ICU pharmaceutical care Sedation Clinical pharmacist Lihua Fang












- Slides: 64
ICU pharmaceutical care 加護病房的藥事照顧 Sedation Clinical pharmacist Lihua Fang Koo Foundation cancer center (2015/01/08) 2020/11/2
Outline 加護病房發展史 照護基本原則Basic principles 臨床服務項目(Sedation, pain control, sepsis campaign, TDM) How to start Services
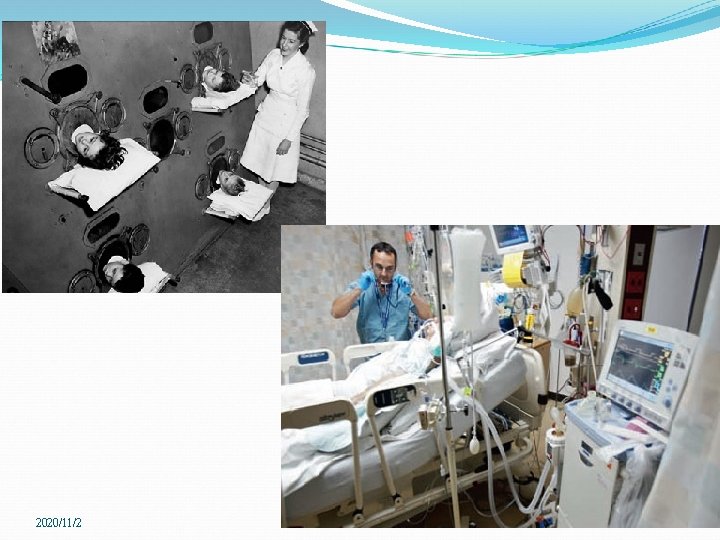
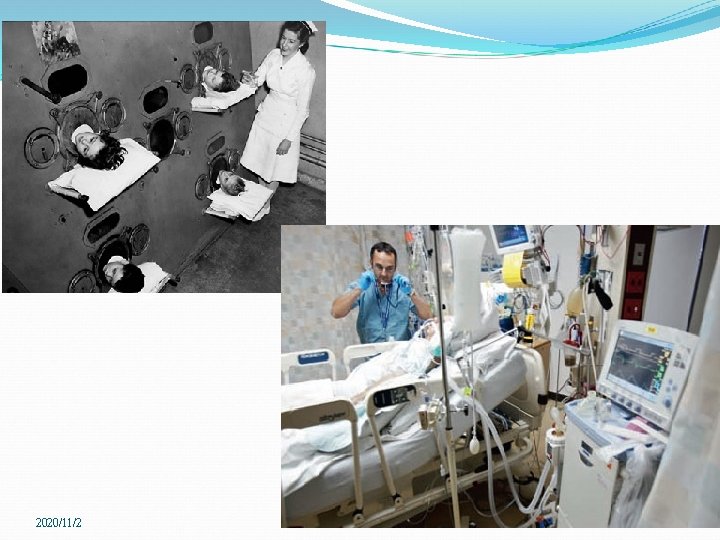
加護病房發展史 Critical Care 2013, 17(Suppl 1): S 2 Florence Nightingale era The Crimean War 1853 (mortality 40%->2%), theoretical and technical nursing education Dandy era (1914 -1946 in John Hopkins hospital) The first ICU in the world, In 1926 for critically ill postoperative neurosurgical patients Ibsen era (Copenhagen) In 1952 poliomyelitis outbreak in Denmark, 2722 pts/ 6 -month , with 316 respiratory or airway paralysis. Positive pressure ventilation by intubation. In 1953, the world's first Medical/Surgical ICU 2020/11/2
加護病房發展史 Safar era 1958 A multidisciplinary ICU was established in Baltimore, and, in 1962, in the University of Pittsburgh, the first Critical Care Residency was established in the United States. In 1970, the Society of Critical Care Medicine was formed The first ICU in Taiwan in 1967, China in 1982 2020/11/2
2020/11/2
ICU revolution Primary specialties Anesthesiology or internal medicine. Setting Surgical and Medical ICUs Respiratory, cardiac, and neurosurgical ICUs Open : managed by their primary admitting physician Close : qualified intensive care physicians and nurses specialist training programs : intensive care medicine

ICU revolution The quantity of critical care research Understanding of the mechanisms of critical illness More sophisticated life-support and invasive monitoring techniques Interventional management The pulmonary artery catheter Fluid , blood transfusions, oxygen, and vasopressors

Education and Training of Clinical Pharmacists ASHP established a formal accreditation process in 1962 ASHP : accreditation for 15 subspecialties of pharmacy practice. Critical care pharmacy residents : 12 -month program Multiple skill sets direct patient care, drug information, policy development, and practice management) Rounding providing education to various members of the healthcare team in formal and informal settings. Residency applicants : 11% Board of Pharmaceutical Specialties (BPS) nuclear, nutrition , pharmacotherapy, psychiatric pharmacy, and oncology pharmacy, Ambulatory Care 2015 : add critical care and pediatric 2020/11/2

Critical care: the present Mechanical ventilators : smaller, more mobile, and more user-friendly Portable ultrasound Less invasive, less interventional, more humane Unrestricted visiting Improved communication with pts and families in daily practice and decision-making Multidisciplinary approach nutritionists, physiotherapists, pharmacists, infectious disease consultants, other relevant specialties Local, regional, and international surveillance systems to monitor antibiotic resistance and microbiology patterns. Critical Care 2013, 17(Suppl 1): S 2 2020/11/2
ICU is a place : Complicated 2020/11/2
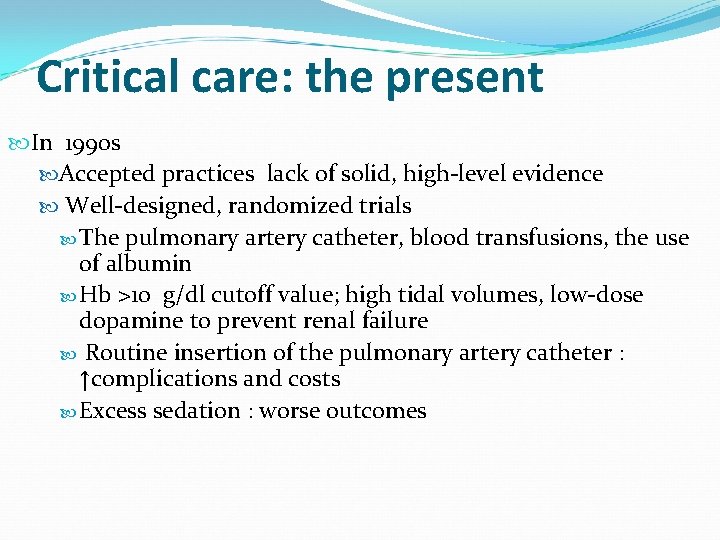
Critical care: the present In 1990 s Accepted practices lack of solid, high-level evidence Well-designed, randomized trials The pulmonary artery catheter, blood transfusions, the use of albumin Hb >10 g/dl cutoff value; high tidal volumes, low-dose dopamine to prevent renal failure Routine insertion of the pulmonary artery catheter : ↑complications and costs Excess sedation : worse outcomes
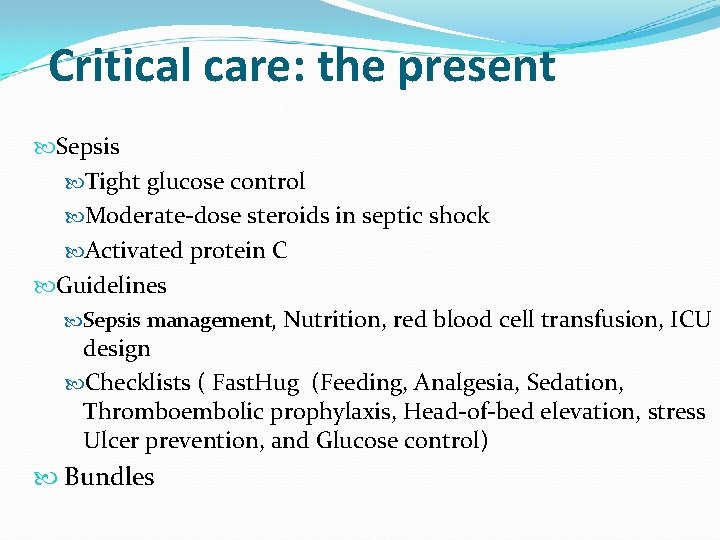
Critical care: the present Sepsis Tight glucose control Moderate-dose steroids in septic shock Activated protein C Guidelines Sepsis management, Nutrition, red blood cell transfusion, ICU design Checklists ( Fast. Hug (Feeding, Analgesia, Sedation, Thromboembolic prophylaxis, Head-of-bed elevation, stress Ulcer prevention, and Glucose control) Bundles

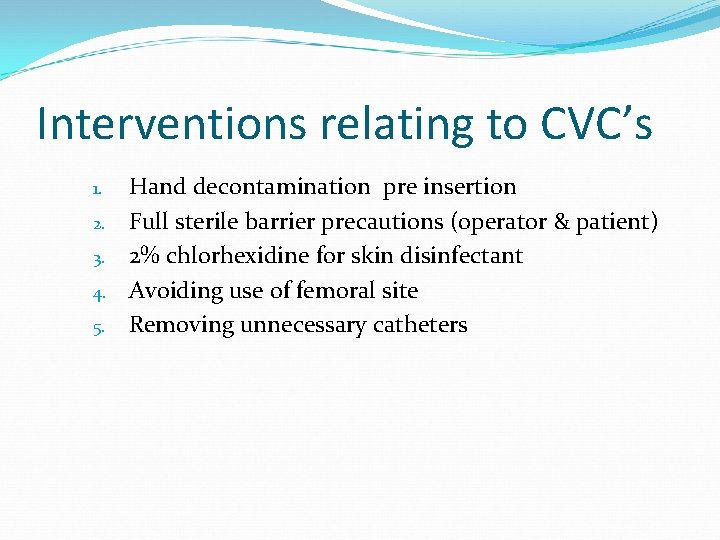
Background to Care Bundles Dr. Peter Pronovost is accredited with developing the 1 st Care Bundle – insertion and management of CVC’s Intensivist in a hospital in Michigan Developed a checklist for insertion and management of CVC’s to ensure that key interventions recommended by the CDC 2002 guidelines were implemented every time a CVC was inserted
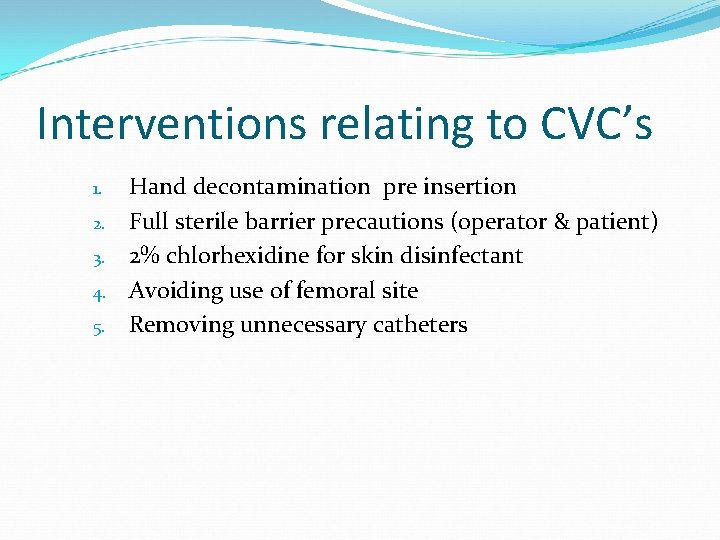
Interventions relating to CVC’s 1. 2. 3. 4. 5. Hand decontamination pre insertion Full sterile barrier precautions (operator & patient) 2% chlorhexidine for skin disinfectant Avoiding use of femoral site Removing unnecessary catheters
Results 103 ITU’s in 67 hospitals data was included in the study results Medium rate of catheter-related blood stream infections per 1000 catheter days decreased from 2. 7 at baseline to 0 at 3 months after implementation 67% reduction in catheter related blood stream infections over the 18 months
Types of Care Bundles WHO Surgery Safety Checklist Urinary Catheter Care Bundle Insertion and Management Clostridium difficile care bundle Ventilator assisted Pneumonia care bundle Palliative care bundle Pressure area care bundle Sepsis care bundle PVC care Bundle
2020/11/2
Critical care: the future In 2010 Halpern and Pastores in USA 4% decrease hospital beds, ICU beds increased by 7%. Non-ICU inpatient days increased by 5%, but ICU inpatient days increased by 10%. Annual critical care medicine costs : increased 44%, the proportion of hospital costs and national health expenditures allocated to critical care medicine decreased by 1. 6% and 1. 8% Crit Care Med 2010, 38: 65 -71

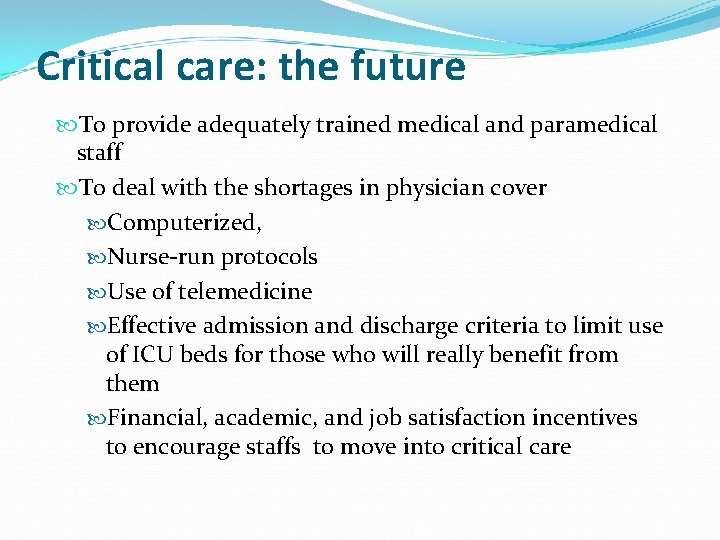
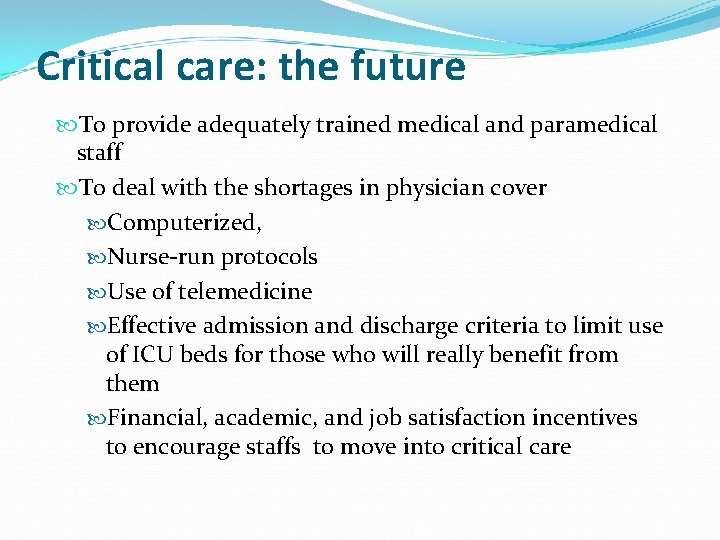
Critical care: the future To provide adequately trained medical and paramedical staff To deal with the shortages in physician cover Computerized, Nurse-run protocols Use of telemedicine Effective admission and discharge criteria to limit use of ICU beds for those who will really benefit from them Financial, academic, and job satisfaction incentives to encourage staffs to move into critical care

2020/11/2
2020/11/2
Clinical pharmacists Getting started (set the scene) One sentence for this patient Age, gender, occupation, presentation, duration Major past medical histories Major events and treatment
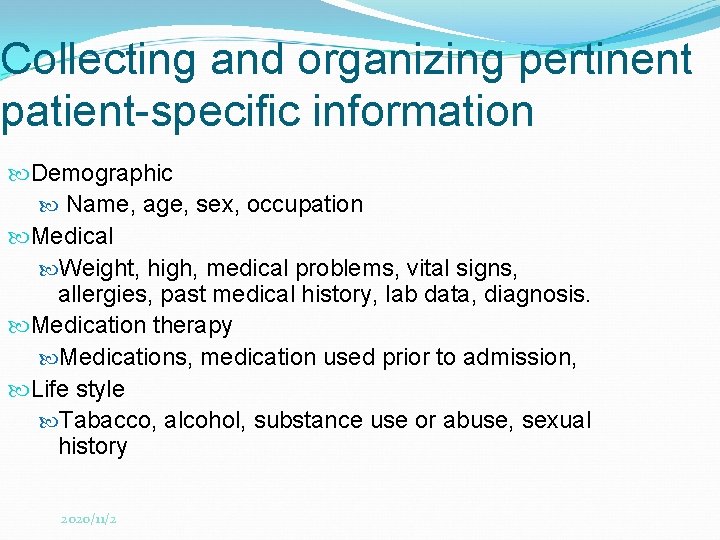
Collecting and organizing pertinent patient-specific information Demographic Name, age, sex, occupation Medical Weight, high, medical problems, vital signs, allergies, past medical history, lab data, diagnosis. Medication therapy Medications, medication used prior to admission, Life style Tabacco, alcohol, substance use or abuse, sexual history 2020/11/2
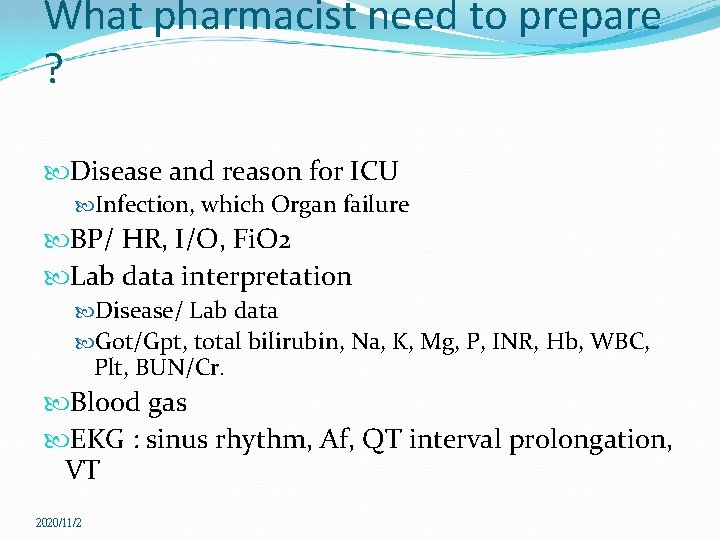
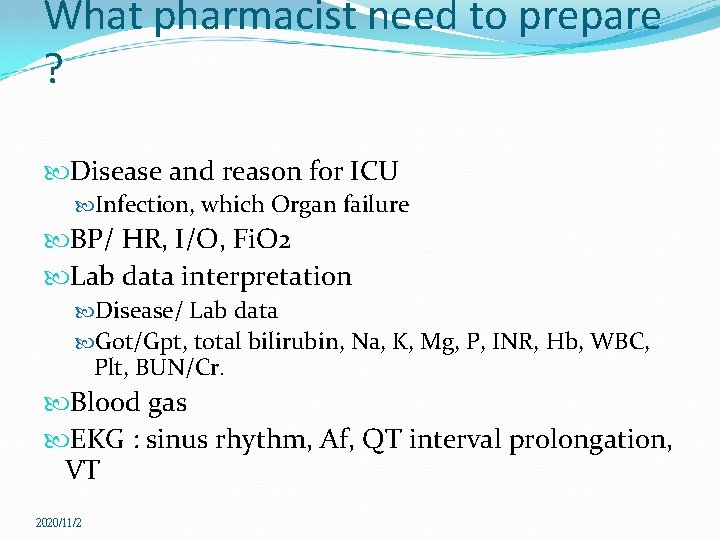
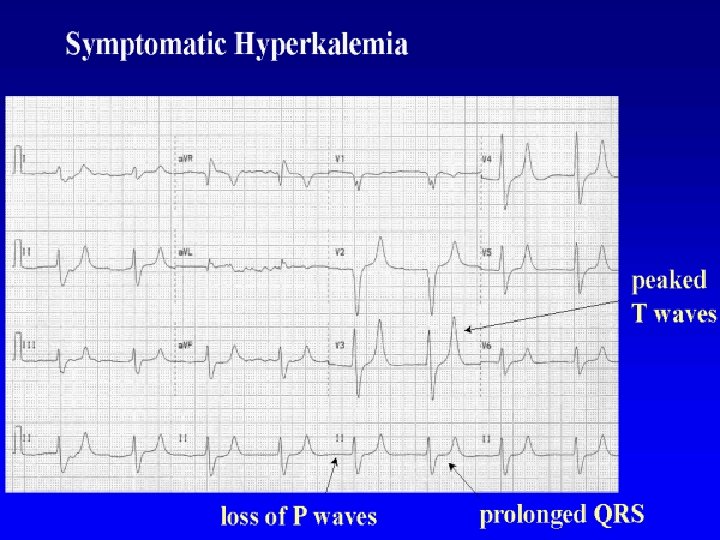
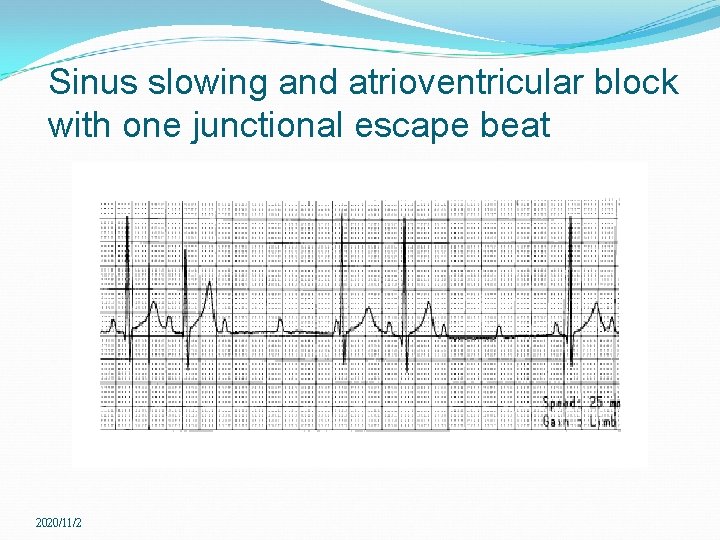
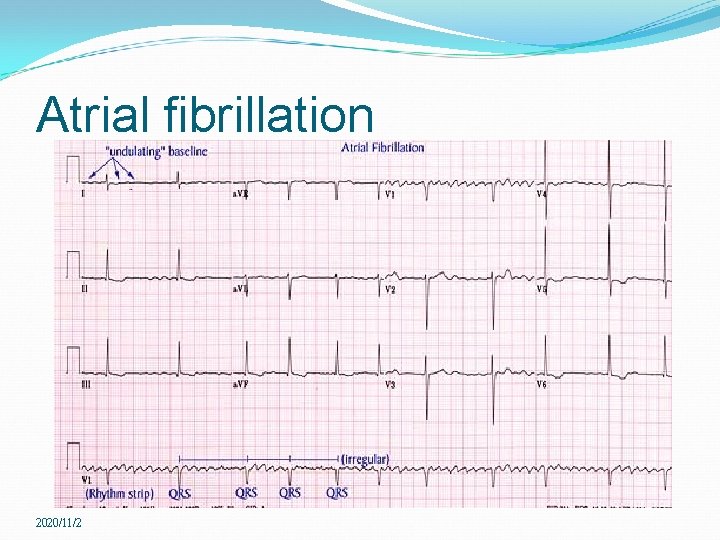
What pharmacist need to prepare ? Disease and reason for ICU Infection, which Organ failure BP/ HR, I/O, Fi. O 2 Lab data interpretation Disease/ Lab data Got/Gpt, total bilirubin, Na, K, Mg, P, INR, Hb, WBC, Plt, BUN/Cr. Blood gas EKG : sinus rhythm, Af, QT interval prolongation, VT 2020/11/2
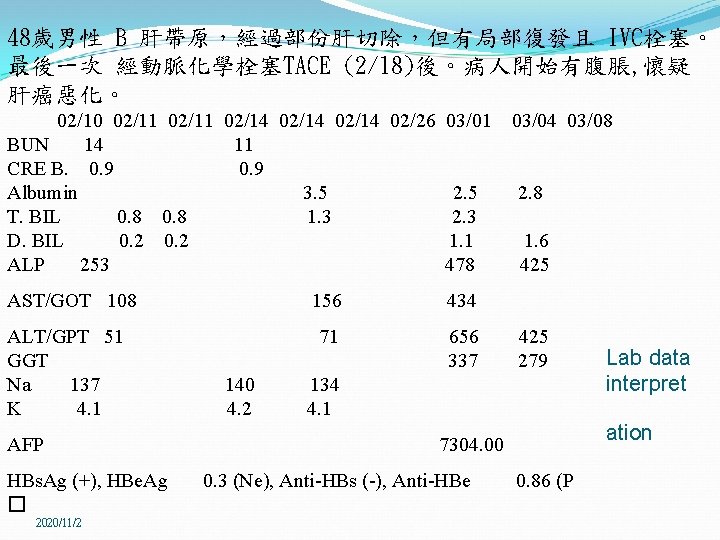
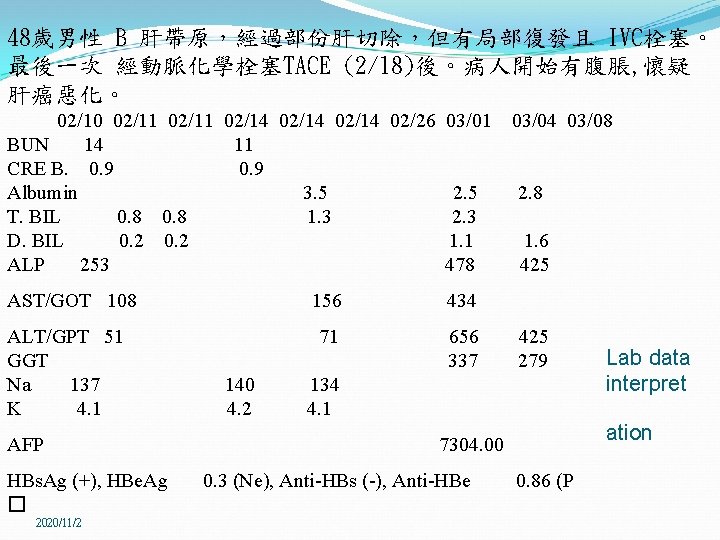
48歲男性 B 肝帶原,經過部份肝切除,但有局部復發且 IVC栓塞。 最後一次 經動脈化學栓塞TACE (2/18)後。病人開始有腹脹, 懷疑 肝癌惡化。 02/10 02/11 02/14 02/26 03/01 03/04 03/08 BUN 14 11 CRE B. 0. 9 0. 9 Albumin 3. 5 2. 5 2. 8 T. BIL 0. 8 1. 3 2. 3 D. BIL 0. 2 1. 1 1. 6 ALP 253 478 425 AST/GOT 108 156 434 ALT/GPT 51 71 656 425 Lab data GGT 337 279 interpret Na 137 140 134 K 4. 1 4. 2 4. 1 AFP 7304. 00 HBs. Ag (+), HBe. Ag 0. 3 (Ne), Anti-HBs (-), Anti-HBe 0. 86 (P � 2020/11/2 ation
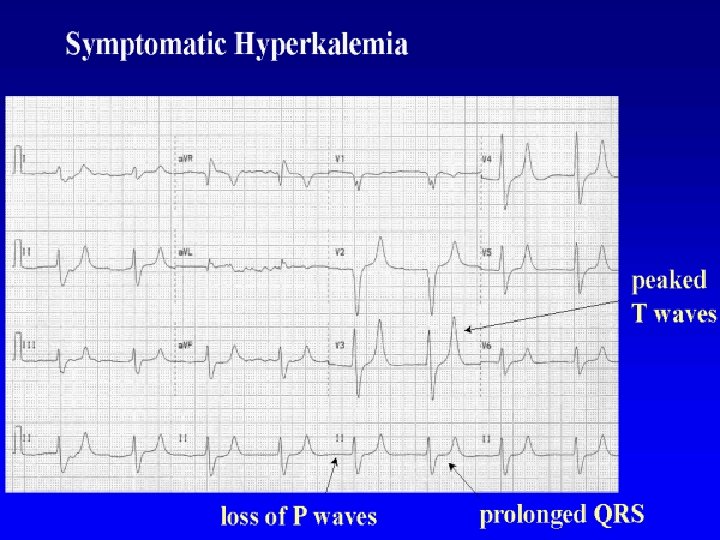
Hyperkalemia 2020/11/2
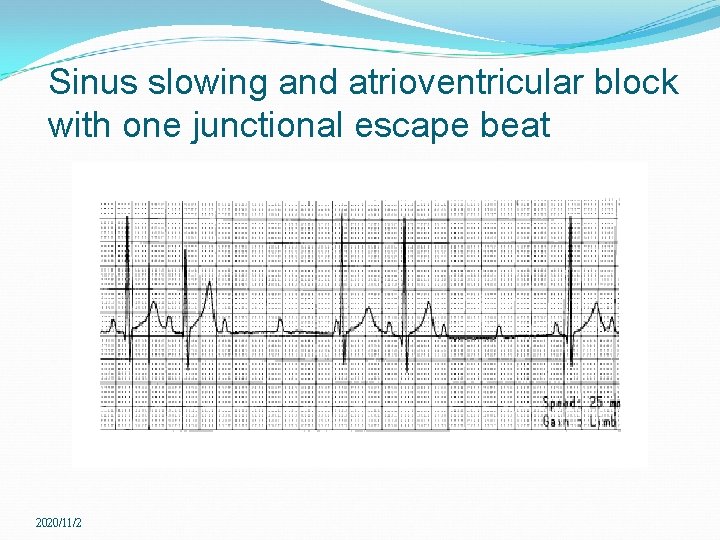
Sinus slowing and atrioventricular block with one junctional escape beat 2020/11/2
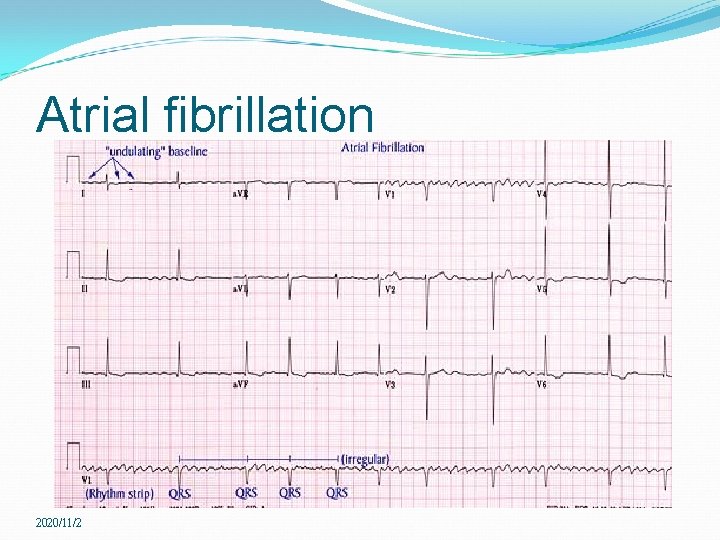
Atrial fibrillation 2020/11/2
Active problems ? Forming a hypothesis Looking for supportive evidence Management and intervention A dynamic feedback loop !
Apply parameters ! Vitals (TPR) Sp 02, EKG monitor, Swan-Ganz catheter I & O, diets, fluids, transfusions Lines, tubes & ostomies Medications Ventilator setting Blood tests Image
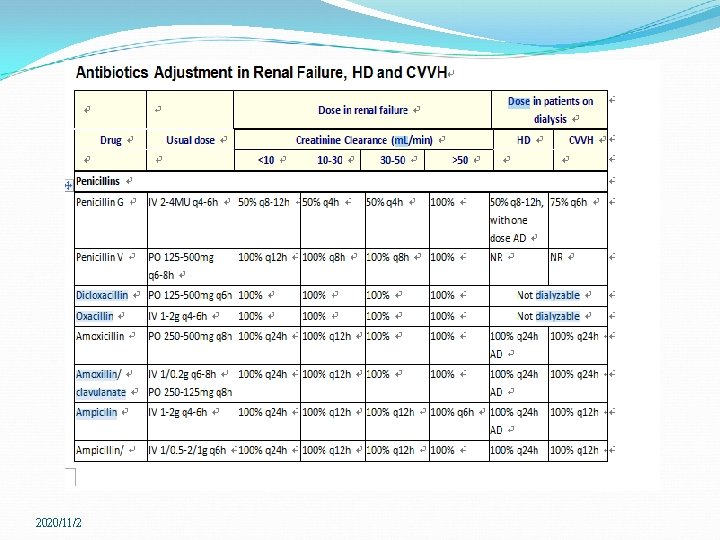
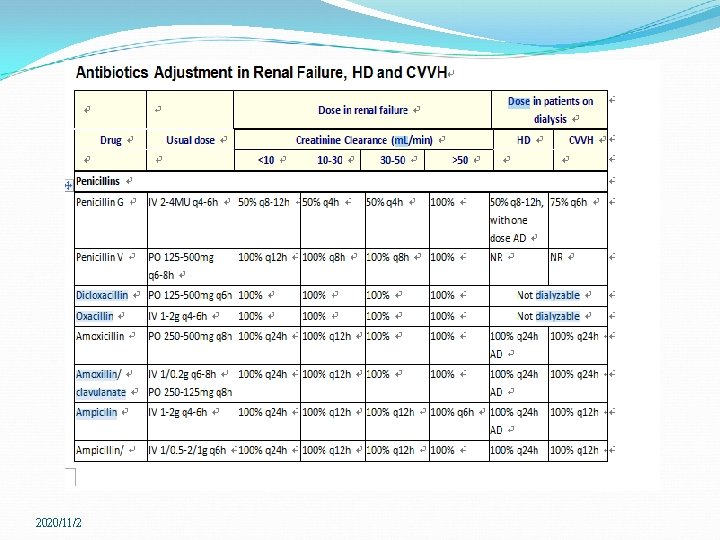
Checklist Pain control (morphine, NSAIDs) Intensive Care Unit Sedation Protocol Sepsis campaign Pressors (dopamine, norepinephrine), fluid (albumin, N/S), steroid (hydrocortisone dose, when to give), antibiotics (how to choose) Stress ulcer prophylaxis ( who is candidate? ) Sugar control ( <150 mg/dl, <200 mg/dl) Drug adjustment Renal , liver impairment ADR 2020/11/2
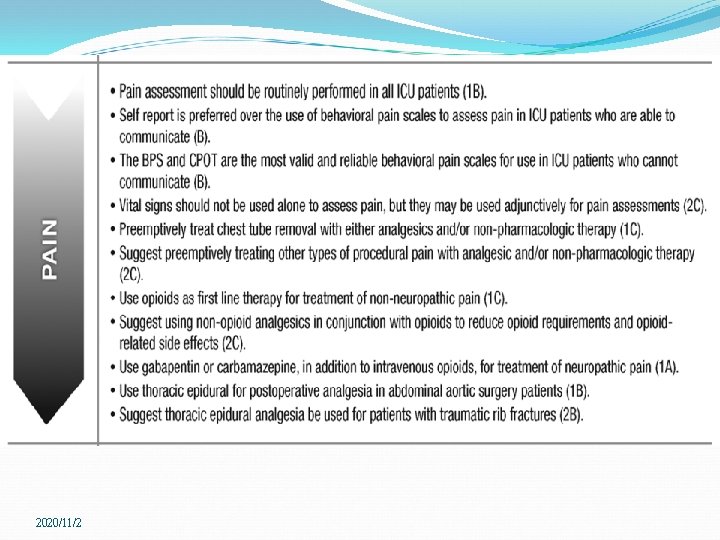
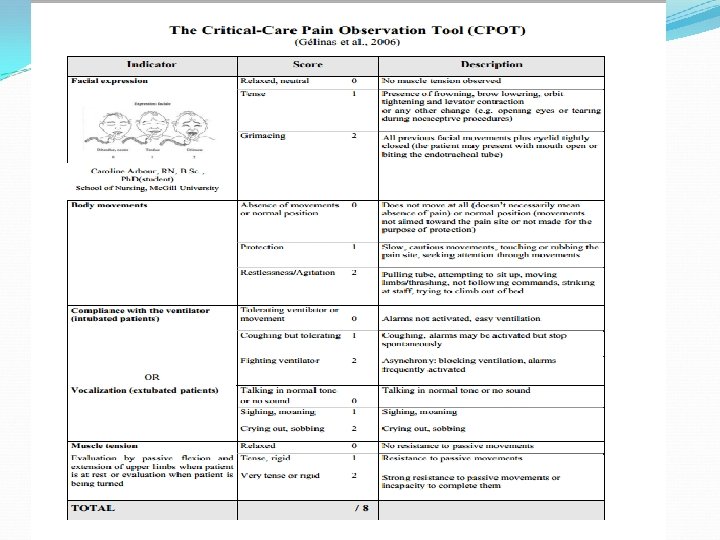
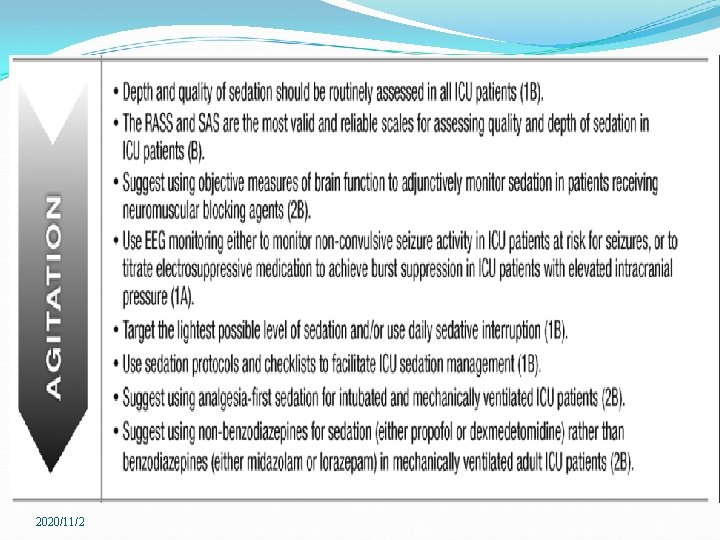
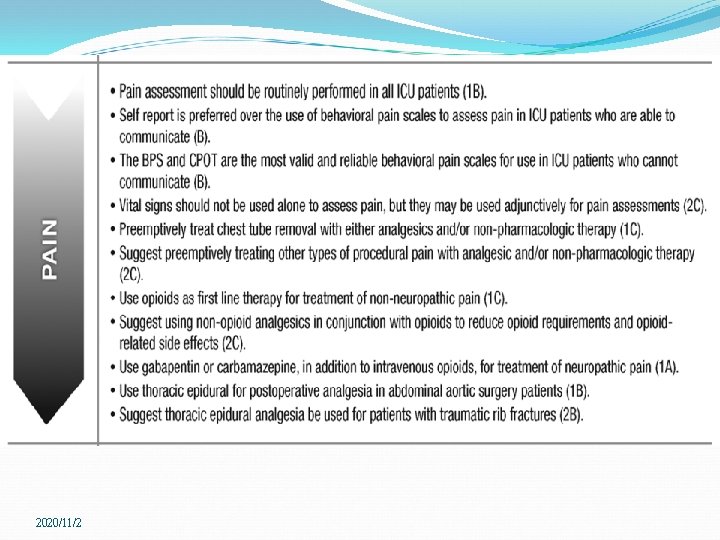
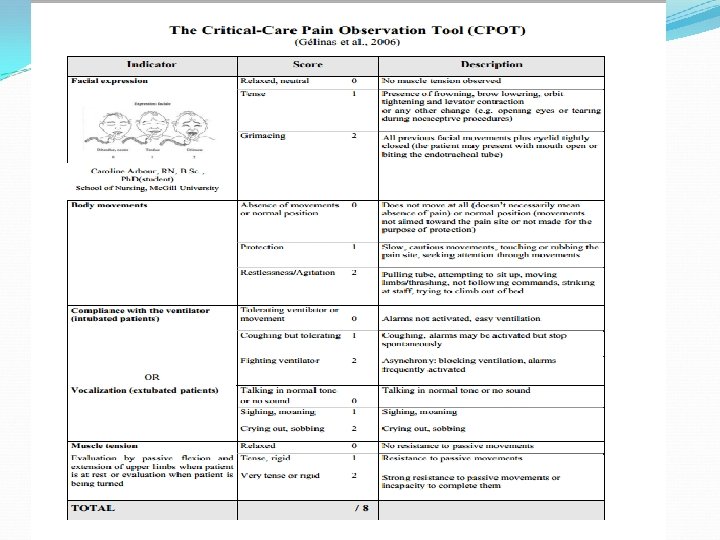
Sedation and Analgesia Crit Care Med 2013; 41: 263– 306 The Society of Critical Care Medicine(SCCM)and the American College of critical care medicine( ACCM)in 1995 published clinical practice guideline for sedation and analgesia for the critically ill patients. ACCM and SCCM have joined with ASHP to develop new clinical practice guidelines in 2002 The recommendations were graded according to the strength and quality of the scientific evidence. “pain, agitation, and delirium” (PAD) guidelines
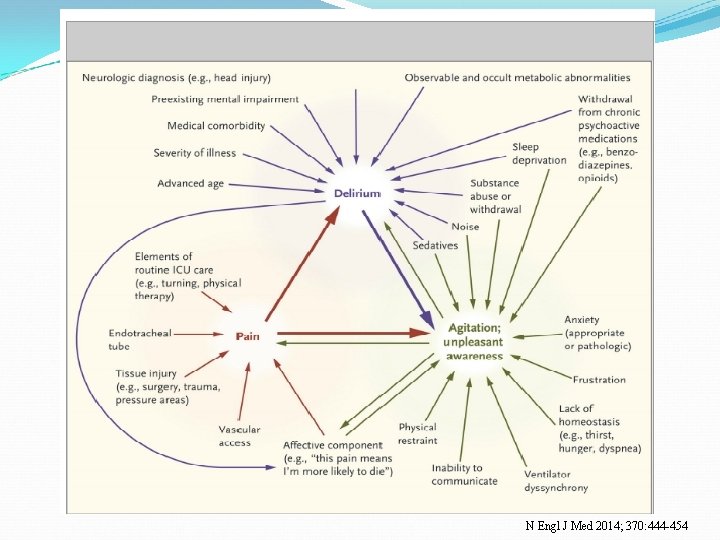
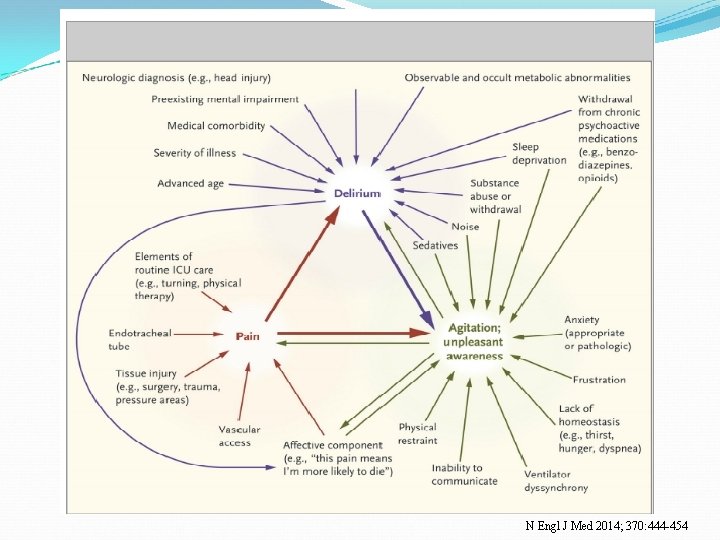
N Engl J Med 2014; 370: 444 -454
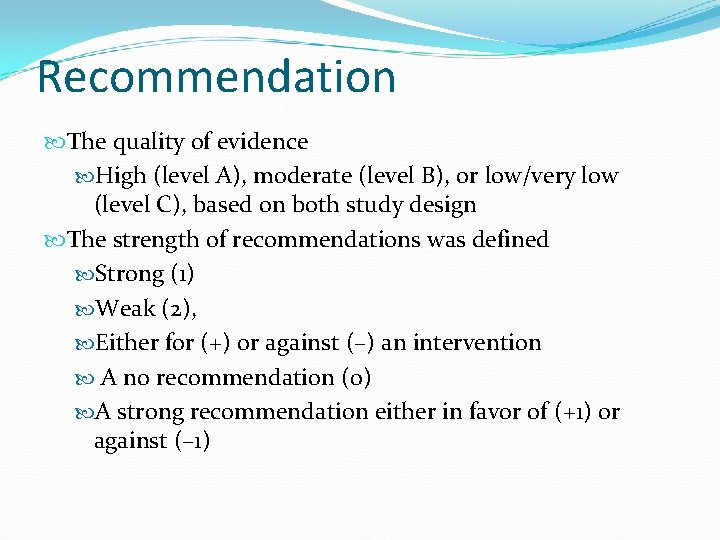
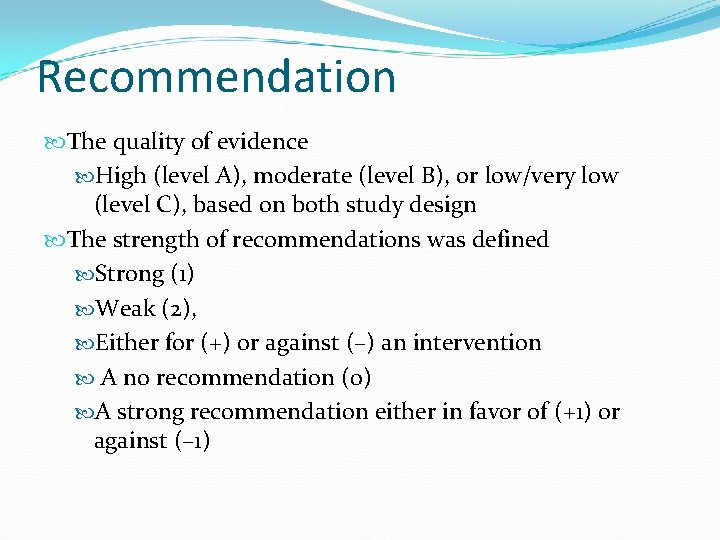
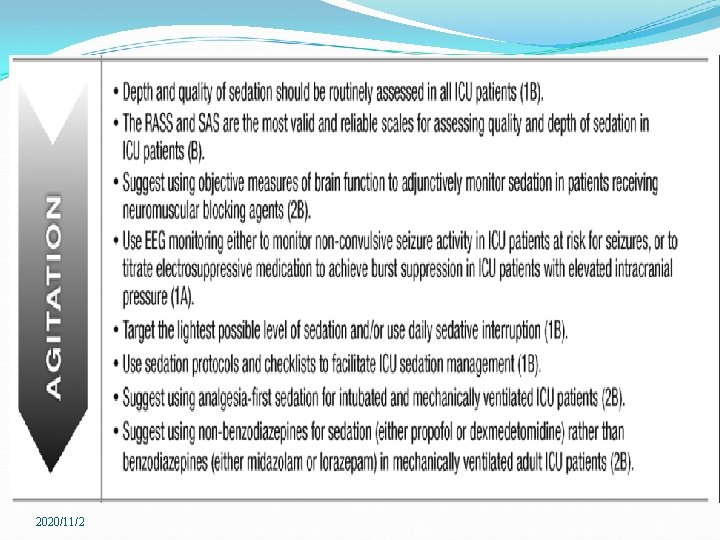
Recommendation The quality of evidence High (level A), moderate (level B), or low/very low (level C), based on both study design The strength of recommendations was defined Strong (1) Weak (2), Either for (+) or against (–) an intervention A no recommendation (0) A strong recommendation either in favor of (+1) or against (– 1)
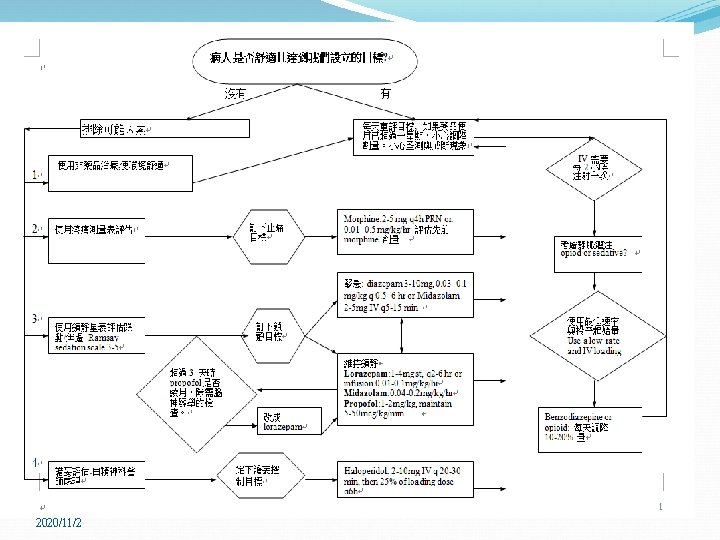
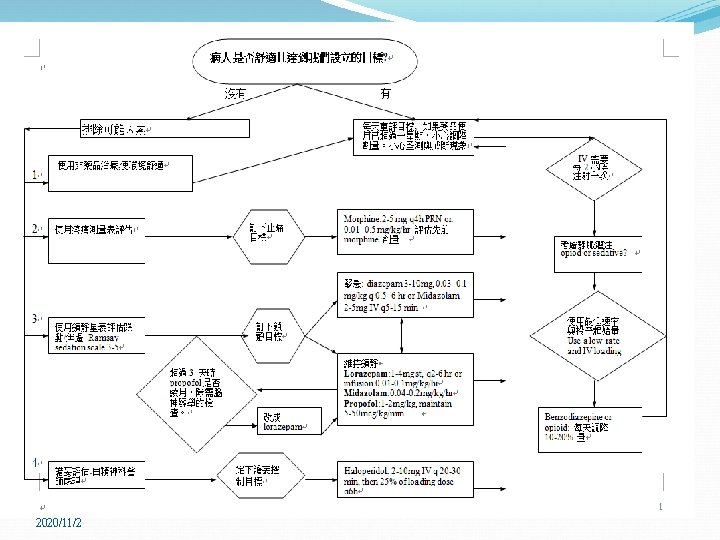
ICU 病房的止痛與鎮靜 目的: 不痛 使病人在半睡半醒中,保持安靜與放鬆狀態. 止痛劑(analgesia) Morphine 是最好的選擇。 Meperidine (no more than 48 hrs or dose>600 mg/24 hrs): metabolize to normeperidine. Contraindication 1. renal impairment 2. MAOI. Duration of the morphine and meperidine : 3 -4 hrs.
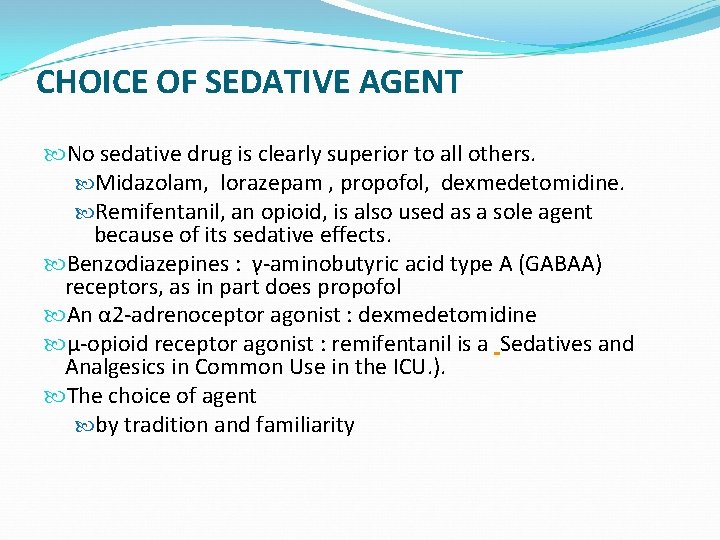
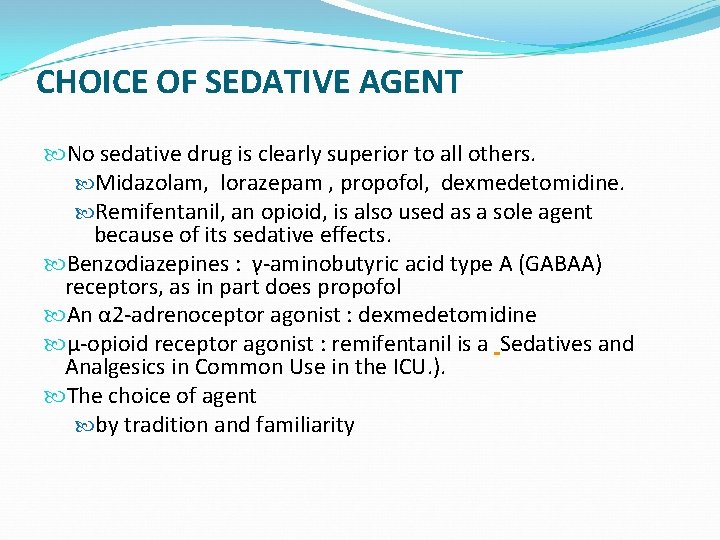
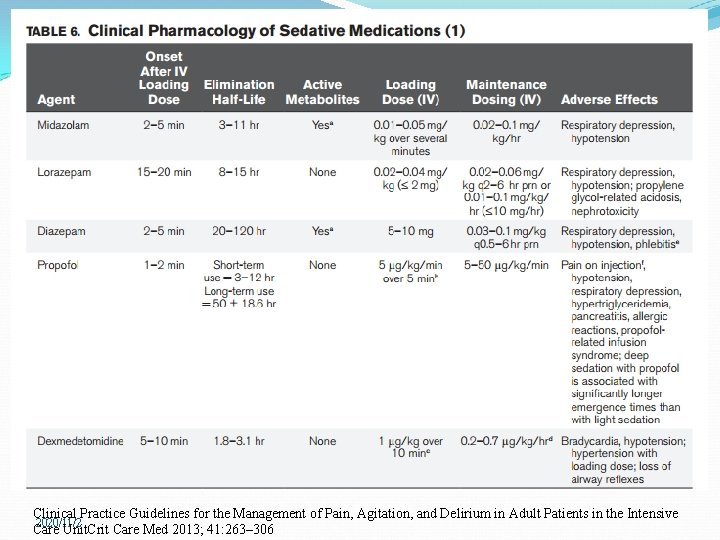
CHOICE OF SEDATIVE AGENT No sedative drug is clearly superior to all others. Midazolam, lorazepam , propofol, dexmedetomidine. Remifentanil, an opioid, is also used as a sole agent because of its sedative effects. Benzodiazepines : γ-aminobutyric acid type A (GABAA) receptors, as in part does propofol An α 2 -adrenoceptor agonist : dexmedetomidine μ-opioid receptor agonist : remifentanil is a Sedatives and Analgesics in Common Use in the ICU. ). The choice of agent by tradition and familiarity

CHOICE OF SEDATIVE AGENT For rapidly adjusted : propofol or remifentanil Propofol vs BZD : reduction in the length of stay in the ICU. Dexmedetomidine has advantages over benzodiazepines analgesia, less respiratory depression, more interactive to communicate their needs. Less delirium and a shorter duration of mechanical ventilation not reduced stays in the ICU or hospital. Remifentanil : T 1/2 3 to 4 minutes that is independent of the infusion duration or organ function. Surgical patients in ICU Small trials Not a common choice in most ICUs.
2020/11/2
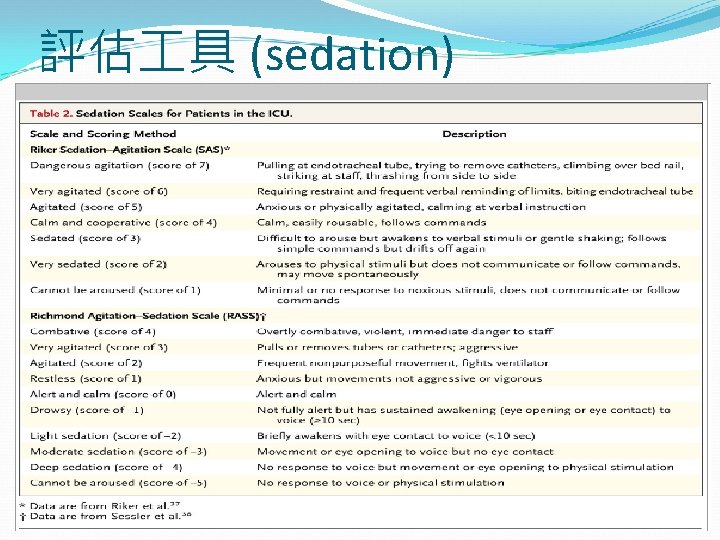
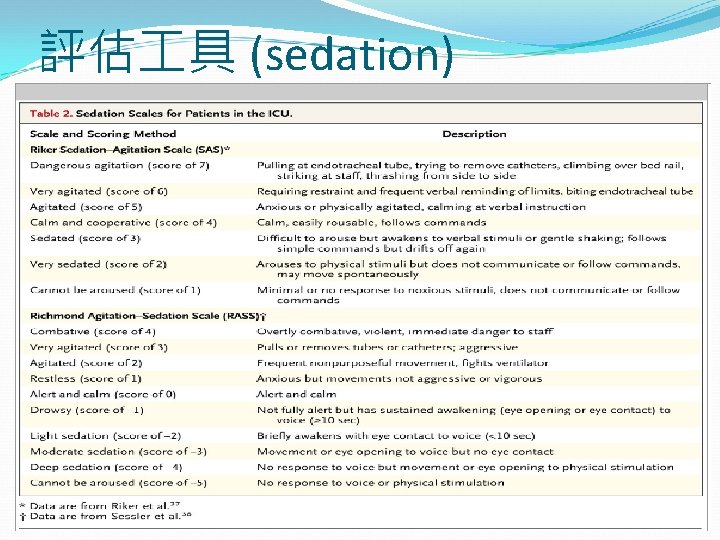
評估 具 (sedation)
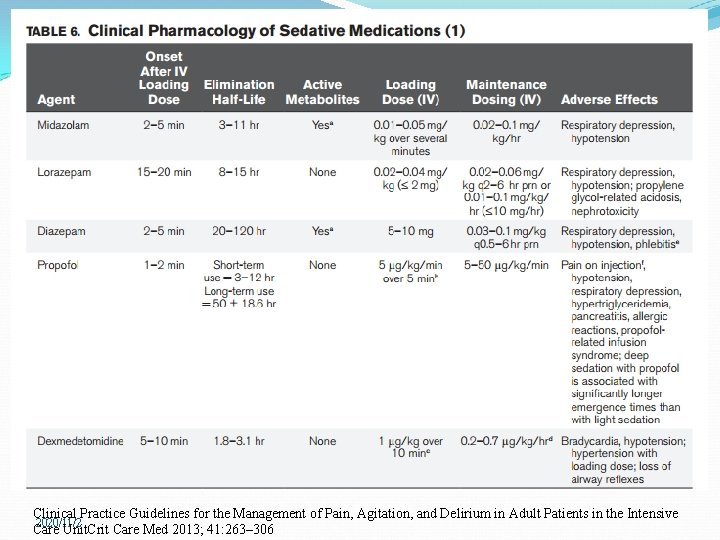
Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intensive 2020/11/2 Care Unit. Crit Care Med 2013; 41: 263– 306
ICU 病房的鎮靜藥物使用 Propofol 用於BZA (lorazepam)無法成功鎮靜的病人。as a last resort for patients not successfully sedated with high dose lorazepam (>20 mg/h or >240 mg/day, morphine, and haloperidol. 限住加護病房使用人 呼吸器治療且需要每日進行 神智評估之病例使用。 每日劑量 10 -25 amps,每次使用以不超過72小時為 原則。 不得作為例如性使用。
Propofol 主要用於鎮靜安眠,但也有抗癲癇與輕微失 憶作用。 高脂溶性,開始作用速度快 (< 1 minute)與停藥快速恢 復。經肝臟 conjugation 成為不活性代謝物, 再經腎臟 排除。 肝腎功能不全並不影響藥物排除。 抗嘔吐作用 : short duration of action. 副作用 : 低血壓 ( especially a bolus dose) 重要問題 propofol is prepared in a solution of soybean oil, glycerol, and purified egg phosphatide. ( sepsis and death) 呼吸與心臟. (Apnea and hypotension )
Propofol 輸注時間超過 24到 48 hrs hypertriglyceridemia, pancreatitis, increased carbon dioxide production, and an excessive caloric load (the emulsion contains approximately 1. 1 kcal/m. L). 藥廠建議每 12小時丟棄針筒(Tube ) 5個案報告 “ propofol 增加兒童死亡率. 漸進式代謝性酸中毒, bradyarrhythmia, 心臟衰竭, 急救反應無效. propofol 不建議用於兒童
ICU 病房的鎮靜藥物使用 Lorazepam 用於所有 ICU 病人,使用鎮靜時間超過24小時 (starting dose=2 -4 mg iv q 1 -4 hrs) 如果插管超過24 小時,可考慮將 midazolam 轉換成 lorazepam。. Intermittent iv bolus administration is preferred. (no maximum dose) Midazolam 限於會在 24小時內拔管病人 (starting dose =1 -2 mg iv every 1 -2 hrs) 用於短期的鎮靜。

2020/11/2
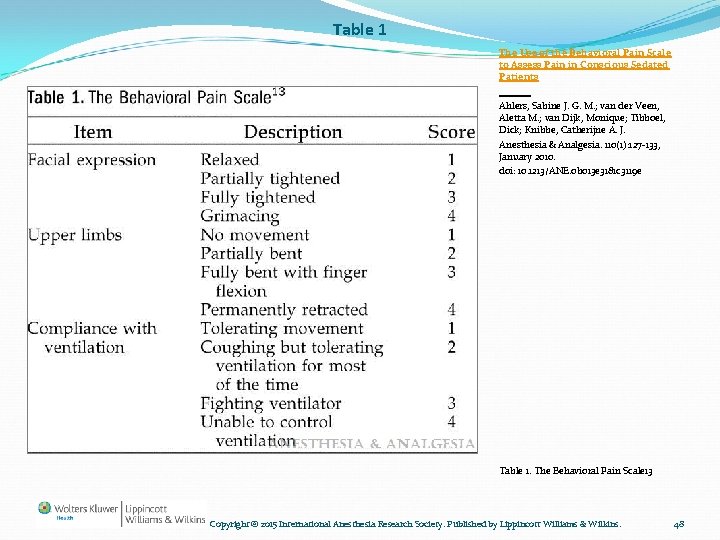
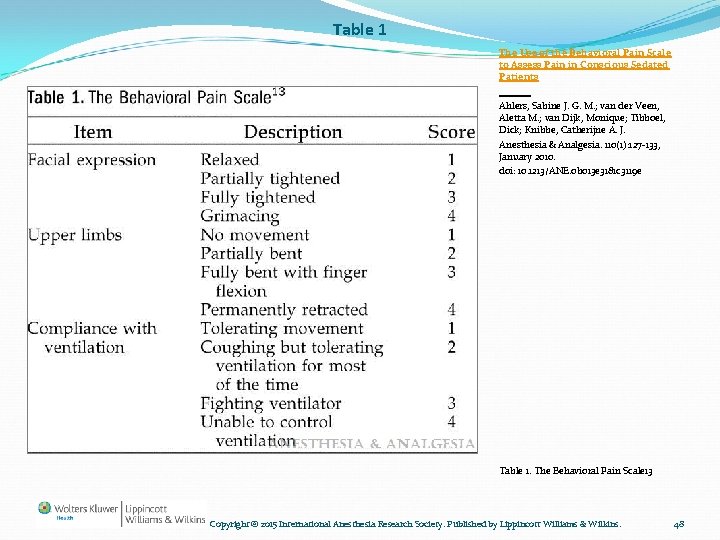
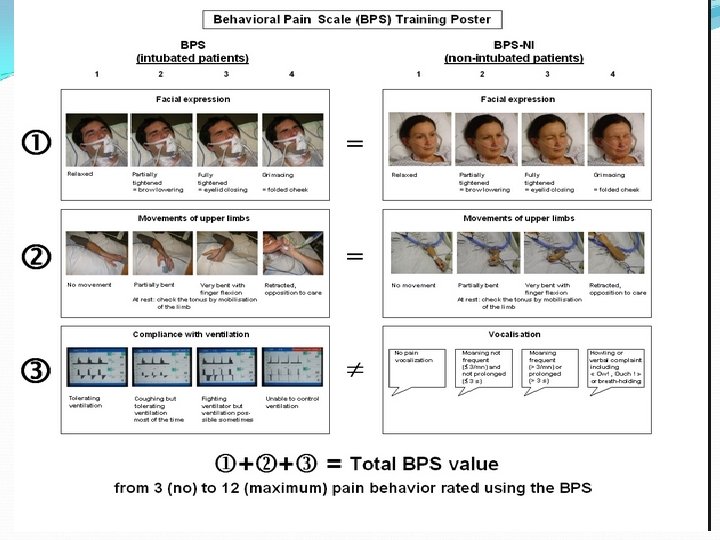
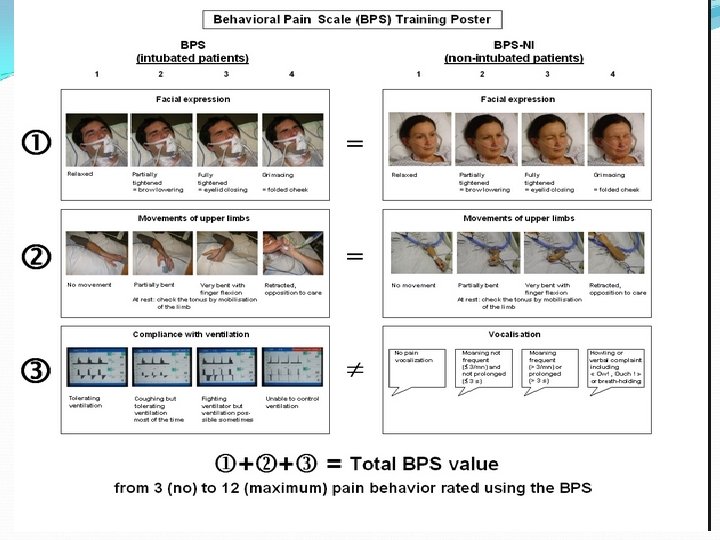
Table 1 The Use of the Behavioral Pain Scale to Assess Pain in Conscious Sedated Patients Ahlers, Sabine J. G. M. ; van der Veen, Aletta M. ; van Dijk, Monique; Tibboel, Dick; Knibbe, Catherijne A. J. Anesthesia & Analgesia. 110(1): 127 -133, January 2010. doi: 10. 1213/ANE. 0 b 013 e 3181 c 3119 e Table 1. The Behavioral Pain Scale 13 Copyright © 2015 International Anesthesia Research Society. Published by Lippincott Williams & Wilkins. 48
2020/11/2
2020/11/2

Analgesia therapy(Opiates) *Pharmacology of selected IV analgesics Drug Active Equiv. metabol Dose(m ites g) onset Halflife (hr) 1. 5~6 Dosage Fentanyl N 0. 2 1 -2 min Hydromorphone N 1. 5 5 -15 min 2~3 10~30 mcg/kg, q 1~2 h 7~15 mcg/kg/hr Morphine Y 10 5 -10 min 3~7 0. 01~0. 15 mg/kg, q 1~2 h 0. 07~0. 5 mg/kg/hr Ramifentanil N 1 -3 min 3~4 min 1. 5 mcg/kg IV loading 0. 15 -15 mcg/kg/hr 1 -2 h 15~29 Not recommended (0. 1 mg/kg, q 6~12 h) (hydrolysis in plasma) Methadone Y Unit. Crit Care Med 2013; 41: 263– 306 7. 5~10 0. 35~1. 5 mcg/kg, q 0. 5~1 h 0. 1~10 mcg/kg/hr
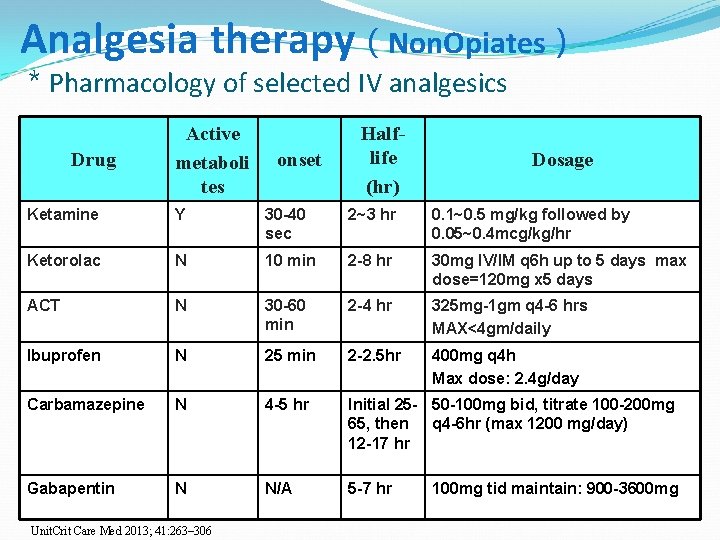
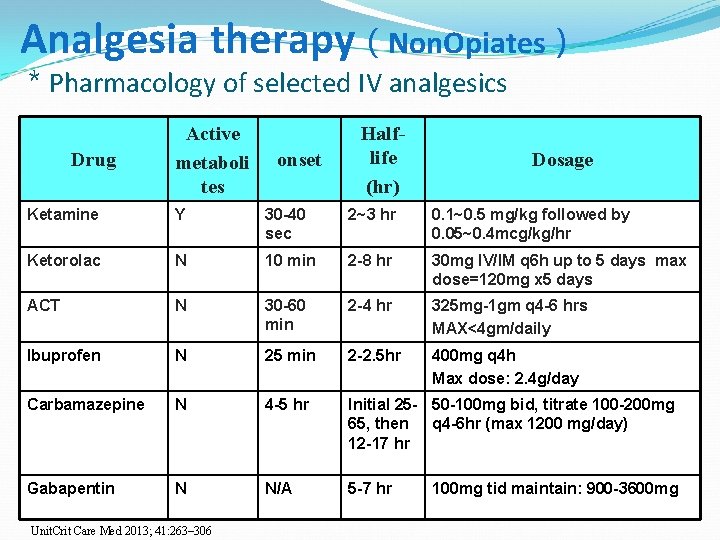
Analgesia therapy(Non. Opiates) *Pharmacology of selected IV analgesics Drug Active metaboli tes onset Halflife (hr) Dosage Ketamine Y 30 -40 sec 2~3 hr 0. 1~0. 5 mg/kg followed by 0. 05~0. 4 mcg/kg/hr Ketorolac N 10 min 2 -8 hr 30 mg IV/IM q 6 h up to 5 days max dose=120 mg х5 days ACT N 30 -60 min 2 -4 hr 325 mg-1 gm q 4 -6 hrs MAX<4 gm/daily Ibuprofen N 25 min 2 -2. 5 hr 400 mg q 4 h Max dose: 2. 4 g/day Carbamazepine N 4 -5 hr Initial 25 - 50 -100 mg bid, titrate 100 -200 mg 65, then q 4 -6 hr (max 1200 mg/day) 12 -17 hr Gabapentin N N/A 5 -7 hr Unit. Crit Care Med 2013; 41: 263– 306 100 mg tid maintain: 900 -3600 mg

Haloperidol vs olanzapine showed equivalent dexmedetomidine : a more rapid resolution of delirium versus 2020/11/2 midazolam
2020/11/2

2020/11/2

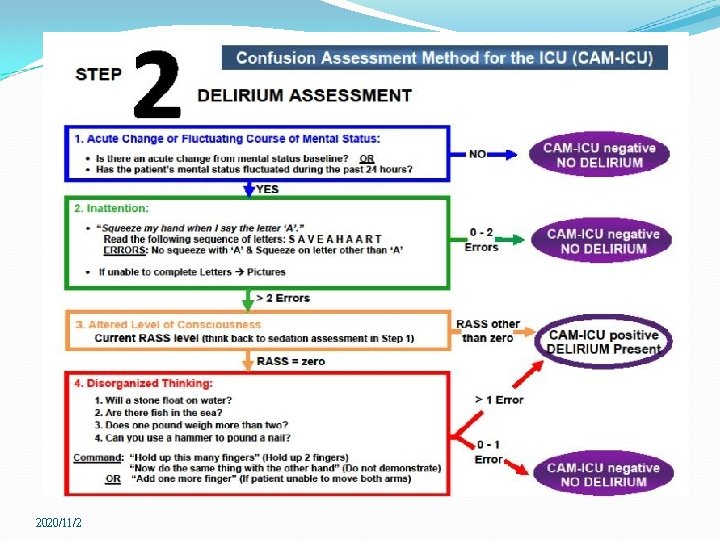
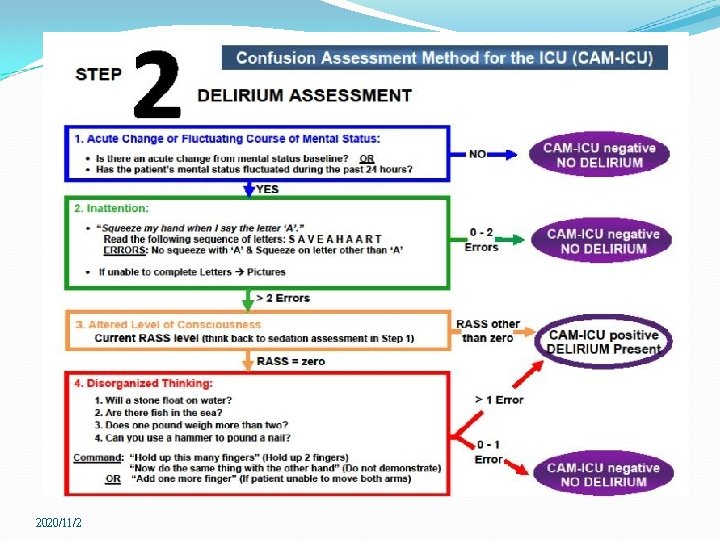
PREVENTION AND TREATMENT OF DELIRIUM (DSM-IV) : Delirium Disturbance of consciousness Change in cognition, Development over a short period Fluctuation Delirium defined by NIH “sudden severe confusion and rapid changes in brain function that occur with physical or mental illness. ” The most common feature of delirium cardinal sign, inattention. reversible manifestation of acute illness , including recovery from a sedated or oversedated state.
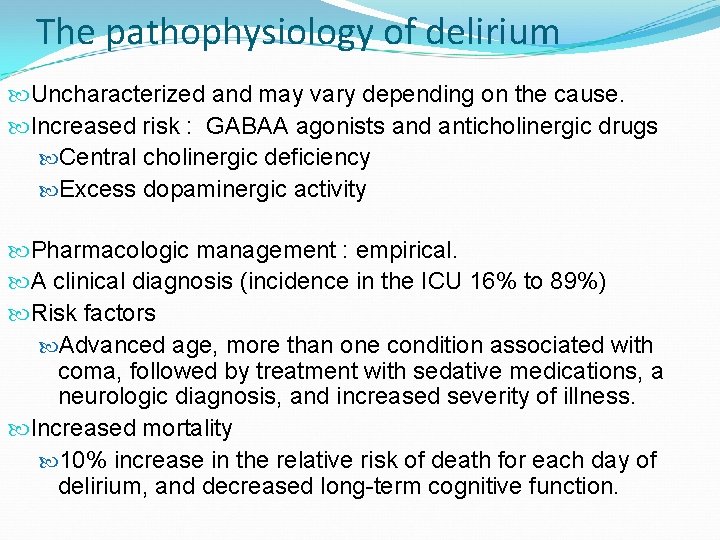
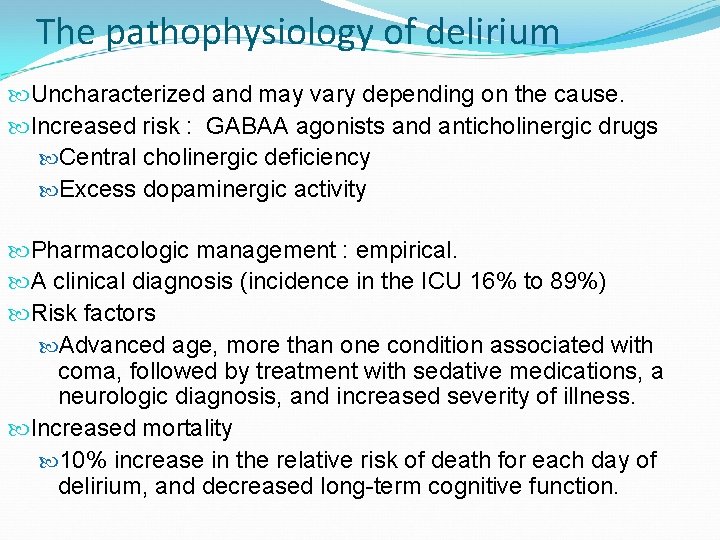
The pathophysiology of delirium Uncharacterized and may vary depending on the cause. Increased risk : GABAA agonists and anticholinergic drugs Central cholinergic deficiency Excess dopaminergic activity Pharmacologic management : empirical. A clinical diagnosis (incidence in the ICU 16% to 89%) Risk factors Advanced age, more than one condition associated with coma, followed by treatment with sedative medications, a neurologic diagnosis, and increased severity of illness. Increased mortality 10% increase in the relative risk of death for each day of delirium, and decreased long-term cognitive function.
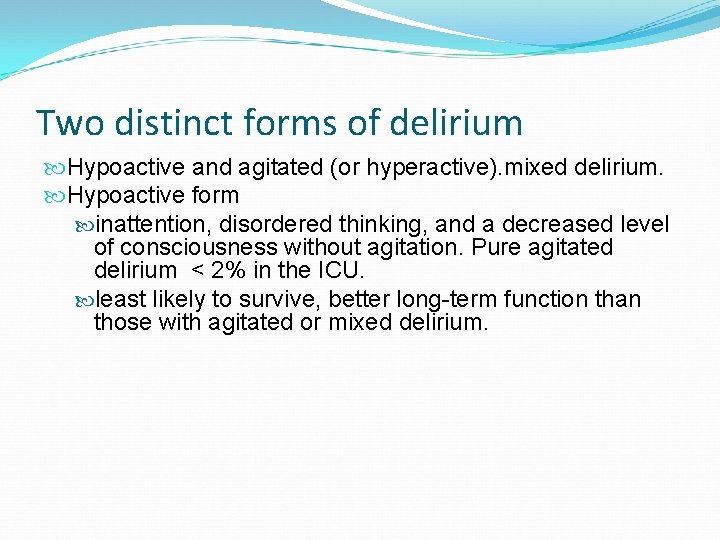
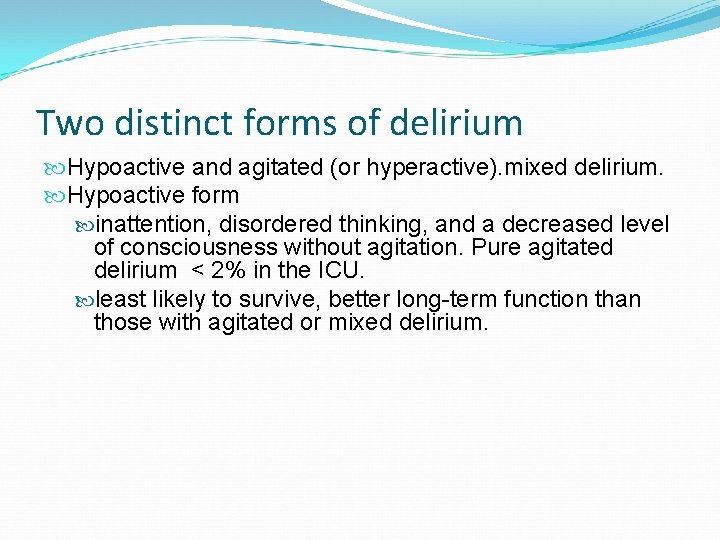
Two distinct forms of delirium Hypoactive and agitated (or hyperactive). mixed delirium. Hypoactive form inattention, disordered thinking, and a decreased level of consciousness without agitation. Pure agitated delirium < 2% in the ICU. least likely to survive, better long-term function than those with agitated or mixed delirium.
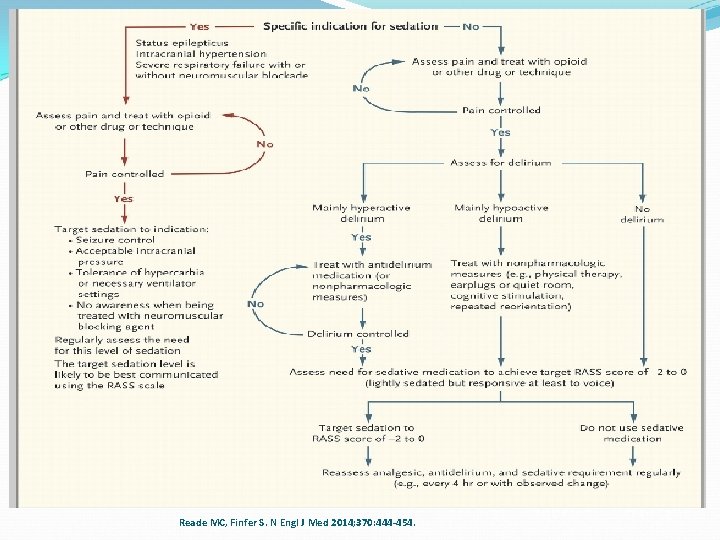
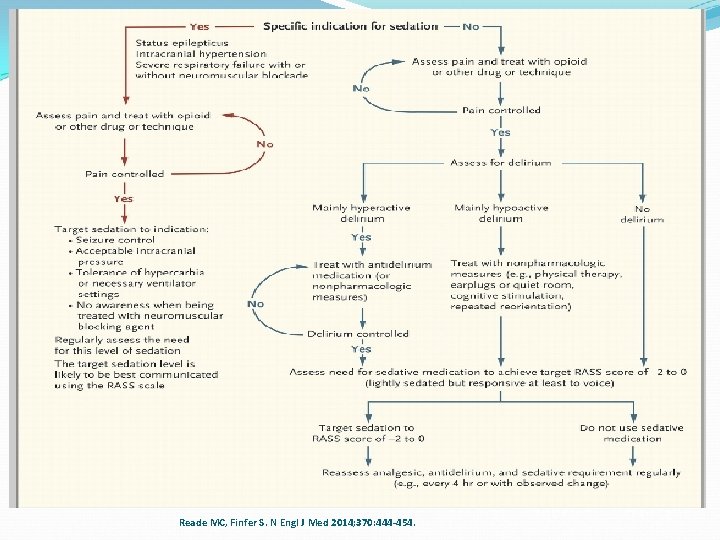
Algorithm for the Coordinated Management of Pain, Agitation, and Delirium. Reade MC, Finfer S. N Engl J Med 2014; 370: 444 -454.
2020/11/2
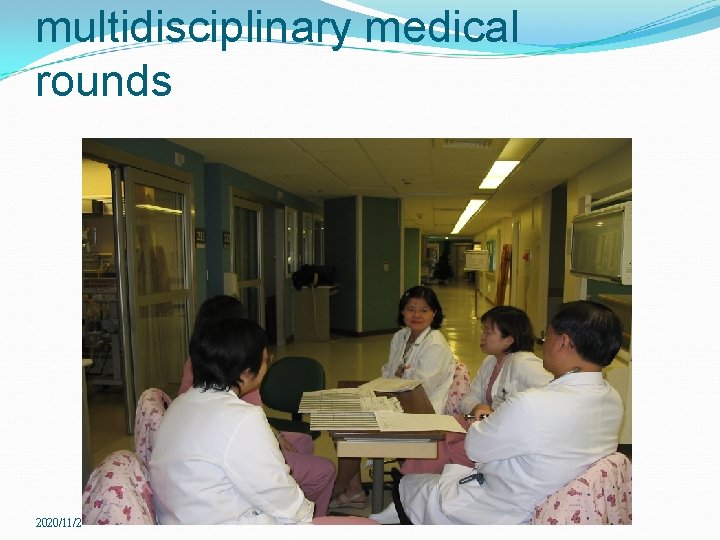
multidisciplinary medical rounds 2020/11/2
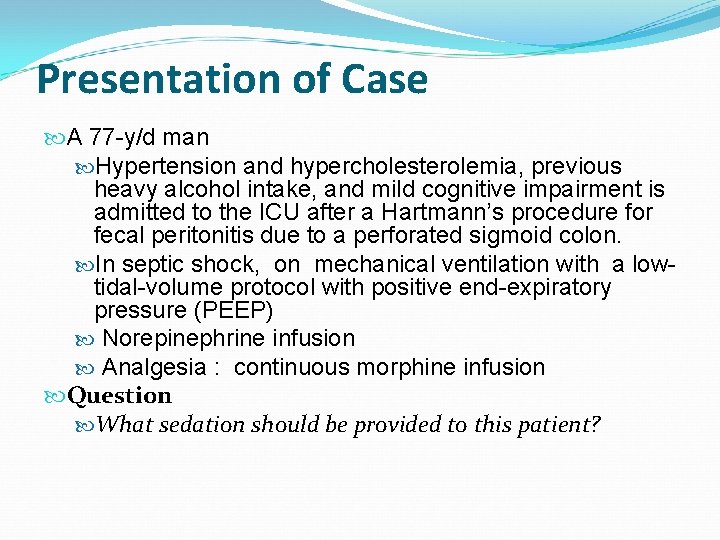
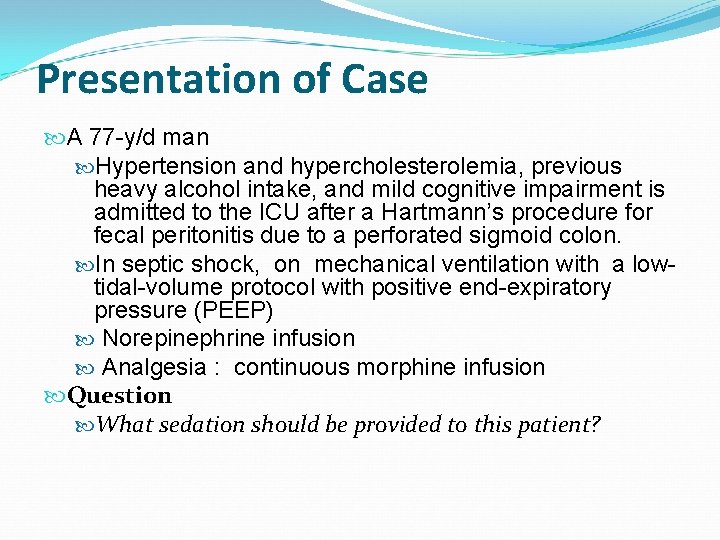
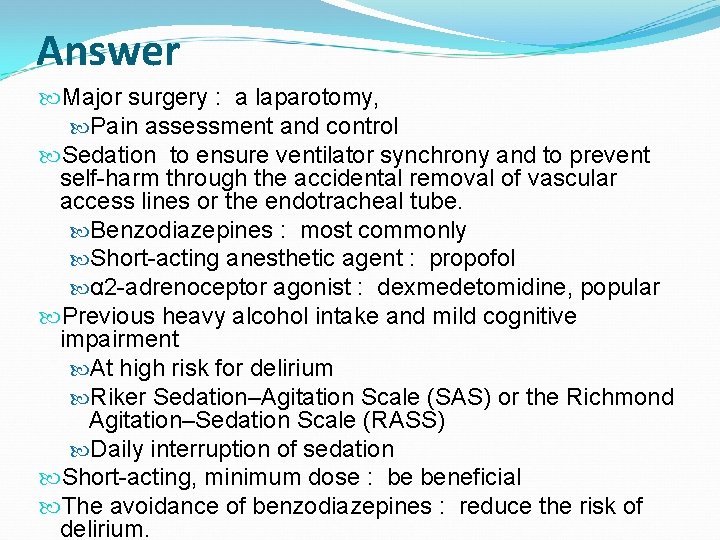
Presentation of Case A 77 -y/d man Hypertension and hypercholesterolemia, previous heavy alcohol intake, and mild cognitive impairment is admitted to the ICU after a Hartmann’s procedure for fecal peritonitis due to a perforated sigmoid colon. In septic shock, on mechanical ventilation with a lowtidal-volume protocol with positive end-expiratory pressure (PEEP) Norepinephrine infusion Analgesia : continuous morphine infusion Question What sedation should be provided to this patient?
Answer Major surgery : a laparotomy, Pain assessment and control Sedation to ensure ventilator synchrony and to prevent self-harm through the accidental removal of vascular access lines or the endotracheal tube. Benzodiazepines : most commonly Short-acting anesthetic agent : propofol α 2 -adrenoceptor agonist : dexmedetomidine, popular Previous heavy alcohol intake and mild cognitive impairment At high risk for delirium Riker Sedation–Agitation Scale (SAS) or the Richmond Agitation–Sedation Scale (RASS) Daily interruption of sedation Short-acting, minimum dose : be beneficial The avoidance of benzodiazepines : reduce the risk of delirium.
Thanks for listening May start your ICU pharmaceuti cal service ! www. sylvianickerson. ca
 Meaning of clinical pharmacy
Meaning of clinical pharmacy Clinical pharmacist job description
Clinical pharmacist job description End of life care in icu
End of life care in icu Pharmacist patient care process example
Pharmacist patient care process example Hip fracture care clinical care standard
Hip fracture care clinical care standard Poss scale vs rass scale
Poss scale vs rass scale Rikers sedation scale
Rikers sedation scale Rass sedation scale
Rass sedation scale Sédation
Sédation Richmond agitation sedation scale
Richmond agitation sedation scale Sccm padis guidelines
Sccm padis guidelines Over-sedation
Over-sedation Levels of nursing care primary secondary tertiary
Levels of nursing care primary secondary tertiary Au pharmaceutical care center
Au pharmaceutical care center Skema pharmaceutical care
Skema pharmaceutical care Pengertian pharmaceutical care
Pengertian pharmaceutical care Luyuan fang
Luyuan fang Fang din by
Fang din by W fang
W fang Wenbin fang
Wenbin fang Steven fang
Steven fang Criterios de fang
Criterios de fang Vecurium
Vecurium Steven fang
Steven fang Fang enginer
Fang enginer Fixtures and fastenings in railway
Fixtures and fastenings in railway Dr huafeng shen
Dr huafeng shen Angela fang
Angela fang Kp icu jpm
Kp icu jpm Icu orientation
Icu orientation Pressors icu
Pressors icu Escala rass
Escala rass Icu case presentation
Icu case presentation Cheetah nicom monitor
Cheetah nicom monitor Perbandingan perawat dan pasien
Perbandingan perawat dan pasien Klasifikasi pelayanan icu
Klasifikasi pelayanan icu Manitol mechanism of action
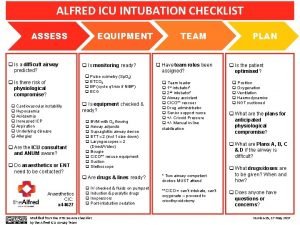
Manitol mechanism of action Alfred icu
Alfred icu Ideal icu setup
Ideal icu setup Icu for dummies
Icu for dummies Icu library
Icu library Escala de morse y braden
Escala de morse y braden Lidocaine acls
Lidocaine acls Icu transliterator
Icu transliterator Abcde methode ehbo
Abcde methode ehbo Escala sas
Escala sas Information and communication university zambia location
Information and communication university zambia location Chatecholamine
Chatecholamine List of lecturers at icu zambia
List of lecturers at icu zambia Icu layout and design
Icu layout and design Cam icu
Cam icu Types of iv fluid
Types of iv fluid Icu unicode
Icu unicode Icu medical b3108
Icu medical b3108 Intensive care unit definition
Intensive care unit definition 5hs and 5ts
5hs and 5ts Icu security group
Icu security group Icu acuity tool
Icu acuity tool Icu case presentation
Icu case presentation Cam icu escala
Cam icu escala Icu localization
Icu localization Diet chart for icu patients
Diet chart for icu patients Icu security group
Icu security group Tresiba to lantus conversion pharmacist letter
Tresiba to lantus conversion pharmacist letter My future profession pharmacist
My future profession pharmacist