Psychotherapy Post Traumatic Stress Disorder Psychotherapy Trauma Aims






- Slides: 53
Psychotherapy Post Traumatic Stress Disorder
Psychotherapy: Trauma Aims of session: • Review the risk factors for developing PTSD • Summary of NICE Guidelines on PTSD • Psychological therapies for PTSD • Summary of research on outcomes of therapy
Psychotherapy: Trauma To achieve this • • • Case Presentation Journal Club 555 Presentation Expert-Led Session MCQs • Please sign the register and complete the feedback
Psychotherapy: Trauma Expert Led Session Psychological Approaches to Trauma Author: Dr. Rachel Jukes Consultant Psychiatrist in Psychotherapy
What is a psychological Trauma? “There is an interval…. . of suspended animation, a kind of psychological shock or paralysis. It is caused by a traumatic or sub-traumatic experience which explodes, as it were, the world that is familiar to the person as well as his image of himself (sic) within that world. ”
Historical descriptions of PTSD • Galen, father of Greek medicine, described trauma symptoms among soldiers in the Peloponnesian wars • 1862 American Civil War = “Soldier’s heart” • 1891 Boer War = “Disordered action of the heart” (DAH) • WW 1 = “Shell shock” • WW 2 = “Battle fatigue” or “Lack of moral fibre” LMF

Historical descriptions of PTSD • • • 1950 Korean War = “Old Sergeant syndrome” 1972 “Buffalo Creek syndrome” in USA 1979 Vietnam War = PTSD 1982 Falklands/ Malvinas War = “Battleshock” 1993 = “Gulf War syndrome” 1993 ICD-10 WHO defined clinical criteria for diagnosis of PTSD
Most common disorders after a trauma • • • Depression Substance misuse Acute stress reaction Panic disorder Personality change 80% Comorbidity is expected , unusual to have only one disorder in isolation • Don’t miss physical health problems
PTSD • PTSD is a neuro physiological disorder which arises out of impact on; • hypothalamic-pituitary axis • Hippocampal volume • Endogenous opioid function
PTSD Diagnosis • 6 Criteria ICD-10 (1993) WHO, • Person is exposed to traumatic event or events that involve actual or threatened death or serious injury. Response involves intense fear, helplessness or horror • Intrusion - event is relived by the person • Avoidance - stimuli associated with the event are avoided • Physical - persistent physical symptoms of arousal or hypervigilance • Social – disruption in social, occupational or other areas of functioning • Time – above symptoms last longer than 1 month
Traumatic memories • • Prevalence of traumatic exposure is underestimated Traumatic memories are far more prevalent than PTSD Leave a significant minority hyper-reactive to cues Traumatic preoccupation and orientation remains but link to arousal and avoidance is not recognized particularly in simple phobia • Risk of further activation • Marker of general risk for psychopathology • Clinically seldom documented
Types of Trauma • Recent Single Event • • • Acute Stress reaction (dissociative and hypervigilant qualities often prominent) PTSD Acute (hypervigilant and avoidant qualities often prominent) PTSD Chronic ( symptoms after 3 months) • Complex Acute PTSD • Other co-existing psychological or physical problems • Complex Chronic PTSD/Trauma • Delayed PTSD

Differential Diagnosis • • • Medical condition eg brain injury Substance induced condition Dissociative disorder Depression Borderline personality disorder Malingering
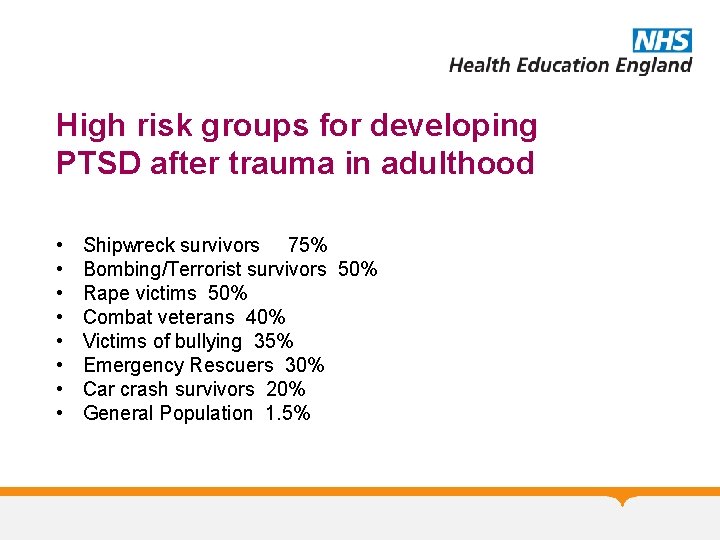
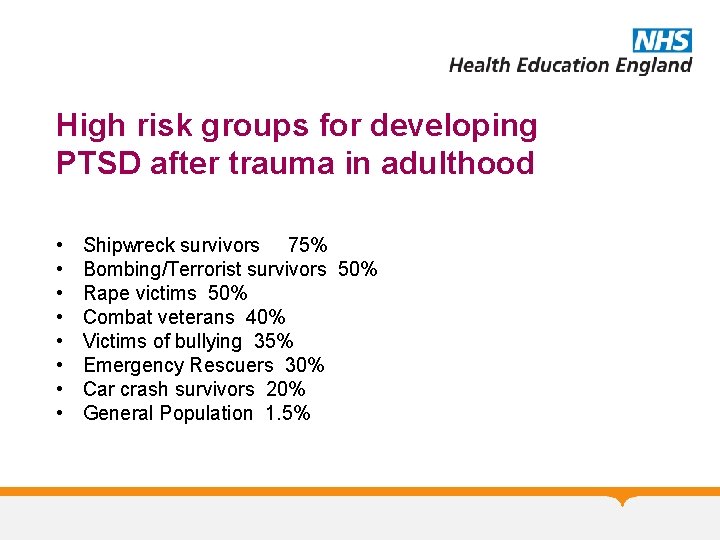
High risk groups for developing PTSD after trauma in adulthood • • Shipwreck survivors 75% Bombing/Terrorist survivors 50% Rape victims 50% Combat veterans 40% Victims of bullying 35% Emergency Rescuers 30% Car crash survivors 20% General Population 1. 5%

Higher risk of exposure to traumatic event • • • Male Lower educational achievement Extroversion Neuroticism Early conduct disorder Family psychiatric history

Higher risk of developing PTSD • • • Female Neuroticism Early separation from parents Previous depression and anxiety Family history of antisocial PD
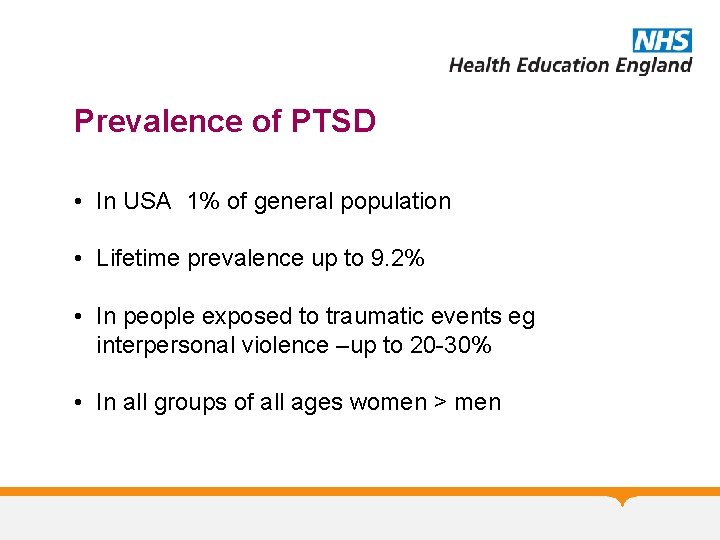
Prevalence of PTSD • In USA 1% of general population • Lifetime prevalence up to 9. 2% • In people exposed to traumatic events eg interpersonal violence –up to 20 -30% • In all groups of all ages women > men
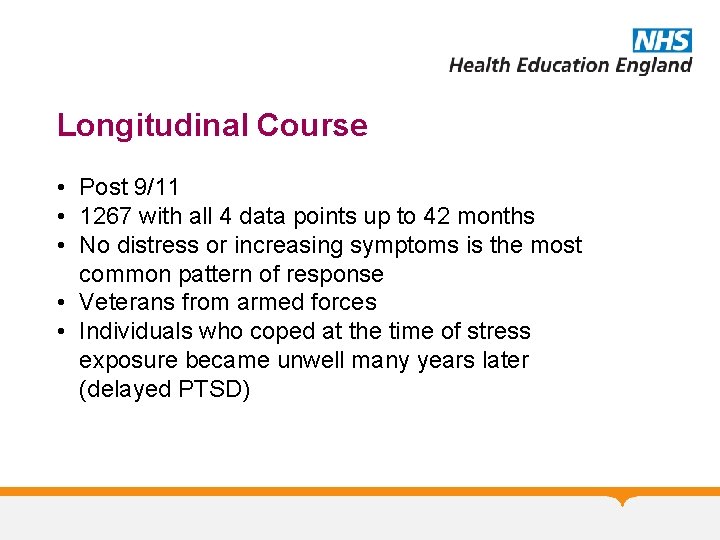
Longitudinal Course • Post 9/11 • 1267 with all 4 data points up to 42 months • No distress or increasing symptoms is the most common pattern of response • Veterans from armed forces • Individuals who coped at the time of stress exposure became unwell many years later (delayed PTSD)
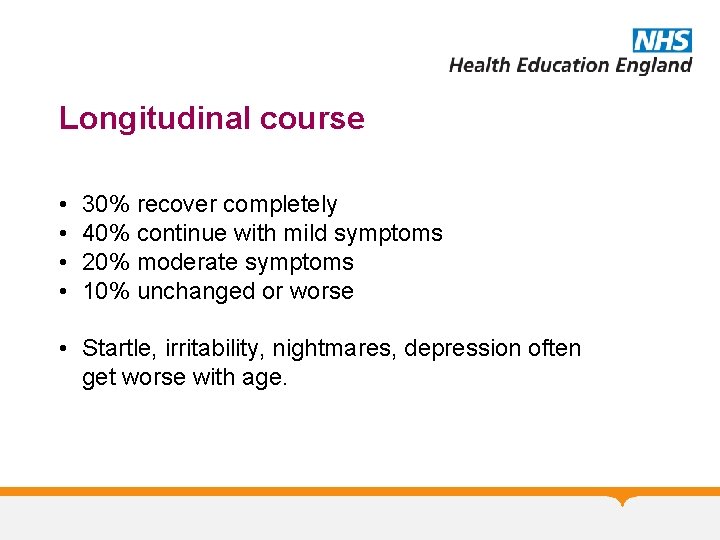
Longitudinal course • • 30% recover completely 40% continue with mild symptoms 20% moderate symptoms 10% unchanged or worse • Startle, irritability, nightmares, depression often get worse with age.
Trauma in childhood affects everything… • • Developmental milestones Attachment Intellectual capacity Cognitive ability Affect regulation Interpersonal functioning Mental health Immune/Autoimmune system
Risk factors for developing PTSD • Early experiences leave a chemical “signature” on genes that determines whether and how the genes are turned on or off i. e. “epigenetic adaptation, ” • It shapes neurological, emotional, immunological and physical development • High risk of poor physical and psychological health in adulthood
NICE Guidelines for PTSD (2005 & revised 2018) • For individuals who have experienced a traumatic event, the systematic provision to that individual alone of a brief, single-session interventions( debriefing) that focuses on the traumatic incident, should not be routine practice. • For mild symptoms present for less than 4 weeks after the trauma, employ watchful waiting with a follow-up contact should be arranged within 1 month.
NICE Guidelines for PTSD (2005 /18) • Individual Trauma-focused cognitive behavioural therapy should be offered for severe post-traumatic symptoms or with severe PTSD in the first month after the traumatic event. • All people with PTSD should be offered a course of traumafocused psychological treatment (trauma-focused cognitive behavioural therapy [CBT] or eye movement desensitisation and reprocessing [EMDR]). • These treatments should normally be provided on an individual outpatient basis.
NICE Guidelines for PTSD (2005 /18) • Drug treatments for PTSD should not be used as a routine first -line treatment for adults (in general use or by specialist mental health professionals) in preference to a trauma-focused psychological therapy. • Drug treatments (paroxetine or mirtazapine for general use, and amitriptyline or phenelzine for initiation only by mental health specialists) should be considered for the treatment of PTSD in adults who express a preference not to engage in trauma-focused psychological treatment[1].
Psychological Interventions • Exposure Therapy- Education about common reactions to trauma, breathing retraining, and repeated exposure to the past trauma in graduated doses. The goal is for the traumatic event to be remembered without anxiety or panic resulting. • Cognitive Therapy- Separating the intrusive thoughts from the associated anxiety that they produce. • Stress inoculation training- variant of exposure training teaches client to relax. Helps the client relax when thinking about traumatic event exposure by providing client a script.
Psychological Interventions • EMDR • Psychodynamic Therapy
Exposure Therapy • Prolonged Exposure usually involves 8 -15 weekly sessions (so treatment lasts about 3 months), • When people are fearful of something, they tend to avoid the feared objects, activities or situations. Although this avoidance might help reduce feelings of fear in the short term, over the long term it can make the fear become even worse. In such situations, a psychologist might recommend a program of exposure therapy in order to help break the pattern of avoidance and fear. • create a safe environment in which to “expose” individuals to the things they fear and avoid. The exposure to the feared objects, activities or situations in a safe environment helps reduce fear and decrease avoidance.
Exposure Therapy • In vivo exposure • Imaginal exposure • Virtual reality exposure • Interoceptive exposure
Trauma Focussed CBT • 12 -20 individual or group sessions as outpatient • Identify and modify excessively negative cognitions (thoughts and beliefs) that lead to disturbing emotions and impaired functioning. • Focus on identification and modification of misinterpretations that lead the patient to overestimate threat arising out of trauma and its aftermath • Maybe strong guilt or shame related to the trauma • May overestimate current danger they are encountering in everyday life. Accident survivors may become convinced that they are at great risk of having a further accident. • May interpret intrusive re-experiencing symptoms eg flashbacks as a sign that they are going mad or have no control.
Trauma Focussed CBT • Discussing the evidence for and against the interpretations, • Testing out the predictions (behavioural experiments) derived from the interpretations with the help of therapist, the patient arrives at more adaptive conclusions. • The patient is encouraged to drop behaviours and cognitive strategies that prevent a disconfirmation of the negative interpretations, e. g. excessive precautions to prevent further trauma or excessive rumination about what one could have done differently during the event. • nearly all trauma-focused CBT treatments that include cognitive therapy use some form of exposure (e. g. narrative writing, imaginal exposure) to access problematic meanings.
Eye Movement Desensitisation and Reprocessing (EMDR) • Patient attends to emotionally disturbing material in brief sequential doses while simultaneously focusing on an external stimulus. • Most commonly used external stimuli are Therapist directed lateral eye movements but also hand-tapping and audio stimulation. • Hypothesised that facilitates access to traumatic memory network to enhance information processing, making new associations between the traumatic memory and more adaptive memories or information • Results in new learning, elimination of emotional distress, and development of cognitive insights.
EMDR • Phase 1: History taking, initial focus may be on past distressing events • Phase 2: May teach stress reduction techniques and imagery to manage distress during and between sessions • Phase 3 to 6: Target identified and processed involving • 1. The vivid visual image related to the memory 2. A negative belief about self 3. Related emotions and body sensations. • 4. A positive belief about themselves
EMDR • Phase 7 and 8 work to identify new targets, consolidate progress and closure • Not good evidence that eye movements are necessary for good outcomes
Psychodynamic Psychotherapy • Some aspects of the traumatic experience are not integrated and experienced as flashbacks and in changed way of relating interpersonally to others. • Flashbacks, anxiety, irritability etc. forms of affective dysregulation • The Trauma will be emotionally linked to previous traumatic experiences • All trauma results in loss which maybe more or less aware of • PTSD arises out of inability to process loss due to intensity/severity of trauma or problems with mourning
Outcomes • CBT and EMDR similar outcomes -more than half improve • Most have residual symptoms • Psychoeducation and non specific factors account for 30% of the effect • Nonspecific factors are more important than acknowledged by the advocates of each for of treatment • High rates of dropouts (approx. 25%) • Possible loss of effectiveness with time • Need more effective treatments • Bradley et al 2005 Am J Psychiatry • Benish, Imel and Wampold 2008 Clin Psych Review
Complex Post Traumatic Stress Disorder • Complex PTSD is typically the result of exposure to repeated or prolonged instances or multiple forms of interpersonal trauma, often occurring under circumstances where escape is not possible due to physical, psychological, maturational, family/environmental, or social constraints (Herman, 1992). • Childhood physical and sexual abuse, • Recruitment into armed conflict as a child, • Being a victim of domestic violence, sex trafficking or slave trade; experiencing torture, and exposure to genocide campaigns or other forms of organized violence.
Complex PTSD • The ISTSS task force definition of Complex PTSD includes the core symptoms of PTSD (reexperiencing, avoidance/numbing, and hyper-arousal) and disturbance in the following areas • Emotional Regulation. May include persistent sadness, suicidal thoughts, explosive anger, or inhibited anger. • Consciousness. Includes forgetting traumatic events, reliving traumatic events, or having episodes in which one feels detached from one's mental processes or body (dissociation). • Self-Perception. May include helplessness, shame, guilt, stigma, and a sense of being completely different from other human beings.
Complex PTSD • Distorted Perceptions of the Perpetrator. Examples include attributing total power to the perpetrator, becoming preoccupied with the relationship to the perpetrator, or preoccupied with revenge. • Relations with Others. Examples include isolation, distrust, or a repeated search for a rescuer. • One's System of Meanings. May include a loss of sustaining faith or a sense of hopelessness and despair. • Somatic distress or disorganisation

Treatment of Complex PTSD • 3 Phased treatment; • Phase 1; • focuses on ensuring the individual’s safety, reducing symptoms, and increasing important emotional, social and psychological competencies. • Focus on stability; housing, diet, sleep, routine, self care etc. • CMHT care coordination, anxiety/stress management • Behavioural interventions eg. Structured clinical management, distress tolerance, grounding techniques, DBT, medication
Treatment of Complex PTSD • Phase 2; • focuses on processing the unresolved aspects of the individual’s memories of traumatic experiences. This phase emphasizes the review and re-appraisal of traumatic memories so that they are integrated into an adaptive representation of self, relationships and the world. • Trauma focused CBT • EMDR • Exposure therapy • Psychodynamic therapy
Treatment Complex PTSD • Phase 3; • Involves consolidation of treatment gains to facilitate the transition from the end of the treatment to greater engagement in relationships, work or education, and community life.
Outcomes • Lack of research • Complicated clinical presentation – outcome depends on many factors. • Critical is ability to engage in a sufficiently trusting relationship…. .
Psychotherapy: Trauma MCQs 1. The following treatments are indicated in PTSD: A. B. C. D. E. EMDR Debriefing Psychoanalysis Schema Focused CBT Psychodynamic Psychotherapy
Psychotherapy: Trauma MCQs 1. The following treatments are indicated in PTSD: A. B. C. D. E. EMDR Debriefing Psychoanalysis Schema Focused CBT Psychodynamic Psychotherapy
Psychotherapy: Trauma MCQs 2. The following are risk factors for an increased likelihood of PTSD: A. Male gender. B. Introverted character. C. Family history of Narcissistic Personality Disorder. D. Bereavement. E. Low educational attainment.
Psychotherapy: Trauma MCQs 2. The following are risk factors for an increased likelihood of PTSD: A. Male gender. B. Introverted character. C. Family history of Narcissistic Personality Disorder. D. Bereavement. E. Low educational attainment.
Psychotherapy: Trauma MCQs 3. The following are part of the six diagnostic criteria for PTSD in ICD-10: A. Exposure to any sort of trauma. B. Occasional memories of the traumatic event. C. Avoidance of situations that remind the person of the trauma. D. Normal social functioning. E. Symptoms of at least one week duration.

Psychotherapy: Trauma MCQs 3. The following are part of the six diagnostic criteria for PTSD in ICD-10: A. Exposure to any sort of trauma. B. Occasional memories of the traumatic event. C. Avoidance of situations that remind the person of the trauma. D. Normal social functioning. E. Symptoms of at least one week duration.
Psychotherapy: Trauma MCQs 4. The following have been used in military circles as terms for what we now would call PTSD: A. B. C. D. E. Shell Shock Lack of Moral Fibre Vietnam War Syndrome Old Soldier’s Syndrome Battle Paralysis
Psychotherapy: Trauma MCQs 4. The following have been used in military circles as terms for what we now would call PTSD: A. B. C. D. E. Shell Shock Lack of Moral Fibre Vietnam War Syndrome Old Soldier’s Syndrome Battle Paralysis
Psychotherapy: Trauma MCQs 5. The following statements are true of PTSD: A. Comorbidity is unusual B. There are detectable effects on the hypothalamopituitary axis C. “flashbacks’ or intrusive memories of the trauma are characteristic D. Endogenous opioids function is affected in PTSD E. Soldiers are at less risk of PTSD than rape victims
Psychotherapy: Trauma MCQs 5. The following statements are true of PTSD: A. Comorbidity is unusual B. There are detectable effects on the hypothalamopituitary axis C. “flashbacks’ or intrusive memories of the trauma are characteristic D. Endogenous opioids function is affected in PTSD E. Soldiers are at less risk of PTSD than rape victims
Psychotherapy: Trauma Any Questions? Thank you.
 Acute stress disorder diagnosis
Acute stress disorder diagnosis Post traumatic stress disorder
Post traumatic stress disorder C ptsd
C ptsd Post traumatic cervical dystonia
Post traumatic cervical dystonia Post trumatic stress disorder
Post trumatic stress disorder Somatic vs factitious
Somatic vs factitious Traumatic insemination
Traumatic insemination Csf traumatic tap
Csf traumatic tap Traumatic brain injury concept map
Traumatic brain injury concept map Hyponuria
Hyponuria Edh sdh sah
Edh sdh sah Traumatic overbite
Traumatic overbite Tbi long term servival after traumatic
Tbi long term servival after traumatic Raccoon
Raccoon Traumatic brain injury concept map
Traumatic brain injury concept map Define axial stress
Define axial stress Chapter 10 stress responses and stress management
Chapter 10 stress responses and stress management True fracture strain
True fracture strain Cognitive psychology ppt
Cognitive psychology ppt Limitations of psychotherapy
Limitations of psychotherapy Rogerian psychotherapy
Rogerian psychotherapy Definitions of counselling
Definitions of counselling Eclectic therapy psychology example
Eclectic therapy psychology example Fah nicol
Fah nicol Padesky 5 aspects. 1986
Padesky 5 aspects. 1986 What is ethical bracketing
What is ethical bracketing College of registered psychotherapists of ontario
College of registered psychotherapists of ontario Quantum psychotherapy
Quantum psychotherapy Psychotherapy refers to
Psychotherapy refers to Re-educative individual psychotherapy
Re-educative individual psychotherapy Advanced psychotherapy
Advanced psychotherapy Dodo bird verdict psychology
Dodo bird verdict psychology 2 difference between guidance and counselling
2 difference between guidance and counselling Transference meaning psychology
Transference meaning psychology Imaginal disputation
Imaginal disputation Sadaf sajjad
Sadaf sajjad Cpp triangle of explanation
Cpp triangle of explanation Psychotherapy examples
Psychotherapy examples General issues in psychotherapy
General issues in psychotherapy Andrew pethebridge
Andrew pethebridge Counselling psychology doctorate
Counselling psychology doctorate The common factors approach to psychotherapy integration:
The common factors approach to psychotherapy integration: Trauma institut mainz
Trauma institut mainz Family trauma
Family trauma Pasg trauma
Pasg trauma Trauma vicario definición
Trauma vicario definición Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Tibia fracture ao
Tibia fracture ao Kampala trauma score
Kampala trauma score Kampala trauma score
Kampala trauma score Trauma timeline template
Trauma timeline template Facial trauma
Facial trauma Dr ray padilla
Dr ray padilla Trauma dumping examples
Trauma dumping examples