Whiplash Associated Disorder The pathway from acute to











- Slides: 106
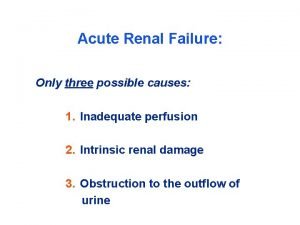
Whiplash Associated Disorder: The pathway from acute to chronic pain (Hours 7 -10) James J. Lehman, DC, FACO Associate Professor of Clinical Sciences Director of Community Health Clinical Education University of Bridgeport
Learning Objectives • Able to demonstrate: • Clinical plan to evaluate and manage a post‐traumatic, whiplash type injury and past history of a “widow maker, ” and numerous nerve compression syndromes • Appropriate interview and differential diagnosis process • Appropriate evaluation process to rule‐in and rule‐out diagnoses • A differential diagnosis that includes a working diagnosis • A continuum of diagnosis as patient progresses with care • Therapeutic recommendations • Prognosis
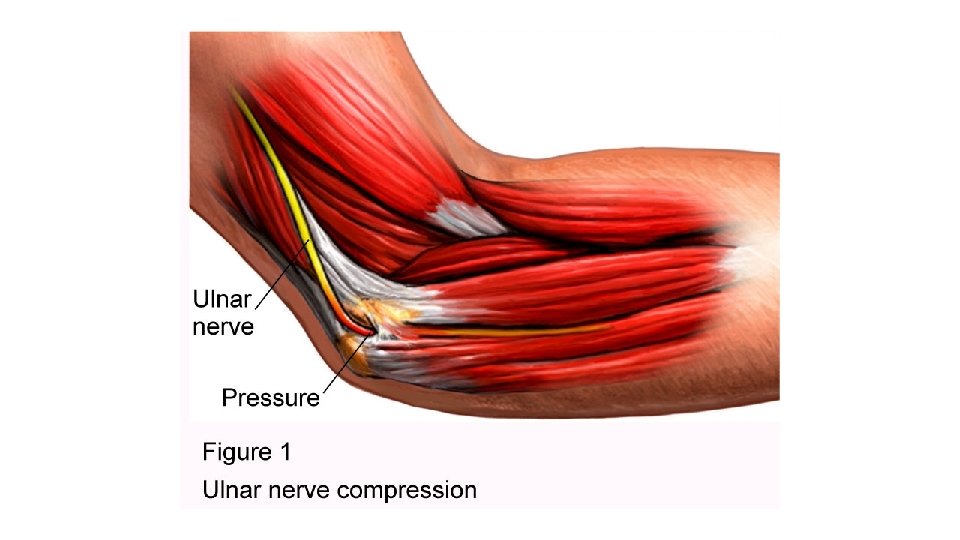
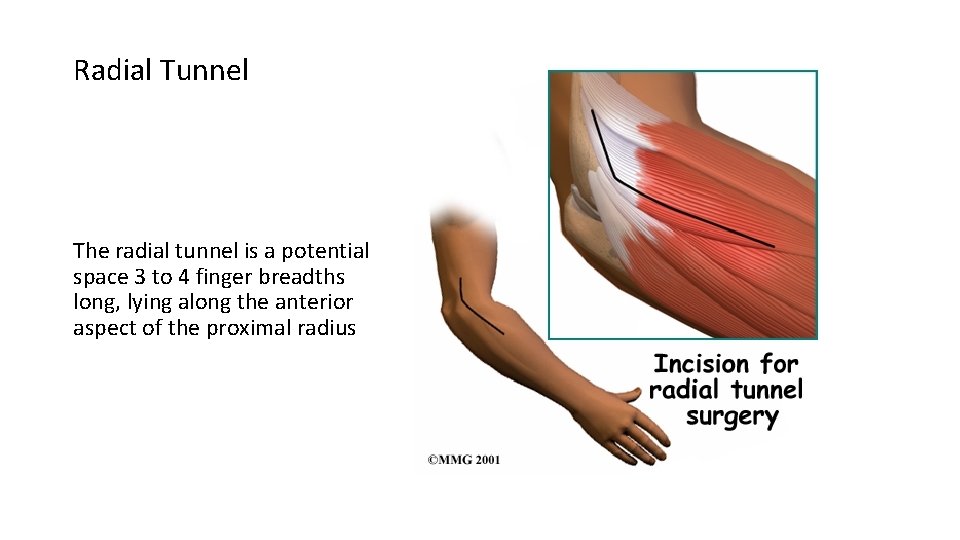
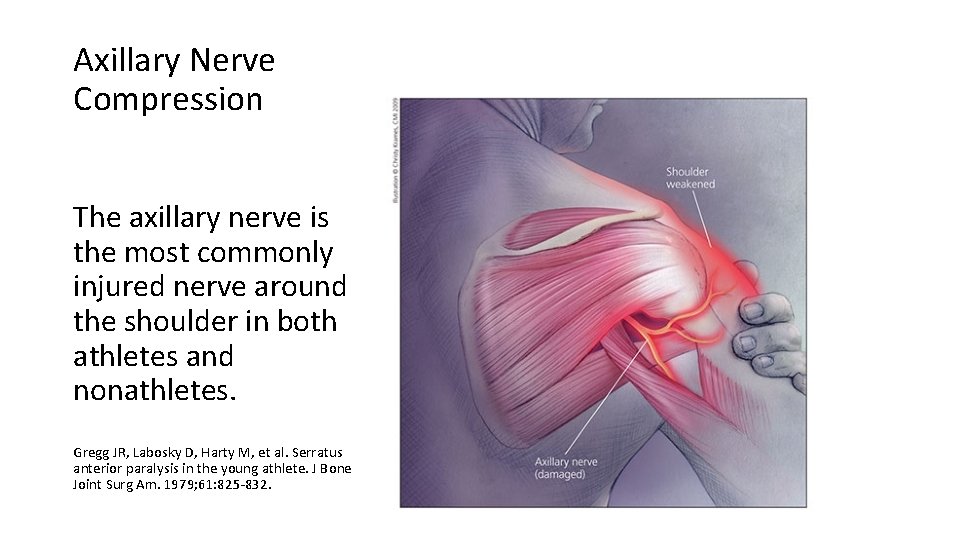
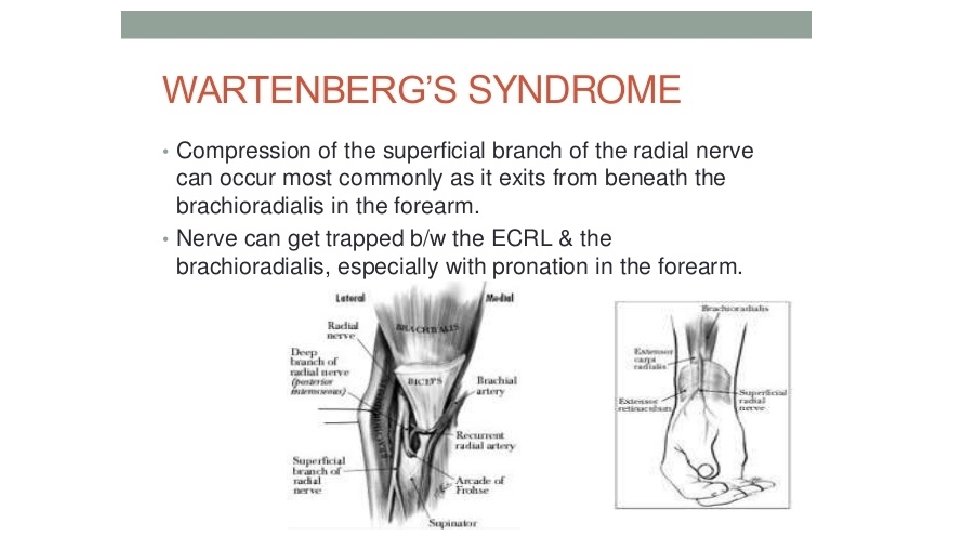
Patient Presentation • 60 year‐old, male, university professor • Chief concern is pain and numbness in the left lower extremity, which started 3 weeks post‐stent implant, with history of whiplash associated disorder. • Past history • Suffered myocardial infarct of the left anterior descending coronary artery 12 months prior to this visit • Several motor vehicle incidents over past 30 years with whiplash associated disorders • Ulnar neuropathy left upper extremity 17 years prior to this visit • Axillary nerve compression left upper extremity 15 years prior to this visit • Cervicobrachial neuropathy right upper extremity 14 years prior to this visit • Radial tunnel syndrome right upper extremity 10 years prior to this visit • Wartenberg’s syndrome left upper extremity 5 years prior to this visit • Responds well to chiropractic management
What is your list of subjective questions regarding the Chief Concern?
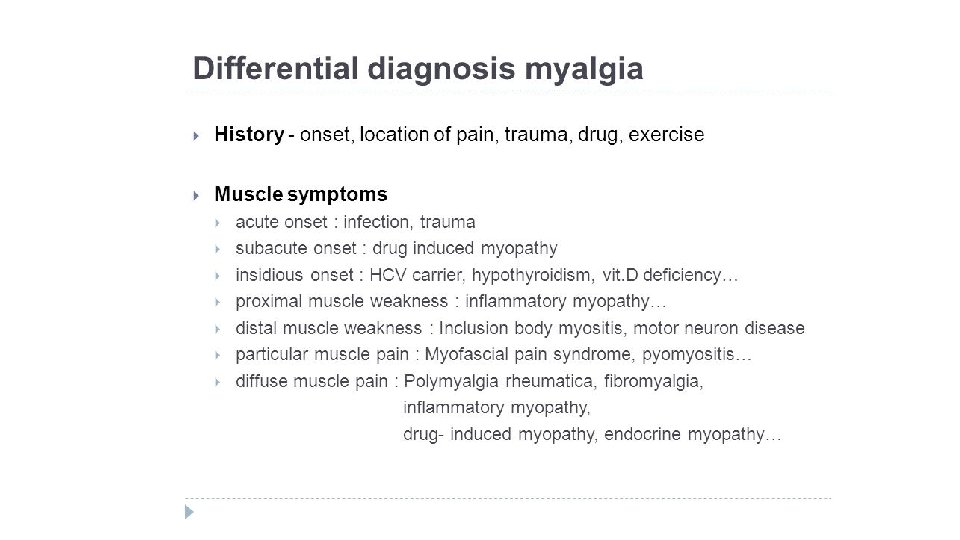
Did you consider a list of Differential Diagnoses for Lower Extremity Condition?
What tests would you perform to rule-in and ruleout your differential diagnoses of Chief Concern?

Did you investigate the post MI care including surgery and medications?


Create list of differential diagnoses regarding Chief Concern

Rule-in and Rule-out with specific questions
Rule-in and rule-out with objective testing and determine working diagnosis
Definition of an orthopedic test • Most often, a provocative maneuver that reproduces the patient’s chief concern pain by stretching, compressing and/or contracting of tissues in order to identify the involved tissues.
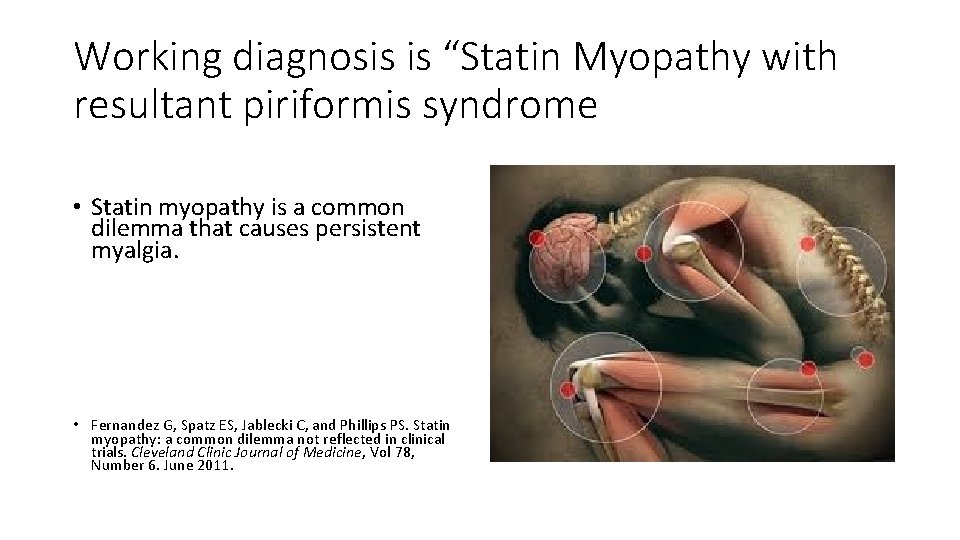
Working diagnosis is “Statin Myopathy with resultant piriformis syndrome • Statin myopathy is a common dilemma that causes persistent myalgia. • Fernandez G, Spatz ES, Jablecki C, and Phillips PS. Statin myopathy: a common dilemma not reflected in clinical trials. Cleveland Clinic Journal of Medicine, Vol 78, Number 6. June 2011.
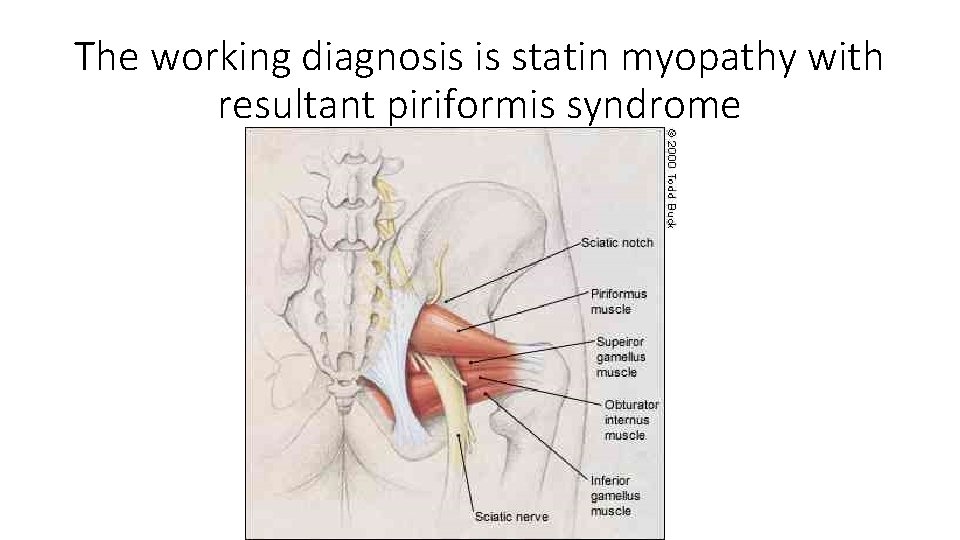
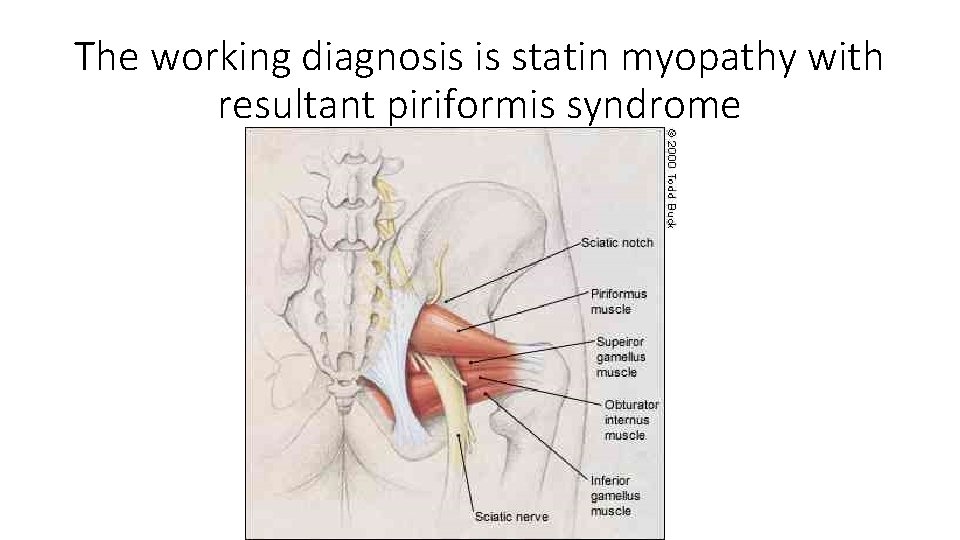
The working diagnosis is statin myopathy with resultant piriformis syndrome


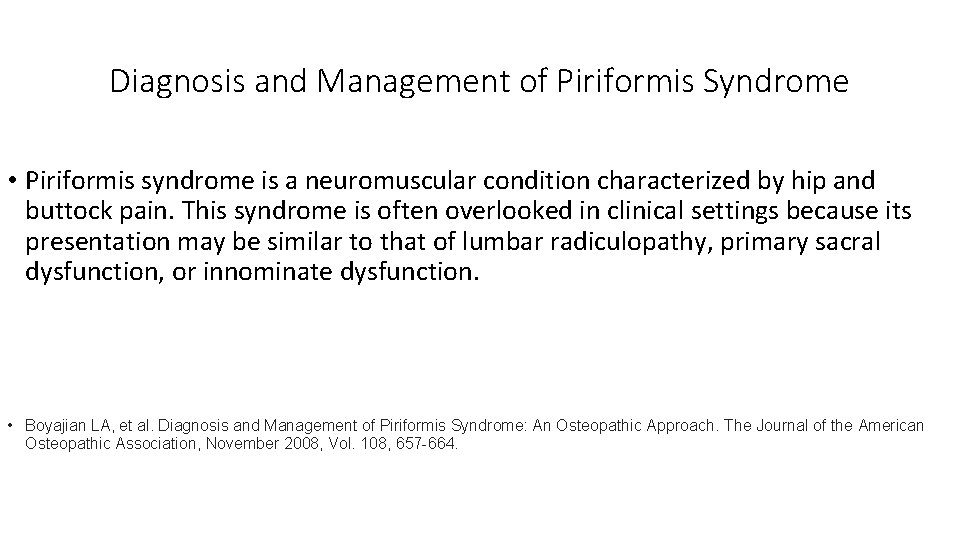
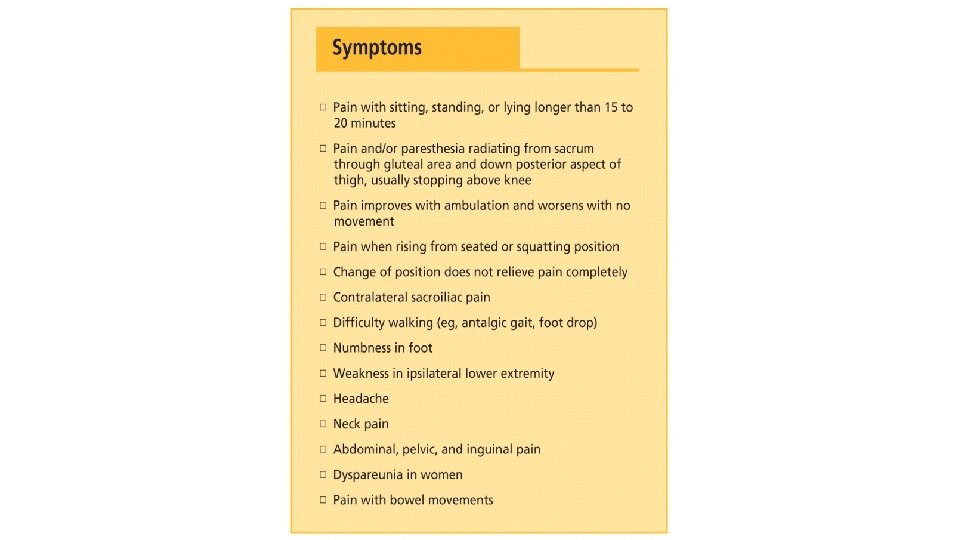
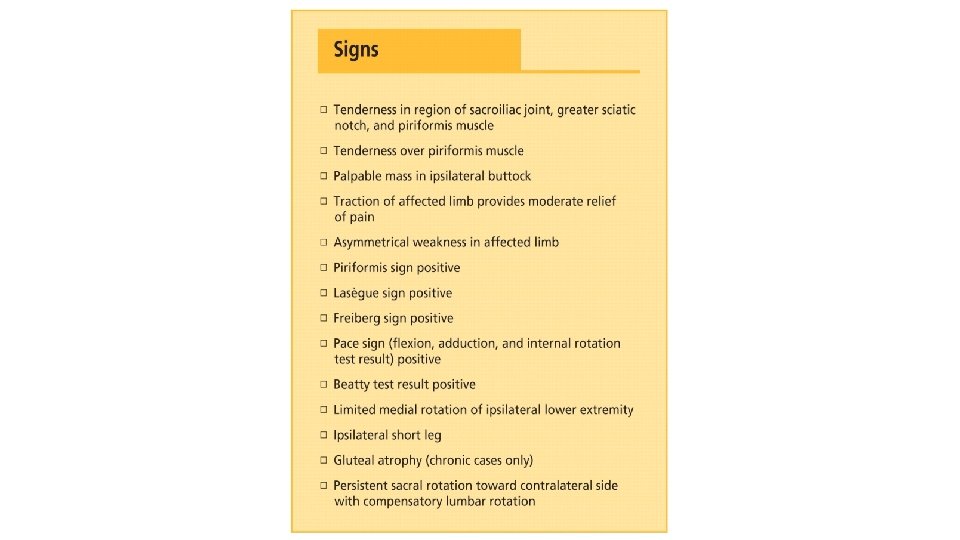
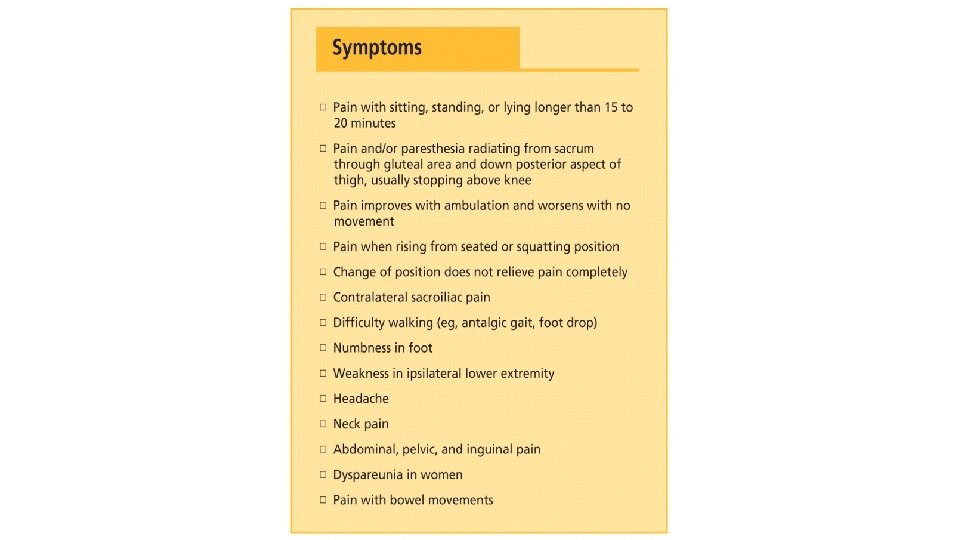
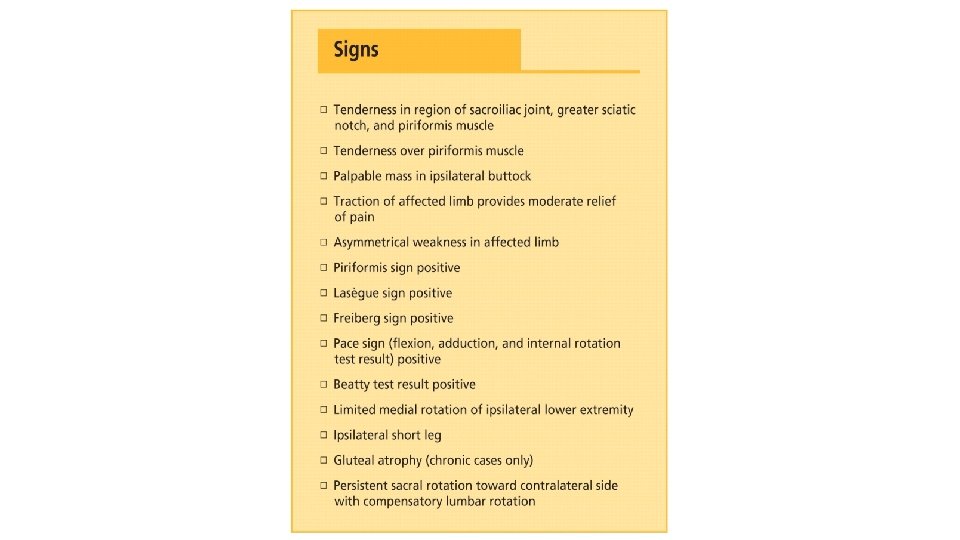
Diagnosis and Management of Piriformis Syndrome • Piriformis syndrome is a neuromuscular condition characterized by hip and buttock pain. This syndrome is often overlooked in clinical settings because its presentation may be similar to that of lumbar radiculopathy, primary sacral dysfunction, or innominate dysfunction. • Boyajian LA, et al. Diagnosis and Management of Piriformis Syndrome: An Osteopathic Approach. The Journal of the American Osteopathic Association, November 2008, Vol. 108, 657 -664.

FAIR Test Flexion, Adduction and Internal Rotation of the affected hip
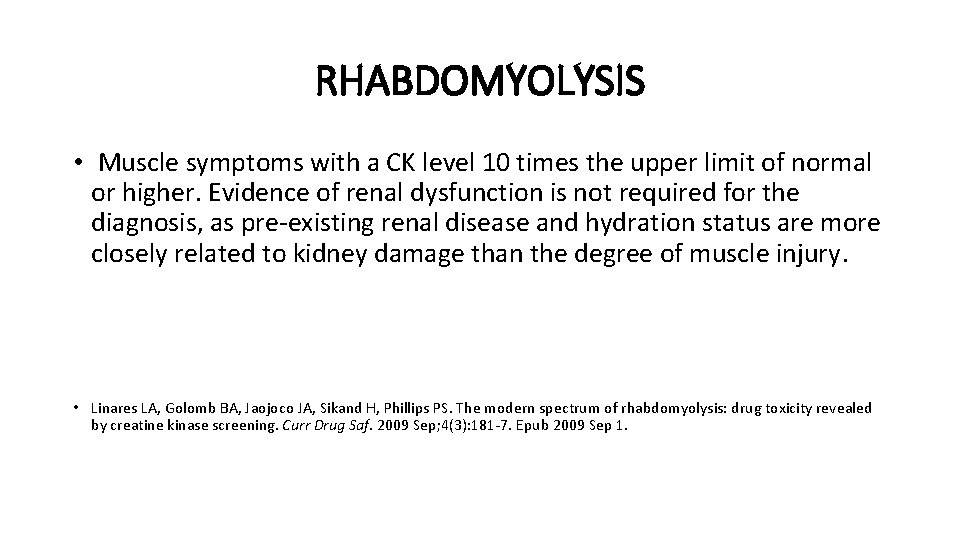
RHABDOMYOLYSIS • Muscle symptoms with a CK level 10 times the upper limit of normal or higher. Evidence of renal dysfunction is not required for the diagnosis, as pre‐existing renal disease and hydration status are more closely related to kidney damage than the degree of muscle injury. • Linares LA, Golomb BA, Jaojoco JA, Sikand H, Phillips PS. The modern spectrum of rhabdomyolysis: drug toxicity revealed by creatine kinase screening. Curr Drug Saf. 2009 Sep; 4(3): 181‐ 7. Epub 2009 Sep 1.
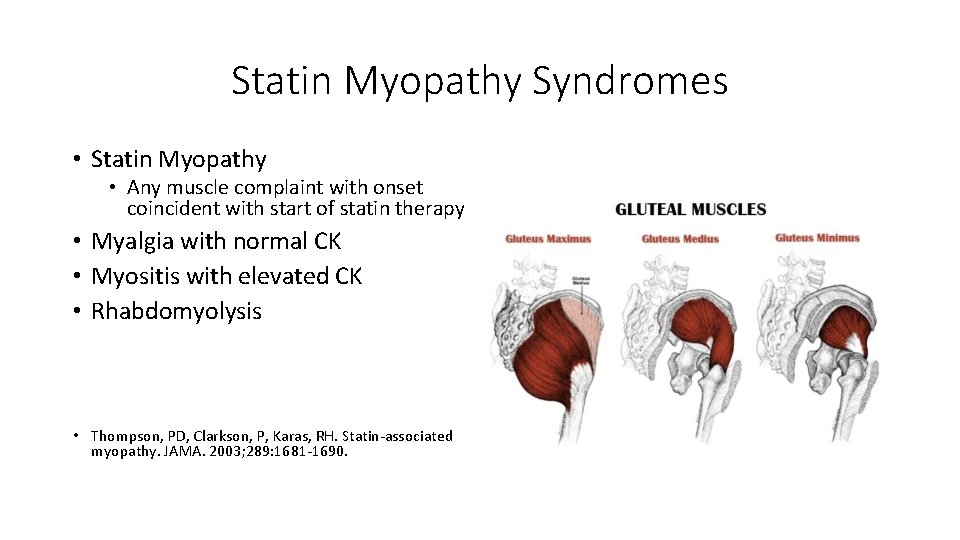
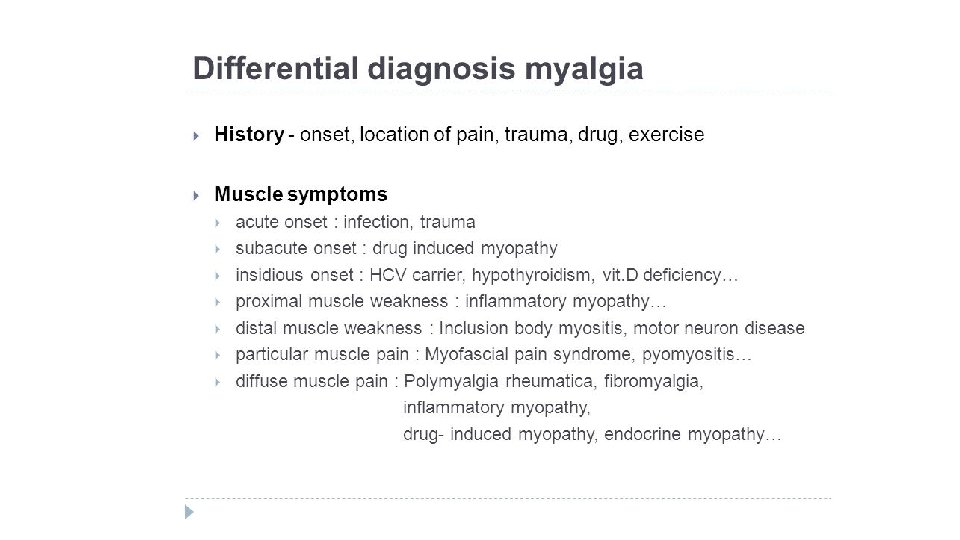
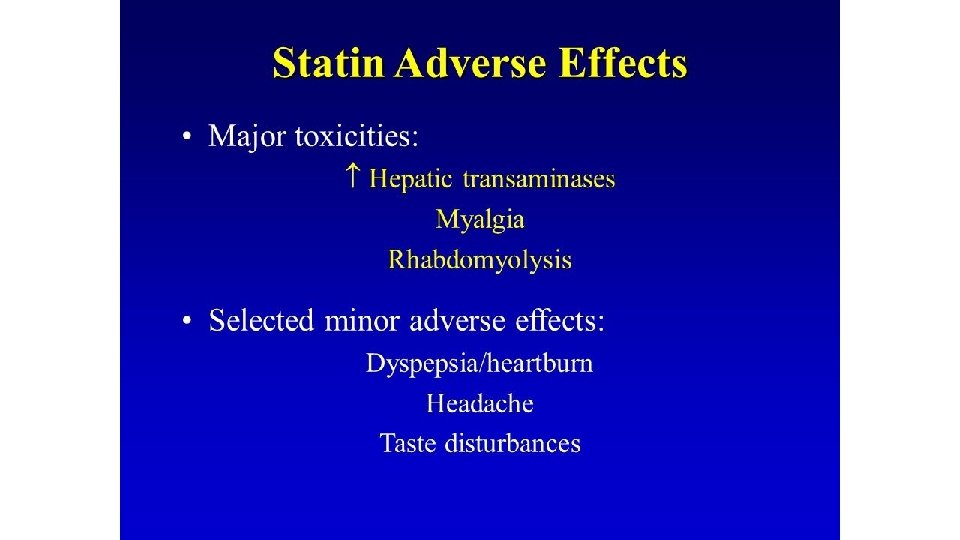
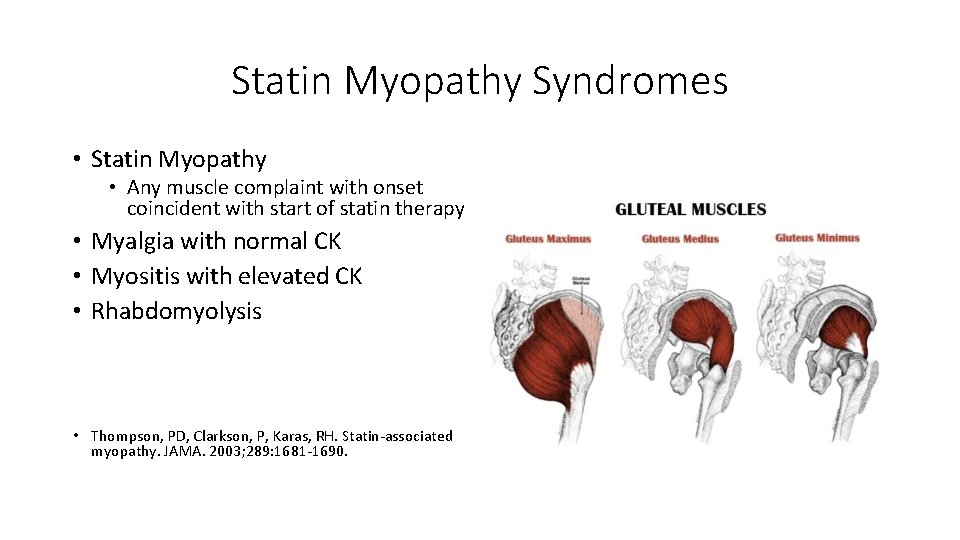
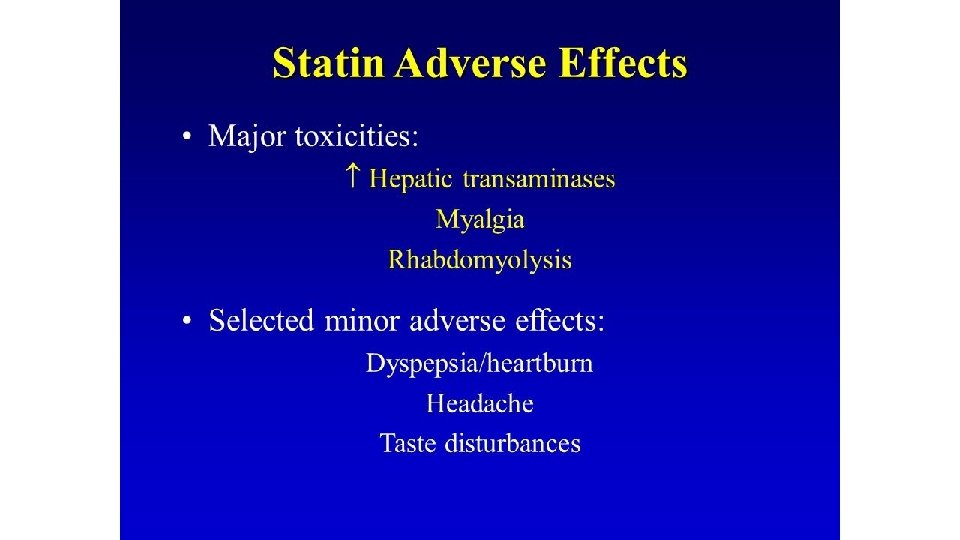
Statin Myopathy Syndromes • Statin Myopathy • Any muscle complaint with onset coincident with start of statin therapy • Myalgia with normal CK • Myositis with elevated CK • Rhabdomyolysis • Thompson, PD, Clarkson, P, Karas, RH. Statin‐associated myopathy. JAMA. 2003; 289: 1681‐ 1690.

Caveat Emptor • Perhaps more dangerous, statins provide false reassurances that may discourage patients from taking the steps that actually reduce cardiovascular disease. • According to the World Health Organization, 80 percent of cardiovascular disease is caused by smoking, lack of exercise, an unhealthy diet, and other lifestyle factors. • Statins give the illusion of protection to many people, who would be much better served, for example, by simply walking an extra 10 minutes per day. JOHN D. ABRAMSON and RITA F. REDBERG. Don’t Give More Patients Statins. NYT. Published: November 13, 2013.
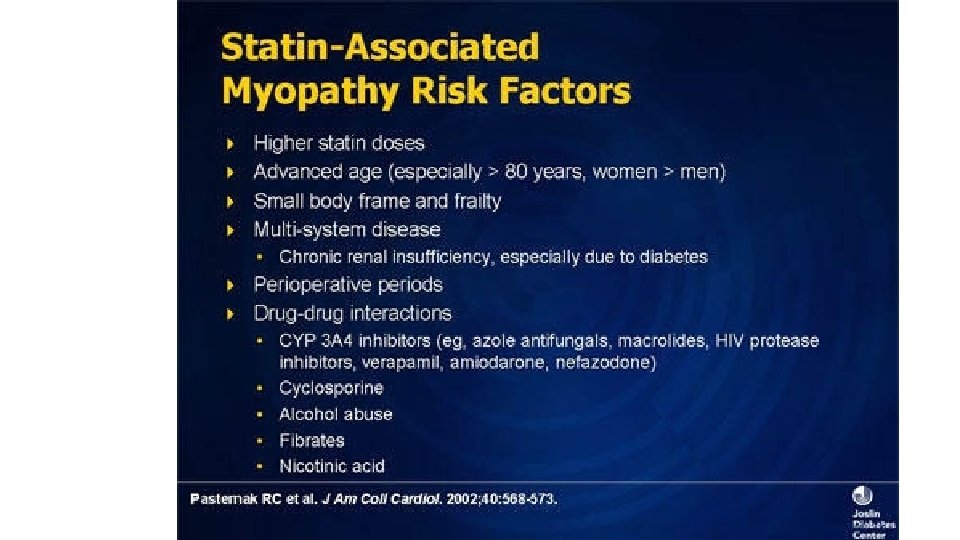
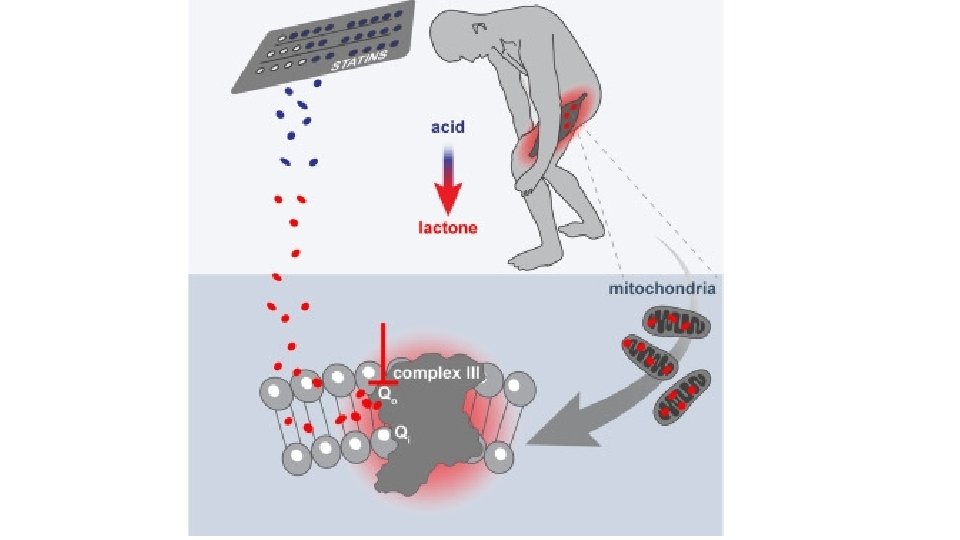
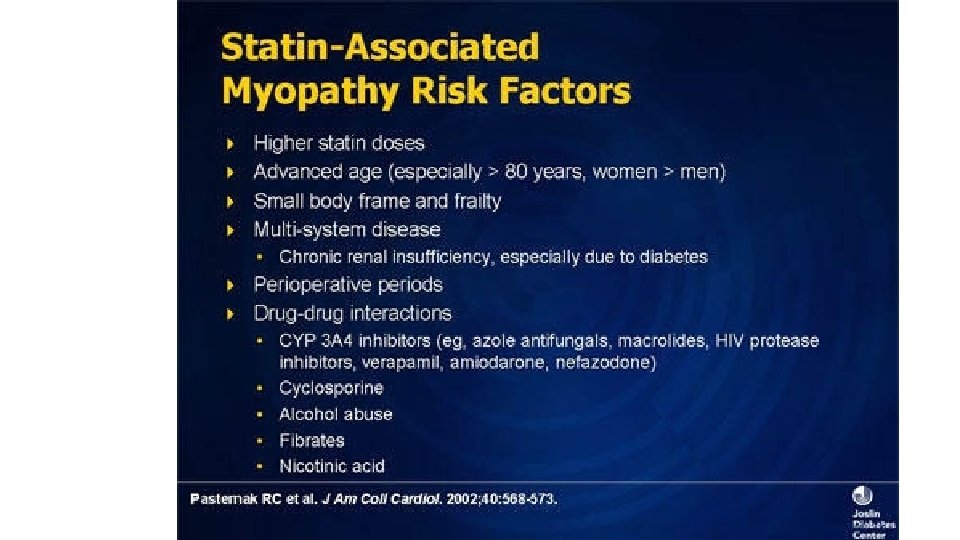
Statin Myopathy • Statins are associated with adverse side effects of skeletal myopathy.
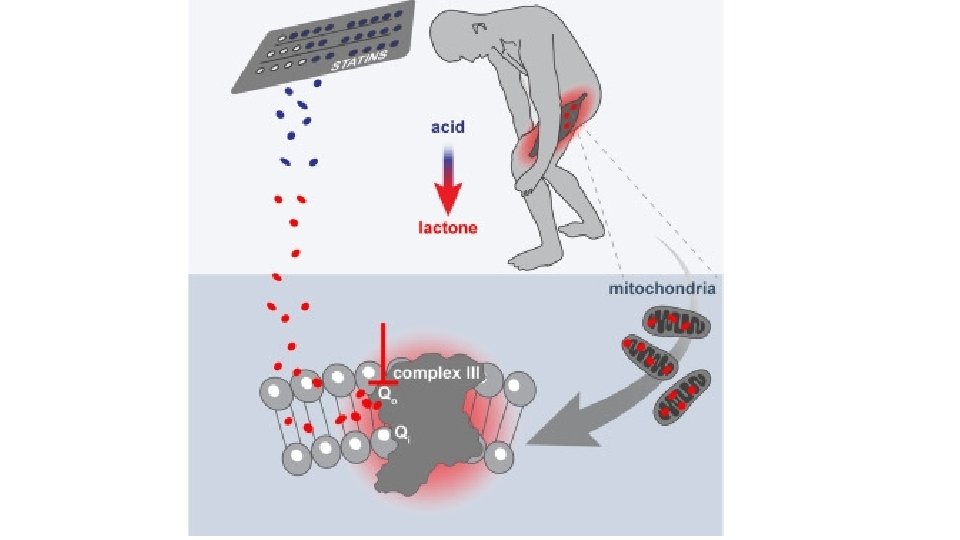
Statin Myopathy • Statin treatment reduces ubiquinone levels in the cholesterol synthesis pathway, which may be associated with mitochondrial dysfunction. In addition, reactive oxygen species (ROS) production and apoptosis induced by statins may provide cellular and molecular mechanisms in skeletal myopathy. • Kwak HB. Statin‐induced Myopathy in Skeletal Muscle: the Role of Exercise. J Lifestyle Med. 2014 Sep; 4(2): 71‐ 9. doi: 10. 15280/jlm. 2014. 4. 2. 71. Epub 2014 Sep 30.
Statin Myopathy Symptoms • The myopathies are neuromuscular disorders in which the primary symptom is muscle weakness due to dysfunction of muscle fiber.
Statin Myopathy Symptoms • Other symptoms of statin myopathy can include muscle cramps, stiffness, and spasm.
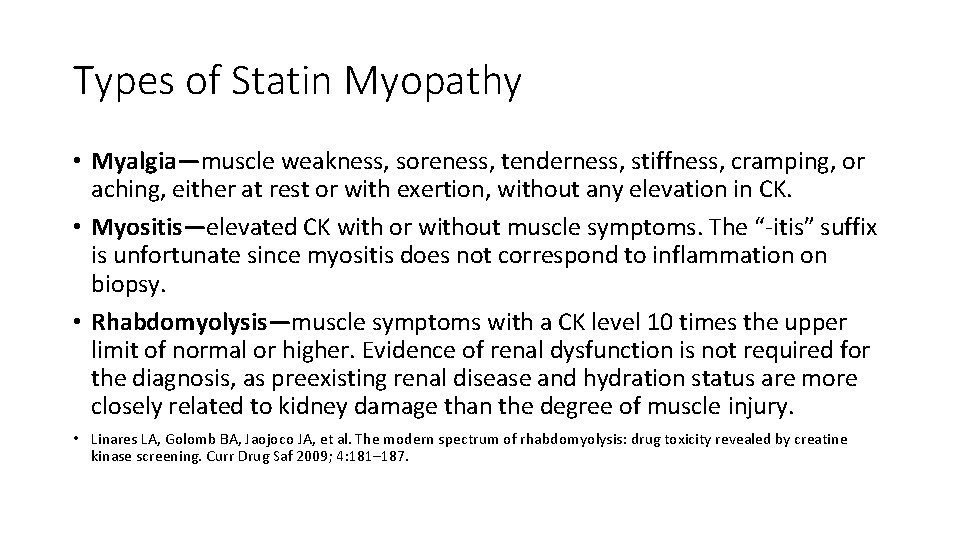
Types of Statin Myopathy • Myalgia—muscle weakness, soreness, tenderness, stiffness, cramping, or aching, either at rest or with exertion, without any elevation in CK. • Myositis—elevated CK with or without muscle symptoms. The “‐itis” suffix is unfortunate since myositis does not correspond to inflammation on biopsy. • Rhabdomyolysis—muscle symptoms with a CK level 10 times the upper limit of normal or higher. Evidence of renal dysfunction is not required for the diagnosis, as preexisting renal disease and hydration status are more closely related to kidney damage than the degree of muscle injury. • Linares LA, Golomb BA, Jaojoco JA, et al. The modern spectrum of rhabdomyolysis: drug toxicity revealed by creatine kinase screening. Curr Drug Saf 2009; 4: 181– 187.
Physician Denial Eighty‐seven percent of patients reportedly spoke to their physician about the possible connection between statin use and their symptom. Golomb BA, Mc. Graw JJ, Evans MA, Dimsdale JE. Physician response to patient reports of adverse drug effects: implications for patient‐targeted adverse effect surveillance. Drug Saf. 2007; 30(8): 669‐ 75.
Physician Denial • Patients reported that they and not the doctor most commonly initiated the discussion regarding the possible connection of drug to symptom (98% vs 2% cognition survey, 96% vs 4% neuropathy survey, 86% vs 14% muscle survey; p < 10(‐ 8) for each). • Physicians were reportedly more likely to deny than affirm the possibility of a connection. • Golomb BA, Mc. Graw JJ, Evans MA, Dimsdale JE. Physician response to patient reports of adverse drug effects: implications for patient‐targeted adverse effect surveillance. Drug Saf. 2007; 30(8): 669‐ 75.
Physician Denial CONCLUSIONS • Since low reporting rates are considered to contribute to delays in identification of adverse drug reactions (ADRs), findings from this study suggest that additional putative cases may be identified by targeting patients as reporters, potentially speeding recognition of ADRs. • Golomb BA, Mc. Graw JJ, Evans MA, Dimsdale JE. Physician response to patient reports of adverse drug effects: implications for patient‐targeted adverse effect surveillance. Drug Saf. 2007; 30(8): 669‐ 75.
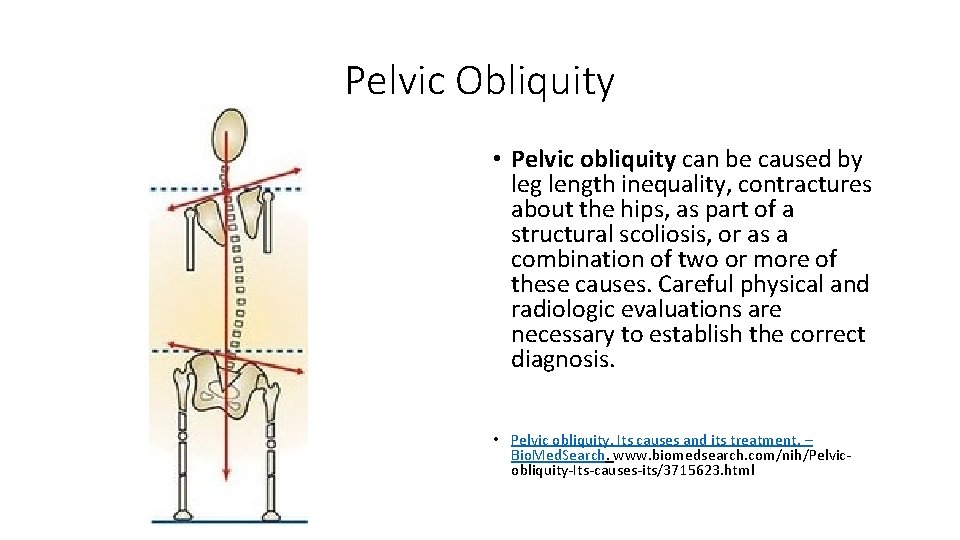
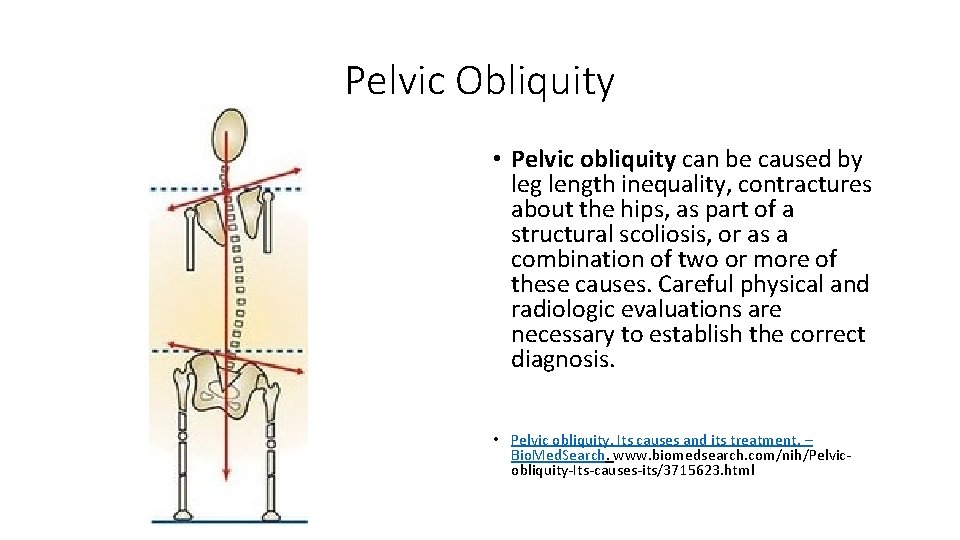
Pelvic Obliquity • Pelvic obliquity can be caused by leg length inequality, contractures about the hips, as part of a structural scoliosis, or as a combination of two or more of these causes. Careful physical and radiologic evaluations are necessary to establish the correct diagnosis. • Pelvic obliquity. Its causes and its treatment. – Bio. Med. Search. www. biomedsearch. com/nih/Pelvic‐ obliquity‐Its‐causes‐its/3715623. html
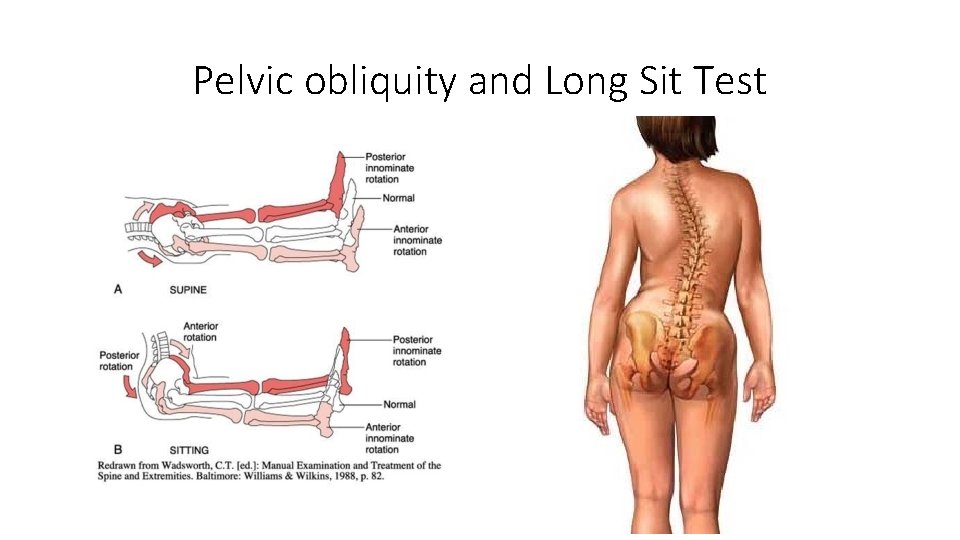
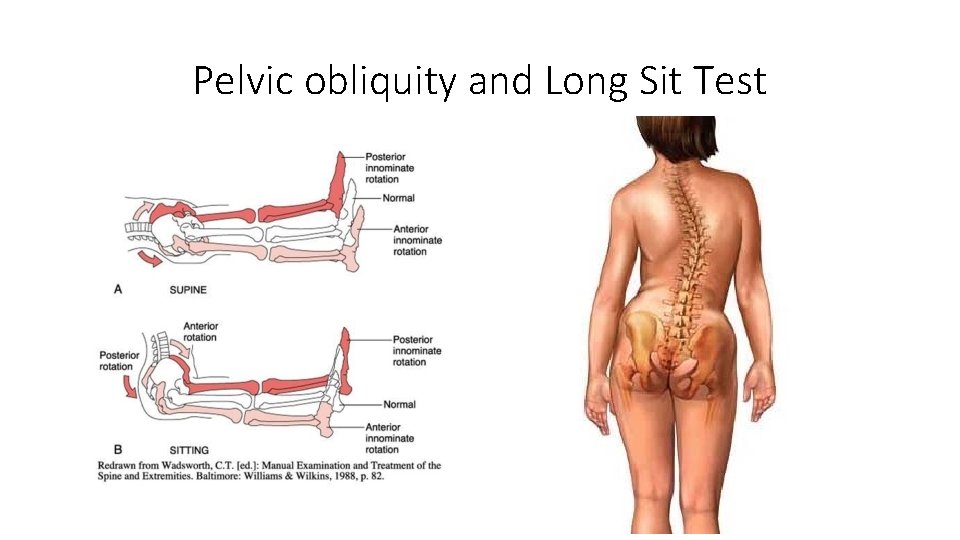
Pelvic obliquity and Long Sit Test
Long Sit Test • Terry Bemis, et al. Validation of the Long Sitting Test on Subjects with lliosacral Dysfunction. JOSPT January 1987. • Available from: https: //www. jospt. org/doi/pdf/10. 25 19/jospt. 1987. 8. 7. 336
Is this patient presenting with a posttraumatic chronic pain syndrome?
How Would You Manage a Patient with Statin Myopathy?
Why so many neuropathies?
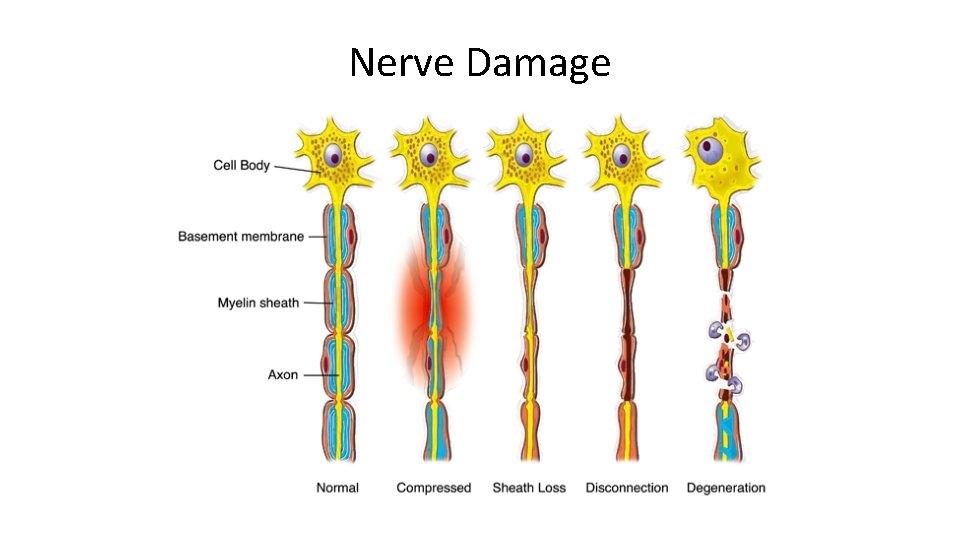
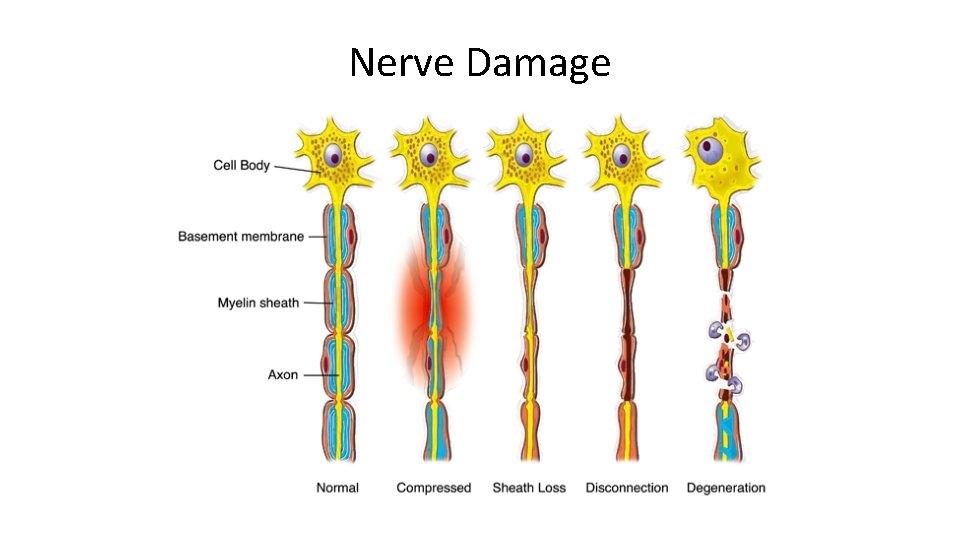
Nerve Damage
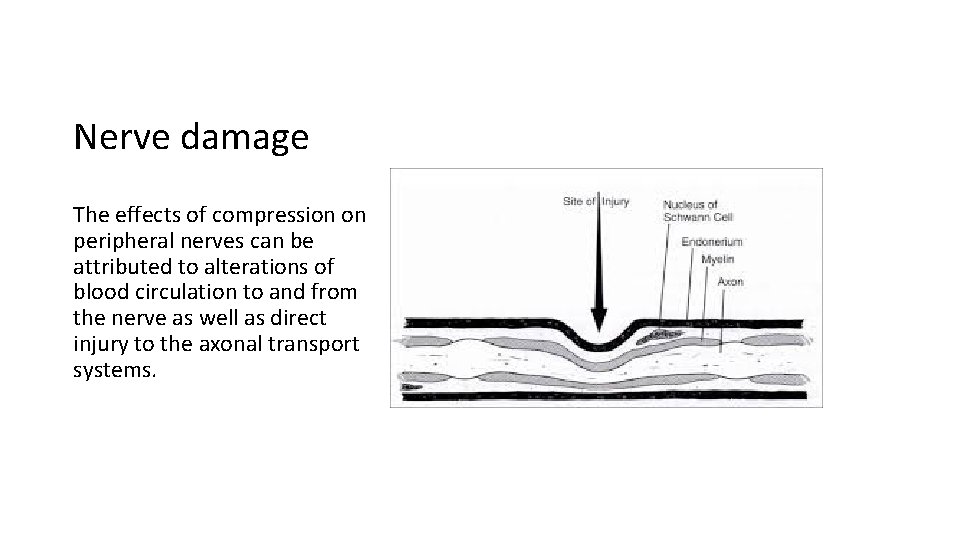
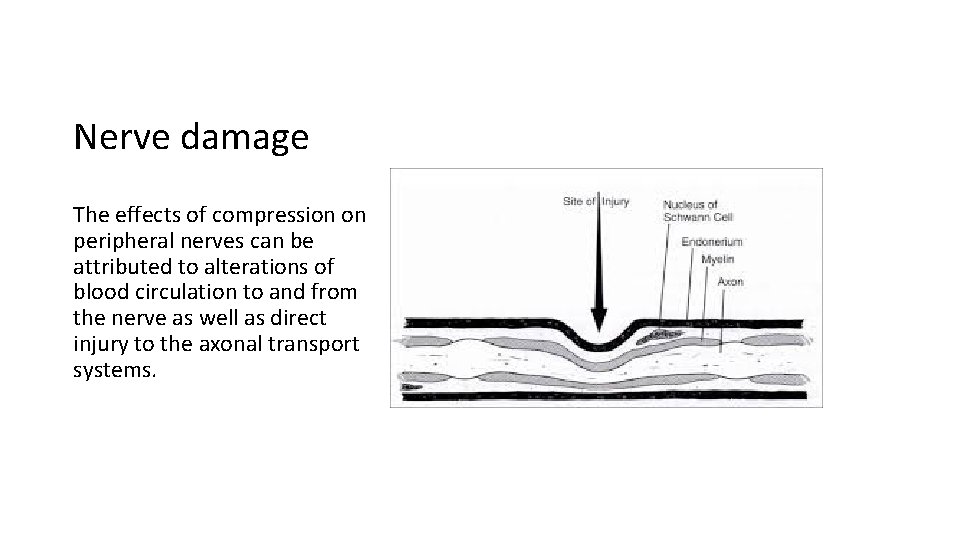
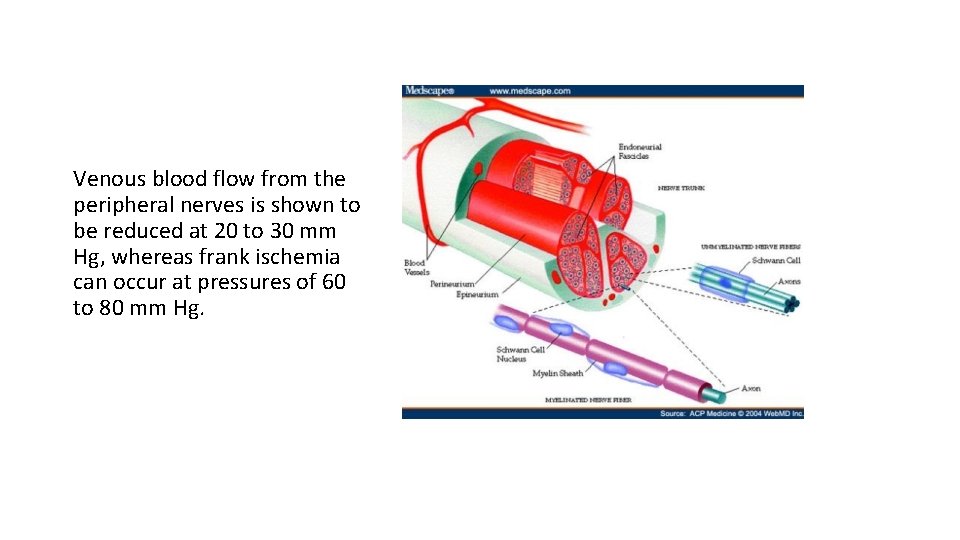
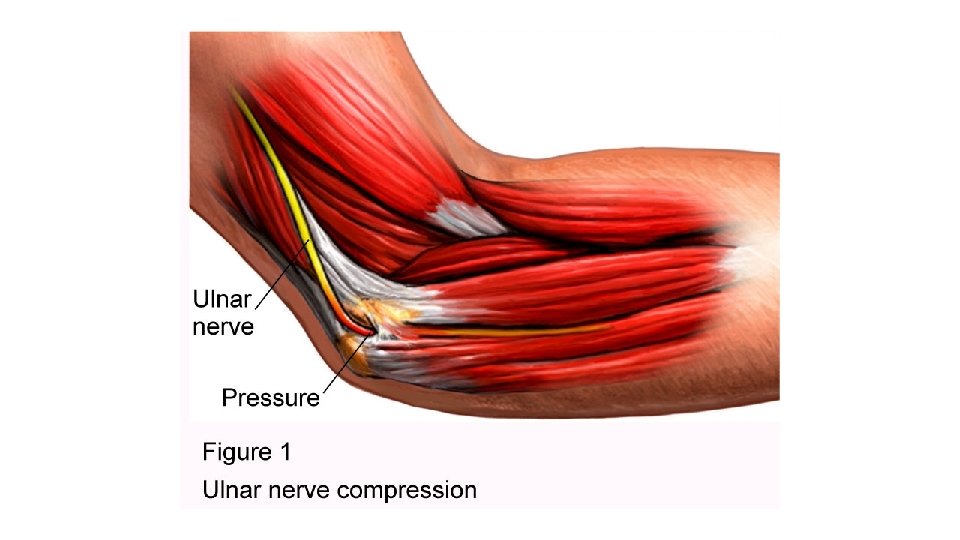
Nerve damage The effects of compression on peripheral nerves can be attributed to alterations of blood circulation to and from the nerve as well as direct injury to the axonal transport systems.
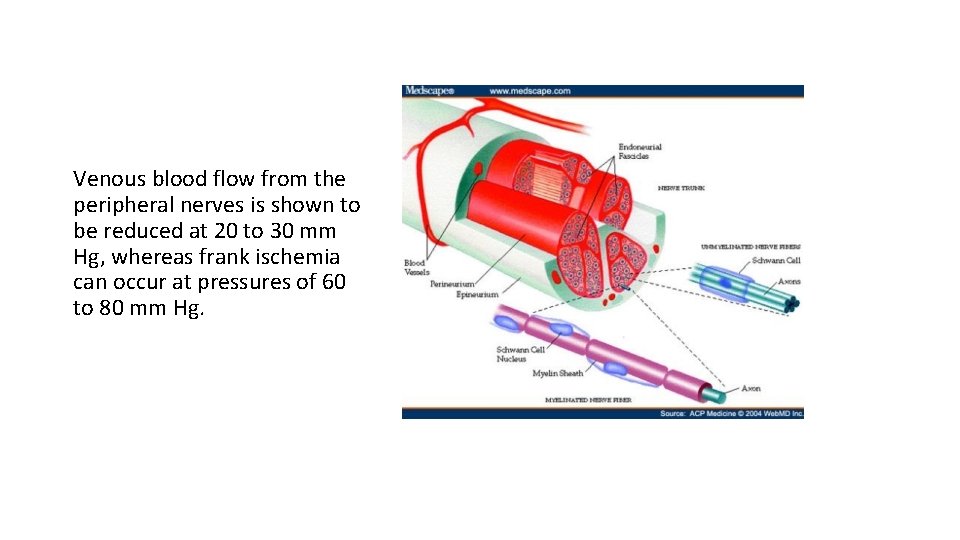
Venous blood flow from the peripheral nerves is shown to be reduced at 20 to 30 mm Hg, whereas frank ischemia can occur at pressures of 60 to 80 mm Hg.
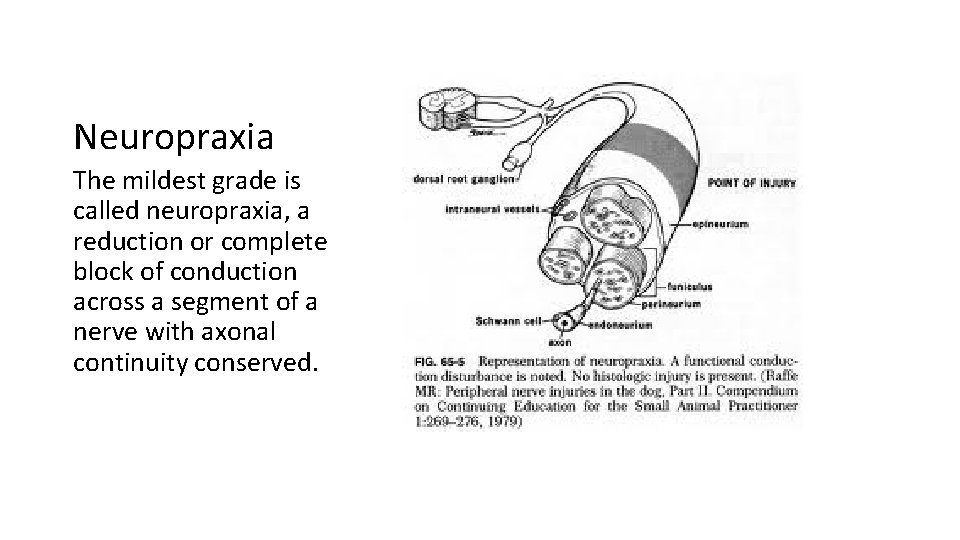
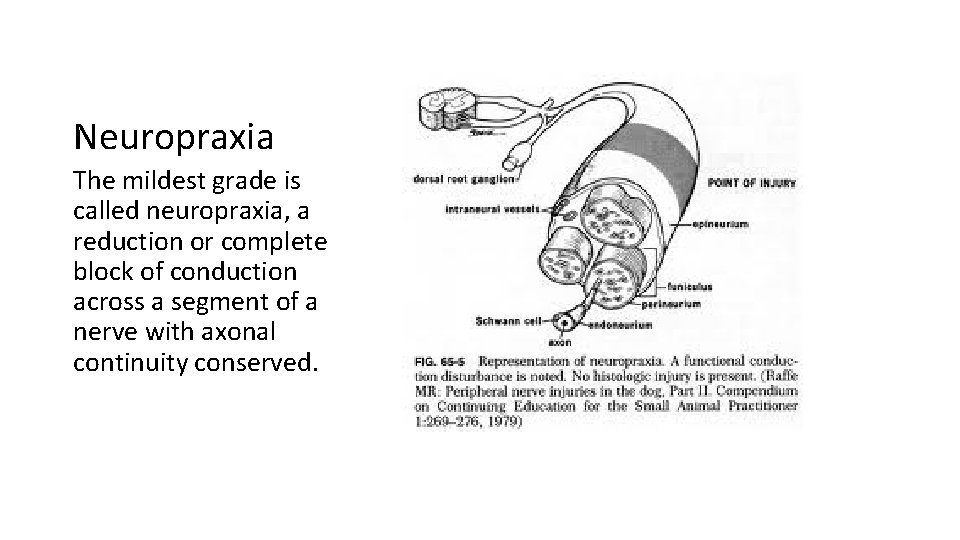
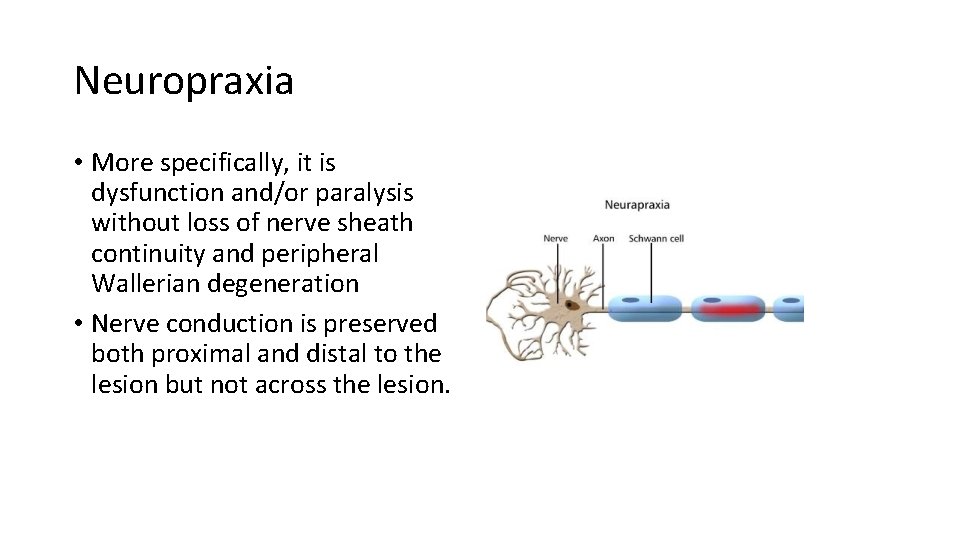
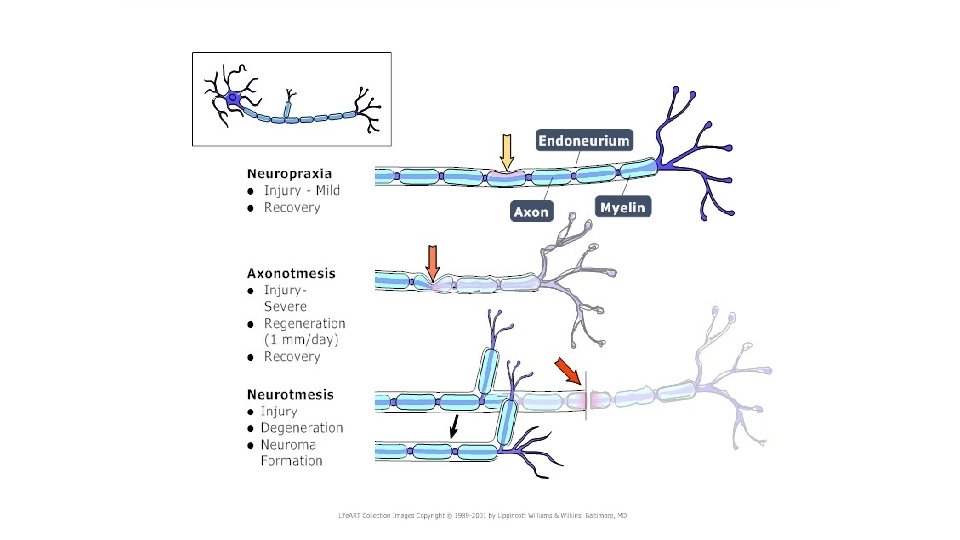
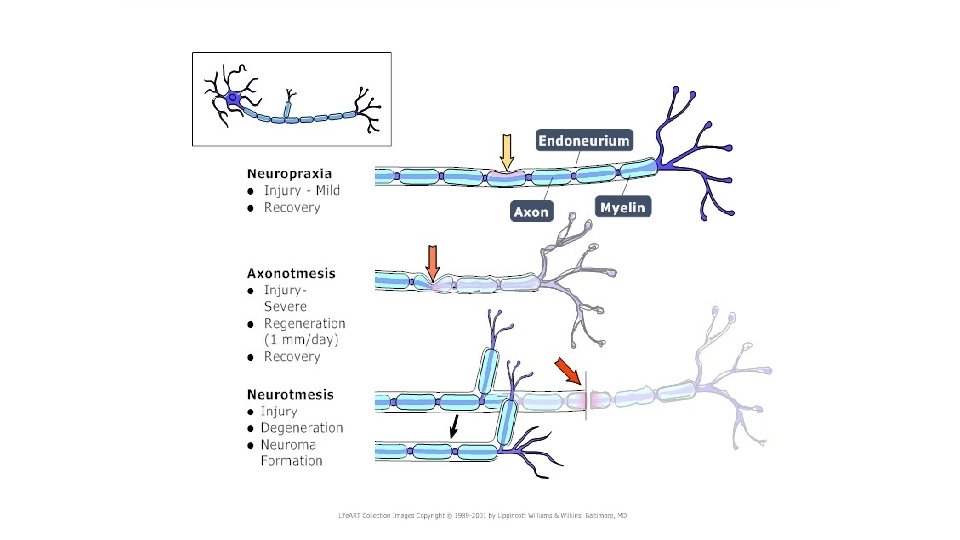
Neuropraxia The mildest grade is called neuropraxia, a reduction or complete block of conduction across a segment of a nerve with axonal continuity conserved.
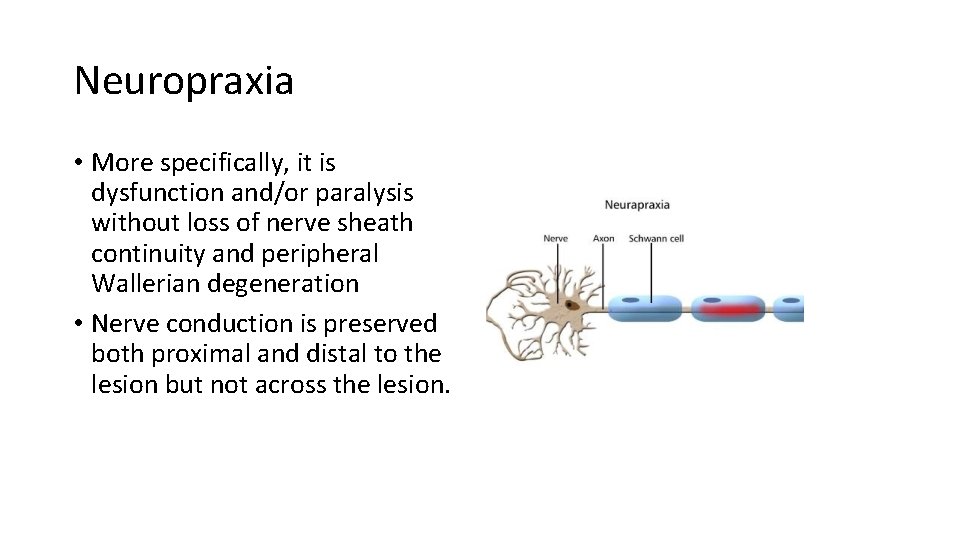
Neuropraxia • More specifically, it is dysfunction and/or paralysis without loss of nerve sheath continuity and peripheral Wallerian degeneration • Nerve conduction is preserved both proximal and distal to the lesion but not across the lesion.
Neuropraxia A person's foot "falling asleep" after her legs have been crossed is an example of a functional loss without abnormal change.
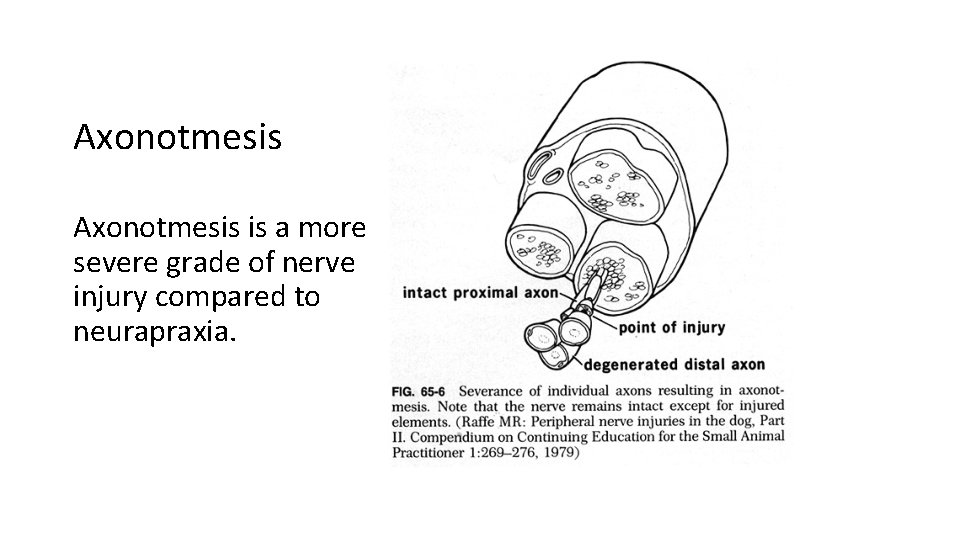
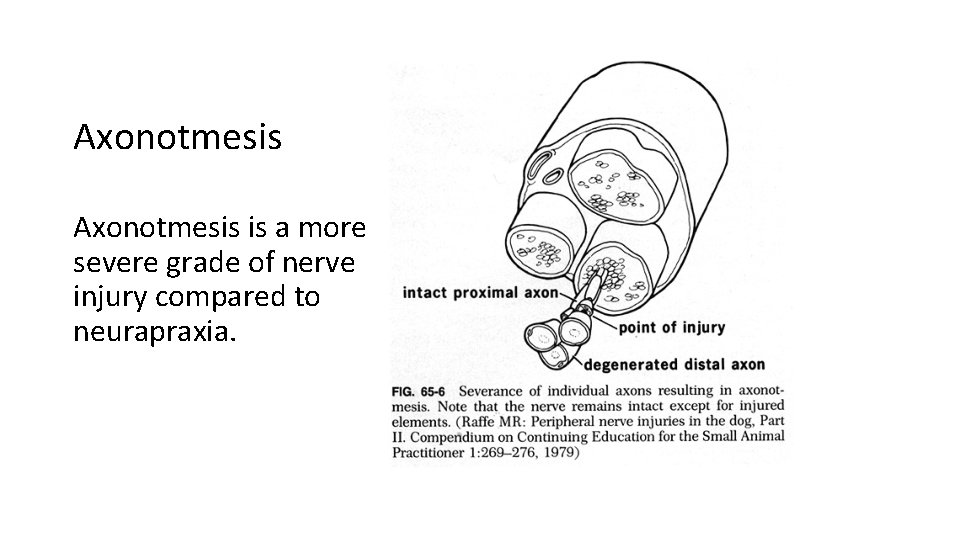
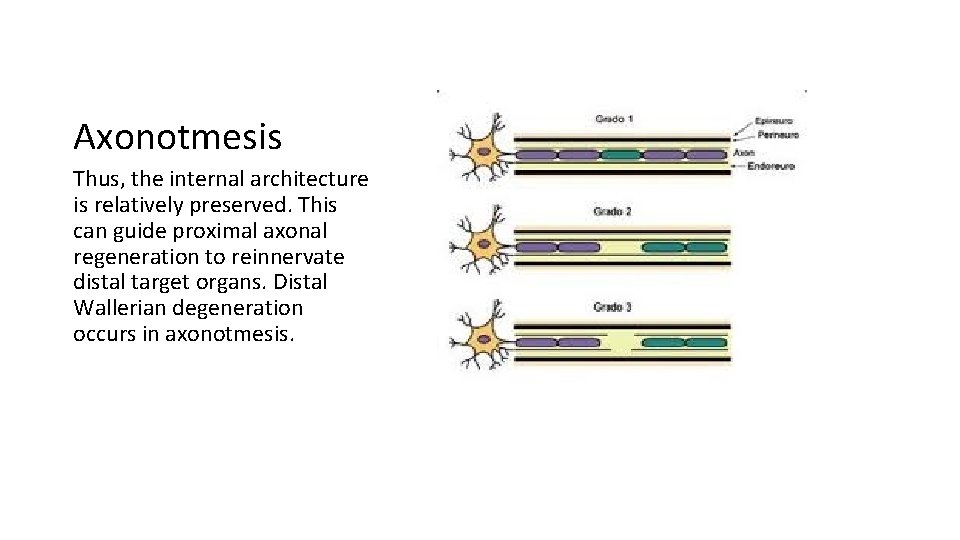
Axonotmesis is a more severe grade of nerve injury compared to neurapraxia.
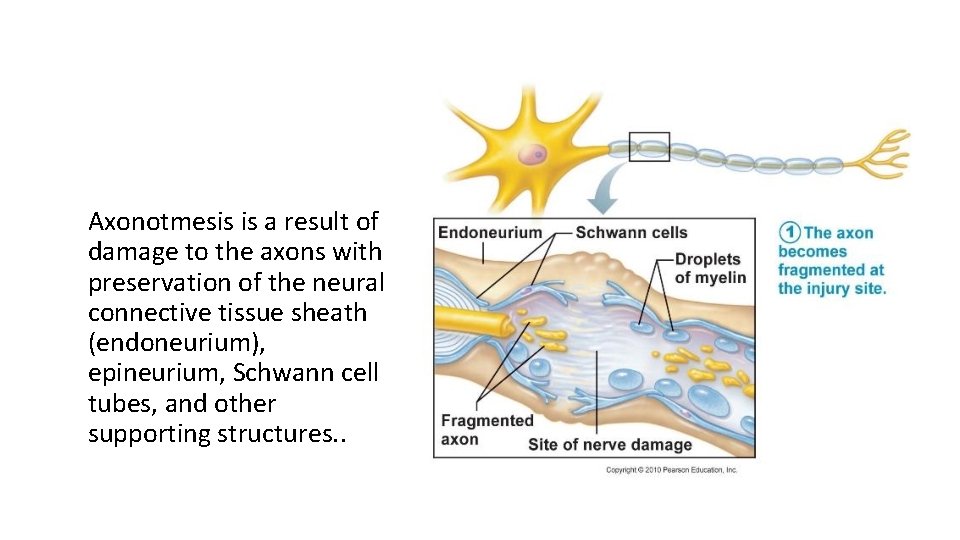
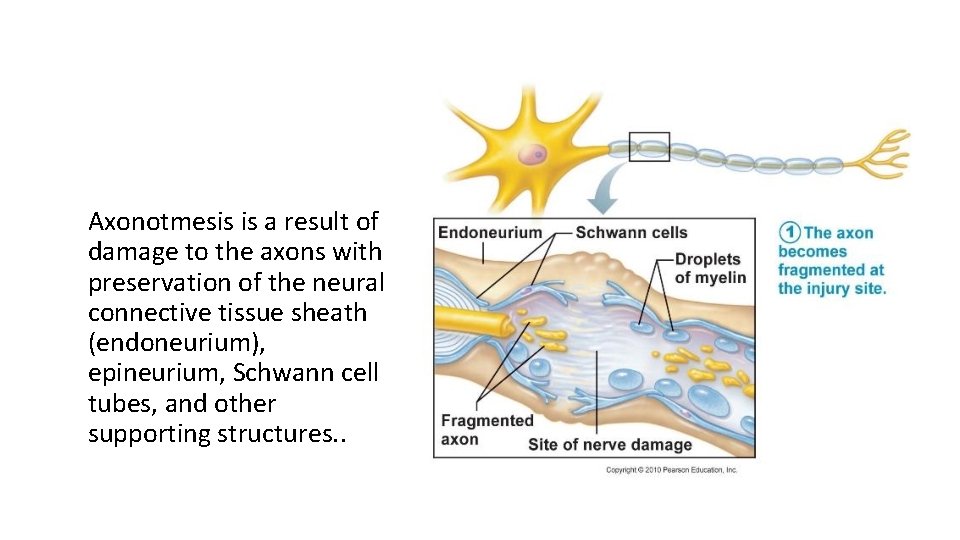
Axonotmesis is a result of damage to the axons with preservation of the neural connective tissue sheath (endoneurium), epineurium, Schwann cell tubes, and other supporting structures. .
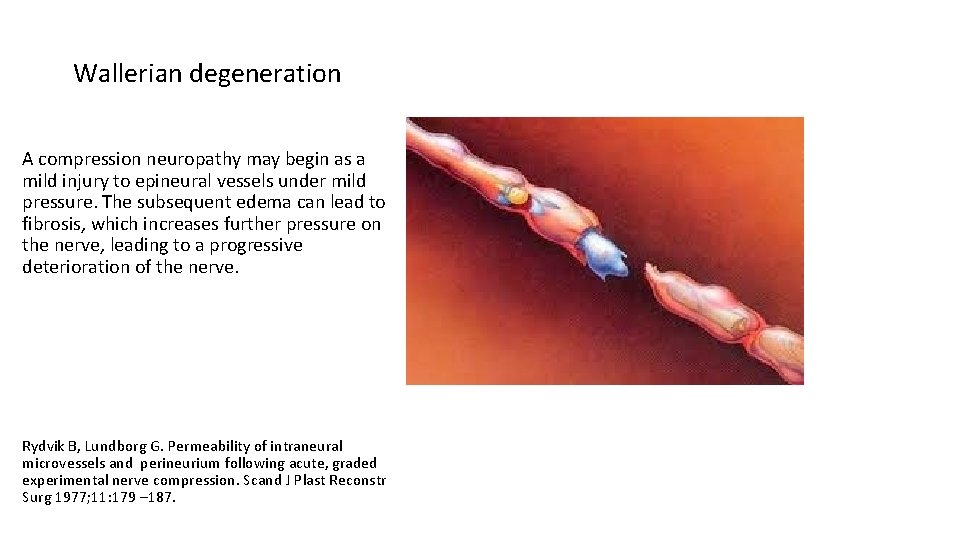
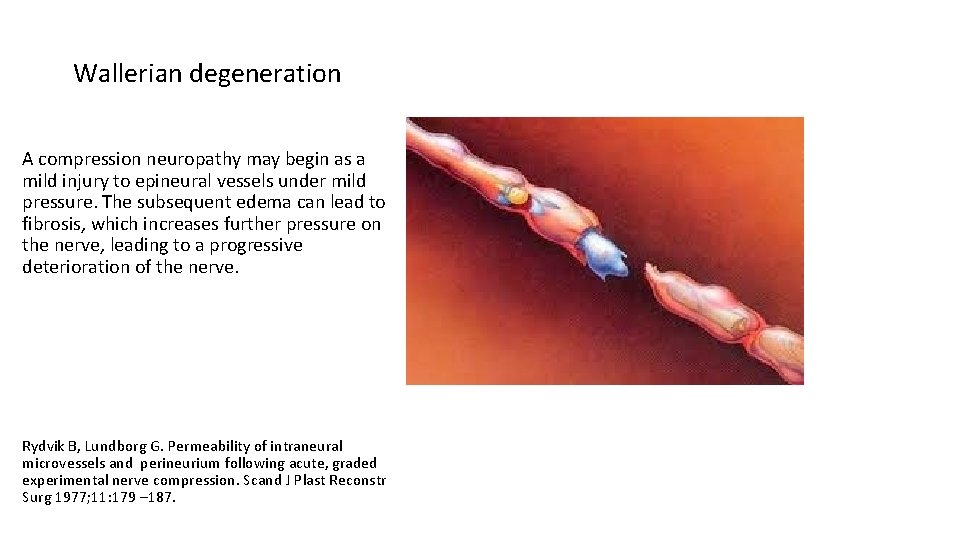
Wallerian degeneration A compression neuropathy may begin as a mild injury to epineural vessels under mild pressure. The subsequent edema can lead to fibrosis, which increases further pressure on the nerve, leading to a progressive deterioration of the nerve. Rydvik B, Lundborg G. Permeability of intraneural microvessels and perineurium following acute, graded experimental nerve compression. Scand J Plast Reconstr Surg 1977; 11: 179 – 187.
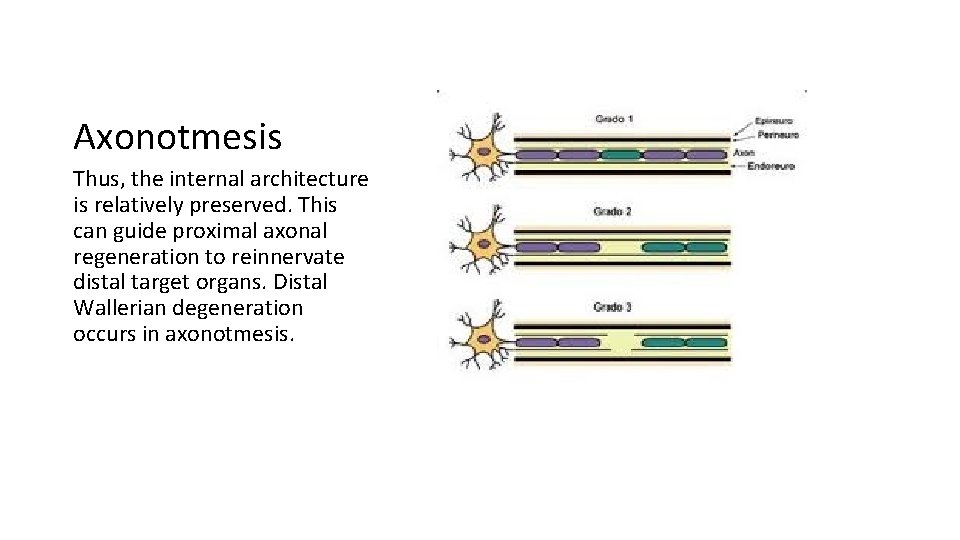
Axonotmesis Thus, the internal architecture is relatively preserved. This can guide proximal axonal regeneration to reinnervate distal target organs. Distal Wallerian degeneration occurs in axonotmesis.
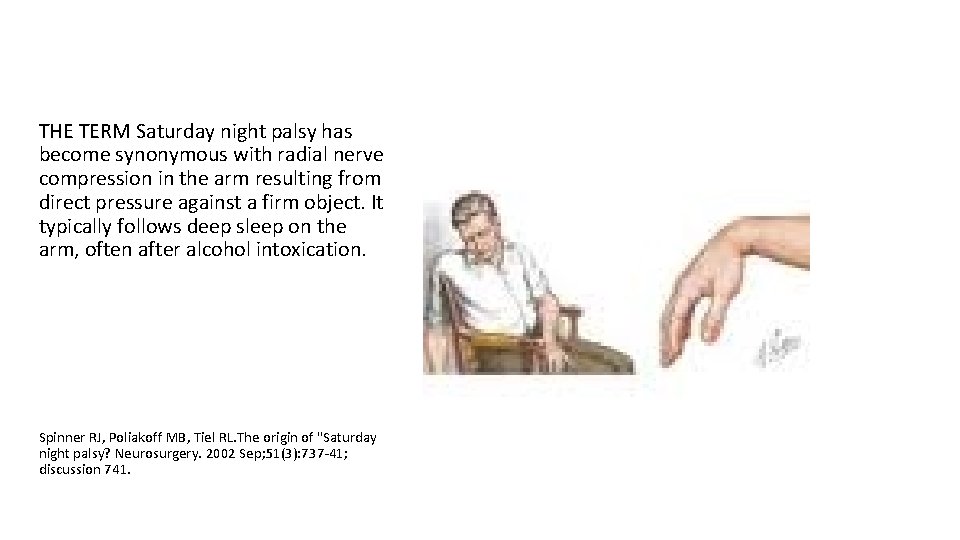
THE TERM Saturday night palsy has become synonymous with radial nerve compression in the arm resulting from direct pressure against a firm object. It typically follows deep sleep on the arm, often after alcohol intoxication. Spinner RJ, Poliakoff MB, Tiel RL. The origin of "Saturday night palsy? Neurosurgery. 2002 Sep; 51(3): 737‐ 41; discussion 741.
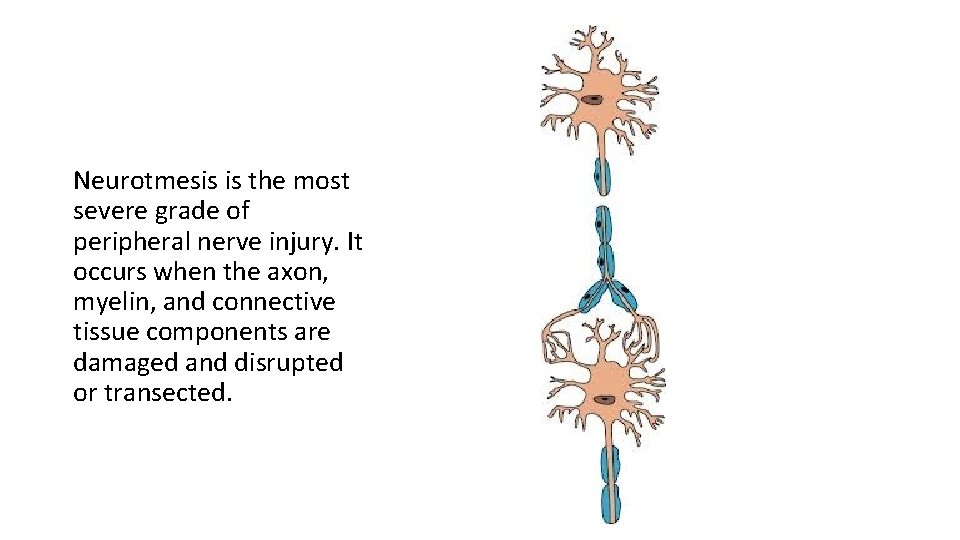
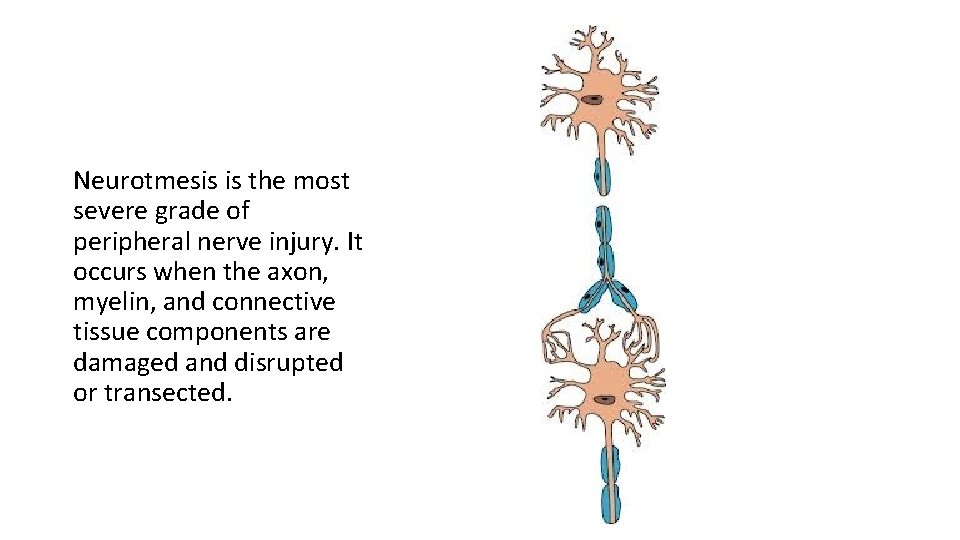
Neurotmesis is the most severe grade of peripheral nerve injury. It occurs when the axon, myelin, and connective tissue components are damaged and disrupted or transected.

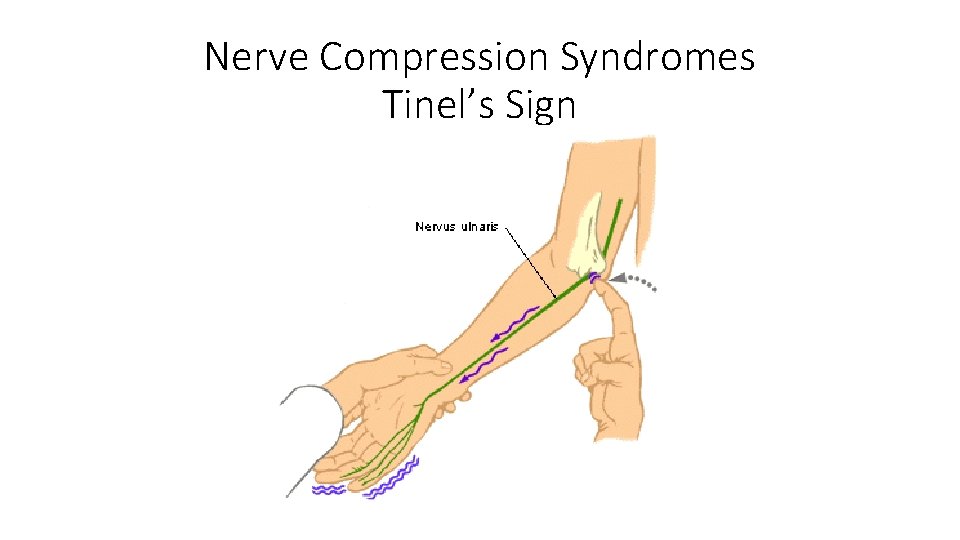
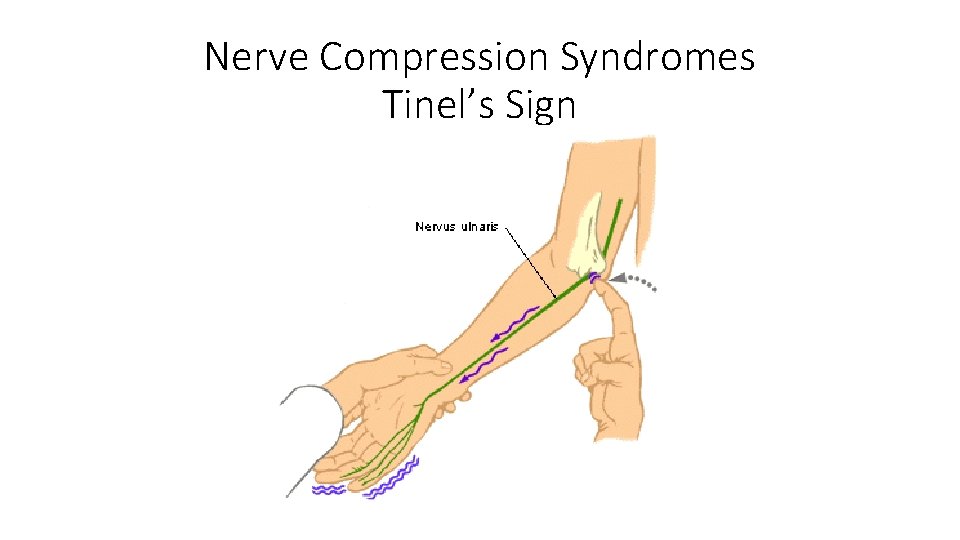
Nerve Compression Syndromes Tinel’s Sign
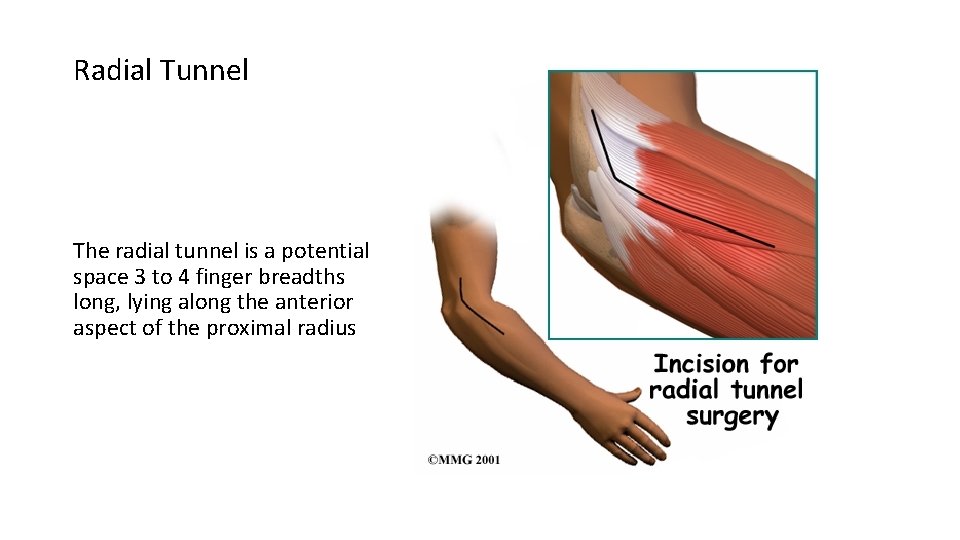
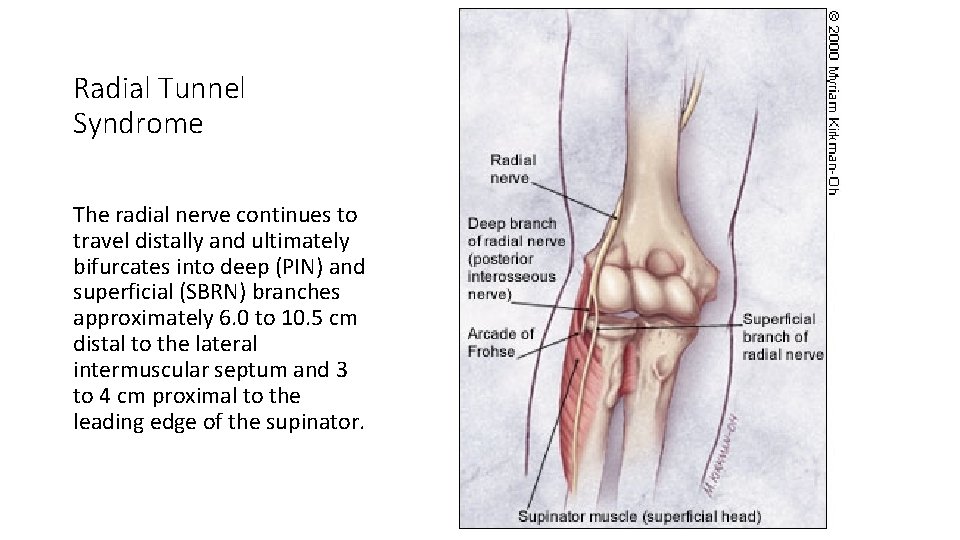
Radial Tunnel The radial tunnel is a potential space 3 to 4 finger breadths long, lying along the anterior aspect of the proximal radius
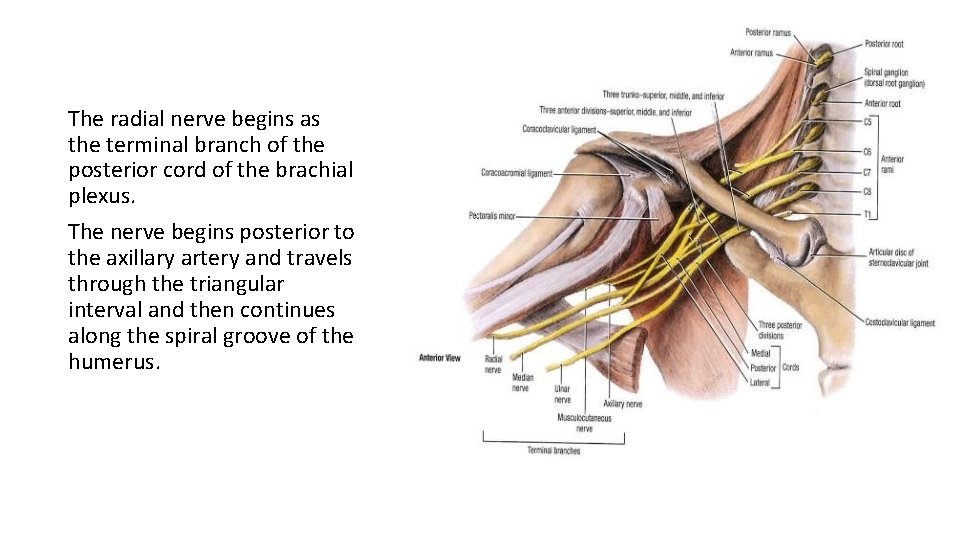
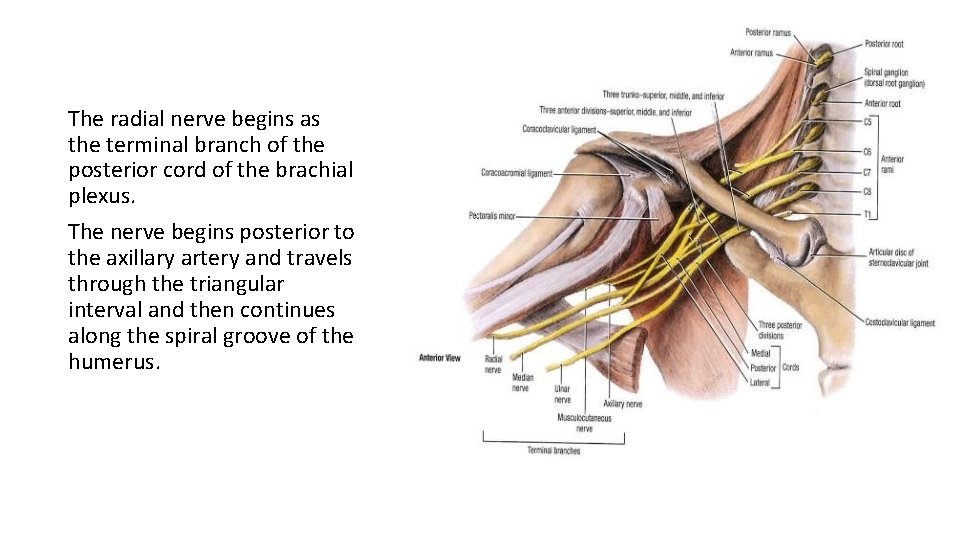
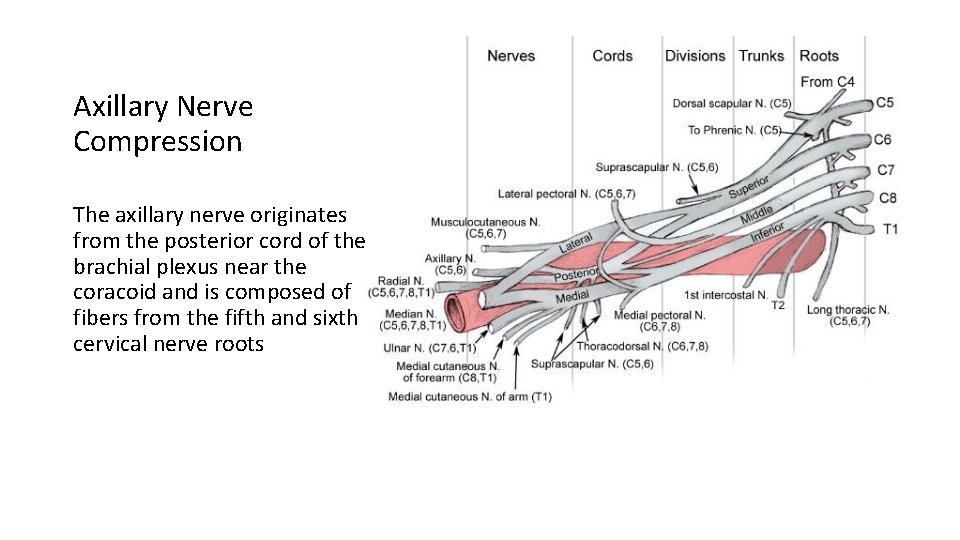
The radial nerve begins as the terminal branch of the posterior cord of the brachial plexus. The nerve begins posterior to the axillary artery and travels through the triangular interval and then continues along the spiral groove of the humerus.
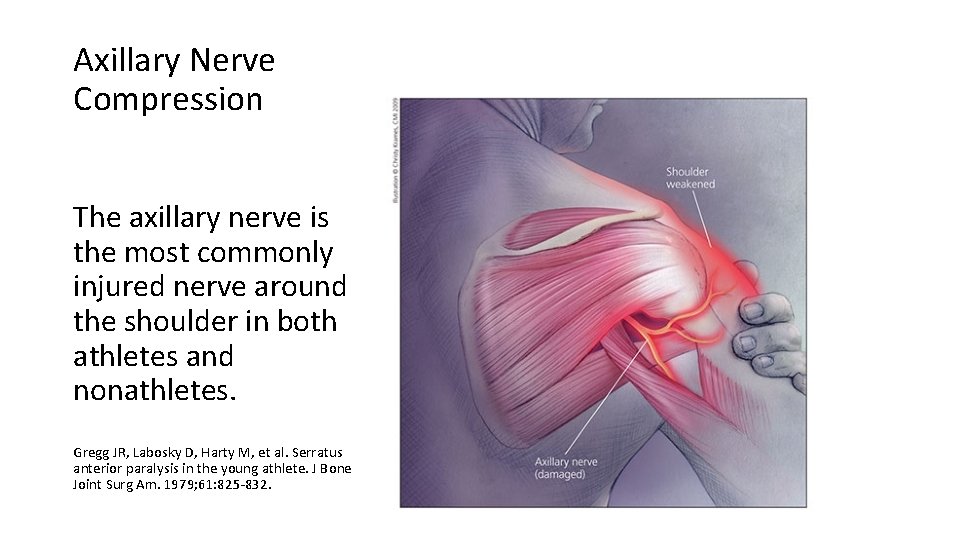
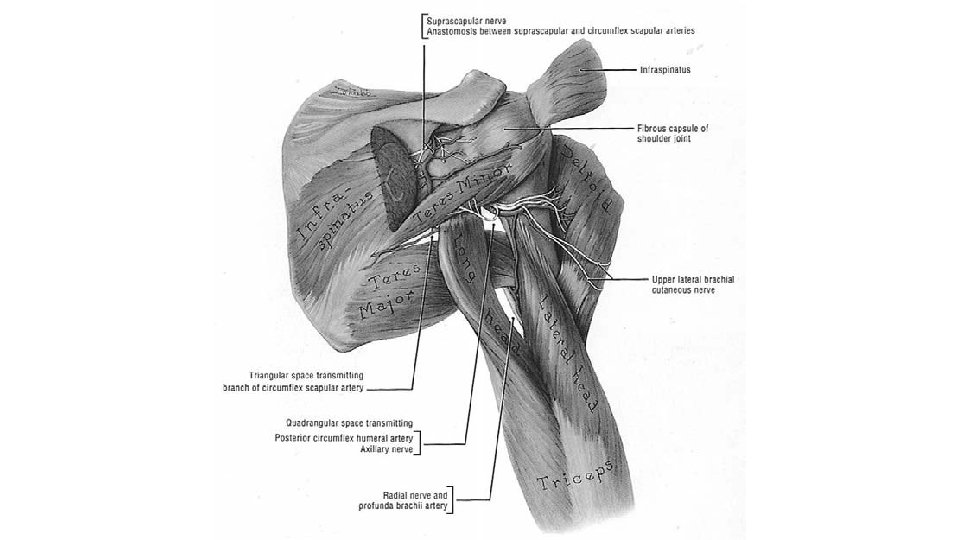
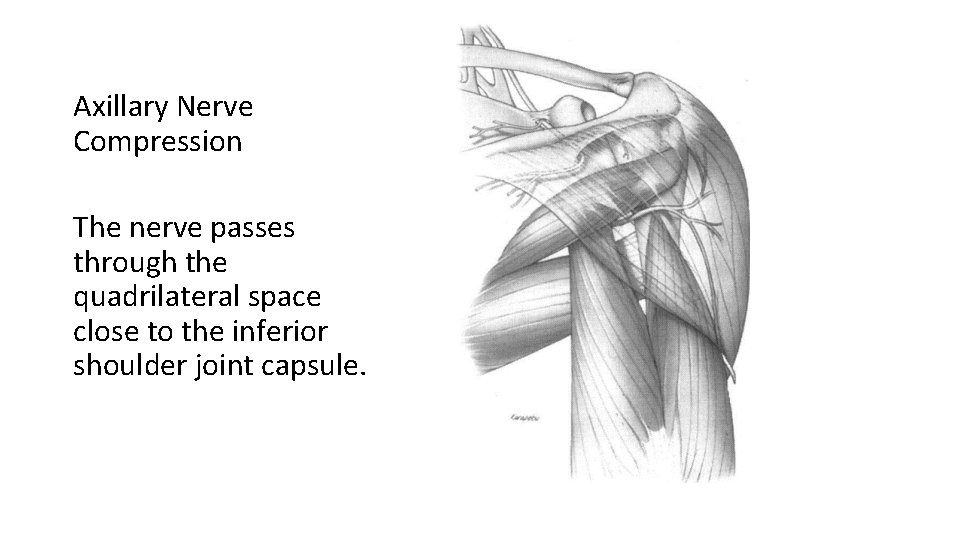
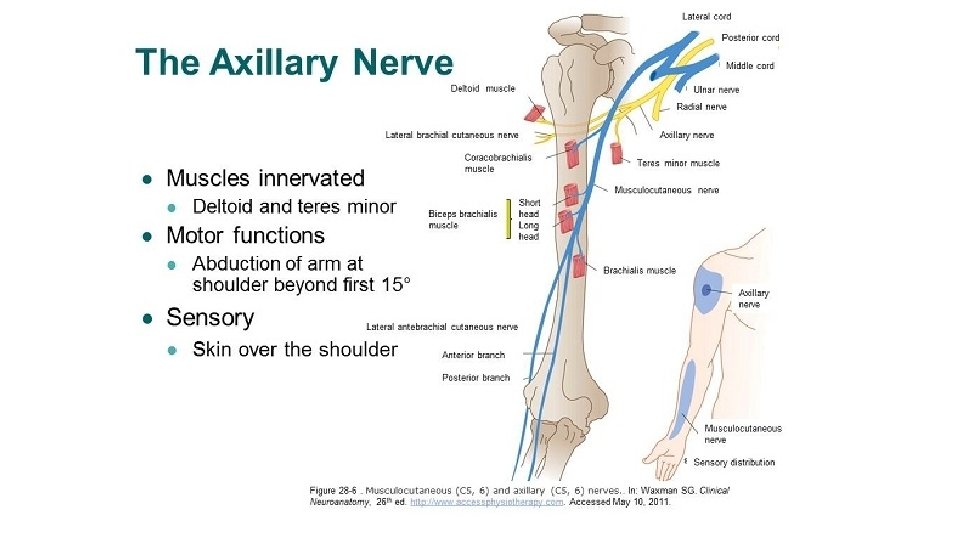
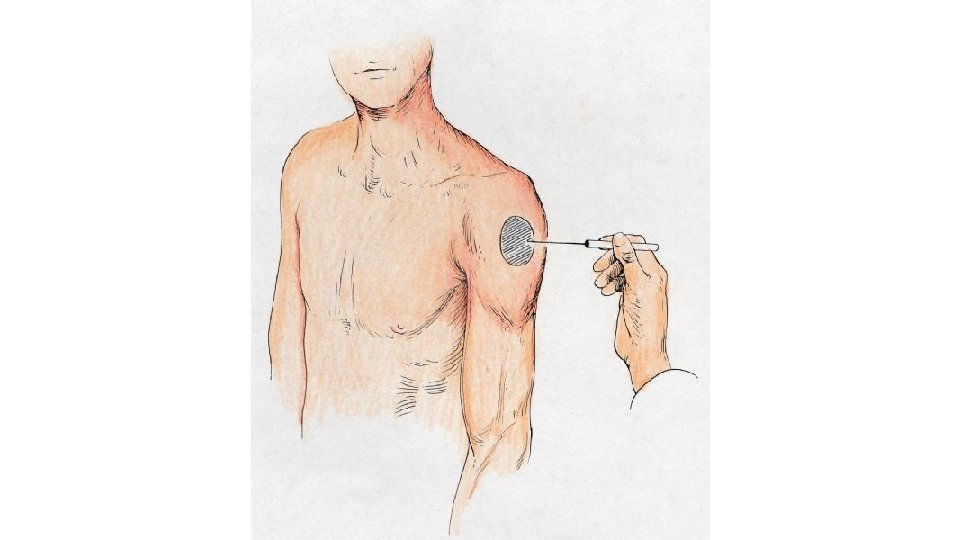
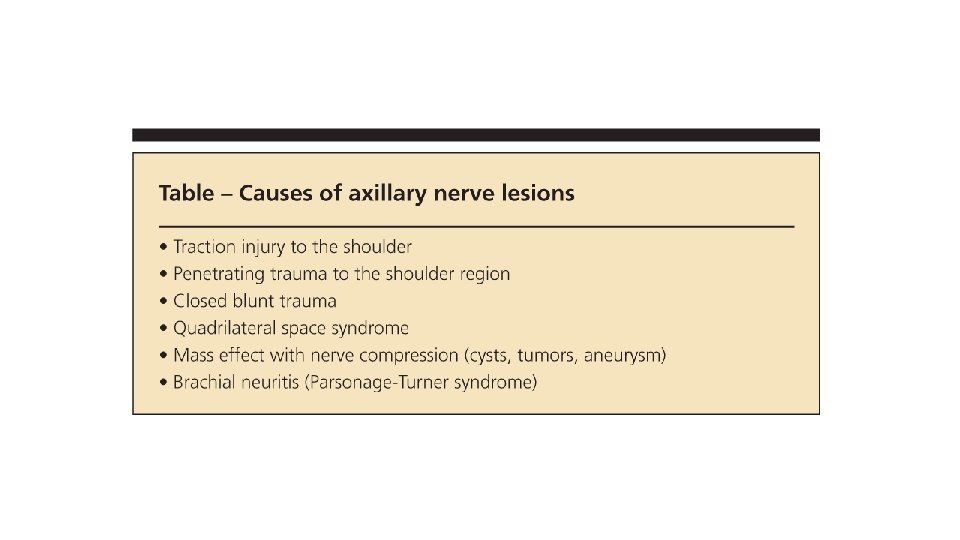
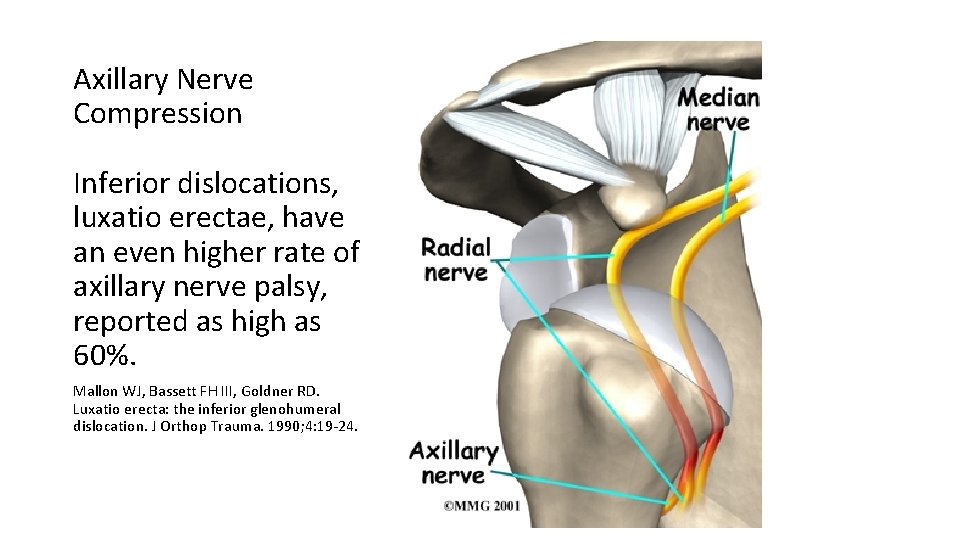
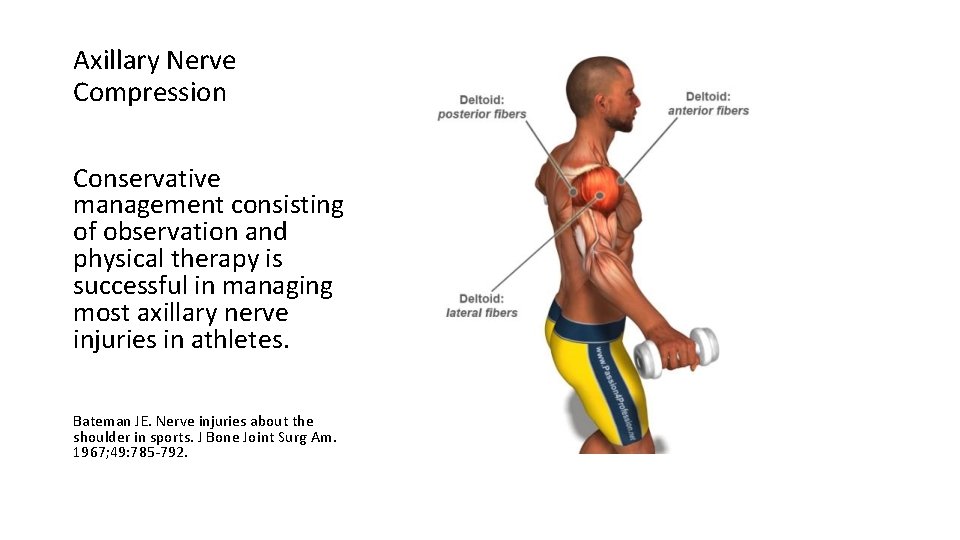
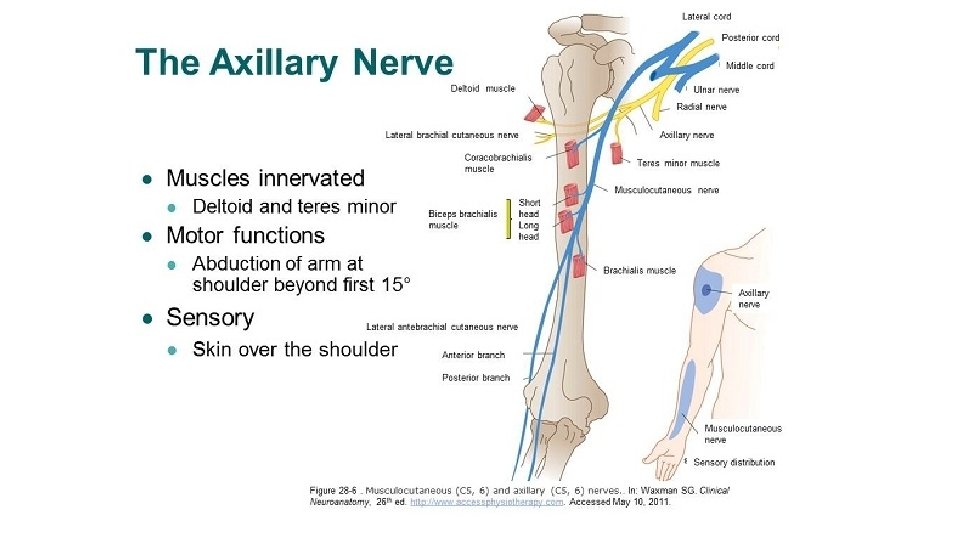
Axillary Nerve Compression The axillary nerve is the most commonly injured nerve around the shoulder in both athletes and nonathletes. Gregg JR, Labosky D, Harty M, et al. Serratus anterior paralysis in the young athlete. J Bone Joint Surg Am. 1979; 61: 825‐ 832.
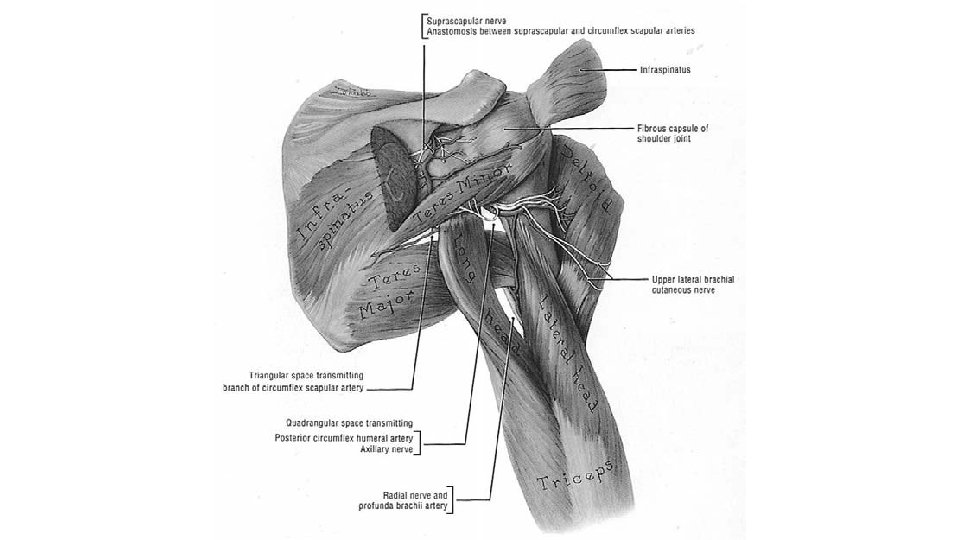
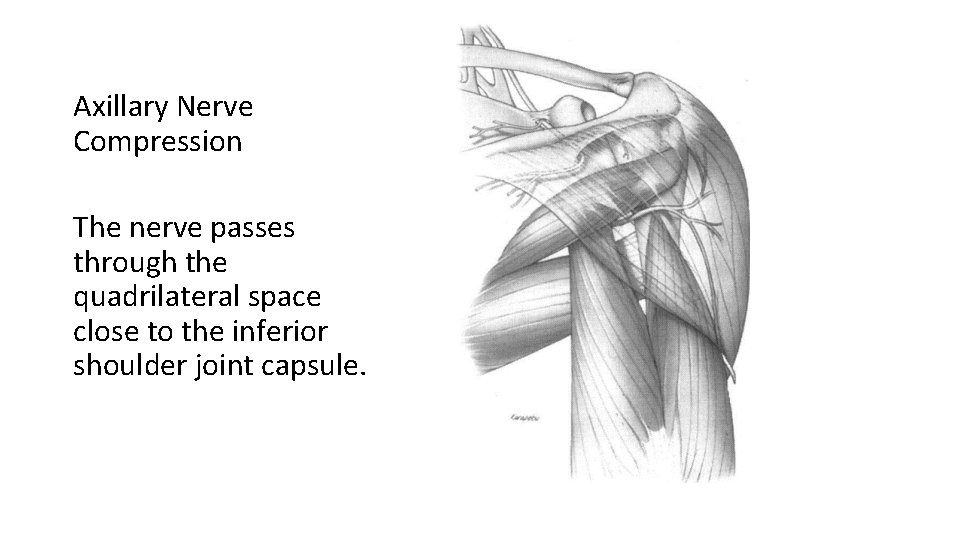
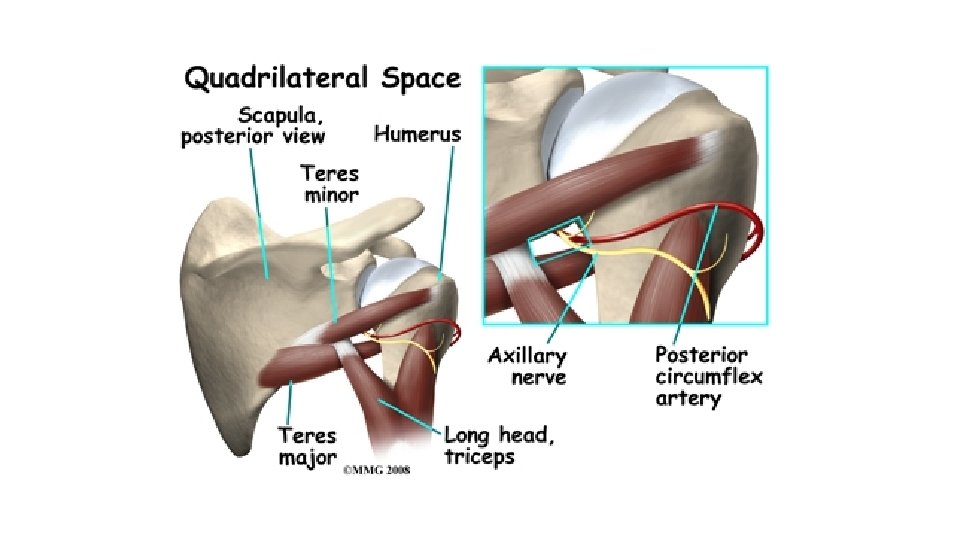
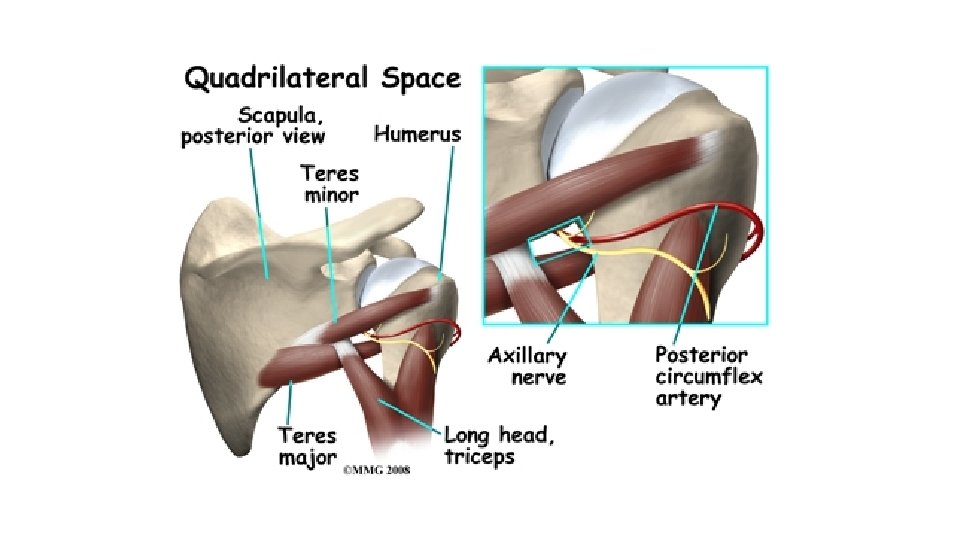
Axillary Nerve Compression The nerve passes through the quadrilateral space close to the inferior shoulder joint capsule.
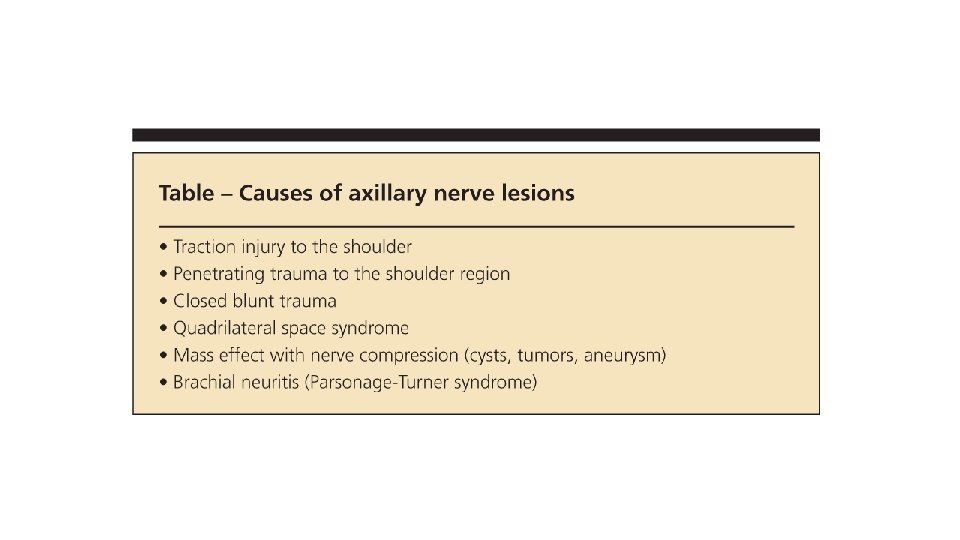
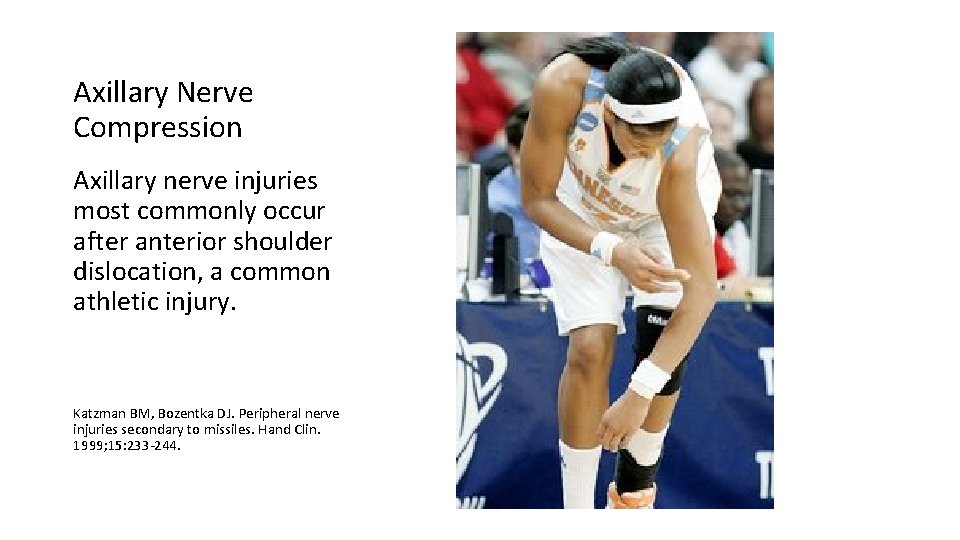
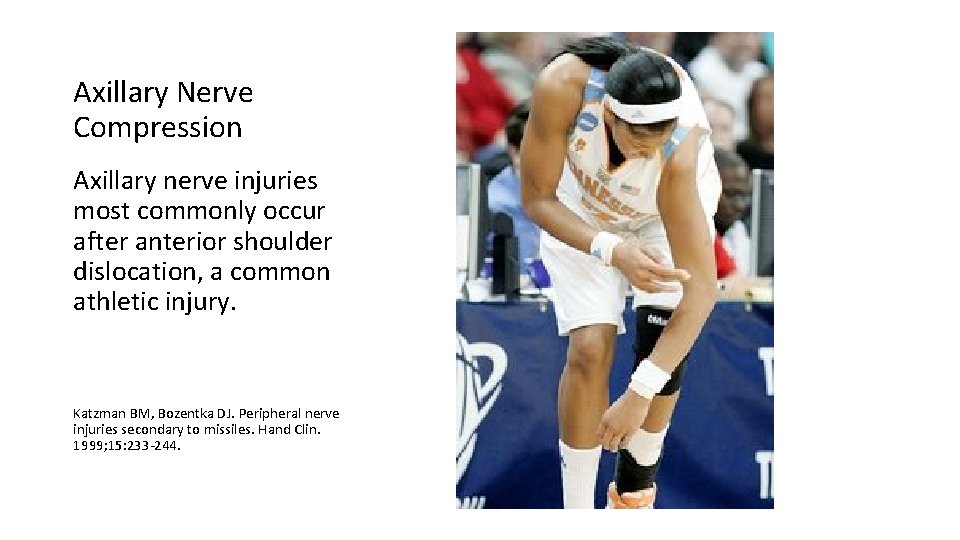
Axillary Nerve Compression Axillary nerve injuries most commonly occur after anterior shoulder dislocation, a common athletic injury. Katzman BM, Bozentka DJ. Peripheral nerve injuries secondary to missiles. Hand Clin. 1999; 15: 233‐ 244.
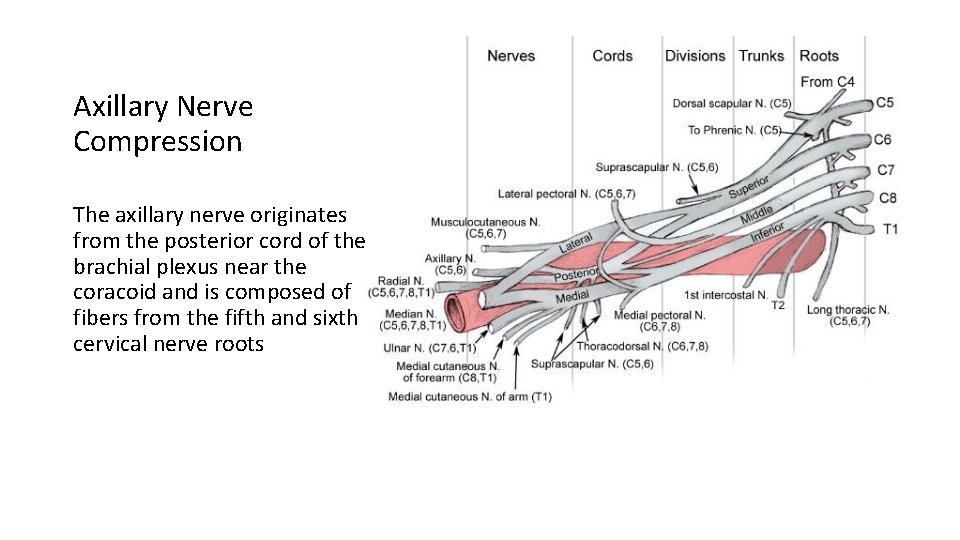
Axillary Nerve Compression The axillary nerve originates from the posterior cord of the brachial plexus near the coracoid and is composed of fibers from the fifth and sixth cervical nerve roots
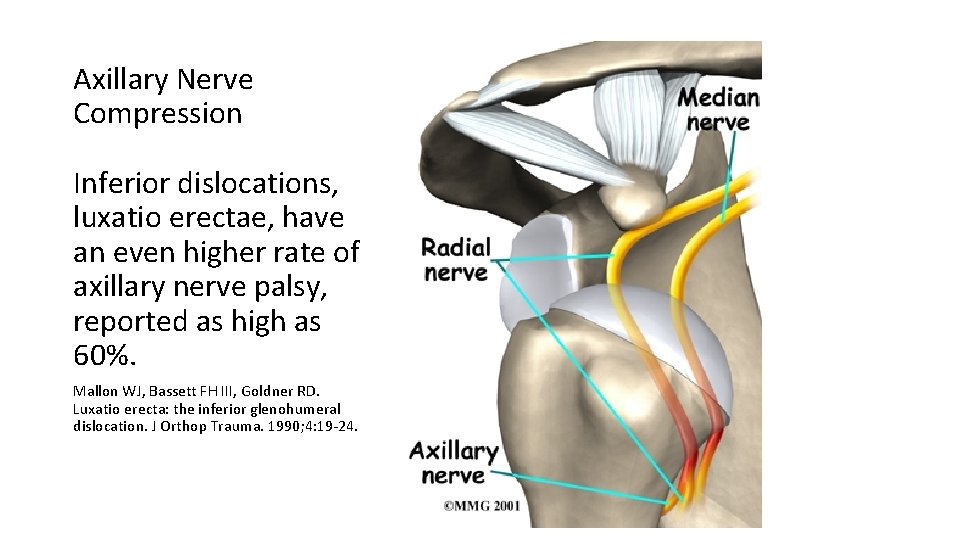
Axillary Nerve Compression Inferior dislocations, luxatio erectae, have an even higher rate of axillary nerve palsy, reported as high as 60%. Mallon WJ, Bassett FH III, Goldner RD. Luxatio erecta: the inferior glenohumeral dislocation. J Orthop Trauma. 1990; 4: 19‐ 24.
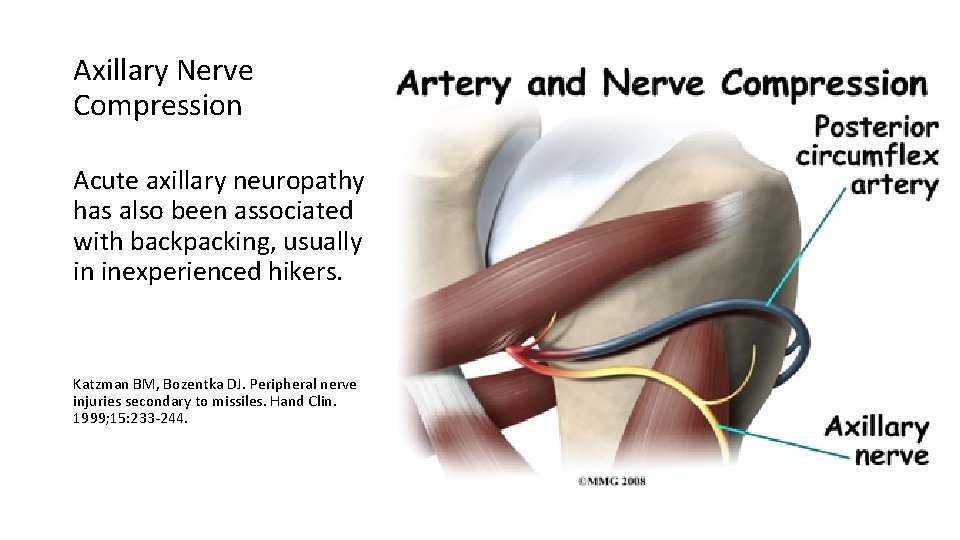
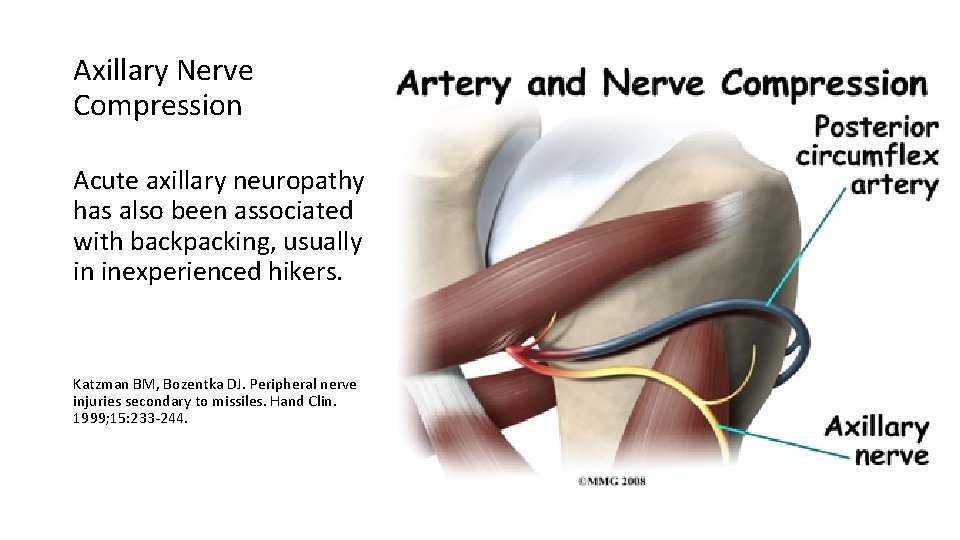
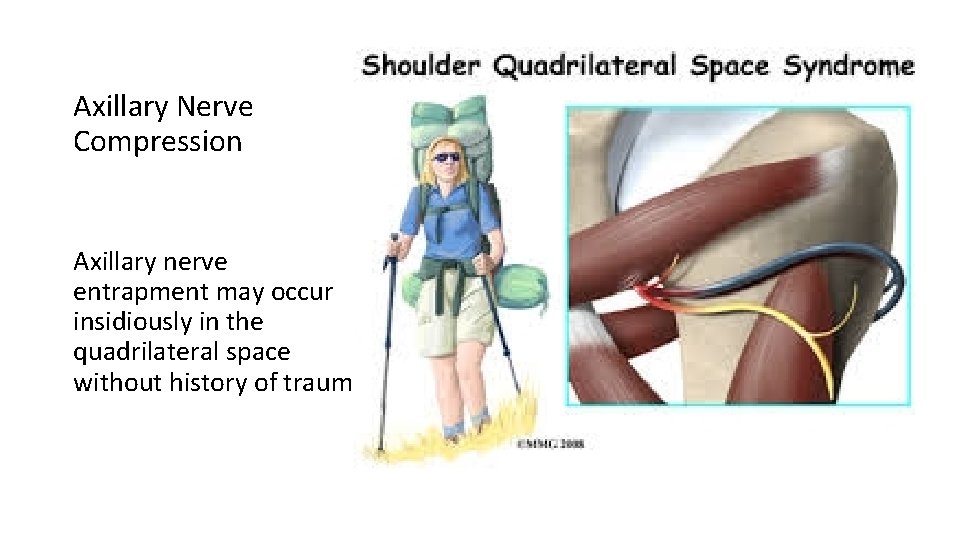
Axillary Nerve Compression Acute axillary neuropathy has also been associated with backpacking, usually in inexperienced hikers. Katzman BM, Bozentka DJ. Peripheral nerve injuries secondary to missiles. Hand Clin. 1999; 15: 233‐ 244.
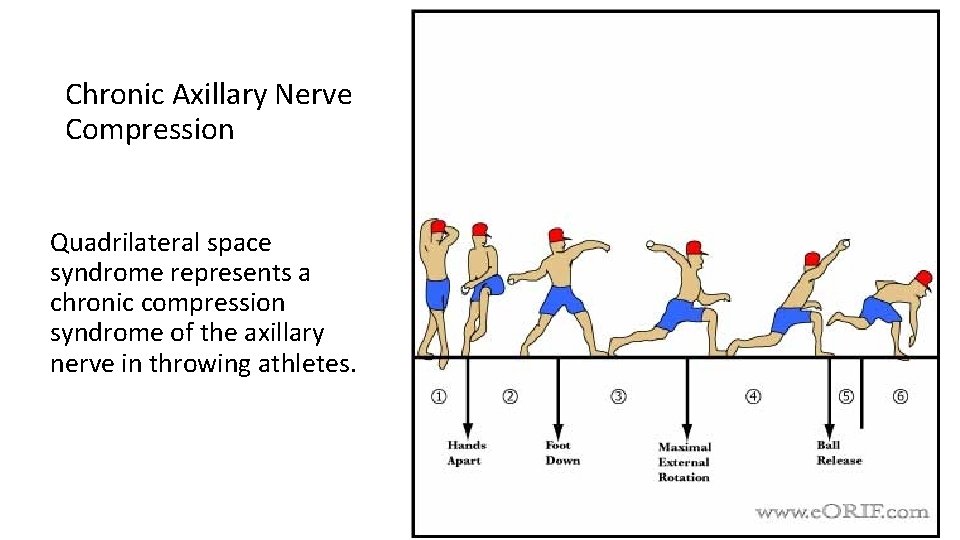
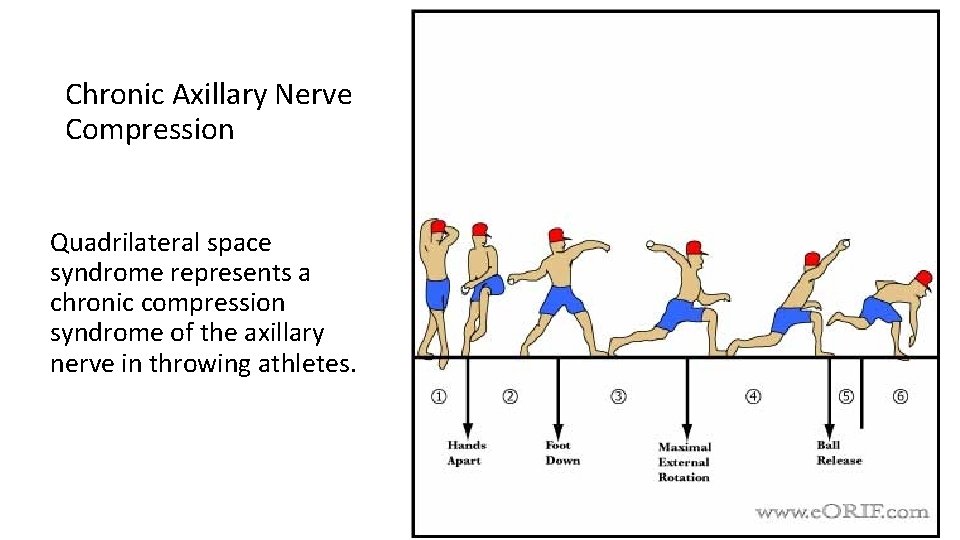
Chronic Axillary Nerve Compression Quadrilateral space syndrome represents a chronic compression syndrome of the axillary nerve in throwing athletes.
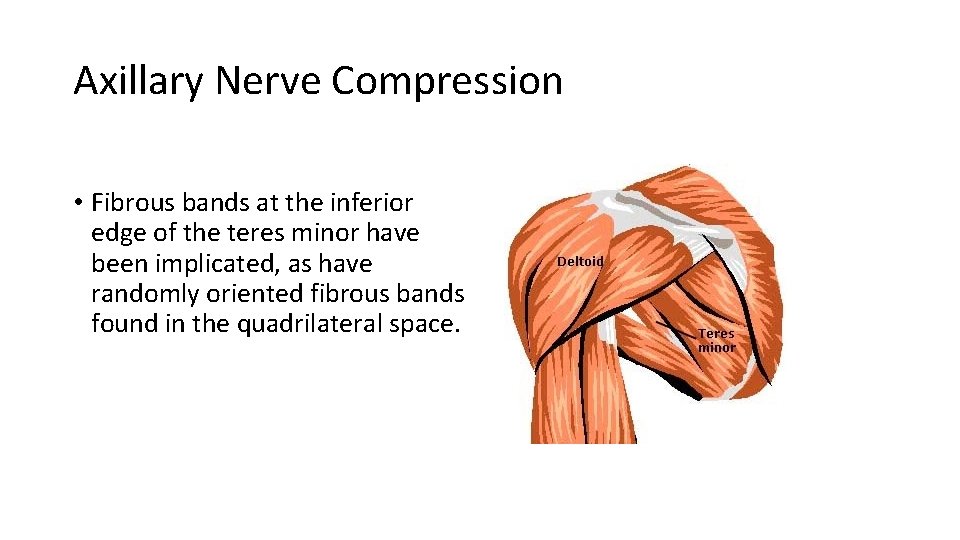
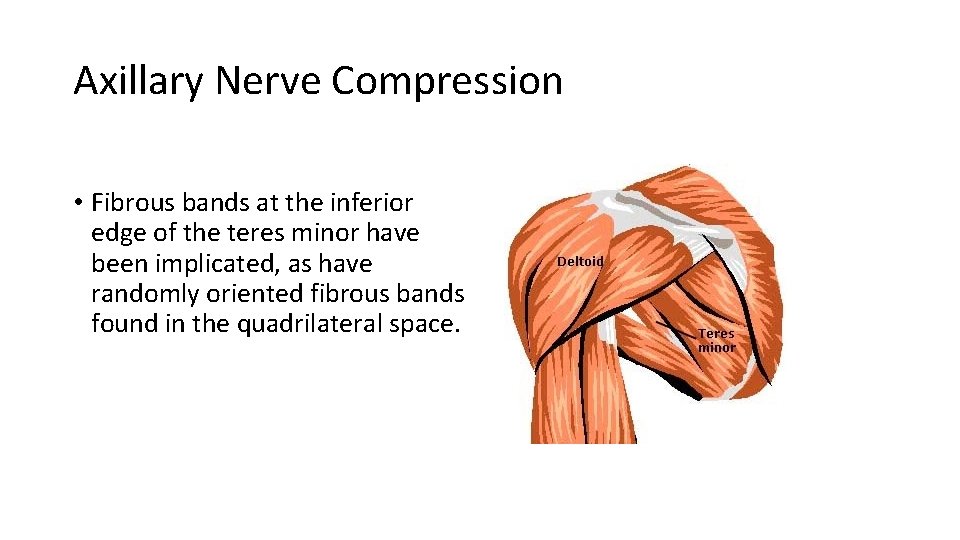
Axillary Nerve Compression • Fibrous bands at the inferior edge of the teres minor have been implicated, as have randomly oriented fibrous bands found in the quadrilateral space.
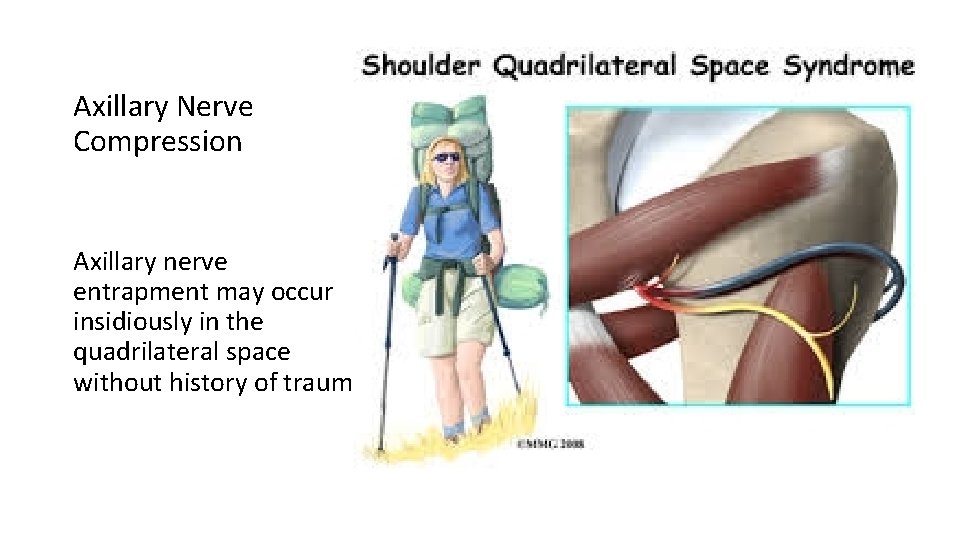
Axillary Nerve Compression Axillary nerve entrapment may occur insidiously in the quadrilateral space without history of trauma.
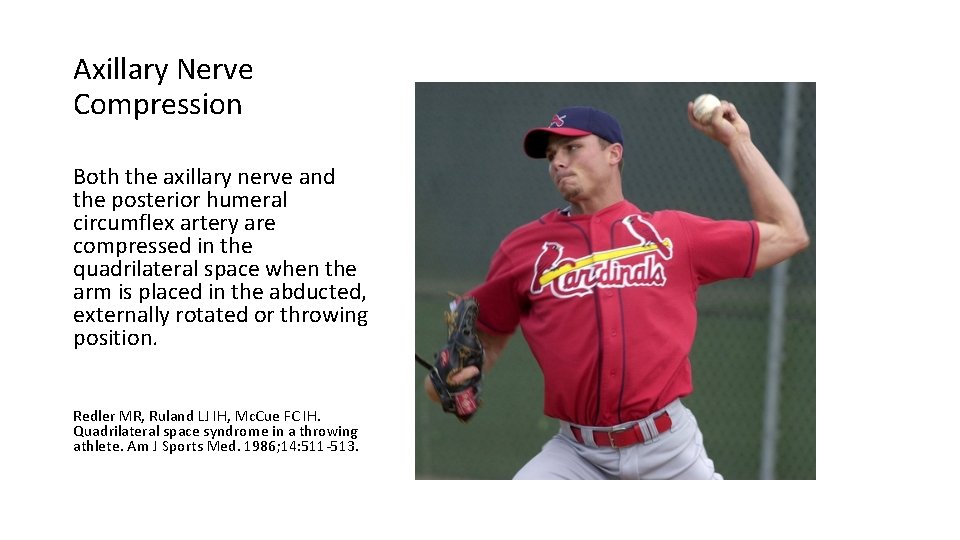
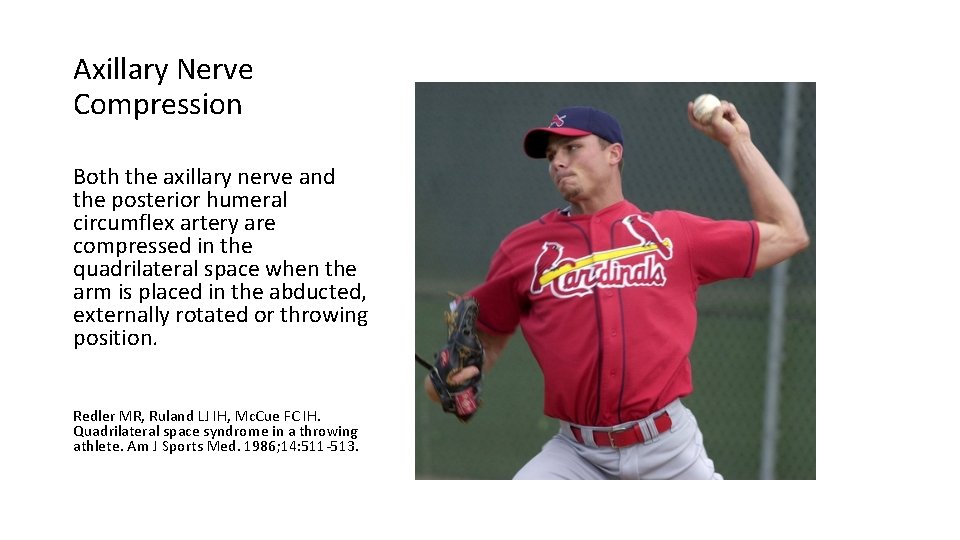
Axillary Nerve Compression Both the axillary nerve and the posterior humeral circumflex artery are compressed in the quadrilateral space when the arm is placed in the abducted, externally rotated or throwing position. Redler MR, Ruland LJ IH, Mc. Cue FC IH. Quadrilateral space syndrome in a throwing athlete. Am J Sports Med. 1986; 14: 511‐ 513.
Ruth, Musial, Sisler, and Ankiel shared a rare accomplishment
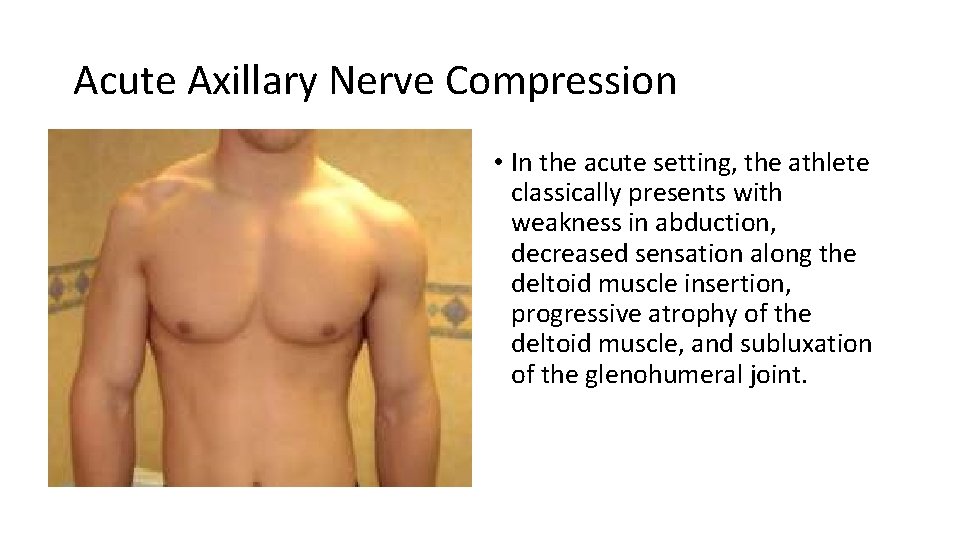
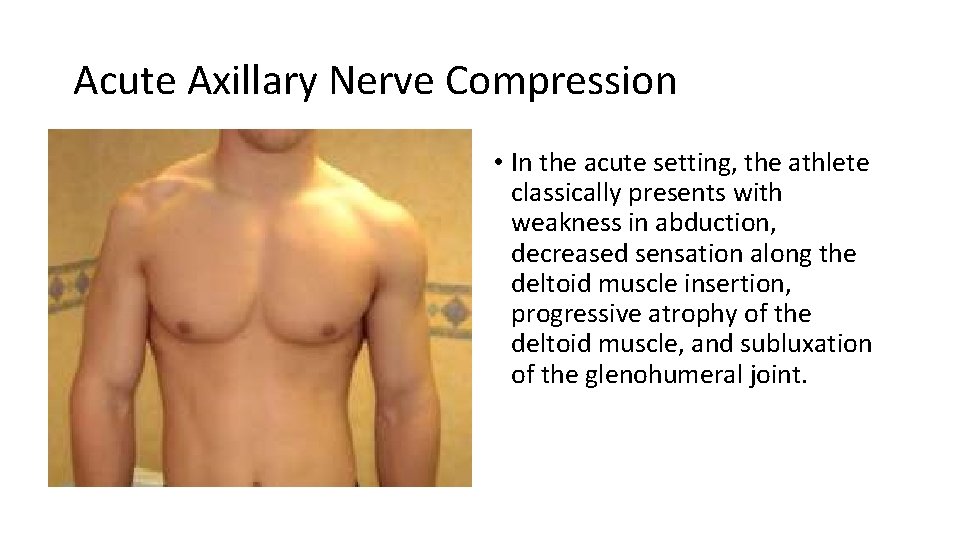
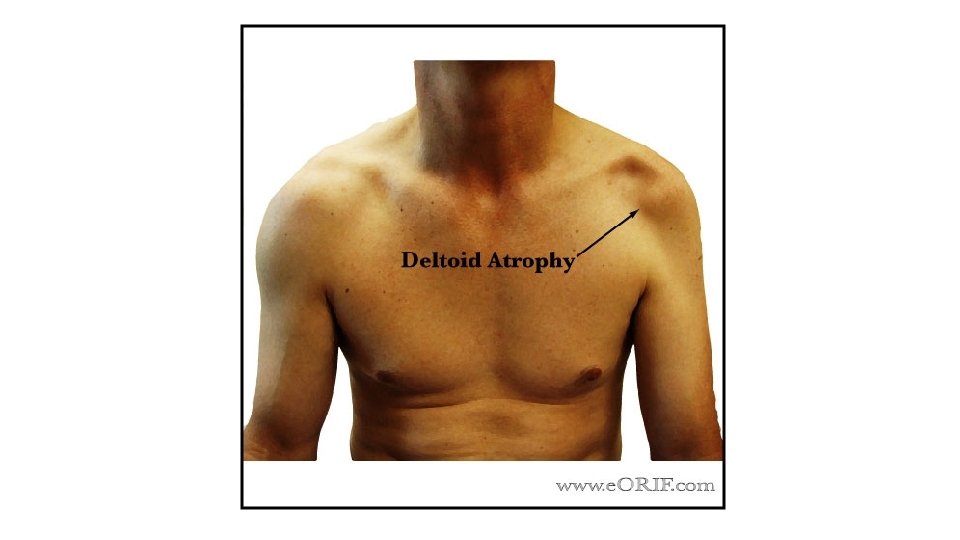
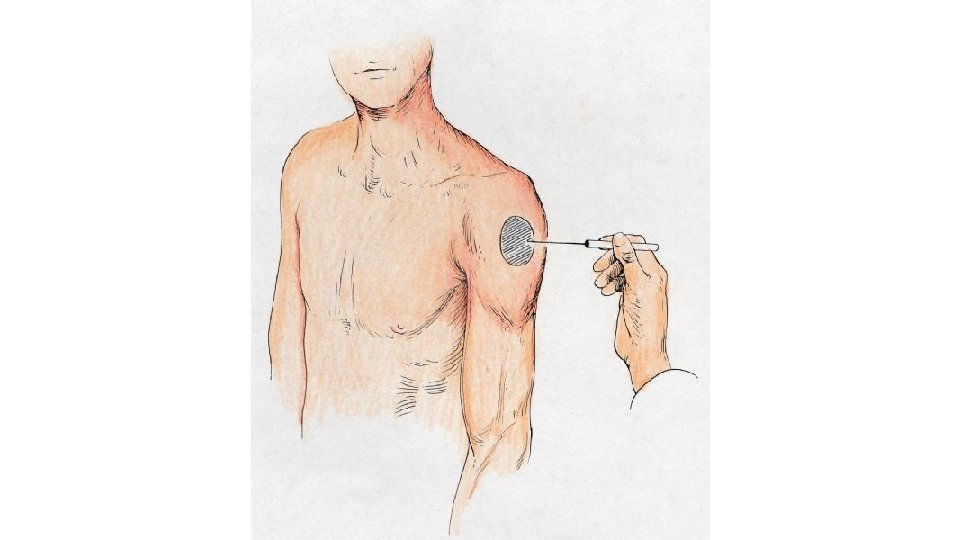
Acute Axillary Nerve Compression • In the acute setting, the athlete classically presents with weakness in abduction, decreased sensation along the deltoid muscle insertion, progressive atrophy of the deltoid muscle, and subluxation of the glenohumeral joint.
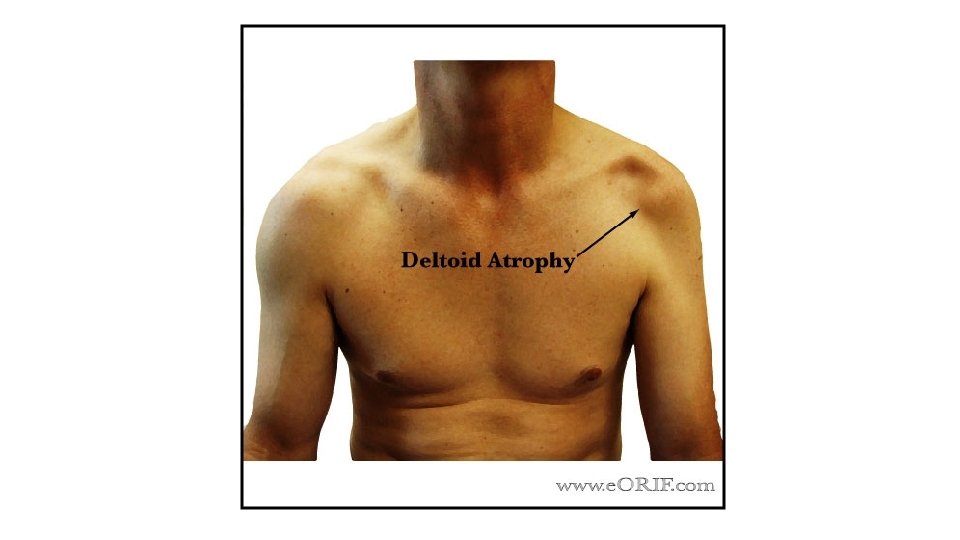
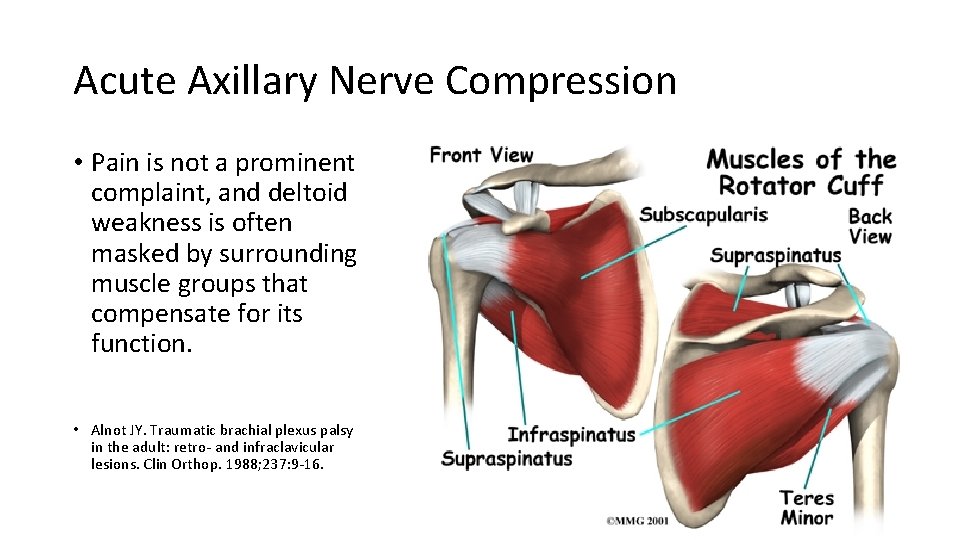
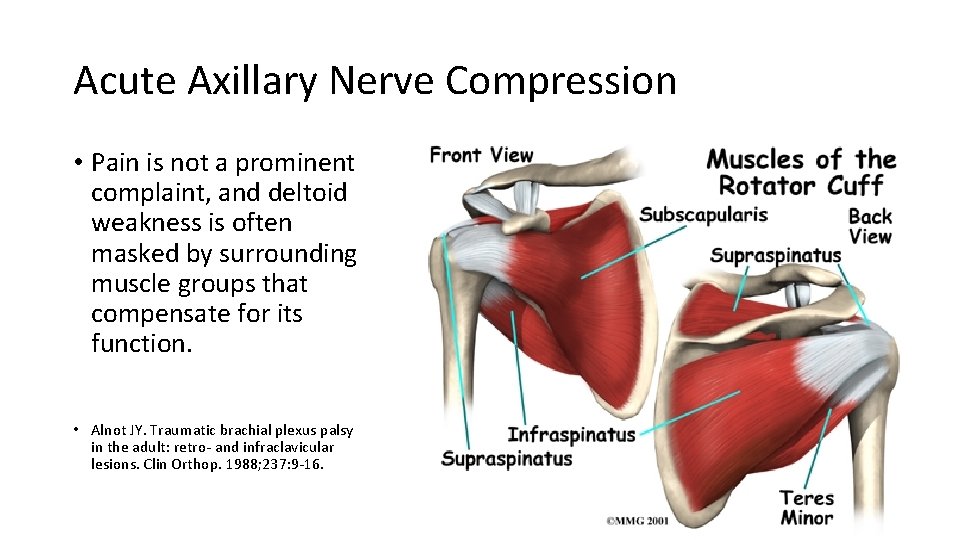
Acute Axillary Nerve Compression • Pain is not a prominent complaint, and deltoid weakness is often masked by surrounding muscle groups that compensate for its function. • Alnot JY. Traumatic brachial plexus palsy in the adult: retro‐ and infraclavicular lesions. Clin Orthop. 1988; 237: 9‐ 16.
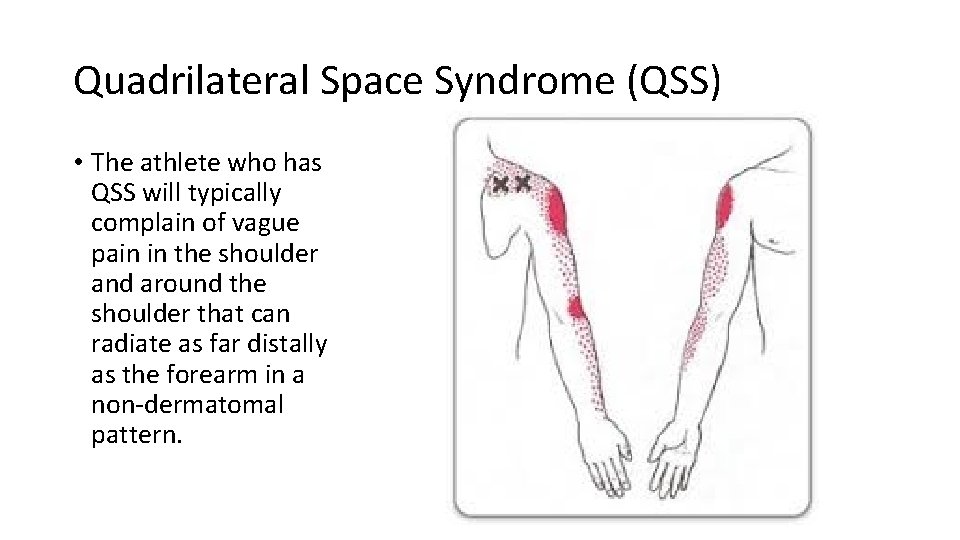
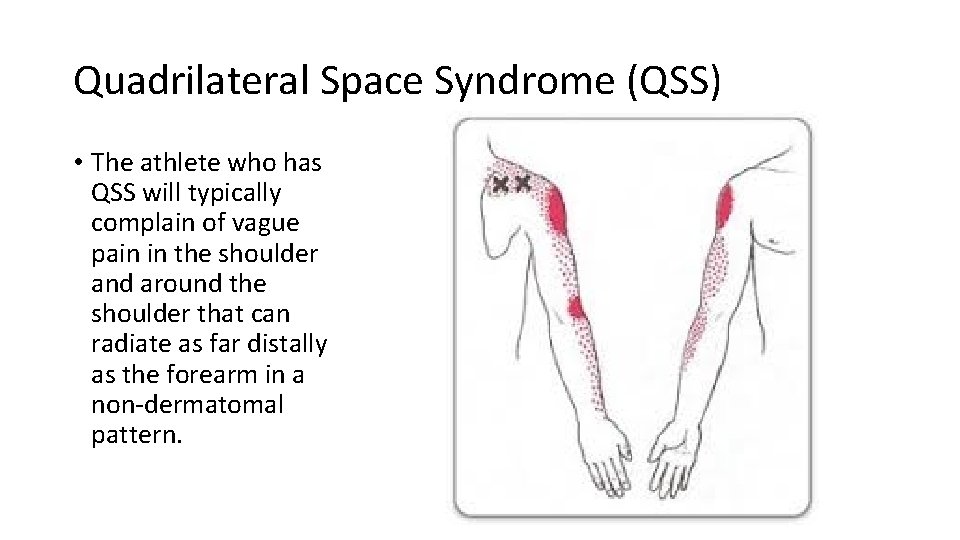
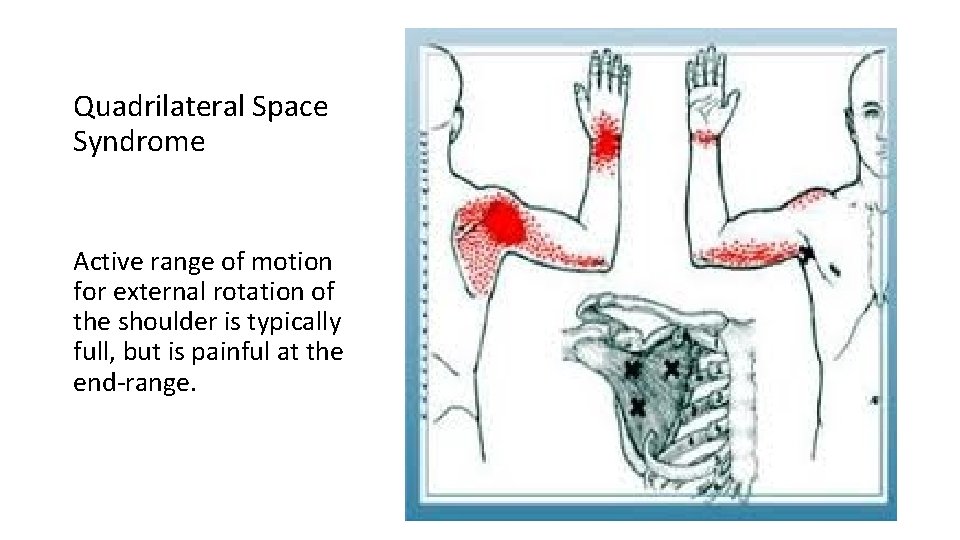
Quadrilateral Space Syndrome (QSS) • The athlete who has QSS will typically complain of vague pain in the shoulder and around the shoulder that can radiate as far distally as the forearm in a non‐dermatomal pattern.
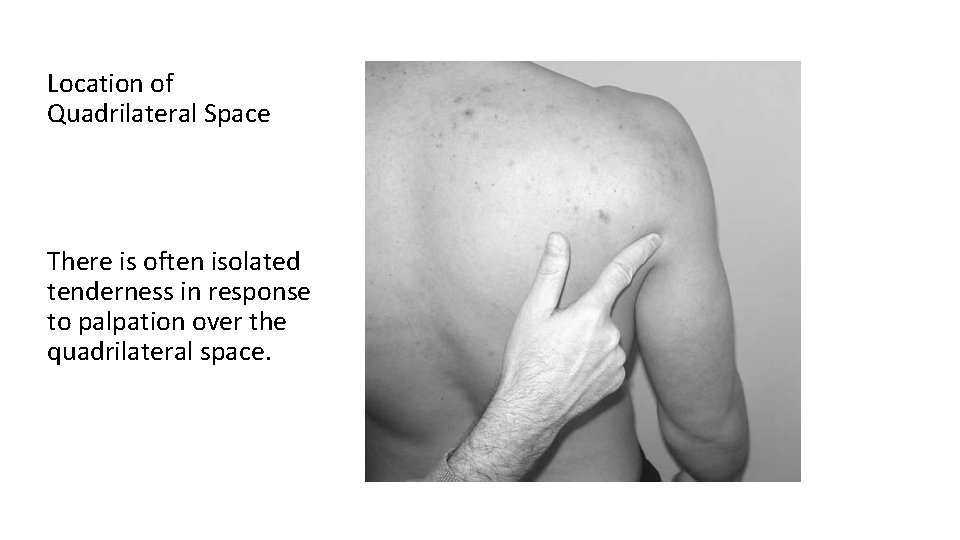
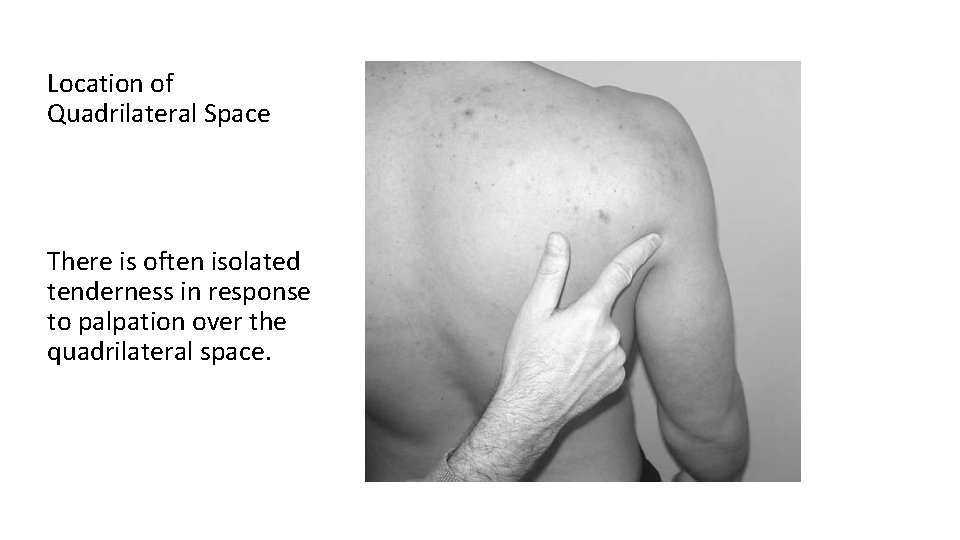
Location of Quadrilateral Space There is often isolated tenderness in response to palpation over the quadrilateral space.
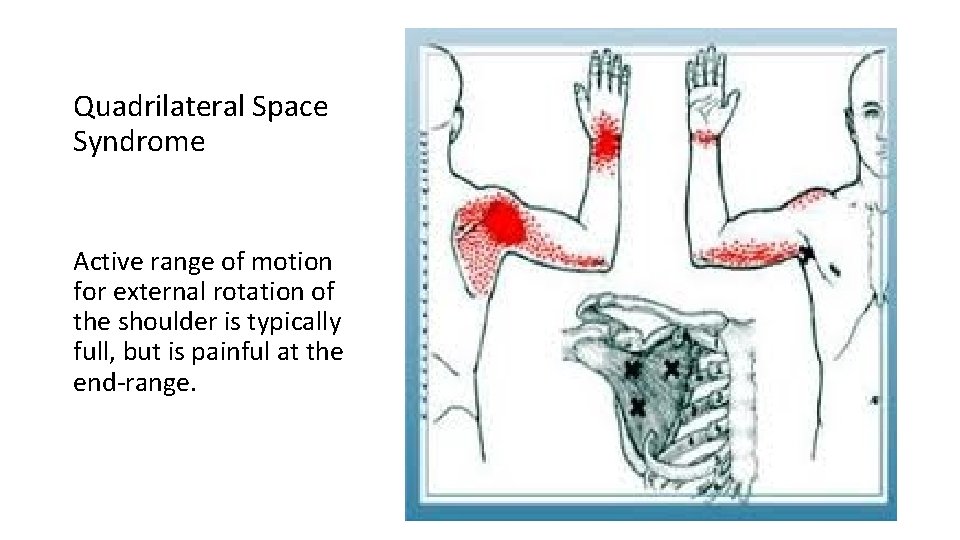
Quadrilateral Space Syndrome Active range of motion for external rotation of the shoulder is typically full, but is painful at the end‐range.
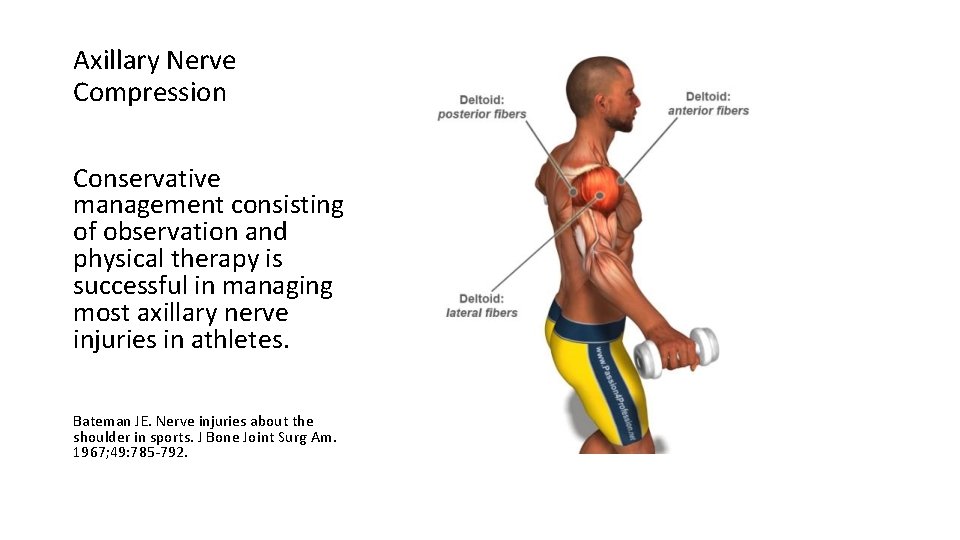
Axillary Nerve Compression Conservative management consisting of observation and physical therapy is successful in managing most axillary nerve injuries in athletes. Bateman JE. Nerve injuries about the shoulder in sports. J Bone Joint Surg Am. 1967; 49: 785‐ 792.
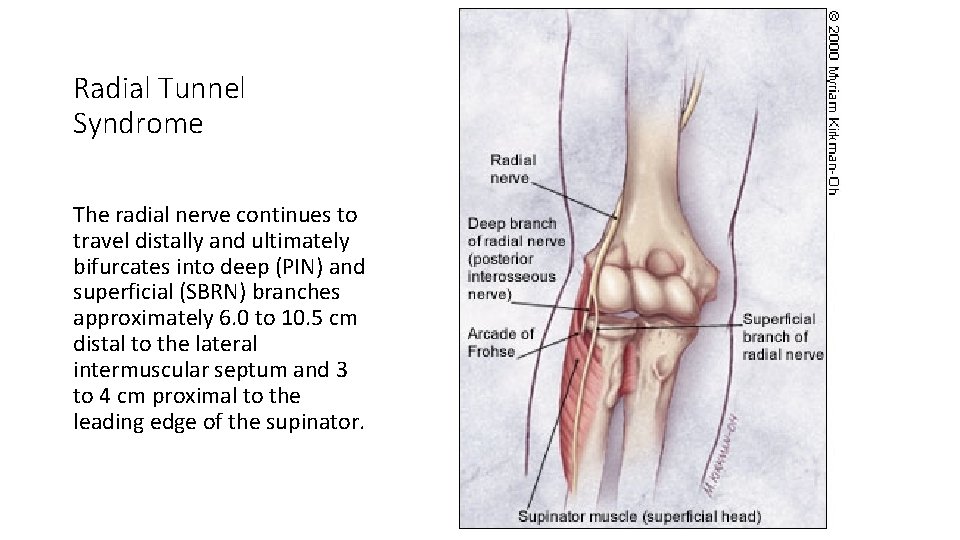
Radial Tunnel Syndrome The radial nerve continues to travel distally and ultimately bifurcates into deep (PIN) and superficial (SBRN) branches approximately 6. 0 to 10. 5 cm distal to the lateral intermuscular septum and 3 to 4 cm proximal to the leading edge of the supinator.
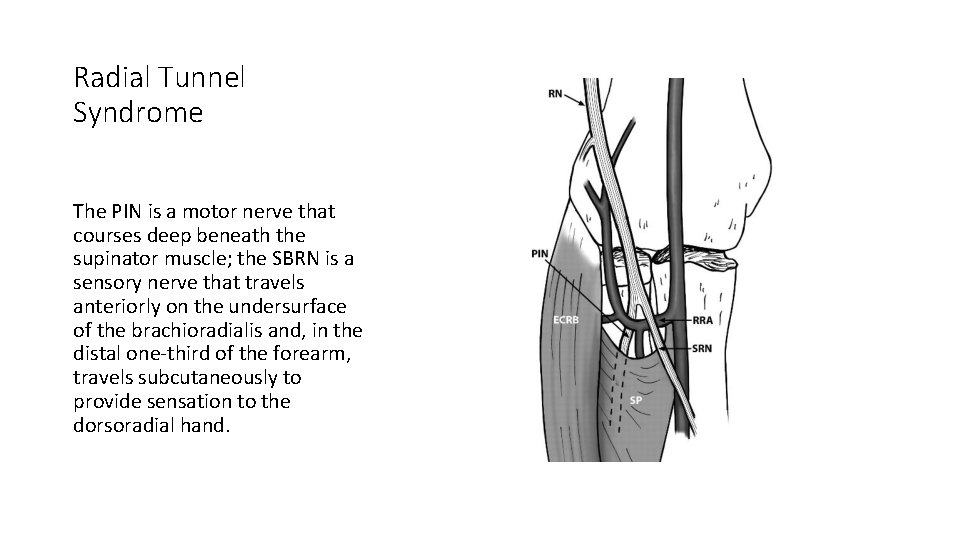
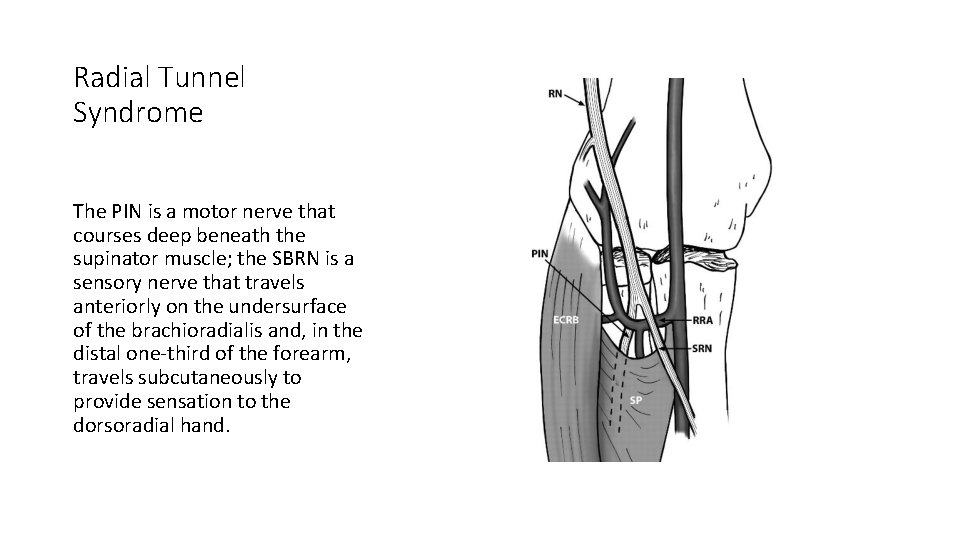
Radial Tunnel Syndrome The PIN is a motor nerve that courses deep beneath the supinator muscle; the SBRN is a sensory nerve that travels anteriorly on the undersurface of the brachioradialis and, in the distal one‐third of the forearm, travels subcutaneously to provide sensation to the dorsoradial hand.

Risk Factors • Regular use of force of at least 1 kg for more that 10 repetitions per hour with the elbow constantly extended between 0 degrees and 45 degrees with frequent pronation and supination of the forearm would increase the chance of developing radial tunnel syndrome. • Roquelaure Y, Raimbeau G, Saint‐Cast Y, et al. Occupational risk factors for radial tunnel syndrome in factory workers. Chir Main 2003; 22: 293‐ 8.
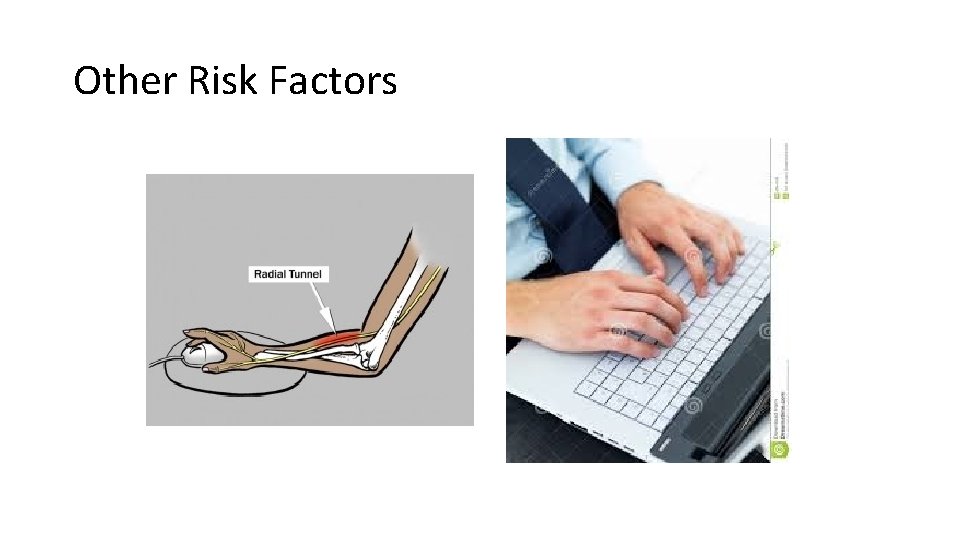
Other Risk Factors

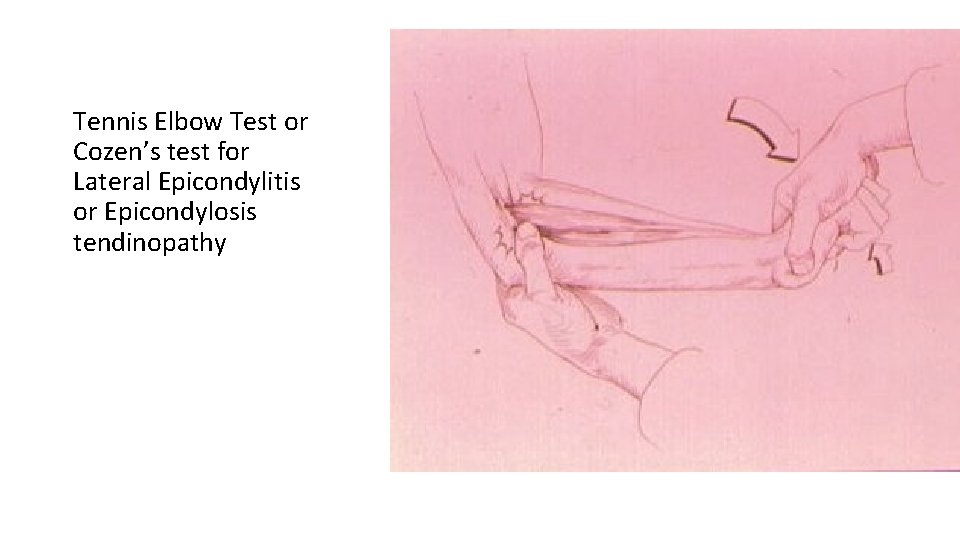
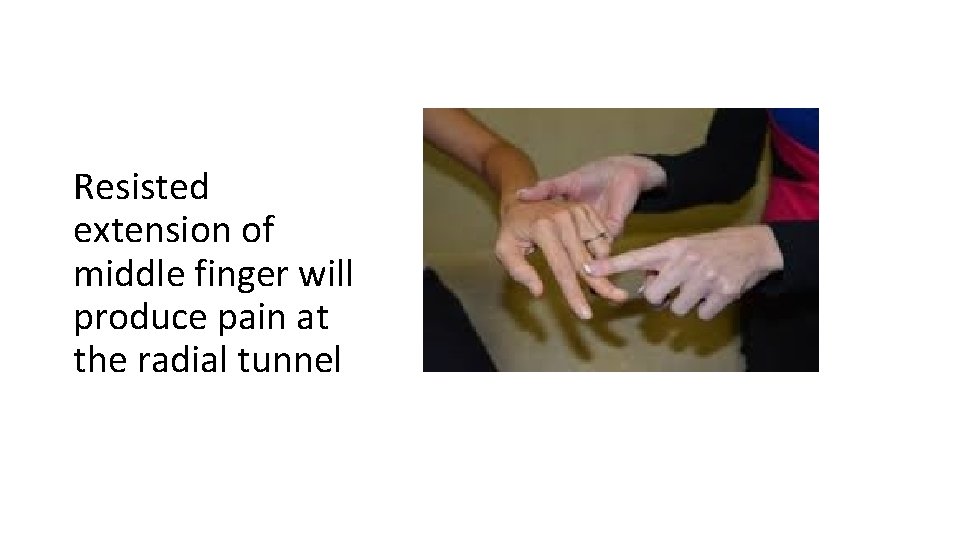
Physical Examination • Localized focal tenderness over the anatomical landmark, approximately 3‐ 5 cm distal to the lateral epicondyle over the supinator mass (Loh and “Rule of Nine”). • Cozen’s test is usually negative for pain but active forearm supination or extension of middle finger with resistance produces pain at radial tunnel.
Definition of an orthopedic test • Most often, a provocative maneuver that reproduces the patient’s chief concern pain by stretching, compressing and/or contracting of tissues in order to identify the involved tissues.
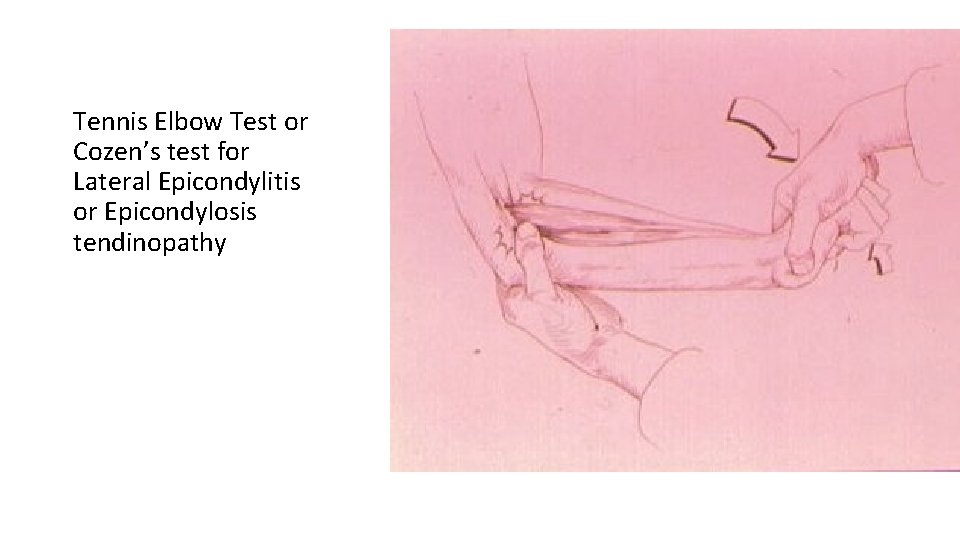
Tennis Elbow Test or Cozen’s test for Lateral Epicondylitis or Epicondylosis tendinopathy
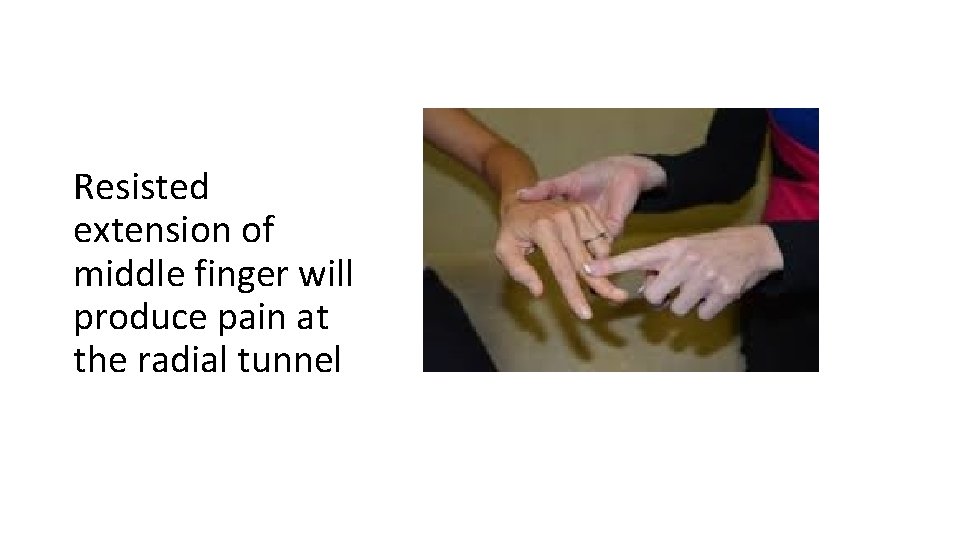
Resisted extension of middle finger will produce pain at the radial tunnel
Examination of Related Areas
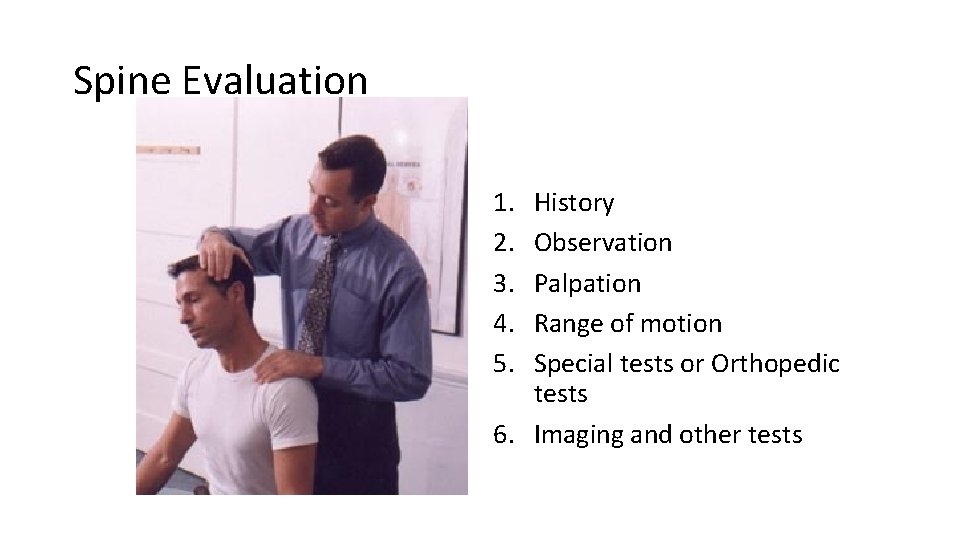
Spine Evaluation 1. 2. 3. 4. 5. History Observation Palpation Range of motion Special tests or Orthopedic tests 6. Imaging and other tests
Differential Diagnoses • Lateral epicondylosis • Posterior interosseous nerve syndrome (Deep branch of the radial nerve) “motor nerve” • Radial tunnel syndrome (Superficial branch of the radial nerve) “sensory nerve” • Wartenberg’s Syndrome • Ulnar Neuropathy
Treatment • Conservative care should precede surgical intervention • Wrist splinting • Activity modification • NSAIDS • Avoid activities or treatments that increase the symptoms
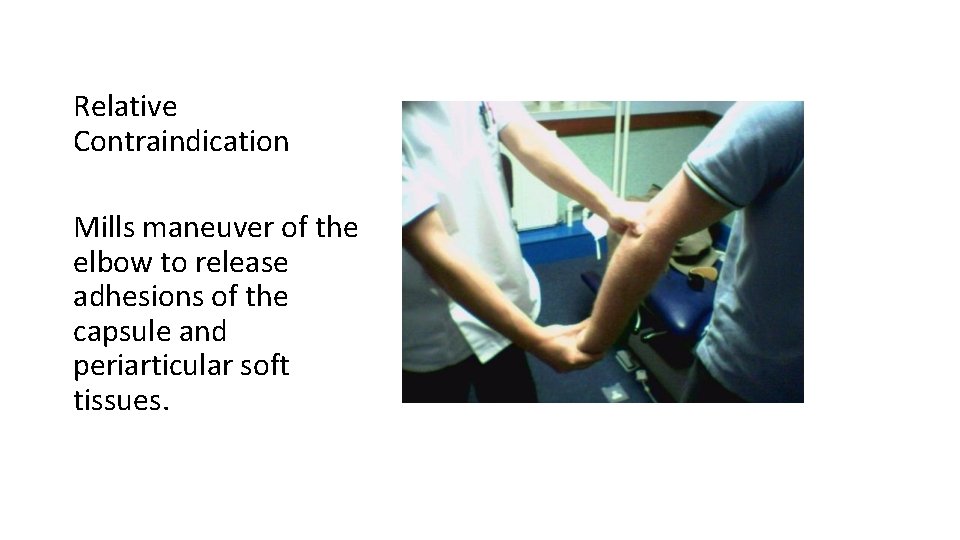
Relative Contraindication Mills maneuver of the elbow to release adhesions of the capsule and periarticular soft tissues.
Absolute Contraindications • Soft tissue treatments (Instrument assisted, deep friction massage, and stretching) • Heat/Ultrasound • Tennis elbow brace • Repetitive strain activities such as progressive resistive exercises, walking dog, use of laptop and tools that require pronation of forearm
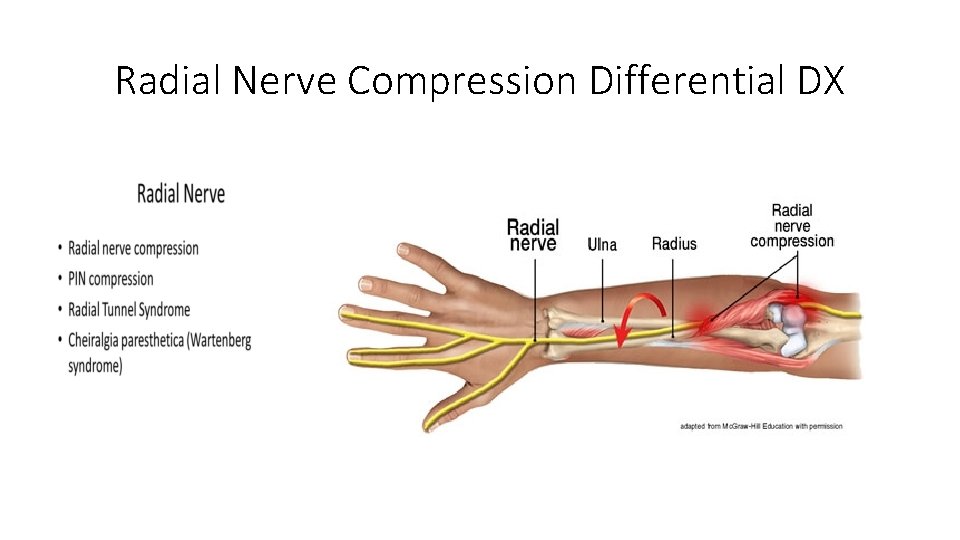
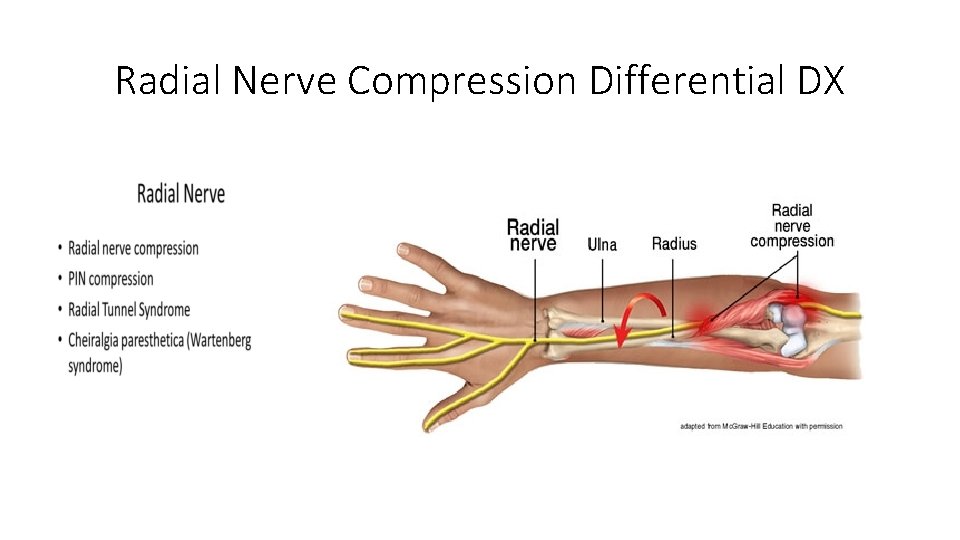
Radial Nerve Compression Differential DX
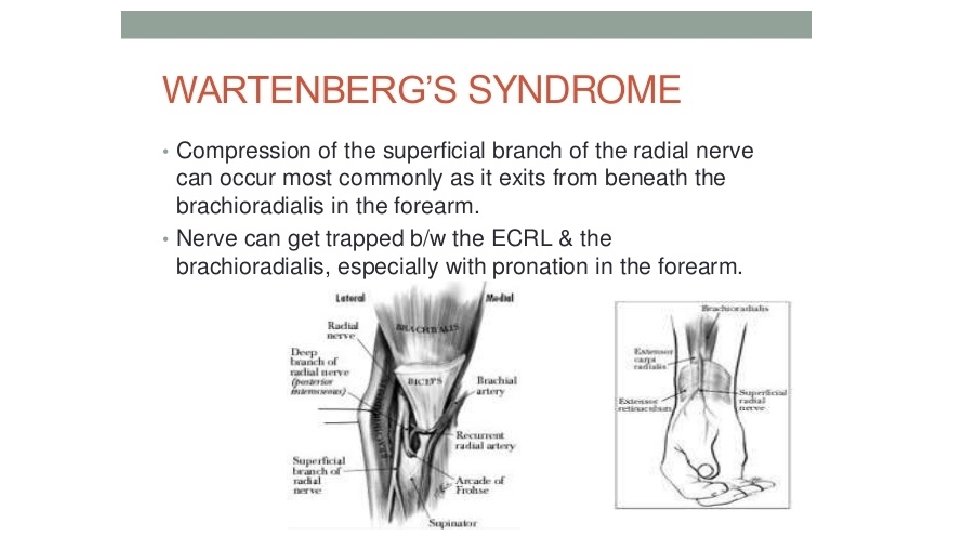
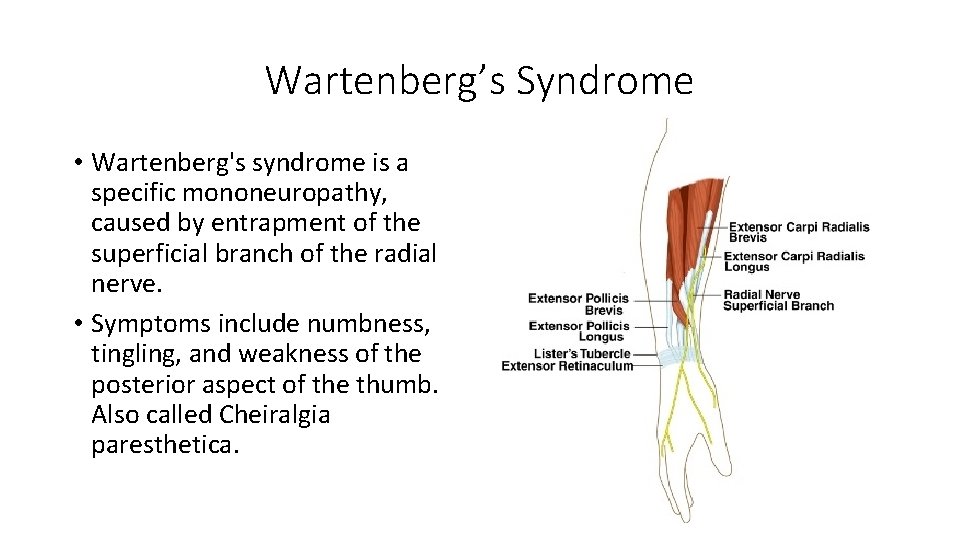
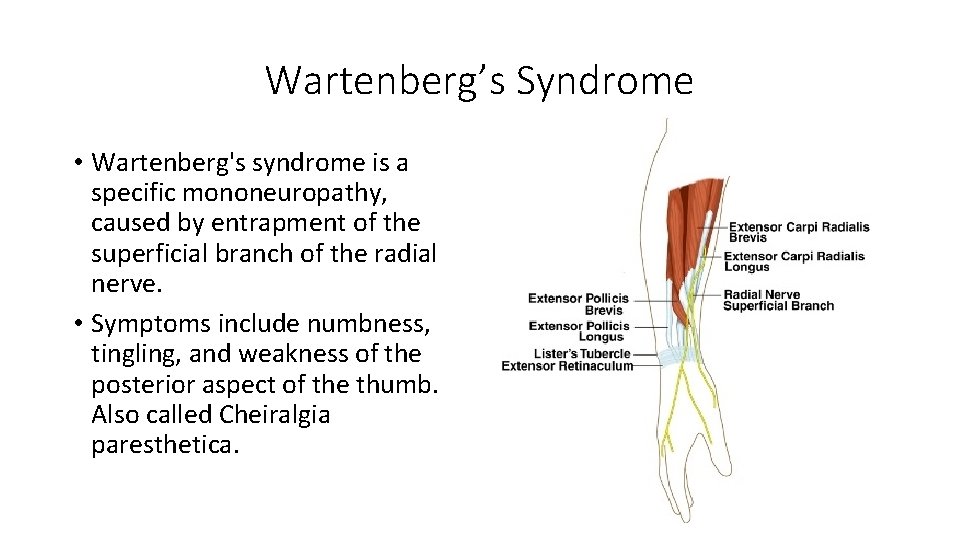
Wartenberg’s Syndrome • Wartenberg's syndrome is a specific mononeuropathy, caused by entrapment of the superficial branch of the radial nerve. • Symptoms include numbness, tingling, and weakness of the posterior aspect of the thumb. Also called Cheiralgia paresthetica.
Recommendations prior to treating patients with whiplash injuries. Discover mechanism of injury Determine history of neck pain prior to whiplash injury Reveal pain severity with Numerical Pain Rating Scale (NPRS) Identify the injured tissues and pain generators Understand biopsychosocial factors Perform differential diagnosis Determine a reasonable prognosis Offer appropriate treatment with the use of a team of health care providers • Avoid nocebo effect and promote placebo effect… • •
Recommended Reading • Lehman JJ. Statin Myopathy: A Common Cause of Chronic Pain. ACA News “Feature Article. ” • Lehman S. and Lehman J. NNT for Statins vs. the Mediterranean Diet. ACA News. • Fernandez G, et al. Statin myopathy: A common dilemma not reflected in clinical trials. CLEVELAND CLINIC JOURNAL OF MEDICINE VOLUME 78 • NUMBER 6 JUNE 2011.
Videos • Statin drugs and memory loss/diabetes. https: //www. bing. com/videos/search? q=statin+myopathy+abc&&view=de tail&mid=55 F 99 CBE 9 C 196962 F 363&&FORM=VRD GAR • Matters of the heart. ABC • Dietary Villians https: //www. bing. com/videos/search? q=heart+of+the+matter+australian+ broadcasting&&view=detail&mid=BE 7 C 234 A 79 A 107 B 9 BB 13&&FORM=VRDGAR • Cholesterol Drug Wars • https: //www. bing. com/videos/search? q=cholesterol+drug+war+abc&&vie w=detail&mid=C 9 D 5507 C 80443 BE 9871 A&&FOR M=VRDGAR
References 1. Barnsley L, Lord S, Bogduk N. Whiplash injury. Pain. 1994; 58: 283– 307. 2. Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on Whiplash‐Associated Disorders: redefining “whiplash” and its management. Spine. 1995; 20: 1 S– 73 S. 3. Elliot JM, et al. Characterization of Acute and Chronic Whiplash‐Associated Disorders. Journal of Orthopaedic & Sports Physical Therapy, 2009, Volume: 39 Issue: 5 Pages: 312‐ 323. 4. Jouko Kivioja, Irene Jensen, and Urban Lindgren. Neither the WAD‐classification nor the Quebec Task Force follow‐up regimen seems to be important for the outcome after a whiplash injury. A prospective study on 186 consecutive patients. Eur Spine J. 2008 Jul; 17(7): 930– 935. Hasue M. Pain and the nerve root. An interdisciplinary approach. Spine. 1993; 18: 2053‐ 2058. 6. Jansen J, Bardosi A, Hildebrandt J, Lucke A. Cervicogenic, hemicranial attacks associated with vascular irritation or compression of the cervical nerve root C 2. Clinical manifestations and morphological findings. Pain. 1989; 39: 203‐ 212. 7. Kaale BR, Krakenes J, Albrektsen G, Wester K. Head position and impact direction in whiplash injuries: associations with MRI‐verified lesions of ligaments and membranes in the upper cervical spine. J Neurotrauma. 2005; 22: 1294‐ 1302. 8. Kaale BR, Krakenes J, Albrektsen G, Wester K. Whiplash‐associated disorders impairment rating: neck disability index score according to severity of MRI findings of ligaments and membranes in the upper cervical spine. J Neurotrauma. 2005; 22: 466‐ 475. 9. Jonsson H, Jr, Bring G, Rauschning W, Sahlstedt B. Hidden cervical spine injuries in traffic accident victims with skull fractures. J Spinal Disord. 1991; 4: 251. 10. Pettersson K, Hildingsson C, Toolanen G, Fagerlund M, Bjornebrink J. Disc pathology after whiplash injury. A prospective magnetic resonance imaging and clinical investigation. Spine. 1997; 22: 283‐ 287; discussion 288. 263.
References 11. Borchgrevink GE, Kaasa A, Mc. Donagh D, Stiles TC, Haraldseth O, Lereim I. Acute treatment of whiplash neck sprain injuries. A randomized trial of treatment during the first 14 days after a car accident. Spine. 1998; 23: 25‐ 31. 12. Kasch H, Qerama E, Bach FW, Jensen TS. Reduced cold pressor pain tolerance in non‐recovered whiplash patients: a 1‐year prospective study. Eur J Pain. 2005; 9: 561‐ 569. 13. Tjell, C. and U. Rosenhall (1998). “Smooth pursuit neck torsion test: a specific test for cervical dizziness. ” Otology & Neurotology 19(1): 76. 14. Treleaven, J. , G. Jull, et al. (2003). “Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. ” Journal of Rehabilitation Medicine 35(1): 36‐ 43. 15. Treleaven, J. , G. Jull, et al. (2005). “Smooth pursuit neck torsion test in whiplash‐associated disorders: relationship to self‐reports of neck pain and disability, dizziness and anxiety. ” Journal of Rehabilitation Medicine 37(4): 219‐ 223. 16. Treleaven, J. , G. Jull, et al. (2005). “Standing balance in persistent whiplash: a comparison between subjects with and without dizziness. ” Journal of Rehabilitation Medicine 37(4): 224‐ 229. 17. Jull, G. , D. Falla, et al. (2007). “Retraining cervical joint position sense: The effect of two exercise regimes. ” Journal of Orthopaedic Research 25(3): 404‐ 412. 18. Treleaven J, Jull G, Sterling M. Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med. 2003 Jan; 35(1): 36‐‐‐ 43. 19. Sterling M, et al. Sensory hypersensitivity occurs soon after whiplash injury and is associated with poor recovery Pain 104 (2003) 509‐ 517. 20. Adams JH, Doyle D, Ford I, Gennarelli TA, Graham DI, Mc. Lellan DR. Diffuse axonal injury in head injury: definition, diagnosis and grading. Histopathology. 1989; 15: 49– 59. 21. Walton DM, & Elliott JM. An Integrated Model of Chronic Whiplash‐Associated Disorder. Journal of Orthopedic and Sports Physical Therapy. July 2017, Volume 47, Number 7.
 Whiplash symptoms
Whiplash symptoms Whiplash tic
Whiplash tic Whiplash injury
Whiplash injury Diagnosis of post traumatic stress disorder
Diagnosis of post traumatic stress disorder Offender personality disorder pathway
Offender personality disorder pathway Malingering
Malingering Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Bổ thể
Bổ thể Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Chúa yêu trần thế
Chúa yêu trần thế Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Số nguyên tố là
Số nguyên tố là đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới ưu thế lai là gì
ưu thế lai là gì Hệ hô hấp
Hệ hô hấp Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Tư thế ngồi viết
Tư thế ngồi viết Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Cái miệng nó xinh thế
Cái miệng nó xinh thế Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Tư thế ngồi viết
Tư thế ngồi viết Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Chó sói
Chó sói Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Diễn thế sinh thái là
Diễn thế sinh thái là Frameset trong html5
Frameset trong html5 Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau 101012 bằng
101012 bằng Lời thề hippocrates
Lời thề hippocrates Tư thế worm breton là gì
Tư thế worm breton là gì đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Cong thức tính động năng
Cong thức tính động năng Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dot
Dot Acute toxic encephalopathy icd 10
Acute toxic encephalopathy icd 10 Acute pancreatitis ct
Acute pancreatitis ct Pncreas pain
Pncreas pain Definition of acute appendicitis
Definition of acute appendicitis Panophtalmitis
Panophtalmitis Whats an acute angle
Whats an acute angle Cholecystitis pathogenesis
Cholecystitis pathogenesis All triangles have equal sides and angles true or false
All triangles have equal sides and angles true or false Lyphadenitis
Lyphadenitis Lchad deficiency
Lchad deficiency Acute productive cough differential diagnosis
Acute productive cough differential diagnosis Acute triangle
Acute triangle Interference figure
Interference figure Acute glomerulonephritis causes
Acute glomerulonephritis causes Aki aki aki
Aki aki aki Acute blood loss anemia
Acute blood loss anemia Acute care toolkit
Acute care toolkit Iga nephropathy vs psgn
Iga nephropathy vs psgn Acute fulminating preeclampsia
Acute fulminating preeclampsia Odynophagia vs dysphagia
Odynophagia vs dysphagia Excecerbate
Excecerbate Ghs pictogram depicts which hazard
Ghs pictogram depicts which hazard Neuroleptic drug
Neuroleptic drug Opt.model
Opt.model Pes statement for acute pancreatitis
Pes statement for acute pancreatitis Cholecystitis nursing care plan
Cholecystitis nursing care plan Acute abdomen treatment
Acute abdomen treatment An acute highly contagious viral disease
An acute highly contagious viral disease I think i have schizophrenia
I think i have schizophrenia Vascular response in acute inflammation
Vascular response in acute inflammation Acute apical periodontitis clinical features
Acute apical periodontitis clinical features Functions of plasma proteins
Functions of plasma proteins Acute liver failure criteria
Acute liver failure criteria Nsaids and ulcers
Nsaids and ulcers Acute coronary syndrome
Acute coronary syndrome Importance of toxicology
Importance of toxicology Acute bronchospasm
Acute bronchospasm Lodcraft
Lodcraft Joo acute nasopharyngitis
Joo acute nasopharyngitis Object with obtuse angle
Object with obtuse angle Stroke algorithm
Stroke algorithm Acute megaloblastic anemia
Acute megaloblastic anemia Acute vs subacute rehab
Acute vs subacute rehab Name 2 objects with acute angles
Name 2 objects with acute angles Acute mylogenous leukemia
Acute mylogenous leukemia Cellular events of acute inflammation
Cellular events of acute inflammation Acute care collaboration
Acute care collaboration Acute brain failure
Acute brain failure Causes of dysphagia
Causes of dysphagia Sce physical examination
Sce physical examination Acute inflammation
Acute inflammation Steatorrhea pictures
Steatorrhea pictures Ranson criteria
Ranson criteria Accs acute medicine
Accs acute medicine Ukons triage tool
Ukons triage tool Acute radiation sickness (ars)
Acute radiation sickness (ars) Na triangle
Na triangle Acute tubular necrosis causes
Acute tubular necrosis causes 8-5 the tangent ratio
8-5 the tangent ratio