NURSING MANAGEMENT OF ADULTS WITH DISORDERS OF THE
- Slides: 78
NURSING MANAGEMENT OF ADULTS WITH DISORDERS OF THE LIVER Spring 2009
TOPICS TO BE REVIEWED • • HEPATITIS CIRRHOSIS STEATOHEPATITIS (FATTY LIVER) HEPATIC ABSCESS LIVER TRAUMA CANCER OF LIVER TRANSPLANT
NORMAL FUNCTION OF LIVER MAIN FUNCTIONS OF THE LIVER: storage, protection, metabolism • Maintains normal serum glucose levels • Ammonia conversion • Protein metabolism • Fat metabolism • Vitamin and Iron storage • Drug metabolism and detoxification
LIVER FUNCTION: GLUCOSE METABOLISM • • • What happens to glucose in the liver? Where is it stored? When is it released? What is gluconeogenesis? When does it take place?
LIVER FUNCTION: AMMONIA CONVERSION • When gluconeogenesis takes place what is the byproduct of the process? • What happens to the byproduct? • What do the bacteria in the intestines produce as a byproduct? • How is this byproduct removed?
LIVER FUNCTION: PROTEIN METABOLISM • What is the liver’s job in terms of synthesizing plasma proteins? • What does the liver need to complete it’s job?
LIVER FUNCTION: FAT METABOLISM • What is the liver’s job in terms of fat metabolism? • When does the liver do this? • What are the results of this metabolism used for?
LIVER FUNCTION: VITAMIN & IRON STORAGE • Stores which fat soluble vitamins? • What other vitamins are stored in the liver? • What are these vitamins responsible for? • Which minerals are stored in the liver?
LIVER FUNCTION: DRUG METABOLISM and DETOXIFICATION • THE FOLLOWING CLASSIFICATION OF DRUGS ARE METABOLIZED BY THE LIVER? • What else is metabolized by the liver? • What does the liver do in terms of detoxification?
NORMAL FUNCTION: bile secretion • • • What is the liver’s job with Bile? When is bile secreted? Where is Bile collected and stored? How is this related to Billirubin? When do Billirubin levels increase?
LIVER FUNCTION: PROTECTION • What does the liver’s protection function involve? • What do the cells do?
LIVER FUNCTION CONTINUED • Inactivates Hormones – Estrogen – Testoterone – Progesterone – Aldosterone – cortisol • Sinusoids store blood (about 200 -400 cc)
DISORDER OF THE LIVER HEPATITIS
Hepatitis Widespread viral inflammation of liver cells • Hepatitis A (HAV) • Hepatitis B (HBV) • Hepatitis C (HCV) • Hepatitis D (HDV) • Hepatitis E (HEV) • Hepatitis F and G are uncommon (HFV, HGV) • DRUG INDUCED HEPATITIS • Occurs as a secondary infection
Hepatitis A (HAV) • Similar to that of a typical viral syndrome; often goes unrecognized • Spread via the fecal-oral route by oral ingestion of fecal contaminants • Contaminated water, shellfish from contaminated water, food contaminated by handlers infected with hepatitis A • Also spread by oral-anal sexual activity (Continued)
Hepatitis A (HAV)(Continued) • Incubation period for hepatitis A is 15 to 50 days. • Disease is usually not life threatening. • Disease may be more severe in individuals older than 40 years of age. • Many people who have hepatitis A don’t know it; symptoms are similar to a gastrointestinal illness.
Hepatitis B (HBV) • Spread is via unprotected sexual intercourse with an infected partner, sharing needles, accidental needle sticks, blood transfusions, hemodialysis, maternal-fetal route. • Symptoms occur in 25 to 180 days after exposure; symptoms include anorexia, nausea and vomiting, fever, fatigue, right upper quadrant pain, dark urine, light stool, joint pain, and jaundice. (Continued)
Hepatitis B (HBV) (Continued) • Hepatitis carriers can infect others, even if they are without symptoms.
Hepatitis C (HCV) • Spread is by sharing needles, blood products, or organ transplants (prior to 1992), needle stick injury, tattoos, intranasal cocaine use. • Incubation period is 21 to 140 days. • Most individuals are asymptomatic; damage occurs over decades. • Hepatitis C is the leading indication for liver transplantation in the U. S. • NOT TRANSMITTED BY CAUSUAL OR INTIMATE HOUSEHOLD CONTACT
Hepatitis D (HDV) • Transmitted primarily by parenteral routes • Incubation period 14 to 56 days • HDV coinfects with HBV and needs it presence to replicate
Hepatitis E (HEV) • Present in endemic areas where waterborne epidemics occur and in travelers to those areas (India, Asia, Africa, Middle East, Mexico, Central America & South America) • Also seen in travellers coming from these areas • Transmitted via fecal-oral route • Resembles hepatitis A • Incubation period 15 to 64 days
Clinical Manifestations of all Hepatitis • Abdominal pain • Changes in skin or eye color • Arthralgia (joint pain) • Myalgia (muscle pain) • Diarrhea/constipation • Wgt loss • Hepatomegaly • • Fever Lethargy/Malaise Nausea/vomiting Intolerance to fats/dyspepsia • Pruritus • CHANGES IN COLOR OF URINE AND STOOL
ASSESSMENT HEALTH HISTORY • Suspected exposure • Medical history SIGNS/SYMPTOMS • Pre-icteric stage • Icteric stage • Post-icteric stage
SIGNS/SYMPTOMS • PRE-ICTERIC STAGE • Lasts about 1 week
SIGNS AND SYMPTOMS • ICTERIC STAGE • Lasts 2 -6 weeks • Jaundice appears • Yellow skin, sclera, mucous membranes • Dark amber urine • Clay colored stools
SIGNS AND SYMPTOMS • POST-ICTERIC STAGE • Lasts 2 -6 weeks • Jaundice subsides • Liver decreases in size • Good appetite
LABORATORY TESTS FOR HEPATITIS • There will be an increase of liver enzymes and serologic markers INDICATING A PRESENCE OF HEPATITIS A, B, C
LABORATORY TESTS FOR HEPATITIS A (HAV) • Presence of hepatitis A in client: when hepatitis A (HAV) antibodies (anti-HAV) are found in the blood • Presence of immunoglobulin M(Ig. M) antibodies means that ongoing inflammation of liver present (persisits for 4 -6 wks) • Previous infection indicated by presence of immunoglbulin G (Ig. G) antibodies which provides permanent immunity to disease
LABORATORY TESTS FOR HEPATITIS B (HBV) Serologic markers which indicate client has Hepatitis B (HBV) are: • HBs. Ag (Hepatitis B surface Antigen) • Anti-HBc Ig. M (Ig. M antibodies to hepatitis B core antigen) If these levels are elevated after 6 months: chronic or carrier state Presence of antibodies to HBs. Ab (hepatitis B surface antibody): indicates recovery and immunity to hepatitis B Someone immunized will have a positive HBs. Ab
LABORATORY TESTS FOR HEPATITIS C (HCV) • ELISA (enzyme linked immunosorbent assay ) SCREENS INITIALLY & for HCV antibodies (anti. HCV): can detect antibodies in 4 wks • RIBA: (recumbent immunoblot assay): used to confirm that client has been exposed and has developed antibody • HCV PCR (HCV polymerase chain reaction test): confirms presence of circulating active virus
LABORATORY TEST FOR HEPATITIS D (HDV) • Presence of virus confirmed by identification of intrahepatic delta antigen • Also by rise in hepatitis D virus antibodies (anti-HDV) titer • Found within a few days of infection
LBORATORY TESTS FOR HEPATITIS E (HEV) • VIRUS CANNOT BE DETECTED • Presence of hepatitis E antibodies (anti. HEV) is found in people infected with virus
LABORATORY TESTS CONTINUED • A person having a previous infection is indicated by immunoglobulin G (Ig. G) antibodies. They persist in blood and provide permanent immunity to HAV
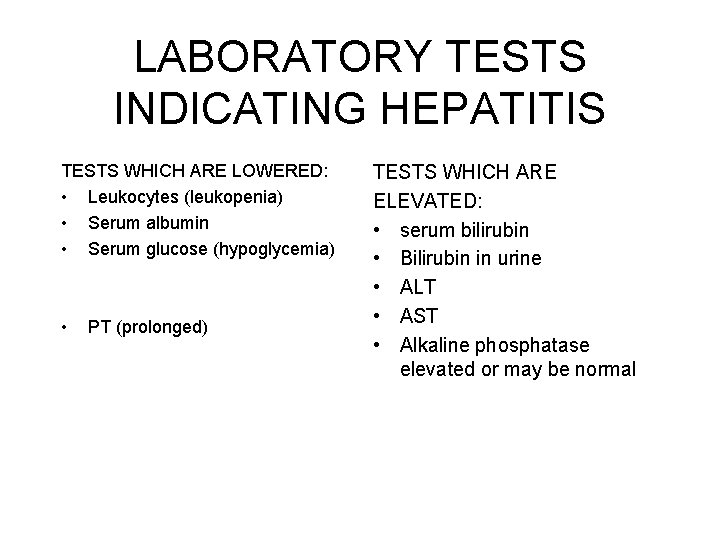
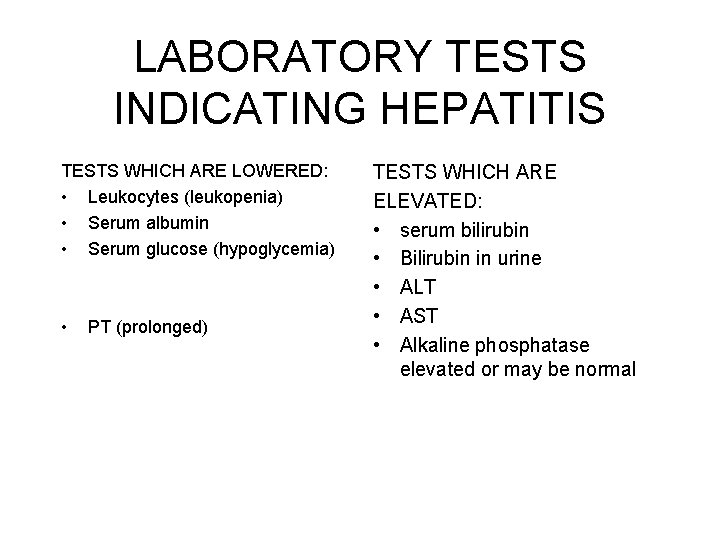
LABORATORY TESTS INDICATING HEPATITIS TESTS WHICH ARE LOWERED: • Leukocytes (leukopenia) • Serum albumin • Serum glucose (hypoglycemia) • PT (prolonged) TESTS WHICH ARE ELEVATED: • serum bilirubin • Bilirubin in urine • ALT • AST • Alkaline phosphatase elevated or may be normal
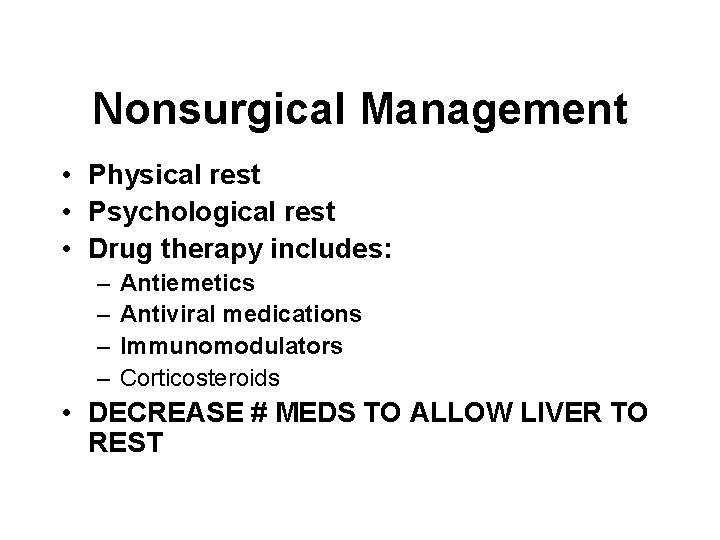
Nonsurgical Management • Physical rest • Psychological rest • Drug therapy includes: – – Antiemetics Antiviral medications Immunomodulators Corticosteroids • DECREASE # MEDS TO ALLOW LIVER TO REST
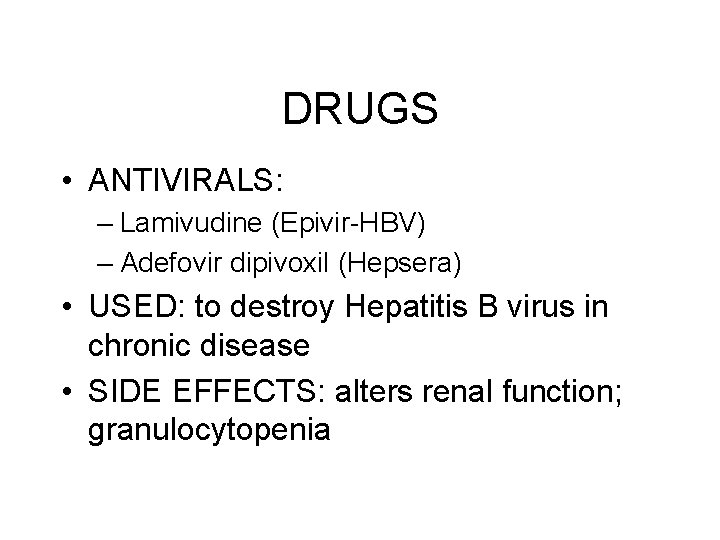
DRUGS • ANTIVIRALS: – Lamivudine (Epivir-HBV) – Adefovir dipivoxil (Hepsera) • USED: to destroy Hepatitis B virus in chronic disease • SIDE EFFECTS: alters renal function; granulocytopenia
DRUGS IMMUNOMODULATING DRUGS: – Interferon(peginterferon alfa-2 a) (Pegasys) – Oral ribavirin (Virazole)
NURSING CARE Diet therapy • Hydration • No alcohol • Low fat, moderate protein, high CHO diet, high calorie • Small frequent meals • Vit B, C, K
PATIENT EDUCATION • Prevention to health care professionals • Knowledge of transmission routes • Proper personal hygiene and good sanitation • Gamma Globulin • Avoid sex until antibody results (negative) • Hepatitis A Vaccine • Hepatitis B vaccine • No vaccine for Hepatitis E • Hepatitis C mainly spread through blood transfusions: (screen blood products)
CIRRHOSIS DEFINED • • Chronic Degenerative Causes liver enlargement Causes loss of normal liver function
PATHOPHYSIOLOGY • Fibrotic bands of connective tissue change the structure of the liver • Inflammation causes degeneration and destruction of liver cells • Tissue becomes nodular • Nodules block bile ducts and normal blood flow throughout the liver • Blood flow changes occur from compression by the fibrous tissue
TYPES OF CIRRHOSIS • Laennec’s cirrhosis: chronic ETOH, nutritional deficiencies • Biliary • Postnecrotic cirrhosis: hepatic necrosis • Cardiac: congestion and tissue damage due to heart failure
ETIOLOGY • Known causes of liver disease include: – Alcohol – Viral hepatitis – Autoimmune hepatitis – Steatohepatitis – Drugs and toxins – Biliary disease (Continued)
ETIOLOGY CONTINUED – Metabolic/genetic causes – Cardiovascular disease
EARLY SIGNS AND SYMPTOMS CIRRHOSIS • • • Same for all types regardless of the cause Start out vague, like flu General weakness, Fatigue Anorexia, Indigestion Abnormal bowel function (constipation, or diarrhea) Abdominal pain/liver tenderness
LATE S & S • Jaundice, pruritus, dry skin, warm bright red palms of hands (palmar erythema), rashes • Edema, ascites, significant wgt change, peripheral dependent edema extremities and sacrum • Bleeding tendencies/Anemia/petecchiae, echymosis • Infections • Menstrual irreg/gynecomastia/impotence • Renal failure/dark amber urine • Clay colored stools
ASSESSMENT INSPECTION: • Jaundice • Caput medusae: dilated abd veins, • striae, • spider angiomas • Contour of abdomen: Distension: massive ascites • Everted umbilicus (umbilicus protrusion) • HEPATOMEGALY, SPLENOMEGALY
Other Physical Assessments • Assess nasogastric drainage, vomitus, and stool for presence of blood • Fetor hepaticus (breath odor) • Amenorrhea • Gynecomastia, testicular atrophy, impotence • Neurologic changes: changes in LOC, leading to coma, Asterixis
HOW TO ELICIT ASTERIXIS • • Have client extend the arm, dorsiflex the wrist Extend the fingers OBSERVE rapid non-rhythmic extensions and flexions
Laboratory Assessment • AST: Aminotransferase serum levels and LDH: lactate dehydrogenase may be elevated from hepatic cell destruction. • Alkaline phosphatase levels may increase from obstructive jaundice. • Total serum bilirubin from hepatic disease and urobilinogen levels may rise from hepatocellular obstruction or liver disease. • decrease. (Continued)
Laboratory Assessment (Continued) • Fecal urobilinogen is decreased due to obstructive liver disease • Total serum protein and albumin levels decreased • Prothrombin time prolonged; platelet count low • Decreased hemoglobin and hematocrit values due to anemia and white blood cell count
LABORATORY ASSESSMENT CONTINUED • Elevated ammonia levels: liver cannot excrete ammonia • BUN and Serum creatinine level possibly elevated due to decreased renal function
COMPLICATIONS: PORTAL HYPERTENSION • Increase pressure in portal vein • Comes from obstruction of blood flow from pressure by CT bands (see patho) • New channels looked for • Blood flows back to spleen (splenomegaly) • Veins become dilated (esophagus, stomach, intestines, abdomen, rectum)
PORTAL HYPERTENSION (CONTINUED) • Results in: – Ascites – Esophageal varices – Prominent abdominal veins (caput medusae) – hemorroids
COMPLICATION: ASCITES DEFINED AS: • Accumulation of free fluid within the peritoneal cavity • With increased hydrostatic pressure from portal hypertension fluid leaks into peritoneal cavity • Albumin in fluid hypoalbuminemia
ASCITES CONTINUED • • • Hypovolemia renal vasoconstriction Renin-angiotensin system triggered Sodium and water retention Leads to increased hydrostatic pressure Perpetuates the cycle of ASCITES
COMPLICATIONS ASCITES: • Bed rest, HOB up 30 degrees or higher; or sitting in chair • Abdominal girth measurements • bid wgts standing • Strict fluid restriction; strict I & O, vitamin supplements • Salt free diet/diuretics/electrolyte replacement
Excess Fluid Volume (Continued) Paracentesis is insertion of trocar catheter into abdomen to remove & drain fluid from the peritoneal cavity. – Observe for possibility of impending shock, electrolyte imbalances: albumin IV.
EXCESS FLUID SURGICAL MANAGEMENT CONTINUED – LAVEEN SHUNT (peritoneovenous shunt): surgical procedure, tube placed in peritoneal cavity, drain fluid into superior vena cava – PORTACAVAL SHUNT: (See p 1378 fig 62. 4) surgical shunting diverts portal venous blood flow from the liver TIPS (transjugular intrahepatic portalsystemic shunt): non surgical procedure creating a connection within the liver between the portal and systemic circulation to reduce portal pressure
COMPLICATION: BLEEDING ESOPHAGEAL VARICES DEFINED: fragile thin walled esophageal veins become distended from pressure Portal hypertension blood backs up from liver to esophageal and gastric vessels
COMPLICATIONS ESOPHAGEAL VARICES MEDICAL EMERGENCY LIFE THREATENING S&S: hematemesis, melena, shock Can occur spontaneously Can be caused by any activity that Abdominal pressure
TREATMENT OF BLEEDING ESOPHAGEAL VARICES • IV fluids/electrolytes/volume expander/ transfuse • ESOPHAGOGASTRIC BALLOON TAMPONADE: via Sengstaken. Blakemore tube – Compressing bleeding vessels with this tube
SENGSTAKEN-BLAKEMORE TUBE Used to control bleeding • Esophageal balloon • Gastric balloon • 3 lumens – 1 for gastric lavage – 1 for inflating the esophageal balloon – 1 for inflating the gastric balloon
SENGSTAKEN-BLAKEMORE TUBE: NRSG CARE • MD inserts tube with HOB 30 -45 degrees MOST SERIOUS COMPLICATION: ASPIRATION AND AIRWAY OCCLUSION SURGICAL SCISSORS AT BEDSIDE • Monitor for respiratory distress • Suction saliva from upper esophagus, nasopharynx • Check nostrils frequently, cleanse and lubricate to prevent ulceration • Removed after bldg controlled
RUPTURE OF ESOPHAGEAL VARICIES • Vasopressin: constriction arterial bed • Somatostatin: decreases bldg without vasoconstrictive effects of Vasopressin • Propranolol: beta blocker to decrease portal pressure
COMPLICATION: COAGULATION DEFECTS • synthesis of bile in liver • Prevents absorption of fat soluble vitamins (vit K) • Without vit K clotting factors are not produced • susceptible to bleeding • Abnormal PT (prolonged or )
COMPLICATION: SPLENOMEGALY • Backup of blood into spleen • Spleen destroys platelets • thrombocytopenia (first sign of liver dysfunction)
COMPLICATION: JAUNDICE • Liver cells cannot excrete bilirubin • circulating bilirubin levels LABORATORY TESTS: changes with hepatocellular jaundice Serum bilirubin (indirect and direct) Urine bilirubin Urobilinogen stool: normal to Urobilinogen urine: normal to
COMPLICATIONS: PORTAL SYSTEMIC ENCEPHALOPATHY (PSE) • Also called HEPATIC ENCEPHALOPATHY AND HEPATIC COMA SEE: neurologic symptoms Impaired LOC Impaired thinking Impaired neuromuscular disturbances ACUTE AND REVERSIBLE with early intervention CAUSED BY: elevated ammonia levels
NURSING DIAGNOSIS • • • Activity intolerance Fluid volume deficit Fluid volume excess Ineffective breathing patterns Risk for hemorrhage Risk for infection Altered nutrition Pain Sexual dysfunction
NURSING DIAGNOSIS CONTINUED • Altered thought processes • Risk for violence
NURSING CARE • • Bed rest with controlled activity, prevent clots Prevent infection (pneumonia) Assess for bleeding Treat dry itching skin: no soap, soft linens, lotions, antihistamines • Assess F & E status, bid wgts, abd girth once shift, I&O, fluid restriction, amt of dietary protein • Assess neuro status q 2 hr • Psychological support/abstinence of alcohol
Fatty Liver (Steatohepatitis) • Fatty liver is caused by the accumulation of fats in and around the hepatic cells. • Causes include: – Diabetes mellitus – Obesity – Elevated lipid profile • Many clients are asymptomatic.
Hepatic Abscess • Liver invaded by bacteria or protozoa causing abscess • Pyrogenic liver abscess; amebic hepatic abscess • Treatment usually involves: – Drainage with ultrasound guidance – Antibiotic therapy
Liver Trauma • The liver is the most common organ injured in clients with penetrating trauma of the abdomen, such as gunshot wounds and stab wounds. • Clinical manifestations include abdominal tenderness, distention, guarding, rigidity. • Treatment involves surgery, multiple blood products.
Cancer of the Liver • One of the most common tumors in the world • LIVER BX: done in same day surgery, local anesthetic, done through skin. CRITICAL THAT COAGULATION TESTING BE DONE. MAJOR SE: hemorrhage • Most common c/o: abd discomfort • Tx includes: Chemotherapy/Surgery
Liver Transplantation • Used in the treatment of end-stage liver disease, primary malignant neoplasm of the liver • Donor livers obtained primarily from trauma victims who have not had liver damage • Donor liver transported to the surgery center in a cooled saline solution that preserves the organ for up to 8 hours
Complications • • Acute, chronic graft rejection Infection Hemorrhage Hepatic artery thrombosis Fluid and electrolyte imbalances Pulmonary atelectasis Acute renal failure Psychological maladjustment
 Who analgesic ladder
Who analgesic ladder Pathophysiology of intestinal obstruction
Pathophysiology of intestinal obstruction Nursing diagnosis for undescended testis
Nursing diagnosis for undescended testis Hirschberg test
Hirschberg test Pneumatic reduction of intussusception
Pneumatic reduction of intussusception Nursing care plan of cataract
Nursing care plan of cataract Type 1 diabetes in adults diagnosis and management
Type 1 diabetes in adults diagnosis and management Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Thang điểm glasgow
Thang điểm glasgow Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Functional nursing care delivery model
Functional nursing care delivery model Post operative nursing management
Post operative nursing management Nursing rationale examples
Nursing rationale examples Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Selective mutism in adults
Selective mutism in adults Normal vitals for adults
Normal vitals for adults Normal vital range for adults
Normal vital range for adults Bluegrass billbugs overwinter as adults
Bluegrass billbugs overwinter as adults Emotional love language
Emotional love language Apical radial pulse
Apical radial pulse Examples of problem-solving scenarios
Examples of problem-solving scenarios Normal stool
Normal stool Self-advocacy worksheets for adults
Self-advocacy worksheets for adults Pedalute
Pedalute Odd diagnostic criteria
Odd diagnostic criteria Nvld
Nvld Jaundice grading in adults
Jaundice grading in adults Token economy prison
Token economy prison Mental health and older adults
Mental health and older adults Lady neck
Lady neck Amoebiasis symptoms
Amoebiasis symptoms Hep b vaccine schedule for adults
Hep b vaccine schedule for adults Healthy relationship scenarios
Healthy relationship scenarios Gama iq test
Gama iq test Riddle fruit
Riddle fruit Male and female skeleton differences
Male and female skeleton differences Placement of aed pads on adults
Placement of aed pads on adults Fasd
Fasd Hpv vaccine schedule adults
Hpv vaccine schedule adults Oppositional defiant disorder in adults
Oppositional defiant disorder in adults