Head Injury Head Injury Any trauma to the









- Slides: 31
Head Injury

Head Injury • Any trauma to the scalp, skull, or brain • Head trauma includes an alteration in consciousness no matter how brief
Head Injury • Causes – Motor vehicle accidents – Firearm-related injuries – Falls – Assaults – Sports-related injuries – Recreational accidents
Head Injury • High potential for poor outcome • Deaths occur at three points in time after injury: – Immediately after the injury – Within 2 hours after injury – 3 weeks after injury
Head Injury Types of Head Injuries • Scalp lacerations – The most minor type of head trauma – Scalp is highly vascular profuse bleeding – Major complication is infection
Head Injury Types of Head Injuries • Skull fractures – Linear or depressed – Simple, comminuted, or compound – Closed or open – Direct & Indirect – Coup & Contrecoup
Head Injury Types of Head Injuries • Skull fractures – Location of fracture alters the presentation of the manifestations – Facial paralysis – Conjugate deviation of gaze – Battle’s sign

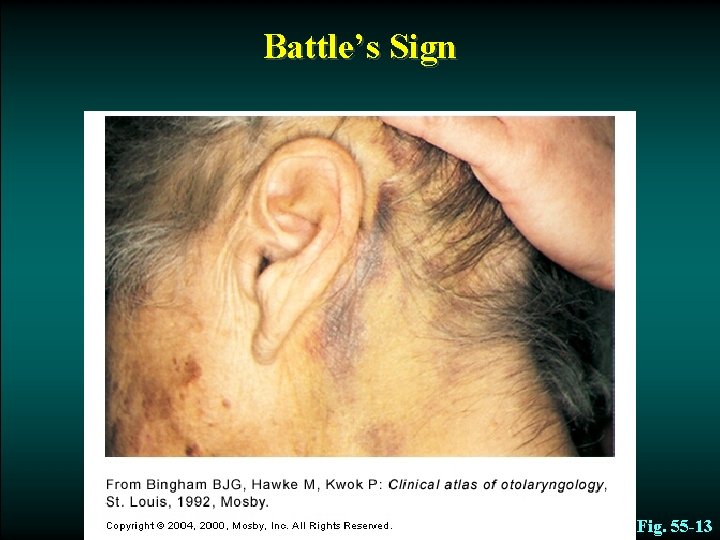
Head Injury Types of Head Injuries • Basal Skull fractures – CSF leak (extravasation) into ear (Otorrhea) or nose (Rhinorrhea) – High risk infection or meningitis – “HALO Sign (Battle Sign)” on clothes of linen – Possible injury to Internal carotid artery – Permanent CSF leaks possible
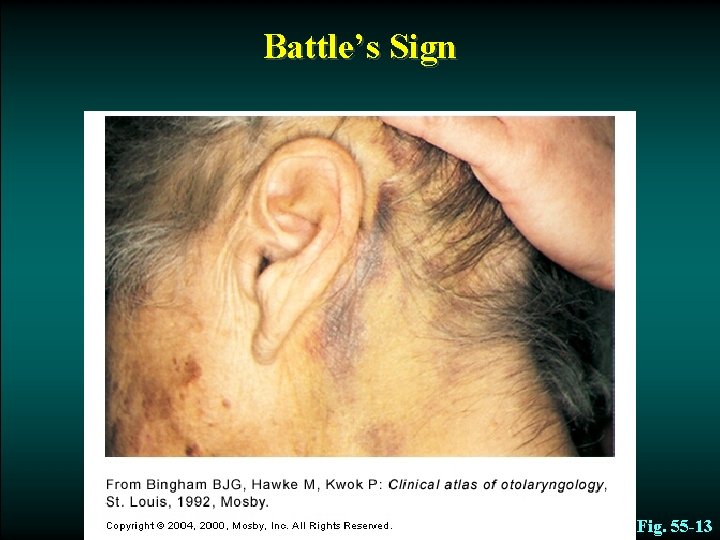
Battle’s Sign Fig. 55 -13
Nursing Care of Skull Fractures • Minimize CSF leak – Bed flat – Never suction orally; never insert NG tube; never use Q-Tips in nose/ears; caution patient not to blow nose • Place sterile gauze/cotton ball around area • Verify CSK leak: – DEXTROSTIX: positive for glucose • Monitor closely: Respiratory status+++
Head Injury Types of Head Injuries • Minor head trauma – Concussion • A sudden transient mechanical head injury with disruption of neural activity and a change in LOC • Brief disruption in LOC • Amnesia • Headache • Short duration
Head Injury Types of Head Injuries • Minor head trauma – Postconcussion syndrome • 2 weeks to 2 months • Persistent headache • Lethargy • Personality and behavior changes
Head Injury Types of Head Injuries • Major head trauma – Includes cerebral contusions and lacerations – Both injuries represent severe trauma to the brain

Head Injury Types of Head Injuries • Major head trauma – Contusion • The bruising of brain tissue within a focal area that maintains the integrity of the pia mater and arachnoid layers – Lacerations • Involve actual tearing of the brain tissue • Intracerebral hemorrhage is generally associated with cerebral laceration
Head Injury Pathophysiology • Diffuse axonal injury (DAI) – Widespread axonal damage occurring after a mild, moderate, or severe TBI – Process takes approximately 12 -24 hours
Head Injury Pathophysiology • Diffuse axonal injury (DAI) – Clinical signs: • LOC • ICP • Decerebration or decortication • Global cerebral edema

Head Injury Complications • Epidural hematoma – Results from bleeding between the dura and the inner surface of the skull – A neurologic emergency – Venous or arterial origin
Head Injury Complications • Subdural hematoma – Occurs from bleeding between the dura mater and arachnoid layer of the meningeal covering of the brain

Epidural and Subdural Hematomas Epidural Hematoma Subdural Hematoma Fig. 55 -15
Head Injury Complications • Subdural hematoma – Usually venous in origin – Much slower to develop into a mass large enough to produce symptoms – May be caused by an arterial hemorrhage
Head Injury Complications • Subdural hematoma – Acute subdural hematoma • High mortality • Signs within 48 hours of the injury • Associated with major trauma (Shearing Forces) • Patient appears drowsy and confused • Pupils dilate and become fixed
Head Injury Complications • Subdural hematoma – Subacute subdural hematoma • Occurs within 2 -14 days of the injury • Failure to regain consciousness may be an indicator
Head Injury Complications • Subdural hematoma – Chronic subdural hematoma • Develops over weeks or months after a seemingly minor head injury

Head Injury Diagnostic Studies and Collaborative Care • CT scan considered the best diagnostic test to determine craniocerebral trauma • MRI • Cervical spine x-ray • Glasgow Coma Scale (GCS) • Craniotomy • Craniectomy • Cranioplasty • Burr-hole
Head Injury Nursing Management Nursing Assessment – GCS score – Neurologic status – Presence of CSF leak
Head Injury Nursing Management Nursing Diagnoses – Ineffective tissue perfusion – Hyperthermia – Acute pain – Anxiety – Impaired physical mobility

Head Injury Nursing Management Planning – Overall goals: • Maintain adequate cerebral perfusion • Remain normothermic • Be free from pain, discomfort, and infection • Attain maximal cognitive, motor, and sensory function

Head Injury Nursing Management Nursing implementation Health Promotion • Prevent car and motorcycle accidents • Wear safety helmets

Head Injury Nursing Management Nursing implementation Acute Intervention • Maintain cerebral perfusion and prevent secondary cerebral ischemia • Monitor for changes in neurologic status
Head Injury Nursing Management Nursing implementation Ambulatory and Home Care • Nutrition • Bowel and bladder management • Spasticity • Dysphagia • Seizure disorders • Family participation and education
Head Injury Nursing Management Evaluation Expected Outcomes • Maintain normal cerebral perfusion pressure • Achieve maximal cognitive, motor, and sensory function • Experience no infection, hyperthermia, or pain
 How to protect yourself from intentional injuries
How to protect yourself from intentional injuries Chapter 24 trauma overview
Chapter 24 trauma overview Head trauma classification
Head trauma classification There are some cake
There are some cake Any to any connectivity
Any to any connectivity Informational probes adalah
Informational probes adalah Nrl head injury recognition and referral form
Nrl head injury recognition and referral form Head injury nursing management
Head injury nursing management Patrick lynch head injury colorado
Patrick lynch head injury colorado Head injury assessment
Head injury assessment Nursing care plan for head injury slideshare
Nursing care plan for head injury slideshare Cholesteatoma
Cholesteatoma Diễn thế sinh thái là
Diễn thế sinh thái là Tư thế ngồi viết
Tư thế ngồi viết Lp html
Lp html Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Vẽ hình chiếu vuông góc của vật thể sau
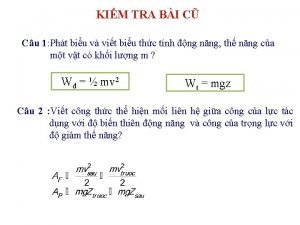
Vẽ hình chiếu vuông góc của vật thể sau Công của trọng lực
Công của trọng lực Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dot
Dot Lời thề hippocrates
Lời thề hippocrates Bổ thể
Bổ thể Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập