NUR 316 Management of the Diseases in the

- Slides: 59
NUR 316 Management of the Diseases in the Respiratory System
Learning objectives At the end of this modules, students will be able: q Describe the structures and functions of the upper and the lower respiratory tracts. q Discriminate between normal and abnormal assessment findings identified by inspection, palpation, percussion, and auscultation of the respiratory system. q Recognize and evaluate the major symptoms of respiratory dysfunction. q Identify the diagnostic tests to evaluate respiratory function.
Glossary Apnea: temporary cessation of breathing. Bronchoscopy: direct examination of the larynx, trachea, and bronchi using an endoscope. Dyspnea: difficulty/ shortness of breath. Hypoxemia: decrease in arterial oxygen tension in the blood. Hypoxia: decrease in oxygen supply to the tissue and cells. Hemoptysis: expectoration of blood from the respiratory tract. Orthopnea: inability to breathe easily except in an upright position. Tachypnea: abnormal rapid respiration.
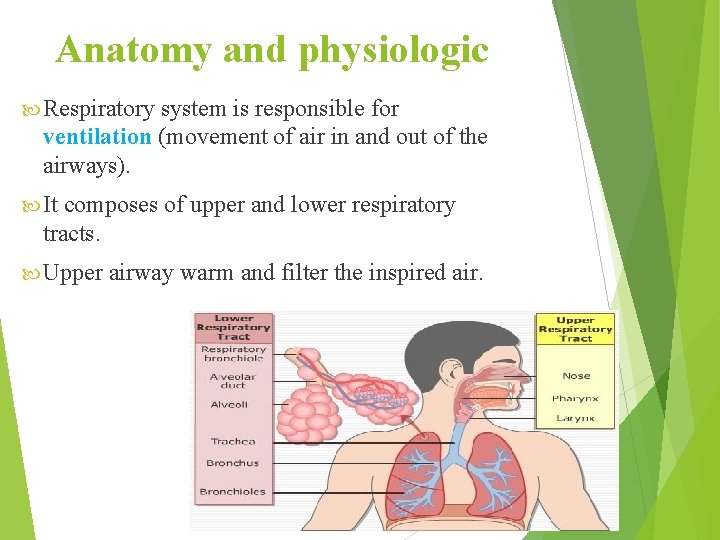
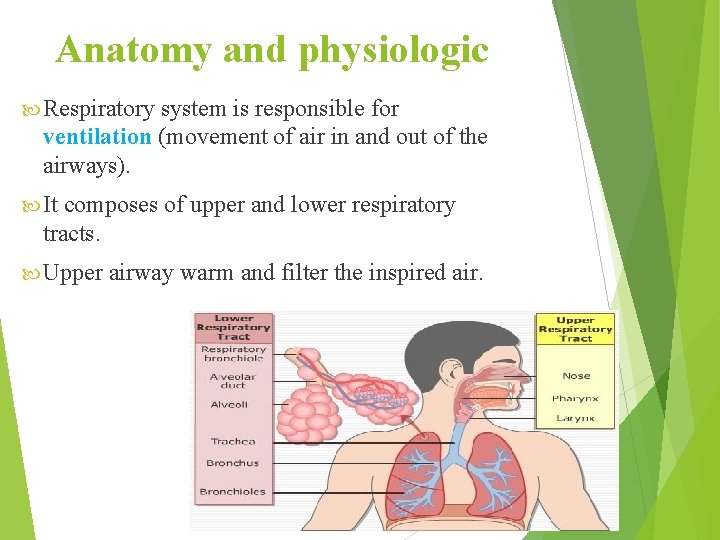
Anatomy and physiologic Respiratory system is responsible for ventilation (movement of air in and out of the airways). It composes of upper and lower respiratory tracts. Upper airway warm and filter the inspired air.
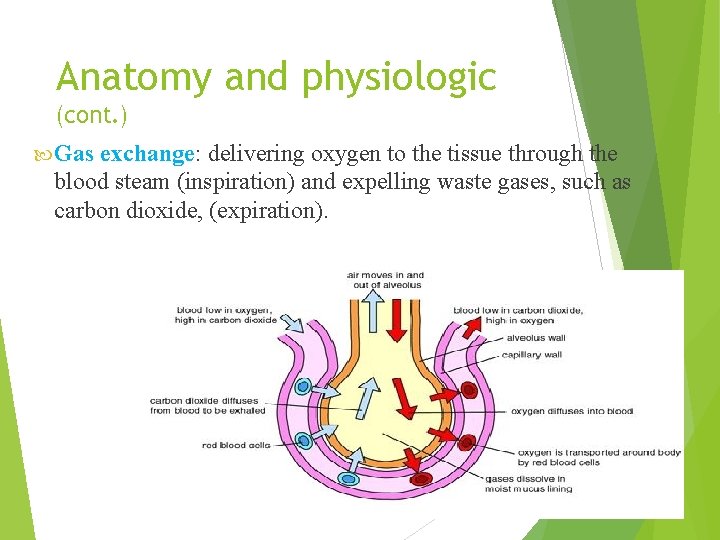
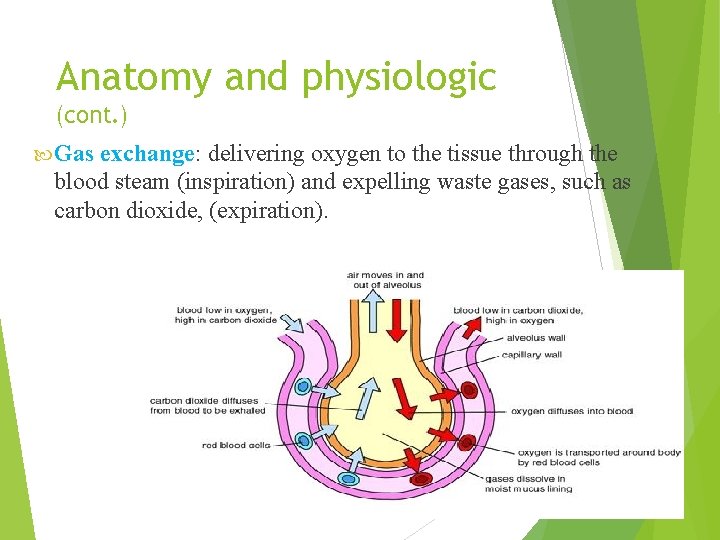
Anatomy and physiologic (cont. ) Gas exchange: delivering oxygen to the tissue through the blood steam (inspiration) and expelling waste gases, such as carbon dioxide, (expiration).
Anatomy and physiologic (cont. ) Ventilation is effected by three factors: q Airway pressure: the movement of the diagram during inspiration create a negative pressure which permits ventilation. q Airway resistance: determined by the size/radius of airways. q Compliance: is the elasticity and expandability of lung and the thoracic cavity. Requires the presence of the “surfactant”.
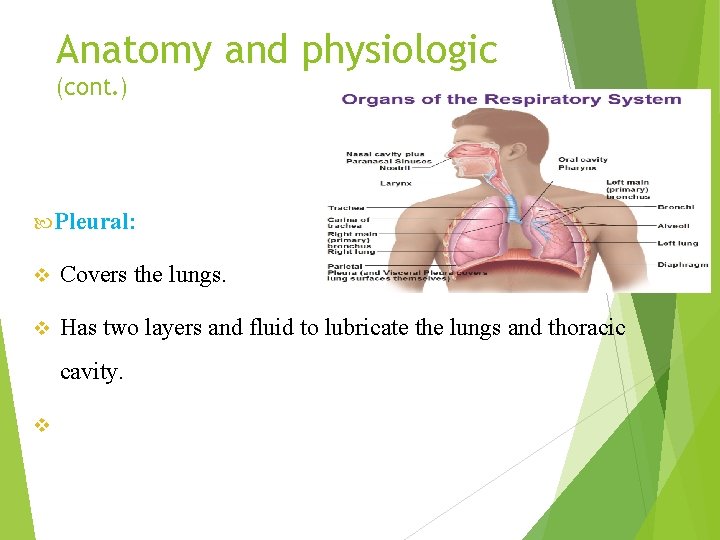
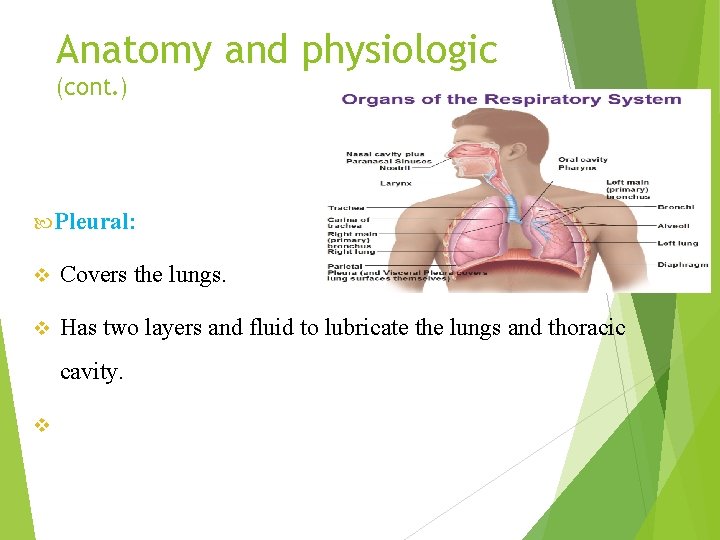
Anatomy and physiologic (cont. ) Pleural: v Covers the lungs. v Has two layers and fluid to lubricate the lungs and thoracic cavity. v
I-Health history Elicit a description of the present illness and chief complaint, including onset, course, duration, location, and precipitating and alleviating factors. Cardinal signs and symptoms of respiratory dysfunction include: - Dyspnea Orthopnea Cough which may be productive or non productive Increased sputum, which may be purulent (yellow or green), rusty, bloody, or mucoid sputum Chest pain Wheezing and crackles Clubhing of fingers Hemoptysis Cyanosis (e. g. buccal, peripheral)
- b-Explore the client's health history for risk factors associated with respiratory disease including : (1) Personal or family history of lung disease (2) Smoking (the most significant contributing factor in lung disease) (3) Occupational or vocational exposure to allergens or environmental pollutants ( 4) Age-related changes in lung capacity and respiratory function (5) History of upper respiratory infection (6) Postoperative changes resulting in diminished respiratory excursion
Physical examination a- Inspection (1) observe general appearance, noting body size, age, skin quality and color, and posture. (2) Inspect configuration and movement of the thorax during respiration. (3)Assess characteristics of respiration, including rate, rhythm, depth and muscles used for breathing. (4) Note presence of cough and the nature and character of sputum (e. g. purulent, bloody)
Palpation. Palpate the chest to detect painful areas or masses on the chest surface and evaluate chest excursion and the presence or absence of fremitus (i. e. vibration). Percussion. Assess chest sounds to evaluate underlying tissues. Resonant sound indicates air-filled lung (normal), whereas dull or flat sound suggests presence of firm mass (usually abnormal). Hyperresonant sound in emphysema.
Auscultation. Listen to air movement in lungs to detect normal or adventitious breath sounds. (1) Vesicular sounds are low-pitched, rustling sounds heard over most of lung field, most prominently on inspiration. They indicate normal, clear lungs. (2) Bronchial sounds are high-pitched tubular sounds with a slight pause between inspiration and expiration. They are normal over large airways. (3) Bronchovesicular sounds are combination of vesicular and bronchial sounds, normally heard anterior to the right or left of the sternum and posterior between the scapulae; inspiration and expiration are equal. ' (4) Adventitious breath sounds are crackles (i. e. fine to coarse), wheezes and pleural friction rub. https: //www. youtube. com/watch? v=5 JA 6 D 1 Mguh 0
Laboratory and diagnostic studies Radiographic and scanning studies are done to visualize respiratory system structures. The studies include: Chest radiography, chest tomography Lung scan Computed tomography (CT) scan Magnetic Resonance Imaging(MRI).
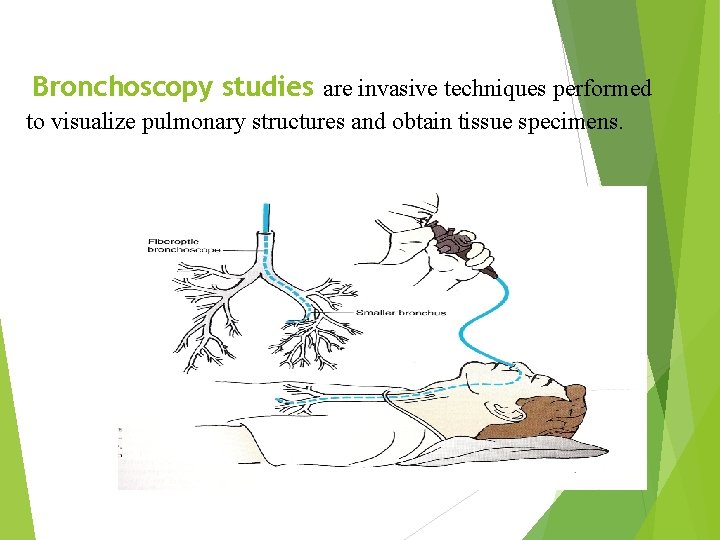
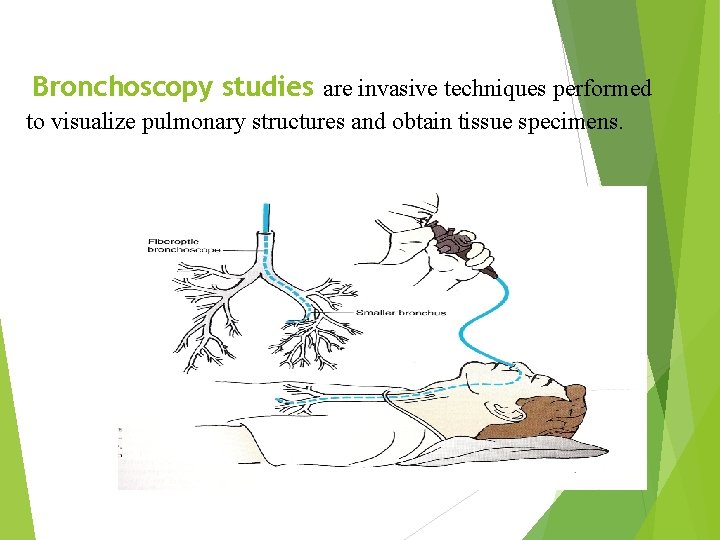
Bronchoscopy studies are invasive techniques performed to visualize pulmonary structures and obtain tissue specimens.
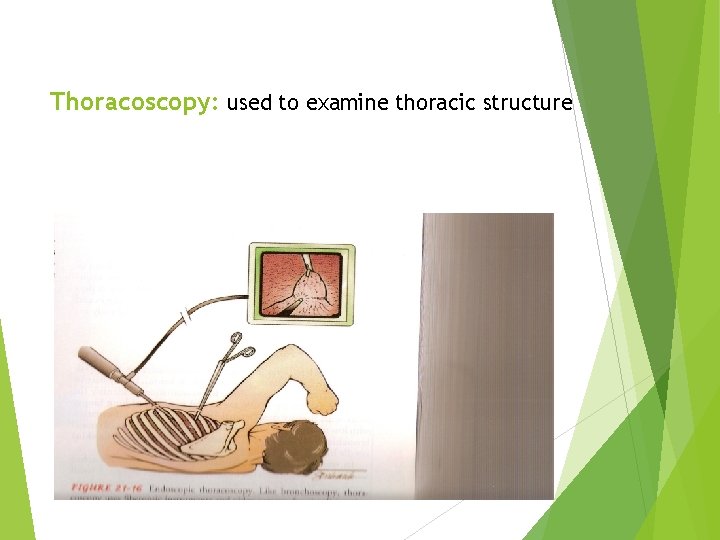
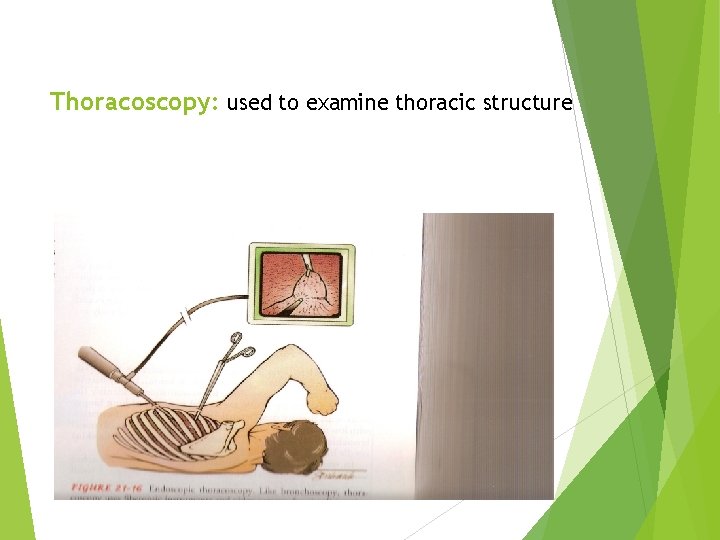
Thoracoscopy: used to examine thoracic structure
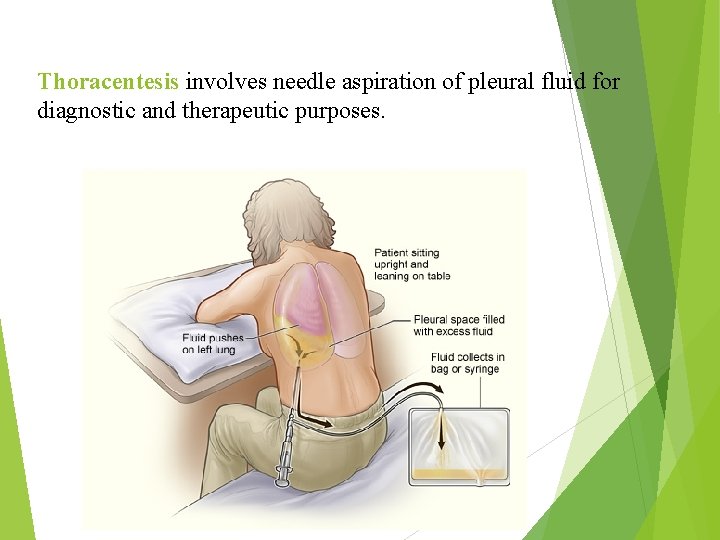
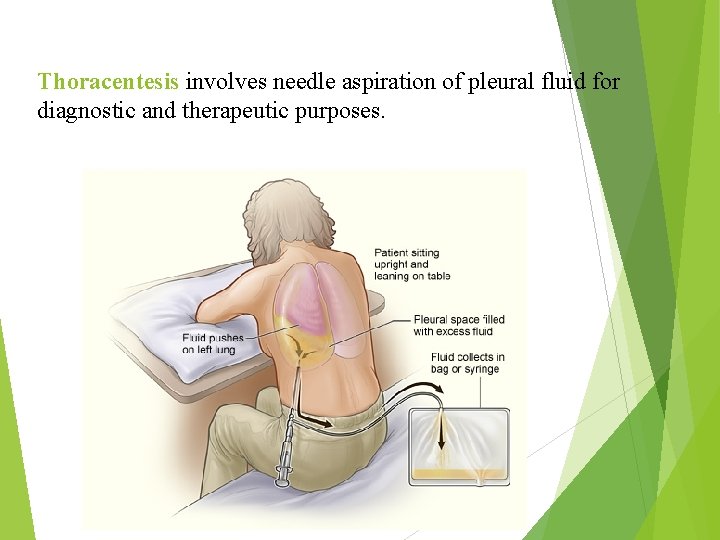
Thoracentesis involves needle aspiration of pleural fluid for diagnostic and therapeutic purposes.
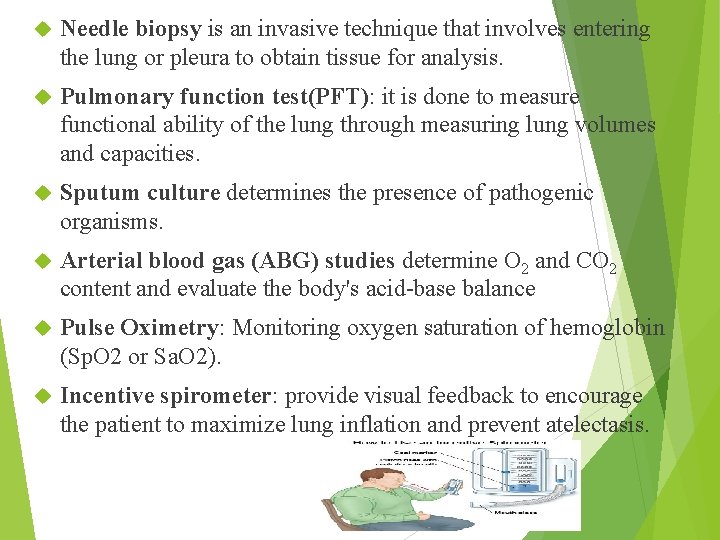
Needle biopsy is an invasive technique that involves entering the lung or pleura to obtain tissue for analysis. Pulmonary function test(PFT): it is done to measure functional ability of the lung through measuring lung volumes and capacities. Sputum culture determines the presence of pathogenic organisms. Arterial blood gas (ABG) studies determine O 2 and CO 2 content and evaluate the body's acid-base balance Pulse Oximetry: Monitoring oxygen saturation of hemoglobin (Sp. O 2 or Sa. O 2). Incentive spirometer: provide visual feedback to encourage the patient to maximize lung inflation and prevent atelectasis.
Nursing diagnosis Ineffective breathing pattern Impaired gas exchange Altered tissue perfusion (peripheral) Activity intolerance Pain Anxiety Ineffective individual coping Knowledge deficit Risk for infection
Implementation Assess respiratory status and tissue perfusion, including respiratory rate, depth and effort; level of consciousness; lung sounds; peripheral cyanosis; cap illary refill time; color and consistency or sputum; and pulse oximetry. Improve breathing patterns. a. Encourage upright position (semi-Fowler or high-Fowler position) b. Encourage the client to increase fluid intake to at least 2 to 3 liters of fluid each day, unless contraindicated as in congestive heart failure. c. Use of incentive spirometer
Promote gas exchange Administering oxygen therapy. Analyze ABG values and pulse oximetry to determine need for oxygen therapy. Assist in administering nebulizer treatment. Encourage effective coughing. Instruct client to take three deep breaths in through the nose and out through the mouth, and on the third breath pull in the abdominal muscles and cough twice forcefully with mouth open. Encourage the client to lie on the affected side to splint the area if there is pain when coughing. Encourage the client to eliminate or minimize exposure to all pulmonary irritants, and advise the client to quit smoking.
Improve activity tolerance. Encourage client to alternate rest with activity to prevent overexertion that may exacerbate symptoms and to increase activity gradually. Provide pain management. Assess the client for pain, and exclude other potential complications. Instruct the client about splinting when the client has chest pain, Promote infection control measures. Instruct the client to avoid crowds or people with known colds, flu, or respiratory infection. b. Implement standard precautions and droplet or airborne precautions as indicated.
Upper respiratory Tract Infection(URTI) URTI follows invasion of the upper respiratory organs by microbes. Upper respiratory organs include the: Nose, sinuses, throat Common cold is an example of an upper respiratory infection. Common cold is caused by a virus Symptoms: - Elevated temperature (fever) Runny nose Watery eyes Treatment of common cold: Use of antipyretic such as aspirin Rest Increased fluid intake Upper respiratory infections sometimes move down into the chest and develop into bronchitis or even pneumonia.
Pneumonia Description. Pneumonia is an inflammatory process involving the respiratory bronchioles, alveolar space and walls, and lobes, caused primarily by chemical irritants or by specific bacterial, viral, fungal, mycoplasmal, or parasitic organisms. Pneumonia is the most common cause of death from infectious disease in North America and the fifth leading cause of death among the elderly.
Types of pneumonia: Community Acquire Pneumonia: (CAP) occurs either in the community setting or within the first 48 hours of hospitalization. The organisms that most frequently cause CAP are Streptococcus pneumonia, Haemophilus influenza, and atypical organisms ( Legionella, Mycoplasma, Chlamydia& viral) Hospital Acquire Pneumonia : (HAP) also known as Nasocomial infection Occurring 48 hours or longer after admission to the hospital. Bacteria are responsible for the majority of HAP infection, including Pseudomonas and Enterobacter, Staphylococcs aureus and Streptococcus pneumonia.
Pneumonia in Immunocompromized Host: E. g. pneumocystic carinii , fungal & tuberculosis. It is occur most commonly in patient with AIDS , nutritional depletion , use of broad –spectrum antimicrobial agent, corticosteroids, chemotherapy, and long term life- support technology (mechanical ventilation) Aspiration Pneumonia: refers to entry of endogenous or exogenous substance into the lower air way such as gastric content.
Causes of and contributing 1 - Smoking and air pollution 3 - Altered consciousness: alcohalizm, head injury, seizure, anaesthesia, drug overdose 4 - Tracheal intubations (endotracheal intubations, trachestomy) 5 - Upper respiratory tract infection 6 - Chronic diseases: chronic lung disease, diabetes mellitus, heart disease, uremia, cancer, 7 - Immunosuppressant 8 - Malnutrition 9 - Inhalation or aspiration of noxious substances 10 - Bed rest and prolonged immobility 11 - Depress cough reflex
Pathophysiology. Pneumonia often affects both ventilation and diffusion. An inflammatory reaction occurs in the alveoli, producing an exudates that interferes with the diffusion of oxygen and carbon dioxide and fill the alveolar air spaces, producing lung consolidation Areas of the lung are not adequately ventilated because of secretions and mucosal edema that cause partial occulsion of the bronchi or alveoli with a resultant decrease in alvelor oxygen tension and bronchospasm may occur. Ventilation – perfusion mismatching or Impaired gas exchange in the alveoli leads to various degrees of hypoxia, depending on the amount of lung tissue affected.
Clinical manifestations A- Typical pneumonia syndrome is characterized by: Sudden onset fever over 40 C , chills, cough productive with Purulent sputum and pleurisy chest pain, dullness with consolidation on percussion of chest , dyspnea, respiratory grunting, and nasal flaring , Flushed cheeks; cyanotic lips and nail beds , anxiety and confusion. In the elderly, the only signs may be mental status change and dehydration. B- Atypical Pneumonia syndrome: is characterized by gradual onset, dry cough and extrapulmonary manifestations as headach, fatigue, sore throat, nausea, vomiting and diarrhea. Crackles are heard.
Laboratory and diagnostic study findings Chest radiograph shows density changes, primarily in the lower lung fields. Sputum culture and sensitivity are positive for a specific causative organism. While blood cell (WBC) count is elevated in pneumonia of bacterial origin; WBC count is depressed or normal in pneumonia of mycoplasma or viral origin.
Nursing management Administer prescribed medications, which may include: Antibiotics (Penicillne, Erthromycine, Gentamicine) Mucolytics. expectorants, or antitussive agents& antipyretic Promote infection control measures, especially droplet precautions as indicated. Prevent aspiration pneumonia in a client receiving tube feedings. Keep the client in an upright position during feedings and for 30 minutes afterward. Check for residual gastric contents; if more than 100 m. L, stop feeding and reevaluate. Oxygen administer Warm, moist inhalation Increase fluid intake
Complication of pneumonia: 1 - Pleurisy: inflammation of pleura 2 - Pleural effusion: accumulation of fluid in pleural space 3 - Empyema: accumulation of pus in pleural space 4 - Atelectasis: collapsed, airless alveoli of one or part of one lobe may ocurr 5 - Pericarditis: inflammation of pericardium 6 - Arthritis: inflammation of joint 7 - Meningitis: inflammation of brain layer 8 - Lung abscess
Chronic obstructive pulmonary disease (COPD) is a group of disorders associated with persistent or recurrent obstruction of air flow, which include chronic bronchitis, emphysema, and asthma. These conditions frequently overlap. Most commonly, bronchitis and emphysema occur together. Asthma frequently occurs alone without the triad of bronchitis, emphysema, and asthma.
Etiology 1 -Chronic bronchitis and emphysema. Major causes and contributing factors to these disorders, which are irreversible, include Smoking Air pollution Occupational exposure to respiratory irritants Allergies Autoimmunity Infection Genetic predisposition Aging
2 - Asthma is a reversible diffuse airway obstruction with a possible genetic component. It may be extrinsic or intrinsic. Extrinsic factors include external agents or specific allergens (e. g. dust, foods, mold spores, insecticides). Intrinsic factors include upper respiratory infection, exercise, emotional stress, cold, or other nonspecific factors. Status asthmatics is a severe and persistent asthma that lasts longer than 24 hours and does not respond to conventional therapy.
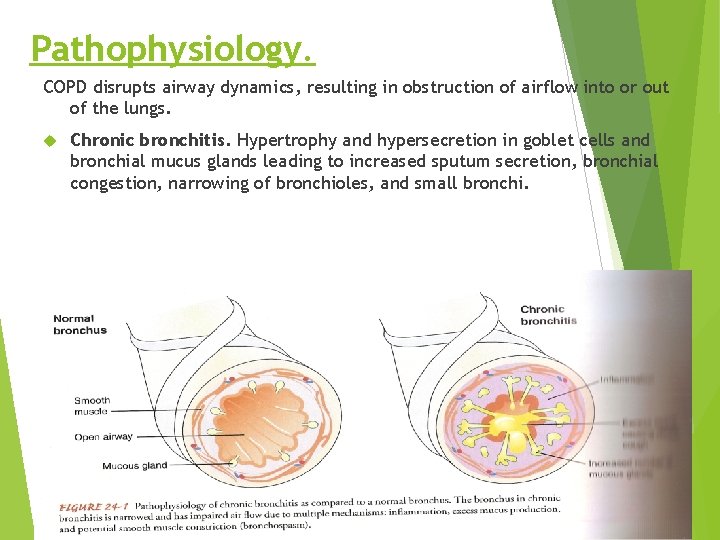
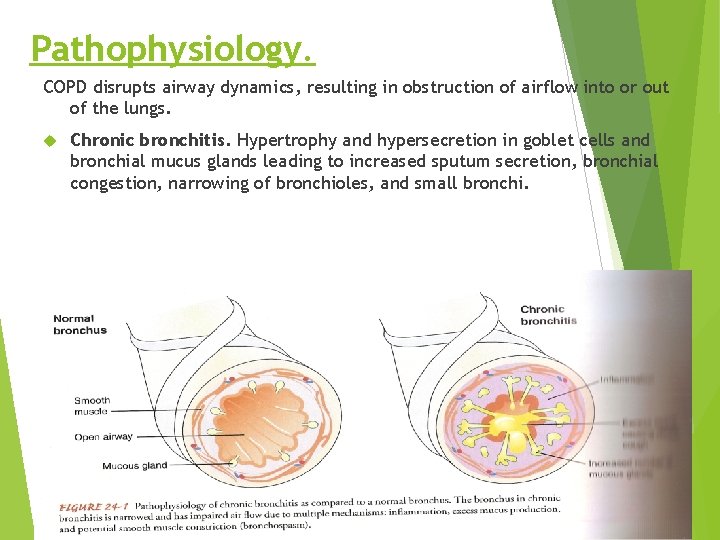
Pathophysiology. COPD disrupts airway dynamics, resulting in obstruction of airflow into or out of the lungs. Chronic bronchitis. Hypertrophy and hypersecretion in goblet cells and bronchial mucus glands leading to increased sputum secretion, bronchial congestion, narrowing of bronchioles, and small bronchi.
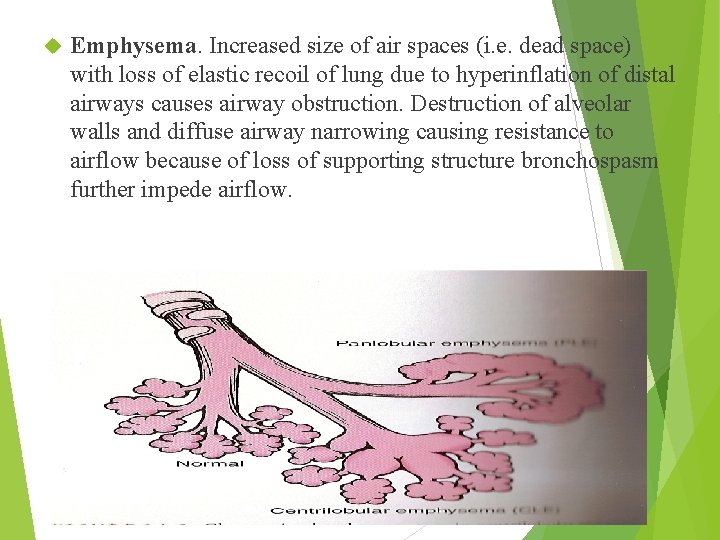
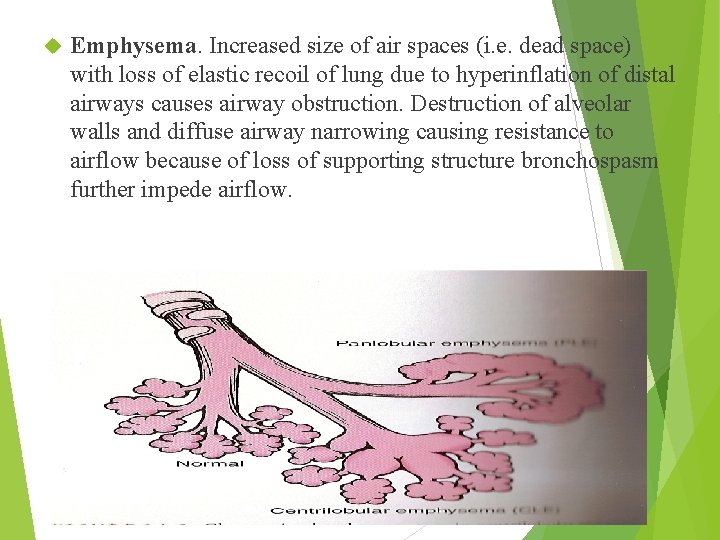
Emphysema. Increased size of air spaces (i. e. dead space) with loss of elastic recoil of lung due to hyperinflation of distal airways causes airway obstruction. Destruction of alveolar walls and diffuse airway narrowing causing resistance to airflow because of loss of supporting structure bronchospasm further impede airflow.
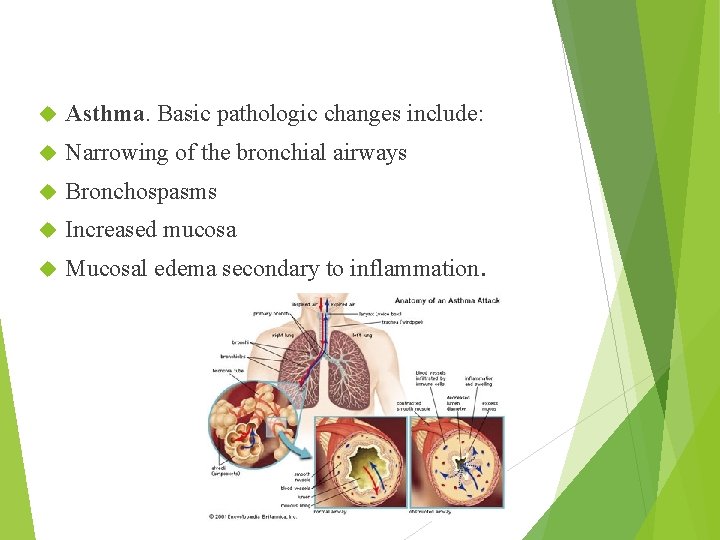
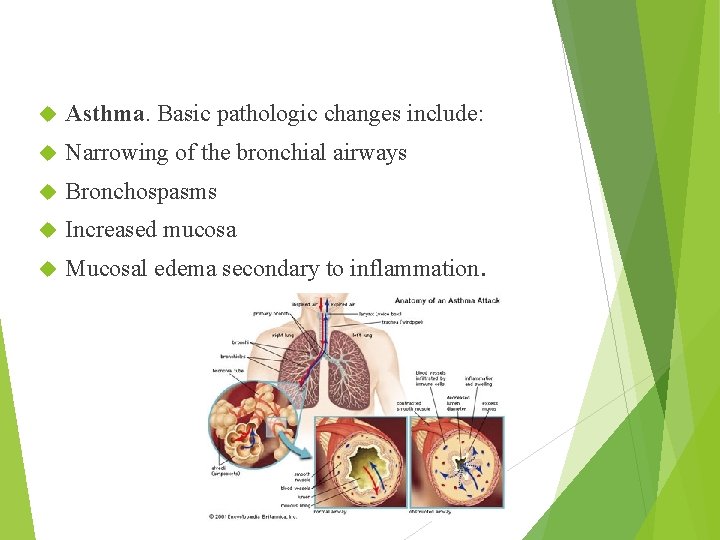
Asthma. Basic pathologic changes include: Narrowing of the bronchial airways Bronchospasms Increased mucosa Mucosal edema secondary to inflammation.
Clinical manifestations Chronic bronchitis (1) History of productive cough that lasts 3 months per year for 2 consecutive years (2) Persistent cough, known as smoker's cough, usually in the winter months (3) Persistent sputum production (4) Recurrent acute respiratory infections (5) "Pink puffer appearance
Emphysema (1) History of chronic bronchitis (2) Slow onset of symptoms (typically over several years), which can lead to right sided heart failure (i. e. cor pulmonale) (3) Progressive dyspnea, initially on exertion and later also at rest (4) Progressive cough and increased sputum production, use of accessory muscles (5) Anorexia with weight loss and profound weakness (6) Dusky color leading to cyanosis (7) Clubbing of fingers
Asthma (1) Chest tightness and dyspnea (2) Cough (3) Wheezing (4) Expiration more strenuous and prolonged than inspiration (5) Use of accessory muscles of respiration & nasal flaring (6) Hypoxia with restlessness, anxiety, cyanosis, weak pulse, and diaphoresis
Laboratory and diagnostic study findings Chronic bronchitis (1) Pulmonary function studies identify decreased forced expiratory volume (FEV), decreased forced vital capacity (FVC), increased residual volume (RV), and total lung capacity (TLC) that is normal to slightly increased. (2) Chest radiograph shows an enlarged heart with a normal or flattened diaphragm. (3) ABG studies during the acute phase show significantly increased Paco 2 and decreased Pa 02. (4) Sputum culture reveals secondary bacterial infection with gram-negative or gram-positive organisms, such as Diplococcus pneumoniae and H. influenzae.

b. Emphysema (1) Pulmonary function studies identify decreased FEV, decreased FVC, increased RV, and increased TLC. (2) Chest radiograph shows a Flattened diaphragm, decreased vascular markings with hyperradiolucence, and increased anteroposterior (AP) diameter (i. e. "barrel chest"). (3) ABG studies detect increased Pa. C 02 and decreased Pa 02 (4) Blood analysis reveals polycythemia (i. e. increased numbers of red blood cells in response to hypoxemia). C. Asthma. (1)-Pulmonary function studies during acute episode identify markedly decreased FEV, increased RV, and increased TLC in response to air trapping. These study values improve after treatment.
Nursing management Provide nursing care for the client with chronic bronchitis or emphysema. a. Administer prescribed medications, which may include antibiotics, bronchodilator, mucolytic agents, and corticosteroids. Antibiotics should be administered at the first sign of infection, such as a change in the sputum. Narcotics, sedatives, and tranquilizers, which can further depress respirations, should be avoided.
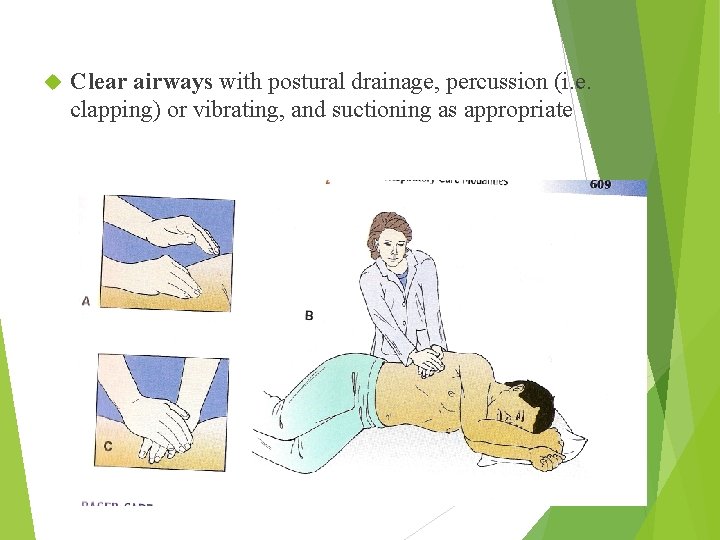
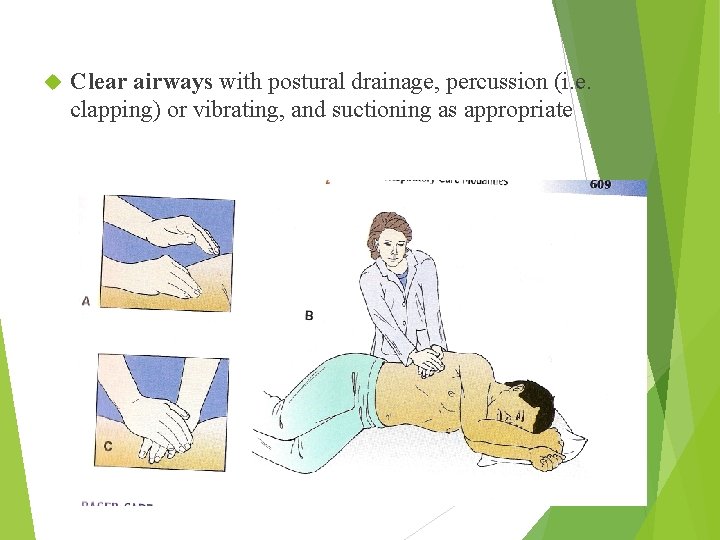
Clear airways with postural drainage, percussion (i. e. clapping) or vibrating, and suctioning as appropriate
Promote infection control. Encourage the client to obtain influenza and pneumonia vaccines at prescribed times. Improve breathing patterns. Demonstrate and encourage diaphragmatic and purse-lip breathing. Have the client take a deep breath and blow out against closed lips.
Provide nursing care for the client with asthma Administer prescribed medications, which may include: Adrenergics( Adrenaline), Bronchodilators(aminophlline) Corticosteroids( Dexamethasone, Solu –cortef) for acute attack . Nebulized aerosol(Ventoline) relive bronchospasme. Oxygen therapy
Provide treatment during an acute asthmatic attack. (1) Stay with the client and keep him calm and in an upright position. (2) Do purse-lip breathing with the client; encourage relaxation techniques.
Implement measures to prevent asthmatic attacks. Teach the client the following skills: (1) Identify and eliminate or minimize exposure to pulmonary irritants. (2) Remove rugs and curtains from the home; change air filters frequently; keep the home as dust free as possible; and keep windows closed during windy and high pollen days. (3) Use an inhaler and take medications as prescribed, and notify the physician when not gaining complete relief. (4) Notify the physician when a respiratory infection occurs. (5) Obtain influenza and pneumonia vaccines at prescribed times. (6) Monitor peak expiratory flow rate.
Pleural effusion Description. Pleural effusion is a collection of fluid in the pleural space, which is located between the visceral and parietal surfaces Etiology. Pleural effusion usually results from diseases such as neoplastic tumors (of which bronchogenic cancer is the most common malignancy), congestive heart failure, tuberculosis, pneumonia, pulmonary infection, and connective tissue disease. Pathophysiology. The pleural space contains a small amount of lubricating fluid that allows the pleural surfaces to move without friction. Excess fluid accumulates in the space until it becomes clinically evident. The effusion can be composed of a clear fluid, or it can be bloody or purulent.
Clinical manifestations Large pleural effusion (1) Shortness of breath (2) Minimal or no breath sounds (3) Dull, flat sound when percussed (4) Tracheal deviation away from the affected side may occur when significant accumulation of fluid occurs. Small to moderate pleural effusion (1) Respiratory difficulty or comprised lung expansion may not be evident. (2) Dyspnea may not be present.
Laboratory and diagnostic study findings Chest radiograph shows fluid in the pleural space. Pleural f 1 uid obtained by thoracentesis and treated with an acidfast bacillus stain may reveal tuberculosis or red and white blood cells. Nursing management. Prepare the client for thoracentesis, which is performed to remove f 1 uid, obtain a specimen for analysis, and relieve dyspnea. Assist the physician with administering chemically irritating agents, which may be instilled to obliterate the pleural space and prevent further accumulation of f 1 uid. Provide pain relief. Position client to decrease pain and administer pain medication, as needed.
Pulmonary Tuberculosis Definition: Pulmonary tuberculosis (T. B) is an infectious disease that primarily affects the lung parenchyma. It also may be transmitted to the other parts of the body including the meninges, kidney, bones and lymph nodes. The primary infectious agent mycobacterium tuberculosis or tubercle bacillus is an acid –fast, aerobic rod that grows slowly and is sensitive to heat and ultraviolet light
Transmission TB spreads from person to person by airborne transmission. An infected person release droplet through talking, coughing, sneezing, laughing, or singing Risk factors for TB 1 - Close contact with an infected person. 2 - Recent positive tuberculosis test i. e. recently converted from negative to positive skin test. 3 - Large tuberculin reaction (12 mm or more in diameter). 4 - Preexisting medical condition e. g. diabetics, malignancy or chronic renal failure, hemodialysis, malnourish 5 - People living in overcrowded homes substandard living, with low, income i. e. low socioeconomic class. 6 - Immunocompromised status (e. g. HIV, cancer, transplanted organ, high dose of corticosteroids 7 - Immigration from countries with high prevalent TB
Pathophysiology A susceptible person inhales mycobacterium bacilli and become infected. The bacteria are transmitted through the airways to the alveoli, where they are deposited and begin to multiply. The bacilli also transported via the lymph system and blood stream to other areas of lung & other area of body (kidney, bone, and cortex). The body’s immune system responds initiating an inflammatory reaction. Phagocytes engulf many of the bacteria and TB specific lymphocytes destroy the bacilli and tissue. Granulomas are transformed to a fibrous tissue mass, the central portion of which is a called Ghon tubercle. The material (bacteria and macrophages) becomes necrotic, forming a cheesy mass. This mass may become calcified and form a collagenous scar.
Clinical manifestation: 1 -Low grade fever 2 -Cough may be nonproductive or mucopurulent sputum 3 -Night sweat 4 -Fatigue 5 -weight loss 6 -Hemoptysis
Assessment and diagnostic studies Sputum testing: Positive Acid fast bacilli, Positive Mycobacterium tuberculosis Chest X-ray: Active or calcified lesion Blood tests: WBCS, ESR are increased
Medical Intervention: TB is treated primarily with chemotherapeutic agent for 6 to 12 months. More than one drug of the following are used: Streptomycine Isoniazid(INH) Para amino salicylic acid Rifampin Ethambutol Pyrazinamide
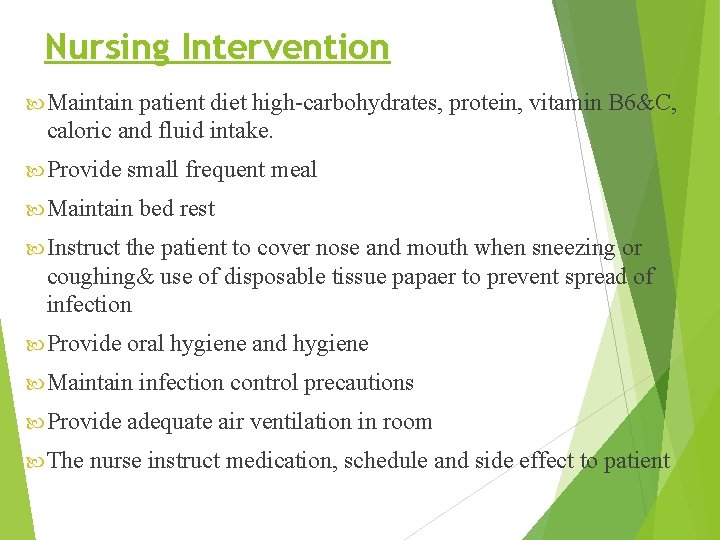
Nursing Intervention Maintain patient diet high-carbohydrates, protein, vitamin B 6&C, caloric and fluid intake. Provide small frequent meal Maintain bed rest Instruct the patient to cover nose and mouth when sneezing or coughing& use of disposable tissue papaer to prevent spread of infection Provide oral hygiene and hygiene Maintain infection control precautions Provide adequate air ventilation in room The nurse instruct medication, schedule and side effect to patient
Question?
 Type 316 stainless steel tables
Type 316 stainless steel tables Princeton cos 316
Princeton cos 316 Cs 316
Cs 316 316 loài vẹt
316 loài vẹt Ee 316
Ee 316 Ee-316
Ee-316 Ucc 2-316
Ucc 2-316 Sonst slovosled
Sonst slovosled Iswari nur hidayati
Iswari nur hidayati Struktur mikrokontroler
Struktur mikrokontroler Iim ibrahim nur
Iim ibrahim nur Astria nur irfansyah
Astria nur irfansyah Nilai dari iim
Nilai dari iim Sterne mit den goldnen füßchen
Sterne mit den goldnen füßchen Nur 102
Nur 102 Nur ahmad husin
Nur ahmad husin Dr nur mohammad hadi zahalan
Dr nur mohammad hadi zahalan Nur azid mahardinata
Nur azid mahardinata Der kabeljau gedicht
Der kabeljau gedicht Nur verrückte haben es eilig
Nur verrückte haben es eilig Nur für heute
Nur für heute Dr nur ahmad tabri
Dr nur ahmad tabri Nur alia file upload
Nur alia file upload Nur ahmad husin
Nur ahmad husin Nur ahmad husin
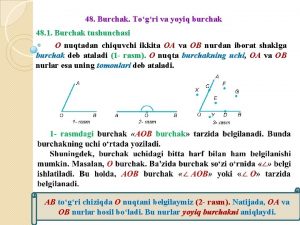
Nur ahmad husin Burchak bissektrisasi nima
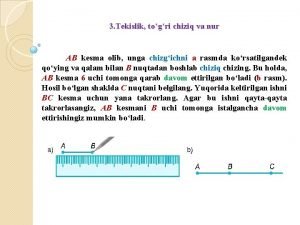
Burchak bissektrisasi nima Togri chiziq
Togri chiziq Keno bültena
Keno bültena Nur alam shah
Nur alam shah Hanif nur widhiyanti
Hanif nur widhiyanti Penyelesaian pada persamaan 16m=64 adalah
Penyelesaian pada persamaan 16m=64 adalah Danti nur indiastuti
Danti nur indiastuti Der jürgen klinsmann und ich wir sind ein gutes trio
Der jürgen klinsmann und ich wir sind ein gutes trio Meral nur ergin
Meral nur ergin Nur hidayat
Nur hidayat Mezonefrik kanal
Mezonefrik kanal Mekke'de islam davetine tepkiler slayt
Mekke'de islam davetine tepkiler slayt şadiye nur güleç
şadiye nur güleç Personal selling nike
Personal selling nike Hanif nur widhiyanti
Hanif nur widhiyanti Nur 211 final exam
Nur 211 final exam Logo nur ihsan
Logo nur ihsan Definisi kartografi
Definisi kartografi Nur endah januarti
Nur endah januarti Nur 302
Nur 302 Nur parts
Nur parts Nur 680
Nur 680 Levy olivia nur
Levy olivia nur Was dich nicht umbringt macht dich nur stärker
Was dich nicht umbringt macht dich nur stärker Aktivitas orang yang sudah meninggal
Aktivitas orang yang sudah meninggal Nur aras
Nur aras Nur masripatin
Nur masripatin Nur
Nur Makhluk sosial
Makhluk sosial Nur 102
Nur 102 Jelaskan bentuk kromosom berdasarkan letak sentromernya
Jelaskan bentuk kromosom berdasarkan letak sentromernya Dr nur rofiah
Dr nur rofiah Wir kannten nur zu gut sein unerhörtes haupt
Wir kannten nur zu gut sein unerhörtes haupt Cornua of uterus
Cornua of uterus Nur 102
Nur 102