Post Traumatic Stress Disorder PTSD Michael Coupland CPsych
![PTSD is diagnosed in 7%-12% of the general population exposed to a trauma[1], but PTSD is diagnosed in 7%-12% of the general population exposed to a trauma[1], but](https://slidetodoc.com/presentation_image/3d67aa5aa65e611bb29627804ef26dda/image-14.jpg)

- Slides: 19
Post Traumatic Stress Disorder (PTSD) Michael Coupland, CPsych, Rpsych, CRC INTEGRATED MEDICAL case solutions
INTEGRATED MEDICAL case solutions National Panel of Psychologists • • • Biopsychosocial Pain Evaluations Trauma and PTSD Evaluation and Treatment Functional Psychological Evaluations Opioid Assessment and Intervention Early Identification of Chronic Pain and Delayed Recovery Michael Coupland, CPsych, CRC Charter and Registered Psychologist (AB) specializing for 35 years in Occupational testing and measurement; Developer of the Assess. Ability Functional Evaluation (FME) system utilized in over 150, 000 functional evaluations Author: AMA text on Functional Evaluation / IAIABC Article Chronic pain Expert to the Federal Government Social Security Disability Determination projects; Police Fire and Aviation Crash Psychologist for 20 years
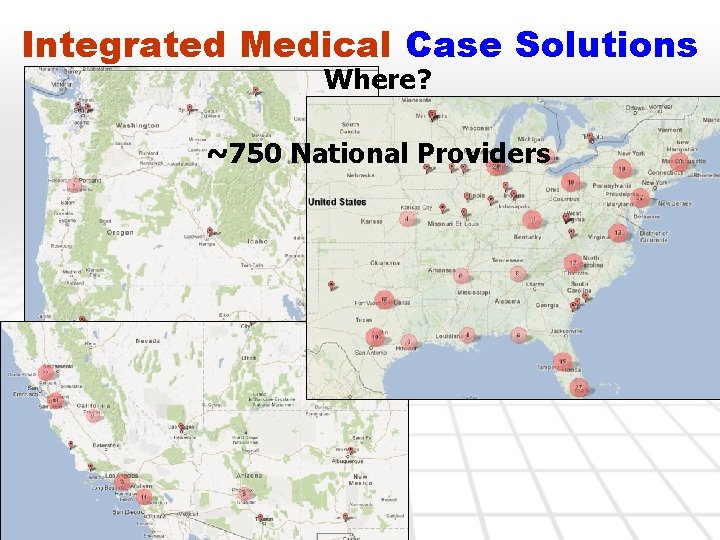
Integrated Medical Case Solutions Where? ~750 National Providers
Rapid Response to A Traumatic Event CISD • ~90% of all exposed recover and do not need further follow up • Of those that need follow up care, 50% recover within 8 -12 weeks of appropriate care • The delayed recovery cases likely are not receiving appropriate care or have preexisting and co-morbid issues prolonging and perpetuating symptoms
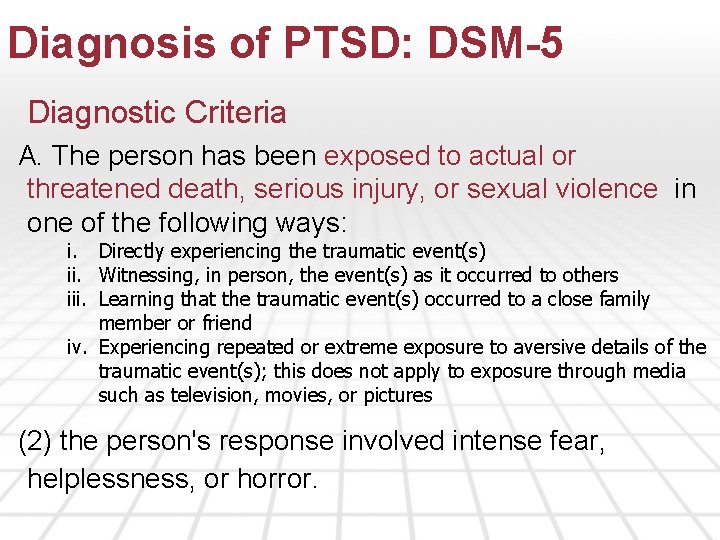
Diagnosis of PTSD: DSM-5 Diagnostic Criteria A. The person has been exposed to actual or threatened death, serious injury, or sexual violence in one of the following ways: i. Directly experiencing the traumatic event(s) ii. Witnessing, in person, the event(s) as it occurred to others iii. Learning that the traumatic event(s) occurred to a close family member or friend iv. Experiencing repeated or extreme exposure to aversive details of the traumatic event(s); this does not apply to exposure through media such as television, movies, or pictures (2) the person's response involved intense fear, helplessness, or horror.
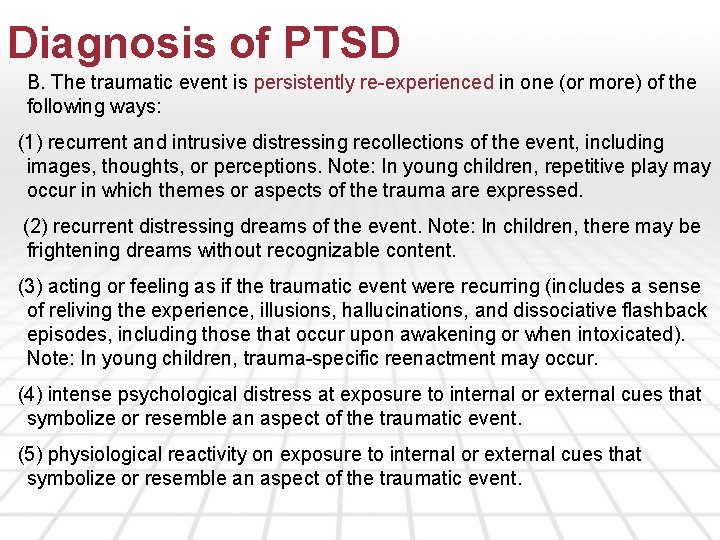
Diagnosis of PTSD B. The traumatic event is persistently re-experienced in one (or more) of the following ways: (1) recurrent and intrusive distressing recollections of the event, including images, thoughts, or perceptions. Note: In young children, repetitive play may occur in which themes or aspects of the trauma are expressed. (2) recurrent distressing dreams of the event. Note: In children, there may be frightening dreams without recognizable content. (3) acting or feeling as if the traumatic event were recurring (includes a sense of reliving the experience, illusions, hallucinations, and dissociative flashback episodes, including those that occur upon awakening or when intoxicated). Note: In young children, trauma-specific reenactment may occur. (4) intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event. (5) physiological reactivity on exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event.
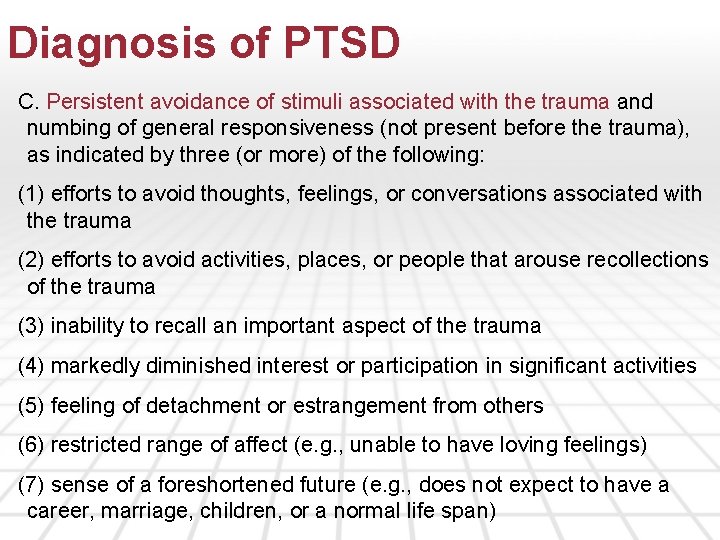
Diagnosis of PTSD C. Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by three (or more) of the following: (1) efforts to avoid thoughts, feelings, or conversations associated with the trauma (2) efforts to avoid activities, places, or people that arouse recollections of the trauma (3) inability to recall an important aspect of the trauma (4) markedly diminished interest or participation in significant activities (5) feeling of detachment or estrangement from others (6) restricted range of affect (e. g. , unable to have loving feelings) (7) sense of a foreshortened future (e. g. , does not expect to have a career, marriage, children, or a normal life span)
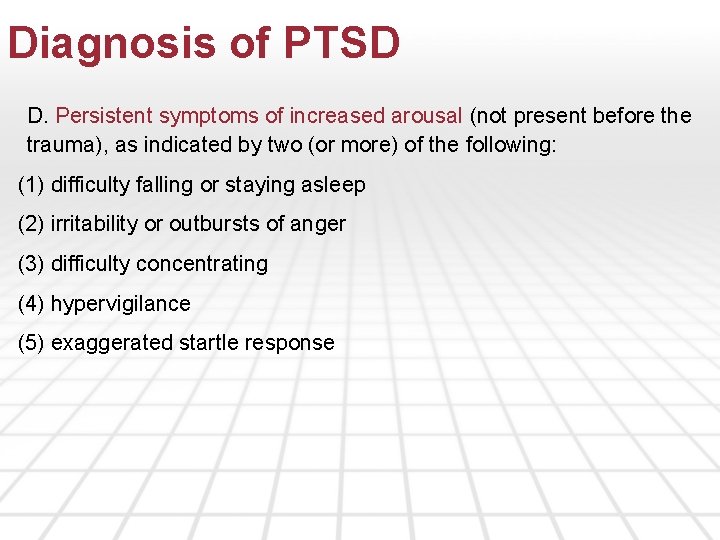
Diagnosis of PTSD D. Persistent symptoms of increased arousal (not present before the trauma), as indicated by two (or more) of the following: (1) difficulty falling or staying asleep (2) irritability or outbursts of anger (3) difficulty concentrating (4) hypervigilance (5) exaggerated startle response
Diagnosis of PTSD E. Duration of the disturbance (symptoms in Criteria B, C, and D) is more than one month. F. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Diagnosis of PTSD Differential Diagnoses and Rule-outs q. Acute stress disorder has the same symptoms as PSTD but with shorter duration. qother anxiety disorders, qdepressive disorders, qobsessive-compulsive disorder. q. Although substance abuse is a frequent complication of PTSD, substance abuse may be the primary problem instead. q. Alcoholics and heavy drug abusers often overemphasize the role of a distant trauma as the cause of their problems and use it to justify their habits. q. Various personality disorders can also resemble PTSD with borderline personality disorder having the closest resemblance to PTSD.
PTSD Causality Is the diagnosis causally related to the injury or accident? Is the treatment causally related to the injury or accident Is there a history or co-morbidities, prior injuries and/or pre-existing conditions that impact on the current injury or accident?
PTSD Causality The cause of PTSD is multifactorial. Some studies have presented a model that does suggest that exposure to trauma has a relationship. The classical conditioning model combined with operant learning lends credibility to the acquisition and persistence of fear[1]. A study of heart rate reactivity to audio reminders has reinforced this model[2]. Furthermore, Amnesia appears to protect against PTSD fears. [1] Kuch k, Evans RJ, Watson PC, Bubela C, Cox, BJ. Road vehicle accidents and phobia in 60 patients with fibromyalgia. Journal of Anxiety Disorders 1994; 8: 181 -7 [2] Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Gerardi RJ. The psychophysiology of motor vehicle accident related posttraumatic stress disorder. Behavior Therapy 1995; 25: 453 -67
PTSD Causality PTSD Dose Response studies: A dose response relationship between the severity of an MVA related trauma and the level of psychopathology has not been demonstrated[1], and the textbook on PTSD found no gradient between the severity of the trauma and the development of PTSD[2] [1] Mayou R, Bryant B, Duthie R. Psychiatric consequences of road traffic accidents. BMJ 1993; 307: 647 -51; O’Brien M. Loss of memory is protective [letter] BMJ 1993; 307: 1283 [2] Yehuda R, ed. Risk factors for posttraumatic stress disorder. Washington DC, American Psychiatric Press; 1999
![PTSD is diagnosed in 712 of the general population exposed to a trauma1 but PTSD is diagnosed in 7%-12% of the general population exposed to a trauma[1], but](https://slidetodoc.com/presentation_image/3d67aa5aa65e611bb29627804ef26dda/image-14.jpg)
PTSD is diagnosed in 7%-12% of the general population exposed to a trauma[1], but is found at a rate of 85% when an opportunity to claim compensation is present[2]. Outcomes vary greatly. Most individuals subjected to an experience outside the normal realm of human experience never become symptomatic. Complete recovery occurs within 3 months in about 50% of the cases of PTSD while others have symptoms lasting longer than 12 months after the trauma. Some individuals improve but when under a new stress may have a period of recurring PTSD symptoms. A subset of individuals with PTSD develop a lifelong illness marked by exacerbations and remissions that makes it extremely difficult to maintain employment or close relationships. Ø[1] Breslau N. The epidemiology of post-traumatic stress disorder: what is the extent of the problem? J Clin Psychiatry. 2001; 62(suppl 17): 16 -22 Ø[2] Rosen GM. The Aleutian Enterprise Sinking and posttraumatic stress disorder: misdiagnosis in clinical and forensic settings. Prof Psychol Res P. 1995; 26: 82 -87
Treatment for PTSD Best Practices q. PTSD has shown the best response when Cognitive Behavioral Therapy (CBT) is utilized. q. CBT utilizes principles of learning and conditioning to treat this disorder and includes components from both behavioral and cognitive therapy. q. Exposure/Desensitization is a treatment recognized as being effective in treating PTSD. Types of exposure therapy include imaginal exposure, which involves exposure to the traumatic event through mental imagery; and in vivo therapy, where a client confronts the actual scene or similar events that are associated with the trauma. [1] Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence; National Academy of Sciences; Fall 2007.
Treatment for PTSD Medications can be utilized in addition to CBT. Patient preference and involvement need to be considered as part of the decision to prescribe specific medications. The severity of symptoms should also be considered. Two selective serotonin reuptake inhibitors (SSRIs) have been approved by the FDA to treat PTSD; sertraline (Zoloft) and paroxetine (Paxil). SSRIs address all common symptom clusters of PTSD. Benzodiazepines (Valium and Klonopin) should be avoided “as there is no evidence they are beneficial in the treatment of chronic PTSD and [there is] some evidence that they can increase the likelihood of developing PTSD when prescribed in the acute aftermath of trauma exposure. ”[1] q[1] Care for Returning Service Members: Providing Mental Health Care for Military Service Members Returning from Iraq and Afghanistan; Christopher Erbes, et al; Minnesota Psychologist, November 2007. [1] Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence; National Academy of Sciences; Fall 2007.
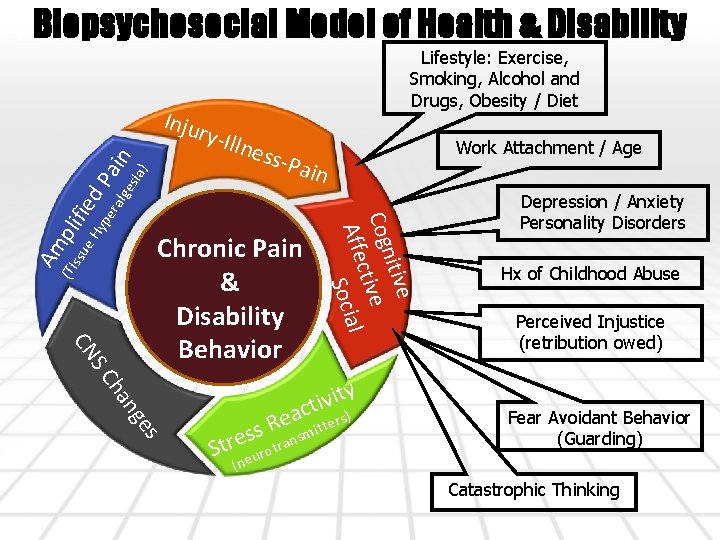
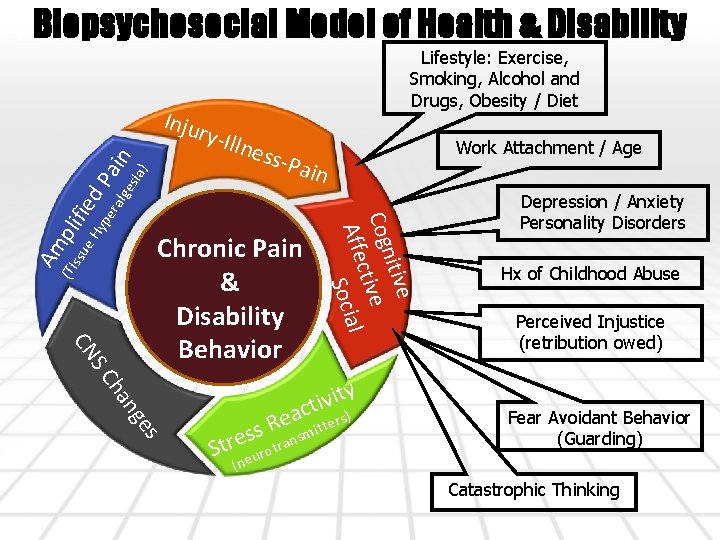
Biopsychosocial Model of Health & Disability Inju Lifestyle: Exercise, Smoking, Alcohol and Drugs, Obesity / Diet lnes in yp era lge s-Pa (Ti ssu Am Chronic Pain & Disability Behavior e nitiv Cog tive c Affe Social pli e H fied sia Pa ) in ry-Il ge n ha SC CN s y t i v i ct ers) a e s R itt s sm n e a r r St rot u (ne Work Attachment / Age Depression / Anxiety Personality Disorders Hx of Childhood Abuse Perceived Injustice (retribution owed) Fear Avoidant Behavior (Guarding) Catastrophic Thinking
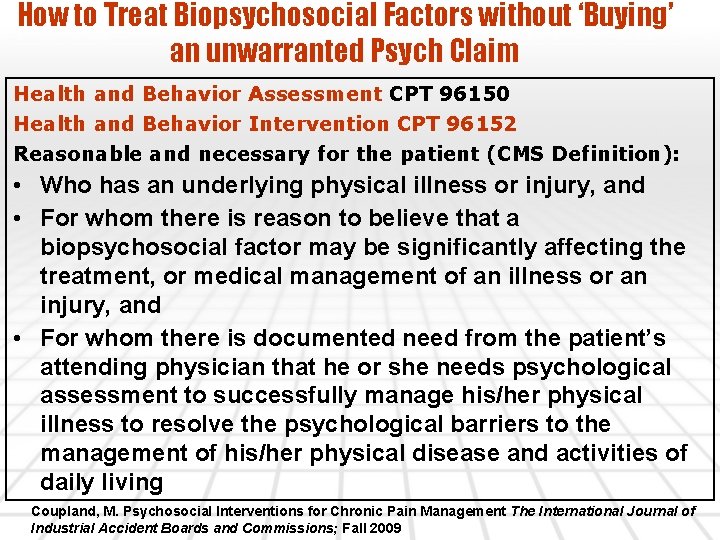
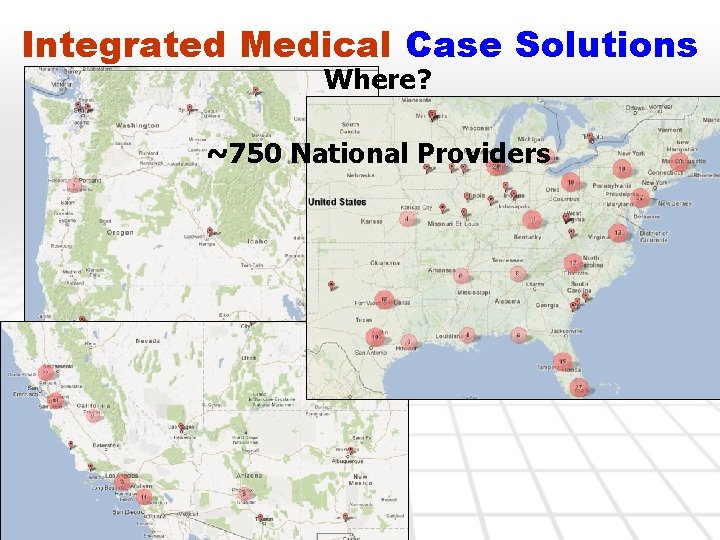
How to Treat Biopsychosocial Factors without ‘Buying’ an unwarranted Psych Claim Health and Behavior Assessment CPT 96150 Health and Behavior Intervention CPT 96152 Reasonable and necessary for the patient (CMS Definition): • Who has an underlying physical illness or injury, and • For whom there is reason to believe that a biopsychosocial factor may be significantly affecting the treatment, or medical management of an illness or an injury, and • For whom there is documented need from the patient’s attending physician that he or she needs psychological assessment to successfully manage his/her physical illness to resolve the psychological barriers to the management of his/her physical disease and activities of daily living Coupland, M. Psychosocial Interventions for Chronic Pain Management The International Journal of Industrial Accident Boards and Commissions; Fall 2009

Questions? www. imcs. us (866) 678 -2924
 Post traumatic stress disorder
Post traumatic stress disorder Complex ptsd
Complex ptsd Diagnosis of post traumatic stress disorder
Diagnosis of post traumatic stress disorder Post traumatic cervical dystonia
Post traumatic cervical dystonia Post trumatic stress disorder
Post trumatic stress disorder Factitious disorder vs somatic symptom disorder
Factitious disorder vs somatic symptom disorder Lever principle of elevators
Lever principle of elevators Howell v coupland
Howell v coupland Coupland elevator principle
Coupland elevator principle Traumatic overbite
Traumatic overbite Basal skull fracture
Basal skull fracture Csf traumatic tap
Csf traumatic tap Traumatic brain injury concept map
Traumatic brain injury concept map Traumatic insemination
Traumatic insemination Hyponuria
Hyponuria Traumatic brain injury concept map
Traumatic brain injury concept map Tbi long term servival after traumatic
Tbi long term servival after traumatic Edh vs sdh
Edh vs sdh Psykoedukation ptsd
Psykoedukation ptsd Ptsd model ehlers and clark
Ptsd model ehlers and clark