Pediatric Physical Assessment Islamic University Nursing College Communication
- Slides: 69
Pediatric Physical Assessment Islamic University Nursing College
Communication n Considered very important to assess infant or child to provide information related to the health of child. n Use clear nonmedical terms when asking family & encourage them to talk. n Introduce your self, your name, your role, start trust relationship. n Use play to relieve anxiety.
Communication cont… n Get on eye level of the child & engage in verbally with child. n Treat adolescent neither child nor adult. n Ask questions that embarrassed when parents out. n Touch child to calm him. n Smile & pleasant face reduce child & parents.
Health Assessment n Collecting Data q By observation q Interviewing the parent q Interviewing the child q Physical examination
Bio-graphic Demographic Nursing history n Name, age, health care provider n Parents name age /siblings age n Ethnicity / cultural practices n Religion / religious practices n Parent occupation n Child occupation: adolescent
Past Medical History n Allergies n Childhood illness n Trauma / hospitalizations n Birth history n Did baby go home with mom / special care nursery n Genetics: anything in the family
Current Health Status n Immunizations n Any underlying illness / genetic condition n What concerns do you have today?
Review of systems n Ask questions about each system n Measuring data: growth chart, head circumference, BMI n Nutrition: breast fed, formula, eating habits n Growth and development: How does parent think child is doing?
Physical Assessment n General appearance & behavior q q q q Facial expression Posture / movement Sleep pattern Eating habits. Drug reactions Hygiene Behavior Development: grossly fits guidelines for age
Vital Signs n Temperature: rectal only when absolutely necessary n Pulse: apical on all children under 1 year n Respirations: infant uses abdominal muscles n Blood pressure: admission base line n Height and weight and head circumference for 2 years and younger
Physical Assessment n Skin, hair nails n Head, neck, lymph nodes: fontanelles n Eyes, nose, throat…look at palate and teeth n Chest: auscultate for breath sounds and adventitious sounds n Breasts: tanner scale n Heart: PMI, murmurs
Physical Assessment n Abdomen n Genitalia: tanner scale, discharge, testicles n Anus: inspect for cracks or fissures n Musculoskeletal: Ortaloni maneuver / Barlows n Feet / legs / back / gait
Neurological n Glasgow coma scale n Observe their natural state: Play games with them, especially children under 5 year n CNS grossly intact: II – XII
Newborn reflexes n Rooting: disappears at 3 -4 months n Sucking: disappears at 10 to 12 months n Palmar grasp: disappears at 3 to 4 months n Plantar grasp: disappears at 8 to 10 months n Tonic neck: disappears by 4 to 6 months n Moro (startle): disappears by 3 months n Babinski: disappears by 2 years n Stepping reflex: disappears by 2 months
Infant Exam n Examine on parent lap n Leave diaper on n Comfort measures such as pacifier or bottle. n Talk softly n Start with heart and lung sounds n Ear and throat exam last
Toddler Exam n Examine on parent lap if uncooperative n Use play therapy n Distract with stories n Let toddler play with equipment / BP n Call by name n Praise frequently n Quickly do exam
Preschool Exam n Allow parent to be within eye contact n Explain what you are doing n Let them feel the equipment
School-age Child n Allow the older child the choice of whether to have a parent present n Teaching about nutrition and safety n Ask if the child has any concerns or questions n How are they doing in school? n Do they have a group of friends they hand out with? n What do they like to do in their free time?
School-age Exam n Allow choice of having parent present n Privacy and modesty. n Explain procedures and equipment. n Interact with child during exam. n Be matter of fact about examining genital area.
Adolescent n Ask about parent in the room n Should have some private interview time: time to ask the difficult questions n HEADSS: home life, education, alcohol, drugs, sexual activity / suicide n Privacy issues
Vital Signs n Choose your words carefully when explaining vital sign measurements to a young child. Avoid saying, for example, “I’m going to take your pulse now. ” The child may think that are going to actually remove something from his or her body. A better phrase would be “I’m going to count how fast your heart beats. ”
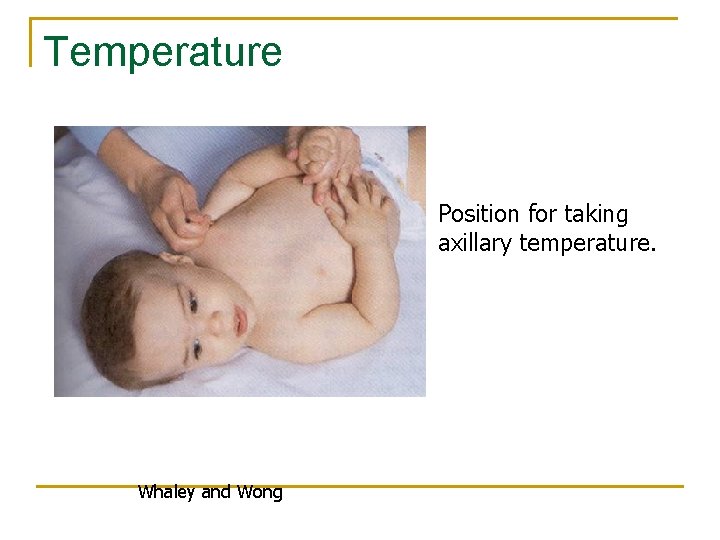
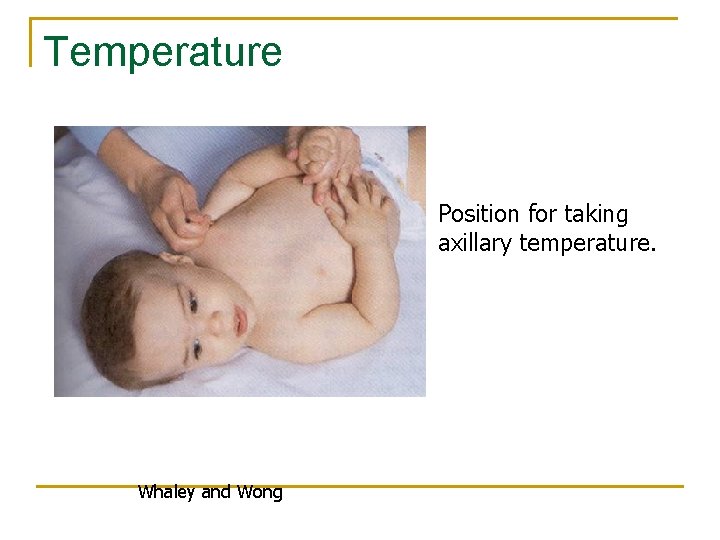
Temperature Position for taking axillary temperature. Whaley and Wong
Temperature n Use of tympanic membrane is controversial. n Oral temperature for children over 5 to 6 years. n Rectal temperatures are contraindicated if the child has had anal surgery, diarrhea, or rectal irritation. n Check with hospital policy.
Pulse n Apical pulse for infants and toddlers under 2 years n Count for 1 full minute n Will be increased with: crying, anxiety, fever, and pain
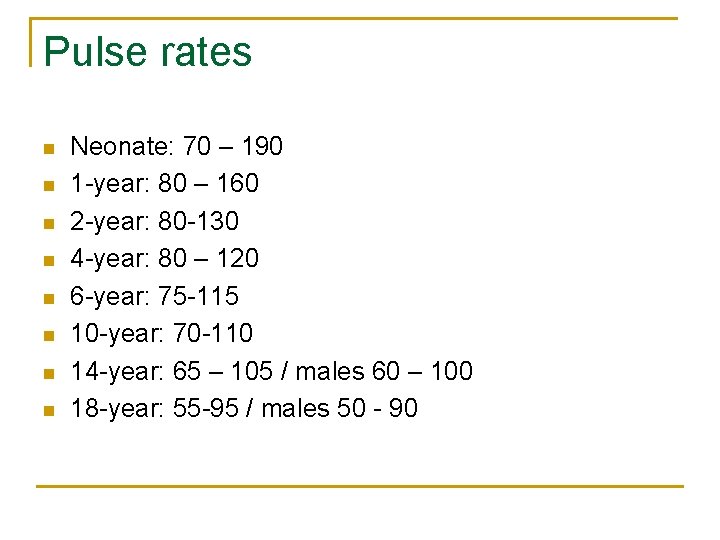
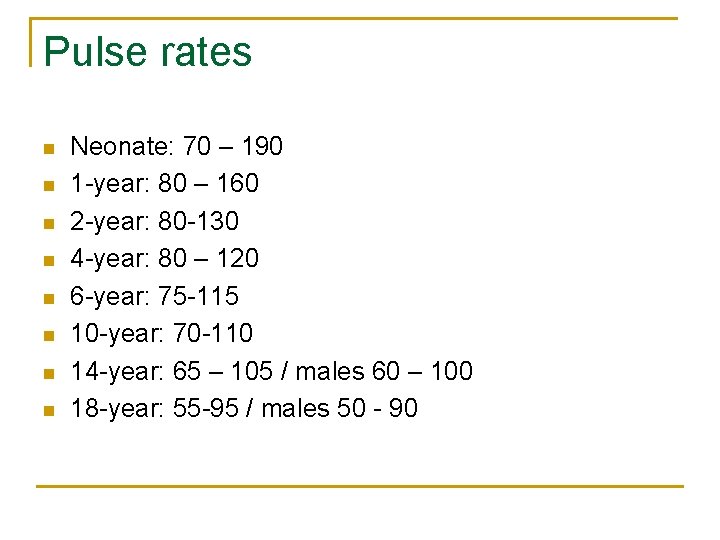
Pulse rates n n n n Neonate: 70 – 190 1 -year: 80 – 160 2 -year: 80 -130 4 -year: 80 – 120 6 -year: 75 -115 10 -year: 70 -110 14 -year: 65 – 105 / males 60 – 100 18 -year: 55 -95 / males 50 - 90
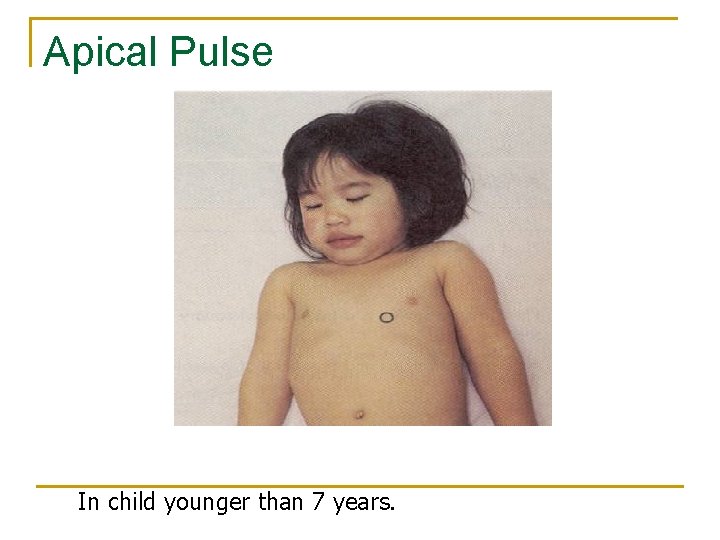
Apical Pulse In child younger than 7 years.
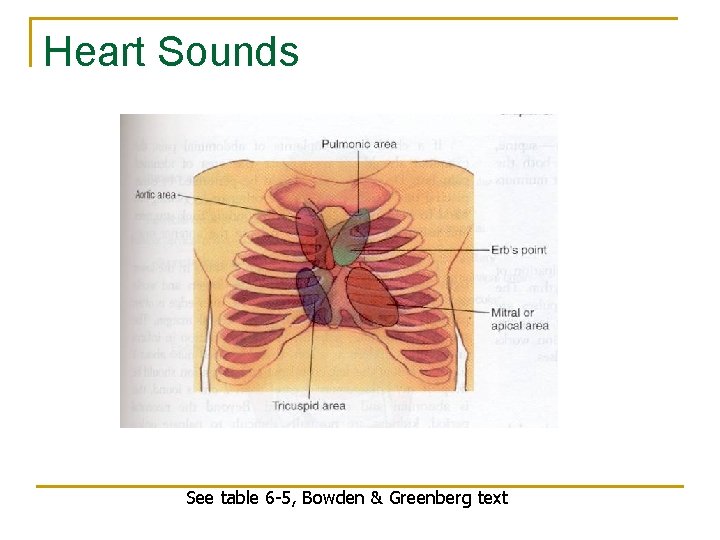
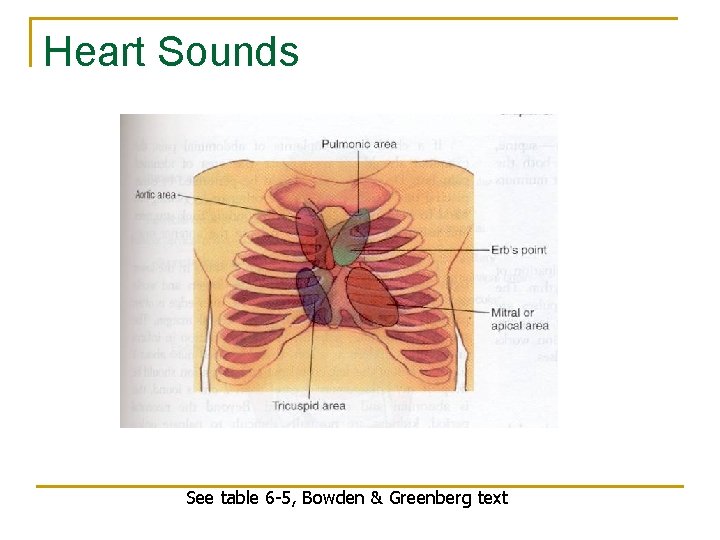
Heart Sounds See table 6 -5, Bowden & Greenberg text
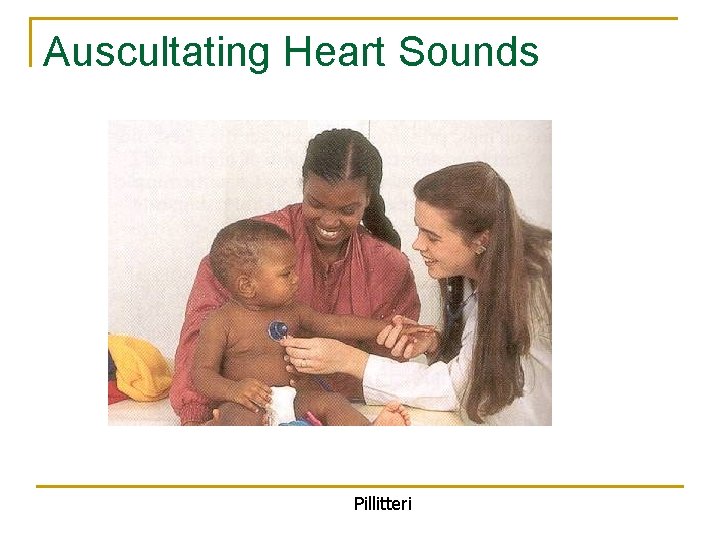
Auscultating Heart Sounds Pillitteri
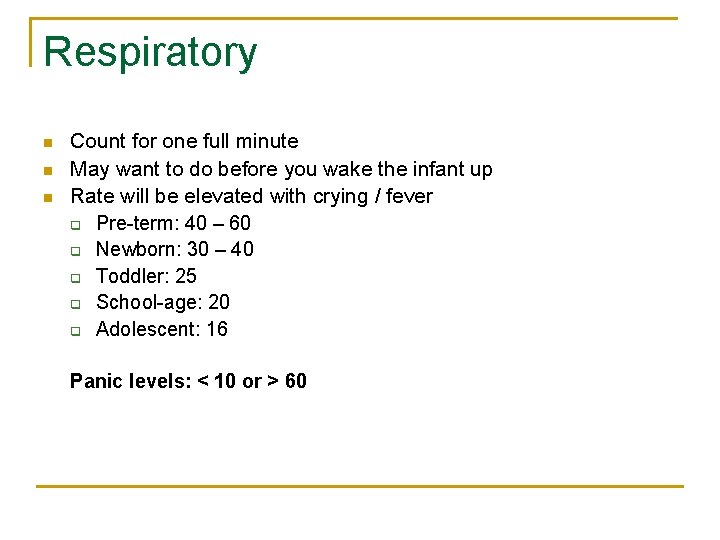
Respiratory n n n Count for one full minute May want to do before you wake the infant up Rate will be elevated with crying / fever q Pre-term: 40 – 60 q Newborn: 30 – 40 q Toddler: 25 q School-age: 20 q Adolescent: 16 Panic levels: < 10 or > 60
Clinical Tip n n n To accurately assess respirations in an infant or small child wait until the baby is sleeping or resting quietly. You might need to do this before you do more invasive exam. Count the number of breaths for an entire minute.
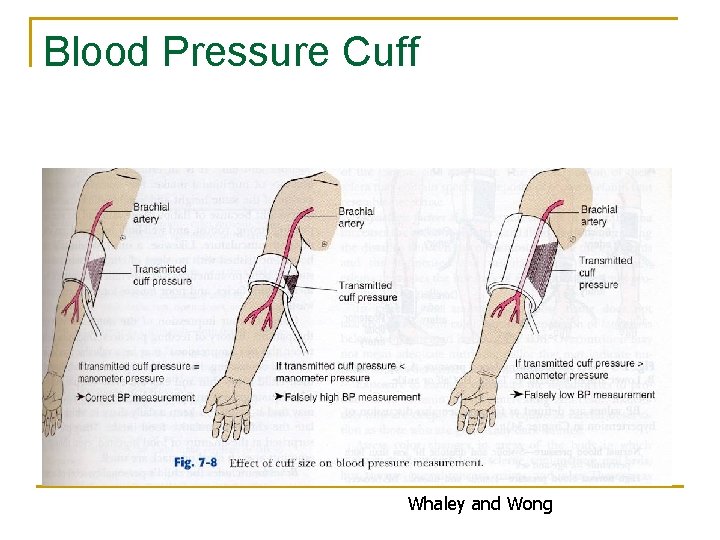
Blood Pressure n n n The width of the rubber bladder should cover two thirds of the circumference of the arm, and the length should encircle 100% of the arm without overlap. Crying can cause inaccurate blood pressure reading. Consider norms for age.
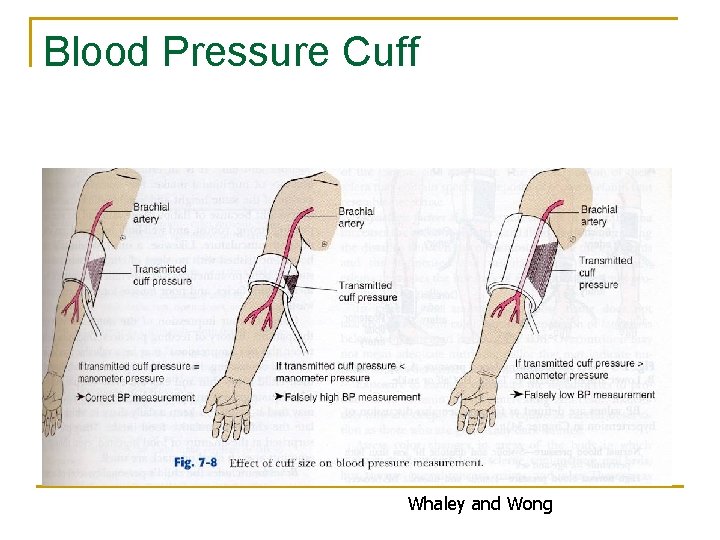
Blood Pressure Cuff Whaley and Wong
Height n n n Needs to be recorded on a growth chart Gain about an inch per month Deviation of height on either extreme may be indication for further investigation: endocrine problems
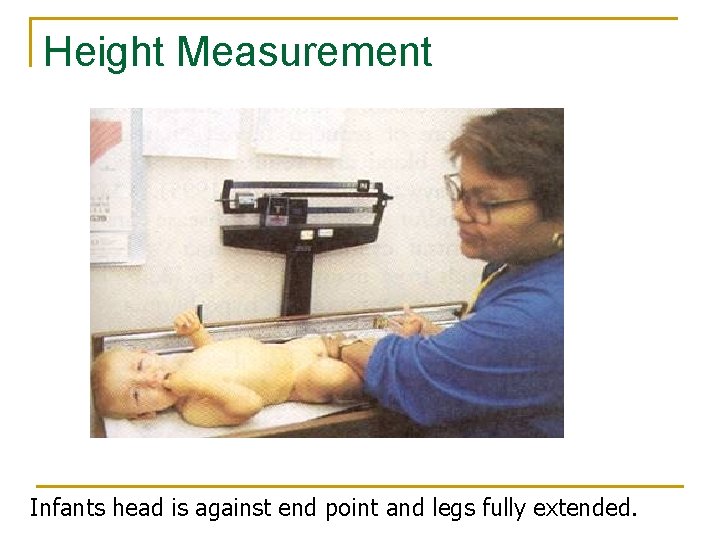
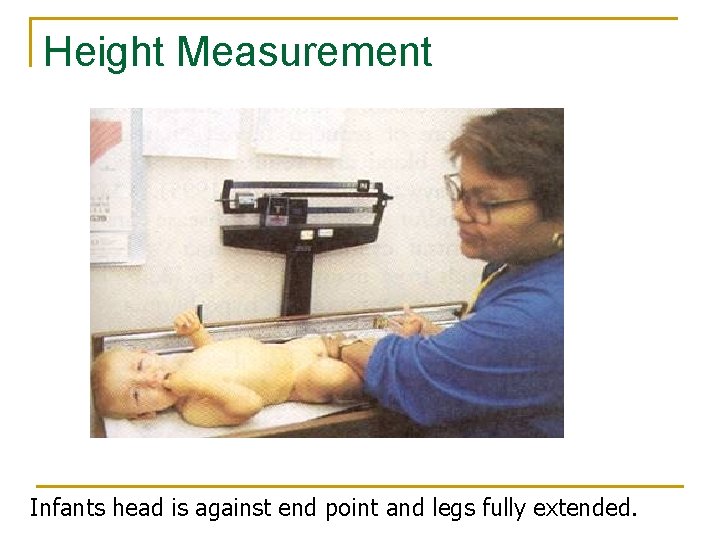
Height Measurement Infants head is against end point and legs fully extended.
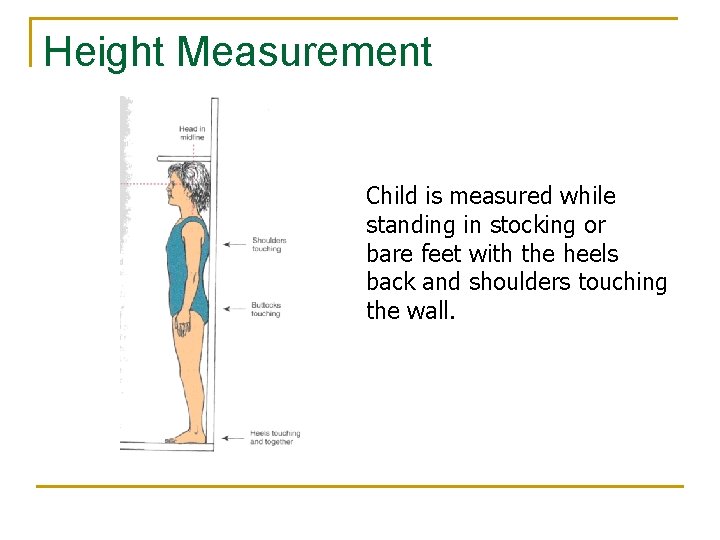
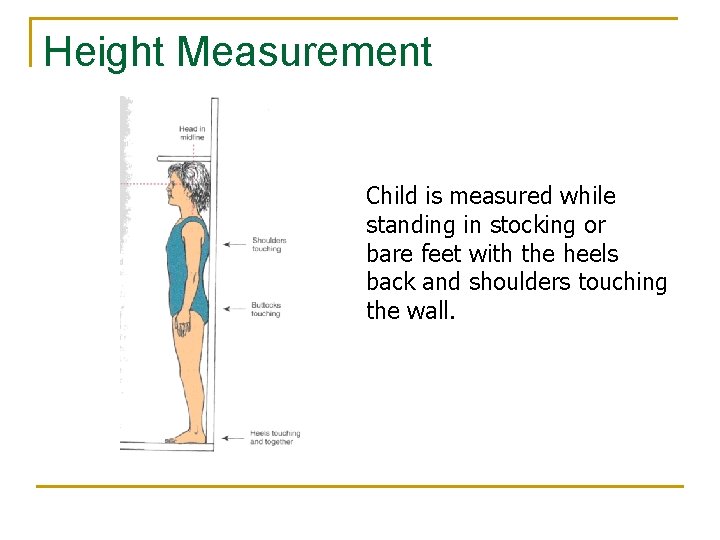
Height Measurement Child is measured while standing in stocking or bare feet with the heels back and shoulders touching the wall.
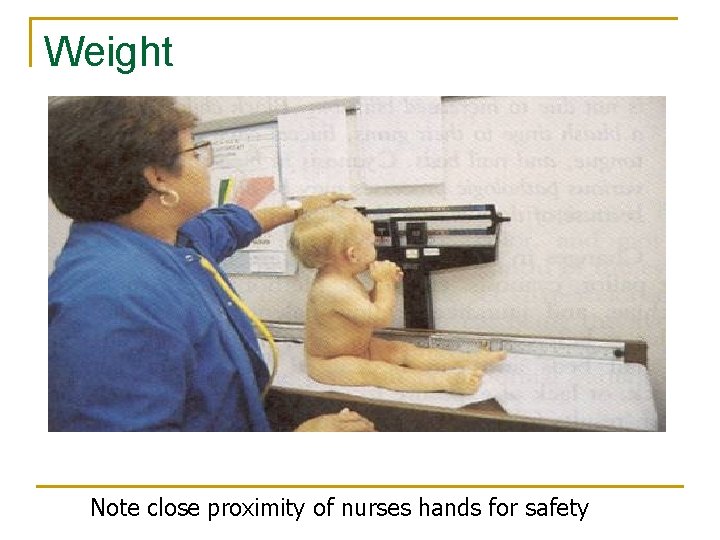
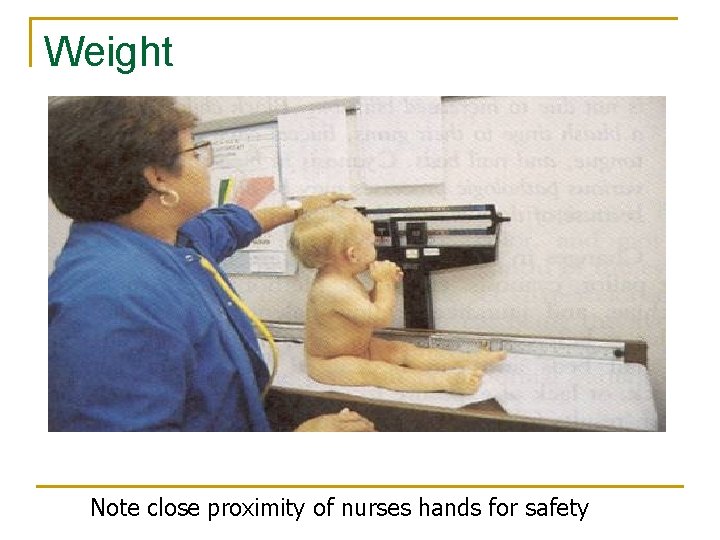
Weight Note close proximity of nurses hands for safety
Weight n n n Needs to be recorded on a growth chart Newborn may lose up to 10% of birth weight in 3 -4 days. Gains about ½ to 1 oz per day after that Too much or too little weight gain needs to be further investigated. Nutritional counseling
Weight norms n n Double birth weigh by 5 -6 months Triple birth weight by 1 year
Nutrition n n How much formula? How often being breast fed? Solid foods: 4 to 6 months of age What are they eating? Over 1 year: How much milk vs solid foods
Nutrition n School age: typical diet Favorite foods I always child if I were to ask their mom what do they need to eat more of what would she say?
Nutrition n Most common nutritional problems: q q q Iron deficiency anemia Obesity Anorexia
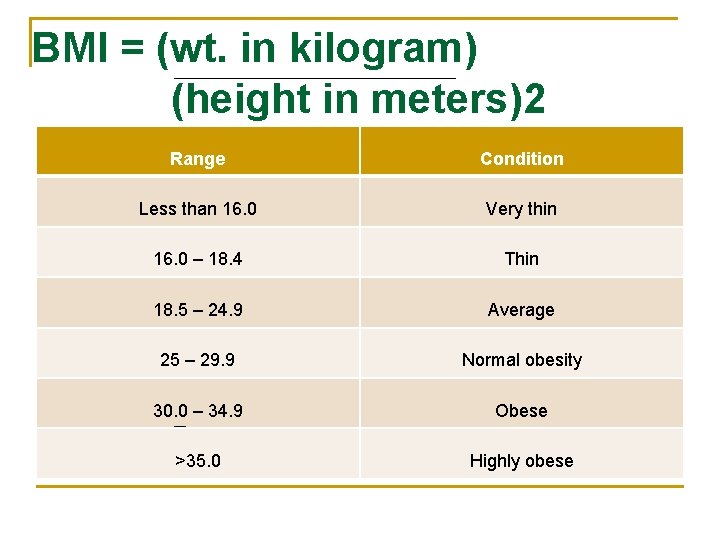
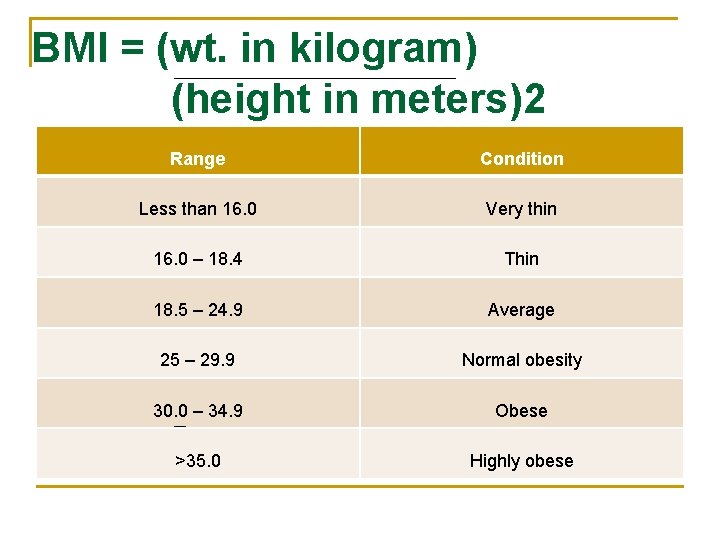
BMI = (wt. in kilogram) (height in meters)2 Range Condition Less than 16. 0 Very thin 16. 0 – 18. 4 Thin 18. 5 – 24. 9 Average 25 – 29. 9 Normal obesity 30. 0 – 34. 9 Obese >35. 0 Highly obese
Steps of physical examination: n n Inspection: color, warmth, odor texture characteristics. Palpation: to validate your inspection. Percussion: location, size, and density of organs or masses. Auscultation: stethoscope to auscultate heart, lungs, abdomen.
Assessment General Appearance n General appearance (clean, nourished, clothes. ) n Behavior & personality, interaction, temperament.
n n Assessment of skin texture: Lesions, abrasions, bruises drainage, color, pale, cyanosis, ecchymosis, petechiae. n Hair Assessment: n Color, cleanliness, loss, brittle, itching, etc. . n Nail Assessment: n Should be smooth & flexible not brittle, clubbing. n Head & Neck Assessment: n n n Shape, symmetry, fontanles, headaches, swollen, neck stiffness, range of movement, neck rigidity, flexion, hyperextension (meningitis) shift of trachea. Eyes & vision Assessment: Size, symmetry, color, eyes lids, pupil, unusual eyes movement, strabismus.
n Mouth, throat, nose Assessment: n Oral lesions, dental problems bleeding nose, nasal flaring, swelling, discharge, dryness, close of nasal by secretions. n Lips redness, drainage, herpes, tonsil enlargement, redness, white patches. n Teeth caries, missing, shape. n Palpate head & neck, lymph nodes, swollen, tender, warm nodes indicate infection.
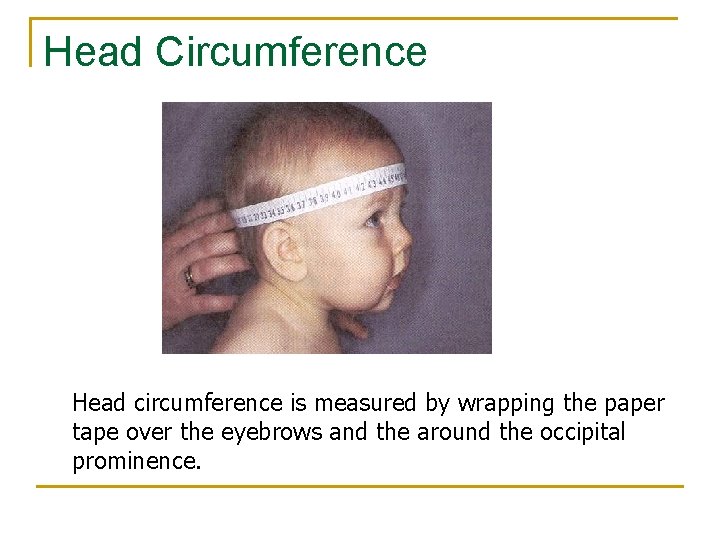
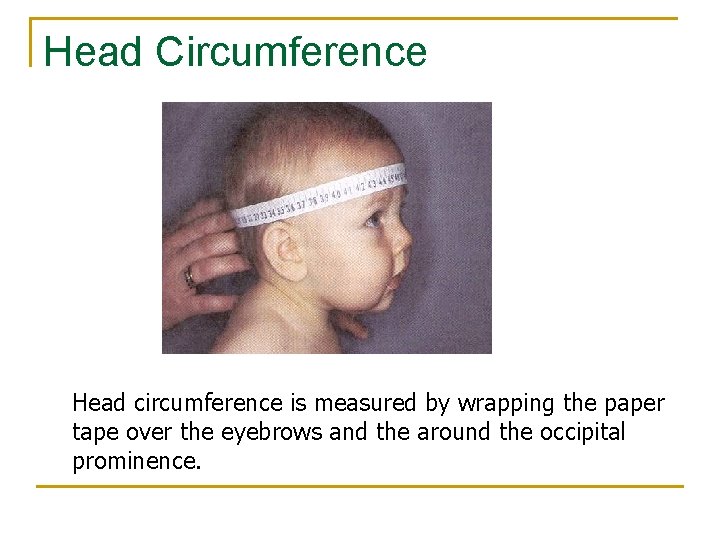
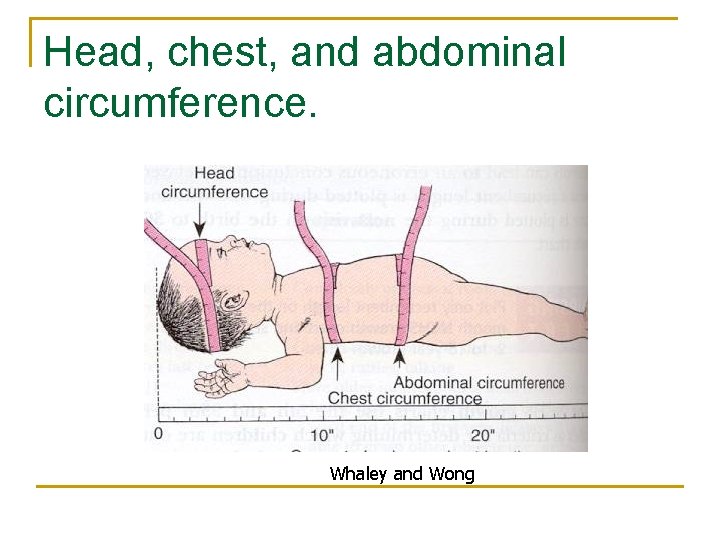
Head Circumference Head circumference is measured by wrapping the paper tape over the eyebrows and the around the occipital prominence.
Head n n n Needs to be measured until age 2 years Plot on growth curve Check fontales: q q n Anterior: 12 to 18 months Posterior: closes by 2 -5 months Shape: flat headed babies due to back-toback sleep position
Mouth n n n Palate Condition of teeth Number of teeth No teeth eruption by 12 months think endocrine disorder Appliances Brushing / visit to dentist
Eyes n n n Check for red-reflex Can the infant see: by parent report Strabismus: q q n Alignment of eye important due to correlation with brain development May need to corrected surgically 5 -year-old and up can have vision screening q Refer to ophthalmologist if there are concerns
Common eye infections: n Conjunctivitis: q q q A red-flag in the newborn may be STD from travel down the birth canal Pre-school: number one reason they are sent home: wash with warm water / topical eye gtts Inflammation of eye: history of juvenile arthritis
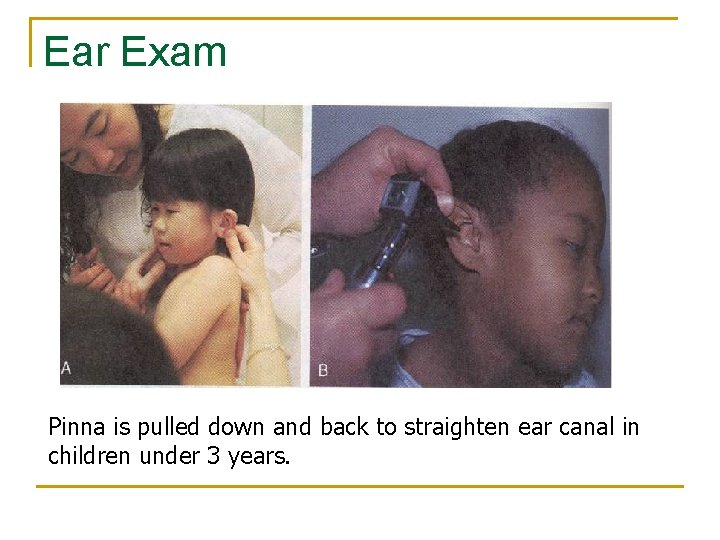
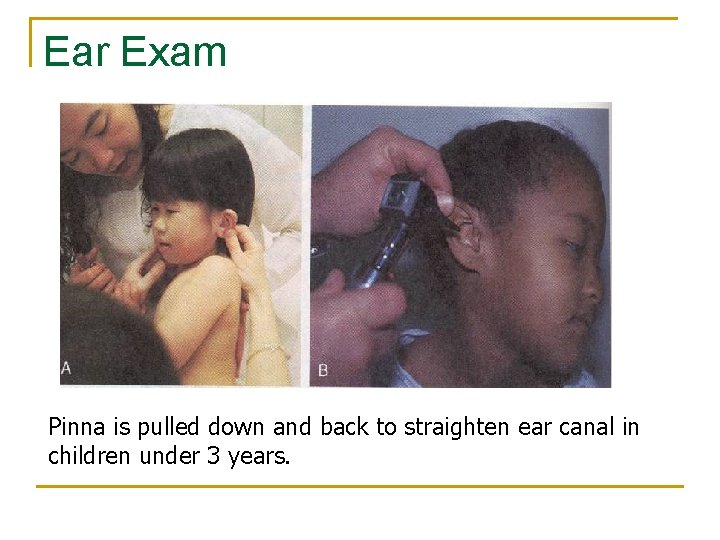
Ear Exam Pinna is pulled down and back to straighten ear canal in children under 3 years.
Otitis Media n n Most common reason children come to the pediatrician or emergency room Fever or tugging at ear Often increases at night when they are sleeping History of cold or congestion
Otitis n n ROM: right otitis media LOM: left otitis media BOM: bilateral otitis media OME: Otitis media with effusion (effusion means fluid collection) Pleural effusion, effusion of knee
Why a problem? n n Infection can lead to rupture of ear drum Chronic effusion can lead to hearing loss OM is often a contributing factor in more serious infections: mastoiditis, cellulitis, meningitis, bacteremia Chronic ear effusion in the early years may lead to decreased hearing and speech problems
Management n n n Oral antibiotics: re-check in 10 days Tylenol for comfort Persistent effusion: q q q PET: pressure equalizing tubes Outpatient procedure Need to keep water out of ears Hearing evaluation Speech evaluation
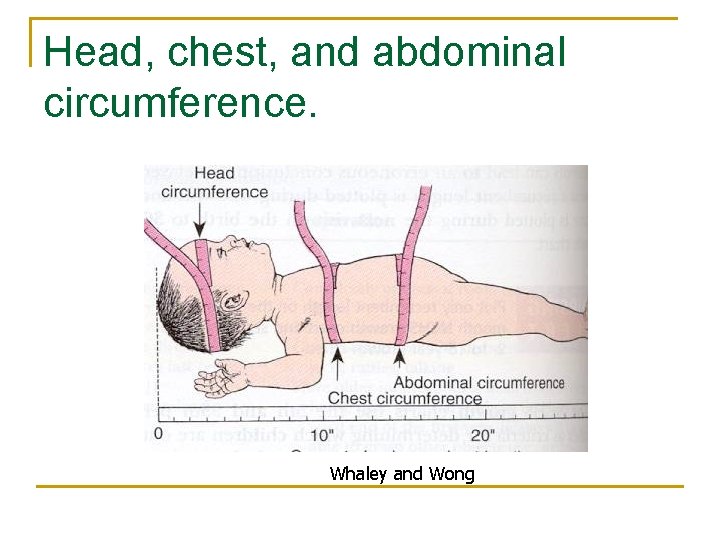
Head, chest, and abdominal circumference. Whaley and Wong
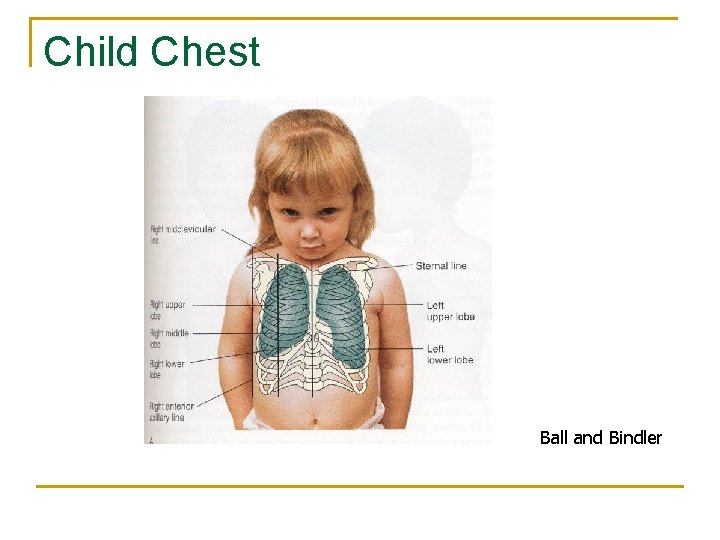
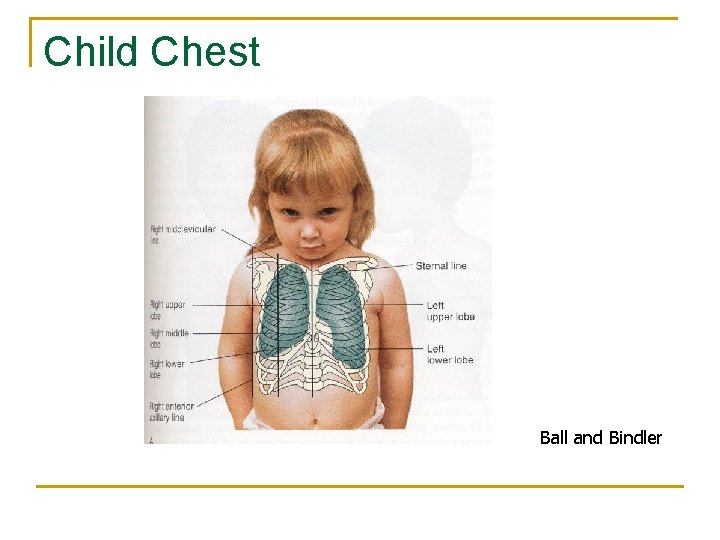
Child Chest Ball and Bindler
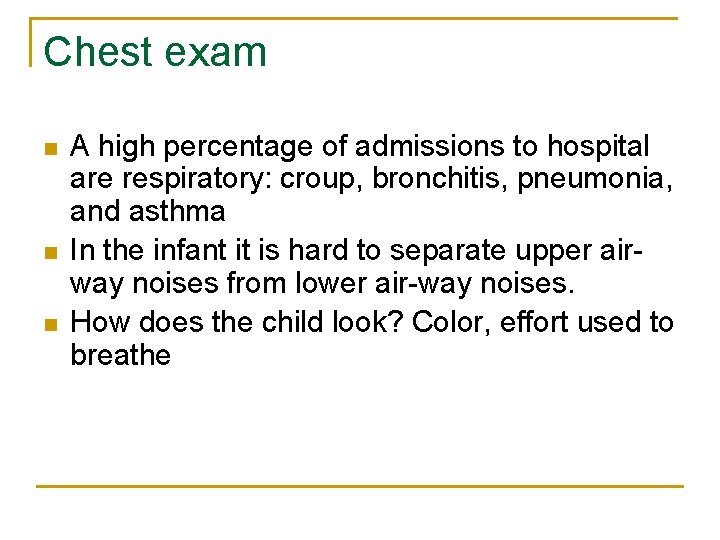
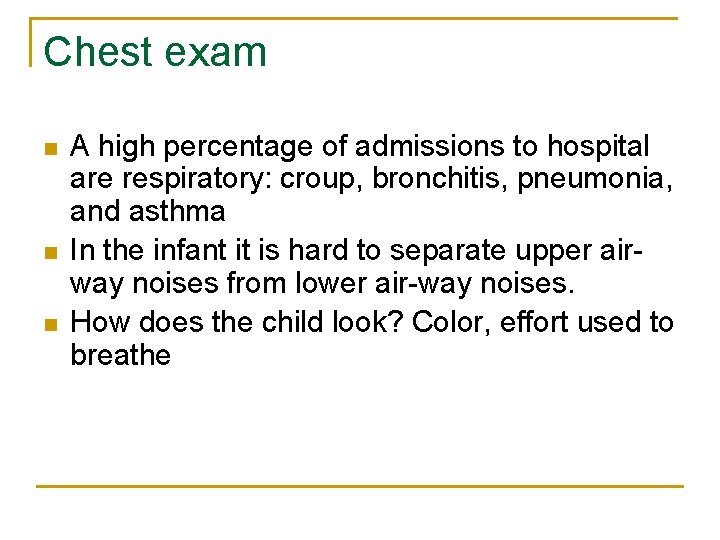
Chest exam n n n A high percentage of admissions to hospital are respiratory: croup, bronchitis, pneumonia, and asthma In the infant it is hard to separate upper airway noises from lower air-way noises. How does the child look? Color, effort used to breathe
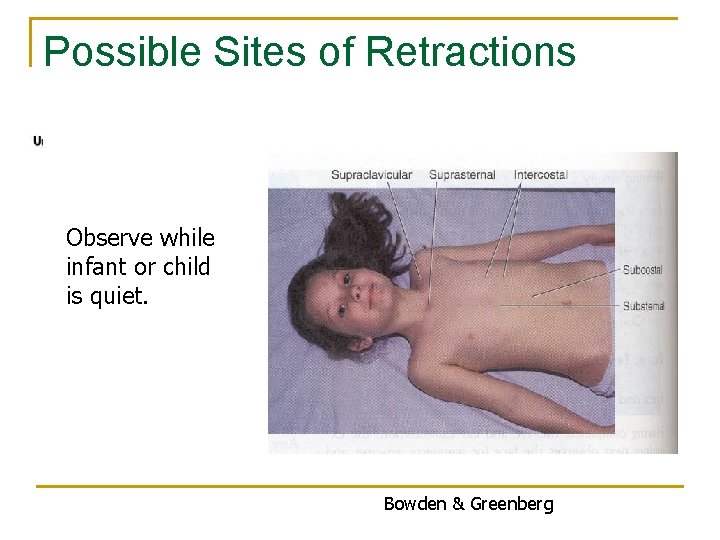
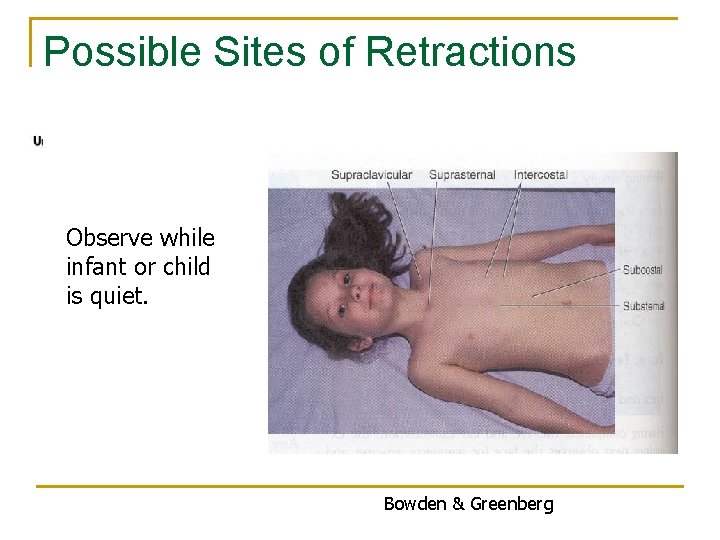
Possible Sites of Retractions Observe while infant or child is quiet. Bowden & Greenberg
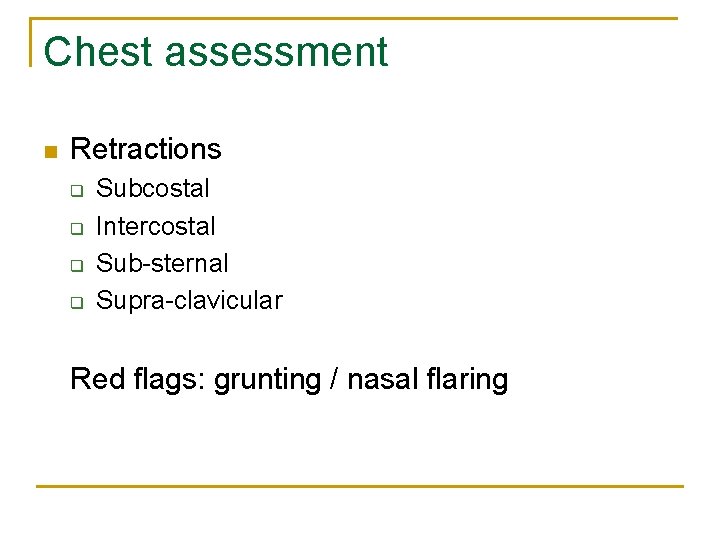
Chest assessment n Retractions q q Subcostal Intercostal Sub-sternal Supra-clavicular Red flags: grunting / nasal flaring
Wheeze or Stridor n n Wheezes occur when air flows rapidly through bronchi that are narrowed nearly to the point of closure. Wheezes is lower airway q n Asthma = expiratory wheezes A stridor is upper airway q Inflammation of upper airway or FB
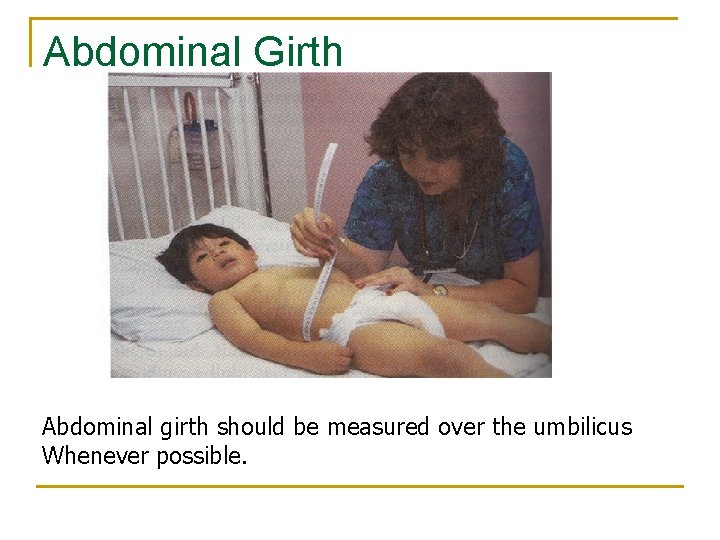
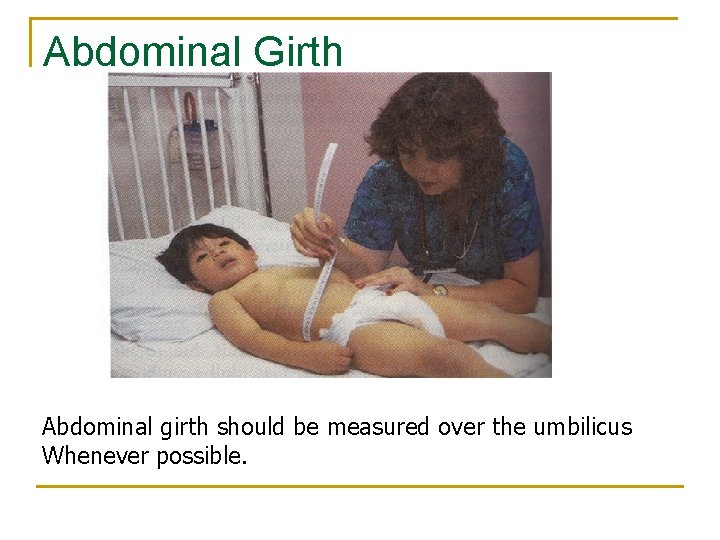
Abdominal Girth Abdominal girth should be measured over the umbilicus Whenever possible.
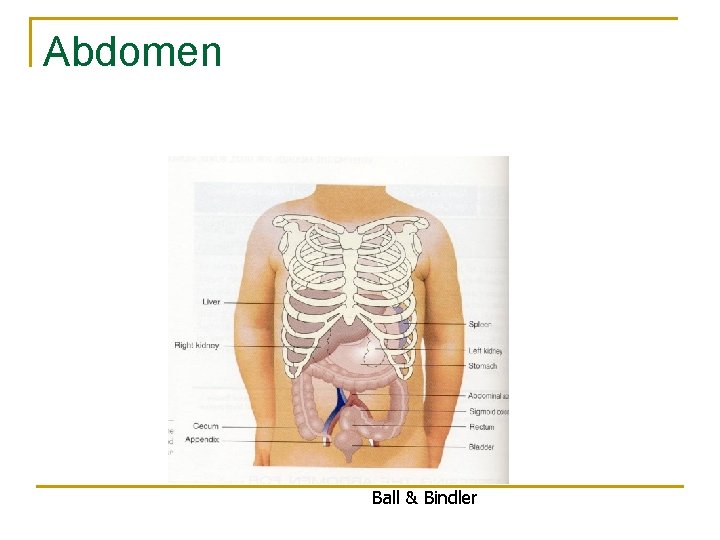
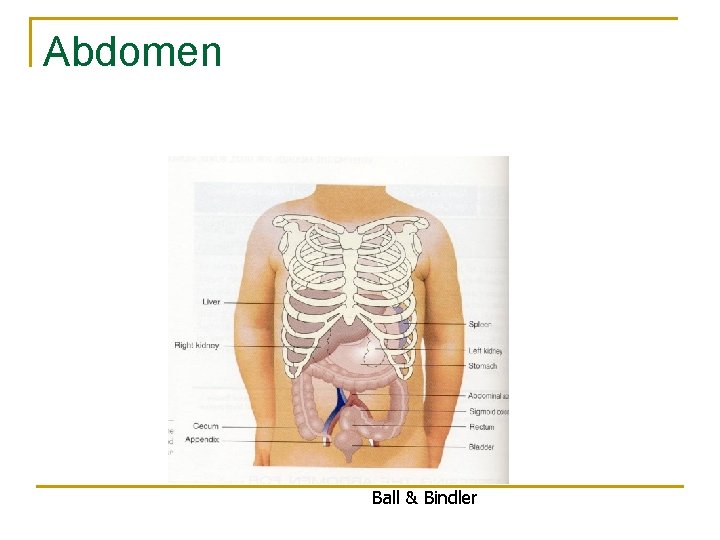
Abdomen Ball & Bindler
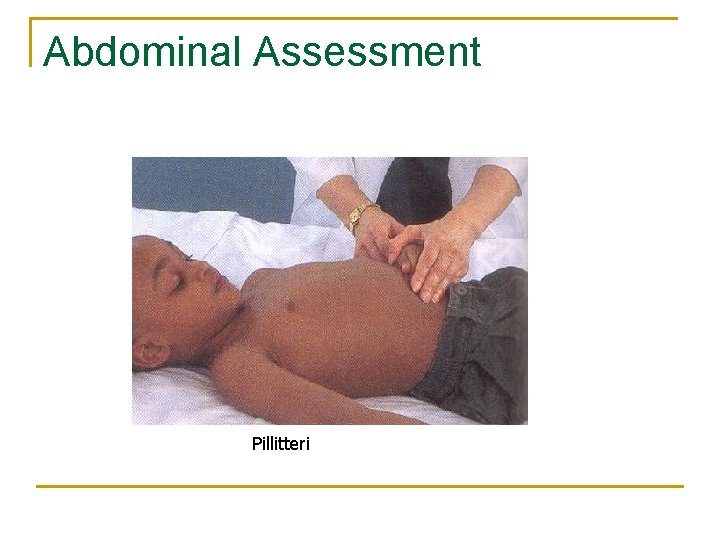
Abdominal Assessment Pillitteri
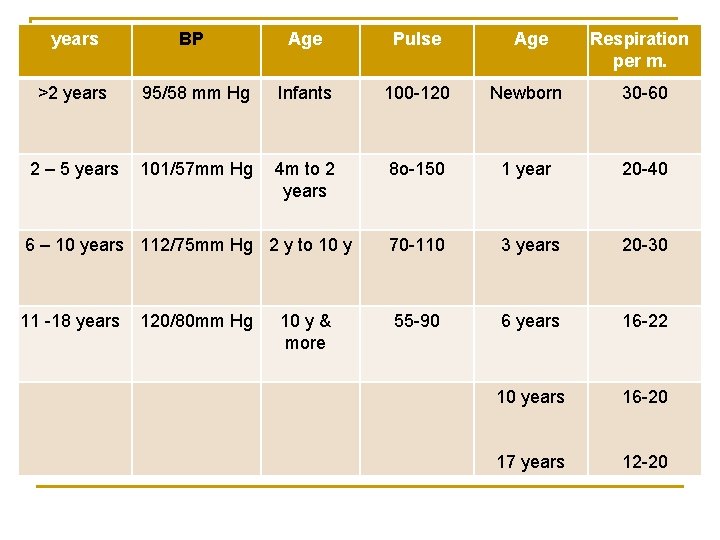
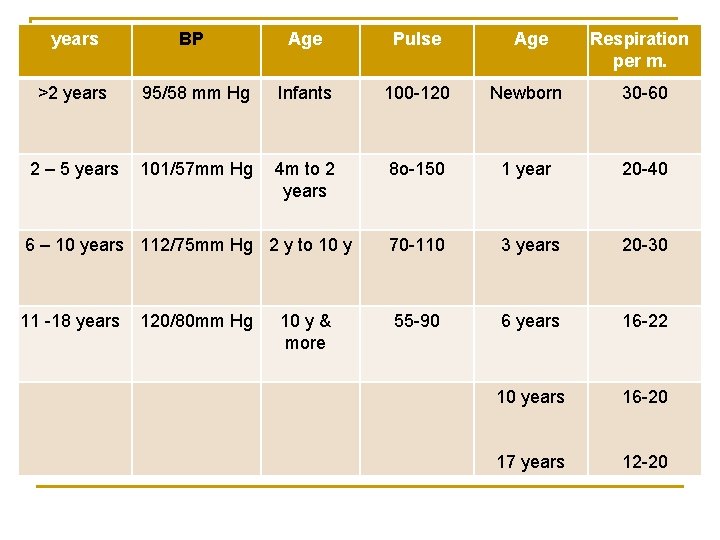
years BP Age Pulse Age Respiration per m. >2 years 95/58 mm Hg Infants 100 -120 Newborn 30 -60 2 – 5 years 101/57 mm Hg 4 m to 2 years 8 o-150 1 year 20 -40 70 -110 3 years 20 -30 55 -90 6 years 16 -22 10 years 16 -20 17 years 12 -20 6 – 10 years 112/75 mm Hg 2 y to 10 y 11 -18 years 120/80 mm Hg 10 y & more
Clinical Tip n Inspection and auscultation are performed before palpation and percussion because touching the abdomen may change the characteristics of the bowel sounds.
Bowel Sounds n n Normally occur every 10 to 30 seconds. Listen in each quadrant long enough to hear at least one bowel sound. Absence of bowel sounds may indicate peritonitis or a paralytic ileus. Hyperactive bowel sounds may indicate gastroenteritis or a bowel obstruction.
 Sucking reflex disappear
Sucking reflex disappear Islamic university college
Islamic university college Pediatric physical therapy outcome measures
Pediatric physical therapy outcome measures Hawler medical university college of nursing
Hawler medical university college of nursing Hawler medical university college of nursing
Hawler medical university college of nursing Yonsei university college of nursing
Yonsei university college of nursing 詹景裕
詹景裕 Trends in pediatric nursing
Trends in pediatric nursing Trends in pediatric nursing
Trends in pediatric nursing Pediatric nursing rimple sharma pdf free download
Pediatric nursing rimple sharma pdf free download Meaning of pediatric nurse
Meaning of pediatric nurse Atraumatic care meaning
Atraumatic care meaning Atraumatic care definition
Atraumatic care definition Family system theory
Family system theory Pediatric nursing definition
Pediatric nursing definition Islamic online university malaysia
Islamic online university malaysia Pediatric history and physical examination
Pediatric history and physical examination Sick child definition in hindi
Sick child definition in hindi Head tilt chin lift
Head tilt chin lift Pediatric assessment triangle
Pediatric assessment triangle Normal vitals
Normal vitals Ticls pat
Ticls pat Pediatric assessment triangle ticls
Pediatric assessment triangle ticls Pediatric assessment triangle
Pediatric assessment triangle Pediatric vital sogns
Pediatric vital sogns Asd college college readiness program
Asd college college readiness program Early college high school at midland college
Early college high school at midland college Www.tamilnadunursingcouncil.com
Www.tamilnadunursingcouncil.com Shoreline community college nursing
Shoreline community college nursing Kidney biopsy
Kidney biopsy Associate of applied science in nursing block vs integrated
Associate of applied science in nursing block vs integrated Jccc rn program
Jccc rn program Glendale community college transcripts
Glendale community college transcripts Glendale community college rn program
Glendale community college rn program History of west african college of nursing
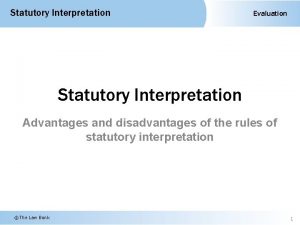
History of west african college of nursing R v allen (1872) lr 1 ccr 367
R v allen (1872) lr 1 ccr 367 Montgomery college nursing application deadline
Montgomery college nursing application deadline Harbor college child development center
Harbor college child development center Glendale community college transcript
Glendale community college transcript Lvn to bsn sacramento
Lvn to bsn sacramento Nursing moraine valley
Nursing moraine valley Montgomery college wdce
Montgomery college wdce Lane community college advising
Lane community college advising Royal college of nursing v dhss 1981
Royal college of nursing v dhss 1981 River valley community college nursing
River valley community college nursing Cscc lpn program
Cscc lpn program Red rocks community college nursing
Red rocks community college nursing Lonestar hesi
Lonestar hesi Lone star lvn program
Lone star lvn program Staffing and nursing care delivery models
Staffing and nursing care delivery models Care plan on ocd
Care plan on ocd Cataract surgery nursing diagnosis
Cataract surgery nursing diagnosis Introduction of nursing process
Introduction of nursing process Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Assessment college of sa (pty) ltd
Assessment college of sa (pty) ltd Landmark college readiness assessment
Landmark college readiness assessment Assessment college of south africa
Assessment college of south africa Tourism definition
Tourism definition Stranmillis university college
Stranmillis university college Norwegian police university college
Norwegian police university college Lincoln memorial university college of veterinary medicine
Lincoln memorial university college of veterinary medicine King faisal university college of medicine
King faisal university college of medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine University of iowa college of dentistry
University of iowa college of dentistry Clark university college board
Clark university college board Artesis plantijn university college of antwerp
Artesis plantijn university college of antwerp Norwegian defence university college
Norwegian defence university college King saud university college of pharmacy
King saud university college of pharmacy King saud university college of medicine
King saud university college of medicine