Nursing Care of the Child With a Hematologic

- Slides: 163
Nursing Care of the Child With a Hematologic, Neoplastic, and Immunologic Disorder
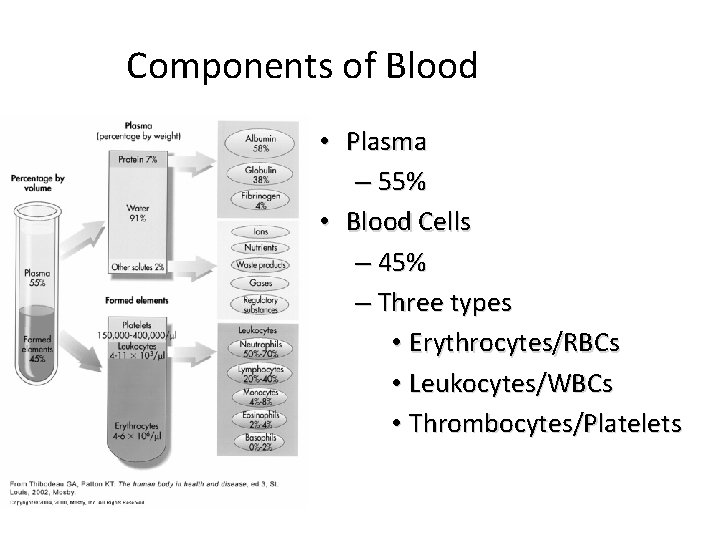
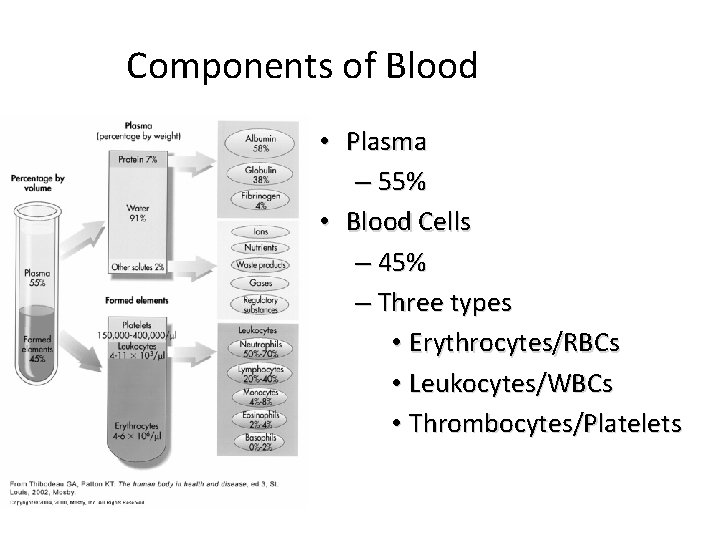
Components of Blood • Plasma – 55% • Blood Cells – 45% – Three types • Erythrocytes/RBCs • Leukocytes/WBCs • Thrombocytes/Platelets
Erythrocytes/Red Blood Cells • Composed of hemoglobin • Erythropoiesis – = RBC production • Stimulated by hypoxia • Controlled by erythropoietin – Hormone synthesized in kidney • Hemolysis – = destruction of RBCs – Releases bilirubin into blood stream – Normal lifespan of RBC = 120 days
Functions of the Hematologic System • Erythrocytes or red blood cells (RBCs) – Responsible for transporting nutrients and oxygen to the body tissues and waste products from the tissues • Thrombocytes or platelets – Responsible for clotting • Leukocytes or white blood cells (WBCs) – Responsible for fighting infection – Granulocytes (neutrophils, eosinophils, and basophils) and agranulocytes (lymphocytes and monocytes)
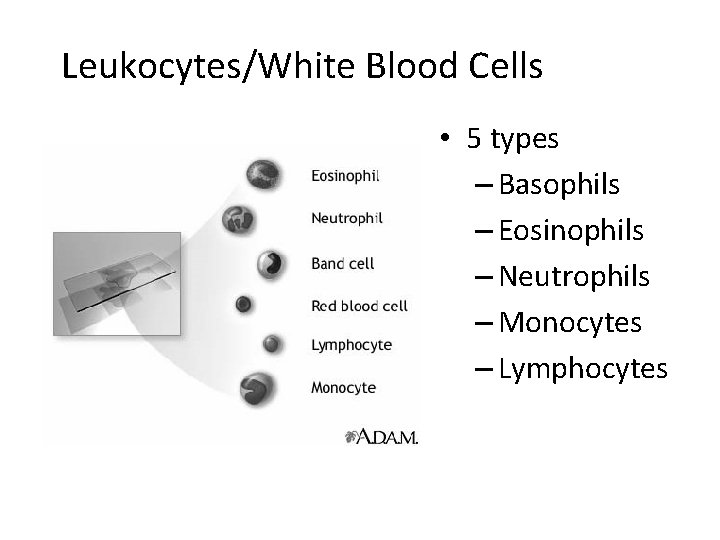
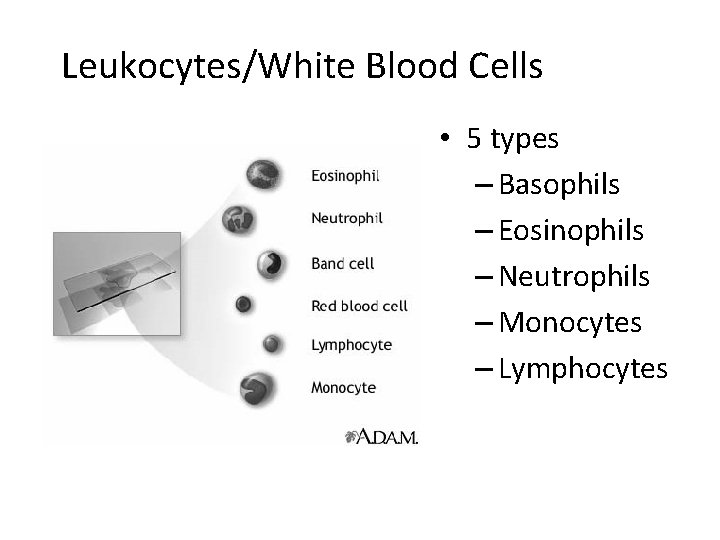
Leukocytes/White Blood Cells • 5 types – Basophils – Eosinophils – Neutrophils – Monocytes – Lymphocytes
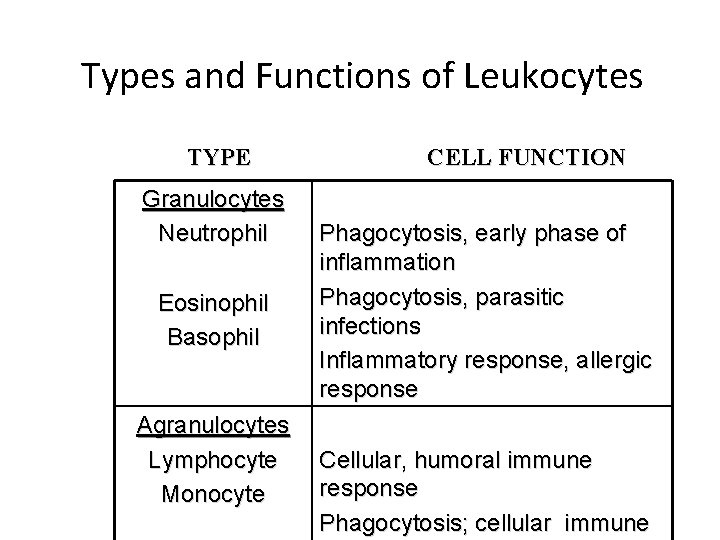
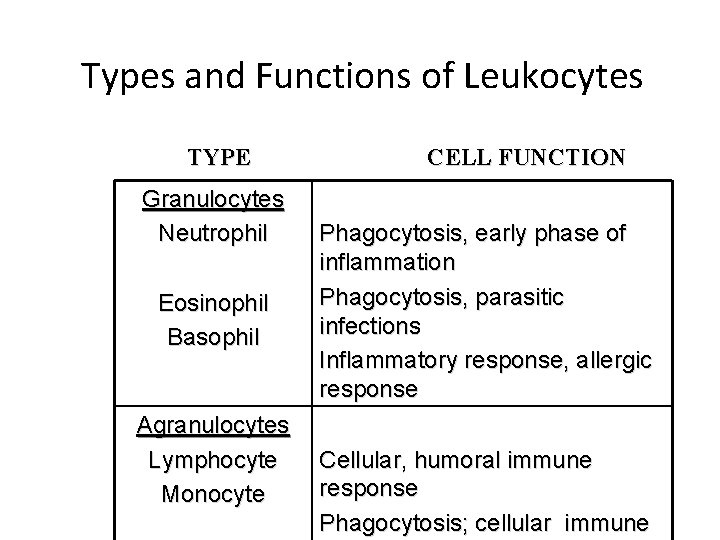
Types and Functions of Leukocytes TYPE Granulocytes Neutrophil Eosinophil Basophil Agranulocytes Lymphocyte Monocyte CELL FUNCTION Phagocytosis, early phase of inflammation Phagocytosis, parasitic infections Inflammatory response, allergic response Cellular, humoral immune response Phagocytosis; cellular immune
Anatomical and Physiological Differences in the Infant and Child Ø Early production of blood cells in the fetus occurs in the liver and spleen Ø After birth, the liver is the primary site for production of most of the blood clotting factors and prothrombin Ø In infants and young children, hematopoiesis occurs in almost every bone until age five (5) because all of the bone contains red marrow. Slide 7
Anatomical and Physiological Differences in the Infant and Child Ø After the age of five, hematopoiesis in the shafts of the long bones is reduced Ø As bone growth ceases near the end of adolescence (between 18 -20), only the marrow of the ribs, sternum, vertebrae, skull, clavicles, scapulas and pelvis continue to produce blood cells Slide 8
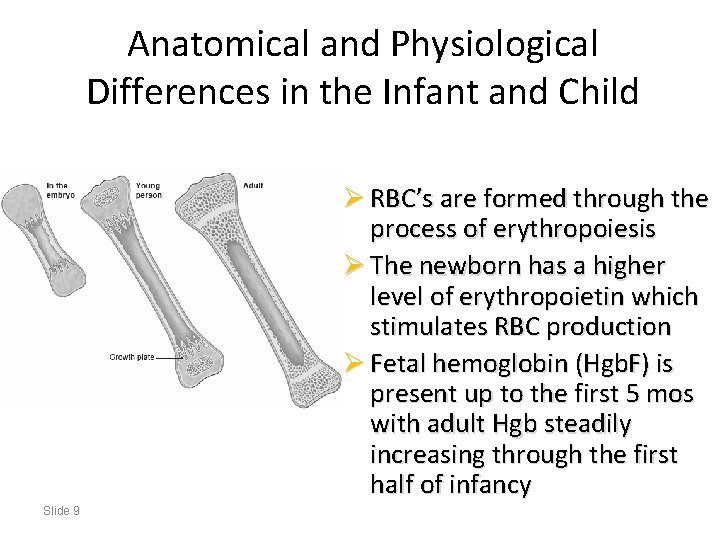
Anatomical and Physiological Differences in the Infant and Child Ø RBC’s are formed through the process of erythropoiesis Ø The newborn has a higher level of erythropoietin which stimulates RBC production Ø Fetal hemoglobin (Hgb. F) is present up to the first 5 mos with adult Hgb steadily increasing through the first half of infancy Slide 9
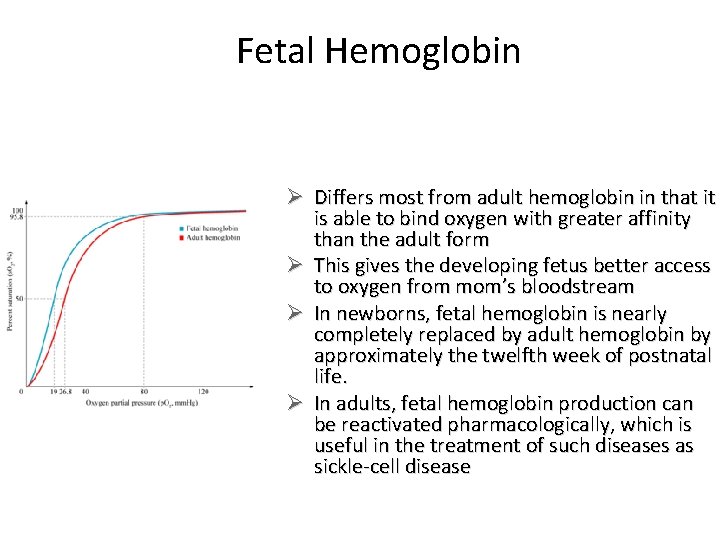
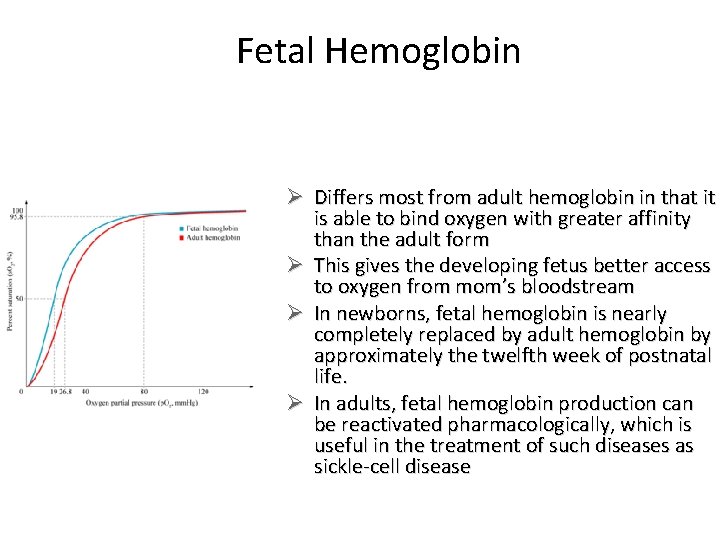
Fetal Hemoglobin Ø Differs most from adult hemoglobin in that it is able to bind oxygen with greater affinity than the adult form Ø This gives the developing fetus better access to oxygen from mom’s bloodstream Ø In newborns, fetal hemoglobin is nearly completely replaced by adult hemoglobin by approximately the twelfth week of postnatal life. Ø In adults, fetal hemoglobin production can be reactivated pharmacologically, which is useful in the treatment of such diseases as sickle-cell disease
Anatomical and Physiological Differences in the Infant and Child Ø The RBC count, Hgb and Hct levels are high in infants, but will stabilize in childhood Ø Platelet levels in newborns are lower than in older children and adults Slide 11
Assessment of Hematologic Function Ø Complete blood count (CBC) Ø History and assessment findings ØInspection ØPalpation ØAuscultation Ø Child’s energy and activity level Ø Growth patterns
Common Diagnostic Studies Ø CBC with differential Ø Direct and indirect Coombs’ test Ø Prothrombin time (PT) and Partial thromboplastin time Ø Bleeding time Ø Platelet agglutination/aggregation to evaluate platelet clumping ability Slide 13
Common Diagnostic Studies ØHemoglobin electrophoresis ØSerum Bone Marrow aspiration and biopsy ØBlood type and cross-match ØIron and lead levels ØReticulocyte count ØSerum Ferritin Slide 14
Health History Related to Hematologic Functioning • Birth and maternal history – Low birthweight, gestational diabetes, if vitamin K given after birth • Recent illnesses related to blood cell distribution • Sleep/wake patterns • Bowel elimination patterns • Family history for inherited disorders • Typical diet for nutritional deficits • Risk for lead exposure
History Ø Frequent or easy bruising? Ø Frequent or heavy nose bleeds? Ø Recurrent or chronic infections? Ø Medications (prescription or OTC) that might impair hematologic function Ø Past medical hx r/t hematologic dysfunction: illnesses, surgeries or injuries Ø Excessively heavy menstrual Flow? Slide 16
Nursing Care of the Child with a Hematologic Disorder • Based on the Disorder • RBC’s – Oxygenation – Circulation – Fluid – Nutrition – Pain Management
Nursing Care of a Child with a Hematologic Disorder • Based on the Disorder • WBC’s – Infection – Oxygenation – Nutrition • Platelets and bleeding disorders – Bleeding – Oxygenation – Circulation – Injury Prevention
Common Laboratory and Diagnostic Tests for Hematologic Disorder • • Blood type and cross-match Clotting studies Coagulating factor concentration Complete blood count with differential Hemoglobin electrophoresis Iron and lead levels Reticulocyte count Serum ferritin
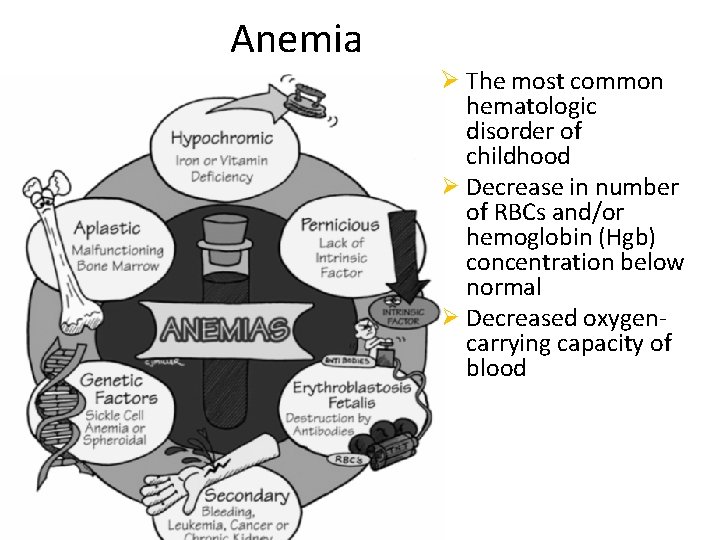
Anemia Ø The most common hematologic disorder of childhood Ø Decrease in number of RBCs and/or hemoglobin (Hgb) concentration below normal Ø Decreased oxygencarrying capacity of blood
Types of Anemia • Nutritional deficiency • Iron deficiency, folic acid deficiency, pernicious anemia • Toxin exposure – Lead poisoning • Aplastic anemia – Adverse reaction to medication • Hemolytic anemia – Sickle cell anemia, Thalassemia
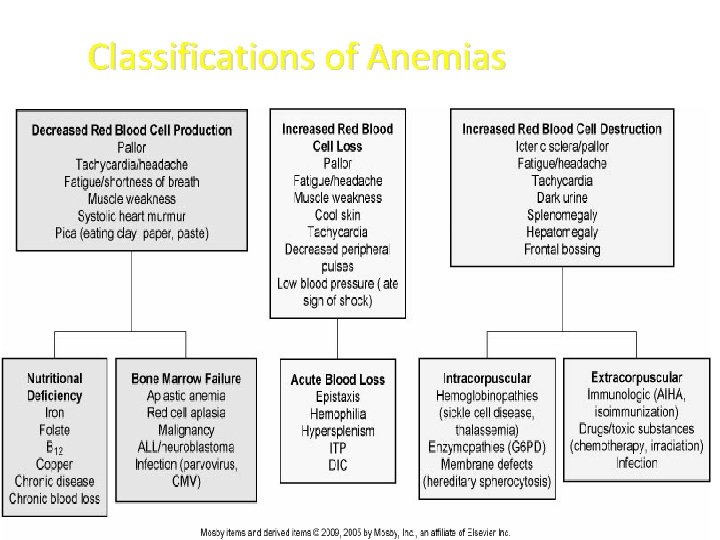
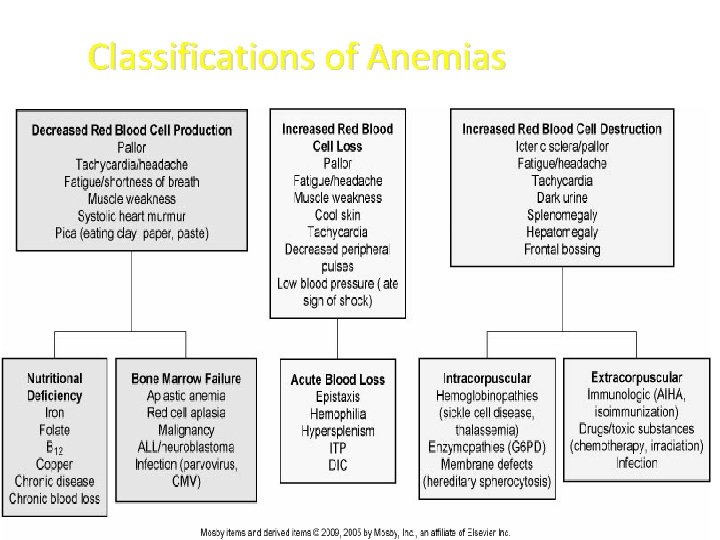
Classifications of Anemias
Classification of Anemias Ø Etiology and physiology: ØRBC and/or Hgb depletion Ø Morphology: ØCharacteristic changes in RBC size, shape, and/or color
Consequences of Anemia Ø Decrease in oxygen-carrying capacity of blood and decreased amount of oxygen available to tissues Ø When anemia develops slowly, child adapts
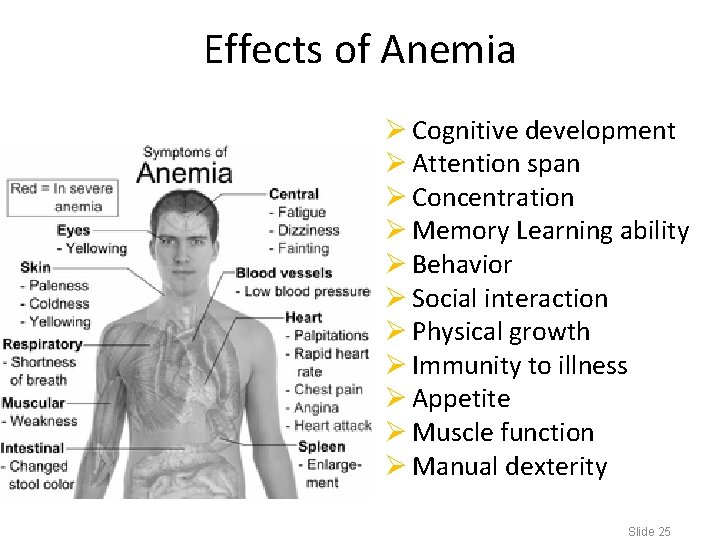
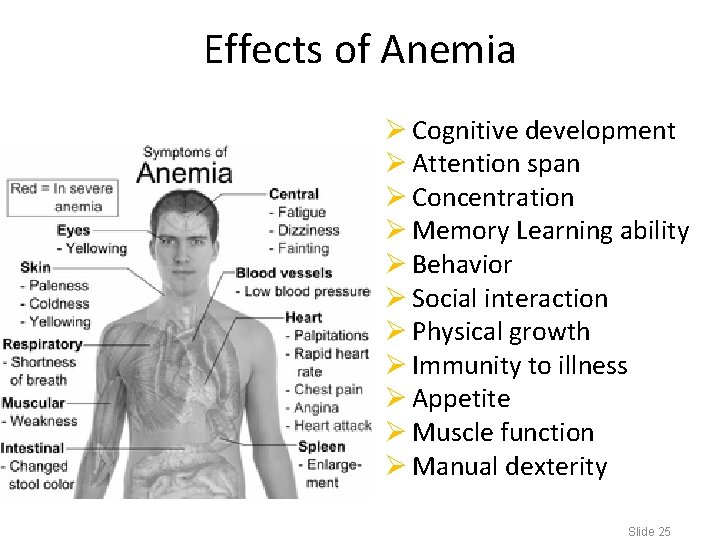
Effects of Anemia Ø Cognitive development Ø Attention span Ø Concentration Ø Memory Learning ability Ø Behavior Ø Social interaction Ø Physical growth Ø Immunity to illness Ø Appetite Ø Muscle function Ø Manual dexterity Slide 25
Effects of Anemia on Circulatory System Ø Hemodilution Ø Decreased peripheral resistance Ø Increased cardiac circulation and turbulence: ØMay have murmur ØMay lead to cardiac failure Ø Cyanosis Ø Growth retardation
Diagnostic Evaluation of Anemia Ø CBC: ØDecreased RBCs ØDecreased Hbg and hematocrit (Hct) Ø Other tests for particular type of anemia
Therapeutic Management of Anemia Ø Treat underlying cause: ØTransfusion after hemorrhage if needed ØNutritional intervention for deficiency anemias Ø Supportive care: ØIV fluids to replace intravascular volume ØOxygen ØBed rest
Nursing Considerations for Anemia ü Prepare child and family for laboratory tests ü Decrease oxygen demands ü Prevent complications ü Support family
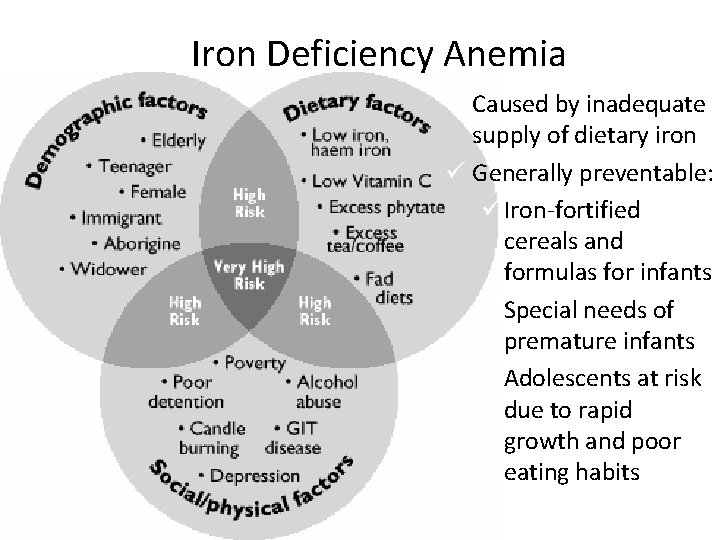
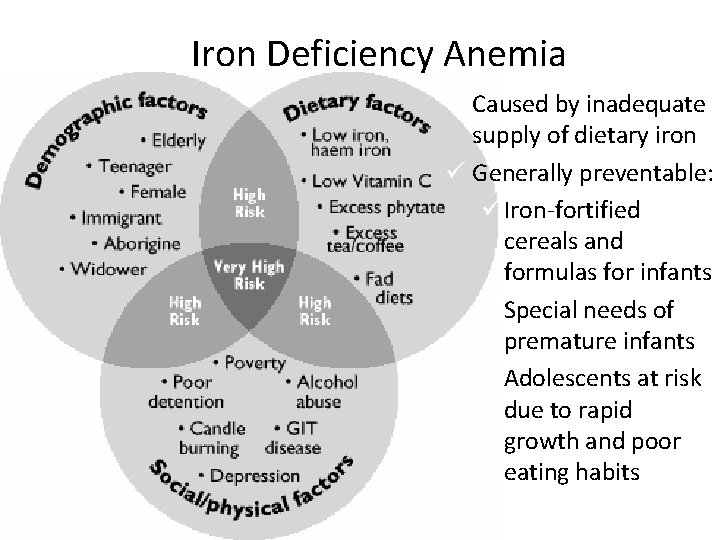
Iron Deficiency Anemia ü Caused by inadequate supply of dietary iron ü Generally preventable: ü Iron-fortified cereals and formulas for infants ü Special needs of premature infants ü Adolescents at risk due to rapid growth and poor eating habits
Iron Deficiency Anemia o o o o Occurs as a result of Blood loss Poor nutritional intake Rapid growth w/increased internal demands for blood production Chronic blood loss Chronic diarrhea Parasitic GI problems Females who have heavy menstrual periods Slide 31
Iron Deficiency Anemia ü Initial Clinical Manifestations ü Pallor ü Irritability ü Fatigue ü Clinical Manifestations seen in prolonged anemia ü Nail bed deformities ü Tachycardia ü Growth Retardation ü Systolic heat murmur ü Developmental delay Slide 32
Iron Deficiency Anemia ü Diagnostic Evaluation includes: ü CBC ü Reticulocyte Count ü Serum Ferritin level; serum Iron ü Therapeutic Management ü Oral Fe supplements may be ordered: ferrous sulfate is the form preferred as it is absorbed best Slide 33
Recommended Dosages of Elemental Iron for Iron-Deficiency Anemia • For prophylaxis: 1 to 2 mg/kg/day, up to a maximum of 15 mg elemental iron per day • Mild to moderate iron deficiency: 3 mg/kg/day of elemental iron in one or two divided doses • Severe iron-deficiency anemia: 4 to 6 mg/kg/day of elemental iron in three divided doses • Make stools GREEN
Foods Rich in Iron • • Red meats (easiest for the body to absorb) Tuna and salmon Eggs Tofu Enriched grains Dried beans, peas, and fruits Leafy green vegetables Iron-fortified breakfast cereals
Iron Deficiency Anemia Nursing Considerations: v. Correct bleeding if it is the cause of anemia v. Implement dietary modifications to provide a high Fe diet v. Promote rest, protect from infection; monitor cardiac functioning v. Transfusion if ordered Slide 36
Iron Deficiency Anemia Nursing Considerations: v. Protein and Vitamin C in order to produce new cells; folic acid to help convert the Fe from ferritin to hemoglobin v. If Fe deficiency due to ingestion of large quantities of milk at the expense of solid food intake, limit to 1 qt of milk/day Slide 37
Aplastic Anemia Ø All formed elements of the blood are simultaneously depressed: pancytopenia Ø Hypoplastic anemia: profound depression of RBCs but normal WBCs and platelets
Aplastic Anemia • Is a deficiency of the blood cells that results from failure of the bone marrow to produce adequate numbers of circulating blood cells • Can be congenital or acquired Clinical Manifestations: Ø Ø Slide 39 Ø Petechiae Ecchymosis Bleeding Pallor Epistaxis Ø Weakness Ø Tachycardia Ø Fatigue Ø Anorexia
Acquired Aplastic Anemia v. Intake of certain medications v. Infected by hepatitis, Epstein-Barr, and even HIV in the past v. Exposed to high-dose radiation v. Aflicted by autoimmune disorders v. Exposure to harmful chemicals
Aplastic Anemia Diagnostic Evaluation: • Hx of bruising immediately after an event that would not normally cause a bruise • CBC • Bone Marrow aspiration and biopsy confirms the diagnosis Slide 41
Nursing Assessment for Aplastic Anemia • Determine history of exposure to myelosuppressive medications or radiation therapy. • Obtain a detailed family, environmental, and infectious disease history. • Note history of epistaxis, gingival oozing, or increased bleeding with menstruation. • Anemia may lead to headache and fatigue. • On physical examination, note ecchymoses, petechiae or purpura, oral ulcerations, tachycardia, or tachypnea.
Aplastic Anemia Nursing Considerations: • Bleeding prevention • Administration and monitoring of blood transfusions as ordered • Infection prevention • Encouraging mobility as tolerated Slide 43
Sources of Lead • Paint in homes built before 1978 and dust from windowsills, walls, and plaster in older homes • Soil where cars that used leaded gas have been in the past • Glazed pottery and stained glass products • Lead pipes supplying water to the home • On the clothing of parents who work in certain manufacturing jobs • Certain folk remedies, such as greta or arzacon • Old painted toys or furniture
Complications of Lead Poisoning • Lower levels – Behavioral problems – Learning difficulties • Higher levels – Encephalopathy – Seizures – Brain damage
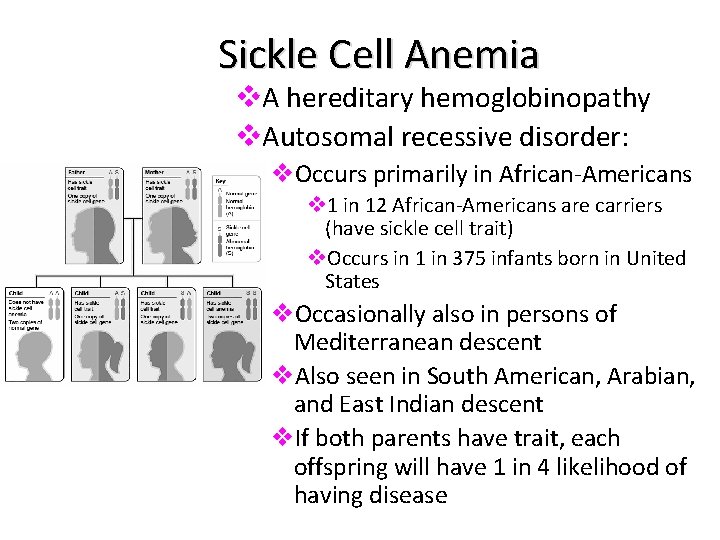
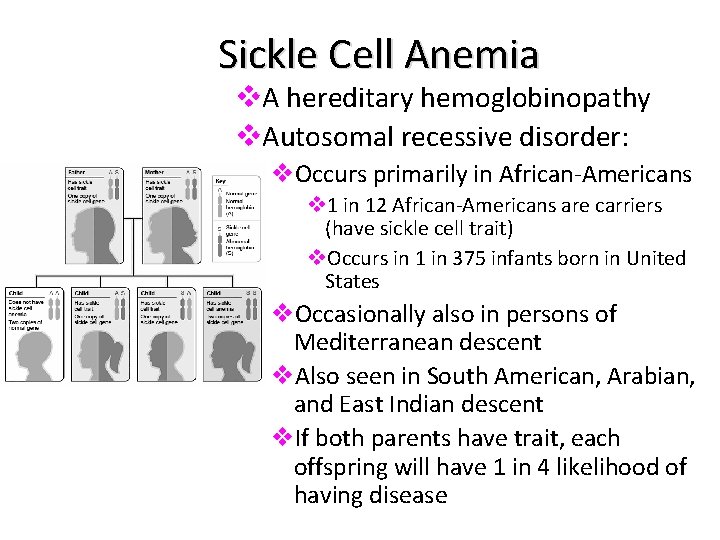
Sickle Cell Anemia v. A hereditary hemoglobinopathy v. Autosomal recessive disorder: v. Occurs primarily in African-Americans v 1 in 12 African-Americans are carriers (have sickle cell trait) v. Occurs in 1 in 375 infants born in United States v. Occasionally also in persons of Mediterranean descent v. Also seen in South American, Arabian, and East Indian descent v. If both parents have trait, each offspring will have 1 in 4 likelihood of having disease
Sickle Cell Anemia • Normal hemoglobin partially or completely replaced by the sickle shaped, hemoglobin S (Hgb S) • Symptoms do not manifest until 4 -6 months of age • Many children must undergo a splenectomy in early childhood, leading to severely compromised immunity Slide 47
Pathophysiology of Sickle Cell Anemia • Partial or complete replacement of normal Hgb with abnormal hemoglobin S (Hgb S) • Hemoglobin in the RBCs takes on an elongated “sickle” shape • Sickled cells are rigid and obstruct capillary blood flow • Microscopic obstructions lead to engorgement and tissue ischemia • Hypoxia occurs and causes sickling
Vaso-occlusive Crisis “Pain Crisis” ü Aka thrombotic crisis ü Most common type of crisis ü Precipitated by dehydration, exposure to cold, acidosis or localized hypoxemia ü Extremely painful ü Caused by stasis of blood w/ clumping of cells in the microciruclation, ischemia and infarction ü Thrombosis and infarction of tissue may occur if crisis not reversed ü Clinical manifestations include fever, pain, tissue engorgement, swelling of joints, hands and feet, priapism and severe abdominal pain
Pathophysiology of Sickle Cell Anemia (cont) Ø Large tissue infarctions occur Ø Damaged tissues in organs; impaired function: ØSplenic sequestration ØMay require splenectomy at early age ØResults in immunity
Sickle Cell Crisis Precipitating factors: Ø Anything that increases body’s need for oxygen or alters transport of oxygen Ø Trauma Ø Infection, fever Ø Physical and emotional stress Ø Increased blood viscosity due to dehydration Ø Hypoxia: ØFrom high altitude, poorly pressurized airplanes, hypoventilation, vasoconstriction due to hypothermia
Sickle Cell Anemia Ø Precipitating factors for sickle cell crisis include: Ø Increased Blood viscosity Ø Hypoxia Ø High altitudes Ø Hypoventilation Ø Vasoconstriction (when cold) Ø Emotional stress Slide 52

Sickle Cell Anemia Ø Vaso-occlusive crisis Ø Painful Episode Ø Acute Chest syndrome Ø Dactylitis Ø Priapism Ø CVA Ø Acute Sequestration crisis (Splenic Sequestration) Ø Aplastic Anemia Slide 54
Sickle Cell Anemia Therapeutic Management: v Opioids (Morphine; No Demerol) v NSAIDs v IV hydration v Oxygen (if patient is hypoxic) v Exchange Transfusions (erythrocytapheresis) v Hydroxyuria v Chelation therapy (for long term RBC transfusion therapy) Slide 55
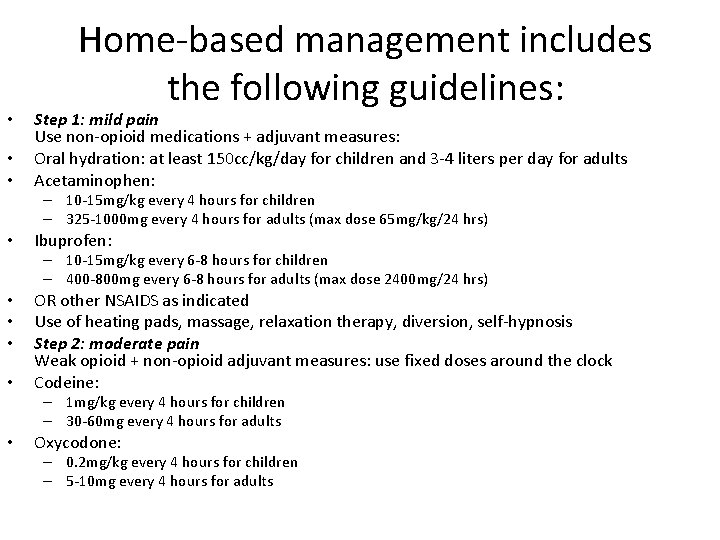
• • • Home-based management includes the following guidelines: Step 1: mild pain Use non-opioid medications + adjuvant measures: Oral hydration: at least 150 cc/kg/day for children and 3 -4 liters per day for adults Acetaminophen: – 10 -15 mg/kg every 4 hours for children – 325 -1000 mg every 4 hours for adults (max dose 65 mg/kg/24 hrs) • Ibuprofen: – 10 -15 mg/kg every 6 -8 hours for children – 400 -800 mg every 6 -8 hours for adults (max dose 2400 mg/24 hrs) • • OR other NSAIDS as indicated Use of heating pads, massage, relaxation therapy, diversion, self-hypnosis Step 2: moderate pain Weak opioid + non-opioid adjuvant measures: use fixed doses around the clock Codeine: – 1 mg/kg every 4 hours for children – 30 -60 mg every 4 hours for adults • Oxycodone: – 0. 2 mg/kg every 4 hours for children – 5 -10 mg every 4 hours for adults
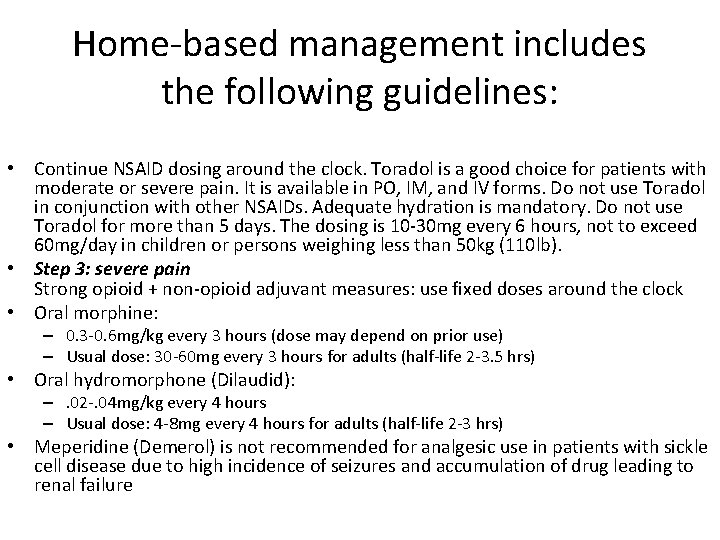
Home-based management includes the following guidelines: • Continue NSAID dosing around the clock. Toradol is a good choice for patients with moderate or severe pain. It is available in PO, IM, and IV forms. Do not use Toradol in conjunction with other NSAIDs. Adequate hydration is mandatory. Do not use Toradol for more than 5 days. The dosing is 10 -30 mg every 6 hours, not to exceed 60 mg/day in children or persons weighing less than 50 kg (110 lb). • Step 3: severe pain Strong opioid + non-opioid adjuvant measures: use fixed doses around the clock • Oral morphine: – 0. 3 -0. 6 mg/kg every 3 hours (dose may depend on prior use) – Usual dose: 30 -60 mg every 3 hours for adults (half-life 2 -3. 5 hrs) • Oral hydromorphone (Dilaudid): –. 02 -. 04 mg/kg every 4 hours – Usual dose: 4 -8 mg every 4 hours for adults (half-life 2 -3 hrs) • Meperidine (Demerol) is not recommended for analgesic use in patients with sickle cell disease due to high incidence of seizures and accumulation of drug leading to renal failure
Prognosis for Sickle Cell Anemia Ø No cure (except possibly bone marrow transplants) Ø Supportive care, prevent sickling episodes Ø Frequent bacterial infections may occur due to immunocompromise Ø Bacterial infection is leading cause of death in young children with sickle cell disease Ø Strokes in 5%-10% of children with disease ØResult in neurodevelopmental delay, mental retardation
Sickle Cell Crisis (cont’d) ü Acute exacerbations that vary in severity and frequency ü Types: üVaso-occlusive (VOC) thrombotic: üMost common type of crisis—very painful üStasis of blood with clumping of cells in microcirculation→ischemia→infarction üSigns: fever, pain, tissue engorgement
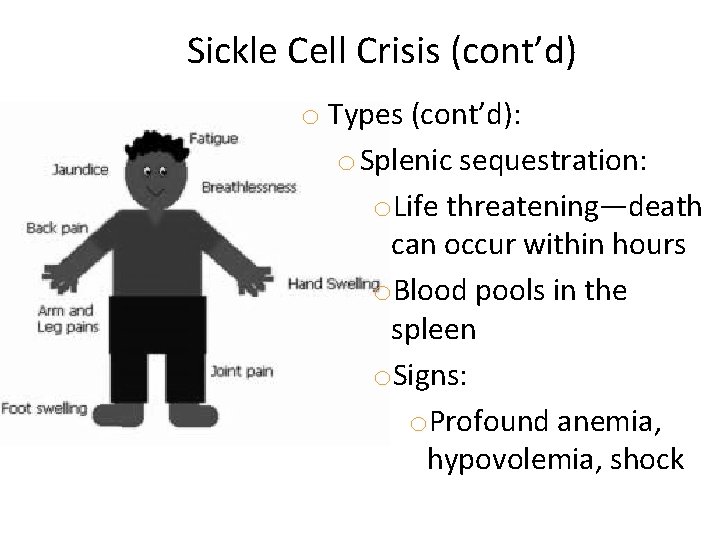
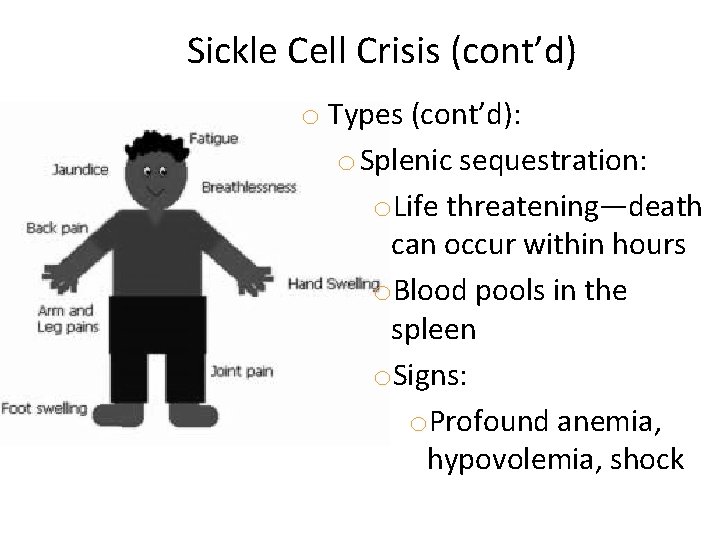
Sickle Cell Crisis (cont’d) o Types (cont’d): o Splenic sequestration: o. Life threatening—death can occur within hours o. Blood pools in the spleen o. Signs: o. Profound anemia, hypovolemia, shock
Sickle Cell Crisis (cont’d) v. Types (cont’d): v. Aplastic crises: v. Diminished production and increased destruction of RBCs v. Triggered by viral infection or depletion of folic acid v. Signs include profound anemia, pallor
Diagnosis of Sickle Cell Anemia ü Cord blood in newborns ü Newborn screening done in 43 states ü Genetic testing to identify carriers and children who have disease ü Sickle-turbidity test: üQuick screening purposes in children >6 months of age
Medical Management of Sickle Cell Anemia ü Aggressive treatment of infection ü Possible prophylactic antibiotics from 2 months to 5 years Ø Monitor reticulocyte count regularly to evaluate bone marrow function Ø Blood transfusion, if given early in crisis, may reduce ischemia ü Frequent transfusion decreases hemosiderosis (iron in tissues) ü Treat with iron-chelation such as feroxamine + vitamin C to promote iron excretion ü Drugs: hydroxyurea (cytotoxic) decreases production of abnormal blood cells and decreases pain
Laboratory and Diagnostic Studies to Assess Sickle Cell Disease • Hemoglobin: baseline is usually 7 to 10 mg/d. L; will be significantly lower with splenic sequestration, acute chest syndrome, or aplastic crisis • Reticulocyte count: greatly elevated • Peripheral blood smear: presence of sickle-shaped cells and target cells • Platelet count: increased • Erythrocyte sedimentation rate: elevated • Abnormal liver function tests with elevated bilirubin
Sickle Cell Anemia Nursing Considerations: Ø Hydration through IVF’s as ordered Ø Hydration through oral intake Ø Administration of O 2 and blood products as ordered Ø Administer Antibiotics as ordered Ø Promote/Encourage rest Slide 65
Sickle Cell Anemia Nursing Considerations: Ø Assist child and family to avoid emotional stress as much as possible Ø Administer analgesics around the clock as ordered when child is in crisis; position for comfort and to decrease stress on painful joints (pain control) Ø Assess for signs and symptoms of worsening anemia, shock and altered neuro function Ø Provide emotional support during crisis
Nursing Management of Sickle Cell Anemia v. Monitor child’s growth—watch for failure to thrive v. Careful multisystem assessment v. Assess pain v. Observe for presence of inflammation or possible infection v. Carefully monitor for signs of shock
Treatment for Sickle Cell Anemia • Treatment consists of sx management • The primary focus being on prevention of sickle cell crisis – Education • Blood transfusions • Hydration: Drinking plenty of water daily – (8 to 10 glasses) or receiving fluid intravenously (to prevent and treat pain crises) • Pain Management
Nursing Dx: Pain r/t sickling of RBCs • Pain can occur in any organ or joint in the body • Pain can be reversed – Oxygenation – Hydration – Pain Management – Rest • Mild pain episodes can be treated w/ OTC pain meds (tylenol, ibuprofen) and heating pads • More severe episodes require hospitalization and IV pain meds • Hydroxyurea
Medications for SS anemia • Hydroxyurea 15 -20 mg/kg/day to start and increase until therapeutic response (not more than 35 mg/kg) – A chemotherapeutic drug used in CA tx – Shown to decrease the number and severity of crises – Increases production of Hemoglobin F – Side effects include bone marrow supression, HA’s dizziness, N/V
Psychosocial Needs ü Coping mechanisms ü Support with genetic counseling ü Financial needs ü Caregiver role strain ü Living with chronic illness in the family
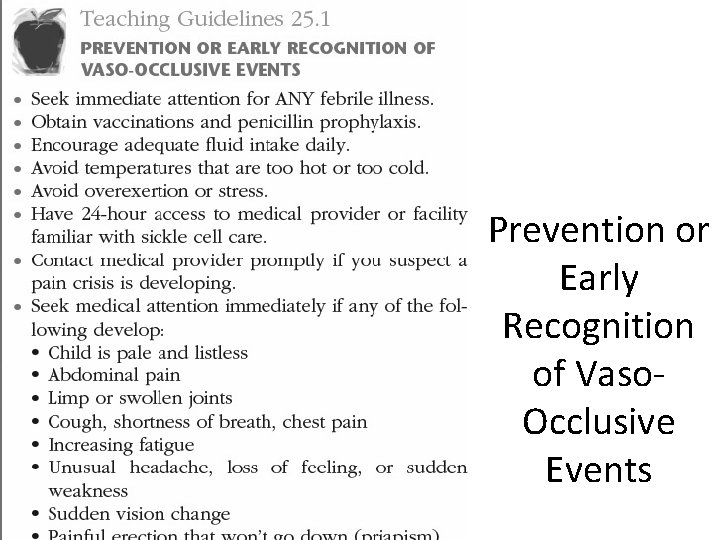
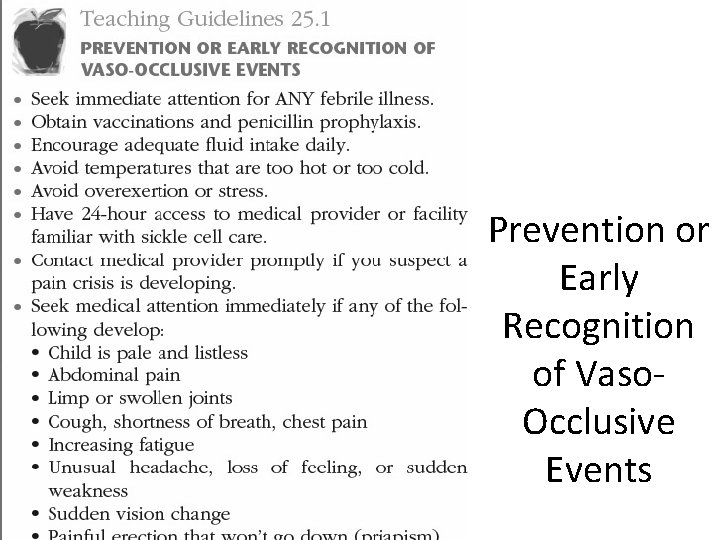
Prevention or Early Recognition of Vaso. Occlusive Events
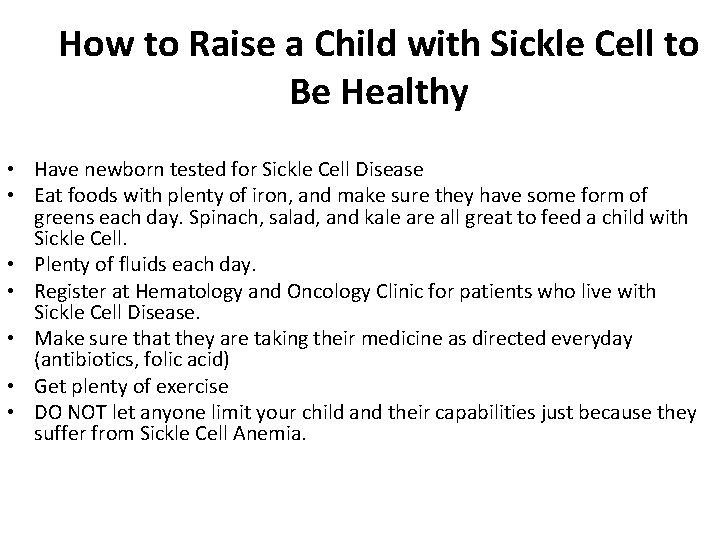
How to Raise a Child with Sickle Cell to Be Healthy • Have newborn tested for Sickle Cell Disease • Eat foods with plenty of iron, and make sure they have some form of greens each day. Spinach, salad, and kale are all great to feed a child with Sickle Cell. • Plenty of fluids each day. • Register at Hematology and Oncology Clinic for patients who live with Sickle Cell Disease. • Make sure that they are taking their medicine as directed everyday (antibiotics, folic acid) • Get plenty of exercise • DO NOT let anyone limit your child and their capabilities just because they suffer from Sickle Cell Anemia.
Beta Thalassemia (Cooley Anemia) • Thalassemias are a group of hereditary blood disorders of hemoglobin synthesis characterized by mild to severe anemia • Autosomal recessive disorder • Causes the synthesis of defective hemoglobin; leads to anemia and hypoxia Slide 74
Thalassemia (cont’d) v -Thalassemia vα-Chains affected v. Occurs in Chinese, Thai, African, and Mediterranean people v -Thalassemia v. Occurs in Greeks, Italians, and Syrians v is most common and has four forms
Pathophysiology of Thalassemia • Anemia results from defective synthesis of Hgb, structurally impaired RBCs, and shortened life of RBCs • Chronic hypoxia: – Headache, irritability, precordial and bone pain, exercise intolerance, anorexia, epistaxis • Detected in infancy or toddlerhood: – Pallor, failure to thrive (FTT), hepatosplenomegaly, severe anemia (Hgb <6 g/dl)
-Thalassemia ü Four types: üThalassemia minor: asymptomatic silent carrier üThalassemia trait: mild microcytic anemia üThalassemia intermediate: moderate to severe anemia + splenomegaly üThalassemia major (Cooley anemia): severe anemia requiring transfusions to survive
Diagnosis of Thalassemia Ø By hemoglobin electrophoresis Ø RBC changes often seen by 6 weeks of age Ø Child seen with severe anemia, FTT Ø Clinical Manifestations: Ø Anemia Ø Frequent epistaxis Ø Skeletal Changes Ø Facial deformities Ø Heart: CHF, myocardial fibrosis, murmurs Ø Liver/Gallbladder: hepatomegaly, hepatic insufficiency
Beta Thalassemia (Cooley Anemia) Therapeutic Management: ØErythrocyte Transfusion ØChelation therapy ØA complication of the frequent blood transfusions in thalassemia is iron overload. Chelation therapy with deferoxamine (an iron-chelating agent) is given with oral supplements of vitamin C to increase iron excretion. ØSplenectomy
Beta Thalassemia (Cooley Anemia) Nursing Considerations: • Adm. Blood product as ordered, observing for complications of multiple transfusions • Assess for signs of Fe overload and hepatitis • Observe for signs of infection • Adm. folic acid as ordered • Fx prevention by encouraging physical activities that do not increase risk • Iron chelation therapy as ordered Slide 80
Medical Management of Thalassemia q. Blood transfusion to maintain normal Hgb levels q. Side effect—hemosiderosis q. Treat with iron-chelating drugs such as deferoxamine (Desferal) q. Binds excess iron for excretion by kidney • • Observe for complications of transfusion Emotional support to family Encourage genetic counseling Parent and patient teaching for self-care
Prognosis for Thalassemia • Retarded growth • Delayed or absent secondary sex characteristics • Expect to live well into adulthood with proper clinical management • Bone marrow transplant is potential cure
Hemophilia: TWO Types • A group of hereditary bleeding disorders that result from deficiencies of specific clotting factors • X linked recessive trait expressed almost exclusively as carrier females and affected males • Hemophilia A (classic hemophilia): – Most common type accounts for 80% of hemophilia cases – X-linked recessive trait – Males are affected (1 in 5000 males) – Females may be carriers – Deficiency of factor VIII – Degree of bleeding depends on amount of clotting factor and Slide 83 severity of a given injury
Hemophilia: TWO Types • Hemophilia B – AKA Christmas disease – Caused by deficiency of factor IX – Accounts for 15% of cases of hemophilia üClinical Manifestations: Range from mild to moderate or severe ü Hemarthrosis - one of the most commonly seen symptoms ü Significant deep tissue and intramuscular hemorrhages may occur ü Extensive bleeding may be seen after circumcision, tooth extractions, lesser injuries, and minor surgical procedures ü Hematuria ü Ecchymosis ü Epistaxis
Manifestations of Hemophilia • Bleeding tendencies range from mild to severe • Symptoms may not occur until 6 months of age: – Mobility leads to injuries from falls and accidents • Hemarthrosis: – Bleeding into joint spaces of knee, ankle, elbow, leading to impaired mobility • Ecchymosis • Epistaxis • Bleeding after procedures: – Minor trauma, tooth extraction, minor surgeries – Large subcutaneous and intramuscular hemorrhages may occur – Bleeding into neck, chest, mouth may compromise airway
Hemophilia Diagnostic Evaluation: • Hx • Presenting symptoms • Lab work (PT, PTT, fibrinogen level, platelet count, quantitative immunoelectrophoretic assay, Factor VIII & IX assays) Therapeutic Management To prevent excessive bleeding & tissue damage through the administration of the missing or ineffective factors Slide 86
Medical Management of Hemophilia • DDAVP (Desmopressin) – IV – Causes 2 -4 times increase in factor VIII activity – Used for mild hemophilia • Replace missing clotting factors • Transfusions – At home with prompt intervention to reduce complications – Following major or minor hemorrhages
Managing Hemarthrosis • During bleeding episodes, elevate and immobilize joint • Ice • Analgesics • Range-of-motion exercises after bleeding stops to prevent contractures • Physical therapy • Avoid obesity to minimize joint stress
Interventions for Hemophilia Ø Close supervision and safe environment Ø Dental procedures in controlled situation Ø Shave only with electric razor Ø Superficial bleeding—apply pressure for at least 15 minutes + ice to vasoconstrict Ø If significant bleeding occurs, transfuse for factor replacement
Hemophilia Nursing Considerations: • Control localized bleeding through topical coagulants, pressure, elevation and ice • Control bleeding of significant bleeds through administration of the necessary factor; monitor factor levels as ordered • Transfuse as ordered to help minimize disease complications Slide 90
Hemophilia Nursing Considerations: • Provide opportunities for normal growth and developmental activities; as indicated, provide injury protection for activities • PT to prevent flexion contractures and to strengthen muscles and joints when bleeding into joints has been controlled Slide 91
Hemophilia A Psychosocial Issues Guilt Challenge of hospitalizations Control issues Financial/ insurance challenges Feeling different/ unable to do certain activities • Counseling needs • Refer for genetic counseling after dx • • •
Hemophilia Nursing Considerations: • • • No rectal temps Analgesics as ordered for pain RICE (Rest, Ice, Compression, Elevation) if joint involved in a bleeding episode to reduce damage
Prognosis for Hemophilia • Historically, most died by 5 years age • Now mild to moderate hemophilia patients live near normal lives • Gene therapy for future – Infused carrier organisms act on target cells to promote manufacture of deficient clotting factor
Von Willebrand Disease • A hereditary bleeding disorder, involving deficiency of von Willebrand factor (a plasma protein, and the carrier for factor VIII) • von Willebrand factor is necessary for platelet adhesion • Transmitted as autosomal dominant trait • Occurs in males and females • Gene for disease is located on chromosome 12
Von Willebrand Disease ü Other clinical manifestations include: üGingival bleeding üEcchymosis üIncreased bleeding w/ lacerations or during surgery and dental extractions üMenorrhagia (increased menstrual bleeding) üGI bleeding
Von Willebrand Disease • Treatment: – Similar to Hemophilia A – Restore clotting factor and prevent complications associated w/ bleeding • Infusion of VWB protein concentrate • DDAVP • Stimate • Amicar for mucous membrane bleeding
Interventions for Von Willebrand Disease • Avoid aspirin or NSAIDs (increase bleeding time and inhibit platelet function) • Nursing Management: – Similar to Hemophilia A • Manage bleeding episodes with prompt infusion therapy • Children with von Willebrand have normal life expectancy if well managed
Immune Thrombocytopenic Purpura (ITP) • AKA autoimmune thrombocytopenic purpura • A disorder characterized by increased destruction of platelets in the spleen, even though platelet production in the bone marrow is normal • Autoimmune – Plts are destroyed as a result of the binding of autoantibodies to PLT antigens
Idiopathic Thrombocytopenic Purpura (ITP) • Most common bleeding disorder in children – Occurs in children 2 -10 years-old, peaks b/t 2 -5 yrs old • An acquired hemorrhagic disorder characterized by: – Thrombocytopenia: excessive destruction of platelets – Purpura: discoloration caused by petechiae beneath the skin • After a viral illness • Usually develops 1 -3 weeks after a viral infection such as chicken pox measles or rubella
Immune Thrombocytopenic Purpura (ITP) • Clinical Manifestations: – Multiple ecchymoses – Petechiae – Purpura (purplish areas where blood has collected d/t bleeding from blood vessels) – Bleeding from gums – Nosebleeds – Hematuria – Heme in stools
Signs and Symptoms of Idiopathic Thrombocytopenia Purpura • Petechiae – Pinpoint hemorrhages occurring on the body that do not blanch to pressure • Purpura – Larger purplish areas of hemorrhage in which blood collects under the tissues
Immune Thrombocytopenic Purpura (ITP) Diagnostic Evaluation: • History and PE • CBC
Immune Thrombocytopenic Purpura (ITP) Therapeutic Management: • Administration of IV or Oral corticosteroids • Intravenous immunoglobulins • Splenectomy may be indicated if treatment ineffective Slide 104
ITP Therapeutic Management: (cont’d) • Intravenous immunoglobulin (IVIg) • Intravenous anti-D, danazol, vinca alkaloids, and other immunosuppressive agents such as azathioprine and cyclophosphamide. • Platelet transfusions have been used in emergency situations.
Disseminated Intravascular Coagulation (DIC) • Life-threatening process which occurs as complication of other serious illnesses in infants and children • Most common cause of DIC is infection • An acquired pathologic process in which the clotting system is abnormally activated, resulting in widespread clot formation in the small vessels throughout the body. • These changes slow blood circulation, cause tissue hypoxia and results in tissue necrosis. • The circulating fibrin also interfere w/ clotting process and bleeding and hemorrhage result
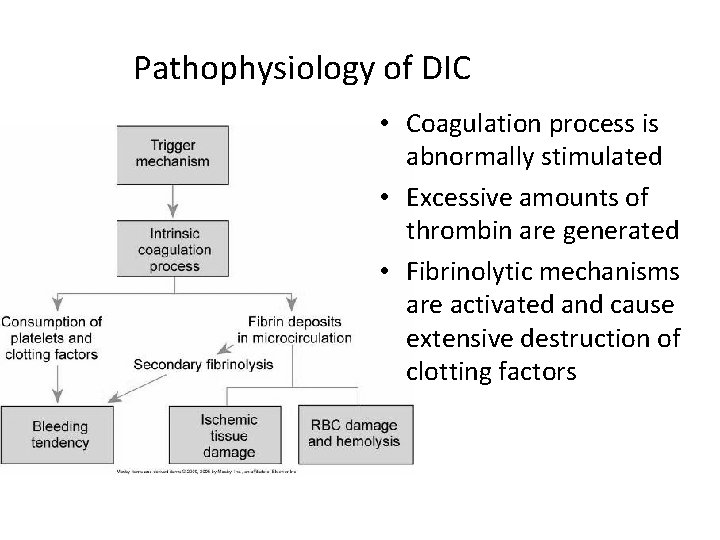
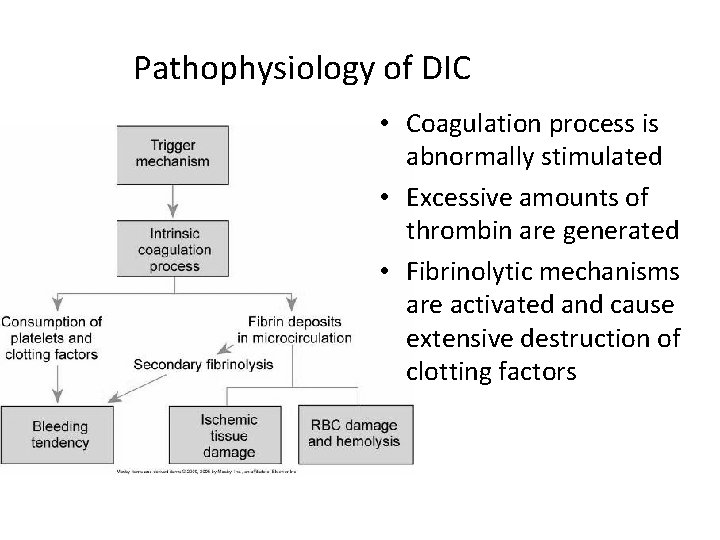
Pathophysiology of DIC • Coagulation process is abnormally stimulated • Excessive amounts of thrombin are generated • Fibrinolytic mechanisms are activated and cause extensive destruction of clotting factors
Disseminated Intravascular Coagulation (DIC) • Disorder of coagulation that occurs as complication of numerous pathologic processes: – Hypoxia – Acidosis – Shock – Endothelial damage • Treatment: – Controlling bleeding, identifying and correcting the primary cause of the disorder, and preventing further activations of clotting mechanisms
Disseminated Intravascular Coagulation (DIC) • Nursing Assessment and Diagnosis: – Involves all body systems, so frequent thorough assessment of entire body is critical – Observe for petechiae, ecchymoses, and oozing every 1 -2 hours – Observe for pooling of blood in dependent areas – Assess IV site Q 15 minutes for oozing – Examine stool for presence of blood – Assess extremities for cap refill, warmth and pulses – Frequently assess VS and LOC – I’s and O’s – Monitor O 2 sat and ABG’s – ID family’s coping strategies and support systems
Epistaxis (Nosebleeding) • Isolated and transient epistaxis is common in childhood • Recurrent or severe episodes may indicate underlying disease: – Vascular abnormalities, leukemia, thrombocytopenia, clotting factor deficiency diseases (von Willebrand disease and hemophilia)
Did you know…. . • The vessel can burst or break as the result of nosepicking, a bump or a cold or hay fever making the tissues inflamed. • Putting head back makes the bleeding continue and causes the blood to run down the child's throat, be swallowed and cause nausea. • Lying down, which slightly raises blood pressure in the head and can increase bleeding.
Nursing Considerations for Epistaxis • Keep child calm • Have child sit up and lean forward • Spit out any blood trickling down at the back of the nose into the throat - that way you can also assess the severity of the bleeding. • Pressure to nose – Point is at the front of the lower end of the septum, so get the child to pinch the soft part of the nose just above the nostrils quite firmly for 5 minutes – An ice pack on the nose can also help to slow the bleeding because it makes the blood vessels constrict. • Further evaluation if bleeding continues
Neoplastic Disorders • Leading cause of death from disease in children past infancy • Almost half of all childhood cancers involve blood or blood-forming organs
Anatomy and Physiology of Pediatric Differences • Immune system more immature in children – This affects how well body can defend itself – Nonspecific and specific cellular responses are immature in infants and premies • Children are still growing and developing – As a result, some cancers grow and progress more rapidly – Apoptosis (programmed-cell death) not welldeveloped in young children – Children more commonly present with metastases at time of dx than adults d/t the difficulty in recognizing s/sx of cancer (usually mistaken for childhood illness)
Differences between adults and children with cancer • Childhood cancers respond better to chemotherapy • Children tolerate chemotherapy better than adults • Childhood survivors of cancer need to be monitored for late-effects and long-term side effects of cancer treatment – “Late-effects” clinics
Etiology and Pathophysiology • Alterations in cellular growth occur in response to external and internal stimuli • Neoplasms are caused by one or a combination of three factors; – External stimuli that cause genetic mutations – Innate immune system and gene abnormalities – Chromosomal abnormalities
Clinical Manifestations • Vary by type and location – Pain – Cachexia • (syndrome characterized by anorexia, weight loss, anemia, asthenia (weakness) and early satiety) – Anemia – Infections – Bruising – Neurologic symptoms – Palpable mass
Diagnostic Tests • CBC • Bone marrow aspiration • Bone marrow biopsy • Lumbar puncture • CXR • Radiographic examination • MRI • CTscan • US • Biopsy of Tumor
Important blood work • CBC w/ diff • Hgb and Hct • RBC – Mean corpuscular volume (MCV), mean corpuscular hgb concentration (MCHC) and mean corpusuclar hgb (MCH) • WBC indices – Basophils, eosinophils, monocytes, lymphocytes, neutrophils (segmented and banded) • ANC – (neutrophils x WBC count)= infection-fighting capacity (ANC > 1, 000 = nml; ANC< 500= risk for infection) • Chem 7 • Others: BUN/ creat, Liver function tests, tumor markers
Clinical Therapy • Child managed by Pediatric Oncology Team • Therapy may be singular or combination – Surgery – Chemotherapy (protocol-action plan for chemo) – Radiation – Biotherapy (antibodies developed to target tumor cells for apoptosis; cancer vaccines) – HSCT (hematopoietic stem cell transplant) – Complementary therapies – Palliative care (presence of palliative care team)
Leukemias Most common form of childhood cancer 3 -4 cases per 100, 000 Caucasian children <15 years old More frequent in males >1 year old Peak onset between 2 and 6 years of age Survivability Leukemia: a broad group of malignant diseases of bone marrow and lymphatic system • Complex disease with varying heterogeneity • Classifications are increasingly complex • • •
Pathophysiology of Leukemia Ø Leukemia is an unrestricted proliferation of immature WBCs in the blood-forming tissues of the body Ø Liver and spleen are the most severely affected organs • Although leukemia is an overproduction of WBCs, often acute form causes low leukocyte count • Cellular destruction takes place by infiltration and subsequent competition for metabolic elements
Consequences of Leukemia • Anemia from decreased RBCs • Infection from neutropenia • Bleeding tendencies from decreased platelet production • Spleen, liver, and lymph glands show marked infiltration, enlargement, and fibrosis
Acute Myelogenous Leukemia (AML) • One fourth of all leukemias – 85% of the acute leukemias in adults • Abrupt, dramatic onset – Serious infections, abnormal bleeding • Uncontrolled proliferation of myeloblasts – Hyperplasia of bone marrow and spleen – AML: granulocytic, myelocytic, monocytic, myelogenous, monoblastic, and nonmyeloblastic leukemia
Acute Lymphocytic Leukemia (ALL) • Most common type of leukemia in children • 15% of acute leukemia in adults • Immature lymphocytes proliferate in the bone marrow • ALL: lymphatic, lymphocytic, lymphoblastic, and lymphoblastoid leukemia
Leukemia Diagnostic Studies • To diagnose and classify – Peripheral blood evaluation – Bone marrow evaluation • To identify cell subtype and stage – Morphologic, histochemical, immunologic, and cytogenic methods • Based on history, physical manifestations • Peripheral blood smear: – Immature leukocytes – Frequently low blood counts • Lumbar puncture to evaluate CNS involvement • Bone marrow aspiration or biopsy
Chromosome Studies ü Children with trisomy 21 have a 20 times greater risk for developing ALL ü Children with more than 50 chromosomes on the leukemic cells have the best prognosis ü Specific translocations of chromosomes on leukemic cells can affect prognosis
Leukemia Clinical Manifestations • Relate to problems caused by – Bone marrow failure • Overcrowding by abnormal cells • Inadequate production of normal marrow elements • Anemia, thrombocytopenia, ↓ number and function of WBCs
Leukemia Clinical Manifestations • Relate to problems caused by – Leukemic cells infiltrate patient’s organs • Splenomegaly • Hepatomegaly • Lymphadenopathy • Bone pain, meningeal irritation, oral lesions (chloromas)
Four Phases of Therapy for Leukemia • Induction therapy: 4 -6 weeks • CNS prophylactic therapy: intrathecal chemotherapy • Intensification (consolidation) therapy: to eradicate residual leukemic cells and prevent resistant leukemic clones • Maintenance therapy: to preserve remission
Leukemia Collaborative Care • Goal is to attain remission • Chemotherapeutic treatment – Induction therapy • Attempt to induce or bring remission • Seeks to destroy leukemic cells in the tissues, peripheral blood, bone marrow • Patient may become critically ill – Provide psychological support as well
Leukemia Collaborative Care • Chemotherapeutic treatment (cont. ) – Intensification therapy • High-dose therapy • May be given after induction therapy • Same drugs at higher doses and/or other drugs • Chemotherapeutic treatment (cont. ) – Consolidation therapy • Started after remission is achieved • Purpose is to eliminate remaining leukemic cells that may not be evident – Maintenance therapy • Lower doses of the same drug
Leukemia Chemotherapy Regimens • Combination chemotherapy – Mainstay treatment – 3 purposes • ↓ drug resistance • ↓ drug toxicity to the patient by using multiple drugs with varying toxicities • Interrupt cell growth at multiple points in the cell cycle • “Vesicants”—sclerosing agents even in minute amounts • Interventions for extravasation • Risk for anaphylaxis
Managing Problems of Drug Toxicity ØNausea and vomiting ØAnorexia ØMucosal ulceration ØNeuropathy ØHemorrhagic cystitis ØAlopecia ØMood changes ØMoon face
Leukemia Bone Marrow and Stem Cell Transplantation • Goal – Totally eliminate leukemic cells from the body using combinations of chemotherapy with or without total body irradiation
Leukemia - Bone Marrow and Stem Cell Transplantation • Eradicates patient’s hematopoietic stem cells • Replaced with those of an HLA-matched • Donors may be: – Relatives or nonrelatives – Antigen matched or mismatched • Peripheral stem cells may be used • Stem cells from umbilical cord blood • • Sibling Volunteer Identical twin Patient’s own stem cells removed before
Risks of Hematopoietic Stem Cell Transplantation (HSCT) • • • Significant risk of morbidity and mortality Graft vs. host disease (GVHD) Overwhelming infection Severe organ damage Cure after HSCT: up to 60%-70%
Hematopoietic Stem Cell Transplantation (HSCT) • Used to establish healthy cells in both malignant and nonmalignant disease • Ablative therapy: high-dose combination chemotherapy (with or without radiation) to eradicate unhealthy cells and suppress immune system to prevent rejection of transplanted marrow • Stem cells harvested from bone marrow, peripheral blood, or umbilical vein of placenta • Stem cells given to patient by IV transfusion • Newly transfused stem cells repopulate ablative bone marrow
Increased Susceptibility to Infection v At time of diagnosis and relapse v During immunosuppressive therapy v After prolonged antibiotic therapy that predisposes to the growth of resistant organism v Infection Control v. Environment v. Hand hygiene v. Visitor restriction
Prognosis for Leukemia v. If relapse after HSCT: dismal prognosis v. Identified factors for determining prognosis: v. Initial WBC count v. Age at time of diagnosis v. Type of cell involved v. Gender v. Karyotype analysis
Nursing Diagnoses for Leukemia • • • Risk for Injury related to malignant process, treatment Risk for Fluid Volume Deficit related to nausea, vomiting Altered Nutrition Impaired Skin Integrity Altered Family Processes Fear related to diagnosis, procedures, treatments
Leukemia Nursing Management • Goals of rehabilitation – Manage • Physical • Psychosocial • Spiritual • Delayed effects – Support groups
Nursing Management Planning • Overall goals – Understand cooperate with the treatment plan – Experience minimal side effects and complications of disease and treatment – Feel hopeful and supported during the periods of treatment, relapse, and remission
Nursing Considerations for Leukemia • • Assessment Nursing diagnosis Planning Implementation: – Prepare child and family for procedures – Pain management – Prevent complication of myelosuppression
Nursing Management • Many physical and psychological needs – Evokes great fear • Family also needs help • Balance demanding technical needs with a humanistic, caring approach v Patient empowered by knowledge of the disease and treatment can have a more positive outlook and improved quality of life v Nurses face special challenges when meeting the intense psychosocial needs of a patient with leukemia • Ongoing care is necessary to monitor for signs and symptoms of disease control or relapse • Teach patient and significant other – Diligence in disease management – Need for follow-up care – When to seek medical attention • Cope effectively with diagnosis, treatment regimen, and prognosis • Attain and maintain adequate nutrition • Experience no complications • Feel comfortable and supported
Lymphomas • Hodgkin disease – More prevalent in those 15 -19 years of age • Non-Hodgkin lymphoma (NHL) – More prevalent in children <14 years of age
Hodgkin Disease • Neoplastic disease originating in lymphoid system • Often metastasizes to spleen, liver, bone marrow, lungs, and other tissues – Disorder of the lymphoid system – Usually arises from a single or group of lymph nodes – Incidence: 3/100, 000; peaks in adolescent boys – Clinical Manifestations include: main sx= a nontender, firm lymphadenopathy, fever, night sweats, weight loss – Prognosis excellent: Tx based on staging: 5 year survival 90%
Four Types of Hodgkin Disease ü Lymphocytic predominance ü Nodular sclerosis ü Mixed cellularity ü Lymphocytic depletion ü Accurate staging is basis for treatment and prognosis
Classifications of Hodgkin Disease • Classification A: asymptomatic • Classification B: temperature of 38° C (100. 4° F) or higher for three consecutive days, night sweats, unexplained weight loss of 10% or more over previous 6 months
Diagnosis of Hodgkin Disease v Clinical manifestations of Hodgkin disease v Lymph node biopsy for diagnosis and staging v Presence of Reed-Sternberg cells is characteristic of Hodgkin disease
Therapeutic Management of Hodgkin Disease • Radiation • Chemotherapy (alone or with radiation) • Prognosis • Nursing considerations
Non-Hodgkin Lymphoma (NHL) • Approximately 60% of pediatric lymphomas are NHL • Clinical appearance: – Disease usually diffuse rather than nodular – Cell type undifferentiated or poorly differentiated – Dissemination occurs early, often, and rapidly – Mediastinal involvement and invasion of meninges
Soft tissue tumors • Non-Hodgkin’s Lymphoma – 3 types: • Lymphoblastic Lymphoma (30 -40%) • Small noncleaved cell (Burkit’s) Lymphoma (40 -50%) • Large cell Lymphoma (15%) – Malignant tumors of lymphoreticular (internal framework of the lymph sx) origin – Peak incidence b/t 7 -11 y. o; 3 X more common in boys
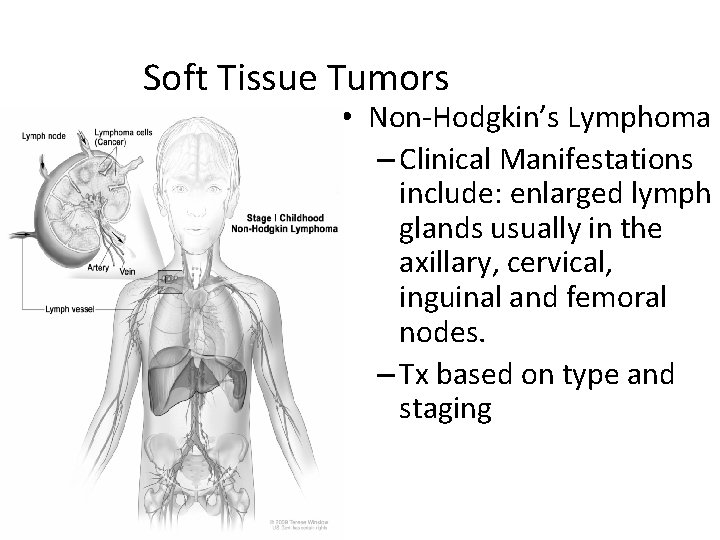
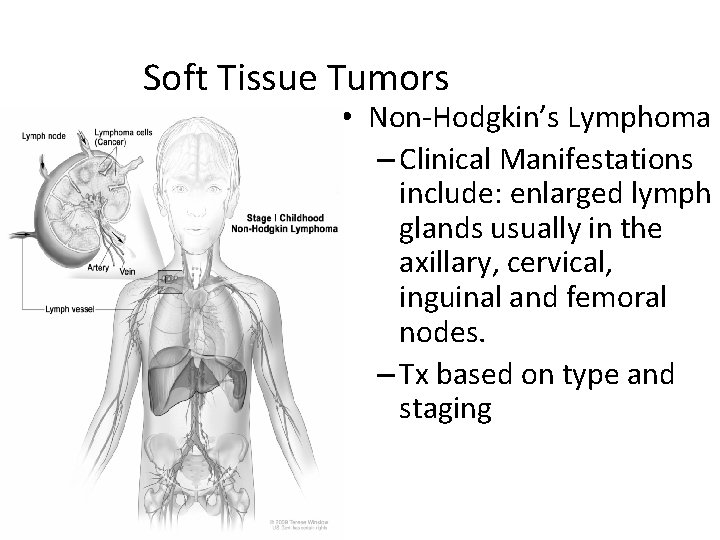
Soft Tissue Tumors • Non-Hodgkin’s Lymphoma – Clinical Manifestations include: enlarged lymph glands usually in the axillary, cervical, inguinal and femoral nodes. – Tx based on type and staging
NHL (cont’d) • Symptoms of Non. Hodgkin's Lymphoma • Painless swollen lymph nodes in one or more places • Neck lymph node swelling • Groin lymph node swelling • No pain in early stages • Enlarged liver and spleen • Unexplained fever with flulike symptoms • Night sweats • Weight loss • Itchy red skin • Fatigue
Wiskott-Aldrich Syndrome • First described by Wiskott in 1937 and was further characterized by Aldrich in 1954. • X-linked recessive immunodeficiency disorder • Characterized by the triad of recurrent bacterial sinopulmonary infections, eczema and a bleeding diathesis caused by thrombocytopenia and platelet dysfunction
Wiskott-Aldrich Syndrome • In addition, children with WAS are at elevated risk for developing: – Other autoimmune diseases – Anemia – Arthritis – Inflammatory bowel syndrome – nephritis (kidney inflammation) – lymphoma and other malignant cancers
Wiskott-Aldrich Syndrome • A diagnosis of WAS is usually made based on: – a complete medical history and physical examination of your child – Serum platelets – presence of the antibody immunoglobin in blood – The diagnosis can be confirmed with a genetic test to detect the presence of the mutation responsible for WAS.
Wiskott-Aldrich Syndrome • Guarding against infection Basic precautions – You should be sure to always: • keep your child away from crowds, dirty environments and sick people • use protective face masks at the recommendation of your child’s doctor • follow a strict handwashing regimen for your child, your family and any visitors •
Wiskott-Aldrich Syndrome • Antibody infusions Does not have healthy B cells that produce antibodies against infection, may need regular infusions (administration through a vein) of the antibody immunoglobin(also known as immune gammaglobin).
Wiskott-Aldrich Syndrome • Guarding against bleeding/bruising Some measures for lowering the risk of uncontrolled bleeding and bruising can include: – taking corticosteroids – receiving infusions of the antibody immunoglobin – receiving platelet transfusions (this is usually only prescribed in an emergency situation) – removing the spleen (this is usually only prescribed in an emergency situation)
Wiskott-Aldrich Syndrome • Managing eczema (atopic dermatitis) • Stem cell/bone marrow transplants This is the only available treatment option that has a chance of providing a permanent cure. • Stem cells are a versatile type of cell found in bone marrow.
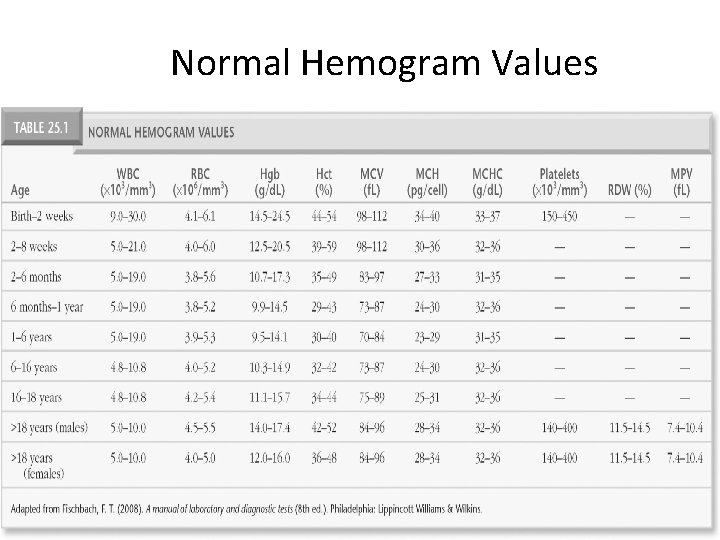
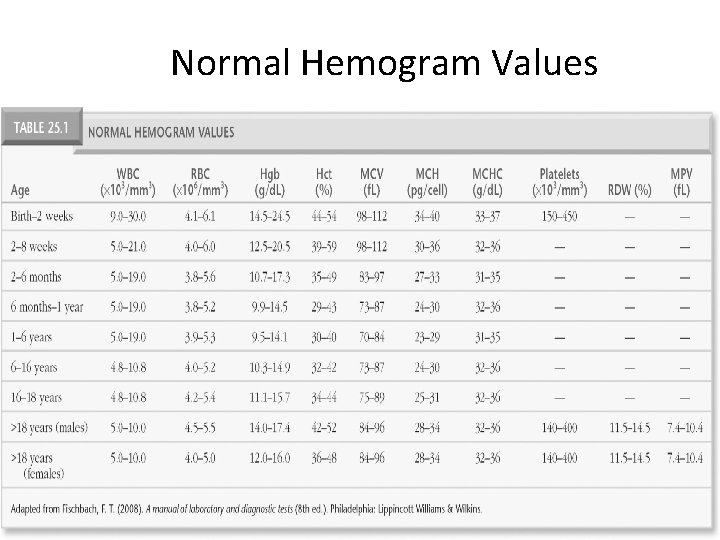
Normal Hemogram Values Adapted from Fischbach, F. T. (2008). A manual of laboratory and diagnostic tests (8 th ed. ). Philadelphia, PA: Lippincott Williams & Wilkins.
 Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Assessment of hematologic system
Assessment of hematologic system Hypochromic red cells
Hypochromic red cells Hematologic system assessment
Hematologic system assessment Nursing care of hospitalized child
Nursing care of hospitalized child Nursing care of hospitalized child
Nursing care of hospitalized child Hospital environment for a sick child ppt
Hospital environment for a sick child ppt Nursing care plan for hoarding disorder
Nursing care plan for hoarding disorder Nursing care plan for cataract
Nursing care plan for cataract Levels of health care primary secondary tertiary
Levels of health care primary secondary tertiary 전위 순회
전위 순회 Modern concept of pediatric nursing
Modern concept of pediatric nursing Modern concept in child health care pdf
Modern concept in child health care pdf Definition pediatric nursing
Definition pediatric nursing Child health nursing gnm 2nd year question paper
Child health nursing gnm 2nd year question paper Illinois ccap
Illinois ccap Hbyc
Hbyc Utah department of health child care licensing
Utah department of health child care licensing Child care facility rules and regulations answers
Child care facility rules and regulations answers Children's responsibilities
Children's responsibilities Cn label fish sticks
Cn label fish sticks Moe childcare leave
Moe childcare leave Child care resource center
Child care resource center Preventive health and safety in the child care setting
Preventive health and safety in the child care setting Manitoba child care association
Manitoba child care association Trilemma of child care
Trilemma of child care Working connections
Working connections Wv dhhr child care assistance
Wv dhhr child care assistance Georgia child care licensing regulations
Georgia child care licensing regulations Section 47 child care act
Section 47 child care act Inclusion works creating child care programs
Inclusion works creating child care programs Ga form 3231 blank
Ga form 3231 blank Maine child care subsidy program
Maine child care subsidy program Pros and cons of child care centers
Pros and cons of child care centers Child care and protection act 3 of 2015
Child care and protection act 3 of 2015 Residential child care institutions
Residential child care institutions Edcc dublin
Edcc dublin Online childcare invoice
Online childcare invoice Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Các số nguyên tố
Các số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Model of nursing care delivery
Model of nursing care delivery How to write a care plan
How to write a care plan Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Evaluation process in nursing
Evaluation process in nursing Functional care delivery model
Functional care delivery model Associative looseness
Associative looseness Nursing bed positions
Nursing bed positions Perioperative definition nursing
Perioperative definition nursing Fluothane
Fluothane Post operative nursing care
Post operative nursing care Nail care procedure in nursing
Nail care procedure in nursing Gingivitis nursing diagnosis
Gingivitis nursing diagnosis Hernia nursing care plan
Hernia nursing care plan Chapter 41 rehabilitation and restorative nursing care
Chapter 41 rehabilitation and restorative nursing care Chest pain care plan
Chest pain care plan Post operative nursing care
Post operative nursing care Atraumatic care definition
Atraumatic care definition What is atraumatic care
What is atraumatic care Virginia henderson philosophy of nursing
Virginia henderson philosophy of nursing Nursing diagnosis of somatoform disorder
Nursing diagnosis of somatoform disorder External fixation device nursing care
External fixation device nursing care Nursing care plan case scenario
Nursing care plan case scenario 10 contraindications that would prevent a manicure
10 contraindications that would prevent a manicure Family care plan in community health nursing
Family care plan in community health nursing Nursing narrative note example
Nursing narrative note example Gout nursing diagnosis
Gout nursing diagnosis Nursing care logo
Nursing care logo Contraindications of colostomy care
Contraindications of colostomy care Different types of cast
Different types of cast Nursing care plan for burns
Nursing care plan for burns Nursing care plan concept map
Nursing care plan concept map Nursing care plan for homicidal ideation
Nursing care plan for homicidal ideation Ngt nursing diagnosis
Ngt nursing diagnosis Nursing division 1
Nursing division 1 Nursing management preoperative care
Nursing management preoperative care Primary nursing vs total patient care
Primary nursing vs total patient care Oncology nursing management in cancer care
Oncology nursing management in cancer care Dorothea orem model
Dorothea orem model Nursing care plan for liver cirrhosis
Nursing care plan for liver cirrhosis Nursing interventions for anxiety
Nursing interventions for anxiety Pulmonary embolism nursing management
Pulmonary embolism nursing management Hepatitis a incubation period
Hepatitis a incubation period Drainage nursing
Drainage nursing Fundamentals of nursing care concepts connections & skills
Fundamentals of nursing care concepts connections & skills Buck's traction
Buck's traction Nursing diagnosis for undescended testis
Nursing diagnosis for undescended testis Ventriculostomy care nursing
Ventriculostomy care nursing Chapter 2 the nursing assistant and the care team
Chapter 2 the nursing assistant and the care team Nursing care plan for typhoid fever slideshare
Nursing care plan for typhoid fever slideshare Nursing management of ophthalmia neonatorum
Nursing management of ophthalmia neonatorum Wernicke-korsakoff syndrome
Wernicke-korsakoff syndrome What is shock
What is shock Schizophrenia disorganized behavior
Schizophrenia disorganized behavior Progressive patient care definition
Progressive patient care definition Nursing management of pph
Nursing management of pph Nursing management of pph
Nursing management of pph Nursing care plan of mumps
Nursing care plan of mumps Physical assessment
Physical assessment Rheumatoid arthritis nursing interventions
Rheumatoid arthritis nursing interventions Nursing care plan of cancer patients ppt
Nursing care plan of cancer patients ppt Nursing care plan for conjunctivitis slideshare
Nursing care plan for conjunctivitis slideshare Nursing care plan for anemia slideshare
Nursing care plan for anemia slideshare Nursing management of fetal distress
Nursing management of fetal distress Homan signs
Homan signs Nursing care for pulmonary tuberculosis slideshare
Nursing care for pulmonary tuberculosis slideshare Nursing diagnosis of meningitis slideshare
Nursing diagnosis of meningitis slideshare Nursing care plan for pneumonia
Nursing care plan for pneumonia Cushing's triad
Cushing's triad Bundle of urinary catheter
Bundle of urinary catheter Battle's sign
Battle's sign Futuristic nursing definition
Futuristic nursing definition Nursing care plan for anemia in pregnancy slideshare
Nursing care plan for anemia in pregnancy slideshare Bulimia nervosa nursing care plan
Bulimia nervosa nursing care plan Nursing care plan for diabetes mellitus slideshare
Nursing care plan for diabetes mellitus slideshare Pyloric valve
Pyloric valve Patho
Patho Nursing care for gastrointestinal disorders
Nursing care for gastrointestinal disorders Chapter 2 the nursing assistant and the care team
Chapter 2 the nursing assistant and the care team Steriotaxis
Steriotaxis Standard 3 care certificate
Standard 3 care certificate Polii magnetului
Polii magnetului Palliative care vs hospice care
Palliative care vs hospice care Se inmultesc prin oua
Se inmultesc prin oua Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate