ORAL MOUTHCAVITY Oral cavity mouth Extends from oral


- Slides: 49
ORAL (MOUTH)CAVITY
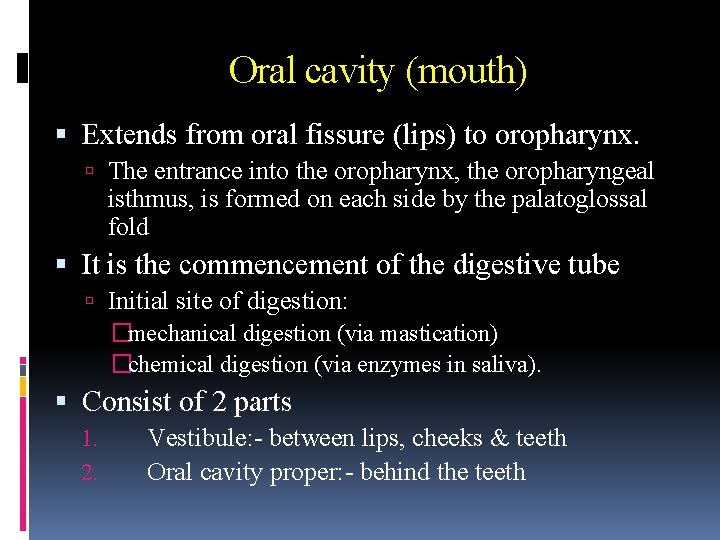
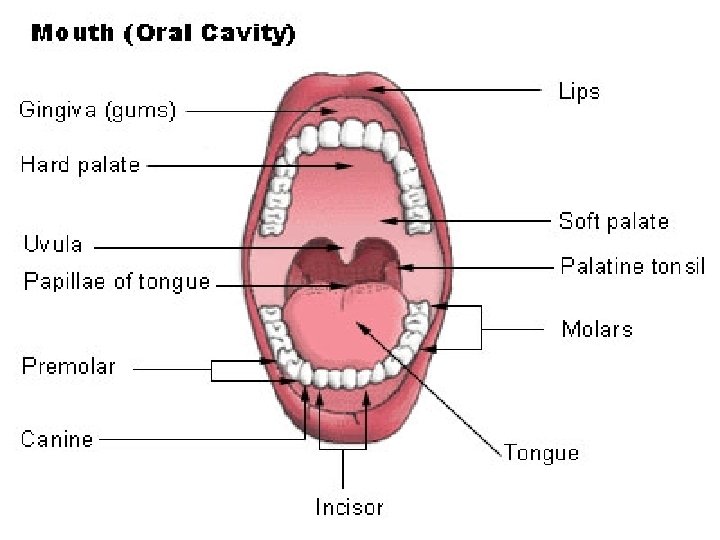
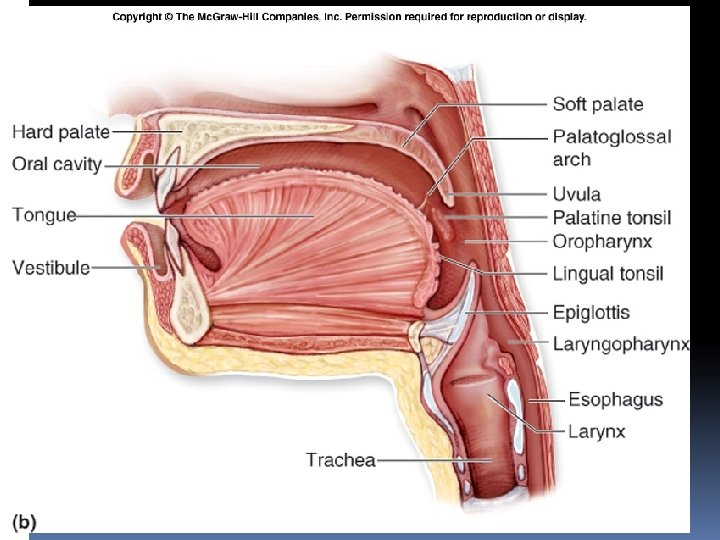
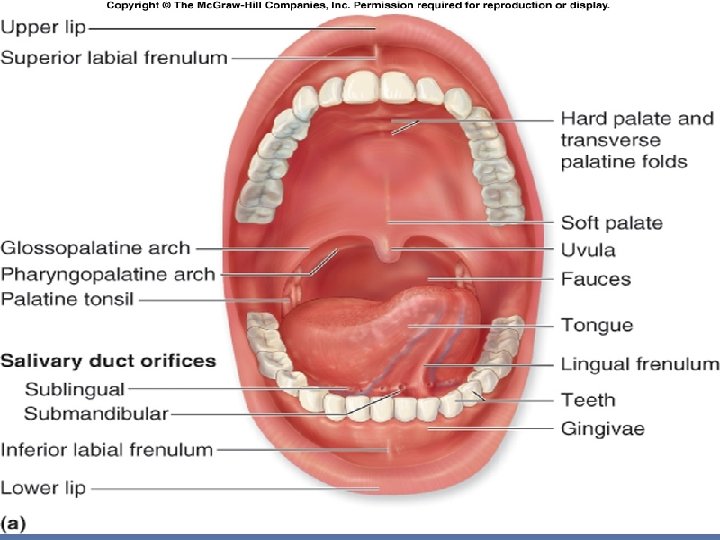
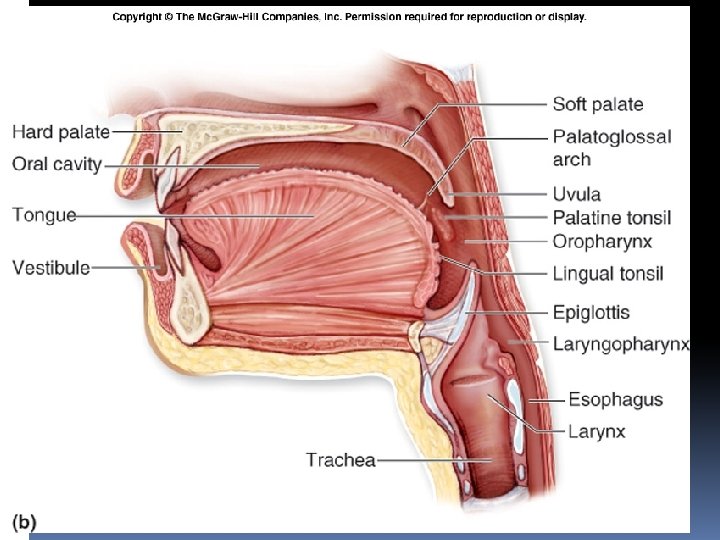
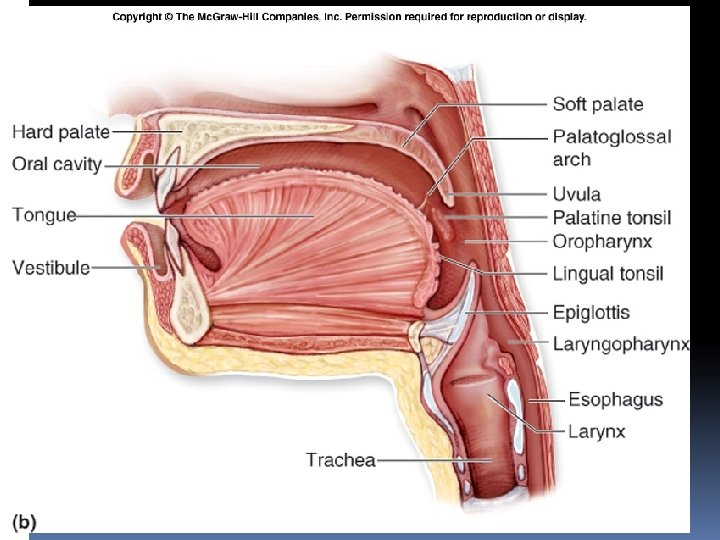
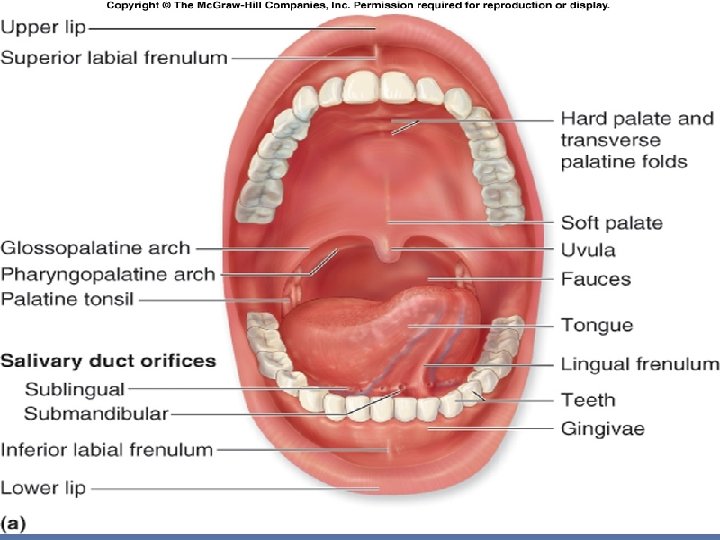
Oral cavity (mouth) Extends from oral fissure (lips) to oropharynx. The entrance into the oropharynx, the oropharyngeal isthmus, is formed on each side by the palatoglossal fold It is the commencement of the digestive tube Initial site of digestion: �mechanical digestion (via mastication) �chemical digestion (via enzymes in saliva). Consist of 2 parts 1. Vestibule: - between lips, cheeks & teeth 2. Oral cavity proper: - behind the teeth
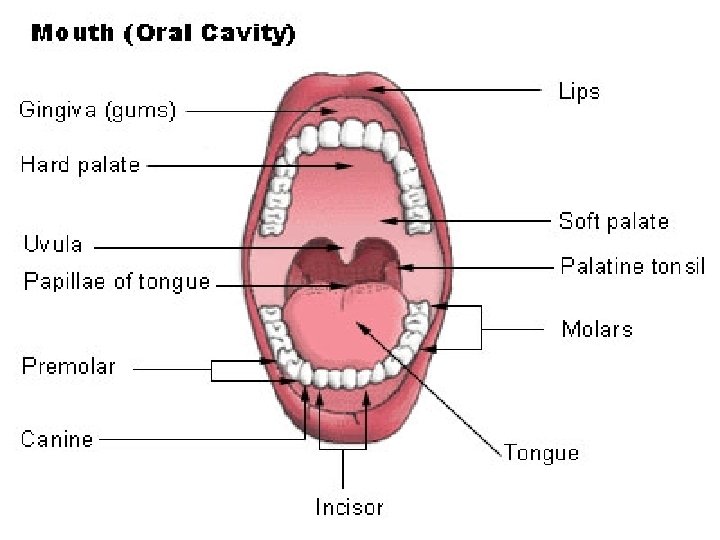
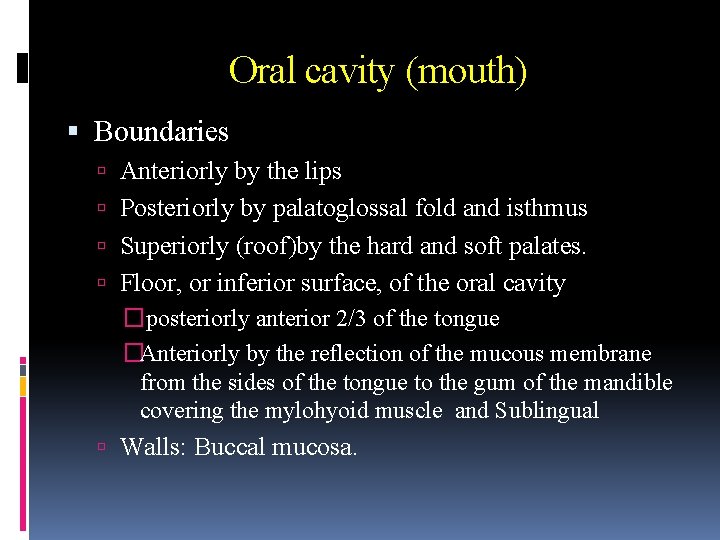
Oral cavity (mouth) Boundaries Anteriorly by the lips Posteriorly by palatoglossal fold and isthmus Superiorly (roof)by the hard and soft palates. Floor, or inferior surface, of the oral cavity � posteriorly anterior 2/3 of the tongue �Anteriorly by the reflection of the mucous membrane from the sides of the tongue to the gum of the mandible covering the mylohyoid muscle and Sublingual Walls: Buccal mucosa.
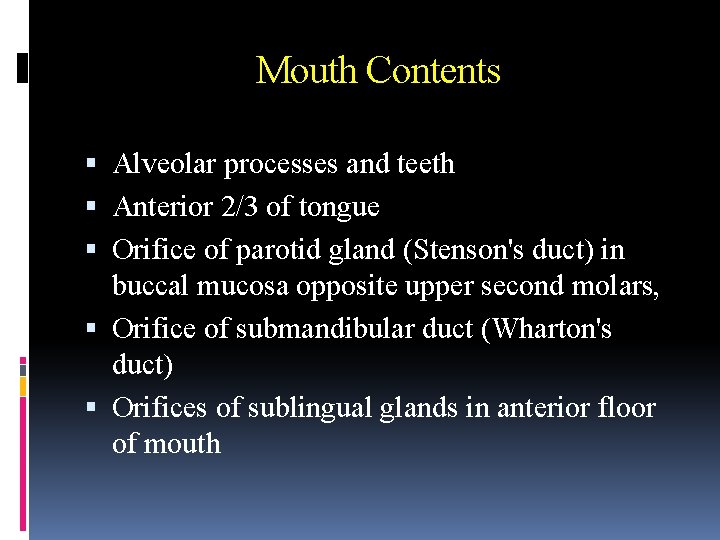
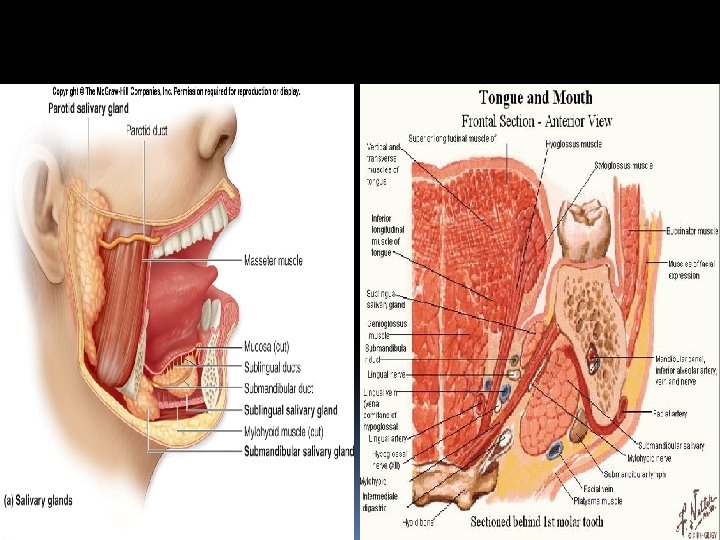
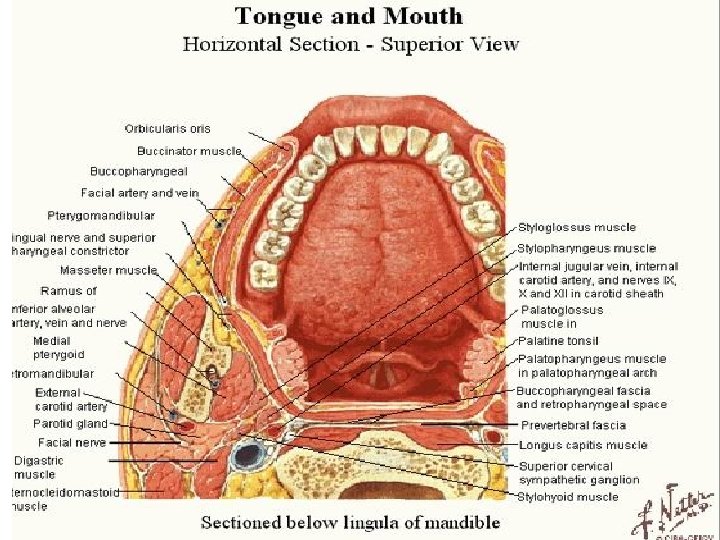
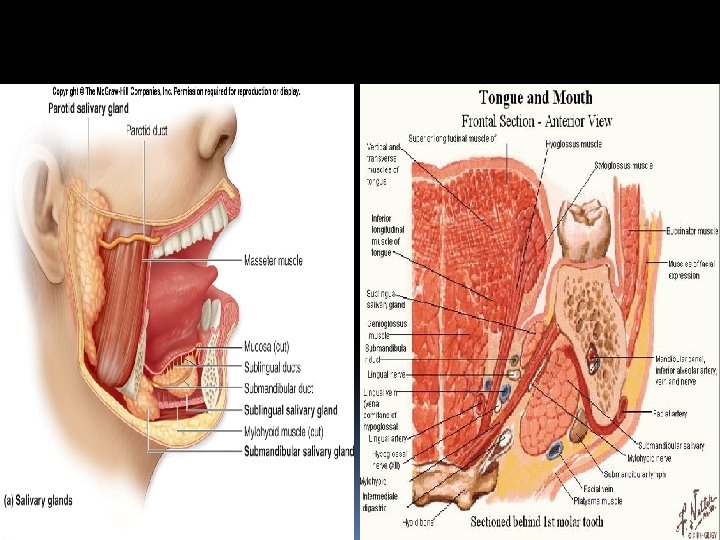
Mouth Contents Alveolar processes and teeth Anterior 2/3 of tongue Orifice of parotid gland (Stenson's duct) in buccal mucosa opposite upper second molars, Orifice of submandibular duct (Wharton's duct) Orifices of sublingual glands in anterior floor of mouth
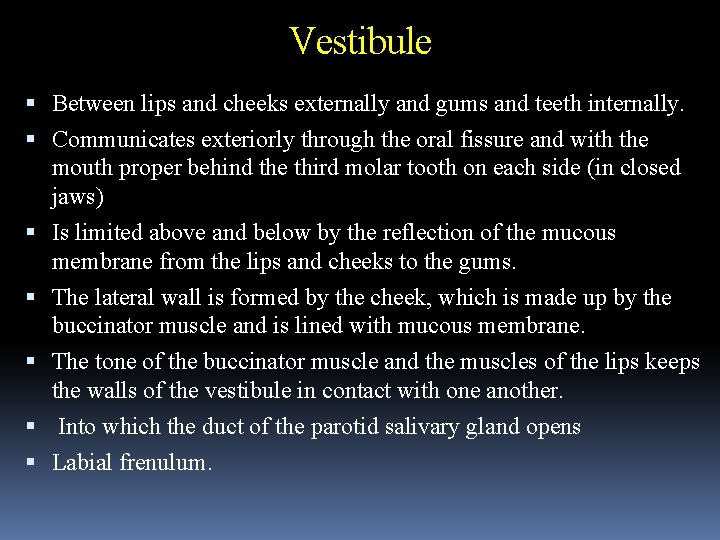
Vestibule Between lips and cheeks externally and gums and teeth internally. Communicates exteriorly through the oral fissure and with the mouth proper behind the third molar tooth on each side (in closed jaws) Is limited above and below by the reflection of the mucous membrane from the lips and cheeks to the gums. The lateral wall is formed by the cheek, which is made up by the buccinator muscle and is lined with mucous membrane. The tone of the buccinator muscle and the muscles of the lips keeps the walls of the vestibule in contact with one another. Into which the duct of the parotid salivary gland opens Labial frenulum.
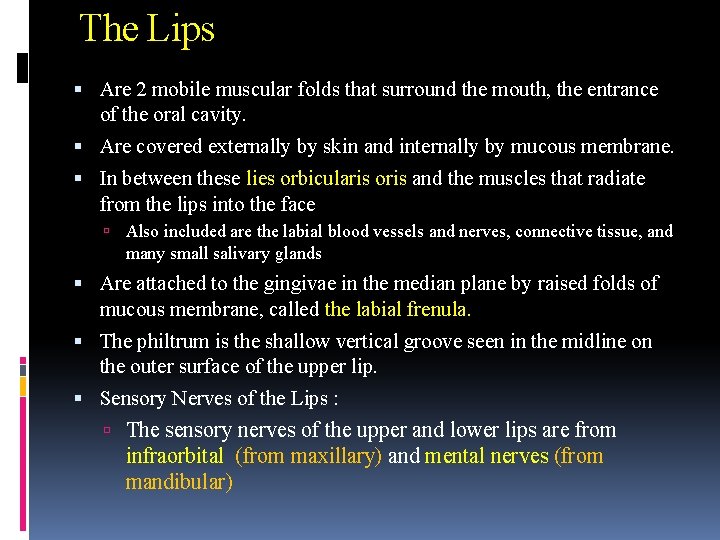
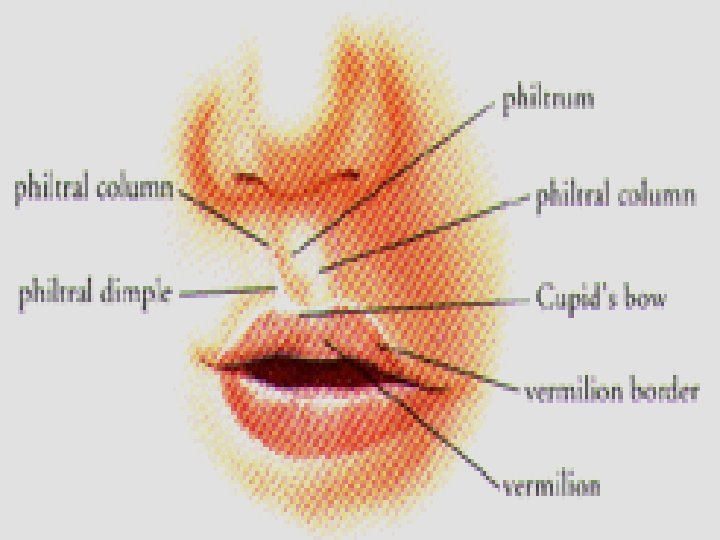
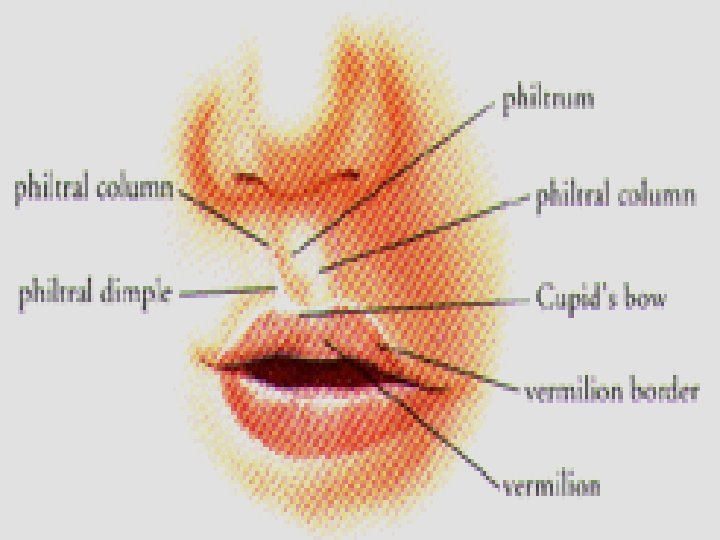
The Lips Are 2 mobile muscular folds that surround the mouth, the entrance of the oral cavity. Are covered externally by skin and internally by mucous membrane. In between these lies orbicularis oris and the muscles that radiate from the lips into the face Also included are the labial blood vessels and nerves, connective tissue, and many small salivary glands Are attached to the gingivae in the median plane by raised folds of mucous membrane, called the labial frenula. The philtrum is the shallow vertical groove seen in the midline on the outer surface of the upper lip. Sensory Nerves of the Lips : The sensory nerves of the upper and lower lips are from infraorbital (from maxillary) and mental nerves (from mandibular)
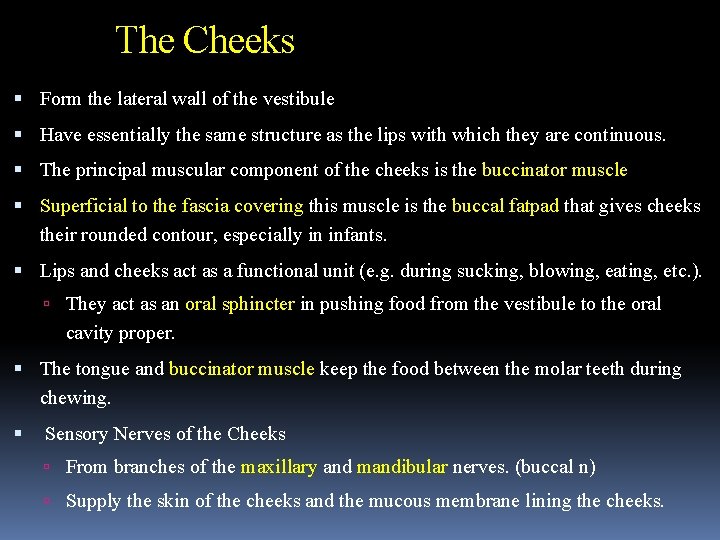
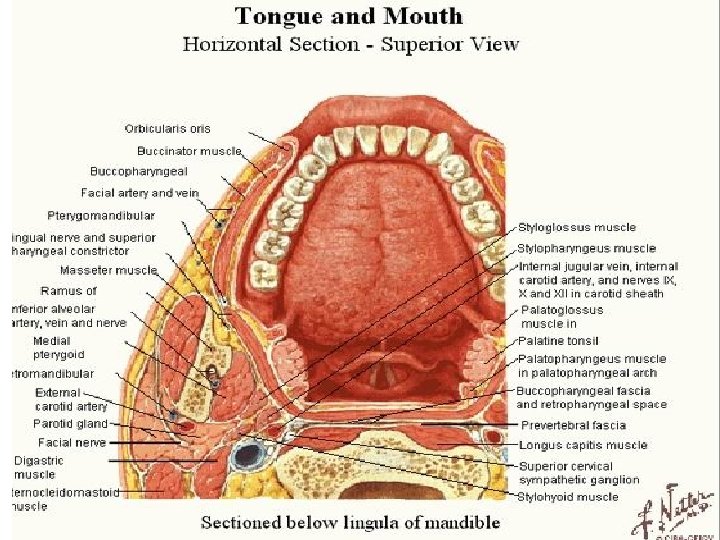
The Cheeks Form the lateral wall of the vestibule Have essentially the same structure as the lips with which they are continuous. The principal muscular component of the cheeks is the buccinator muscle Superficial to the fascia covering this muscle is the buccal fatpad that gives cheeks their rounded contour, especially in infants. Lips and cheeks act as a functional unit (e. g. during sucking, blowing, eating, etc. ). They act as an oral sphincter in pushing food from the vestibule to the oral cavity proper. The tongue and buccinator muscle keep the food between the molar teeth during chewing. Sensory Nerves of the Cheeks From branches of the maxillary and mandibular nerves. (buccal n) Supply the skin of the cheeks and the mucous membrane lining the cheeks.
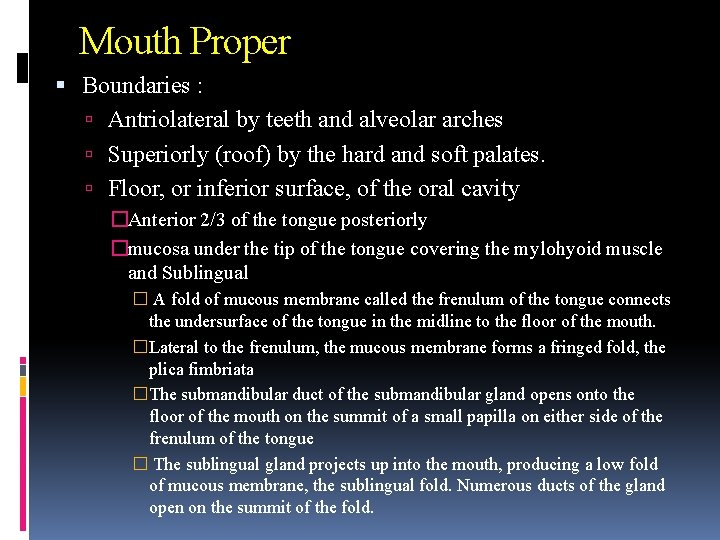
Mouth Proper Boundaries : Antriolateral by teeth and alveolar arches Superiorly (roof) by the hard and soft palates. Floor, or inferior surface, of the oral cavity �Anterior 2/3 of the tongue posteriorly �mucosa under the tip of the tongue covering the mylohyoid muscle and Sublingual � A fold of mucous membrane called the frenulum of the tongue connects the undersurface of the tongue in the midline to the floor of the mouth. �Lateral to the frenulum, the mucous membrane forms a fringed fold, the plica fimbriata �The submandibular duct of the submandibular gland opens onto the floor of the mouth on the summit of a small papilla on either side of the frenulum of the tongue � The sublingual gland projects up into the mouth, producing a low fold of mucous membrane, the sublingual fold. Numerous ducts of the gland open on the summit of the fold.
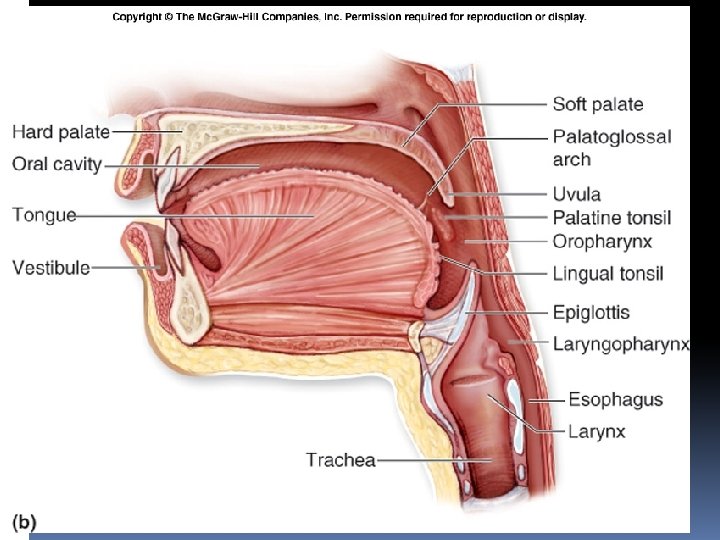
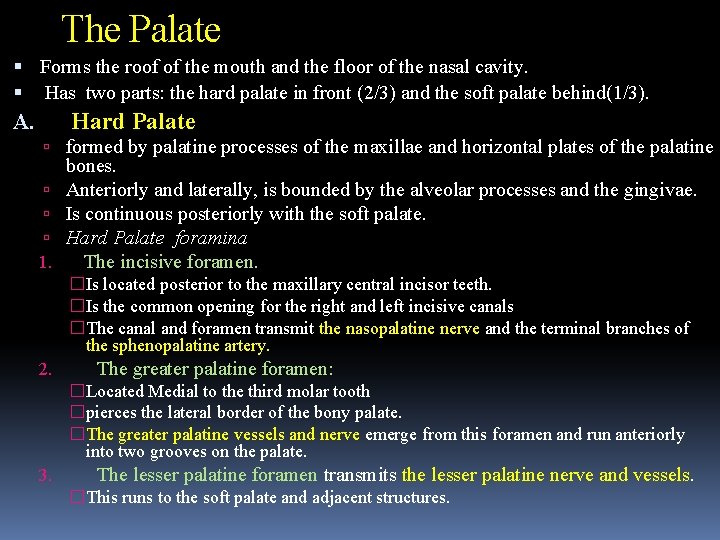
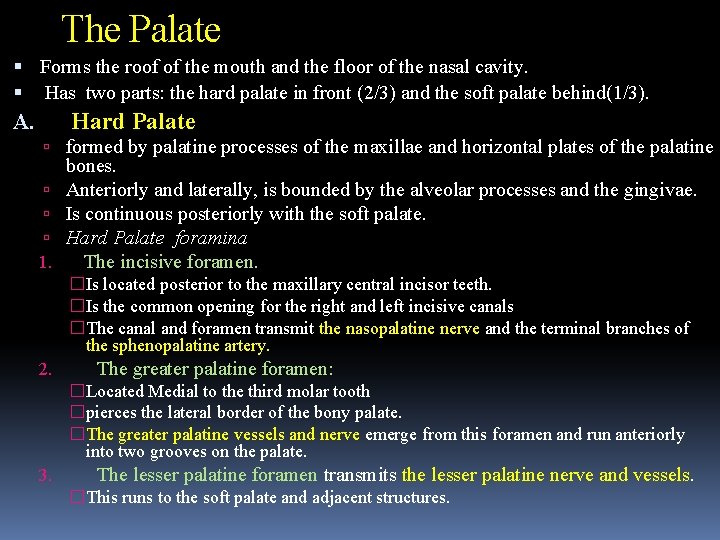
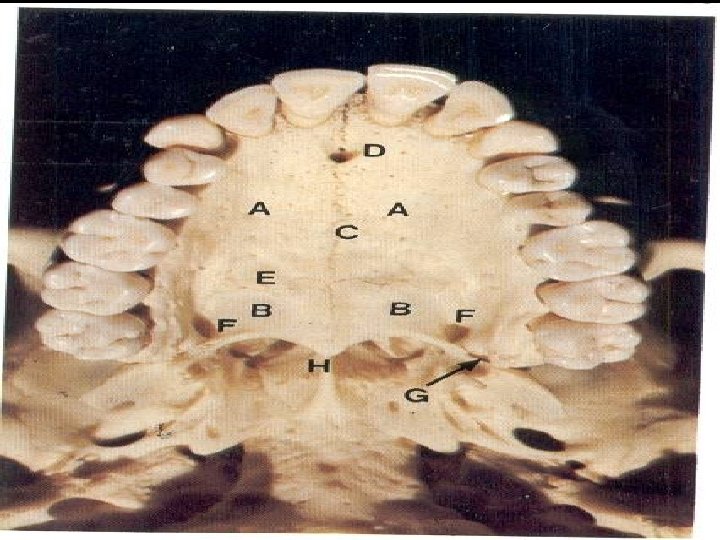
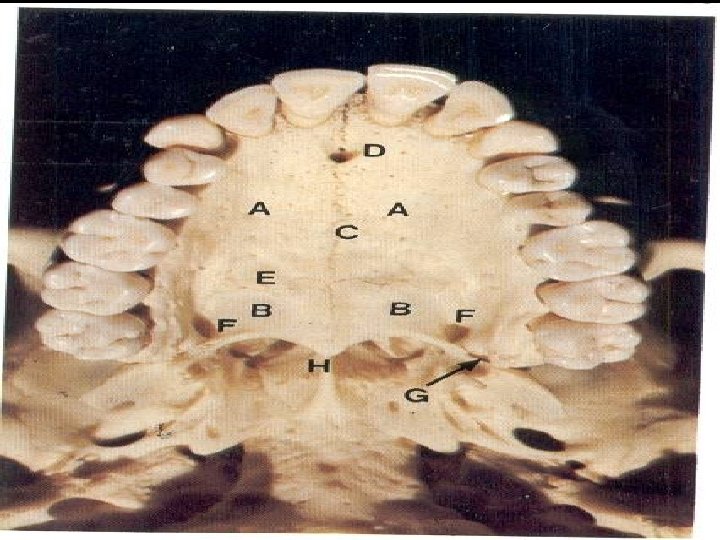
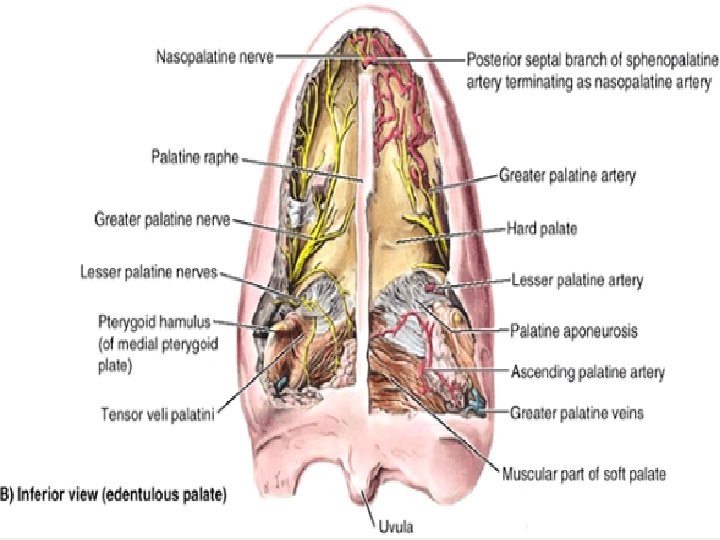
The Palate Forms the roof of the mouth and the floor of the nasal cavity. Has two parts: the hard palate in front (2/3) and the soft palate behind(1/3). Hard Palate A. formed by palatine processes of the maxillae and horizontal plates of the palatine 1. bones. Anteriorly and laterally, is bounded by the alveolar processes and the gingivae. Is continuous posteriorly with the soft palate. Hard Palate foramina The incisive foramen. �Is located posterior to the maxillary central incisor teeth. �Is the common opening for the right and left incisive canals �The canal and foramen transmit the nasopalatine nerve and the terminal branches of the sphenopalatine artery. 2. The greater palatine foramen: �Located Medial to the third molar tooth �pierces the lateral border of the bony palate. �The greater palatine vessels and nerve emerge from this foramen and run anteriorly into two grooves on the palate. 3. The lesser palatine foramen transmits the lesser palatine nerve and vessels. �This runs to the soft palate and adjacent structures.
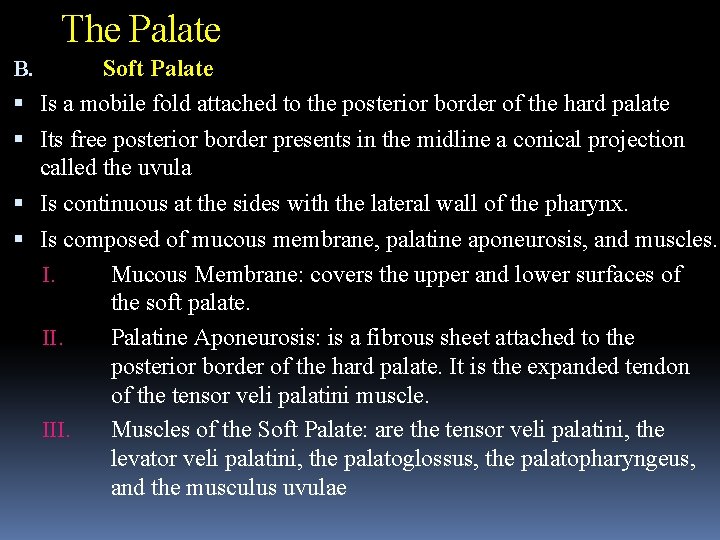
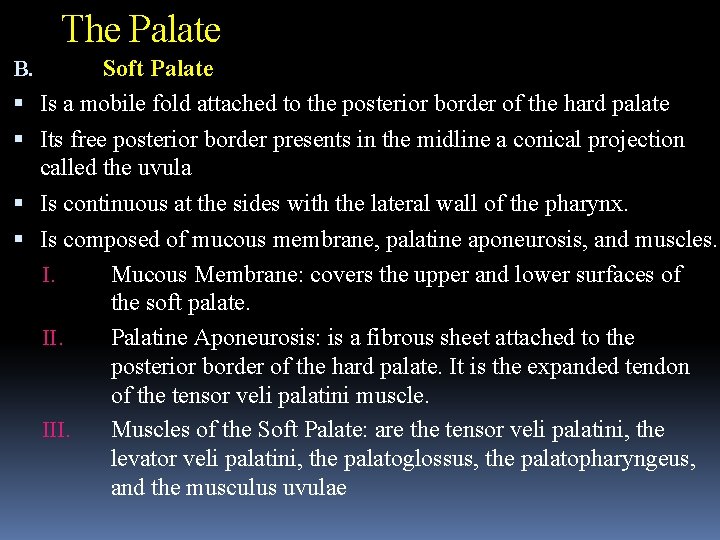
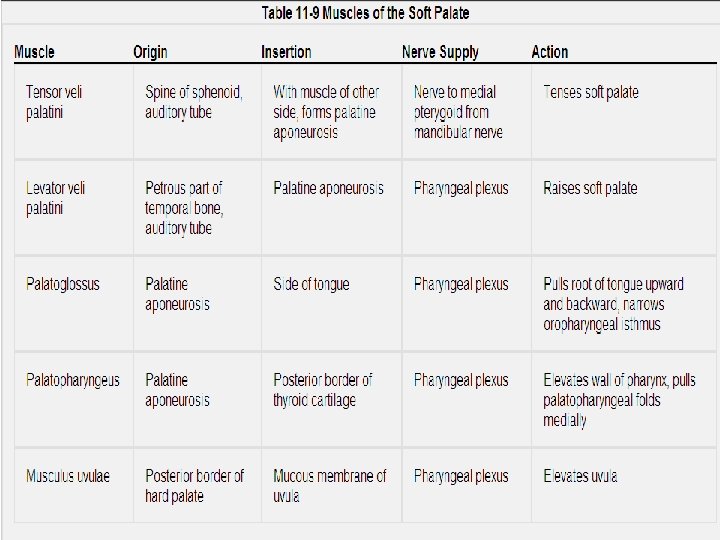
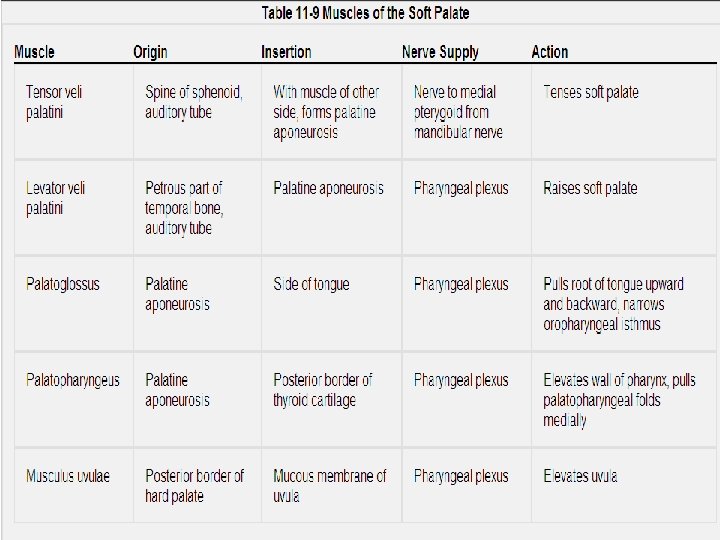
The Palate B. Soft Palate Is a mobile fold attached to the posterior border of the hard palate Its free posterior border presents in the midline a conical projection called the uvula Is continuous at the sides with the lateral wall of the pharynx. Is composed of mucous membrane, palatine aponeurosis, and muscles. I. Mucous Membrane: covers the upper and lower surfaces of the soft palate. II. Palatine Aponeurosis: is a fibrous sheet attached to the posterior border of the hard palate. It is the expanded tendon of the tensor veli palatini muscle. III. Muscles of the Soft Palate: are the tensor veli palatini, the levator veli palatini, the palatoglossus, the palatopharyngeus, and the musculus uvulae
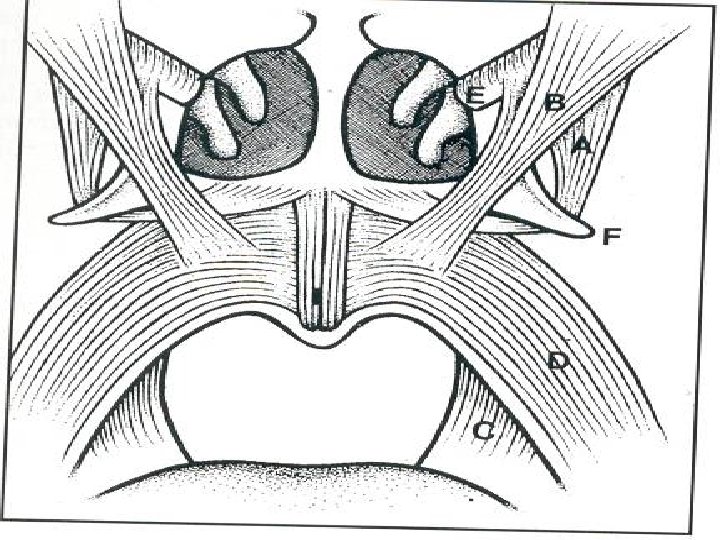
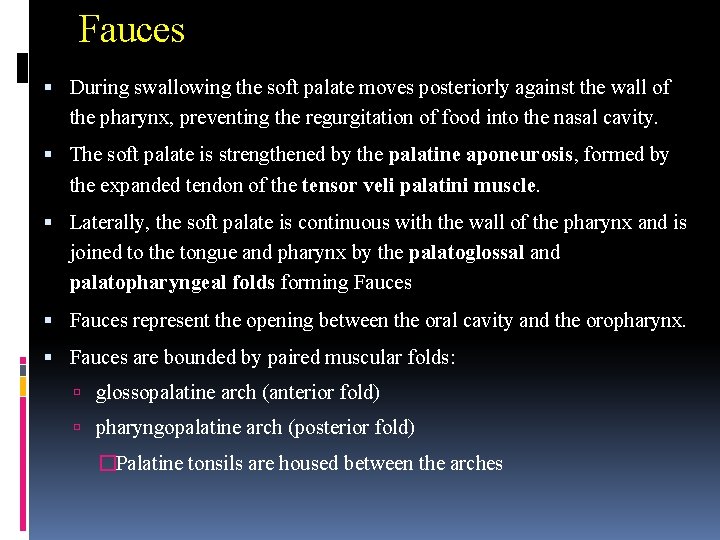
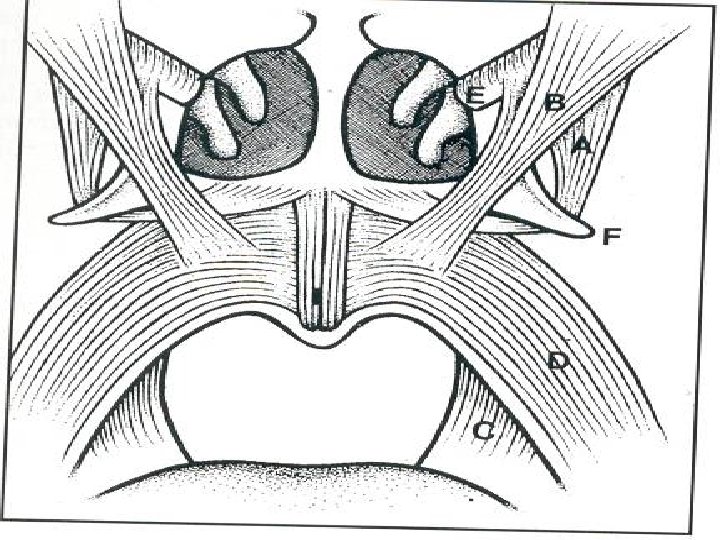
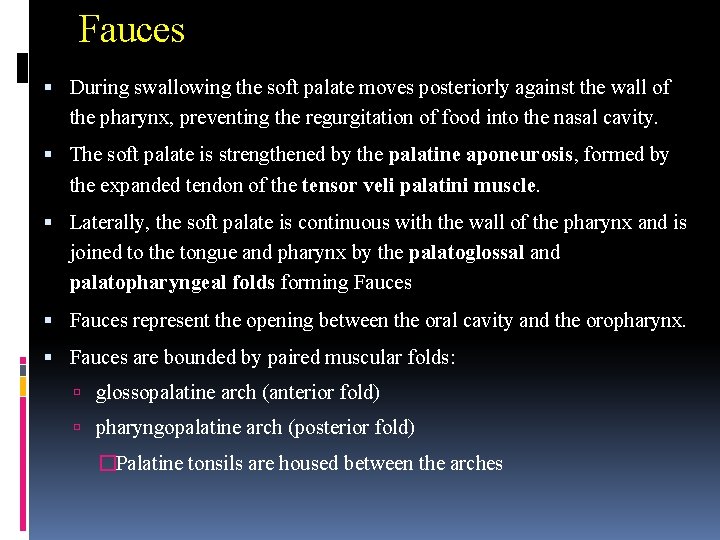
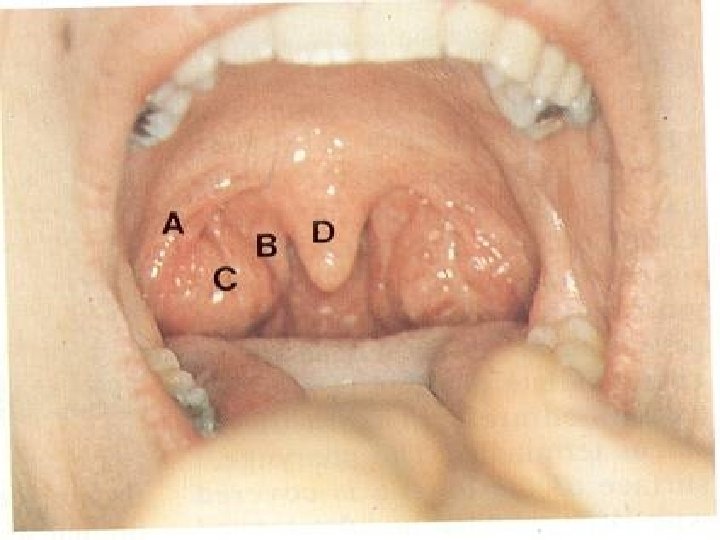
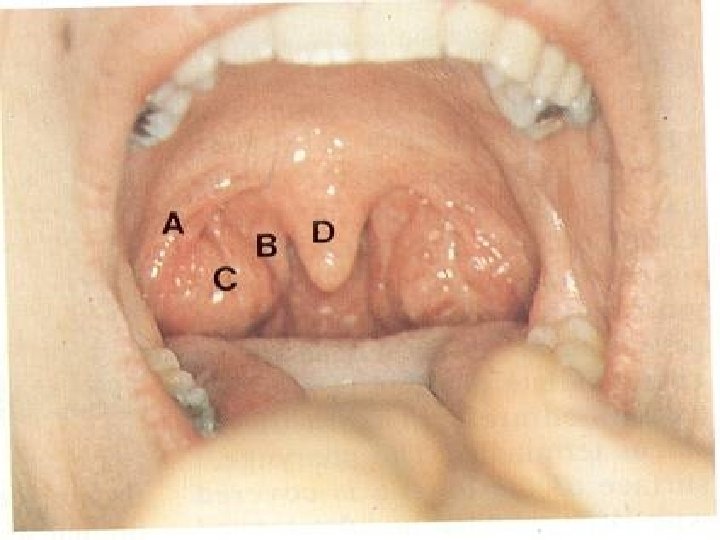
Fauces During swallowing the soft palate moves posteriorly against the wall of the pharynx, preventing the regurgitation of food into the nasal cavity. The soft palate is strengthened by the palatine aponeurosis, formed by the expanded tendon of the tensor veli palatini muscle. Laterally, the soft palate is continuous with the wall of the pharynx and is joined to the tongue and pharynx by the palatoglossal and palatopharyngeal folds forming Fauces represent the opening between the oral cavity and the oropharynx. Fauces are bounded by paired muscular folds: glossopalatine arch (anterior fold) pharyngopalatine arch (posterior fold) �Palatine tonsils are housed between the arches
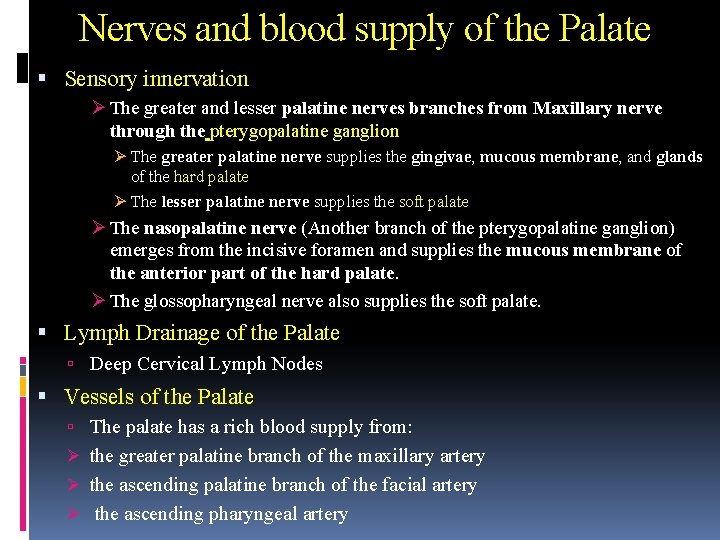
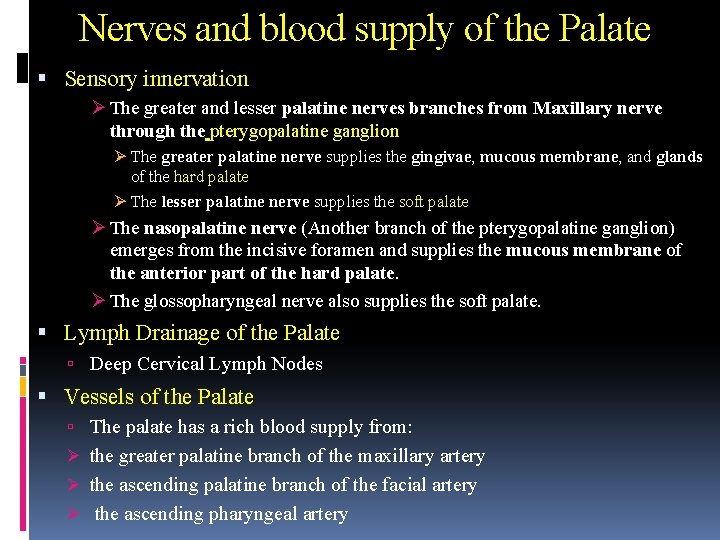
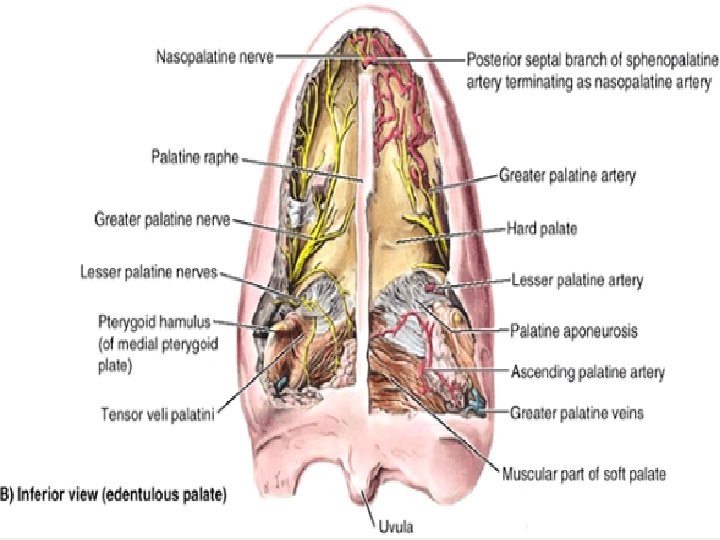
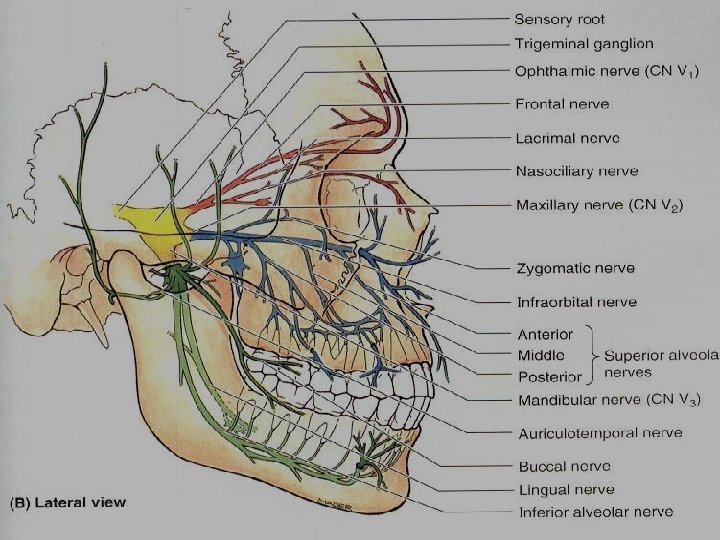
Nerves and blood supply of the Palate Sensory innervation Ø The greater and lesser palatine nerves branches from Maxillary nerve through the pterygopalatine ganglion Ø The greater palatine nerve supplies the gingivae, mucous membrane, and glands of the hard palate Ø The lesser palatine nerve supplies the soft palate Ø The nasopalatine nerve (Another branch of the pterygopalatine ganglion) emerges from the incisive foramen and supplies the mucous membrane of the anterior part of the hard palate. Ø The glossopharyngeal nerve also supplies the soft palate. Lymph Drainage of the Palate Deep Cervical Lymph Nodes Vessels of the Palate The palate has a rich blood supply from: Ø the greater palatine branch of the maxillary artery Ø the ascending palatine branch of the facial artery Ø the ascending pharyngeal artery
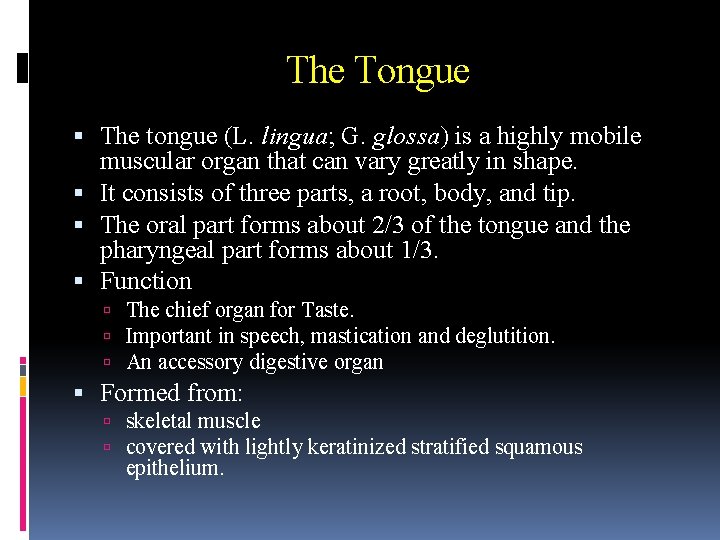
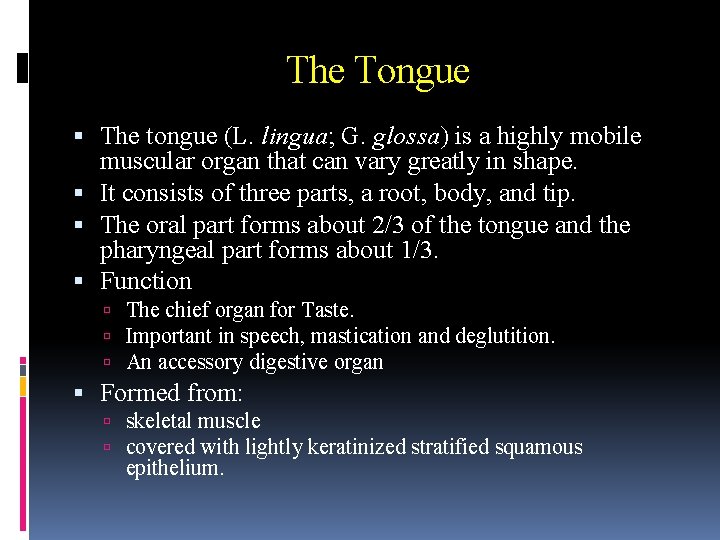
The Tongue The tongue (L. lingua; G. glossa) is a highly mobile muscular organ that can vary greatly in shape. It consists of three parts, a root, body, and tip. The oral part forms about 2/3 of the tongue and the pharyngeal part forms about 1/3. Function The chief organ for Taste. Important in speech, mastication and deglutition. An accessory digestive organ Formed from: skeletal muscle covered with lightly keratinized stratified squamous epithelium.
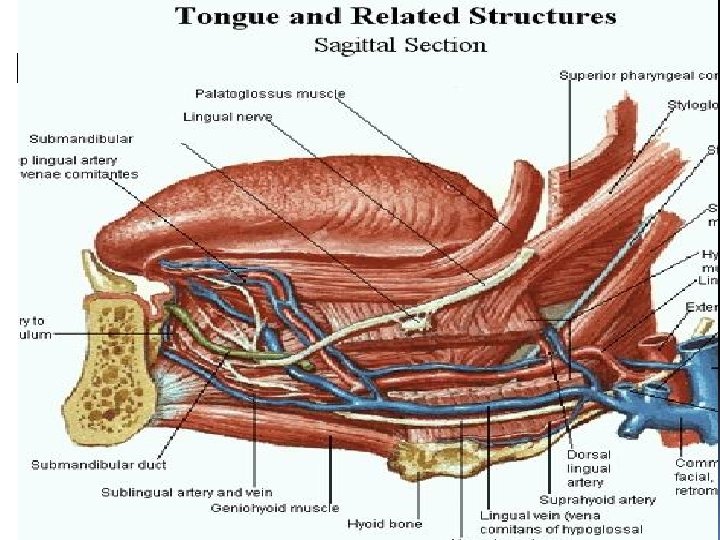
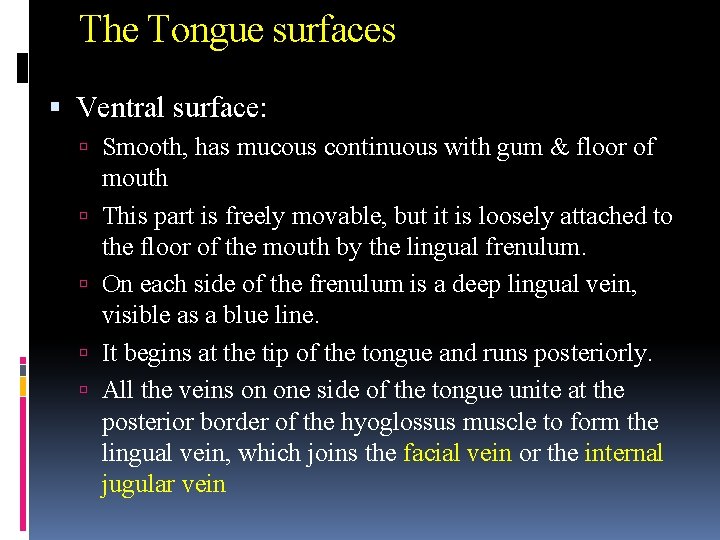
The Tongue surfaces Ventral surface: Smooth, has mucous continuous with gum & floor of mouth This part is freely movable, but it is loosely attached to the floor of the mouth by the lingual frenulum. On each side of the frenulum is a deep lingual vein, visible as a blue line. It begins at the tip of the tongue and runs posteriorly. All the veins on one side of the tongue unite at the posterior border of the hyoglossus muscle to form the lingual vein, which joins the facial vein or the internal jugular vein
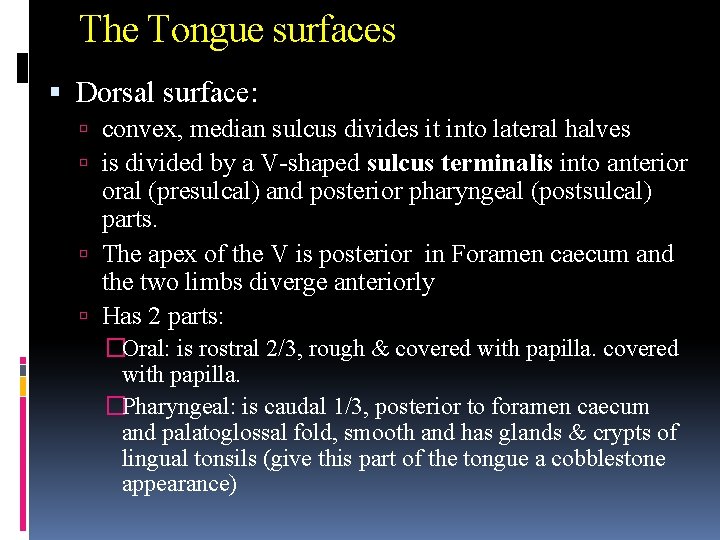
The Tongue surfaces Dorsal surface: convex, median sulcus divides it into lateral halves is divided by a V-shaped sulcus terminalis into anterior oral (presulcal) and posterior pharyngeal (postsulcal) parts. The apex of the V is posterior in Foramen caecum and the two limbs diverge anteriorly Has 2 parts: �Oral: is rostral 2/3, rough & covered with papilla. �Pharyngeal: is caudal 1/3, posterior to foramen caecum and palatoglossal fold, smooth and has glands & crypts of lingual tonsils (give this part of the tongue a cobblestone appearance)
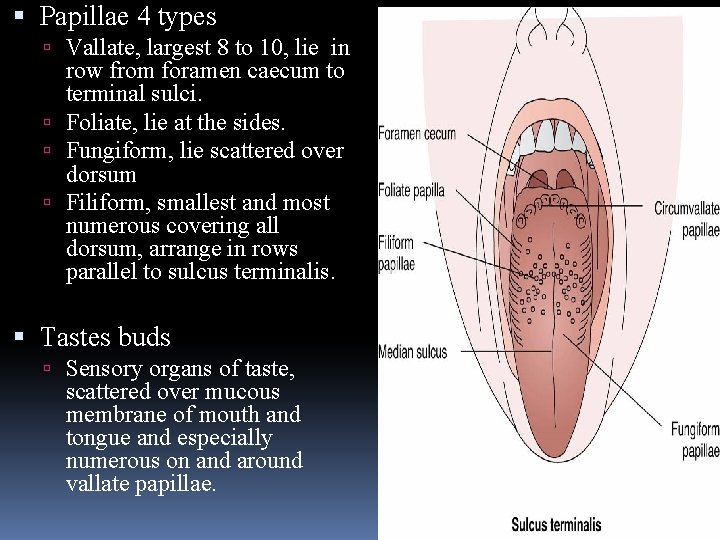
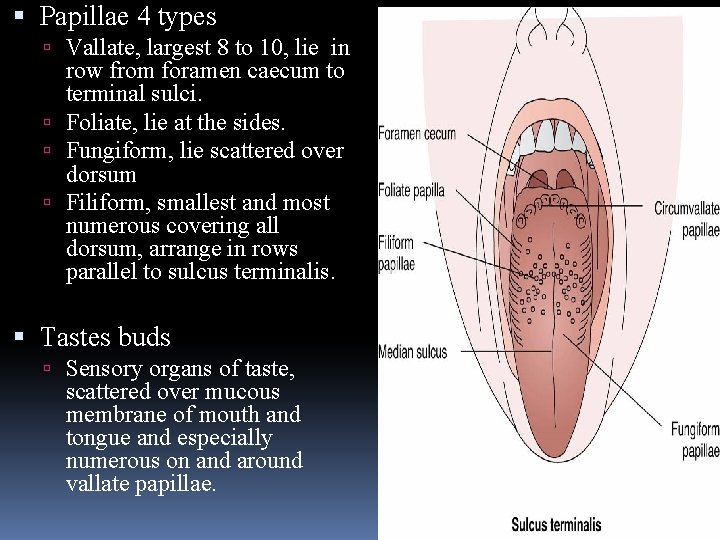
Papillae 4 types Vallate, largest 8 to 10, lie in row from foramen caecum to terminal sulci. Foliate, lie at the sides. Fungiform, lie scattered over dorsum Filiform, smallest and most numerous covering all dorsum, arrange in rows parallel to sulcus terminalis. Tastes buds Sensory organs of taste, scattered over mucous membrane of mouth and tongue and especially numerous on and around vallate papillae.
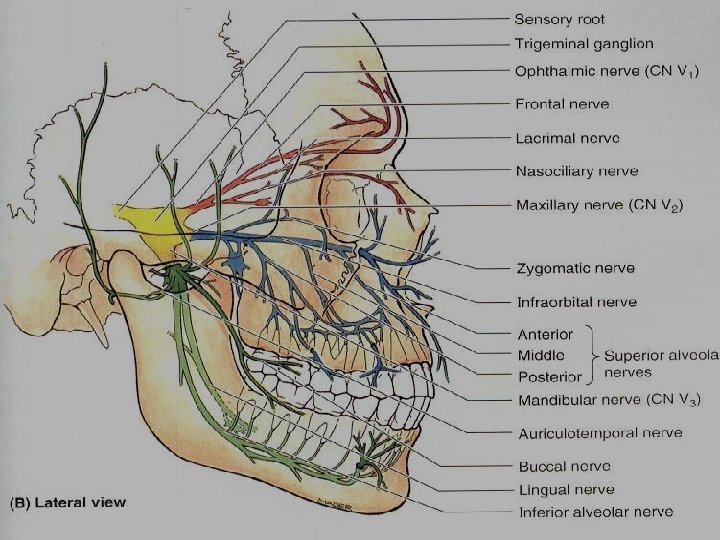
Nerves of the tongue Sensory a. General sensation = lingual br. Mandibular CN V for ant. 2/3, For caudal 1/3, Lingual br, of glossopharyngeal CN 1 X, and lingual br. of superior laryngeal of vagus near epiglottis. b. Special sensation ( taste) 1. taste buds on ant. 2/3, thru lingual, chorda tympani & nervus intermedius thru Facial CNV 11 2. buds at caudal 1/3, lingual br, of glossopharyngeal CN 1 X 3. buds at epiglottic region, laryngeal br. Of vagus CNX Motor: Motor Innervation. All muscles by hypoglossal nerve (CN XII) except palatoglossus muscle (by the pharyngeal plexus)
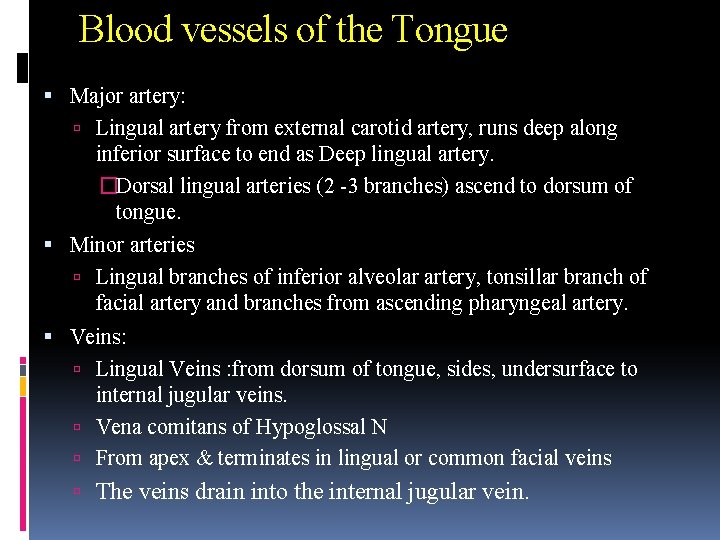
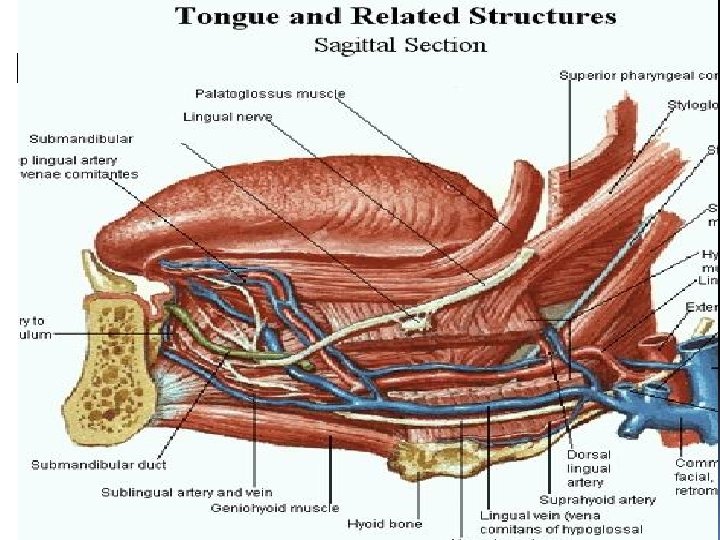
Blood vessels of the Tongue Major artery: Lingual artery from external carotid artery, runs deep along inferior surface to end as Deep lingual artery. �Dorsal lingual arteries (2 -3 branches) ascend to dorsum of tongue. Minor arteries Lingual branches of inferior alveolar artery, tonsillar branch of facial artery and branches from ascending pharyngeal artery. Veins: Lingual Veins : from dorsum of tongue, sides, undersurface to internal jugular veins. Vena comitans of Hypoglossal N From apex & terminates in lingual or common facial veins The veins drain into the internal jugular vein.
Lymph Drainage Tip: Submental lymph nodes Sides of the anterior two thirds: Submandibular and deep cervical lymph nodes Posterior third: Deep cervical lymph nodes Remember: Taste Modalities: Sweet at TIP, Bitter Towards ROOT, Salty at SIDES & TIP, Sour at SIDES.
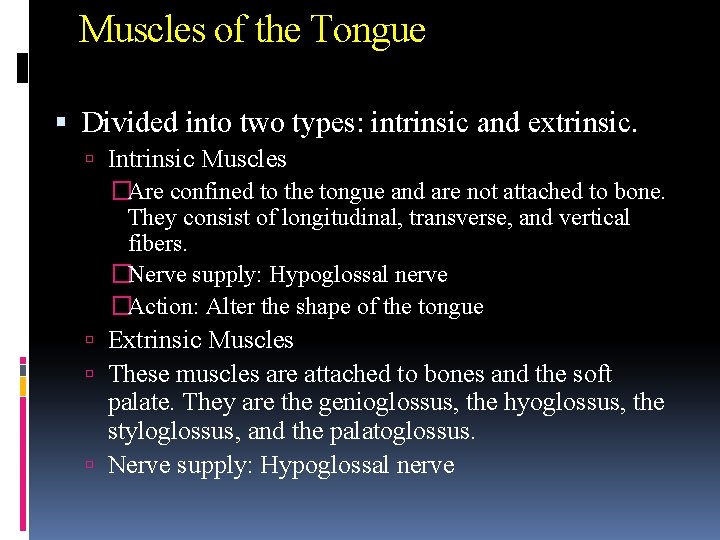
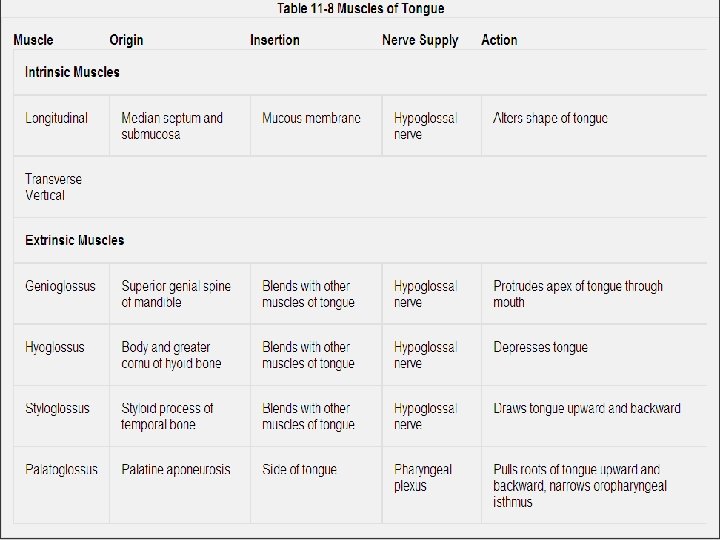
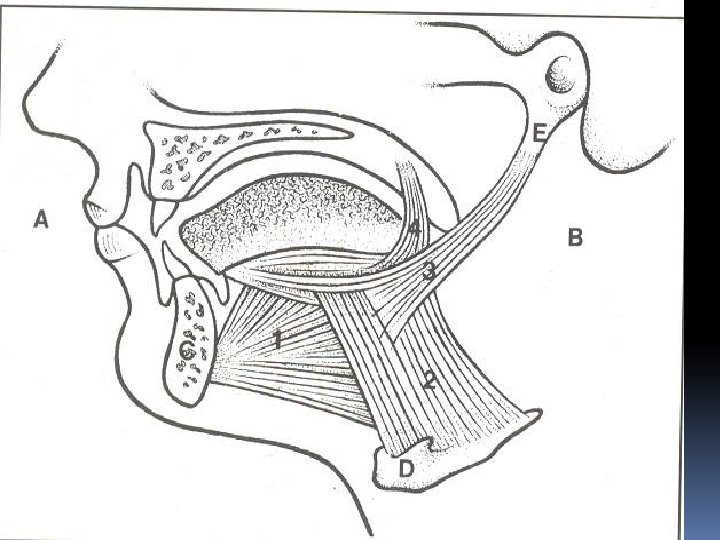
Muscles of the Tongue Divided into two types: intrinsic and extrinsic. Intrinsic Muscles �Are confined to the tongue and are not attached to bone. They consist of longitudinal, transverse, and vertical fibers. �Nerve supply: Hypoglossal nerve �Action: Alter the shape of the tongue Extrinsic Muscles These muscles are attached to bones and the soft palate. They are the genioglossus, the hyoglossus, the styloglossus, and the palatoglossus. Nerve supply: Hypoglossal nerve
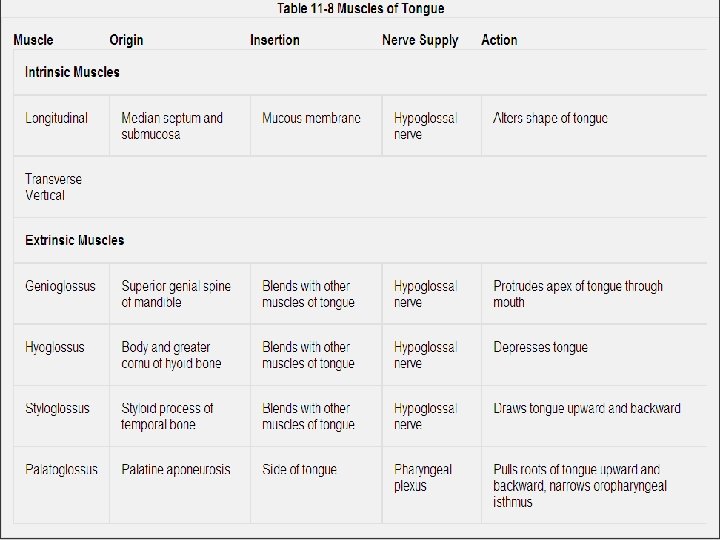

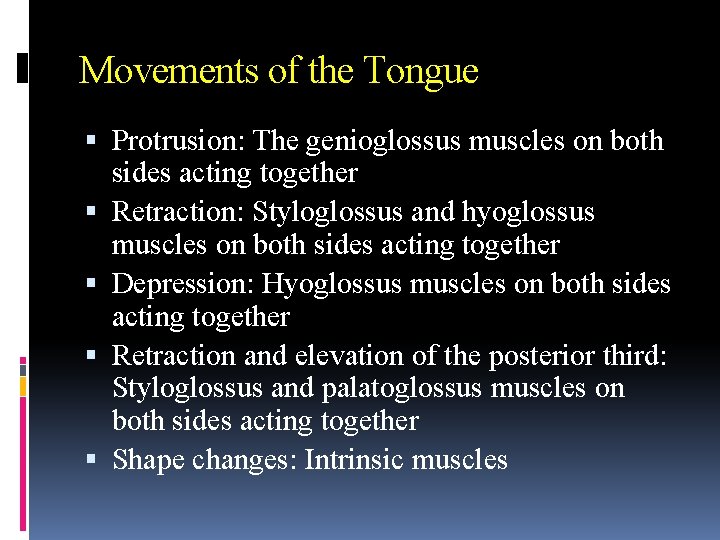
Movements of the Tongue Protrusion: The genioglossus muscles on both sides acting together Retraction: Styloglossus and hyoglossus muscles on both sides acting together Depression: Hyoglossus muscles on both sides acting together Retraction and elevation of the posterior third: Styloglossus and palatoglossus muscles on both sides acting together Shape changes: Intrinsic muscles
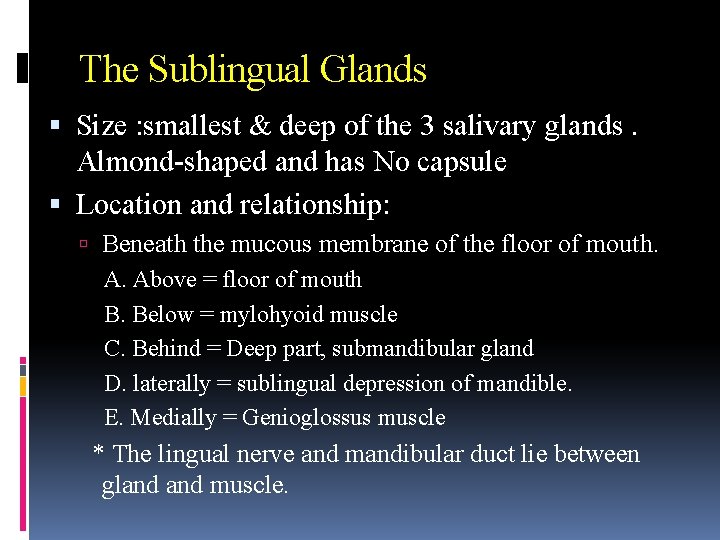
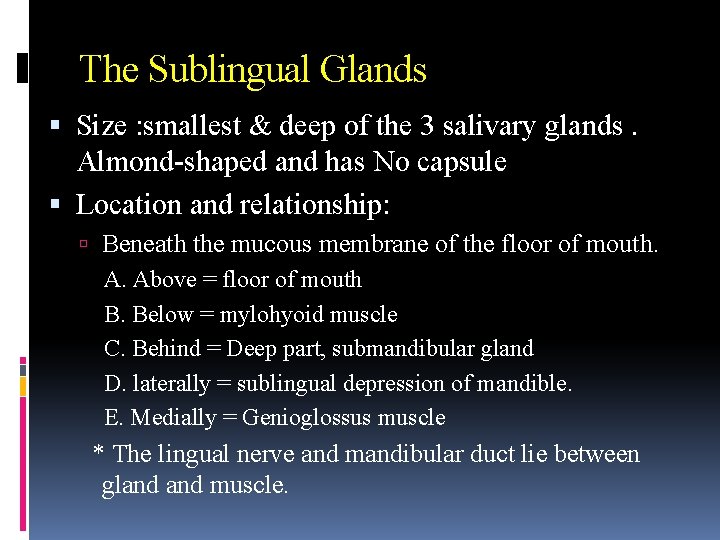
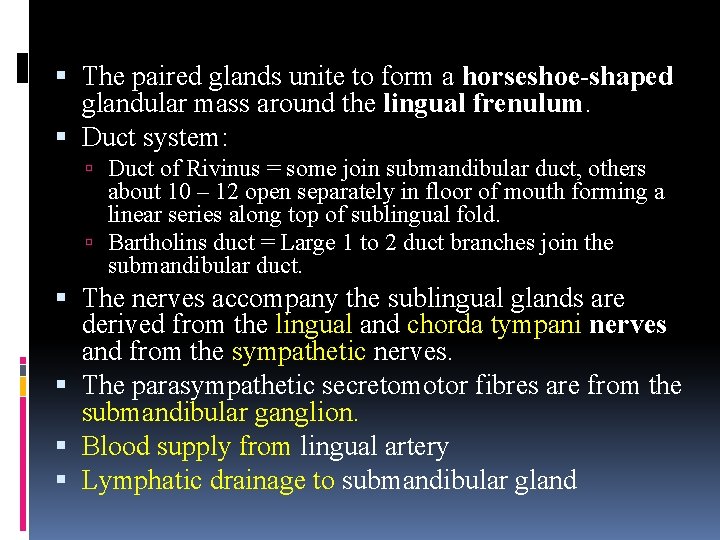
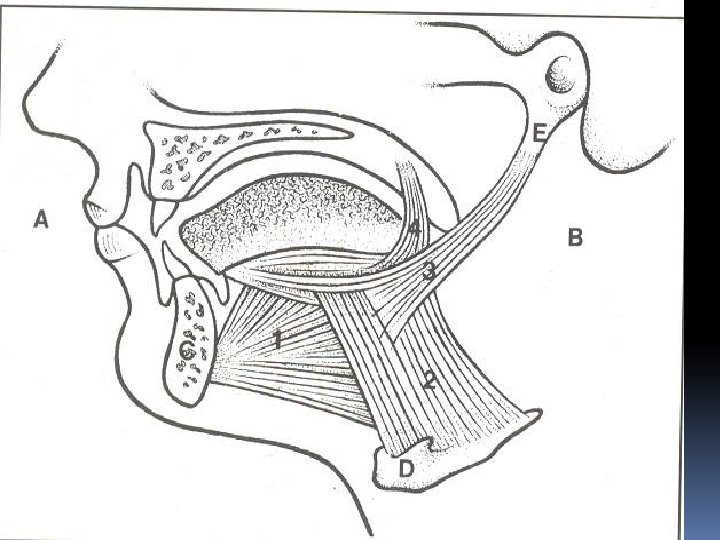
The Sublingual Glands Size : smallest & deep of the 3 salivary glands. Almond-shaped and has No capsule Location and relationship: Beneath the mucous membrane of the floor of mouth. A. Above = floor of mouth B. Below = mylohyoid muscle C. Behind = Deep part, submandibular gland D. laterally = sublingual depression of mandible. E. Medially = Genioglossus muscle * The lingual nerve and mandibular duct lie between gland muscle.
The paired glands unite to form a horseshoe-shaped glandular mass around the lingual frenulum. Duct system: Duct of Rivinus = some join submandibular duct, others about 10 – 12 open separately in floor of mouth forming a linear series along top of sublingual fold. Bartholins duct = Large 1 to 2 duct branches join the submandibular duct. The nerves accompany the sublingual glands are derived from the lingual and chorda tympani nerves and from the sympathetic nerves. The parasympathetic secretomotor fibres are from the submandibular ganglion. Blood supply from lingual artery Lymphatic drainage to submandibular gland
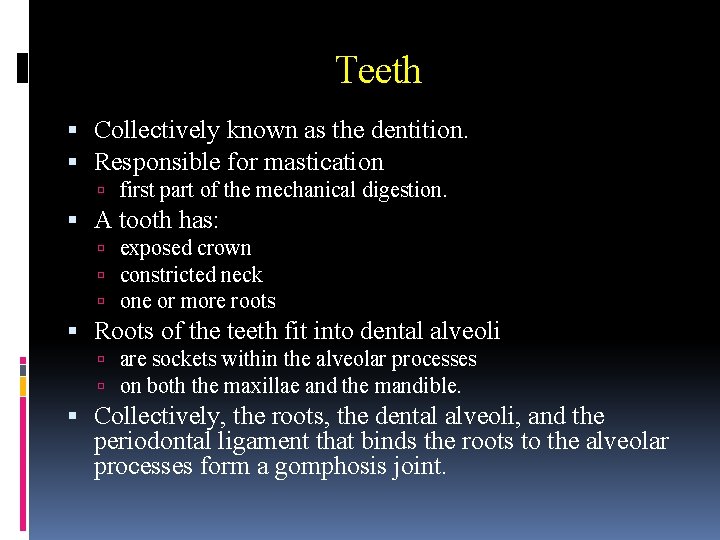
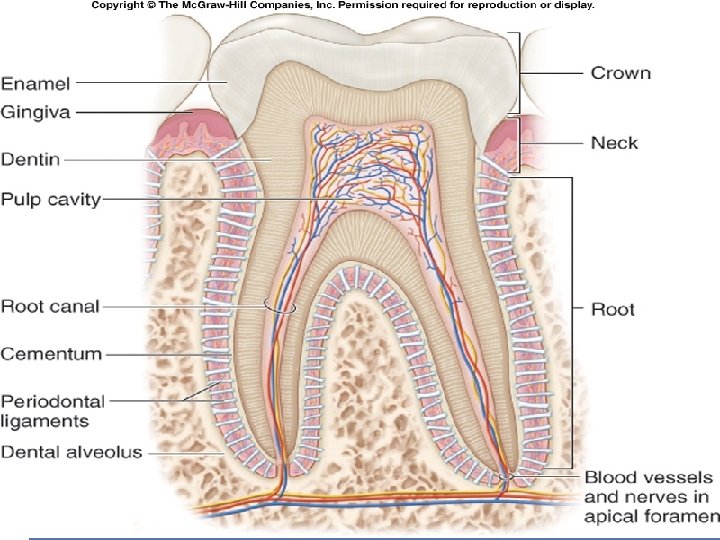
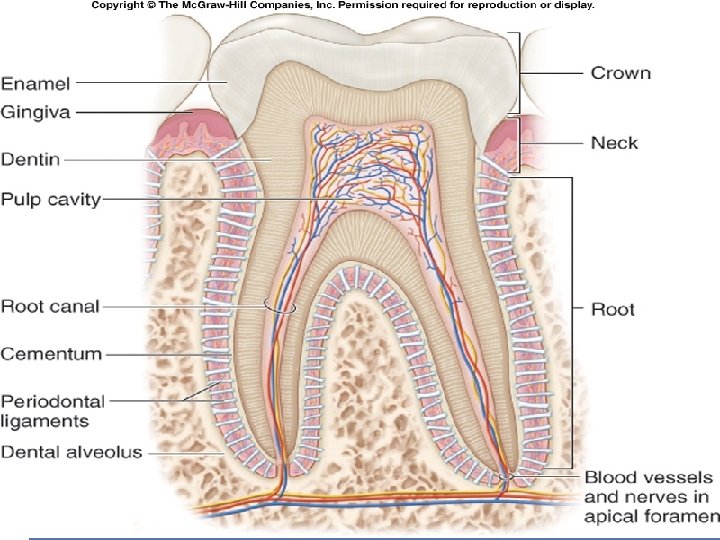
Teeth Collectively known as the dentition. Responsible for mastication first part of the mechanical digestion. A tooth has: exposed crown constricted neck one or more roots Roots of the teeth fit into dental alveoli are sockets within the alveolar processes on both the maxillae and the mandible. Collectively, the roots, the dental alveoli, and the periodontal ligament that binds the roots to the alveolar processes form a gomphosis joint.
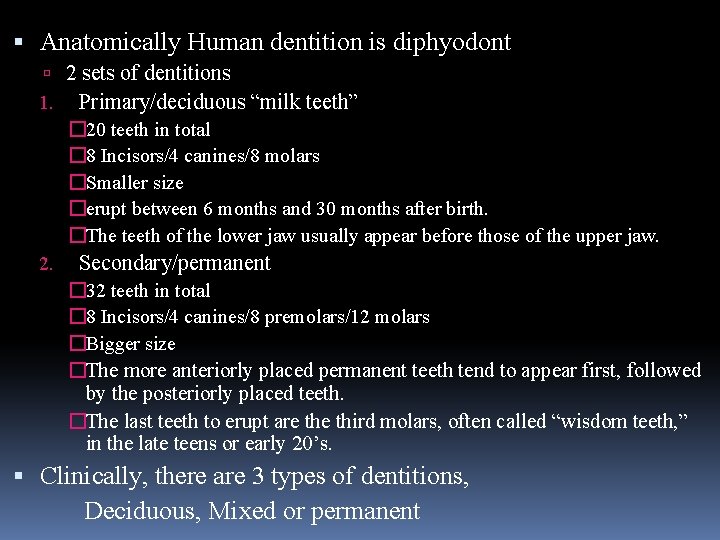
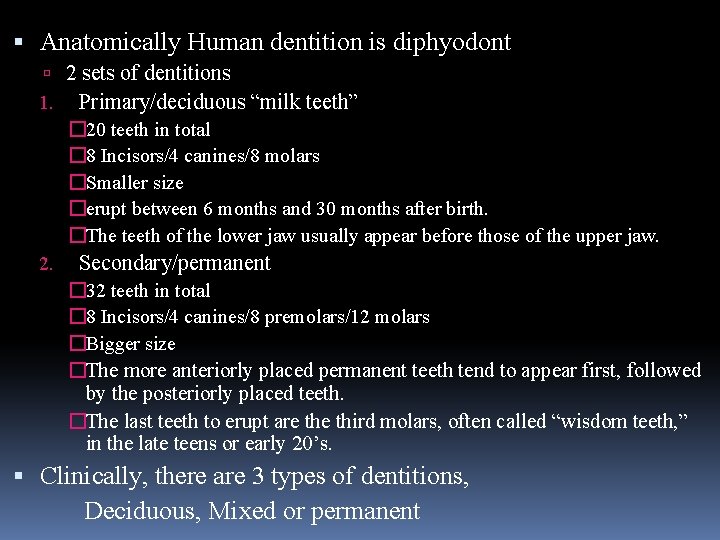
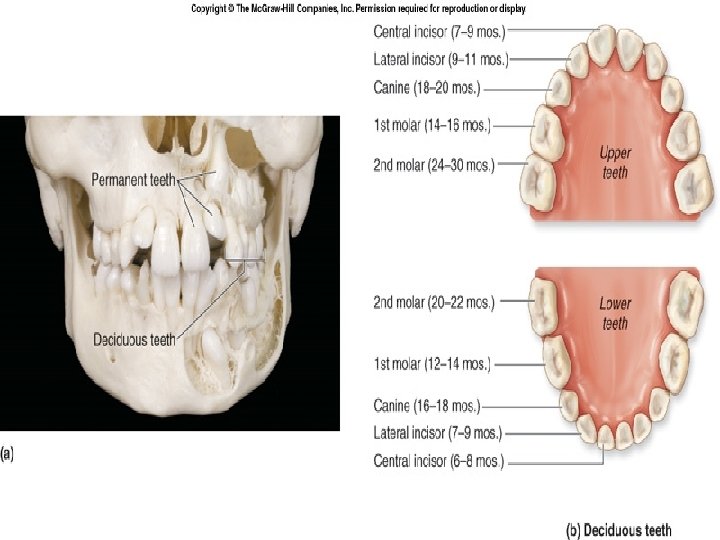
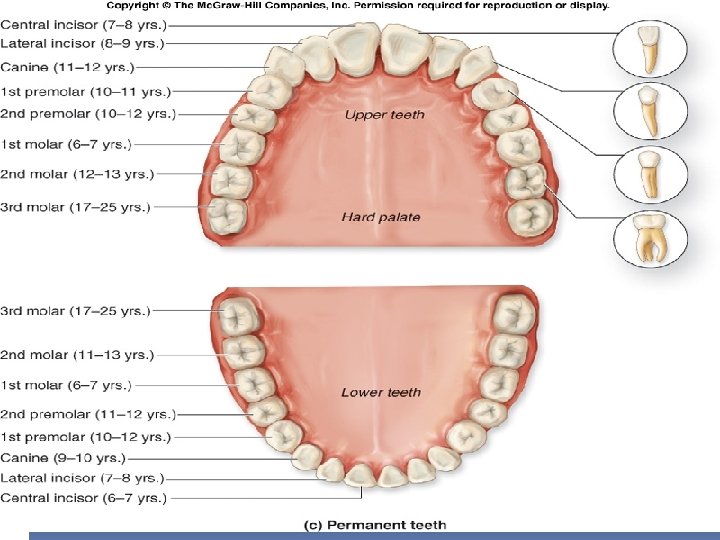
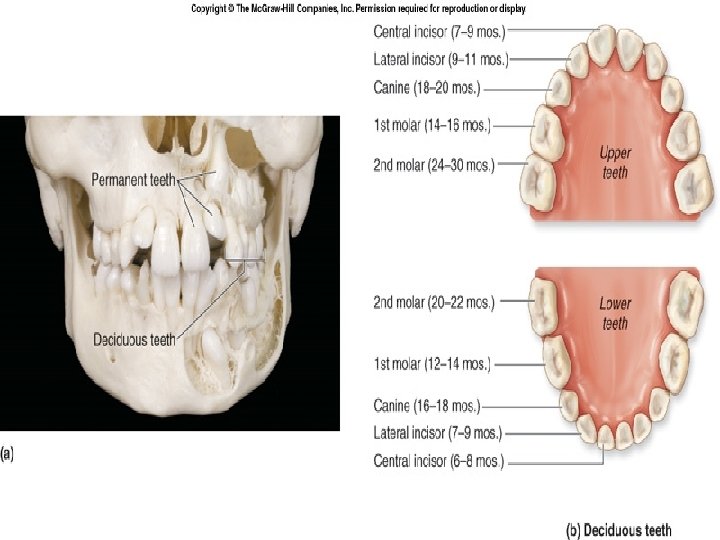
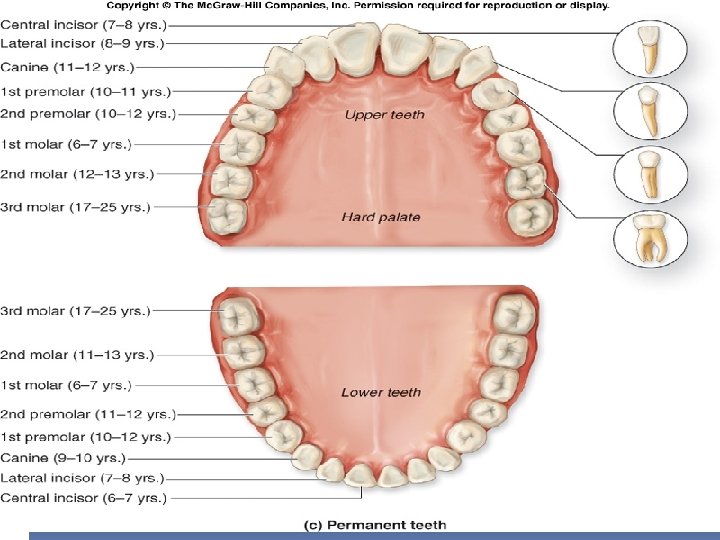
Anatomically Human dentition is diphyodont 2 sets of dentitions 1. Primary/deciduous “milk teeth” � 20 teeth in total � 8 Incisors/4 canines/8 molars �Smaller size �erupt between 6 months and 30 months after birth. �The teeth of the lower jaw usually appear before those of the upper jaw. 2. Secondary/permanent � 32 teeth in total � 8 Incisors/4 canines/8 premolars/12 molars �Bigger size �The more anteriorly placed permanent teeth tend to appear first, followed by the posteriorly placed teeth. �The last teeth to erupt are third molars, often called “wisdom teeth, ” in the late teens or early 20’s. Clinically, there are 3 types of dentitions, Deciduous, Mixed or permanent
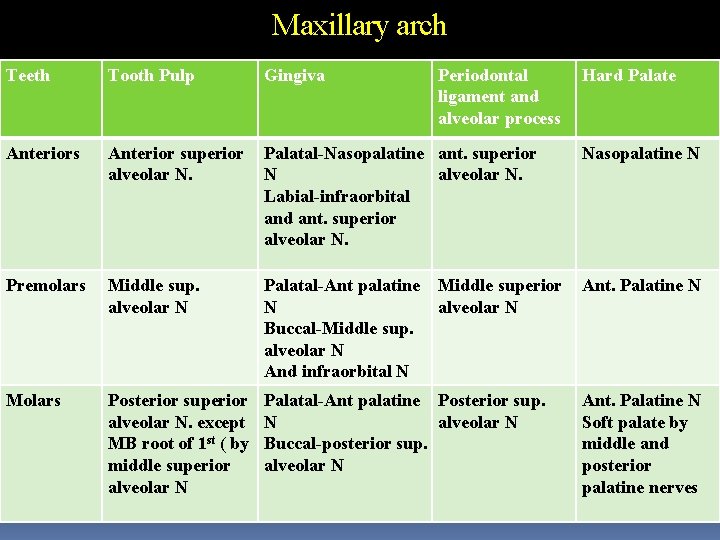
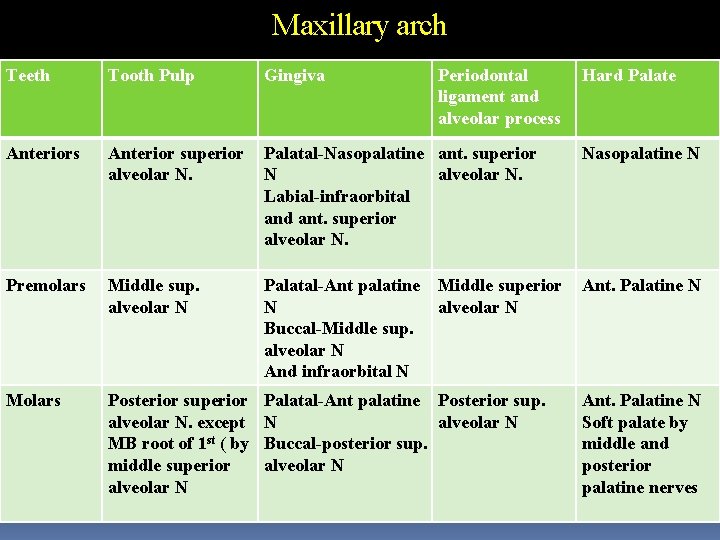
Maxillary arch Teeth Tooth Pulp Gingiva Periodontal ligament and alveolar process Anterior superior alveolar N. Palatal-Nasopalatine ant. superior N alveolar N. Labial-infraorbital and ant. superior alveolar N. Nasopalatine N Premolars Middle sup. alveolar N Palatal-Ant palatine N Buccal-Middle sup. alveolar N And infraorbital N Ant. Palatine N Molars Posterior superior alveolar N. except MB root of 1 st ( by middle superior alveolar N Palatal-Ant palatine Posterior sup. N alveolar N Buccal-posterior sup. alveolar N Middle superior alveolar N Hard Palate Ant. Palatine N Soft palate by middle and posterior palatine nerves
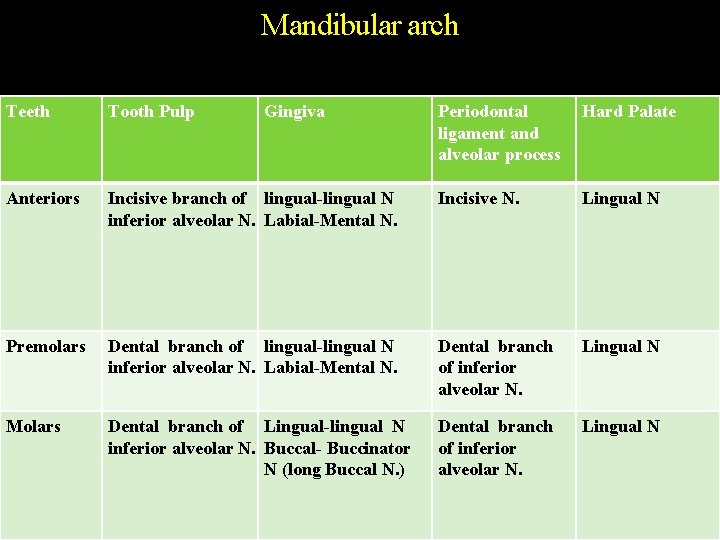
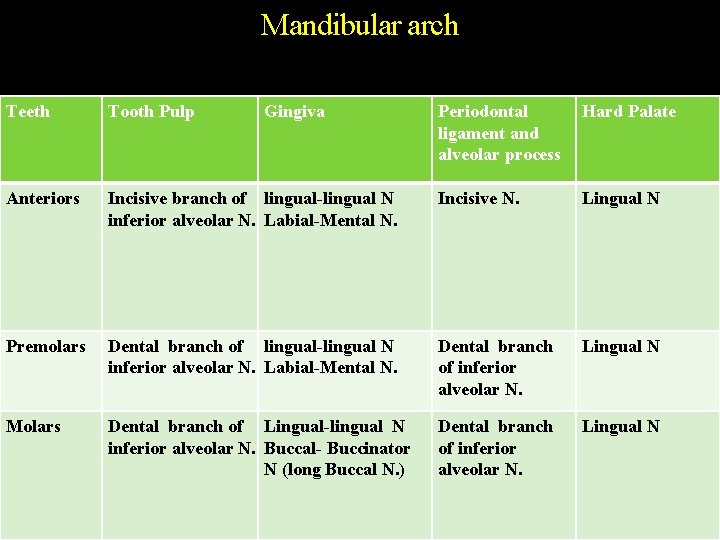
Mandibular arch Teeth Tooth Pulp Anteriors Gingiva Periodontal ligament and alveolar process Hard Palate Incisive branch of lingual-lingual N inferior alveolar N. Labial-Mental N. Incisive N. Lingual N Premolars Dental branch of lingual-lingual N inferior alveolar N. Labial-Mental N. Dental branch of inferior alveolar N. Lingual N Molars Dental branch of Lingual-lingual N inferior alveolar N. Buccal- Buccinator N (long Buccal N. ) Dental branch of inferior alveolar N. Lingual N
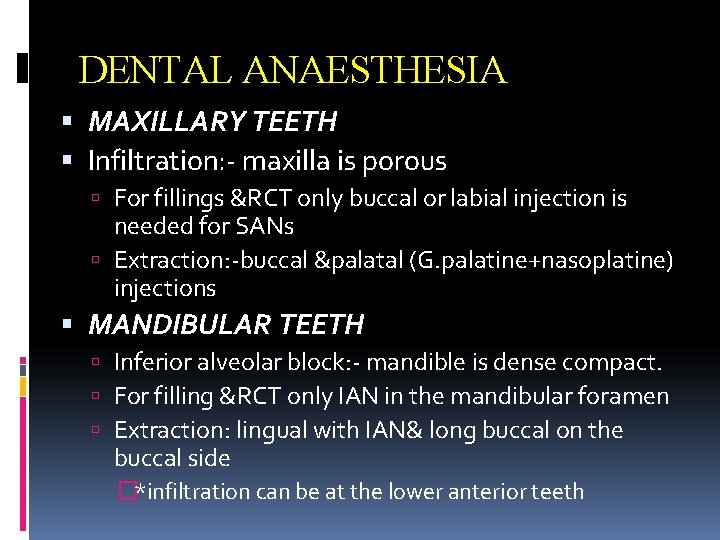
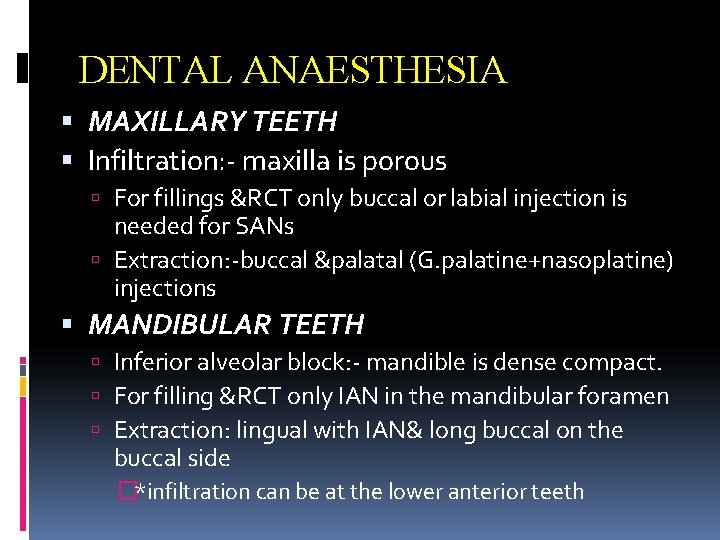
DENTAL ANAESTHESIA MAXILLARY TEETH Infiltration: - maxilla is porous For fillings &RCT only buccal or labial injection is needed for SANs Extraction: -buccal &palatal (G. palatine+nasoplatine) injections MANDIBULAR TEETH Inferior alveolar block: - mandible is dense compact. For filling &RCT only IAN in the mandibular foramen Extraction: lingual with IAN& long buccal on the buccal side �*infiltration can be at the lower anterior teeth
