ACUTE SURGICAL INFECTION NonSpecific Acute Infection NonSpecific Acute
![Boil [Furuncle] Is a staphylococcal infection of a hair follicle or a sebaceous gland. Boil [Furuncle] Is a staphylococcal infection of a hair follicle or a sebaceous gland.](https://slidetodoc.com/presentation_image/d8f352fa7d6f40f05b236a63f4b66ac2/image-21.jpg)

![Prevention n n Immunization [active] with tetanus toxoid with routine childhood immunization, with booster Prevention n n Immunization [active] with tetanus toxoid with routine childhood immunization, with booster](https://slidetodoc.com/presentation_image/d8f352fa7d6f40f05b236a63f4b66ac2/image-52.jpg)



- Slides: 70
ACUTE SURGICAL INFECTION Non-Specific Acute Infection
Non-Specific Acute Infection q q q q q Postoperative Wound Infection Cellulitis Erysipelas Boil (Furuncle) Carbuncle Hydradenitis Suppurativa Acute Abscess Acute Lymphangitis and Lymphadenitis Bacteraemia and Septicaemia
Specific Acute Infections q Tetanus q Gas Gangrene q Necrotizing Fasciitis
Postoperative Wound Infections Are caused by the presence of contaminating microbes derived from : Endogenous OR Exogenous
Postoperative Wound Infection Predisposing Factors: # General 1 - Poor general condition 2 - Systemic disease 3 - Drugs that cause immunosuppression
Postoperative Wound Infection # Local : 1 - Poor blood supply 2 - Poor surgical technique 3 - Presence of foreign bodies 4 - Nature of the operation 5 - Defect in sterilization technique in the operating theatre
Types of surgical wounds Operative wounds are divided into three categories : 1 - Clean The risk of infection is 1 -2% 2 - Clean contaminated The risk of infection 2 -5% 3 - Contaminated The risk of infection is 5 -30%
Pathology Acute inflammatory stage with local vasodilatation and infiltration by polymorph nuclear leucocytes. This is followed by suppuration with purulent discharge
Clinical Picture Wound infection usually appears between the fifth and tenth days postoperative * Fever * Pain in the wound Signs: _ swollen _tenderness _redness _fluctuant
Differential Diagnosis Other causes of postoperative fever - chest infection - DVT - UTI Other causes of wound swelling - heamatoma
Prophylaxis * Improve the defense mechanism * Control the predisposing factors * Prophylactic antibiotics * In bowel surgery, mechanical and chemical preparation of the bowel * Meticulous surgery * Operation in septic areas with heavily contaminated wounds should be left open
Treatment Surgical drainage of the pus n Antibiotics in invasive infections n Look for hospital acquired infection n
Cellulitis Is an invasive non suppurative infection of the loose connective tissue n Organism : Ø streptococci [common] Ø staphylococci [occasionally] Ø mix n
Clinical picture n n n n The affected area is red, indurated, hot and painful It spreads rapidly with ill defined edge The skin may be the seat of blisters Fever Lymphangitis in the form of red streaks No suppuration In severe cases patches of skin necrosis with sloughing of subcutaneous tissues
Differetial Diagnosis n Contact allergy n Chemical inflammation n DVT
Treatment n Rest and elevation of the affected part n Antibiotic penicillin iv
Erysipelas Is a rapidly spreading non-suppurative inflammation of the lymphatics of the skin caused by a specific strain of hemolytic streptococci
Clinical Picture Toxemia n Locally : similar to cellulitis, but there are the following differences: 1. The color of the skin is rose-pink 2. The edge is well defined 3. There may islets of inflammation beyond the spreading margin n
Complications n 1. Facial erysipelas may lead to cavernous sinus thrombosis n 2. Septicemia n 3. Recurrent erysipelas may block the lymphatics leading to elephantiasis.
Treatment n Isolation n Similar to cellulitis
![Boil Furuncle Is a staphylococcal infection of a hair follicle or a sebaceous gland Boil [Furuncle] Is a staphylococcal infection of a hair follicle or a sebaceous gland.](https://slidetodoc.com/presentation_image/d8f352fa7d6f40f05b236a63f4b66ac2/image-21.jpg)
Boil [Furuncle] Is a staphylococcal infection of a hair follicle or a sebaceous gland. n The common sites: face, neck and axilla. n n Common in diabetics.
Clinical Picture A small painful indurated swelling which is - red - hot - and very tender
Treatment n 1. Antibiotics. n 2. Antiseptic.
Carbuncle n Is infective gangrene of the subcutaneous tissues usually secondary to infection by Staphylococcus aureus. It is common in immunocompromised patients as in diabetics. n The common sites: face, nape of the neck, and the back n
Pathology Infection usually starts in a hair follicle n Extends to the subcutaneous fat where other hair follicles get the infection. n Multiple areas of necrosis and thrombosis of blood vessels occur. n Patches of skin undergo sloughing and separate from the underlying granulation tissue n
Clinical Picture There is usually sever toxemia. n Starts as a painful induration of the skin and subcutaneous tissues. n The skin is red. n Swelling its central part becomes soft. n Multiple areas of skin thin out and separate forming multiple sinuses. n
Complications n Local spread of infection. n Pyaemia and septicemia. n Cavernous sinus thrombosis n Epidural abscess or meningitis
Treatment 1. Antibiotics. 2. culture and sensitivity of the discharge. 3. control of diabetes. 4. surgical excision of sloughs.
Hydradenitis Suppurativa Mixed staph. And streptococcal infection of the apocrine sweat glands, in the perineum or the axilla, produces multiple abscesses and pus discharging sinuses.
Treatment n Surgical drainage of abscesses. n Antiseptic and antifungal applications. n Surgical excision of the apocrine sweat -bearing skin following by skin grafting is essential.
Acute Abscess It is a localized suppurative inflammation. n It is caused by pyogenic organisms. The commonest are staphylococci that produce a coagulase enzyme. n
Pathogenesis The organism reach the tissues by : - direct access through wounds, scratches and abrasions. - local extension from an adjacent focus - lymphatic spread. - blood spread.
Pathology An abscess consists of three zones: 1 - A central zone of coagulative necrosis 2 - An intermediate zone of granulation tissue. 3 - A peripheral zone of acute inflammation.
Sequlea n Resolution. n Pointing and rupture. Spread infection – locally - by lymphatics or blood n Chronicity. n
Clinical Picture Locally : - painful tender mass -The covering skin is red, and oedematous -The draining lymph nodes are usually enlarged and tender n Systemic : -Fever -Malaise -Headache -Tachycardia -Anorexia n
When Pus Forms n n n The fever becomes hectic. Skin shows pitting oedema. The pain becomes throbbing. n n n The inflamatory reaction becomes localized Fluctuation test becomes positive. There is shooting leucocytosis
Treatment n Before suppuration: n After suppuration: - antibiotic, rest -hot application. -supportive general measures. -adequate surgical drainage. -a specimen of the pus is sent for culture and sensitivity. -antibiotic if there is systemic manifestation.
Acute Lymphangitis and Lyphadenitis Acute lymphangitis: is due to infection of lymph vessels by organisms usually streptococci. n Acute lymphadenitis: is due to spread of infection along lymphatics from a septic focus in the drainage area to the lymph- nodes. n
Treatment n Antibiotics. n Hot applications. n Surgical drainage if suppuration occurs.
Bacteraemia n n Presence of bacteria which are NOT multiplying, in the blood. It usually follows: - dental work. -instrumentation of the urinary tract It is hazardous in patients with : -damaged heart valves. -prosthetic valves. -immunosuppression Prophylactic antibiotics is essential
Septicemia The presence of multiplying organisms in the blood stream.

Specific Acute Infections
Tetanus It is a specific anaerobic infection that is mediated by neurotoxin of: Clostridium tetani and leads to: nervous irritability and tetanic muscular contractions.
Aetiology Organism: Clostridiuam tetani is gram positive anaerobic bacillus with a terminal spore giving the characteristic drum-stick appearance.
Mode Of Infection n 1. Wounds: -hypoxic, containing devaitalized tissue or a foreign body. n 2. Umbilical stump: tetanus neonatorum
Pathology n n n The neurotoxin is an exotoxin produced locally and reaches the central nervous system along the blood stream, the motor nerves or both. When the toxin reaches the nervous system, it is fixed by the motor cells and can not be detected in the blood or CSF. The antitoxin can only neutralize the toxin before it gets fixed to the nervous tissue.
The toxin increases the exitability of the motor cells of the medulla and spinal cord, so slightest stimuli produce violent spasm. n Death results from exhaustion, hyperpyrexia, heart failure, asphyxia or pneumonia. n
Clinical Picture n n Incubation period: - In non-immunized is short from 24 H to 15 days. - In immunized is longer than 11 days to several weeks or months. Symptoms during incubation period are vague such as : tenderness, rigidity of the muscles, swelling at the site of wound, local twitches, restlessness, and an anxiety.
n Tonic stage: -Pain and tingling in the area of injury. -Limitation of movements of the jaw. -Spasm of the facial muscles. -Stiffness of the neck. -Dysphagia. -Laryngospasm. -Hesitancy in micturition.
n Clonic stage: -Reflex paroxysms of violent muscular contraction. -Relaxation is incomplete during the intervals between clonic contractions. -Spasm of the intercostal muscles and diaphragm lead to long period of apnea. -Temperature elevated with profuse sweating. -Marked tachycardia
Laboratory Finding Polymorphnuclear leucocytosis.
![Prevention n n Immunization active with tetanus toxoid with routine childhood immunization with booster Prevention n n Immunization [active] with tetanus toxoid with routine childhood immunization, with booster](https://slidetodoc.com/presentation_image/d8f352fa7d6f40f05b236a63f4b66ac2/image-52.jpg)
Prevention n n Immunization [active] with tetanus toxoid with routine childhood immunization, with booster injections every 7 -10 years. Individuals who previously received three or more doses, the last within 10 years: need a booster dose of tetanus toxoid. Those who received less than three doses: -need a booster dose of tetanus toxoid and tetanus immunoglobulin [passive]. Individuals not previously immunized: -need full immunization with tetanus toxoid and tetanus immunoglobulin.
Treatment Neutralize toxin with TIG. n Wound debridment. n Avoid sudden stimuli. n Muscle relaxant with mechanical ventilation may require tracheostomy. n Aqueous penicillin G , 10 -40 million units a day IV. n Nursing. n
Gas Gangrene It is an acute spreading infection associated with gas formation and profound toxaemia caused by anaerobic spore-bearing bacilli of the clostridium group.
Pathology n Clostridia proliferate and produce toxins that diffuse into the surrounding tissue. n The toxins destroy local circulation. n This allows further invasion.
Factors predisposing to gas gangrene: Lacerated wounds involving bulky muscles. n Presence of foreign bodies or devitalized tissues. n Ischemia of muscles. n Infection by anaerobic bacteria. n As a complication of above knee amputation in patient with faecal incontinence. n
Bacteriology Organisms falls into two groups: n Saccharolytic organisms: -Cl. welchii, -Cl. septicum, -and Cl. oedematiens n Proteolytic organisms: -Cl. sporogenes, -Cl. histolyticum and Cl. tertium. n
Clinical Picture The incubation period varies from few hours to few days. n Generally ; the patient is pale, anxious, and apprehensive. -The temperature may be raised and there is marked tachycardia. -The hands are cold and clammy. -An icteric tinge may be present and there is oliguria. In severe case there is shock. n
n Locally: -pain and numbness in the affected area. -swelling and there may be crepitus with gas bubbles. -A sanguineous dischrge of a characteristic odour. -The affected muscles brick red then greenish and finally black discolouration, do not contract, do not bleed if cut, the skin black.
Prevention n Adequate debridement of wounds. n Antibiotics. n Avoid tissue hypoxia.
Treatment n Wound management. n Hyperbaric oxygenation. n Antibiotics: penecillin.
Necrotizing Fasciitis n It is an invasive infection usually caused by a mixed microbial flora including microphilic streptococci, staphylococci, Gram-negative bacteria and anaerobes, especially peptostreptococci, and bacteroids.
Pathology The infectious process spreads along the fascial planes and results infectious thrombosis of the vessels passing between the skin and deep circulation. n Superficial skin necrosis follows. n Hemorrhagic bullae appear as the first sign of skin death. n Fascial and subcutaneous fat necrosis involves wider area than the skin. n
Clinical Picture There are manifestations of toxemia with fever and tachycardia. n The skin shows hemorrhagic bullae and necrosis surrounded by oedema and inflammation. n Crepitus is occasionally present. n
Investigations n Swab for culture and sensitivity n At surgery : oedematous, dull gray fascia and subcutaneous tissue with visible thrombi in penetrating vessels
Prevention n Adequate debridement of wounds n Antibiotics
Treatment n Surgical n Antibiotics n Blood transfusion



 Lyphadenitis
Lyphadenitis Surgical site infection bundle checklist
Surgical site infection bundle checklist Active phagocytes that increase rapidly acute infection
Active phagocytes that increase rapidly acute infection Acute upper respiratory infection unspecified คือ
Acute upper respiratory infection unspecified คือ Specific vs nonspecific defense
Specific vs nonspecific defense схема імунної відповіді
схема імунної відповіді Westermark sign
Westermark sign Specific defense vs nonspecific defense
Specific defense vs nonspecific defense Concave ekg
Concave ekg Nonspecific vs specific immunity
Nonspecific vs specific immunity Nonspecific host defense mechanism
Nonspecific host defense mechanism Jordaan surgical
Jordaan surgical Surgical conscience
Surgical conscience Low fowler's position
Low fowler's position Sutures vs stitches
Sutures vs stitches Picc line surgical wound oasis
Picc line surgical wound oasis Wellspan inet
Wellspan inet Avagard surgical scrub instructions
Avagard surgical scrub instructions Surgical team roles and responsibilities
Surgical team roles and responsibilities Esophgeal varices
Esophgeal varices Surgical metabolism
Surgical metabolism Joint hospital surgical grand round
Joint hospital surgical grand round Surgical education week
Surgical education week Ogden surgical medical society
Ogden surgical medical society Hematology word surgery
Hematology word surgery Richter hernia
Richter hernia Surgical neck
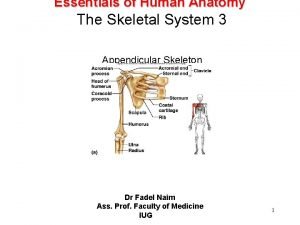
Surgical neck Corrective phase
Corrective phase Aorn eye prep
Aorn eye prep Lithotomy draping
Lithotomy draping Asepsis
Asepsis Bibliography of medical surgical nursing
Bibliography of medical surgical nursing Nasogastrio
Nasogastrio Dusting powder meaning
Dusting powder meaning Cmr surgical
Cmr surgical Hematology suffix
Hematology suffix Gordochom precio
Gordochom precio Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients Joint hospital surgical grand round
Joint hospital surgical grand round Conclusion of medical surgical nursing
Conclusion of medical surgical nursing Joint hospital surgical grand round
Joint hospital surgical grand round Surgical diathermy machine working principle
Surgical diathermy machine working principle Tatum surgical
Tatum surgical Qrc surgical
Qrc surgical Surgical plume evacuator tool
Surgical plume evacuator tool Chapter 22 surgical asepsis
Chapter 22 surgical asepsis History of surgical staplers
History of surgical staplers Joint hospital surgical grand round
Joint hospital surgical grand round Care of critically ill surgical patient
Care of critically ill surgical patient What part of the surgical gown is considered sterile
What part of the surgical gown is considered sterile Tmh
Tmh Surgical metabolism
Surgical metabolism Voluntary surgical contraception
Voluntary surgical contraception Aorn surgical hand scrub
Aorn surgical hand scrub Conclusion of oral medication
Conclusion of oral medication Basic surgical techniques semmelweis
Basic surgical techniques semmelweis Surgical gown
Surgical gown Suture colour coding
Suture colour coding Cpt surgical package
Cpt surgical package A newly admitted patient was found wandering
A newly admitted patient was found wandering Surgical audit definition
Surgical audit definition It is an instrument for grasping and holding
It is an instrument for grasping and holding Surgical bandage types
Surgical bandage types Deltoid tuberosity
Deltoid tuberosity Chapter 27 patient safety and quality
Chapter 27 patient safety and quality Managing surgical smoke
Managing surgical smoke Surgical prep
Surgical prep Difference between medical and surgical asepsis
Difference between medical and surgical asepsis The suffix iatry means
The suffix iatry means Surgical planning laboratory
Surgical planning laboratory What does a prolapsed uterus look like pictures
What does a prolapsed uterus look like pictures