Nursing Assessment Management Hematologic System 1 Structures and

- Slides: 50
Nursing Assessment & Management: Hematologic System 1
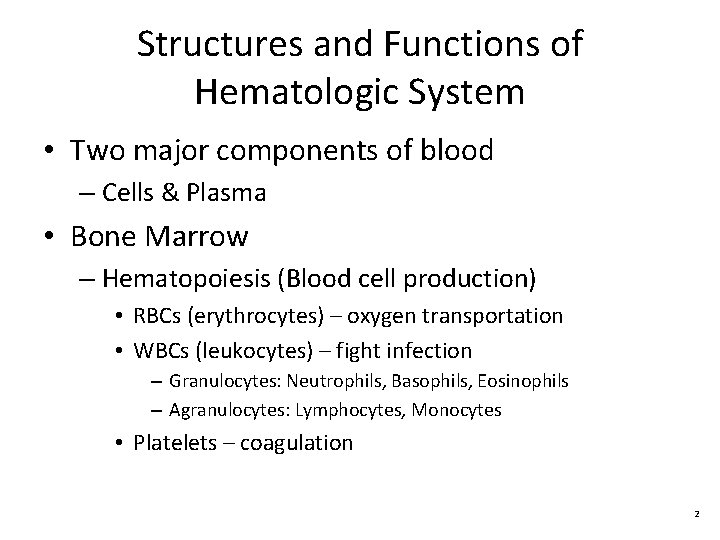
Structures and Functions of Hematologic System • Two major components of blood – Cells & Plasma • Bone Marrow – Hematopoiesis (Blood cell production) • RBCs (erythrocytes) – oxygen transportation • WBCs (leukocytes) – fight infection – Granulocytes: Neutrophils, Basophils, Eosinophils – Agranulocytes: Lymphocytes, Monocytes • Platelets – coagulation 2
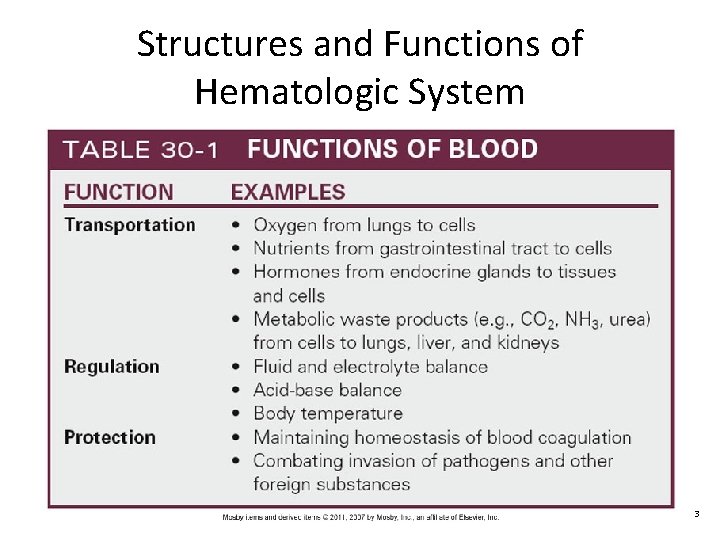
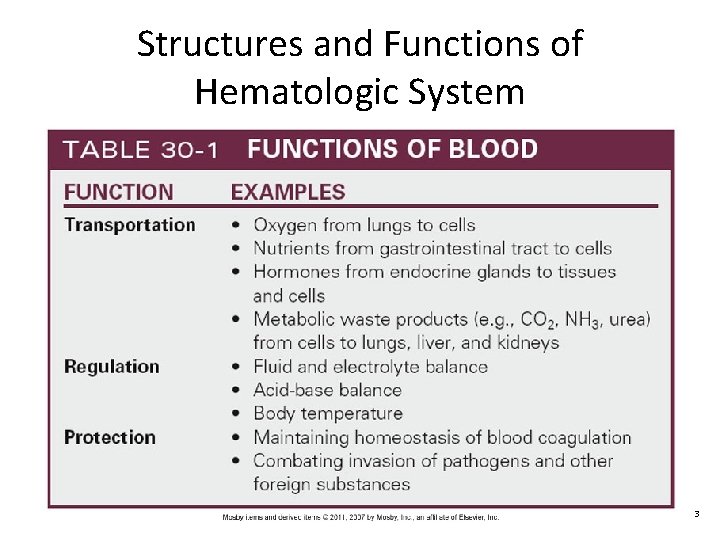
Structures and Functions of Hematologic System 3
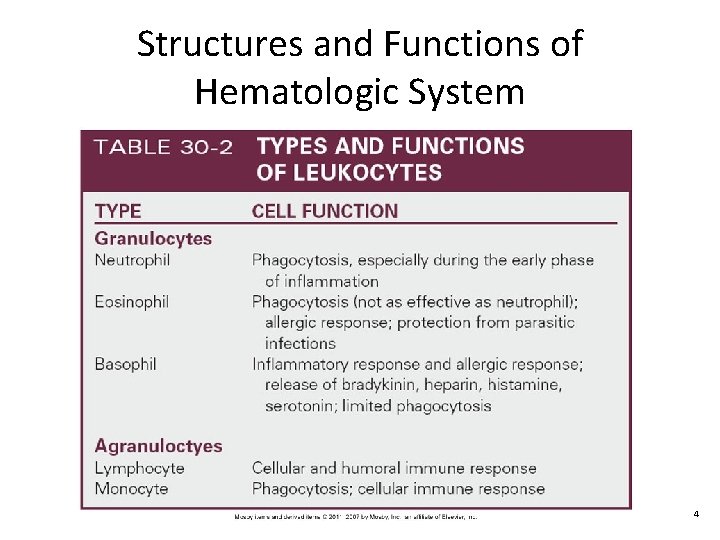
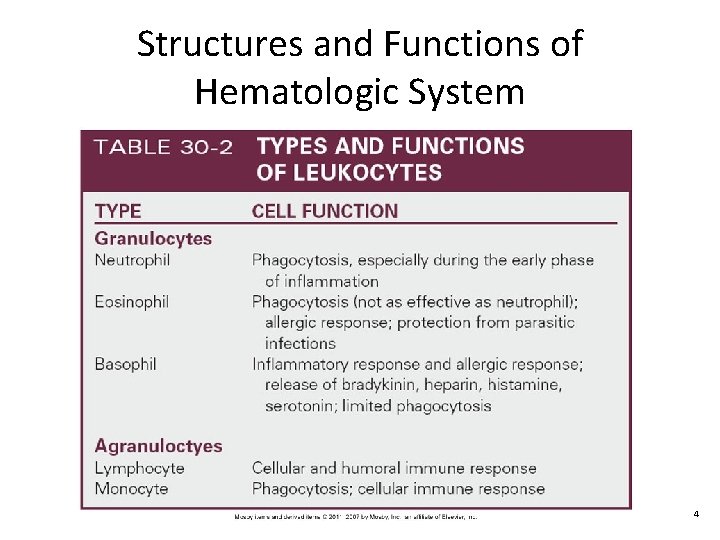
Structures and Functions of Hematologic System 4
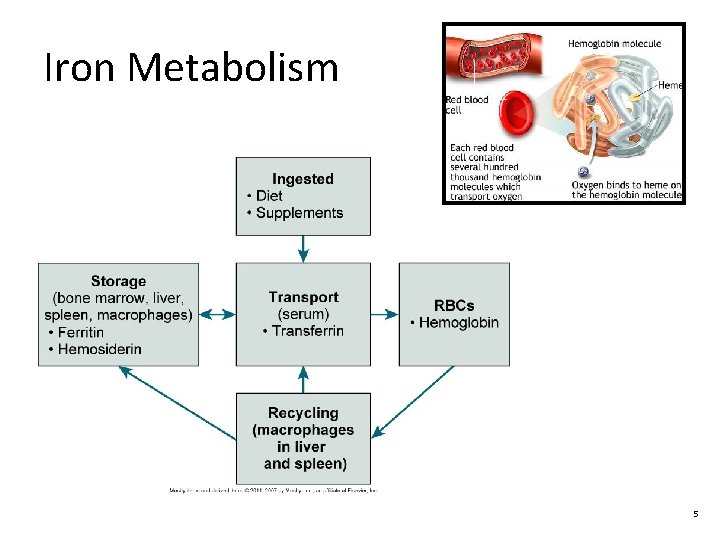
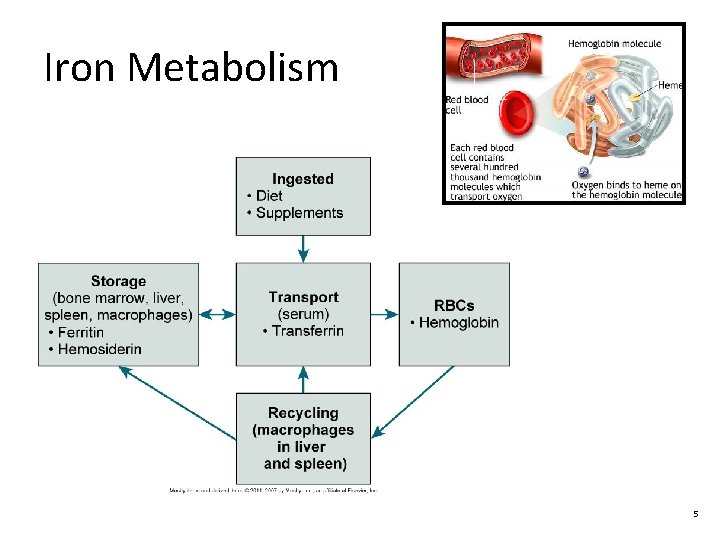
Iron Metabolism 5
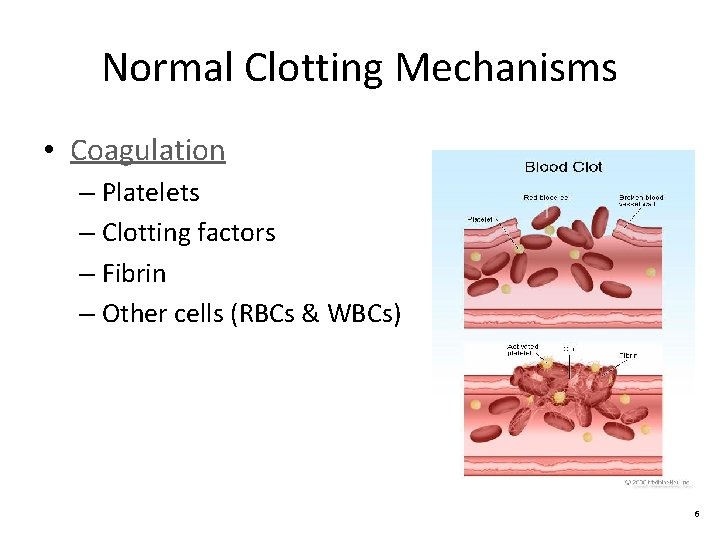
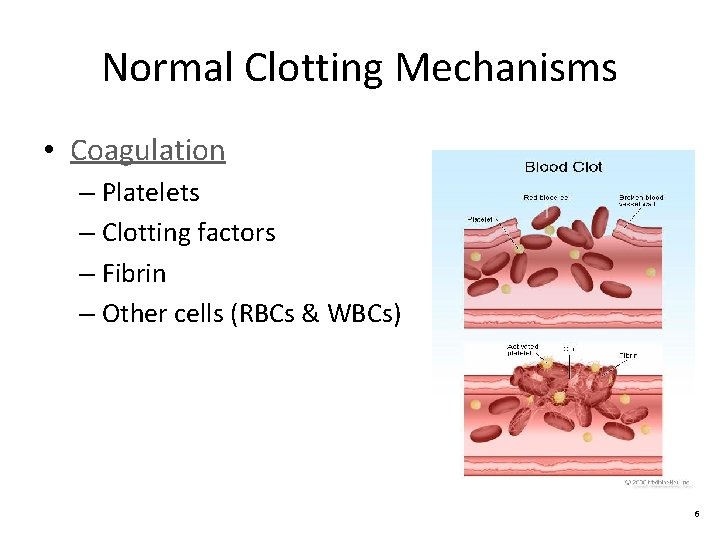
Normal Clotting Mechanisms • Coagulation – Platelets – Clotting factors – Fibrin – Other cells (RBCs & WBCs) 6
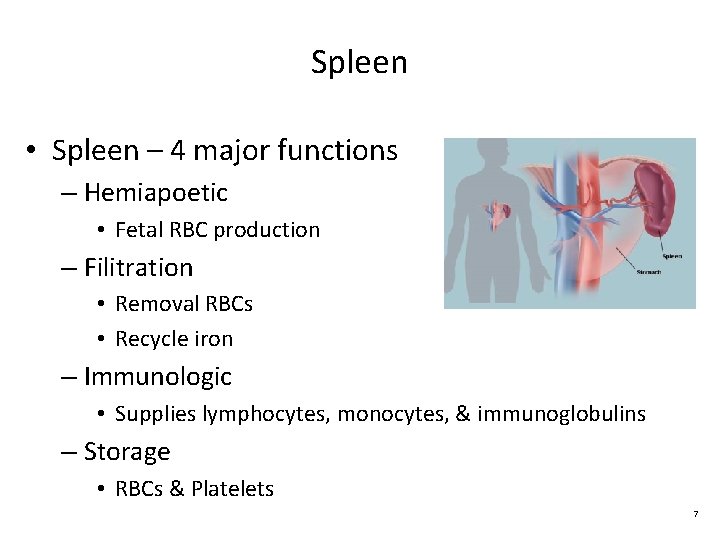
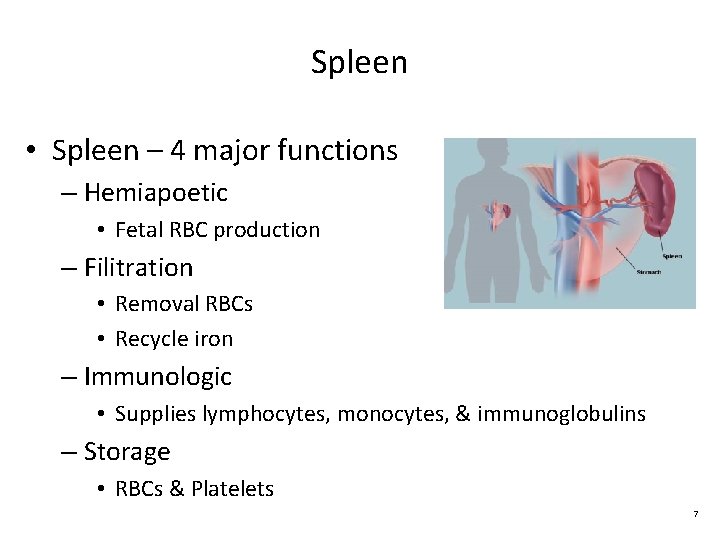
Spleen • Spleen – 4 major functions – Hemiapoetic • Fetal RBC production – Filitration • Removal RBCs • Recycle iron – Immunologic • Supplies lymphocytes, monocytes, & immunoglobulins – Storage • RBCs & Platelets 7
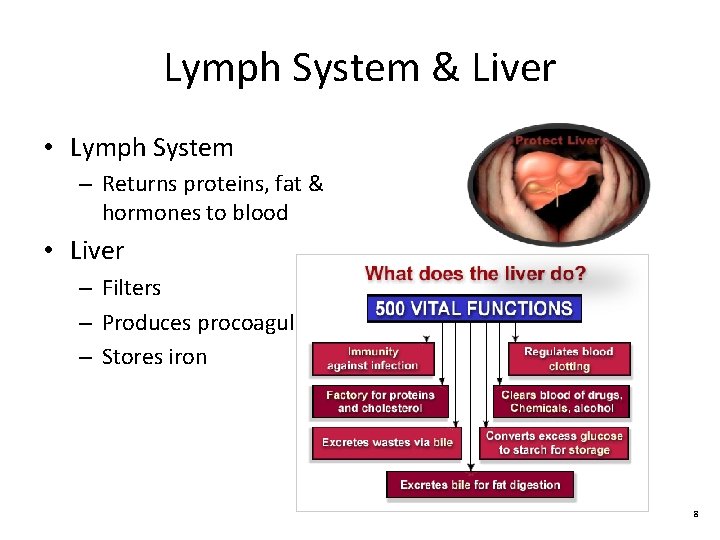
Lymph System & Liver • Lymph System – Returns proteins, fat & hormones to blood • Liver – Filters – Produces procoagulants – Stores iron 8
Gerontologic Considerations: Effects of Aging on Hematologic System • ↓Red marrow & stem cells • ↓Hemoglobin (especially in men) • ↓Nutritional intake of iron • Table 30 -4, p. 648: Differences in lab values 9
Assessment of Hematologic System • Subjective Data – Important health information • Past health history • Medications (Table 30 -5, p. 649) • Surgery or other treatments 10
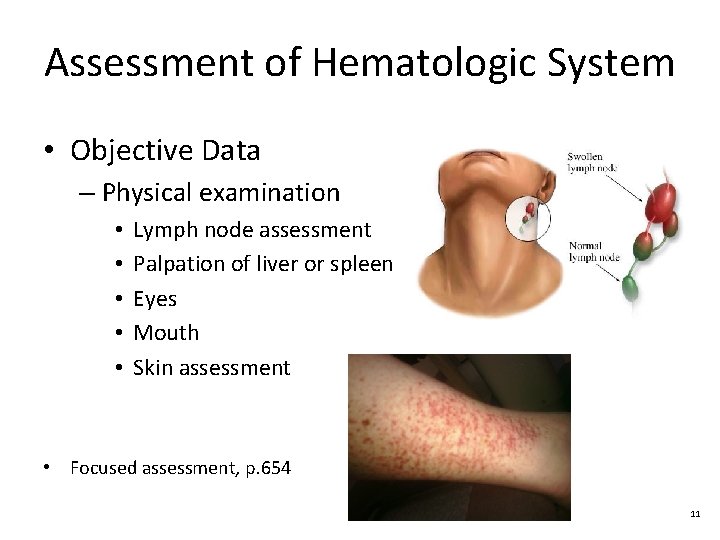
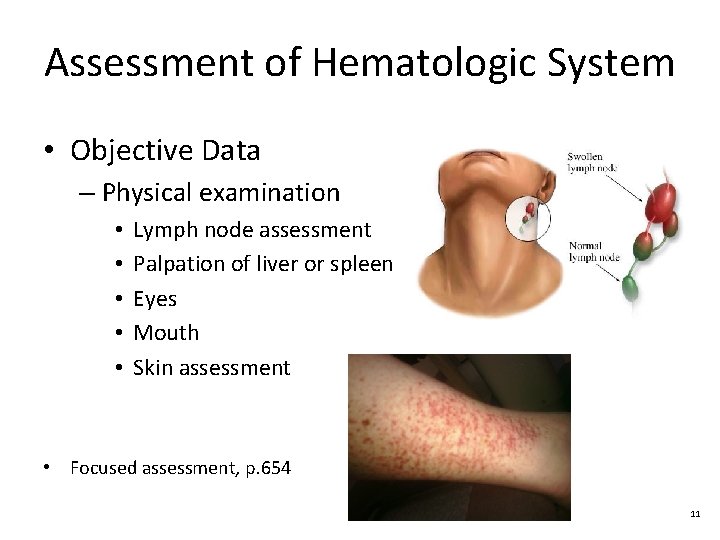
Assessment of Hematologic System • Objective Data – Physical examination • • • Lymph node assessment Palpation of liver or spleen Eyes Mouth Skin assessment • Focused assessment, p. 654 11
Diagnostic Studies • Laboratory Studies – Complete blood count (Table 30 -8, p. 655) – Blood Typing and Rh Factor – Clotting studies (Table 30 -9, p. 656) – Iron metabolism 12
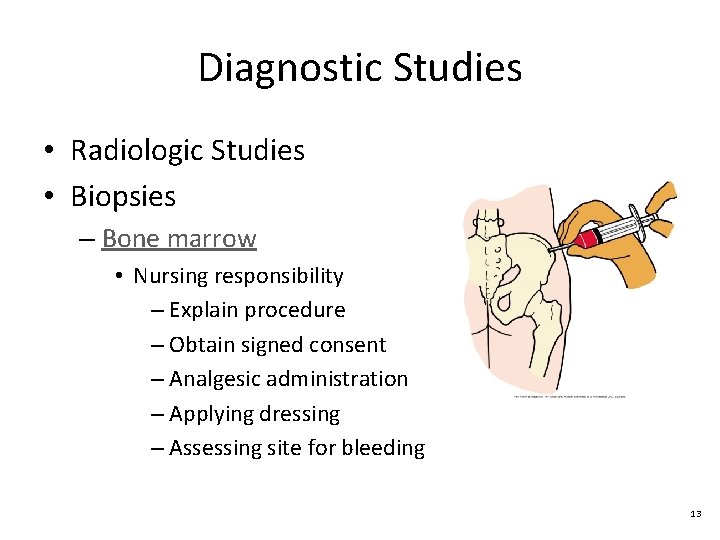
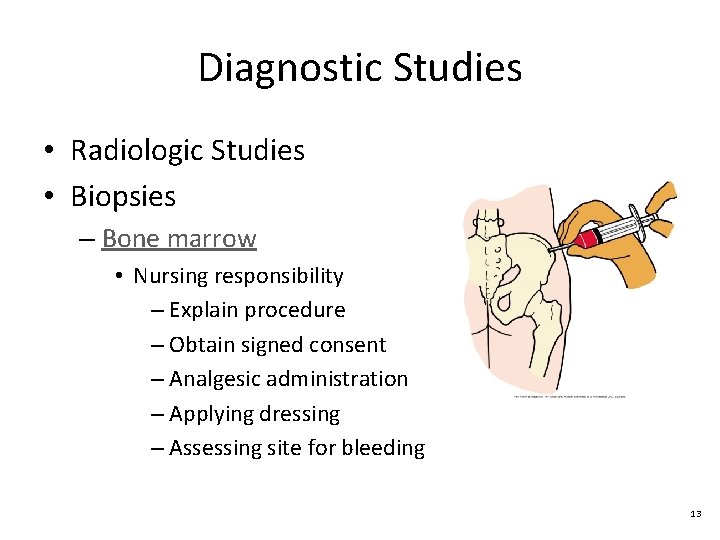
Diagnostic Studies • Radiologic Studies • Biopsies – Bone marrow • Nursing responsibility – Explain procedure – Obtain signed consent – Analgesic administration – Applying dressing – Assessing site for bleeding 13
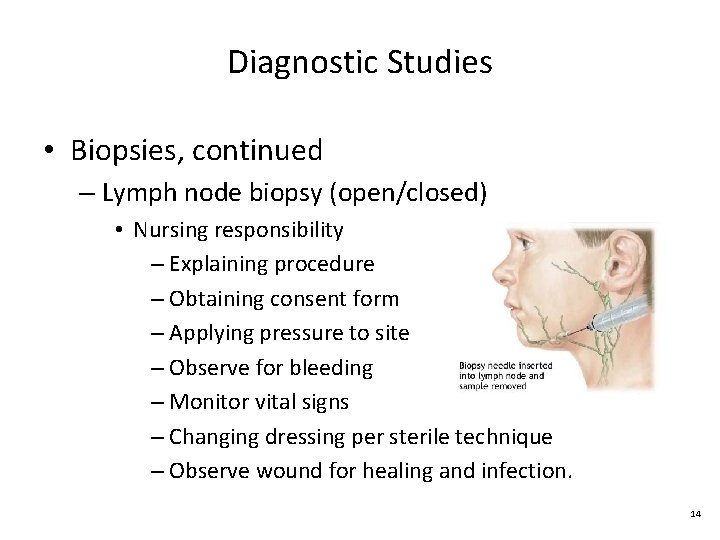
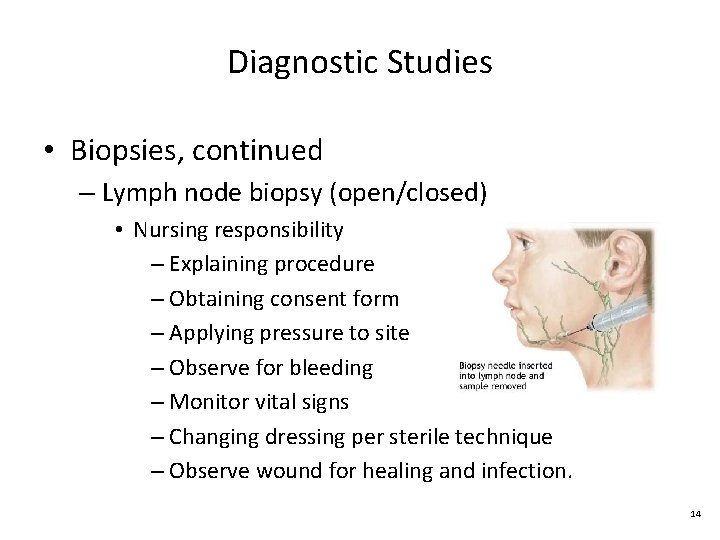
Diagnostic Studies • Biopsies, continued – Lymph node biopsy (open/closed) • Nursing responsibility – Explaining procedure – Obtaining consent form – Applying pressure to site – Observe for bleeding – Monitor vital signs – Changing dressing per sterile technique – Observe wound for healing and infection. 14
Hematologic Health Problems Anemia Copyright © 2011, 2007 by Mosby, Inc. , an affiliate of Elsevier Inc. 15
Anemia • What causes anemia? – More than 400 types divided into 3 groups • Caused by blood loss • Caused by decreased or faulty RBC production • Caused by destruction of RBCs • Treatment based on cause 16
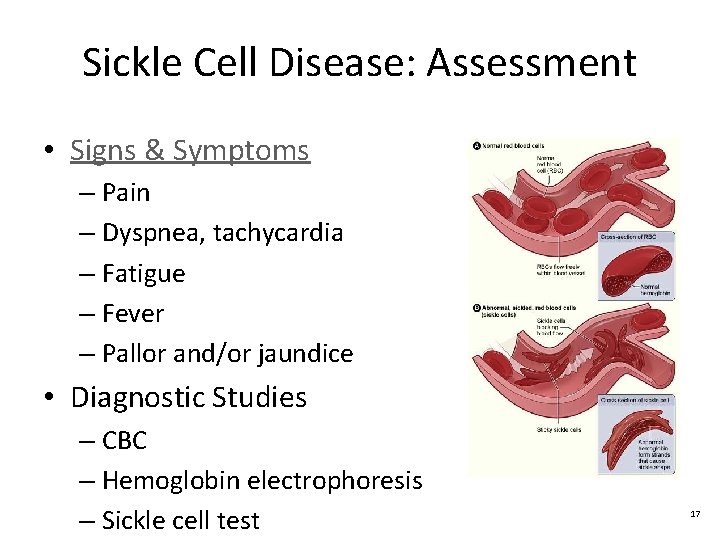
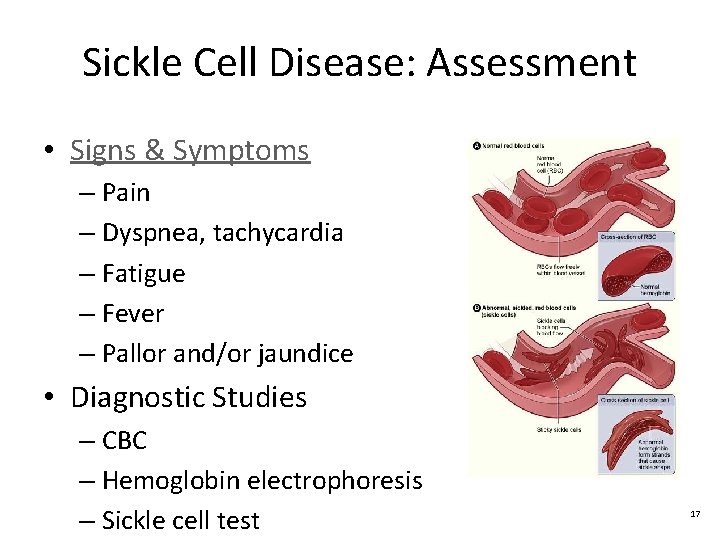
Sickle Cell Disease: Assessment • Signs & Symptoms – Pain – Dyspnea, tachycardia – Fatigue – Fever – Pallor and/or jaundice • Diagnostic Studies – CBC – Hemoglobin electrophoresis – Sickle cell test 17
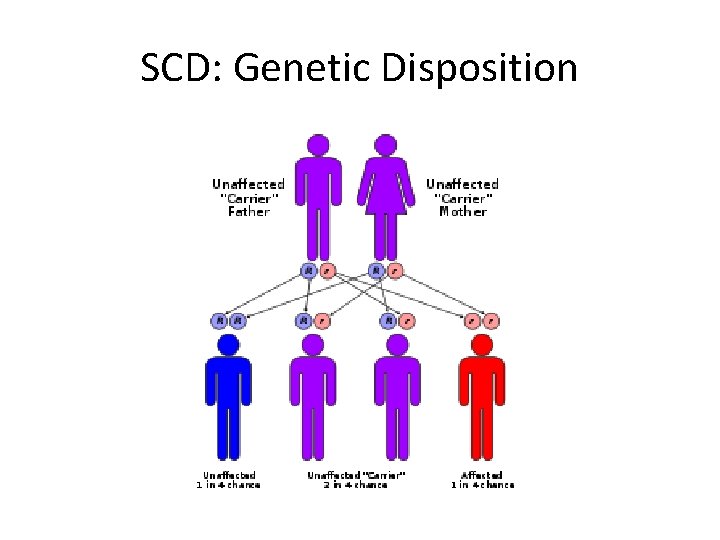
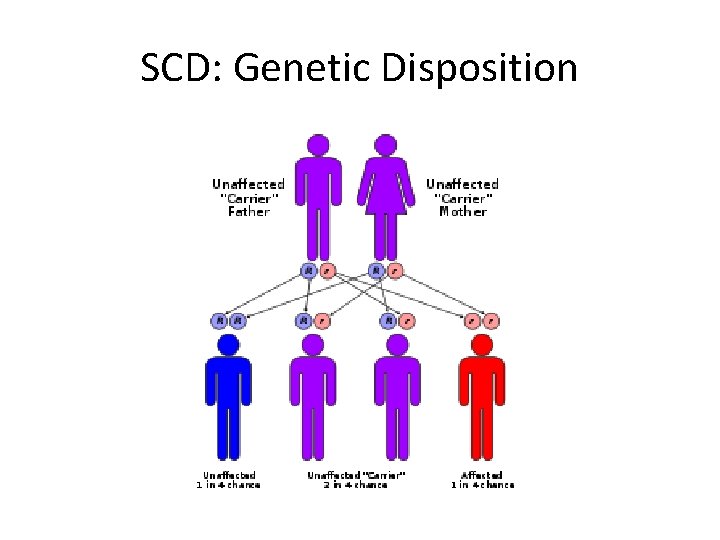
SCD: Genetic Disposition
Nursing & Collaborative Management: Sickle Cell Disease • • Alleviating symptoms Minimizing end organ damage Treating serious complications Teaching – Avoid high altitudes – Maintain adequate fluid intake • Administer immunizations • CLASS ACTIVITY: CASE STUDY 19
Asessment: Polycythemia • S&S r/t hypervolemia and hyperviscosity – Headache, dizziness, tinnitus, vision problems – Hypertension, dyspnea, angina, fatigue – Pruritis, erythema of face, hands, and feet – Petechiae, ecchymoses, excessive bleeding – Symptoms of thrombophlebitis • Diagnostic tests – Bone marrow biopsy – CBC w/ differential – Erythropoietin level 20
Nursing & Collaborative Management: Polycythemia • GOAL: Reduce thickness of blood & prevent bleeding and clotting • Phlebotomy • Myelosuppresives (ex: Hydroxyurea) • Low-dose aspirin • Hydration • Evaluate I&O • Protect from injury 21
Thrombocytopenia • Any disorder causing abnormally low platelet count less than 150, 000/μL • Types – Immune thrombocytopenia purpura – Thrombotic thrombocytopenia purpura – Heparin-induced thrombocytopenia purpura • Diagnostic tests • CBC w/ platelet count less than 150, 000/μL • Bleeding time prolonged • Bone marrow aspiration 22
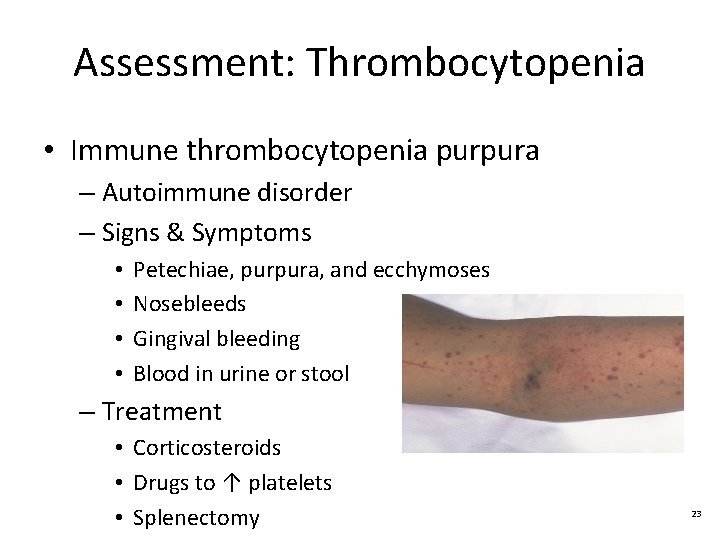
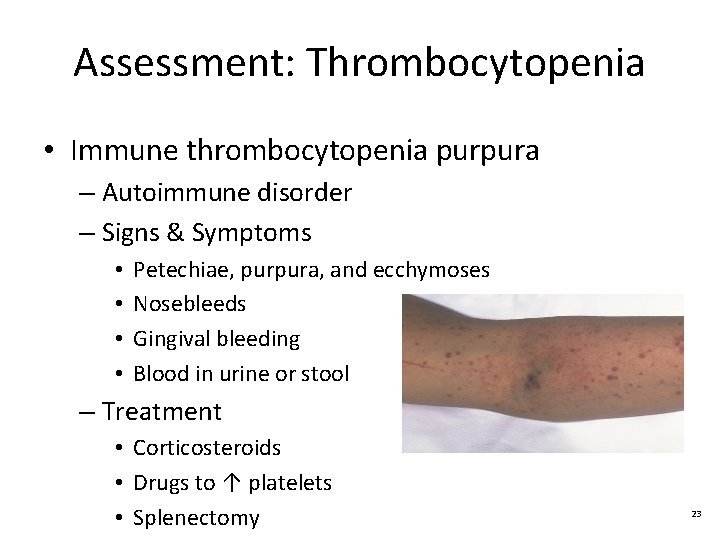
Assessment: Thrombocytopenia • Immune thrombocytopenia purpura – Autoimmune disorder – Signs & Symptoms • • Petechiae, purpura, and ecchymoses Nosebleeds Gingival bleeding Blood in urine or stool – Treatment • Corticosteroids • Drugs to ↑ platelets • Splenectomy 23
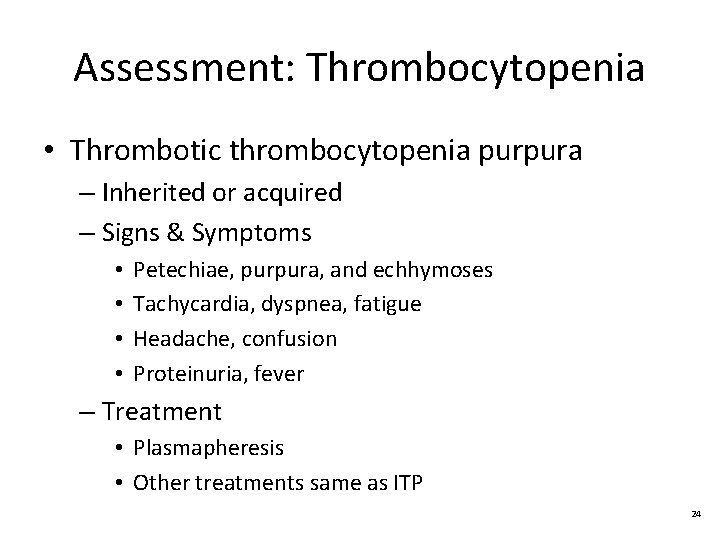
Assessment: Thrombocytopenia • Thrombotic thrombocytopenia purpura – Inherited or acquired – Signs & Symptoms • • Petechiae, purpura, and echhymoses Tachycardia, dyspnea, fatigue Headache, confusion Proteinuria, fever – Treatment • Plasmapheresis • Other treatments same as ITP 24
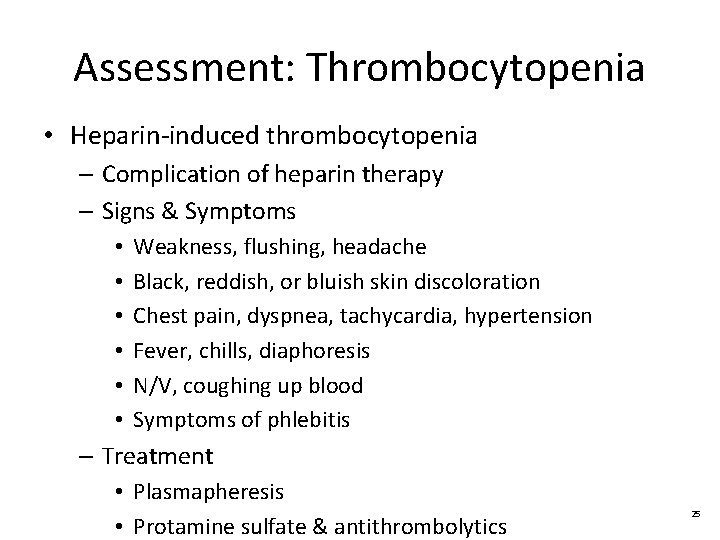
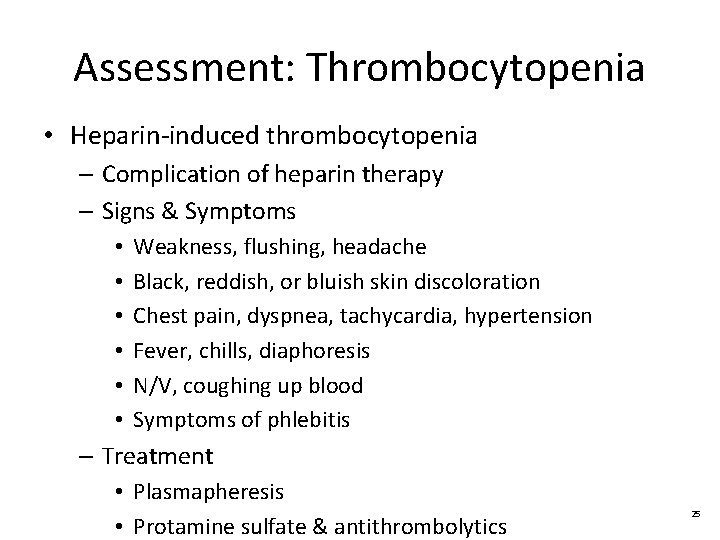
Assessment: Thrombocytopenia • Heparin-induced thrombocytopenia – Complication of heparin therapy – Signs & Symptoms • • • Weakness, flushing, headache Black, reddish, or bluish skin discoloration Chest pain, dyspnea, tachycardia, hypertension Fever, chills, diaphoresis N/V, coughing up blood Symptoms of phlebitis – Treatment • Plasmapheresis • Protamine sulfate & antithrombolytics 25
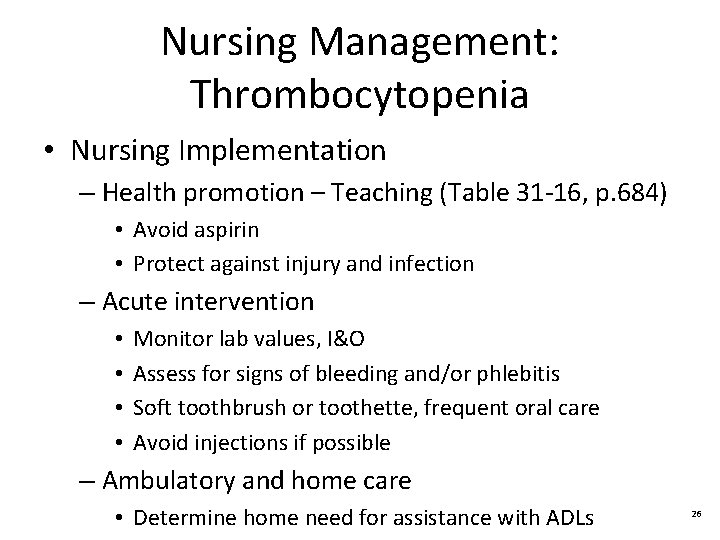
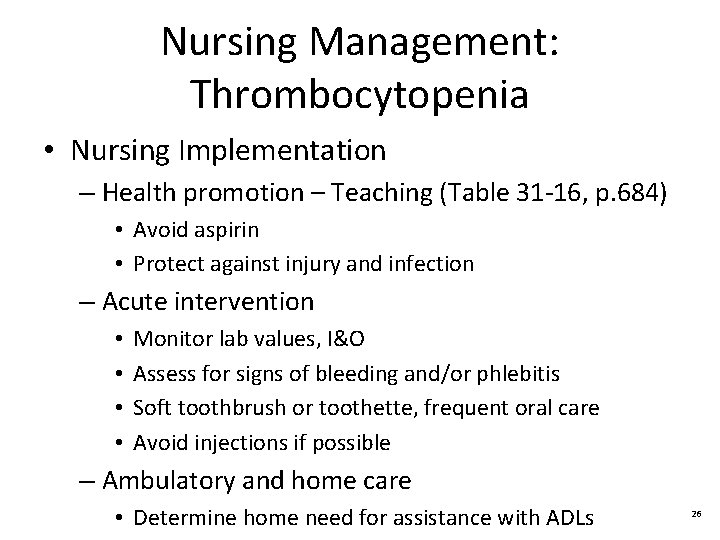
Nursing Management: Thrombocytopenia • Nursing Implementation – Health promotion – Teaching (Table 31 -16, p. 684) • Avoid aspirin • Protect against injury and infection – Acute intervention • • Monitor lab values, I&O Assess for signs of bleeding and/or phlebitis Soft toothbrush or toothette, frequent oral care Avoid injections if possible – Ambulatory and home care • Determine home need for assistance with ADLs 26
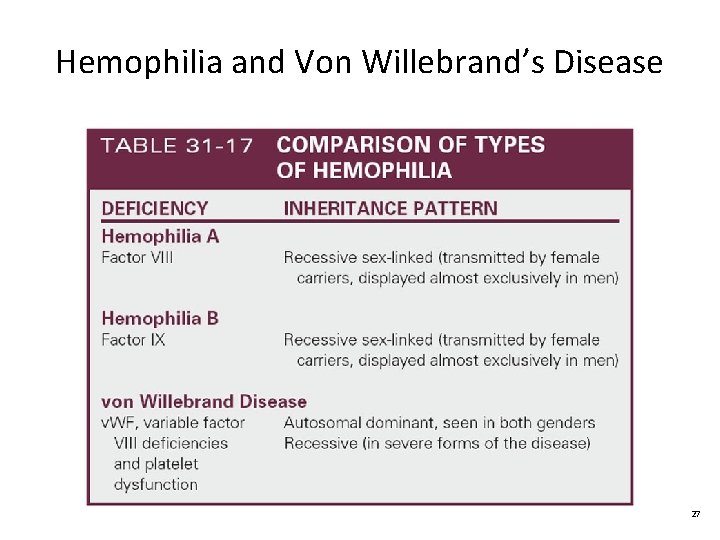
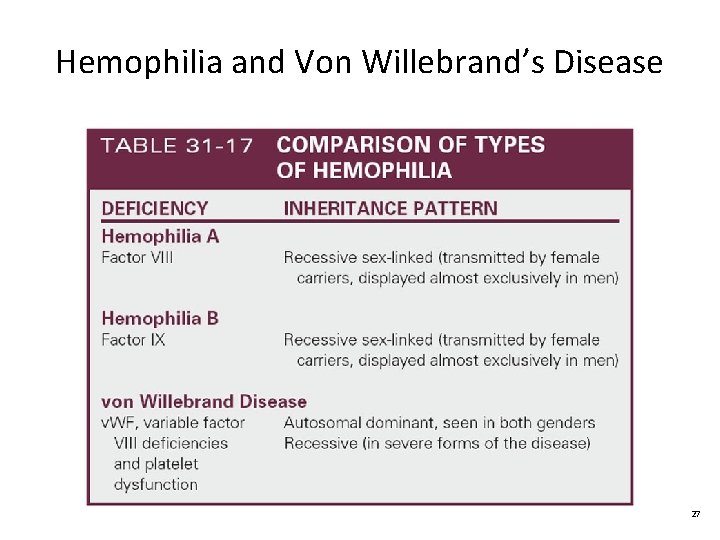
Hemophilia and Von Willebrand’s Disease 27
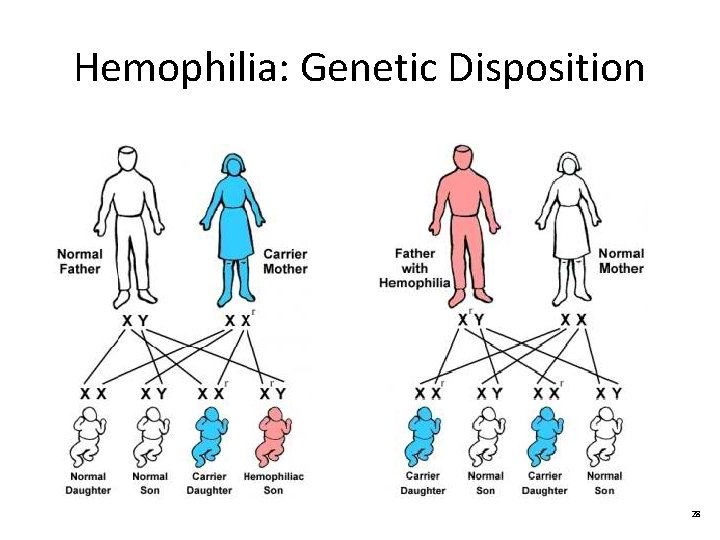
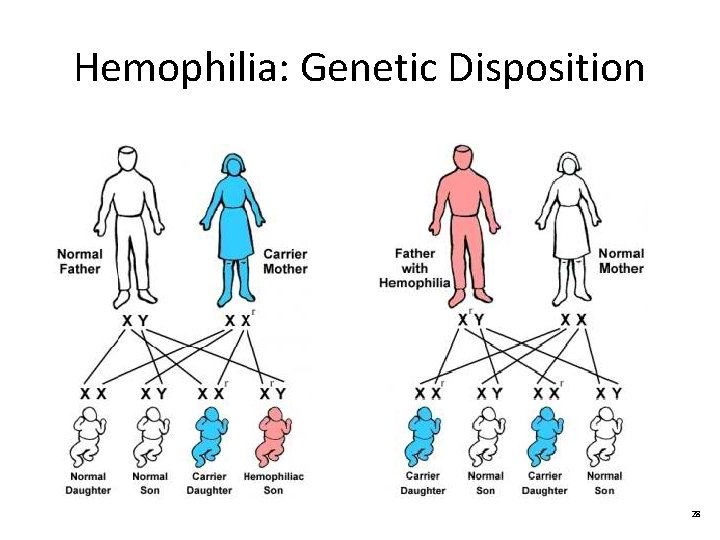
Hemophilia: Genetic Disposition 28
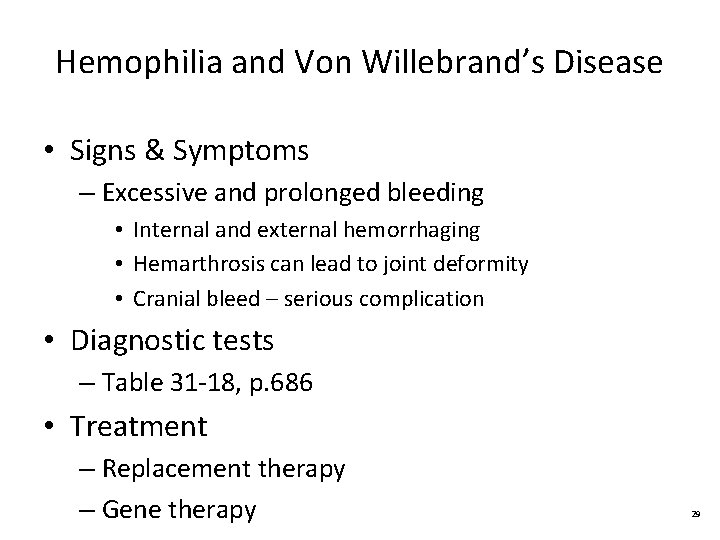
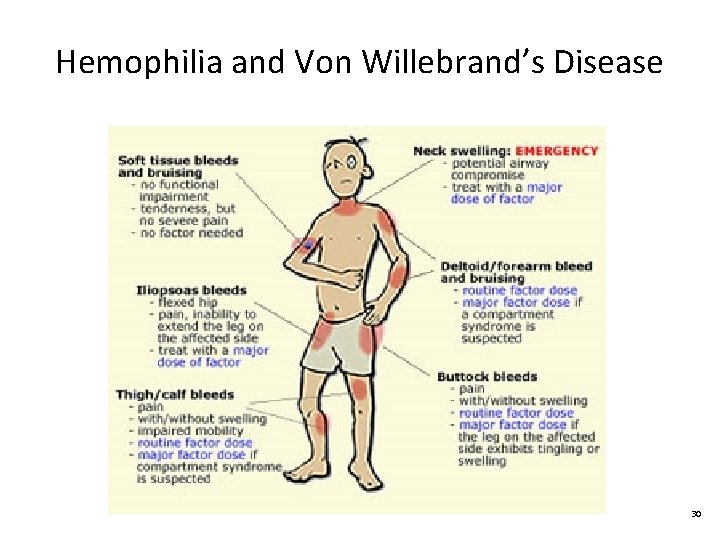
Hemophilia and Von Willebrand’s Disease • Signs & Symptoms – Excessive and prolonged bleeding • Internal and external hemorrhaging • Hemarthrosis can lead to joint deformity • Cranial bleed – serious complication • Diagnostic tests – Table 31 -18, p. 686 • Treatment – Replacement therapy – Gene therapy 29
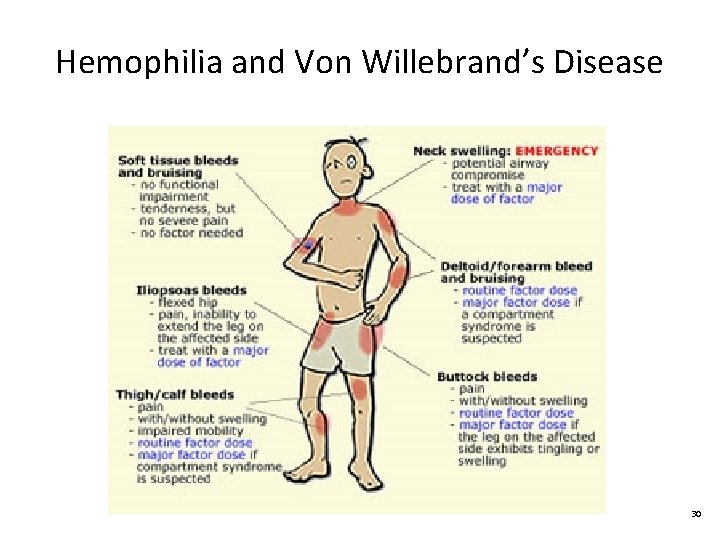
Hemophilia and Von Willebrand’s Disease 30
Nursing Management: Hemophilia • Nursing Implementation – Health promotion • Protect against injury – Acute intervention • • • Control bleeding and administer factor as ordered Bedrest and ice pack if joint bleeding Analgesics as ordered (NO ASPIRIN) Mobilize and ROM exercises when bleeding controlled Monitor for complications and side effects of factor – Ambulatory and home care • Teach S&S and when to notify physician 31
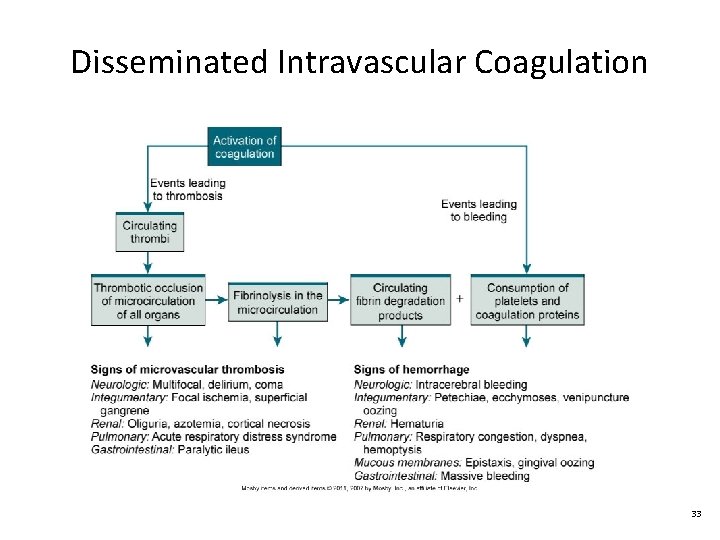
Disseminated Intravascular Coagulation • Signs & Symptoms – Unexpected bleeding (may be multiple sites) – Blood clots – Weakness, malaise, and fever – Hypotension • Diagnostic tests – Table 31 -21, p. 688 32
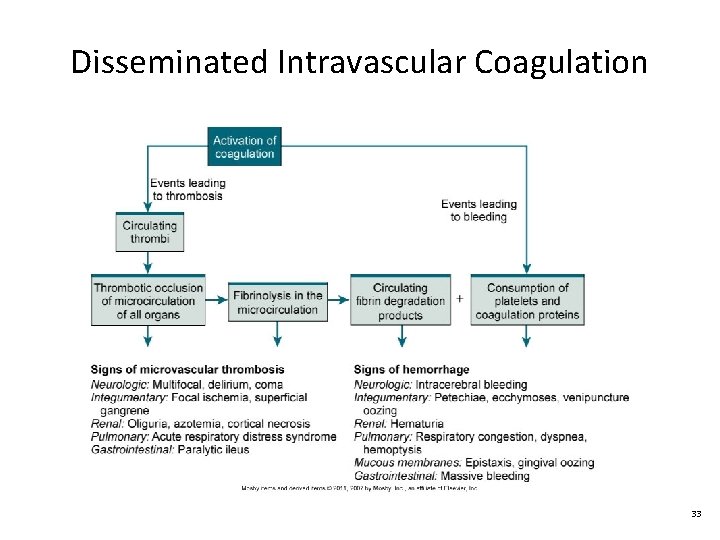
Disseminated Intravascular Coagulation 33

Disseminated Intravascular Coagulation 34
Nursing and Collaborative Management: DIC • Collaborative Care – GOAL: Determine and treat cause – Stabilize patient: O 2 & volume replacement – FFP, platelets, and cryoprecipitate – Heparin therapy • Nursing Implementation – Assess for signs of external & internal bleeding – Assess for organ damage (ex: ↓ renal output) – Administer blood products and medications as ordered 35
Neutropenia • Signs & Symptoms – Fever and signs of infection • Sore throat, dysphagia, oral lesions • Diarrhea, rectal tenderness, vaginal itching/discharge • SOB, nonproductive cough • Diagnostic Studies – CBC w/ differential • Neutrophil count 500 – 1000 cells/μL (moderate risk) • Neutrophil count less than 500 cells/μL (high risk) – Bone marrow 36
Nursing and Collaborative Management: Neutropenia • • • HANDWASHING!!! Identify and treat cause (if possible) Assess for S&S of infection Antibiotic therapy Reverse isolation Frequent oral care Screen visitors No raw veggies/fruits No flowers 37
Leukemia • Signs & Symptoms (most common) – Fever and night sweats – Headaches – Bruising or bleeding easily – Bone or joint pain – Enlarged spleen and/or liver – Swollen lymph nodes – Frequent infections – Fatigue and weakness – Weight loss and anorexia 38
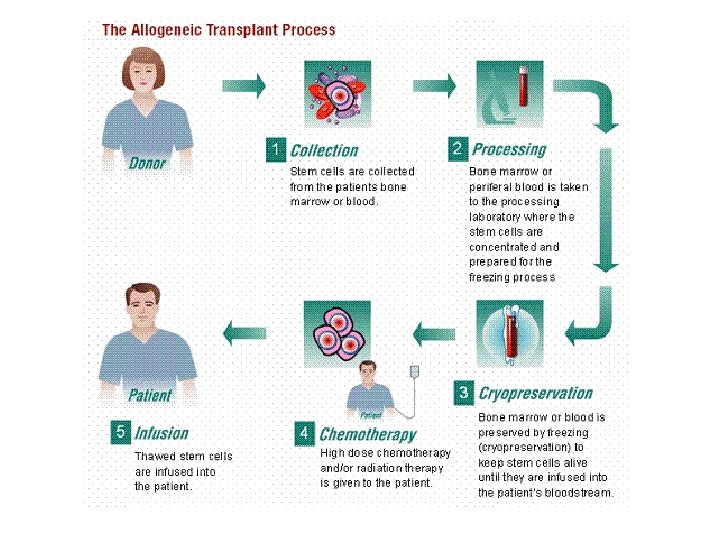
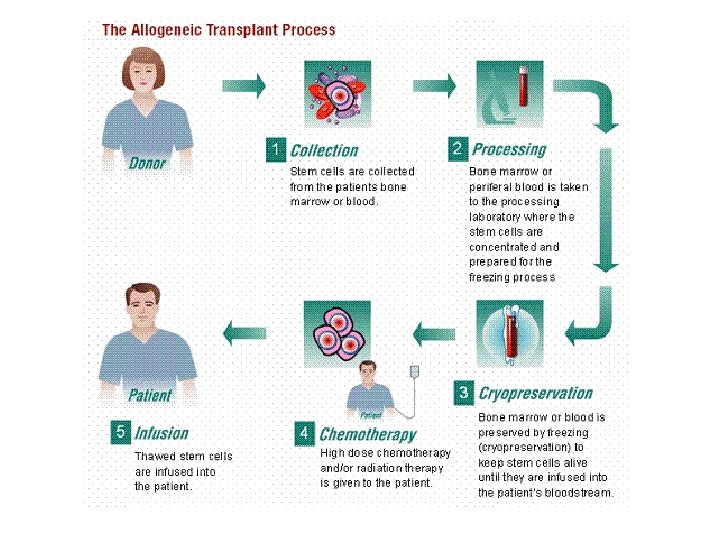
Leukemia • Diagnostic Studies – CBC w/ differential • ↑ WBCs / ↓ other blood cells – Bone marrow aspiration & biopsy – Cytology studies • Collaborative Care (Table 31 -26, p. 697) – Chemotherapy – Radiation therapy – Corticosteroids – Biologic therapy – Hematopoietic stem cell transplantation 39
Nursing Management: Leukemia • Nursing Assessment (Table 31 -27, p. 698) • Nursing Implementation – Psychosocial support measures – Manage side effects of chemo – Protect from infection – Provide frequent rest periods – Encourage nutritional intak – Provide frequent oral care – Assess for CNS changes – Encourage vaccinations 41
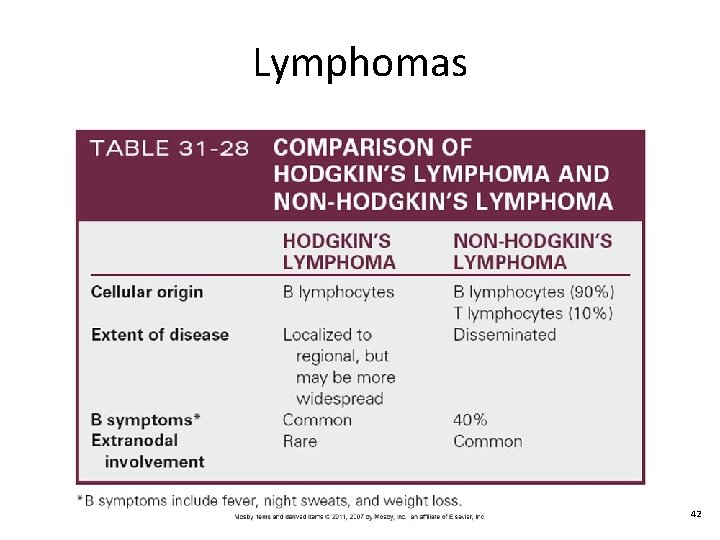
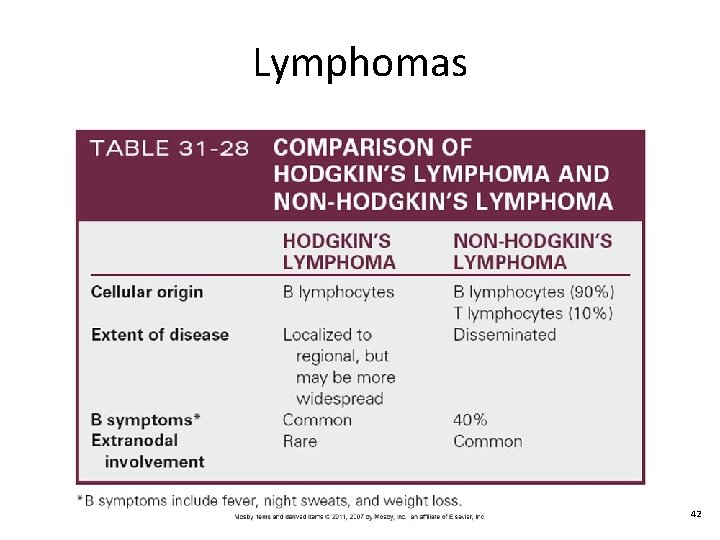
Lymphomas 42
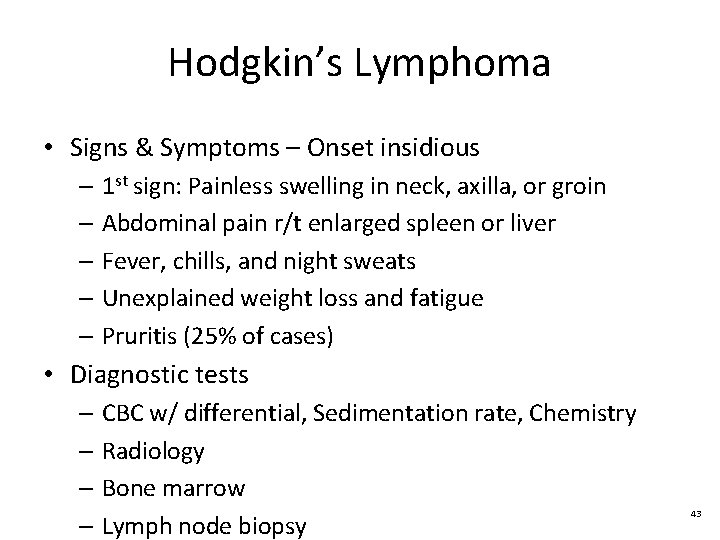
Hodgkin’s Lymphoma • Signs & Symptoms – Onset insidious – 1 st sign: Painless swelling in neck, axilla, or groin – Abdominal pain r/t enlarged spleen or liver – Fever, chills, and night sweats – Unexplained weight loss and fatigue – Pruritis (25% of cases) • Diagnostic tests – CBC w/ differential, Sedimentation rate, Chemistry – Radiology – Bone marrow – Lymph node biopsy 43
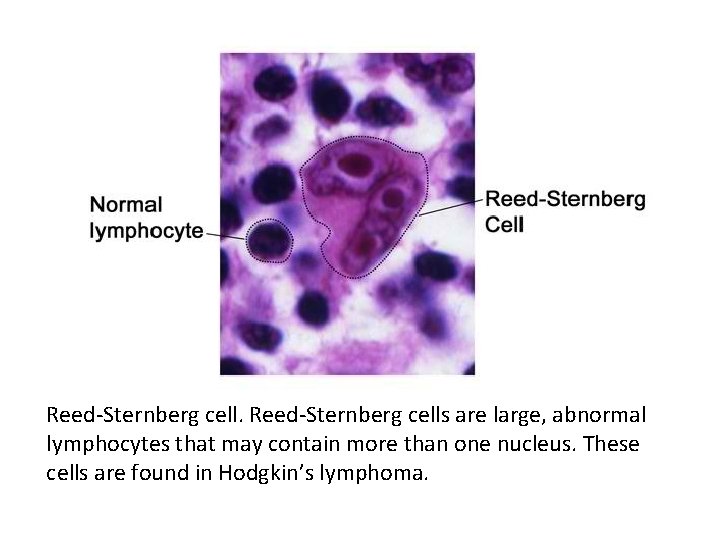
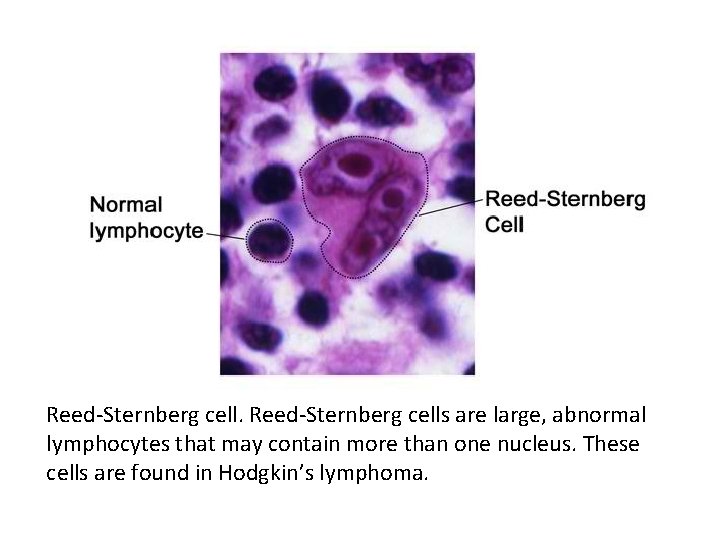
Reed-Sternberg cells are large, abnormal lymphocytes that may contain more than one nucleus. These cells are found in Hodgkin’s lymphoma.
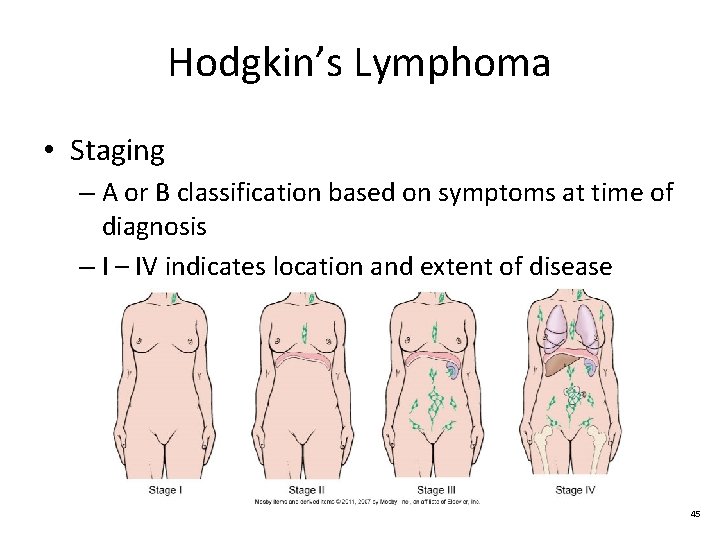
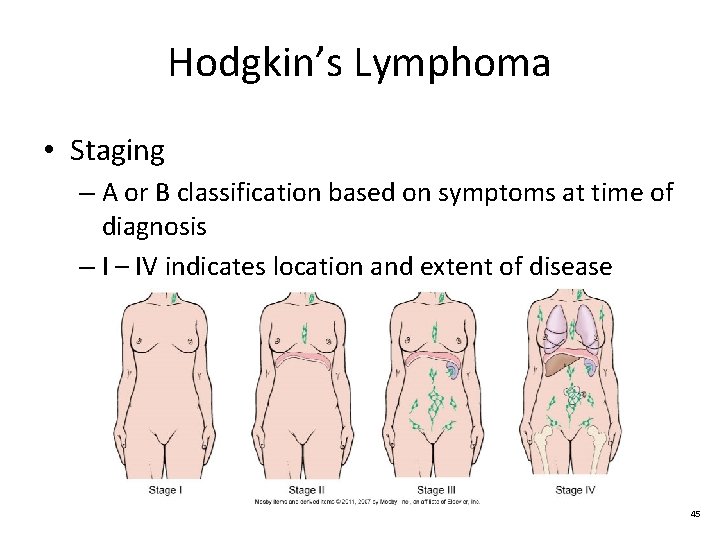
Hodgkin’s Lymphoma • Staging – A or B classification based on symptoms at time of diagnosis – IV indicates location and extent of disease 45
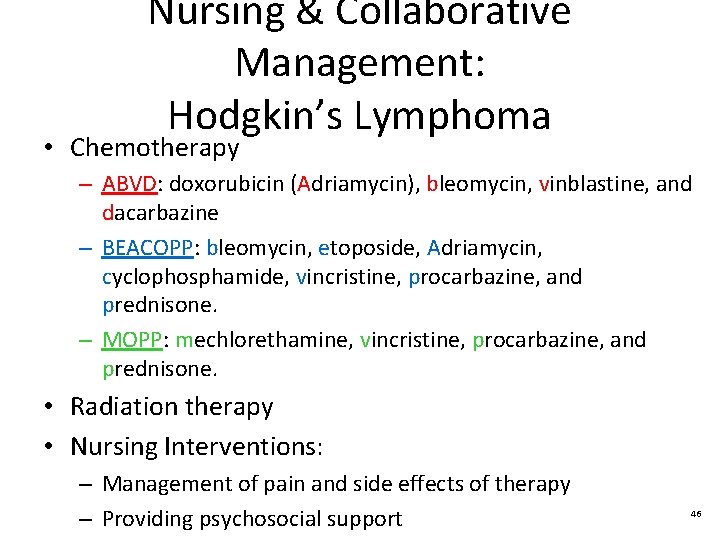
Nursing & Collaborative Management: Hodgkin’s Lymphoma • Chemotherapy – ABVD: doxorubicin (Adriamycin), bleomycin, vinblastine, and dacarbazine – BEACOPP: bleomycin, etoposide, Adriamycin, cyclophosphamide, vincristine, procarbazine, and prednisone. – MOPP: mechlorethamine, vincristine, procarbazine, and prednisone. • Radiation therapy • Nursing Interventions: – Management of pain and side effects of therapy – Providing psychosocial support 46
Non-Hodgkin’ Lymphoma • Signs & Symptoms – Can originate outside lymph nodes – Often disseminated at time of diagnosis – Similar to Hodgkin’s, but additional symptoms depending on site of metastasis • Diagnostic tests – Similar to Hodgkin’s but more extensive • Staging – International Working Formulation (IWF) • Low grade, Intermediate grade, and high grade 47
Nursing & Collaborative Management: Non-Hodgkin’s Lymphoma • Chemotherapy • Radiation therapy • Rituximab (Drug alert, p. 702) • Hematopoietic stem cell transplantation • Nursing interventions: – Management of pain r/t spinal cord compression and/or tumor lysis syndrome – Management of side effects of therapy – Monitor for complication r/t organs involved – Provide psychosocial support 48
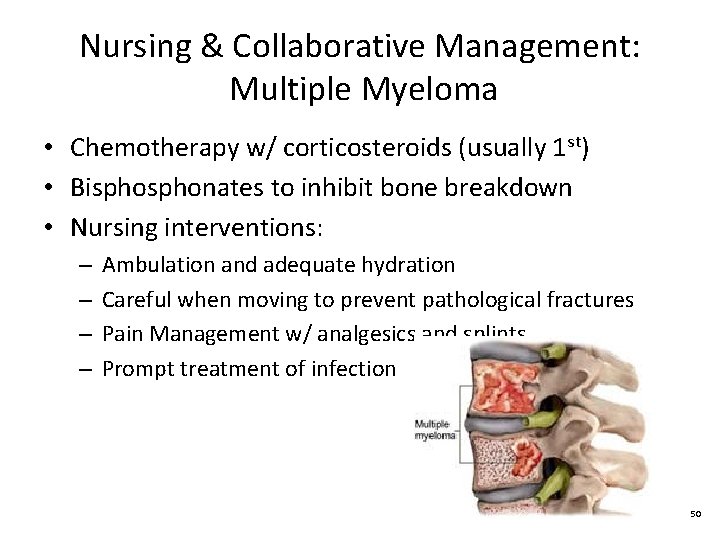
Multiple Myeloma • Signs & Symptoms – Causes anemia dyspnea, fatigue, bleeding – Bone pain (most often back and ribs) – Pathologic fractures – Numb and weak arms & legs r/t spinal compression – Fever without cause • Diagnostic Studies – Blood tests: calcium, total protein, creatinine, CBC – Radiology studies – Bone marrow biopsy – Bone density testing 49
Nursing & Collaborative Management: Multiple Myeloma • Chemotherapy w/ corticosteroids (usually 1 st) • Bisphonates to inhibit bone breakdown • Nursing interventions: – – Ambulation and adequate hydration Careful when moving to prevent pathological fractures Pain Management w/ analgesics and splints Prompt treatment of infection 50