Nursing role in cirrhosis of the liver management







- Slides: 43
Nursing role in cirrhosis of the liver management
Defination Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism. The liver carries out several necessary functions, including detoxifying harmful substances in your body, cleaning your blood and making vital nutrients.
Defination Cirrhosis isn't curable, but it’s treatable. Cirrhosis occurs in response to damage to your liver. Each time your liver is injured, it tries to repair itself. In the process, scar tissue forms. As cirrhosis progresses, more and more scar tissue forms, making it difficult for the liver to function.
Defination Decompensated cirrhosis is life-threatening. The liver damage done by cirrhosis generally can't be undone. But if liver cirrhosis is diagnosed early and the cause is treated, further damage can be limited and, rarely, reversed.
Defination What is cirrhosis of the liver? The liver is the largest solid organ in the body. It performs many important functions, including: Making blood proteins that aid in clotting, transporting oxygen, and helping the immune system Storing excess nutrients and returning some of the nutrients to the bloodstream Manufacturing bile, a substance needed to help digest food Helping the body store sugar (glucose) in the form of glycogen Ridding the body of harmful substances in the bloodstream, including drugs and alcohol Breaking down saturated fat and producing cholesterol
Morbidity Number of adults with diagnosed liver disease: 4. 9 million Percent of adults with diagnosed liver disease: 2. 0%
Mortality Number of deaths: 40, 326 Deaths per 100, 000 population: 12. 5

Causes
The most common causes are: Chronic alcohol abuse Chronic viral hepatitis (hepatitis B and C) Fat accumulating in the liver (nonalcoholic fatty liver disease)
Other possible causes include: Iron buildup in the body (hemochromatosis) Cystic fibrosis Copper accumulated in the liver (Wilson's disease) Poorly formed bile ducts (biliary atresia) Inherited disorders of sugar metabolism (galactosemia or glycogen storage disease) Genetic digestive disorder Liver disease caused by your body's immune system (autoimmune hepatitis) Destruction of the bile ducts (primary biliary cirrhosis) Medications such as methotrexate
Types of cirrhosis

Alcoholic cirrhosis Posthepatic cirrhosis İdiopatic cirrhosis Wilson’s cirrhosis Bilier cirrhosis Hemochromatosis
Symptoms of cirrhosis
The symptoms of cirrhosis depend on the stage of the illness. In the beginning stages, there may not be any symptoms. As the disease worsens, symptoms may include: Loss of appetite Lack of energy (fatigue) Weight loss or sudden weight gain Bruises Yellowing of skin or the whites of eyes (jaundice) Itchy skin Fluid retention (edema) and swelling in the ankles, legs, and abdomen A brownish or orange color to the urine Light-colored stools Confusion, disorientation, personality changes Blood in the stool Fever
Fatigue Bleeding easily Bruising easily Itchy skin Yellow discoloration in the skin and eyes (jaundice) Fluid accumulation in your abdomen (ascites) Loss of appetite Nausea Swelling in your legs Weight loss Confusion, drowsiness and slurred speech (hepatic encephalopathy) Spiderlike blood vessels on your skin Redness in the palms of the hands Testicular atrophy in men Breast enlargement in men
Risk factors Drinking too much alcohol is a risk factor for cirrhosis. For healthy adults, that means no more than one drink a day for women of all ages and men over age 65, and up to two drinks a day for men under 65. Being overweight or obese also increases the risk of cirrhosis. Sharing needles and having unprotected sex can increase your risk of hepatitis B and C, which can lead to cirrhosis.
Diagnosis of cirrhosis
People with early-stage cirrhosis of the liver usually don't have symptoms.
Laboratory tests: Liver function. Your blood is checked for excess bilirubin, which is a product of red blood cells breaking down, as well as for certain enzymes that may indicate liver damage. Kidney function. Your blood is checked for creatinine as kidney function may decline in later stages of cirrhosis (decompensated cirrhosis). Tests for hepatitis B and C. Your blood is checked for the hepatitis viruses. Clotting. Your international normalized ratio (INR) is checked for your blood's ability to clot.
The other tests: Magnetic resonance elastography or transient elastography. Other imaging tests. MRI, CT and ultrasound create images of the liver. Biopsy
If you have cirrhosis, your doctor is likely to recommend regular diagnostic tests to monitor for signs of disease progression or complications, especially esophageal varices and liver cancer.
Stages of cirrhosis
Cirrhosis in itself is already a late stage of liver damage. In the early stages of liver disease there will be inflammation of the liver. If this inflammation is not treated it can lead to scarring (fibrosis). At this stage it is still possible for the liver to heal with treatment.
If fibrosis of the liver is not treated, it can result in cirrhosis. At this stage, the scar tissue cannot heal, but the progression of the scarring may be prevented or slowed. People with cirrhosis who have signs of complications may develop end-stage liver disease (ESLD) and the only treatment at this stage is liver transplantation.
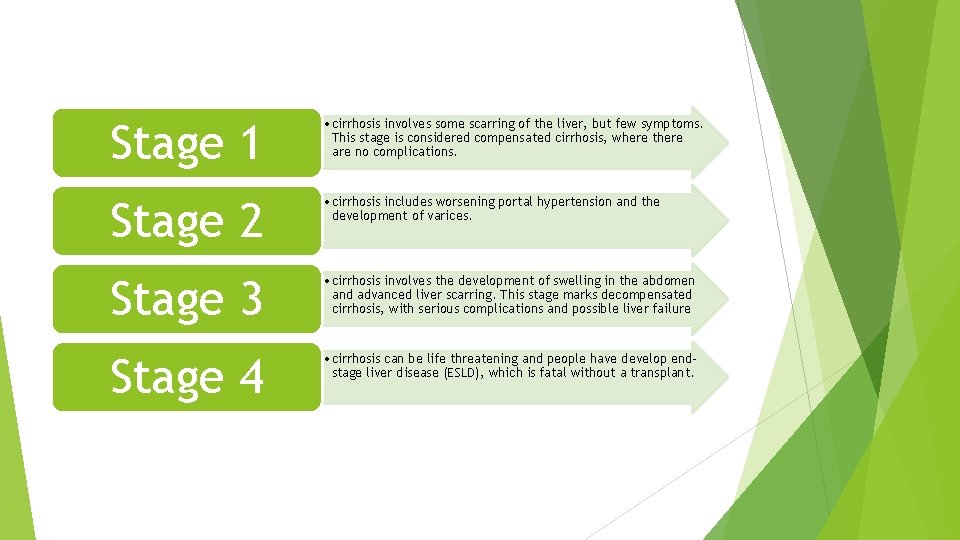
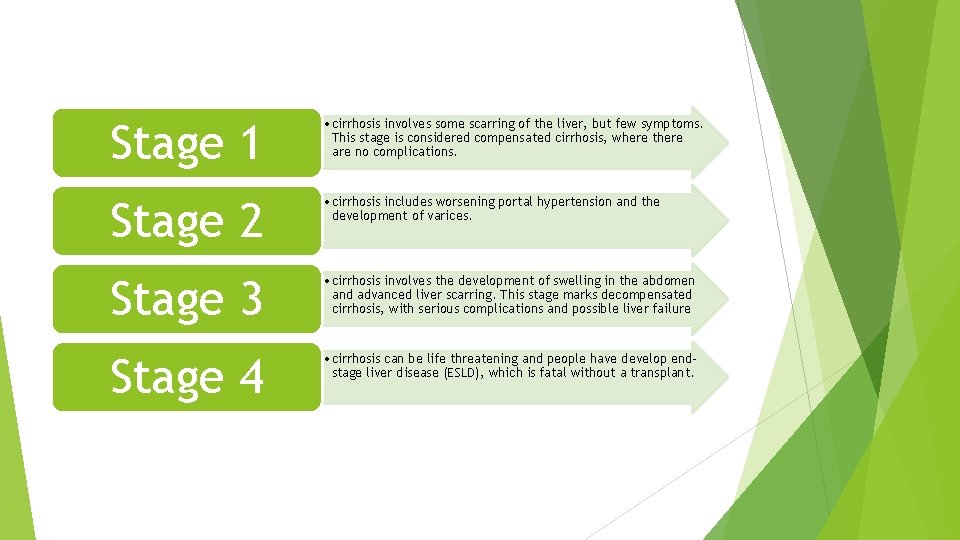
Stage 1 • cirrhosis involves some scarring of the liver, but few symptoms. This stage is considered compensated cirrhosis, where there are no complications. Stage 2 • cirrhosis includes worsening portal hypertension and the development of varices. Stage 3 • cirrhosis involves the development of swelling in the abdomen and advanced liver scarring. This stage marks decompensated cirrhosis, with serious complications and possible liver failure Stage 4 • cirrhosis can be life threatening and people have develop endstage liver disease (ESLD), which is fatal without a transplant.
Treatment of cirrhosis
Two main goals in treating this disease: Stop the damage to your liver Prevent complications
Treatment for cirrhosis depends on the cause and extent of your liver damage. The goals of treatment are to slow the progression of scar tissue in the liver and to prevent or treat symptoms and complications of cirrhosis. You may need to be hospitalized if you have severe liver damage.
Treatment for the underlying cause of cirrhosis
In early cirrhosis, it may be possible to minimize damage to the liver by treating the underlying cause. Treatment for alcohol dependency Weight loss Medications to control hepatitis Medications to control other causes and symptoms of cirrhosi.
Other medications can relieve certain symptoms, such as itching, fatigue and pain. Nutritional supplements may be prescribed to counter malnutrition associated with cirrhosis and to prevent weak bones (osteoporosis).

Treatment for complications of cirrhosis
Excess fluid in your body Portal hypertension Infections Increased liver cancer risk Hepatic encephalopathy

Liver transplantation Potential future treatments

Lifestyle and home remedies
Don't drink alcohol Eat a low-sodium diet Eat a healthy diet Avoid infections Use over-the-counter medications carefully
COMPLICATIONS Portal hypertension Esophagus or Stomach Varices Liver cancer Hepatic encephalopathy Fluid buildup

Nursing care plan

Imbalanced Nutrition: Less Than Body Requirements Excess Fluid Volume Risk for Impaired Skin Integrity Ineffective Breathing Pattern Risk for Injury Risk for Acute Confusion Disturbed Body Image Deficient Knowledge Other Possible Nursing Care Plans
Imbalanced Nutrition: Less Than Body Requirements Measure dietary intake by calorie count. Weigh as indicated. Compare changes in fluid status, recent weight history, skinfold measurements. Encourage patient to eat; explain reasons for the types of diet. Encourage patient to eat all meals including supplementary feedings. Restrict intake of caffeine, gas-producing or spicy and excessively hot or cold foods Encourage frequent mouth care, especially before meals. Monitor laboratory studies: serum glucose, prealbumin and albumin, total protein.
Excess Fluid Volume Monitor BP (and CVP if available). Note JVD and abdominal vein distension. Assess respiratory status, noting increased respiratory rate, dyspnea. Auscultate lungs, noting diminished breath sounds and developing adventitious sounds. Monitor for cardiac dysrhythmias. Auscultate heart sounds, noting development of S 3/S 4 gallop rhythm. Assess degree of peripheral edema. Measure abdominal girth. Encourage bedrest when ascites is present. Monitor serum albumin and electrolytes (particularly potassium and sodium).
Risk for Impaired Skin Integrity Inspect pressure points and skin surfaces closely and routinely. Encourage and assist patient with reposition on a regular schedule. Assist with active and passive ROM exercises as appropriate. Recommend elevating lower extremities. Keep linens dry and free of wrinkles. Provide perineal care following urination and bowel movement. Use alternating pressure mattress, egg-crate mattress, waterbed, sheepskins, as indicated.
Ineffective Breathing Pattern Monitor respiratory rate, depth, and effort. Auscultate breath sounds, noting crackles, wheezes, rhonchi. Investigate changes in level of consciousness. Keep head of bed elevated. Position on sides. Encourage frequent repositioning and deep-breathing exercises and coughing exercises. Monitor temperature. Note presence of chills, increased coughing, changes in color and character of sputum.