The future of mental health MHN 2014 Wednesday


































- Slides: 77

The future of mental health #MHN 2014 Wednesday 26 March 2014 Dexter House, London Follow the conversation on Twitter #MHN 2014
Welcome & introduction Shaun Clee, Chair Mental Health Network

Shaping mental health services of the future Stephen Dalton, Chief Executive Mental Health Network Rebecca Cotton, Director of Mental Health Policy Mental Health Network Chair: Shaun Clee, Chair, Mental Health Network #MHN 2014

The future of mental health Shaping mental health services of the future #MHN 2014 Stephen Dalton, Chief Executive, Mental Health Network Rebecca Cotton, Director of Mental Health Policy, Mental Health Network


Better Services For The Mentally Ill White Paper - 1975 "It will not normally be possible for a mental hospital to be closed until the full range of facilities described has been provided throughout its catchment area and has shown itself capable of providing, for newly arising patients, a comprehensive service independent of the mental hospital. "
Rethink Mental Illness: Lost Generation March 2014 • EIP support reduces risk of suicide in young people from 15% to 1%. • People with EIP support more than 20% less likely to be detained under Mental Health Act. • 50% services say budget has been cut.


Headlines from our recent member survey • 96% of Mental Health Network members who took part are concerned about the effect of an ageing population on services, 90% are concerned about the future impact of long term conditions. • 96% are worried about potential future budget cuts, and 90% think there’s insufficient investment to meet current service requirements. • 89% are concerned about outdated service and workforce models, and the same percentage are worried about the relationship between health and social care. • 90% think the public misunderstand the need for change in the NHS, and 80% think there’s a lack of political support for the change that’s needed. • 85% of Mental Health Network members say the agreement of a long term (ten year) strategy and financial settlement for the NHS as a whole is important. Base: 103 MHN respondents, February 2014

Trends: UK population projections Growing: overall the UK population is predicted to increase by 10. 9 million over the next 25 years, to 73. 2 million at mid-2035. Increasingly diverse: The Economic and Social Research Council predict that in 40 years’ time people from black and minority ethnic groups will make up 20% of the population (from 8% in 2001). They also predict that this population group will become less concentrated in larger urban areas , moving from the inner city to suburbs and surrounding towns. Ageing: Compared to 2010, by 2030 there will be 51% more people aged 65 and over, and a doubling of the numbers of people aged 85 and over in England.
Trends: numbers of people with mental health problems • By 2030 there will be approximately 2 million more adults in the UK with mental health problems than today – assuming prevalence rates remain the same. • But - proportion of people with common mental disorders increased from 15. 5 per cent in 1993 to 17. 6 per cent in 2007. Will this trend continue? • The World Health Organisation predict that depression will be second leading cause of global disability burden by 2020. • As of 2012, there were 800, 000 people in the UK with a form of dementia. By 2021 this is projected to rise to 1 million, and then to 1. 7 million by 2051.
Trends: Changing attitudes and expectations • On the whole, society’s attitude to mental health problems are changing for the better. • Time to Change have found the proportion of people saying they know someone close to them who has had some kind of mental illness has increased from 58% in 2009 to 63% in 2012. • Expectations from service users, carers and professionals are changing – informed by a focus on recovery. • There are generational differences evident. For the NHS as a whole, older people are more likely than younger people to be more positive about their local NHS services. 84 per cent of over 65 s agree that their local NHS is providing them with a good service, compared with 69 per cent of 25 - 34 year olds.
Investment in mental health services • 96% of Mental Health Network members told us they were worried about potential future budget cuts. • Mental health services have already been subject to three years of real terms cuts. • In 2012, the Nuffield Trust predicted that if NHS funding is held flat after this spending review period, then the NHS in England could experience a funding gap of between £ 44 and £ 54 billion by 2021/22 unless productivity gains could be delivered to off-set. • Upwards pressure will result from growing demand for healthcare, and the costs of providing it – of which the largest item is workforce pay
Question: What does the NHS need to do to maintain or improve quality if finances stay the same and there is no large scale service change? • 68% - reduce demand through prevention • 41% - take action on staff costs e. g. continue pay restraint and review terms and conditions • 31% - increase efficiency of procurement by the NHS • 28% - find further efficiency savings • 25% - increase pooling of budgets • 27% - introduce rationing of care • 14% - introduce user charges • 17% - sell off NHS estates Base: 103 MHN respondents, February 2014

Efficiency: the digital revolution? • 83% of homes now have internet access. • 43% of users have accessed health information online, up from just 18% in 2007. • Meeting the expectations of younger service users will require embracing the digital revolution. • Pressure on resources creates a powerful incentive for developing new ways of delivering care and support. • There are great examples of digital being used in mental health – Clintouch, Buddy, Big White Wall – but we have a long way to go.

Efficiency: embracing integration • £ 1 in every £ 8 spent on long-term conditions is linked to poor mental health and wellbeing. • This equates to between £ 8 billion and £ 13 billion of NHS spending in England. • A 2012 Mental Health Network report, Investing in emotional and psychological wellbeing for patients with long-term conditions, highlighted a wide range of innovative services that were both generating much needed savings and improving outcomes for patients with diabetes, chronic obstructive pulmonary disease and a range of other conditions.

Efficiency: embracing integration • Rethink Mental Illness estimates that a third of the 100, 000 annual ‘avoidable deaths’ amongst the under 75 s involve someone with a mental health problem. • Smoking costs the NHS over £ 5 billion a year, yet 42% of all cigarettes smoked in England are by people with a mental health, drug or alcohol problem. • Practical steps such as ensuring service users are offered targeted smoking cessation services, diet and exercise advice, and improving uptake of national screening programmes are all key.
What should our workforce look like? • Do we have the right mix of skills and expertise in our workforce to deliver recovery orientated services? • Debate centres on the balance between specialists and generalists. • A clear vision for the future does not exist – some advocate for the need to move towards more generalist skills, including an increased role for peer support - either formally or informally. Some passionately defend the need to retain clinical roles and expertise. • Impossible to ignore the fact workforce costs make up 40% of the NHS budget – if issues of cost drive the debate this will not be without controversy.

Question: Which of the following statements best describes your views about the future of the NHS as whole? For the sake of this question, please assume there are no significant funding or budgetary changes (i. e. budget stays flat in real terms). • 40% agree with “The NHS needs to make large scale changes to the way it currently operates and provides services in order to maintain current levels of care”. • 52% agree with “Even if the NHS makes large scale changes to the way it currently operates and provides services, this alone will not ensure it can maintain current levels of care”. Base: 103 MHN respondents, February 2014
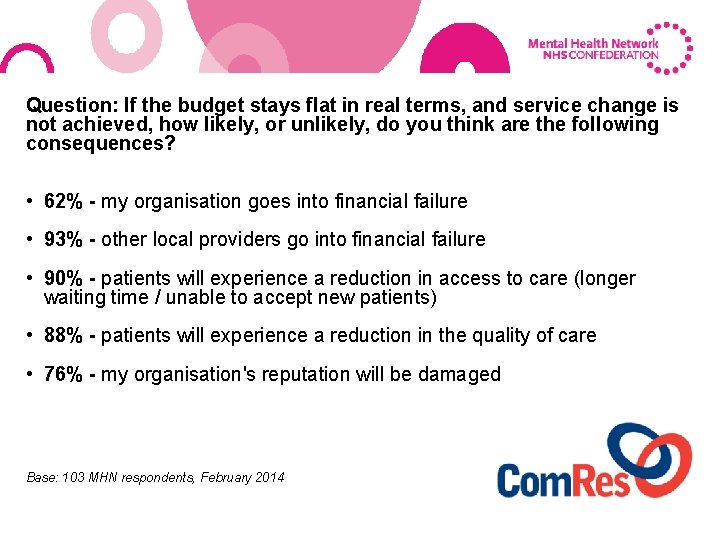
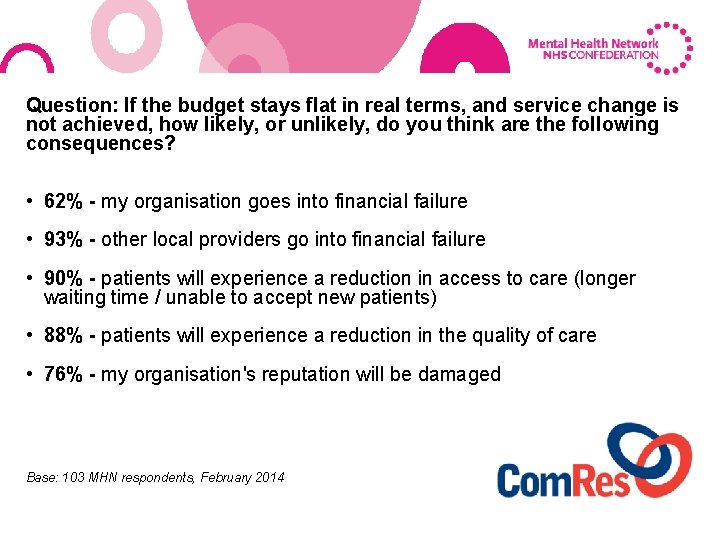
Question: If the budget stays flat in real terms, and service change is not achieved, how likely, or unlikely, do you think are the following consequences? • 62% - my organisation goes into financial failure • 93% - other local providers go into financial failure • 90% - patients will experience a reduction in access to care (longer waiting time / unable to accept new patients) • 88% - patients will experience a reduction in the quality of care • 76% - my organisation's reputation will be damaged Base: 103 MHN respondents, February 2014
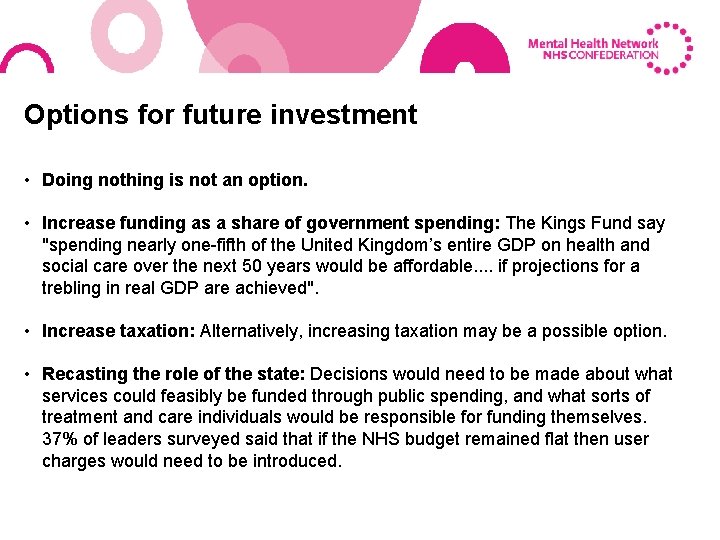
Options for future investment • Doing nothing is not an option. • Increase funding as a share of government spending: The Kings Fund say "spending nearly one-fifth of the United Kingdom’s entire GDP on health and social care over the next 50 years would be affordable. . if projections for a trebling in real GDP are achieved". • Increase taxation: Alternatively, increasing taxation may be a possible option. • Recasting the role of the state: Decisions would need to be made about what services could feasibly be funded through public spending, and what sorts of treatment and care individuals would be responsible for funding themselves. 37% of leaders surveyed said that if the NHS budget remained flat then user charges would need to be introduced.
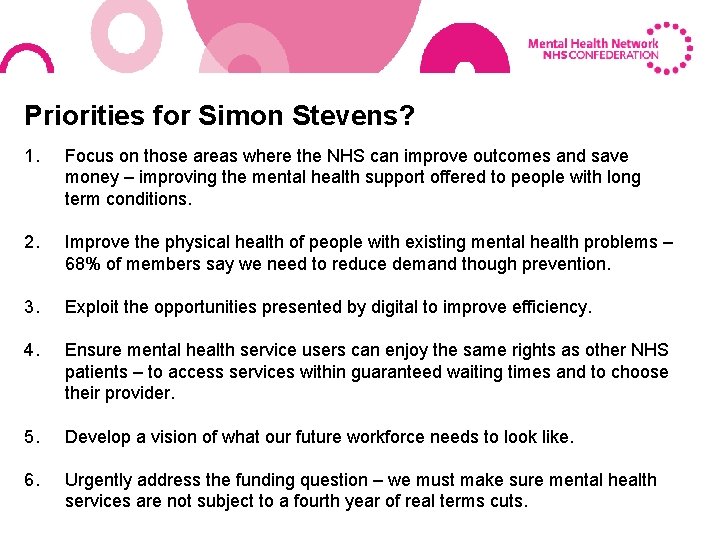
Priorities for Simon Stevens? 1. Focus on those areas where the NHS can improve outcomes and save money – improving the mental health support offered to people with long term conditions. 2. Improve the physical health of people with existing mental health problems – 68% of members say we need to reduce demand though prevention. 3. Exploit the opportunities presented by digital to improve efficiency. 4. Ensure mental health service users can enjoy the same rights as other NHS patients – to access services within guaranteed waiting times and to choose their provider. 5. Develop a vision of what our future workforce needs to look like. 6. Urgently address the funding question – we must make sure mental health services are not subject to a fourth year of real terms cuts.

Thank you stephen. dalton@nhsconfed. org @daltonstephen 3 rebecca. cotton@nhsconfed. org @beckycotton @nhsconfed_mhn #mhn 2014

Right here, right now: improving emergency responses to mental health crisis care Commander Christine Jones, Mental Health Lead Association of Chief Police Officers Lord Victor Adebowale, Chief Executive Turning Point Chair: Dr Geraldine Strathdee OBE, National Clincal Director for Mental Health NHS England #MHN 2014

Changing lives: The future of children and young people's services Professor Martin Knapp, Professor of Social Policy and Director of PSSRU at the London School of Economics; and Director of the NIHR School for Social Care Research Lucie Russell, Director of Campaigns & Media, Young. Minds Jenny Carter, Youth activists, Young. Minds Chair: Stephen Dalton, Chief Executive, Mental Health Network #MHN 2014
London 26 March 2014 Youth mental health: economic issues Martin Knapp PSSRU, London School of Economics and Political Science NIHR School for Social Care Research 29

Youth mental health: economic issues A. The extent of the challenge B. Treatment gaps C. Economic consequences D. Local service evaluations Funding support from NHS Confederation
Prevalence • Children – 10% have mental health problems • Adolescents – 13% of boys and 10% of girls have mental health problems Data from British Child and Adolescent Mental Health Survey (BCAMHS) 2000
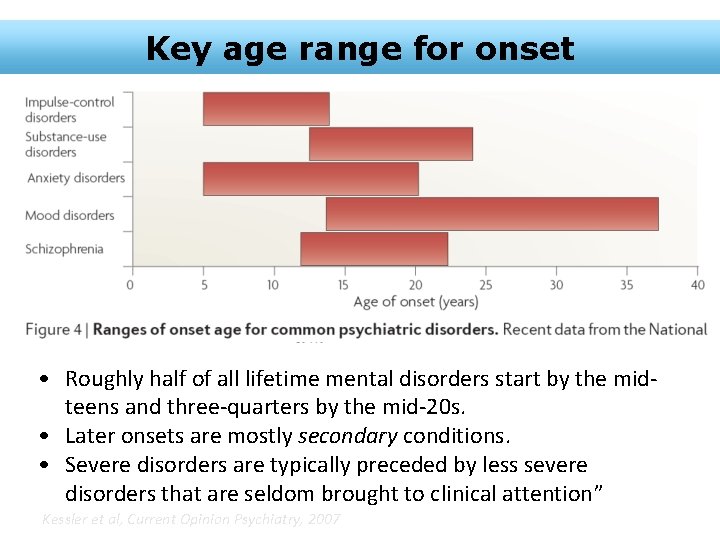
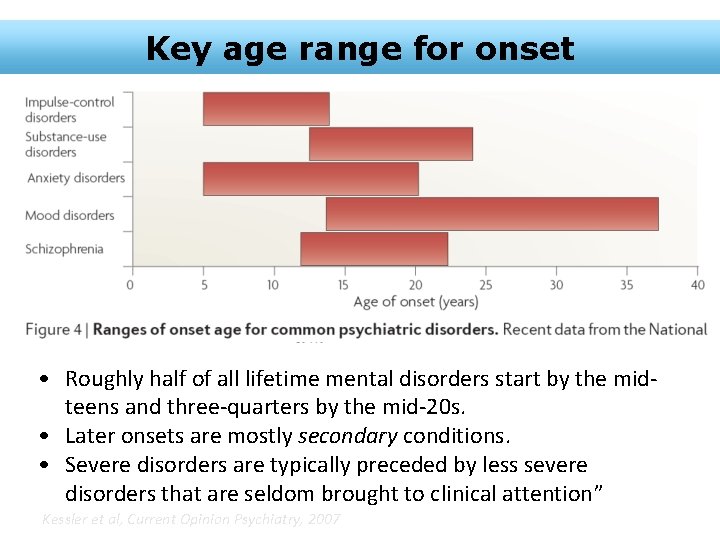
Key age range for onset • Roughly half of all lifetime mental disorders start by the midteens and three-quarters by the mid-20 s. • Later onsets are mostly secondary conditions. • Severe disorders are typically preceded by less severe disorders that are seldom brought to clinical attention” Kessler et al, Current Opinion Psychiatry, 2007
Treatment gap ages 12 -15 Adolescents aged 12 -15 with mental health problems at baseline who were in contact with services linked to their mental health needs in the subsequent 3 years: • Primary care – 26% • Mental health (CAMHS) – 19% • Social care – 9% • Education (frontline) – 12% • Education (specialist) – 13% • Any service – 45% Data from BCAMHS 2000 + 3 -year follow-up

Treatment gap, ages 15 -74 Percentage of people with mental health problems who were using mental health services Data from APMS 2000, follow-up at 18 months
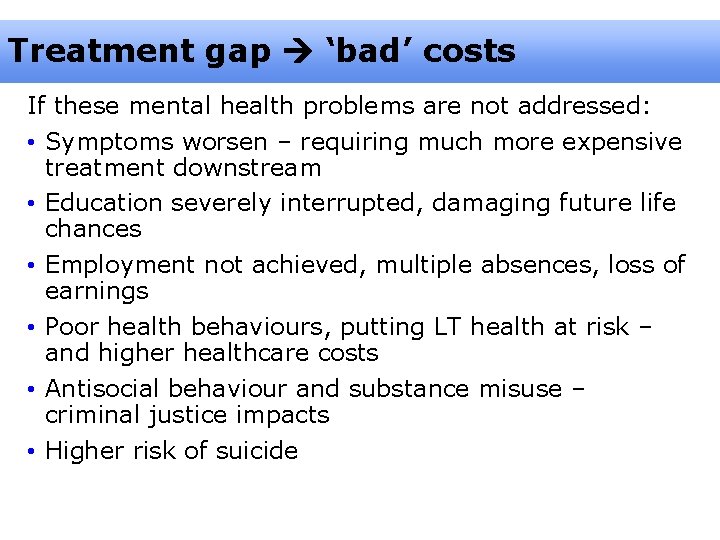
Treatment gap ‘bad’ costs If these mental health problems are not addressed: • Symptoms worsen – requiring much more expensive treatment downstream • Education severely interrupted, damaging future life chances • Employment not achieved, multiple absences, loss of earnings • Poor health behaviours, putting LT health at risk – and higher healthcare costs • Antisocial behaviour and substance misuse – criminal justice impacts • Higher risk of suicide

Service costs (£) between ages 10 -28 by antisocial behaviour at age 10 N= 1689 10 -year olds in South London, 1970 Scott, Knapp, Henderson, Maughan British Medical Journal 2001
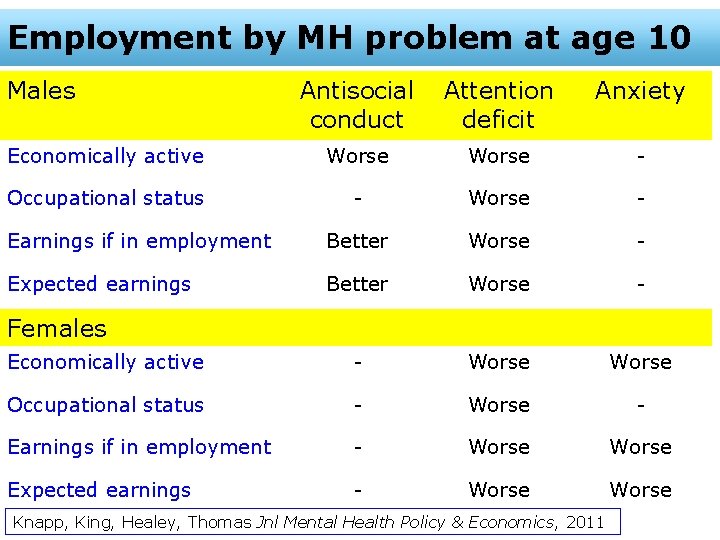
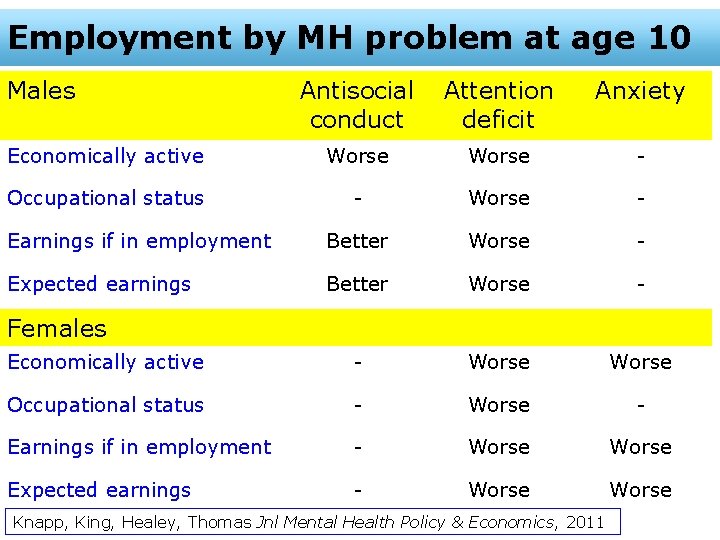
Employment by MH problem at age 10 Males Antisocial conduct Attention deficit Anxiety Economically active Worse - Occupational status - Worse - Earnings if in employment Better Worse - Expected earnings Better Worse - Economically active - Worse Occupational status - Worse - Earnings if in employment - Worse Expected earnings - Worse Females Knapp, King, Healey, Thomas Jnl Mental Health Policy & Economics, 2011
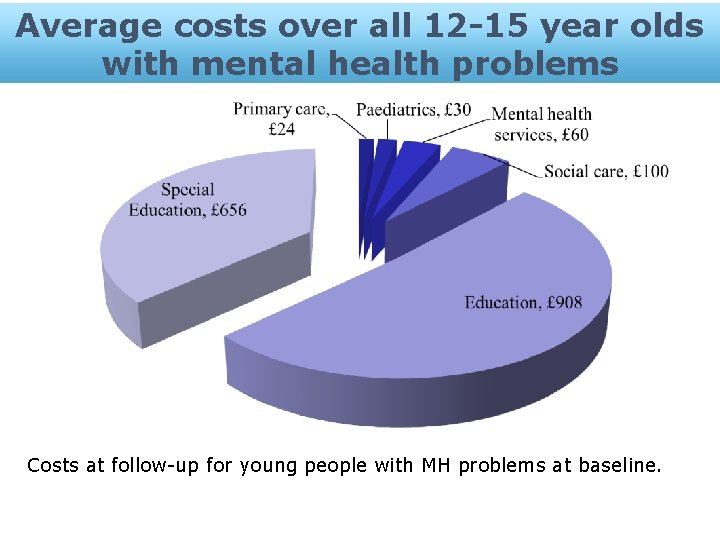
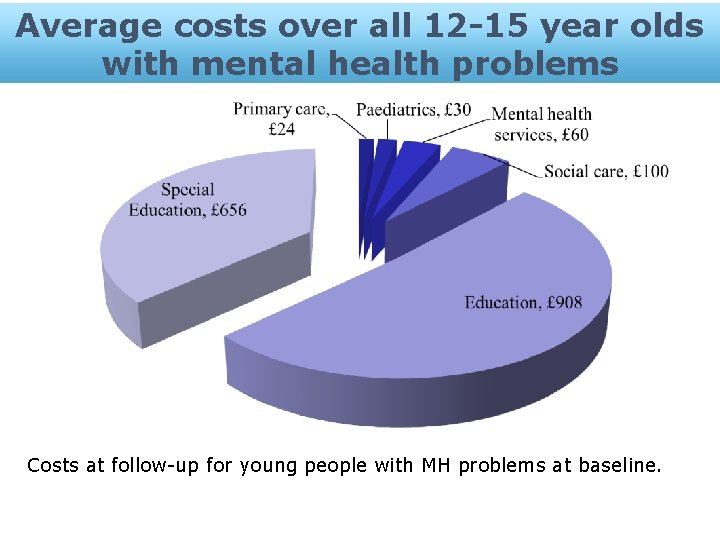
Average costs over all 12 -15 year olds with mental health problems Costs at follow-up for young people with MH problems at baseline.
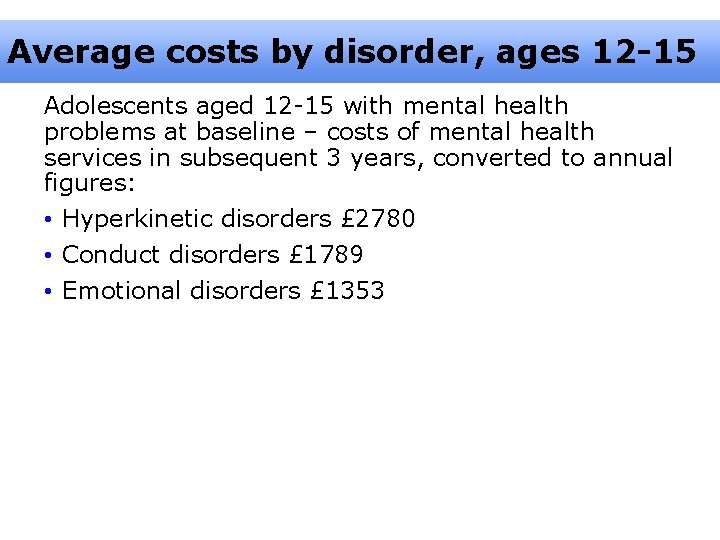
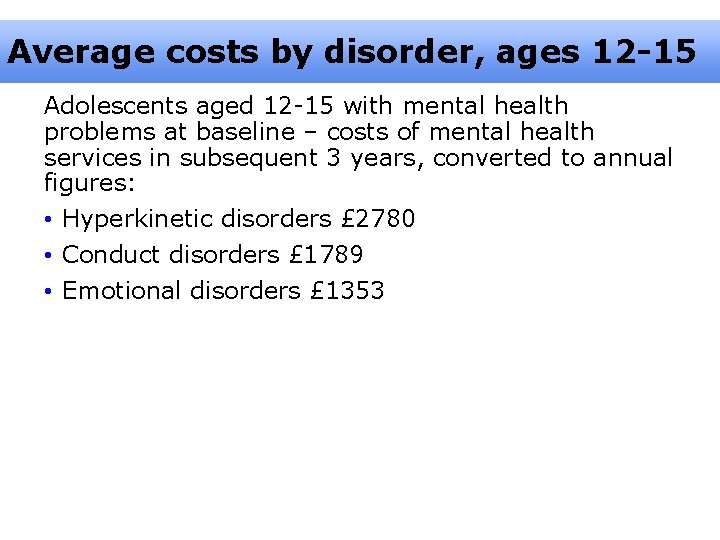
Average costs by disorder, ages 12 -15 Adolescents aged 12 -15 with mental health problems at baseline – costs of mental health services in subsequent 3 years, converted to annual figures: • Hyperkinetic disorders £ 2780 • Conduct disorders £ 1789 • Emotional disorders £ 1353

Worse outcomes for young people not in contact with mental health services For individuals aged 16 -25 with a mental health problem at baseline, who were NOT in contact with mental health services, outcomes 18 months later: • Worse employment rates • Higher NEET • More contact with criminal justice services • No difference in educational engagement Data from APMS 2000 + 18 -month follow-up
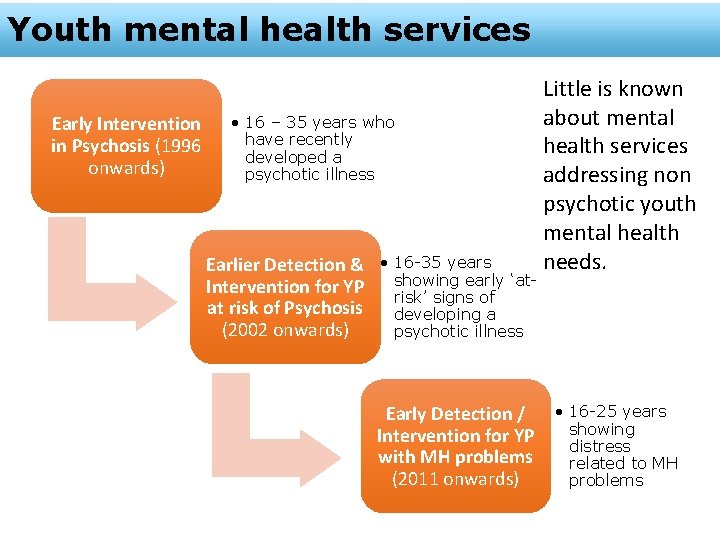
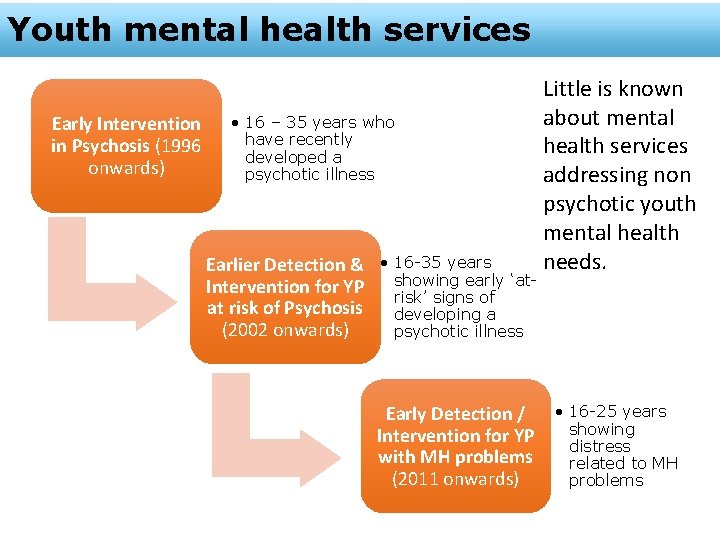
Youth mental health services Early Intervention in Psychosis (1996 onwards) • 16 – 35 years who have recently developed a psychotic illness Earlier Detection & • 16 -35 years Intervention for YP showing early ‘atrisk’ signs of at risk of Psychosis developing a (2002 onwards) psychotic illness Early Detection / Intervention for YP with MH problems (2011 onwards) Little is known about mental health services addressing non psychotic youth mental health needs. • 16 -25 years showing distress related to MH problems

Youth mental health services Poor service models Service delivery models may not be suitable for young people with MH: • Are they acceptable? • Are they accessible? • Are they appropriate? Chief Medical Officer (2013) Prevention Pays: Our Children Deserve Better
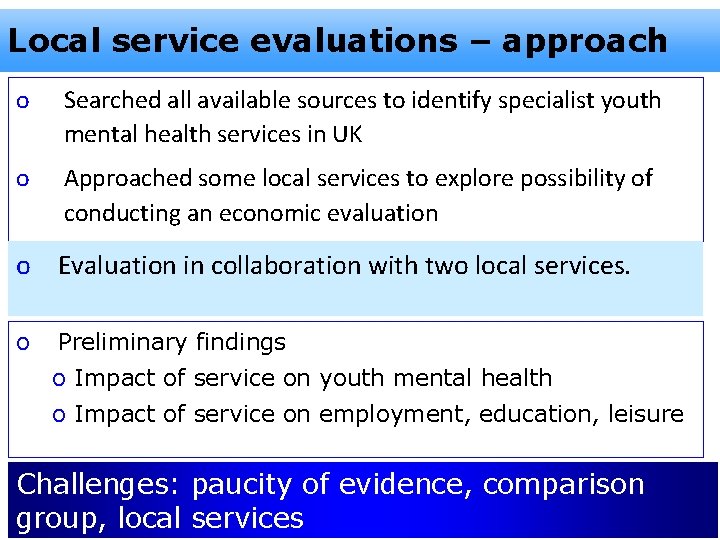
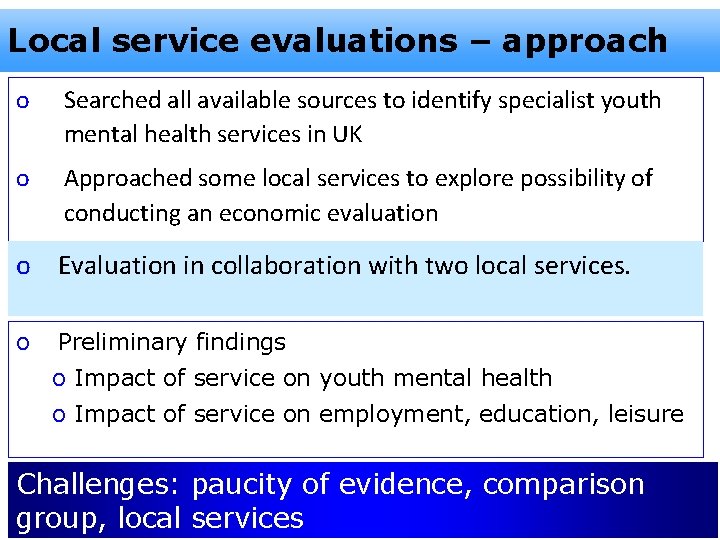
Local service evaluations – approach o Searched all available sources to identify specialist youth mental health services in UK o Approached some local services to explore possibility of conducting an economic evaluation o Evaluation in collaboration with two local services. o Preliminary findings o Impact of service on youth mental health o Impact of service on employment, education, leisure Challenges: paucity of evidence, comparison group, local services
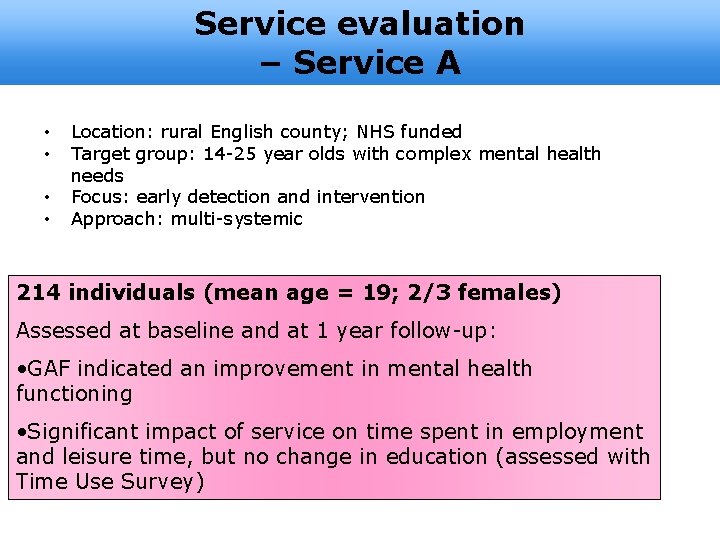
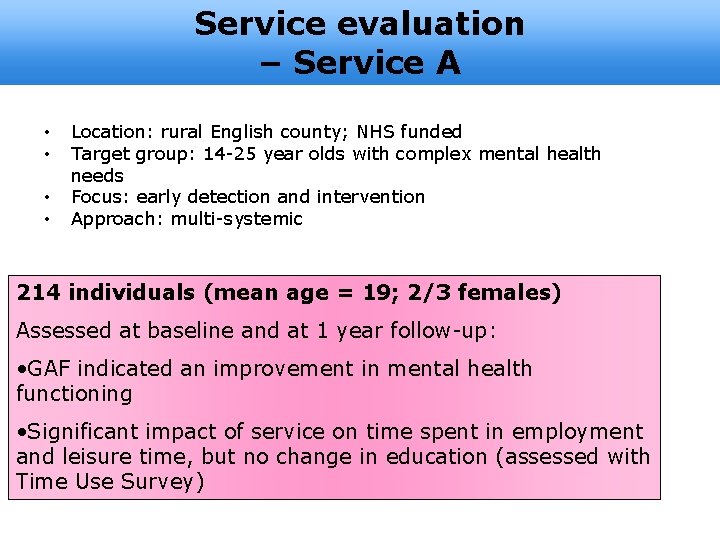
Service evaluation – Service A • • Location: rural English county; NHS funded Target group: 14 -25 year olds with complex mental health needs Focus: early detection and intervention Approach: multi-systemic 214 individuals (mean age = 19; 2/3 females) Assessed at baseline and at 1 year follow-up: • GAF indicated an improvement in mental health functioning • Significant impact of service on time spent in employment and leisure time, but no change in education (assessed with Time Use Survey)

Service evaluation – Service B • Location: deprived inner city area; large BME community • Target group: 16 -25 -year olds in transition from CAMHS to AMHS; no psychosis • Focus: Range of therapies, work and training support • Approach: Integrated Most individuals had moderate or severe symptoms: • Better mental health at 2 years follow-up (measured by GAF) • Not in employment, education or training (NEET) at baseline - but significant improvement (mostly in employment) • External service use decreased; none had returned to secondary services one year after discharge
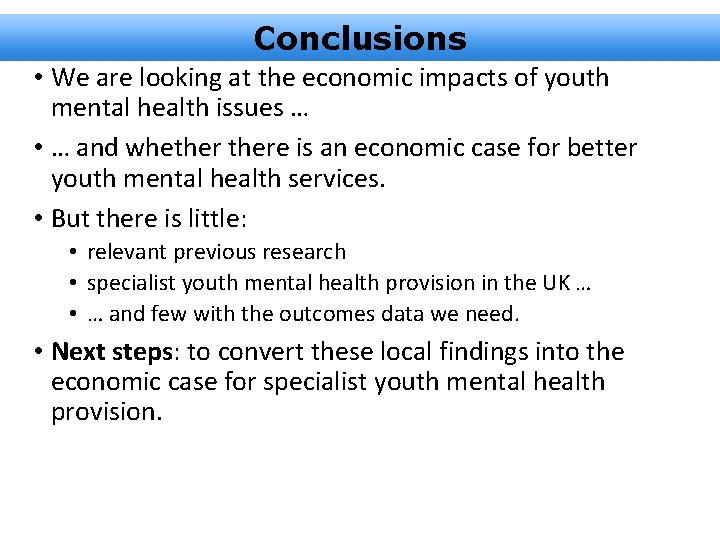
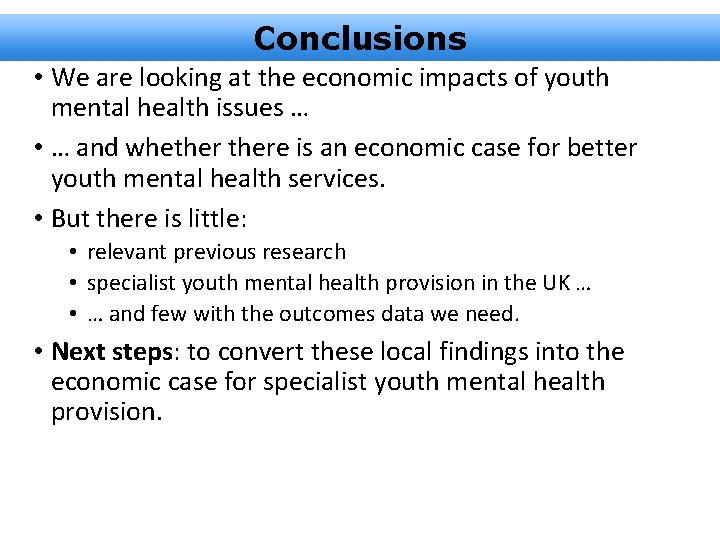
Conclusions • We are looking at the economic impacts of youth mental health issues … • … and whethere is an economic case for better youth mental health services. • But there is little: • relevant previous research • specialist youth mental health provision in the UK … • … and few with the outcomes data we need. • Next steps: to convert these local findings into the economic case for specialist youth mental health provision.

Thank you m. knapp@lse. ac. uk 48

Keynote address: Minister of State for Care and Support Norman Lamb, Member of Parliament #MHN 2014

Choice, competition and aligning incentives - where next for mental health? Ric Marshall, Director of Pricing, Monitor Chair: Stephen Dalton, Chief Executive, Mental Health Network #MHN 2014

Competition, Choice and Pricing Ric Marshall Director of Pricing 26 March 2014 www. monitor. gov. uk

What is Monitor’s role in the NHS? Monitor is the sector regulator for health services in England. Our job is to protect and promote the interests of patients by ensuring that the whole sector works for their benefit 52
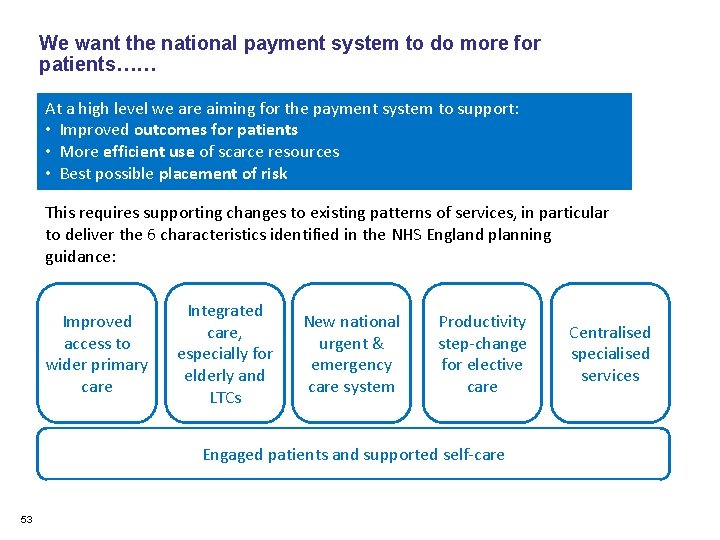
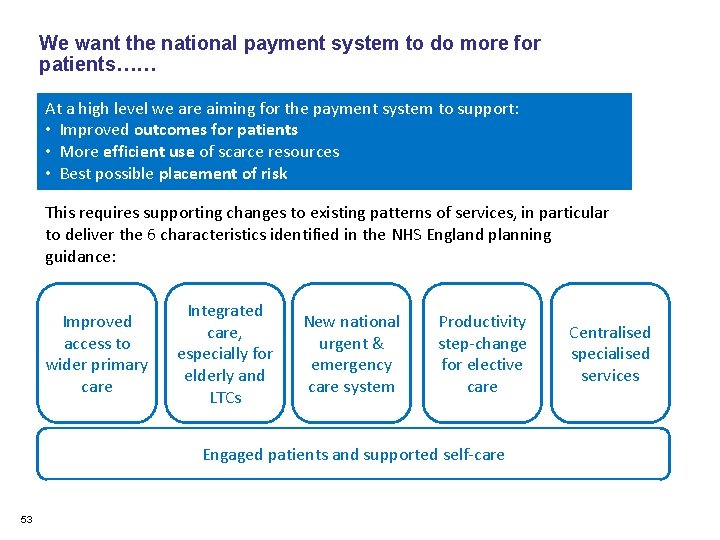
We want the national payment system to do more for patients…… At a high level we are aiming for the payment system to support: • Improved outcomes for patients • More efficient use of scarce resources • Best possible placement of risk This requires supporting changes to existing patterns of services, in particular to deliver the 6 characteristics identified in the NHS England planning guidance: Improved access to wider primary care Integrated care, especially for elderly and LTCs New national urgent & emergency care system Productivity step-change for elective care Engaged patients and supported self-care 53 Centralised specialised services

…. . Within a challenging financial climate Monitor’s Closing the Gap report identifies three improvement opportunities: • Improve ‘as is’: provider efficiency, look again at low value interventions 30 • Right care, right setting: patient self-care, integrated care, shift activity to low cost settings 12 • New models: telemedicine, greater specialisation. . . but a £ 7 bn gap still remains. 4 2 5 7 54 Gap by 2021/22 Improve current services Right care, Innovate Wage freeze Remaining right setting new services to 2014/15 challenge
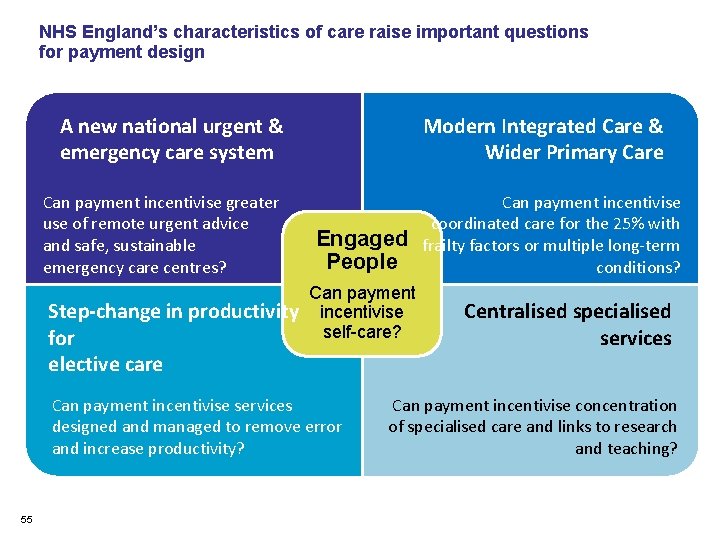
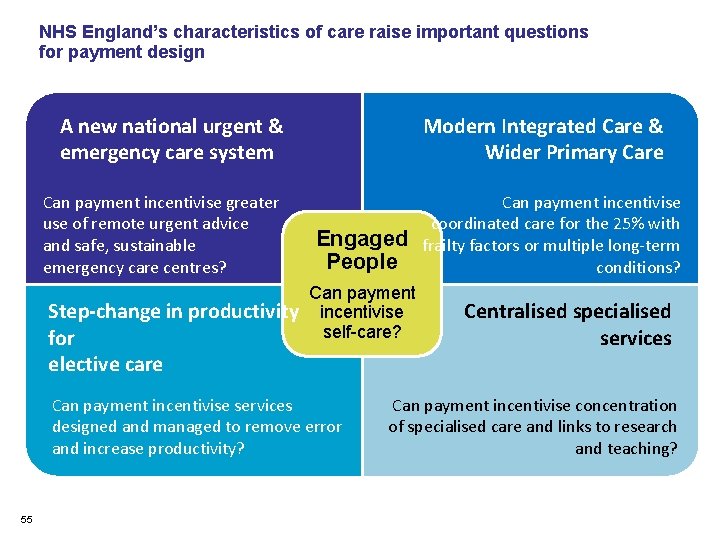
NHS England’s characteristics of care raise important questions for payment design A new national urgent & emergency care system Can payment incentivise greater use of remote urgent advice and safe, sustainable emergency care centres? Step-change in productivity for elective care Modern Integrated Care & Wider Primary Care Engaged People Can payment incentivise self-care? Can payment incentivise services designed and managed to remove error and increase productivity? 55 Can payment incentivise coordinated care for the 25% with frailty factors or multiple long-term conditions? Centralised specialised services Can payment incentivise concentration of specialised care and links to research and teaching?
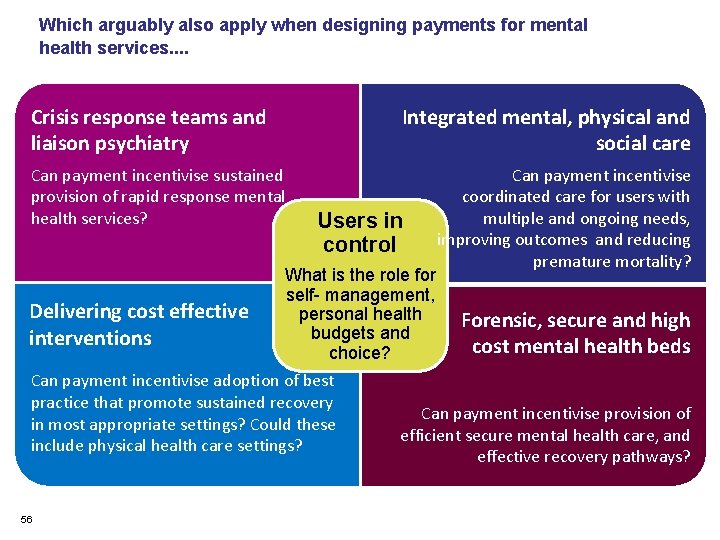
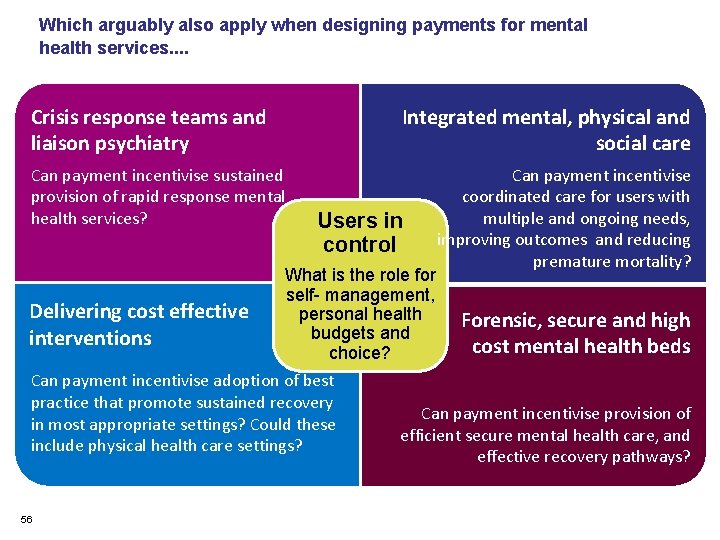
Which arguably also apply when designing payments for mental health services. . Crisis response teams and liaison psychiatry Integrated mental, physical and social care Can payment incentivise sustained provision of rapid response mental health services? Delivering cost effective interventions Can payment incentivise coordinated care for users with multiple and ongoing needs, Users in improving outcomes and reducing control premature mortality? What is the role for self- management, personal health Forensic, secure and high budgets and cost mental health beds choice? Can payment incentivise adoption of best practice that promote sustained recovery in most appropriate settings? Could these include physical health care settings? 56 Can payment incentivise provision of efficient secure mental health care, and effective recovery pathways?
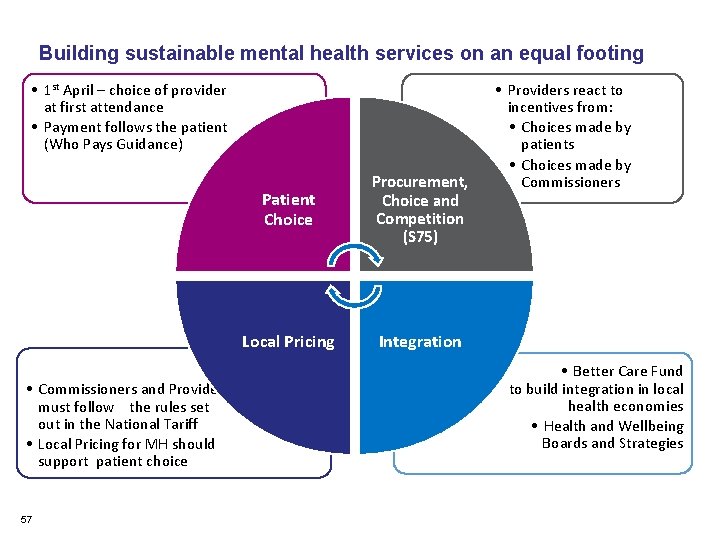
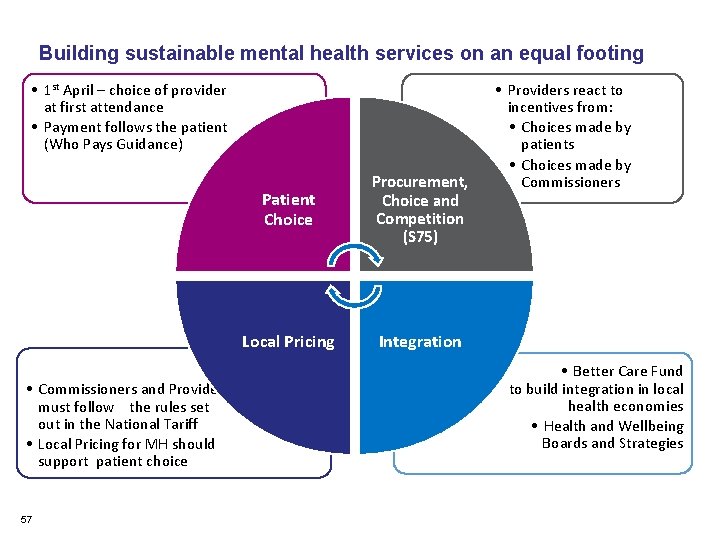
Building sustainable mental health services on an equal footing • 1 st April – choice of provider at first attendance • Payment follows the patient (Who Pays Guidance) • Commissioners and Providers must follow the rules set out in the National Tariff • Local Pricing for MH should support patient choice 57 Patient Choice Procurement, Choice and Competition (S 75) Local Pricing Integration • Providers react to incentives from: • Choices made by patients • Choices made by Commissioners • Better Care Fund to build integration in local health economies • Health and Wellbeing Boards and Strategies
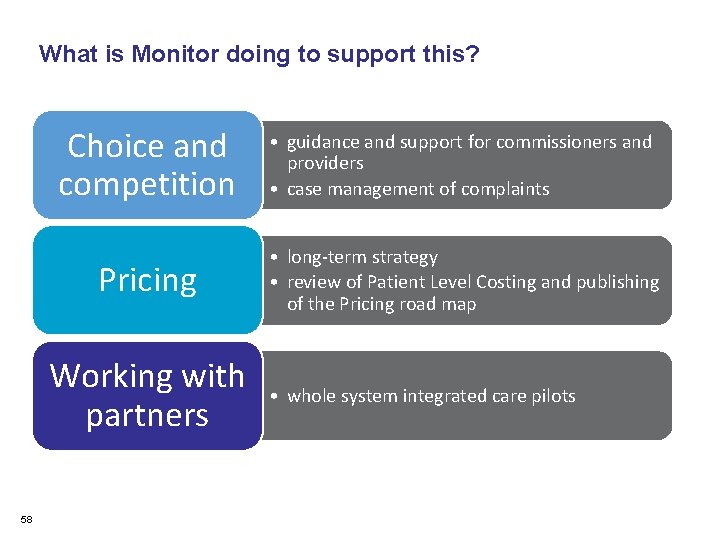
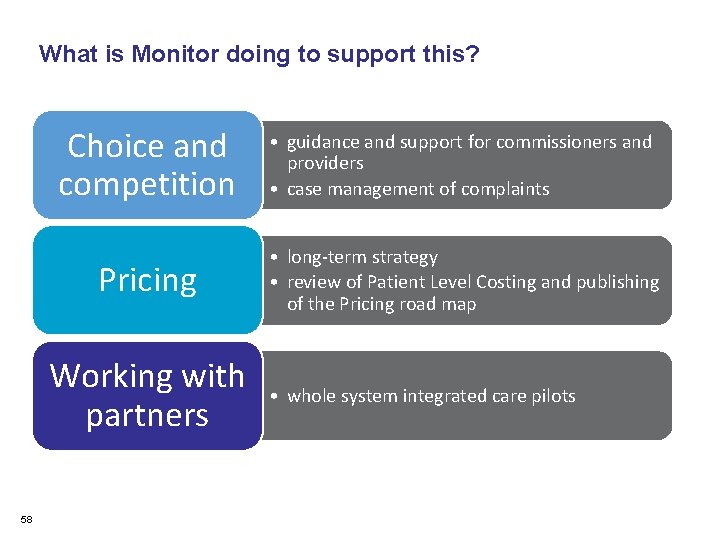
What is Monitor doing to support this? Choice and competition • guidance and support for commissioners and providers • case management of complaints Pricing • long-term strategy • review of Patient Level Costing and publishing of the Pricing road map Working with partners 58 • whole system integrated care pilots
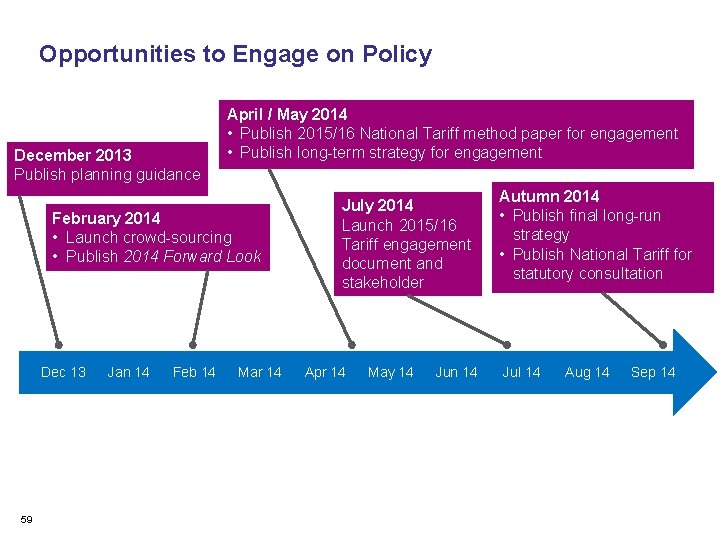
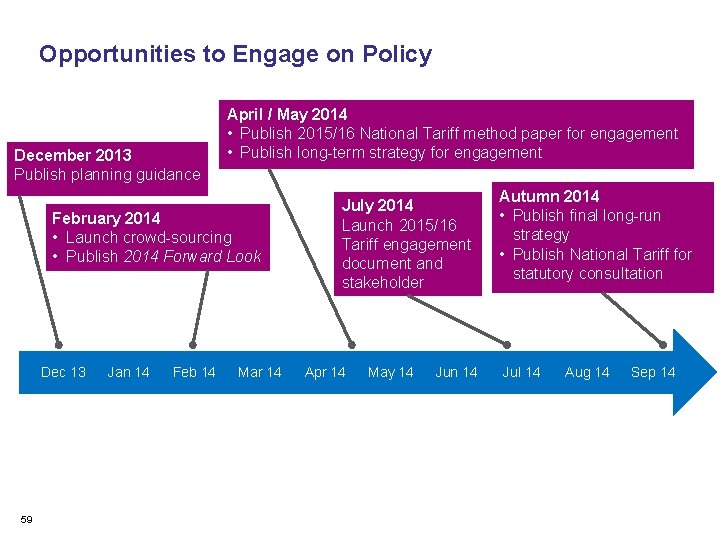
Opportunities to Engage on Policy December 2013 Publish planning guidance April / May 2014 • Publish 2015/16 National Tariff method paper for engagement • Publish long-term strategy for engagement February 2014 • Launch crowd-sourcing • Publish 2014 Forward Look Dec 13 59 Jan 14 Feb 14 Mar 14 July 2014 Launch 2015/16 Tariff engagement document and stakeholder engagement Apr 14 May 14 Jun 14 Autumn 2014 • Publish final long-run strategy • Publish National Tariff for statutory consultation Jul 14 Aug 14 Sep 14
Opportunities to Engage on Policy Monitor and NHS England’s long-term strategy will be accompanied by a number of supporting documents on specific areas, including: - enabling long-term conditions care coordination - delivering Keogh’s urgent & emergency care networks - aligning incentives - options for multi-year tariff cycles - next steps for mental health 60
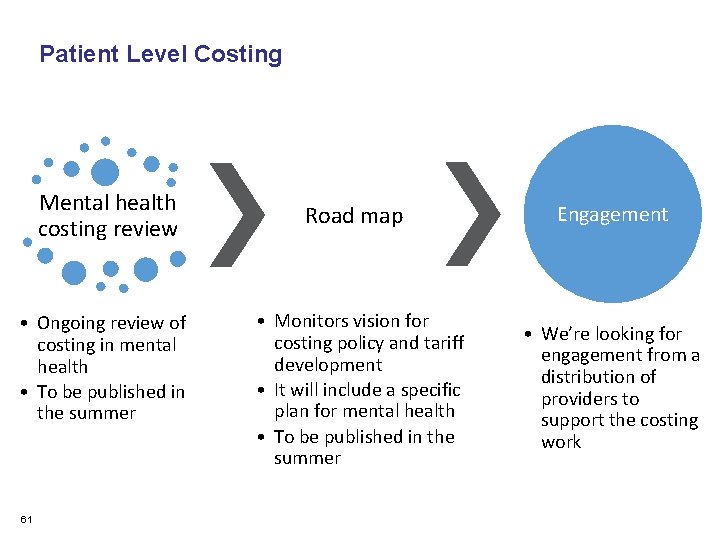
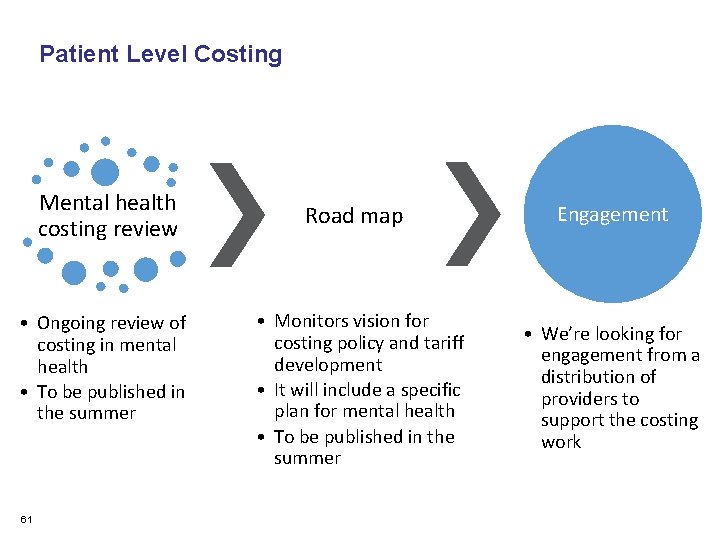
Patient Level Costing Mental health costing review • Ongoing review of costing in mental health • To be published in the summer 61 Road map Engagement • Monitors vision for costing policy and tariff development • It will include a specific plan for mental health • To be published in the summer • We’re looking for engagement from a distribution of providers to support the costing work
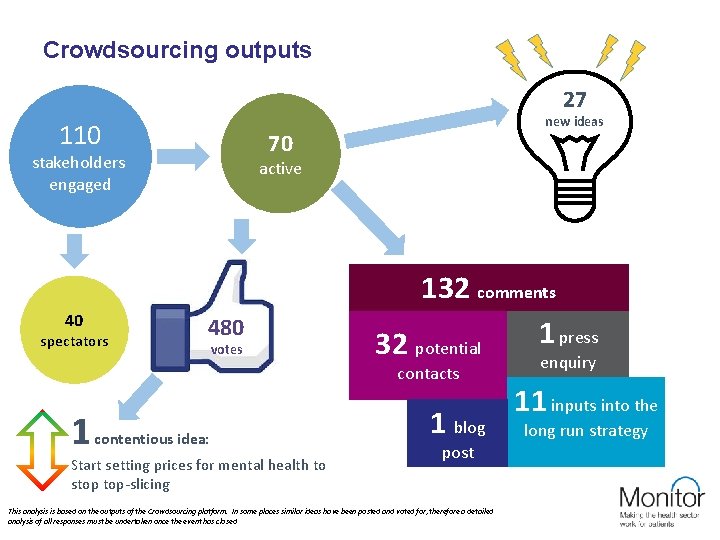
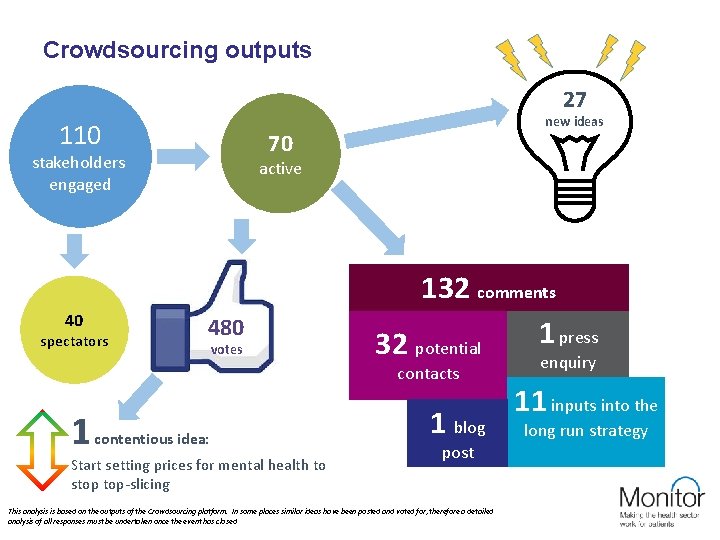
Crowdsourcing outputs 27 110 70 stakeholders engaged 40 spectators new ideas active 480 votes 132 comments 1 press 32 potential contacts 1 contentious idea: Start setting prices for mental health to stop top-slicing 1 blog post This analysis is based on the outputs of the Crowdsourcing platform. In some places similar ideas have been posted and voted for, therefore a detailed analysis of all responses must be undertaken once the event has closed enquiry 11 inputs into the long run strategy
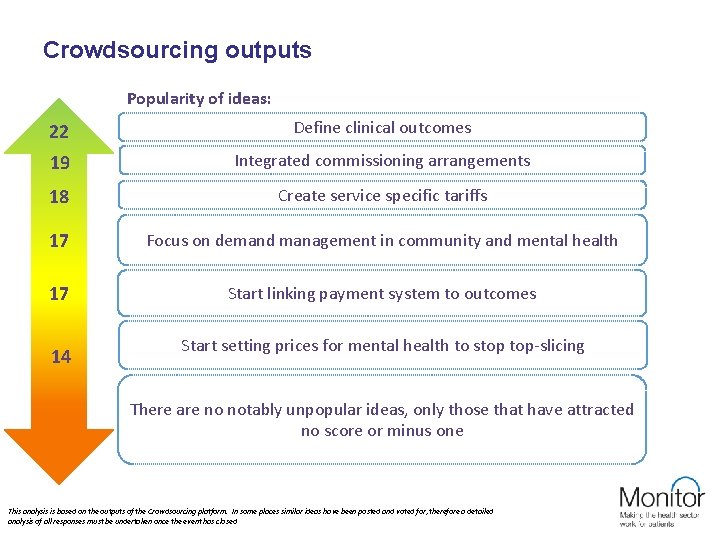
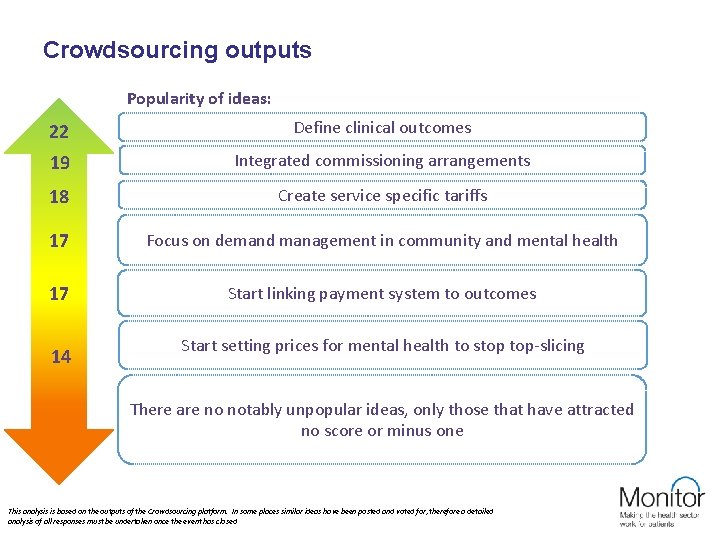
Crowdsourcing outputs Popularity of ideas: 22 Define clinical outcomes 19 Integrated commissioning arrangements 18 Create service specific tariffs 17 Focus on demand management in community and mental health 17 Start linking payment system to outcomes 14 Start setting prices for mental health to stop top-slicing There are no notably unpopular ideas, only those that have attracted no score or minus one This analysis is based on the outputs of the Crowdsourcing platform. In some places similar ideas have been posted and voted for, therefore a detailed analysis of all responses must be undertaken once the event has closed
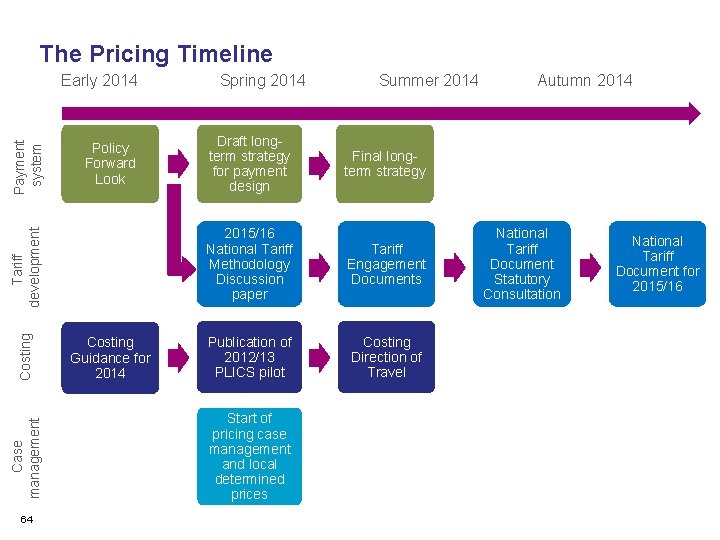
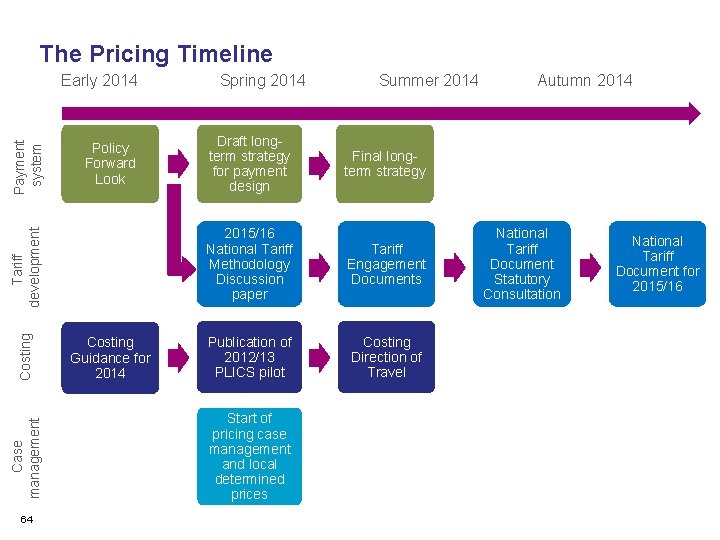
The Pricing Timeline Policy Forward Look Case management Costing Tariff development Payment system Early 2014 64 Costing Guidance for 2014 Spring 2014 Draft longterm strategy for payment design Summer 2014 Final longterm strategy 2015/16 National Tariff Methodology Discussion paper Tariff Engagement Documents Publication of 2012/13 PLICS pilot Costing Direction of Travel Start of pricing case management and local determined prices Autumn 2014 National Tariff Document Statutory Consultation National Tariff Document for 2015/16
Inspecting mental health services David Behan, Chief Executive, Care Quality Commission Chair: Stephen Dalton, Chief Executive, Mental Health Network #MHN 2014

David Behan Chief Executive 26 March 2014 Mental Health Network Annual Conference
• Our purpose We make sure health and social care services provide people with safe, effective, compassionate, high-quality care and we encourage care services to improve 2

Asking the right questions about quality and safety Is the care: Safe? Effective? Caring? Responsive to people’s needs? Well-led? 68
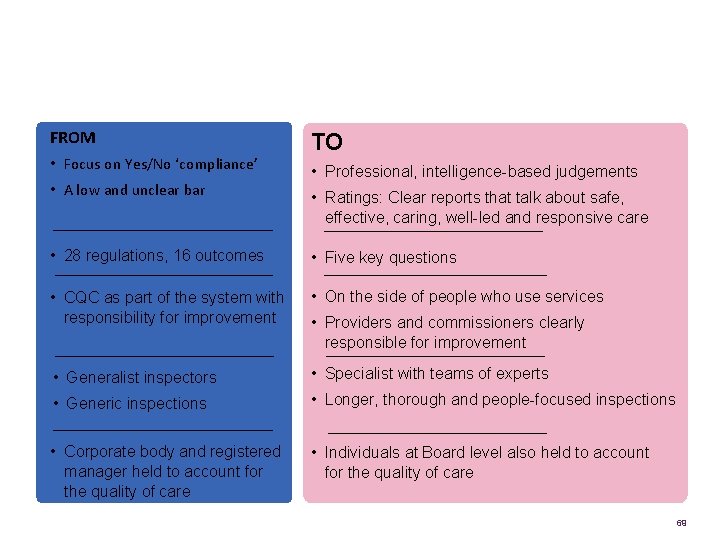
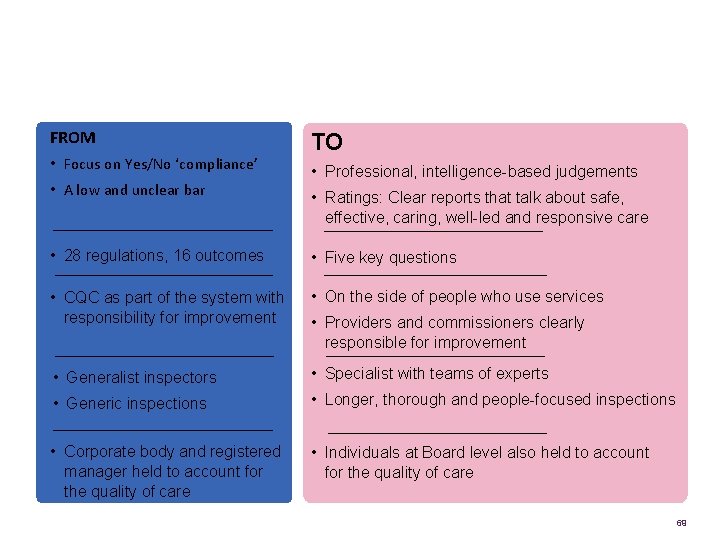
What will be different FROM • Focus on Yes/No ‘compliance’ • A low and unclear bar TO • Professional, intelligence-based judgements • Ratings: Clear reports that talk about safe, effective, caring, well-led and responsive care • 28 regulations, 16 outcomes • Five key questions • CQC as part of the system with responsibility for improvement • On the side of people who use services • Generalist inspectors • Specialist with teams of experts • Generic inspections • Longer, thorough and people-focused inspections • Corporate body and registered manager held to account for the quality of care • Individuals at Board level also held to account for the quality of care • Providers and commissioners clearly responsible for improvement 69
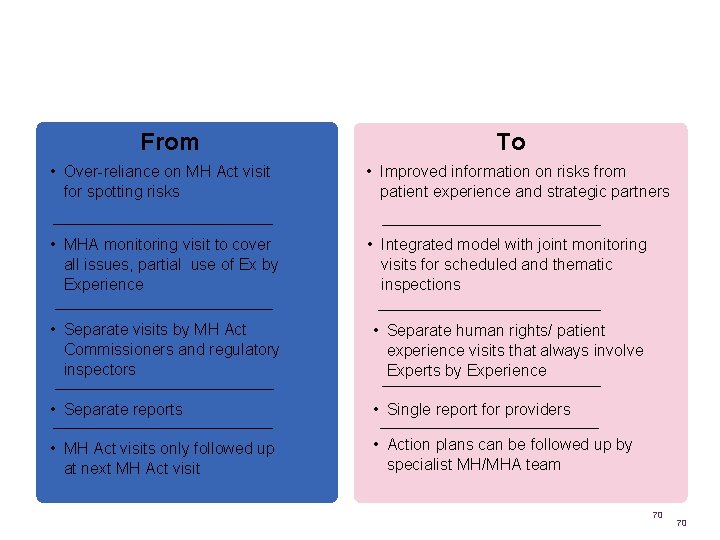
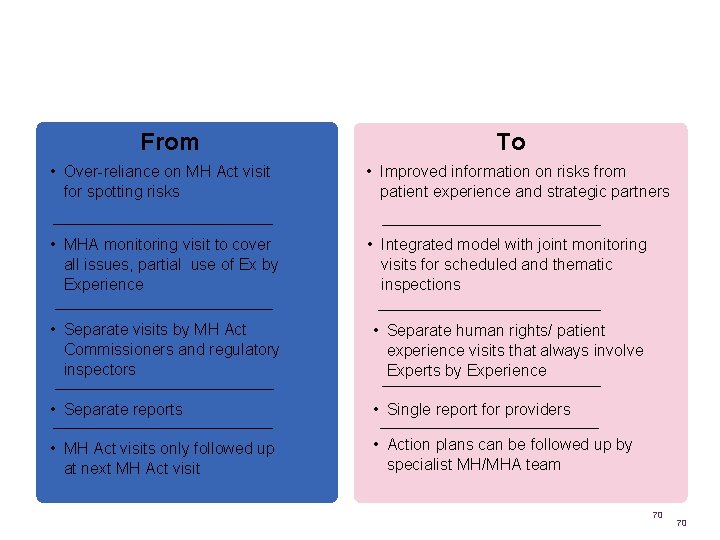
What will be different for mental health providers? From To • Over-reliance on MH Act visit for spotting risks • Improved information on risks from patient experience and strategic partners • MHA monitoring visit to cover all issues, partial use of Ex by Experience • Integrated model with joint monitoring visits for scheduled and thematic inspections • Separate visits by MH Act Commissioners and regulatory inspectors • Separate human rights/ patient experience visits that always involve Experts by Experience • Separate reports • Single report for providers • MH Act visits only followed up at next MH Act visit • Action plans can be followed up by specialist MH/MHA team 70 70

Our new approach 71
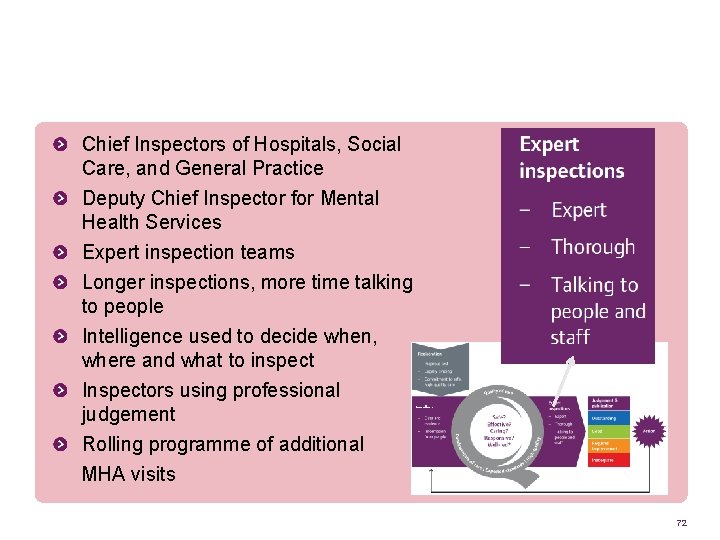
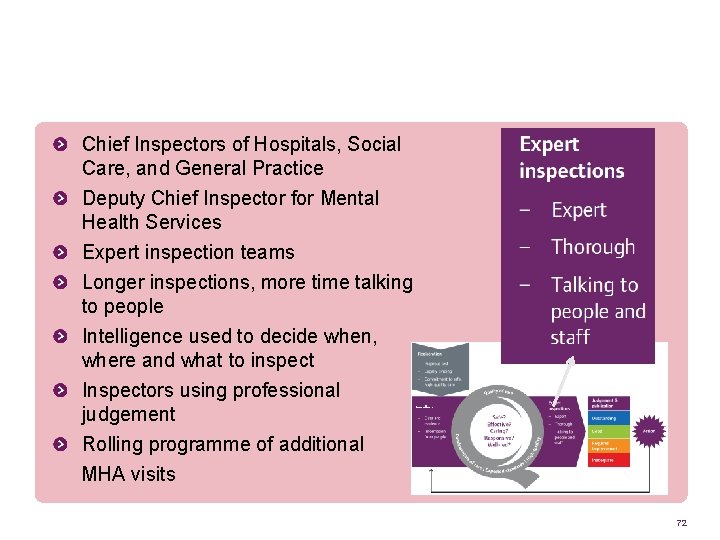
Inspection Chief Inspectors of Hospitals, Social Care, and General Practice Deputy Chief Inspector for Mental Health Services Expert inspection teams Longer inspections, more time talking to people Intelligence used to decide when, where and what to inspect Inspectors using professional judgement Rolling programme of additional MHA visits Surveillance 72

Ratings to help people choose between services and to encourage improvement Ratings for providers, and for separate services as well? Ratings for each question? o o o Safe Effective Caring Responsive to people’s needs Well-led 73

Where are we now? Three ‘wave 1’ pilot inspections complete (apart from report) • Coventry and Warwickshire • Devon • Dudley and Walsall Two more this month • South West London and St George’s • Solent 74
What next? Eight more planned for April-June • • • Nottinghamshire Birmingham & Solihull Avon and Wiltshire Calderstones Camden & Islington Humber Bradford Surrey & Borders Isle of Wight (led by acute) Five sites selected for July – September • Includes independent sector providers 75
Keynote address: Sir David Nicholson, Chief Executive, NHS England #MHN 2014

Chair’s summary Shaun Clee, Chair Mental Health Network

Thank you for attending The future of mental health #MHN 2014 Help us improve the quality of future events by completing the evaluation form #MHN 2014
 Conpot github
Conpot github Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Mental health jeopardy questions
Mental health jeopardy questions Future perfect continuous example
Future perfect continuous example Future continuous and future perfect
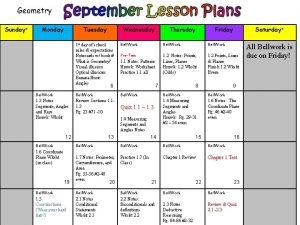
Future continuous and future perfect Monday tuesday wednesday thursday friday calendar
Monday tuesday wednesday thursday friday calendar Wednesday evening prayer
Wednesday evening prayer Wednesday seminar
Wednesday seminar History ia grade boundaries
History ia grade boundaries Web analytics wednesday
Web analytics wednesday How to write wednesday
How to write wednesday Happy wednesday february
Happy wednesday february Monday is my favourite day
Monday is my favourite day Skinny wednesday
Skinny wednesday Flmsg download
Flmsg download Wednesday-saturday
Wednesday-saturday Wise wednesday
Wise wednesday Happy wednesday march
Happy wednesday march Monday tuesday wednesday thursday friday saturday sunday
Monday tuesday wednesday thursday friday saturday sunday English class is wednesday
English class is wednesday Wednesday journal prompts
Wednesday journal prompts Wednesday bellwork
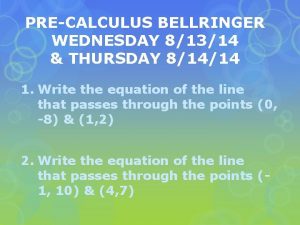
Wednesday bellwork Wednesday bellringer
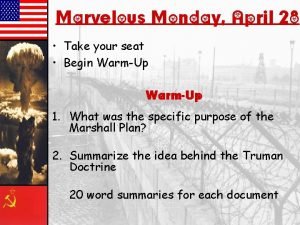
Wednesday bellringer Marvelous monday terrific tuesday wonderful wednesday
Marvelous monday terrific tuesday wonderful wednesday Sunday moday
Sunday moday Wednesday bellwork
Wednesday bellwork Wednesday good morning
Wednesday good morning Thursday prayer
Thursday prayer Wednesday bell ringer
Wednesday bell ringer Wednesday syllables
Wednesday syllables Borwick hall outdoor education centre
Borwick hall outdoor education centre Happy wednesday
Happy wednesday Happy wednesday
Happy wednesday Thursday prayer images
Thursday prayer images Fe exam results wednesday
Fe exam results wednesday Wednesday phonics
Wednesday phonics Sunday monday tuesday wednesday
Sunday monday tuesday wednesday Monday=621 tuesday=732 wednesday=933
Monday=621 tuesday=732 wednesday=933 Monday=621 tuesday=732 wednesday=933
Monday=621 tuesday=732 wednesday=933 Wednesday lo
Wednesday lo Wednesday at 6
Wednesday at 6 Wednesday two of the key
Wednesday two of the key Wednesday
Wednesday Perfect future
Perfect future Future tense of like
Future tense of like Future continuous.
Future continuous. Future nurse future midwife
Future nurse future midwife Present past future continuous tense
Present past future continuous tense How to use present continuous for future
How to use present continuous for future Tense chart
Tense chart Future plans and finished future actions
Future plans and finished future actions Future perfect tense
Future perfect tense Future continuous and future perfect objasnjenje
Future continuous and future perfect objasnjenje Frankston psych ward
Frankston psych ward Lenawee community mental health authority
Lenawee community mental health authority Van buren county cmh
Van buren county cmh The intentional use of unfriendly or offensive behavior
The intentional use of unfriendly or offensive behavior Together for mental health
Together for mental health Mental health act (2007)
Mental health act (2007) Health triangle physical examples
Health triangle physical examples Titles for mental health presentations
Titles for mental health presentations Mental health committee
Mental health committee Kings fund
Kings fund Mental health nursing define
Mental health nursing define Definition of nursing diagnosis
Definition of nursing diagnosis Mental health programme
Mental health programme Objectives of community mental health
Objectives of community mental health Mental health equity
Mental health equity How to make a mind map in photoshop
How to make a mind map in photoshop Middle tennessee mental health institute
Middle tennessee mental health institute Mental health toolbox talk construction
Mental health toolbox talk construction Mental health documentation training
Mental health documentation training Mental health equity
Mental health equity Mental health ordinance
Mental health ordinance Axis 1-5 mental health
Axis 1-5 mental health Learning objectives for mental health
Learning objectives for mental health Mental health and older adults
Mental health and older adults Examples of mental health
Examples of mental health