Neuroleptic Malignant Syndrome NMS Sue Henderson Definition Rare


- Slides: 20
Neuroleptic Malignant Syndrome (NMS) Sue Henderson
Definition • Rare adverse reaction to dopamine receptor antagonists (blockers) • Leading to autonomic dysfunction • Can be fatal if not recognized early
Commonly associated with: • haloperidol (Serenace) • fluphenazine (Prolixin) • chlorpromazine (Largactil)
Less commonly associated with: atypicals: • quetiapine (Seroquel) • risperidone (Risperdal) • olanzapine (Zyprexa) dopamine receptor antagonists: • prochlorperazine (Stemetil) • metoclopramide (Maxalon) • promethazine (Phenergan)
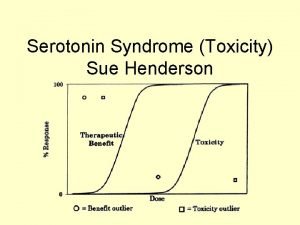
Pathophysiology • Not fully understood • Probably dopaminergic blockade or depletion in CNS • May be a drug induced malignant catatonia (? same underlying pathophysiology) (Fink, 1996, as cited in Strawn, Keck & Caroff, 2007). • Genetics may be involved

Incidence • 0. 5% to 3% of all patients treated with traditional antipsychotics • Recent 0. 01% to 0. 02% (Stubner, 2004, as cited in Strawn, Keck & Caroff, 2007). (? Due to atypical use) • Haloperidol implicated in ½ cases (potency, widespread use) Death in 10% of cases (Strawn, Keck & Caroff, 2007).
Risk Factors • • previous history of NMS/EPSE dehydration discontinuation of antiparkinsonian withdrawal of benzodiazepines history of organic brain syndrome use of high potency agents iron deficiency
Onset At any time - can develop rapidly Most cases when: • drug started • dosage increased • rapidly titrated Mild to severe - depending on individual
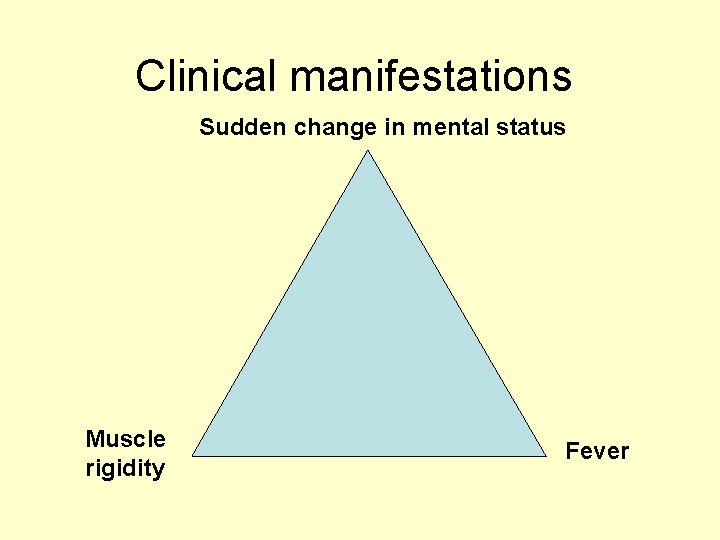
Clinical manifestations Sudden change in mental status Muscle rigidity Fever

Sudden change in mental status Mental state changes precede other signs in 80% of cases Clouding of consciousness ranging from: • confusion to stupor or coma • agitation, • delirium, and • catatonia
Fever • Hyperpyrexia > 38 °C of unknown origin (? caused by dopamine blockade in hypothalamus causing temperature dysregulation and profuse sweating)
Muscle Rigidity • Dystonia abrupt onset stiffening and rigidity in large muscles (especially head & neck) • Severe muscle rigidity produces excess body heat contributing to hyperpyrexia • Sometimes difficulty swallowing or a sensation of tongue thickening that rapidly worsens
Rigidity As the syndrome progresses: • increasing muscle rigidity can lead to diminished chest wall compliance, hypoventilation, and even respiratory failure. Other • EPSEs: parkinsonian tremors, akathisia • elevated or labile blood pressure • tachycardia, tachypnea, tremor, and urinary incontinence
Laboratory • Raised Creatine kinase (muscle enzyme) • Raise Myoglobinuria (muscle protein) • Creatine kinase rises 2 – 4 hours after muscle injury (indicator degree muscle damage), continued rise may indicate onset : • Rhabdomyolysis (skeletal muscle break down) releases myoglobin into circulation. • Once myoglobin in kidneys, it precipitates in renal tubules causing kidney damage and subsequent renal failure.
Lab: other • proteinuria secondary to stress/tissue damage • elevated white blood cell count • Arterial blood gas analysis - assess for adequate oxygenation and metabolic acidosis (Harrison & Mc. Erlane, 2008).
Prevention • • Conservative use of antipsychotics Reduction of risk factors Early diagnosis Prompt discontinuation of offending medications
Medical Management Depending on symptom severity and complications: • See table in handout (Woodbury & Woodbury, 1992 cited in Strawn, Keck & Caroff, 2007). • See video Brvar and Bunc (2007) pre and post Dantrolene
Re-challenge Anti-psychotics • • 30% risk of developing again Check reports on previous episodes for accuracy Clearly documented indications for antipsychotics Consider alternative medications Reduce risk factors Rechallenge at least 2/52 after recovery from NMS Use low doses of low-potency conventional antipsychotics or atypical antipsychotics • Titrate gradually after a test dose • Monitor for early signs of NMS • Obtain informed consent from patients/family regarding benefits of antipsychotic versus risk recurrence (Strawn, Keck, & Caroff, 2007).
Resources Neuroleptic Malignant Syndrome Information Service www. nmsis. org
References Brvar, M. , & Bunc, M. (2007). Video of dantrolene effectiveness on neuroleptic malignant syndrome associated muscular rigidity and tremor. Critical Care 11(3), 415. Fink, M. (1996). Neuroleptic malignant syndrome and catatonia: One entity or two? . Biological Psychiatry, 39, 1 -4. Harrison, P. A. , & Mc. Erlane, K. S. (2008 ). Neuroleptic malignant syndrome American Journal of Nursing, 108(7), 35 -38. Strawn, J. R. , Keck, P. E. , & Caroff, S. N. (2007). Neuroleptic malignant syndrome. American Journal of Psychiatry, 164(6), 870 -876.
 Malignant neuroleptic syndrome
Malignant neuroleptic syndrome Neuroleptic malignant syndrome
Neuroleptic malignant syndrome Catatonic behavior example
Catatonic behavior example Neuroleptic drug
Neuroleptic drug Mesolimbic
Mesolimbic Benign or malignant
Benign or malignant Carotonemia
Carotonemia Malignant hypertension management
Malignant hypertension management Peter hino md
Peter hino md Tom kitwood malignant social psychology
Tom kitwood malignant social psychology Hypertensive encephalopathy
Hypertensive encephalopathy Malignant hypertention
Malignant hypertention Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Malignant mesothelioma
Malignant mesothelioma Perdida de polaridad celular
Perdida de polaridad celular Lipoma
Lipoma Carcinoma in situ
Carcinoma in situ Benign and malignant tumor difference
Benign and malignant tumor difference Hypertensive emergency
Hypertensive emergency Local invasion
Local invasion Malignant hypertension ppt
Malignant hypertension ppt