space, or causing bone destruction and fragments of bone compressing the cord u Retroperitoneal tumours grow through the intervertebral foramina u Compression of blood supply to cord causing ischemia and oedema and hence loss of function

Diagnosis u In the history - especially in a known cancer patient. u MRI spine – urgent u Referral to Oncology - urgent
Treatment u Steroids – dexamethasone 16 mg po with PPI or H 2 antagonist – to reduce oedema Thereafter: Depends on histology u Depends on patient age performance status and if disease is controlled elsewhere u
Options u Surgery u XRT u Chemo u BSC
Surgery u Anterior laminectomy – allows better removal of tumour and reconstruction of vertebral body u Suitable for patients who are fit for surgery, have unstable spine, or radio-resistant tumour, and disease at only one level, with disease elsewhere either absent or controlled
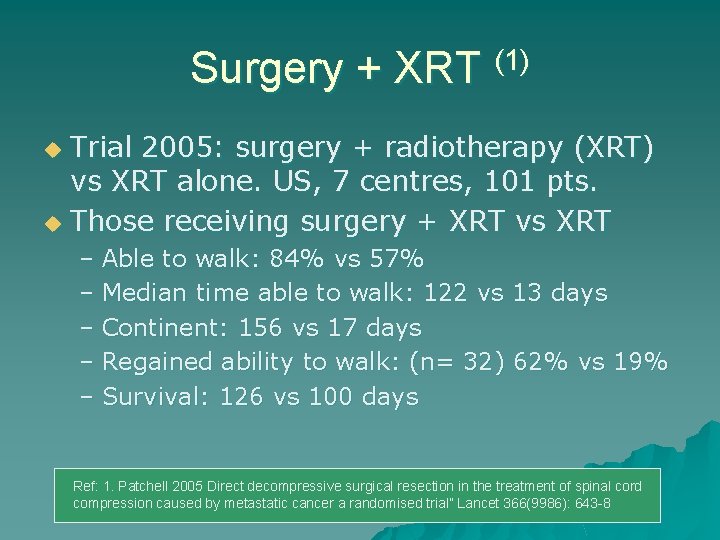
Surgery + XRT (1) Trial 2005: surgery + radiotherapy (XRT) vs XRT alone. US, 7 centres, 101 pts. u Those receiving surgery + XRT vs XRT u – Able to walk: 84% vs 57% – Median time able to walk: 122 vs 13 days – Continent: 156 vs 17 days – Regained ability to walk: (n= 32) 62% vs 19% – Survival: 126 vs 100 days Ref: 1. Patchell 2005 Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer a randomised trial” Lancet 366(9986): 643 -8
Radiotherapy alone u Remains the majority, despite evidence above u In patients unfit for surgery; with multi-level disease; with disease elsewhere that may or may not be controlled; with some residual neurological function
Radiotherapy u Lack of randomised trials – literature review only (1) u 20 Gy in 5 # over 1 week u Started as soon as is reasonably practical u Direct field, prescribed to the depth of the cord Ref: 1. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline DA Loblaw and NJ Laperriere Journal of Clinical Oncology, Vol 16, 1613 -1624,
Radiotherapy u May use higher dose if post op or if only site of metastasis ( 30 Gy in 10#) u If plasmacytoma, use radical dose of 40 Gy in 25#
Side effects u Exit u Skin dose: bowel: diarrhoea oesophagus: odynophagia reaction - mild
Outcomes u No immediate benefit u Some neurological improvement over following weeks; improved pain control; or halting of further deterioration u Glasgow study: 74% patients died within 3 months of diagnosis (1) 1. A Mc. Linton and C Hutchison Malignant spinal cord compression: a retrospective audit of clinical practice at a UK regional cancer centre British Journal of Cancer (2006)
Chemotherapy u Perhaps as follow up to initial treatment but rarely as first line management u e. g. in lymphoma or small cell lung cancer or teratoma

Best Supportive Care u Once neurological function lost, recovery unlikely. u If disease elsewhere is advanced, may be appropriate not to treat actively. u Steroids, physiotherapy, analgaesia, good nursing care

Multidisciplinary care u Rehabilitation u Nursing care – pressure sores; thromboembolic disease; analgaesia u Personal dignity u Lack of autonomy u End stage of illness u If discharge planned, OT, SW and PT input
Multidisciplinary care u Keeping patient and family informed u Financial assistance (DS 1500)
Prevention u Listen to patient history – early detection u If known to have bony metastases, role of bisphonates - prostate and breast cancer patients (1) u Early referral to Oncology 1: J R Ross Systematic review of role of bisphonates on skeletal morbidity in metastatic cancer BMJ 2003; 327: 469

Want our patients out walking, with the dog carrying the stick!
Thank you u Any questions?
 Exercise 15 spinal cord and spinal nerves
Exercise 15 spinal cord and spinal nerves The spinal nerves
The spinal nerves Median nerve innervates
Median nerve innervates Rubrospinal
Rubrospinal Causes of spinal cord compression
Causes of spinal cord compression Spinal cord compression nice
Spinal cord compression nice Spinal cord denticulate ligament
Spinal cord denticulate ligament Hypothalamus
Hypothalamus Anterior ramus of spinal cord
Anterior ramus of spinal cord Main function of spinal cord
Main function of spinal cord Ventral median fissure
Ventral median fissure Intervertebral disc prolapse
Intervertebral disc prolapse Christopher reeve spinal cord injury level
Christopher reeve spinal cord injury level Notochord vs spinal cord
Notochord vs spinal cord What covers the spinal cord
What covers the spinal cord Slidetodoc.com
Slidetodoc.com The tectospinal tract
The tectospinal tract 3 layers of spinal cord
3 layers of spinal cord Tethered cord sindrom
Tethered cord sindrom 31 pairs of spinal nerves
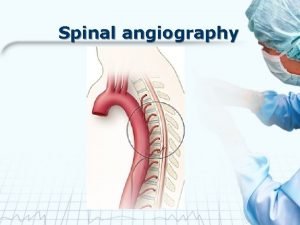
31 pairs of spinal nerves Spinal angiogram
Spinal angiogram Stretch reflex
Stretch reflex Mezgovnice
Mezgovnice Spinal cord
Spinal cord Stretch reflex
Stretch reflex End of spinal cord
End of spinal cord Eat well live well with spinal cord injury
Eat well live well with spinal cord injury