Acute care toolkit 13 Acute care for adolescents

- Slides: 16
Acute care toolkit 13 Acute care for adolescents and young adults
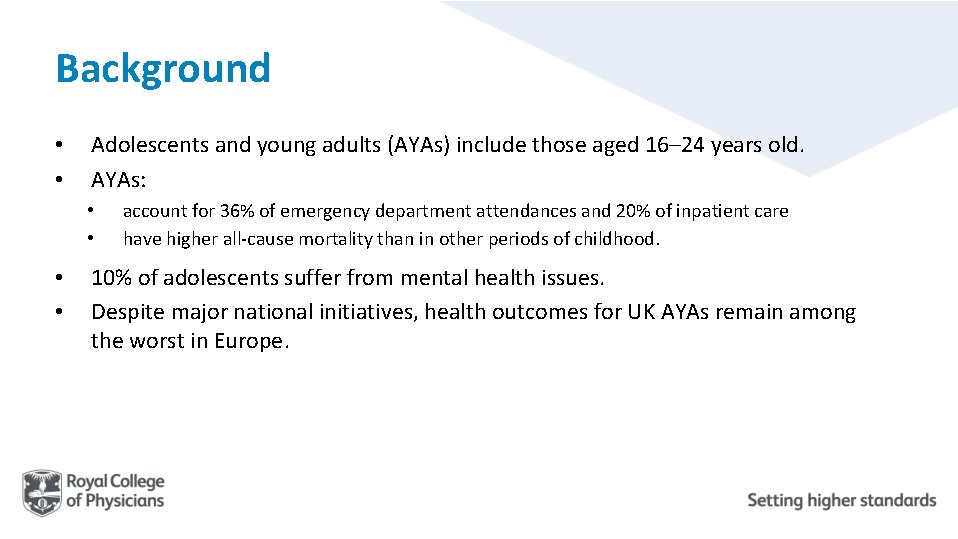
Background • • Adolescents and young adults (AYAs) include those aged 16– 24 years old. AYAs: • • account for 36% of emergency department attendances and 20% of inpatient care have higher all-cause mortality than in other periods of childhood. 10% of adolescents suffer from mental health issues. Despite major national initiatives, health outcomes for UK AYAs remain among the worst in Europe.
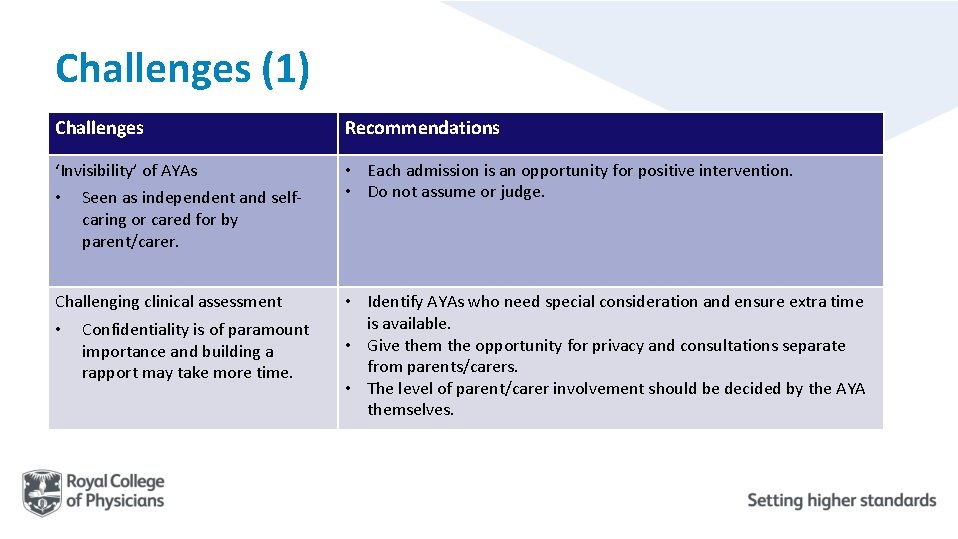
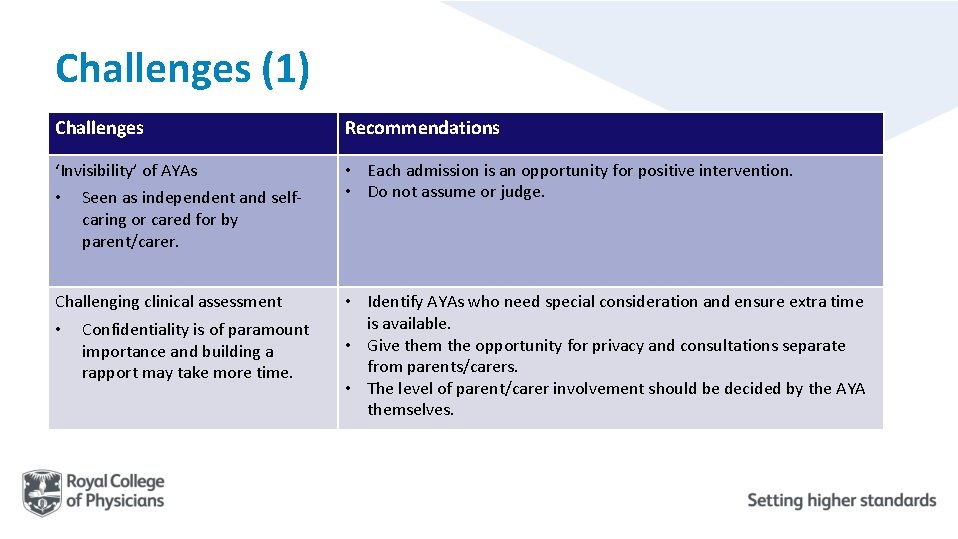
Challenges (1) Challenges Recommendations ‘Invisibility’ of AYAs • Each admission is an opportunity for positive intervention. • Do not assume or judge. • Seen as independent and selfcaring or cared for by parent/carer. Challenging clinical assessment • Confidentiality is of paramount importance and building a rapport may take more time. • Identify AYAs who need special consideration and ensure extra time is available. • Give them the opportunity for privacy and consultations separate from parents/carers. • The level of parent/carer involvement should be decided by the AYA themselves.
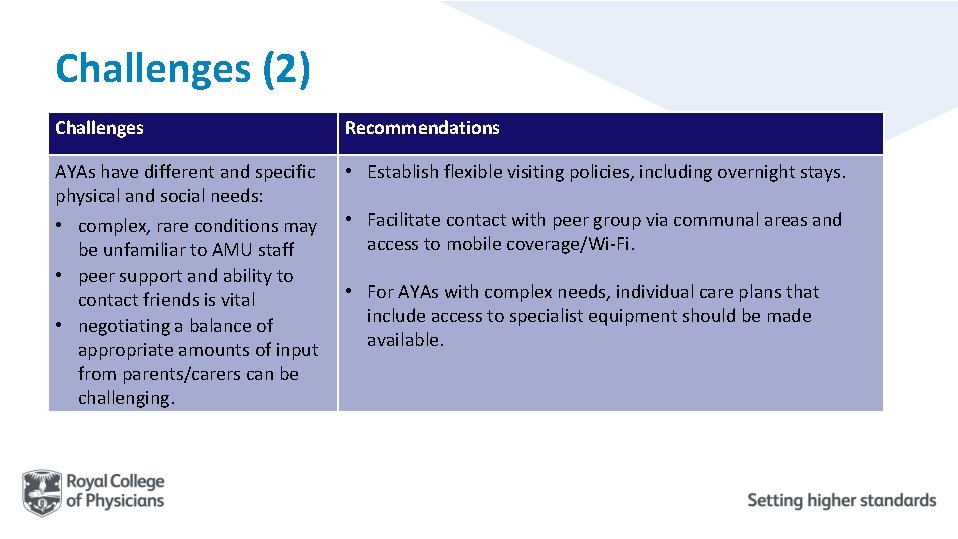
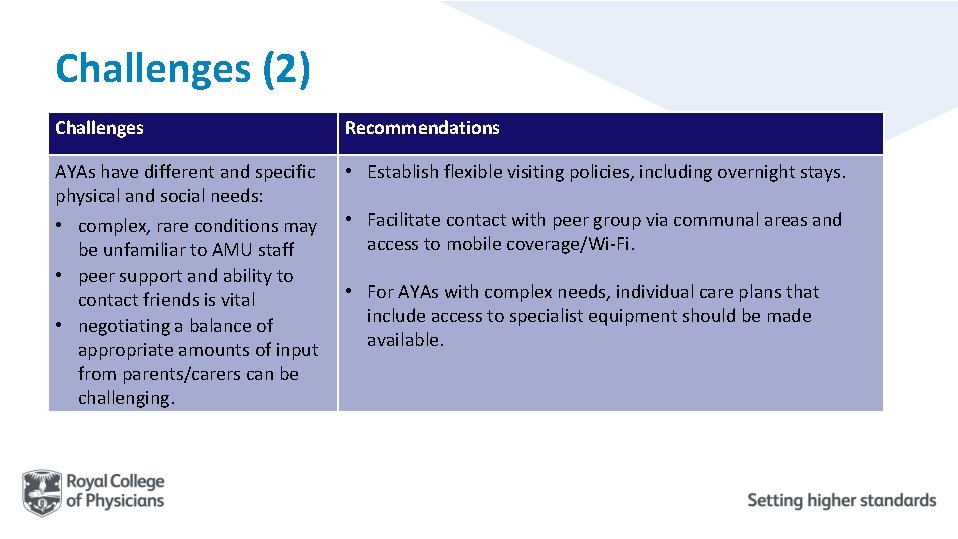
Challenges (2) Challenges Recommendations AYAs have different and specific physical and social needs: • complex, rare conditions may be unfamiliar to AMU staff • peer support and ability to contact friends is vital • negotiating a balance of appropriate amounts of input from parents/carers can be challenging. • Establish flexible visiting policies, including overnight stays. • Facilitate contact with peer group via communal areas and access to mobile coverage/Wi-Fi. • For AYAs with complex needs, individual care plans that include access to specialist equipment should be made available.
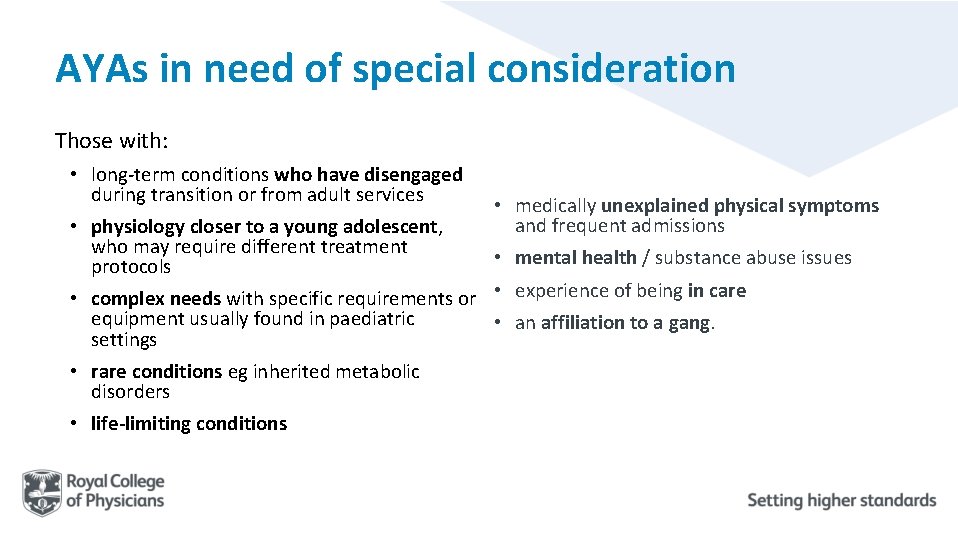
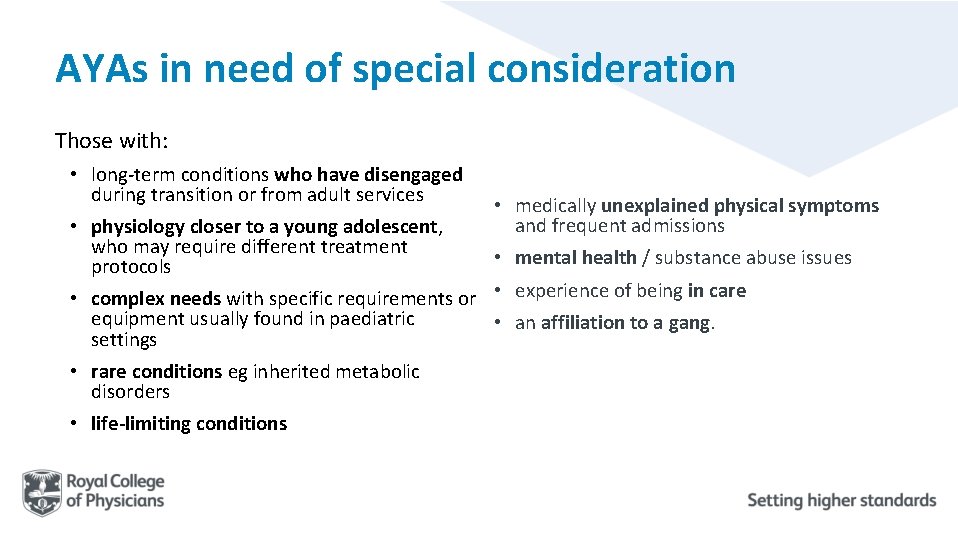
AYAs in need of special consideration Those with: • long-term conditions who have disengaged during transition or from adult services • physiology closer to a young adolescent, who may require different treatment protocols • complex needs with specific requirements or equipment usually found in paediatric settings • rare conditions eg inherited metabolic disorders • life-limiting conditions • medically unexplained physical symptoms and frequent admissions • mental health / substance abuse issues • experience of being in care • an affiliation to a gang.
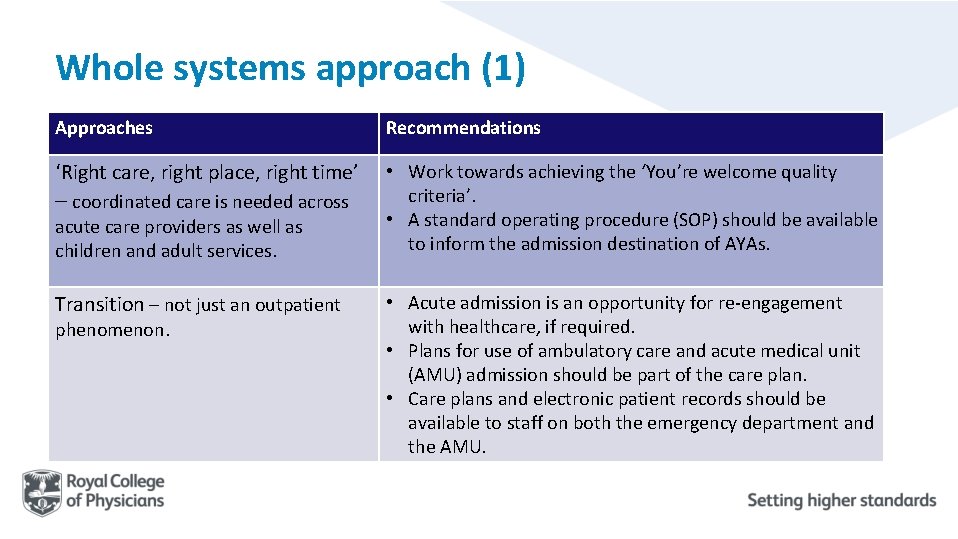
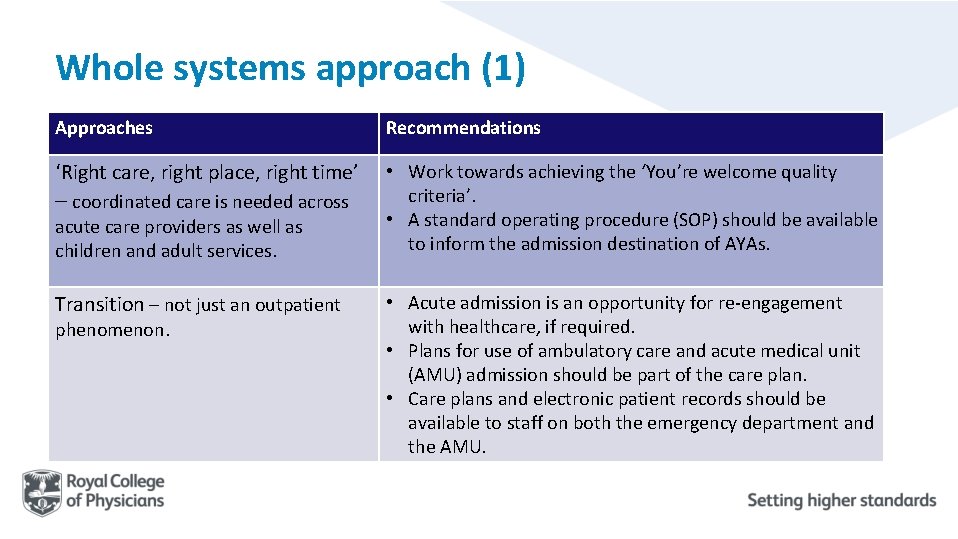
Whole systems approach (1) Approaches Recommendations ‘Right care, right place, right time’ • Work towards achieving the ‘You’re welcome quality criteria’. • A standard operating procedure (SOP) should be available to inform the admission destination of AYAs. – coordinated care is needed across acute care providers as well as children and adult services. Transition – not just an outpatient phenomenon. • Acute admission is an opportunity for re-engagement with healthcare, if required. • Plans for use of ambulatory care and acute medical unit (AMU) admission should be part of the care plan. • Care plans and electronic patient records should be available to staff on both the emergency department and the AMU.
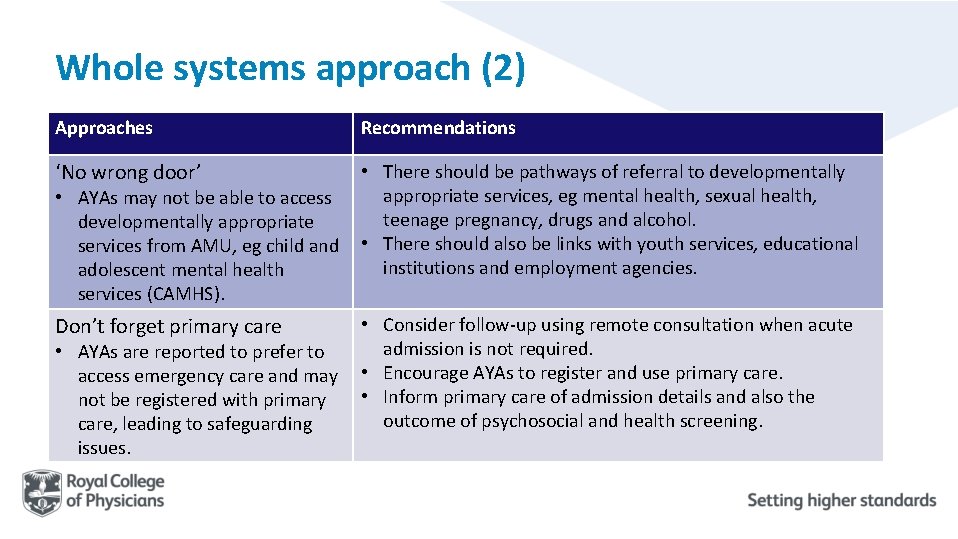
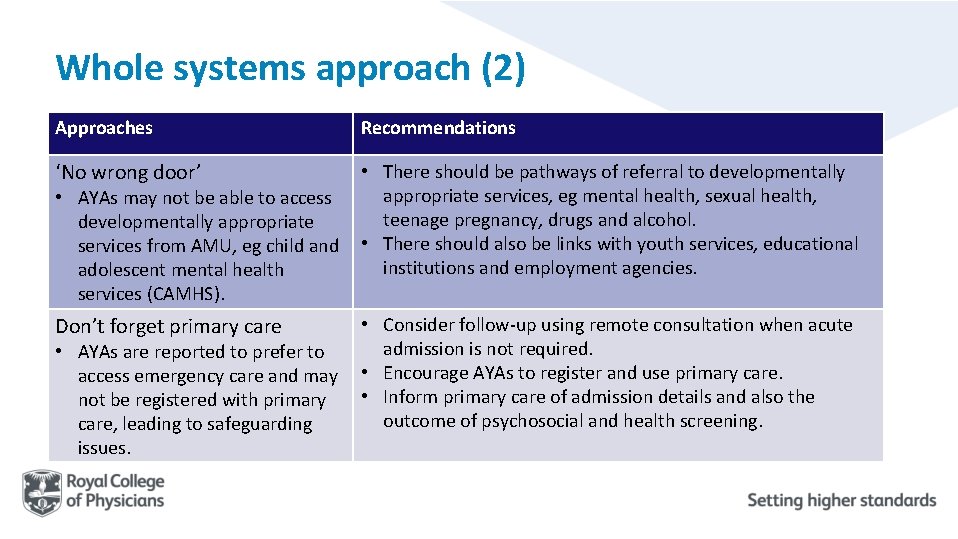
Whole systems approach (2) Approaches Recommendations ‘No wrong door’ • There should be pathways of referral to developmentally appropriate services, eg mental health, sexual health, teenage pregnancy, drugs and alcohol. • There should also be links with youth services, educational institutions and employment agencies. Don’t forget primary care • Consider follow-up using remote consultation when acute admission is not required. • Encourage AYAs to register and use primary care. • Inform primary care of admission details and also the outcome of psychosocial and health screening. • AYAs may not be able to access developmentally appropriate services from AMU, eg child and adolescent mental health services (CAMHS). • AYAs are reported to prefer to access emergency care and may not be registered with primary care, leading to safeguarding issues.
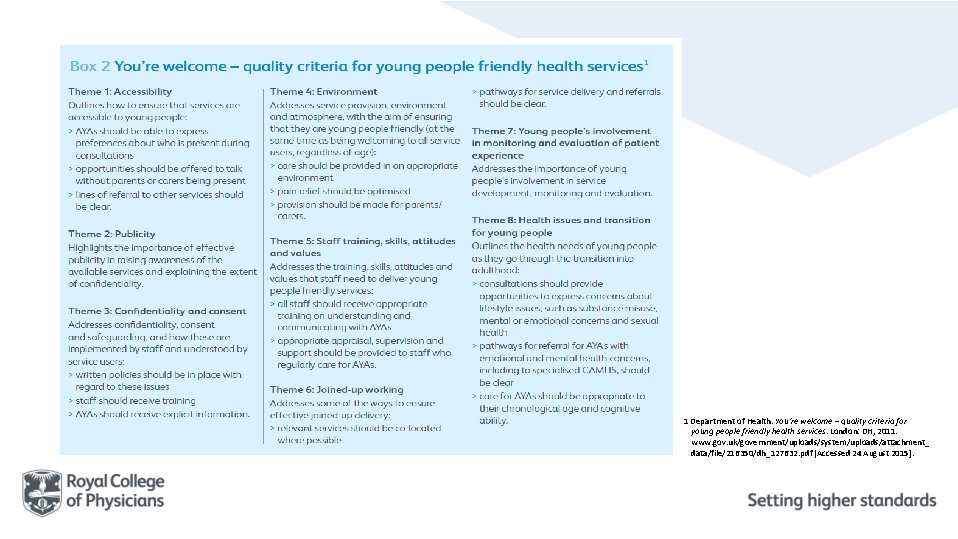
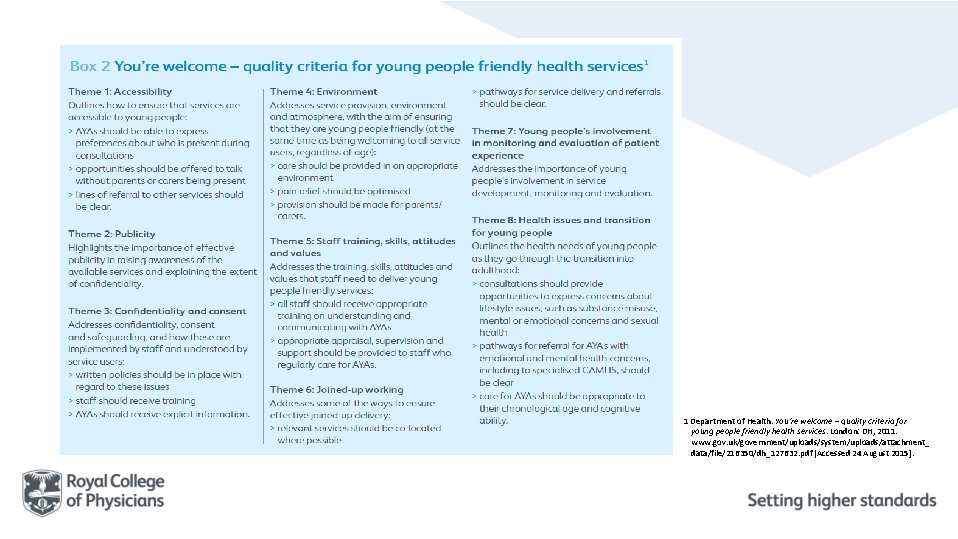
1 1 Department of Health. You’re welcome – quality criteria for young people friendly health services. London: DH, 2011. www. gov. uk/government/uploads/system/uploads/attachment_ data/file/216350/dh_127632. pdf [Accessed 24 August 2015].
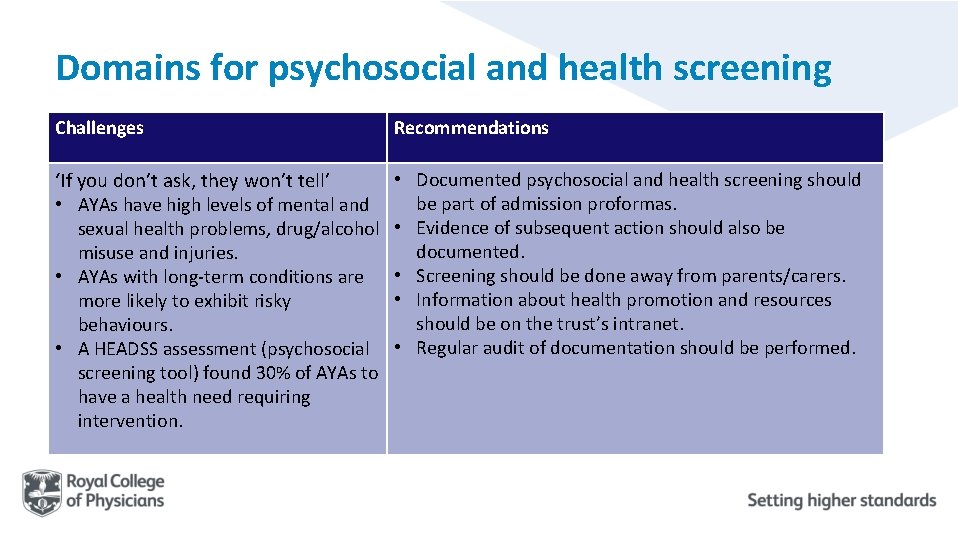
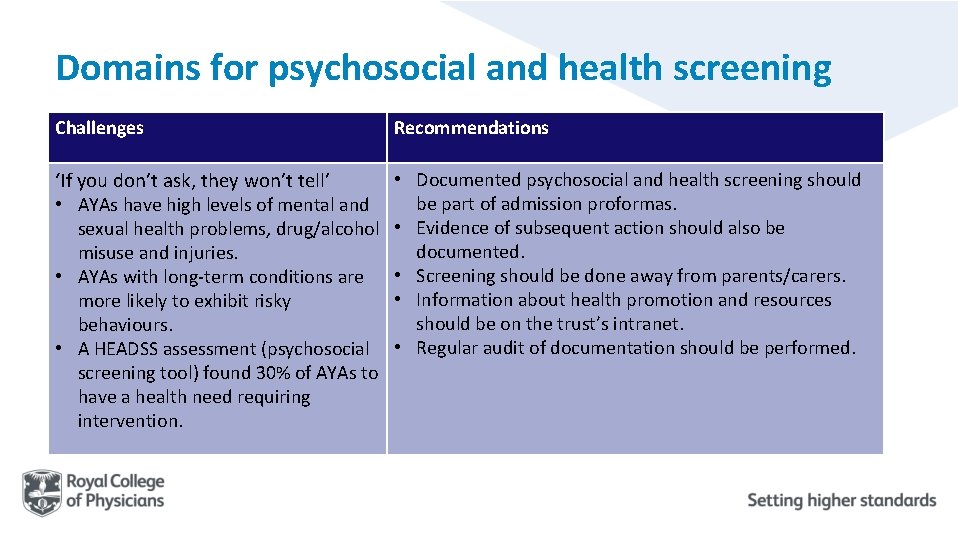
Domains for psychosocial and health screening Challenges Recommendations ‘If you don’t ask, they won’t tell’ • AYAs have high levels of mental and sexual health problems, drug/alcohol misuse and injuries. • AYAs with long-term conditions are more likely to exhibit risky behaviours. • A HEADSS assessment (psychosocial screening tool) found 30% of AYAs to have a health need requiring intervention. • Documented psychosocial and health screening should be part of admission proformas. • Evidence of subsequent action should also be documented. • Screening should be done away from parents/carers. • Information about health promotion and resources should be on the trust’s intranet. • Regular audit of documentation should be performed.
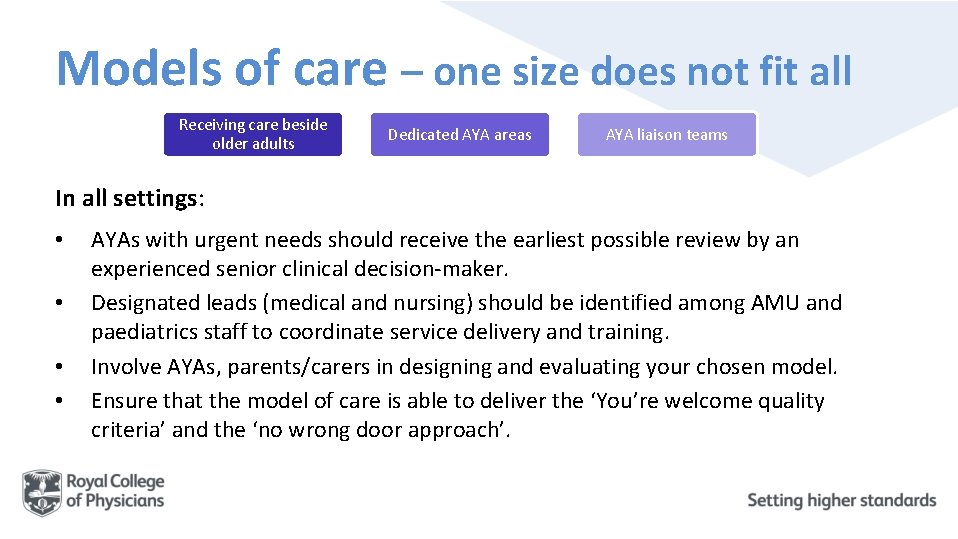
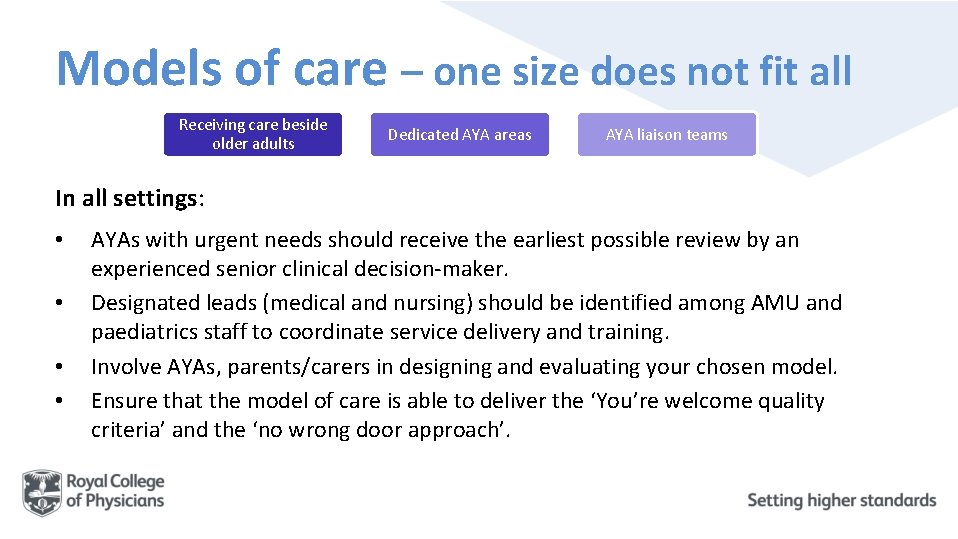
Models of care – one size does not fit all Receiving care beside older adults Dedicated AYA areas AYA liaison teams In all settings: • • AYAs with urgent needs should receive the earliest possible review by an experienced senior clinical decision-maker. Designated leads (medical and nursing) should be identified among AMU and paediatrics staff to coordinate service delivery and training. Involve AYAs, parents/carers in designing and evaluating your chosen model. Ensure that the model of care is able to deliver the ‘You’re welcome quality criteria’ and the ‘no wrong door approach’.
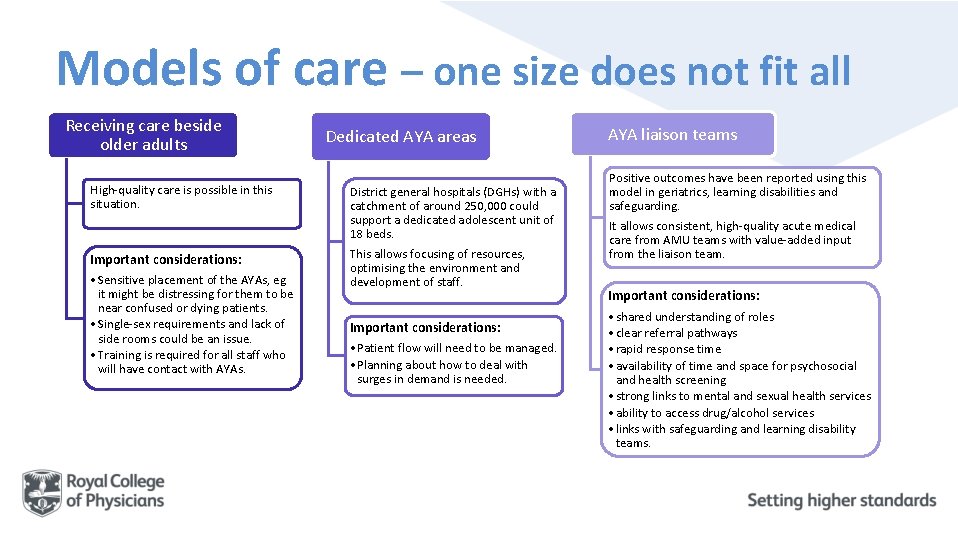
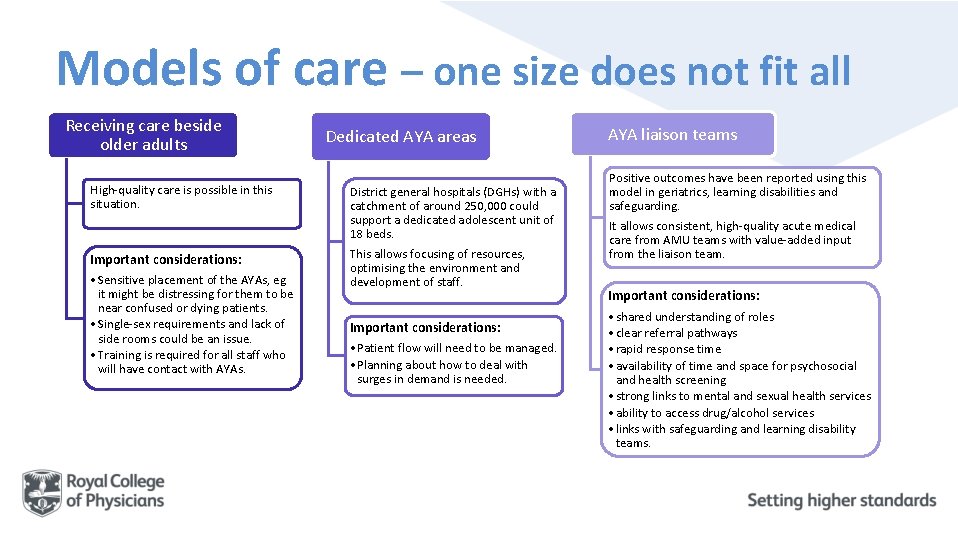
Models of care – one size does not fit all Receiving care beside older adults High-quality care is possible in this situation. Important considerations: • Sensitive placement of the AYAs, eg it might be distressing for them to be near confused or dying patients. • Single-sex requirements and lack of side rooms could be an issue. • Training is required for all staff who will have contact with AYAs. Dedicated AYA areas District general hospitals (DGHs) with a catchment of around 250, 000 could support a dedicated adolescent unit of 18 beds. This allows focusing of resources, optimising the environment and development of staff. Important considerations: • Patient flow will need to be managed. • Planning about how to deal with surges in demand is needed. AYA liaison teams Positive outcomes have been reported using this model in geriatrics, learning disabilities and safeguarding. It allows consistent, high-quality acute medical care from AMU teams with value-added input from the liaison team. Important considerations: • shared understanding of roles • clear referral pathways • rapid response time • availability of time and space for psychosocial and health screening • strong links to mental and sexual health services • ability to access drug/alcohol services • links with safeguarding and learning disability teams.
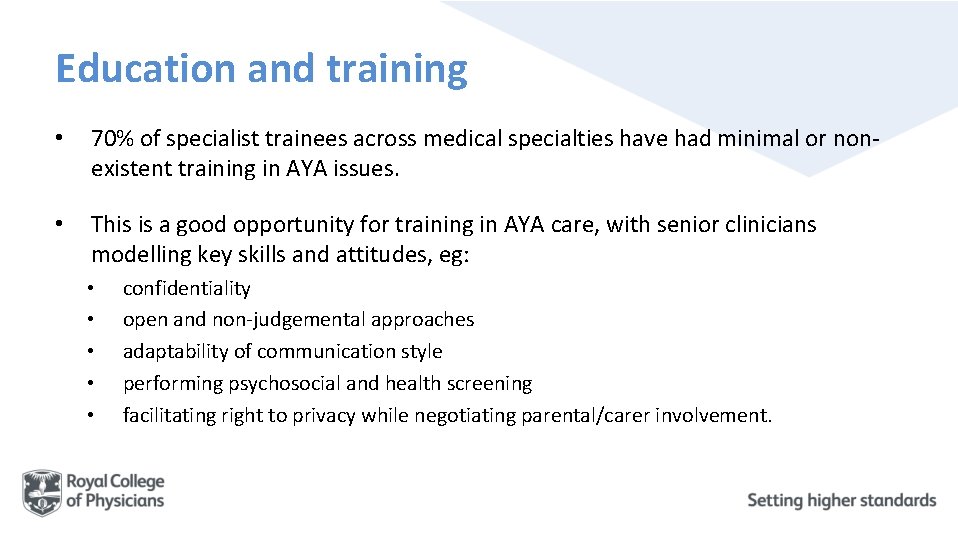
Education and training • 70% of specialist trainees across medical specialties have had minimal or nonexistent training in AYA issues. • This is a good opportunity for training in AYA care, with senior clinicians modelling key skills and attitudes, eg: • • • confidentiality open and non-judgemental approaches adaptability of communication style performing psychosocial and health screening facilitating right to privacy while negotiating parental/carer involvement.
Education and training: recommendations • All AMU staff caring for AYAs should have training on these key skills. • Training should be documented. • E-learning for Healthcare Adolescent Health Programme should be available (via the trust’s intranet) and signposted to all AMU staff.
The RCP produces a series of acute care toolkits on a range of topics including: • • handover teaching on the AMU acute oncology on the AMU ambulatory emergency care sepsis acute medical care for frail older people acute kidney injury. All the toolkits, including the full version of Acute care toolkit 13: Acute care for adolescents and young adults, can be accessed at: www. rcplondon. ac. uk/resources/acute-care-toolkits.

 Rcp acute care toolkit
Rcp acute care toolkit Lara berk
Lara berk What is the difference between courting and dating
What is the difference between courting and dating Discontinuity of development
Discontinuity of development Micmt
Micmt Primary secondary and tertiary health care
Primary secondary and tertiary health care Post-acute care collaboration
Post-acute care collaboration Hepatitis a incubation period
Hepatitis a incubation period Ledarskapsteorier
Ledarskapsteorier Offentlig förvaltning
Offentlig förvaltning Fredsgudinna
Fredsgudinna Datorkunskap för nybörjare
Datorkunskap för nybörjare Rita perspektiv
Rita perspektiv Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tillitsbaserad ledning
Tillitsbaserad ledning Kanaans land
Kanaans land Tack för att ni lyssnade bild
Tack för att ni lyssnade bild