Acute Kidney Injury AKI WHAT IS ACUTE KIDNEY

- Slides: 16
Acute Kidney Injury (AKI)
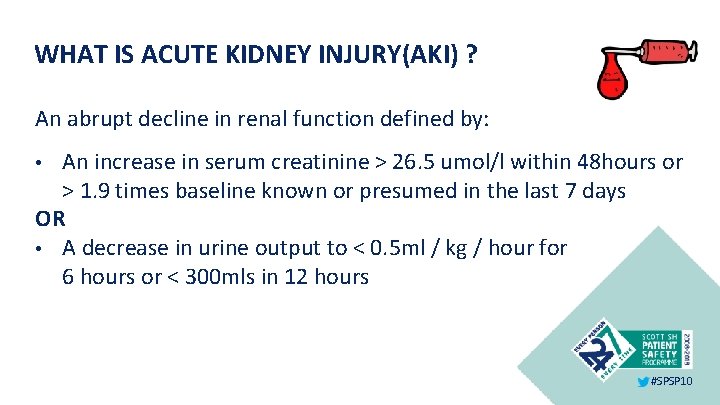
WHAT IS ACUTE KIDNEY INJURY(AKI) ? An abrupt decline in renal function defined by: An increase in serum creatinine > 26. 5 umol/l within 48 hours or > 1. 9 times baseline known or presumed in the last 7 days OR • A decrease in urine output to < 0. 5 ml / kg / hour for 6 hours or < 300 mls in 12 hours • #SPSP 10
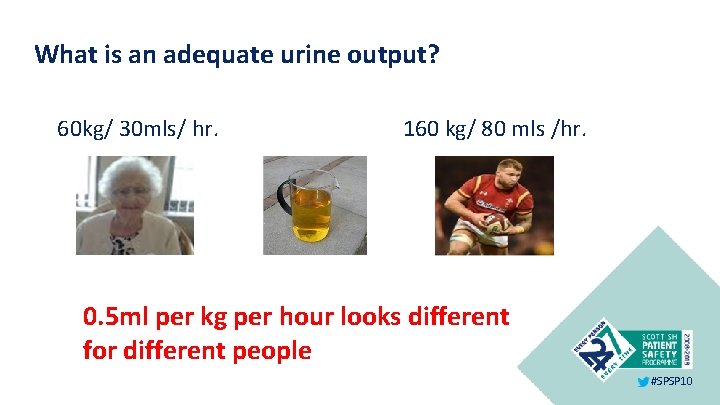
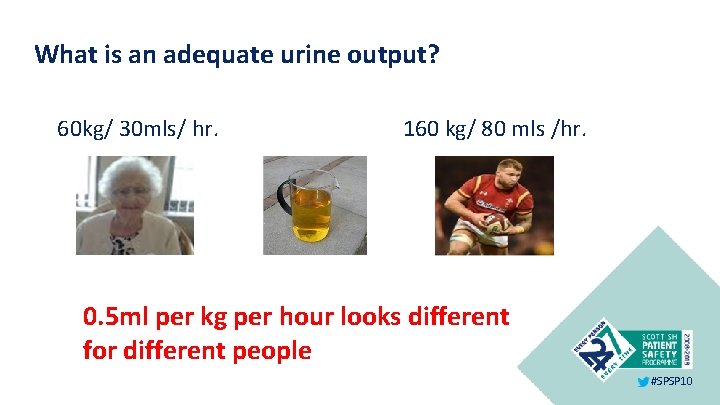
What is an adequate urine output? 60 kg/ 30 mls/ hr. 160 kg/ 80 mls /hr. 0. 5 ml per kg per hour looks different for different people #SPSP 10
Morbidity and mortality from AKI • AKI is associated with high mortality and adverse long-term outcomes and its prevalence in inpatients is believed to be rising. The NCEPOD report indicates that AKI risk factors are often not addressed and that a significant proportion of cases may be avoidable (NCEPOD 2009). • Mortality ranges from 10 – 80% Renal Association (8 th March 2011) #SPSP 10
Uncomplicated AKI has a 10% mortality rate More than 20% of patients with an AKI will die rising to > 35% in those with AKI stage 3 (Think Kidneys) #SPSP 10
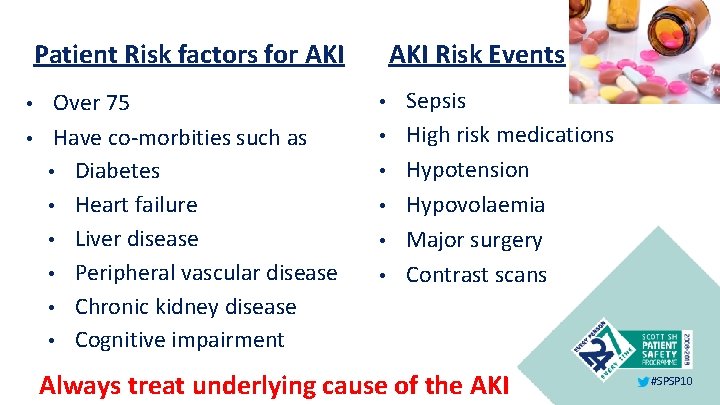
Patient Risk factors for AKI • • Over 75 Have co-morbities such as • Diabetes • Heart failure • Liver disease • Peripheral vascular disease • Chronic kidney disease • Cognitive impairment AKI Risk Events • • • Sepsis High risk medications Hypotension Hypovolaemia Major surgery Contrast scans Always treat underlying cause of the AKI #SPSP 10
Signs and symptoms of AKI • • • Evidence of dehydration Reduced urine output Changes to urine colour Nausea and vomiting Thirst Confusion or drowsiness #SPSP 10
What can we do to: prevent, recognise and respond to an AKI Prevent Identify people at high risk of AKI Improved management of fluid prescription and fluid balance Reduce risk from medications Recognise IT solutions – algorithm and e-alerts Early recognition of deteriorating patients #SPSP 10
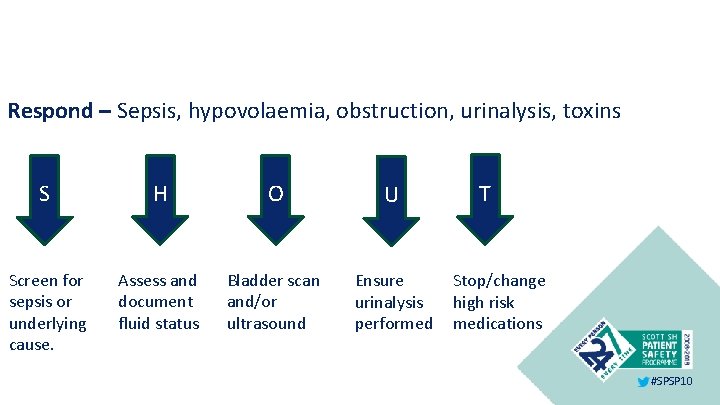
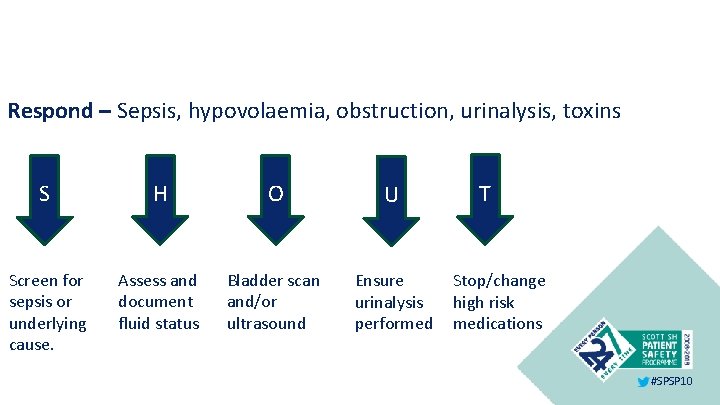
Respond – Sepsis, hypovolaemia, obstruction, urinalysis, toxins S H O U Screen for sepsis or underlying cause. Assess and document fluid status Bladder scan and/or ultrasound Ensure urinalysis performed T Stop/change high risk medications #SPSP 10
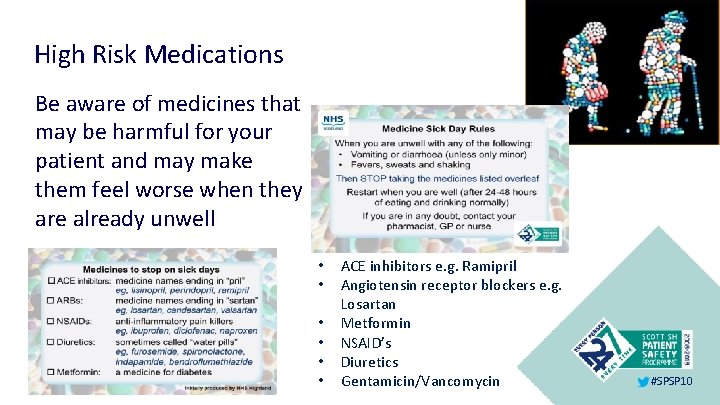
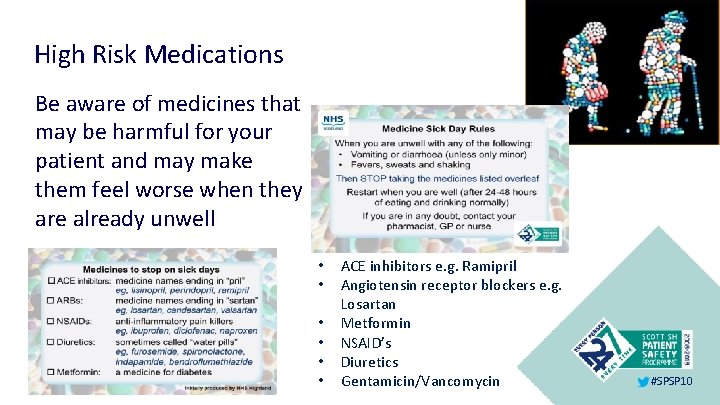
High Risk Medications Be aware of medicines that may be harmful for your patient and may make them feel worse when they are already unwell • • • ACE inhibitors e. g. Ramipril Angiotensin receptor blockers e. g. Losartan Metformin NSAID’s Diuretics Gentamicin/Vancomycin #SPSP 10
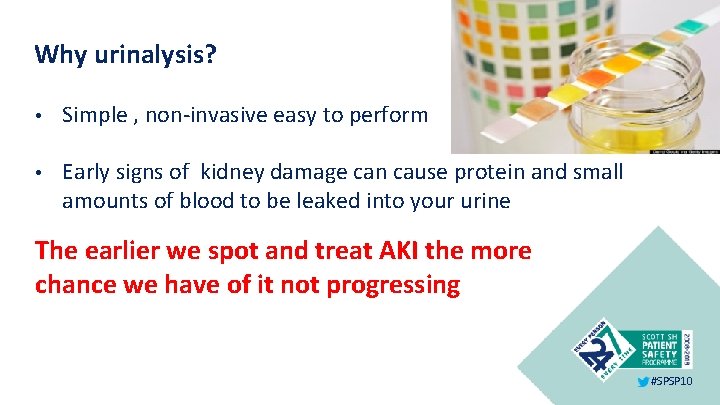
Why urinalysis? • Simple , non-invasive easy to perform • Early signs of kidney damage can cause protein and small amounts of blood to be leaked into your urine The earlier we spot and treat AKI the more chance we have of it not progressing #SPSP 10
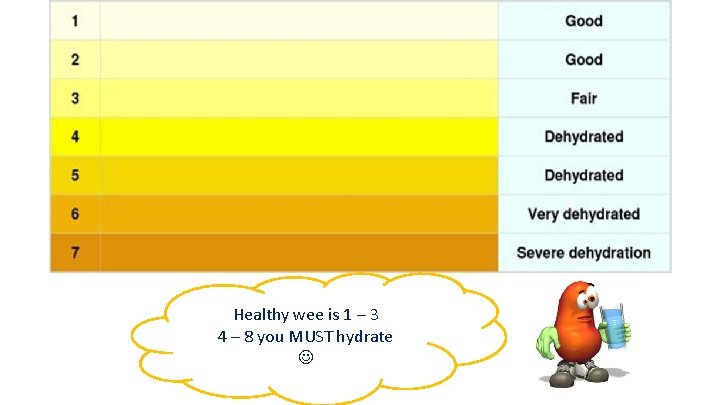
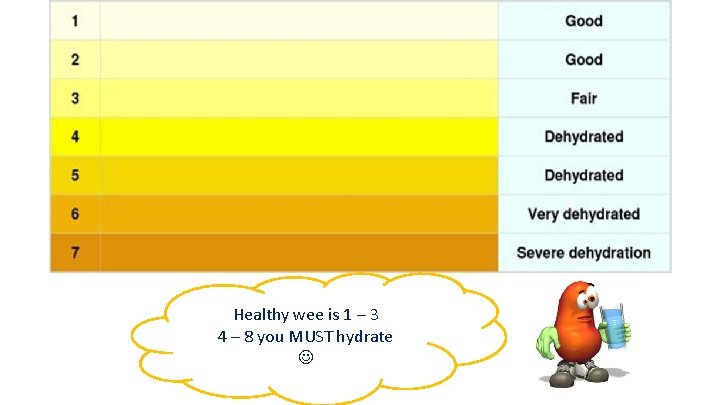
Healthy wee is 1 – 3 4 – 8 you MUST hydrate
Importance of fluid balance • Monitor fluid balance on a daily and cumulative basis • Daily weights are also a good indicator of acute fluid loss or gain • Accurately record fluid input and output #SPSP 10
Summary • • Accurate recording of intake and output Urinalysis – urine colour Discontinuing and / or avoiding certain potentially high risk medicines Monitor NEWS and escalate as indicated for unwell patients Prevention, early identification and early management are key to preventing an AKI, reducing mortality and length of stay and improving our patient outcomes #SPSP 10

NHS Tayside AKI video resource https: //www. youtube. com/watch? v=g. W 0 pg. Xr. Idgo #SPSP 10
References • Adding insult to injury (2009) National confidential enquiry into patient outcome & death. http: //www. ncepod. org. uk/2009 aki. htm • www. renal. org/guidelines • www. thinkkidneys. nhs. uk/aki #SPSP 10
 Acute kidney injury
Acute kidney injury Aki kifelé tekint álmodik aki befelé az ébred
Aki kifelé tekint álmodik aki befelé az ébred Intentional injury examples
Intentional injury examples Kdigo 2012 clinical practice guideline
Kdigo 2012 clinical practice guideline Aki bosnian boy
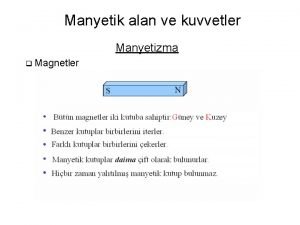
Aki bosnian boy Manyetik akı formülü
Manyetik akı formülü Shews score
Shews score Aki hietanen
Aki hietanen és aki száz meg százezret rabolt
és aki száz meg százezret rabolt Következményes mellékmondat
Következményes mellékmondat Jussi rasku
Jussi rasku Manyetik akı formülü
Manyetik akı formülü Kldi
Kldi Skt aki
Skt aki Normaalijakauma excel
Normaalijakauma excel Nem azert szeretlek aki vagy hanem
Nem azert szeretlek aki vagy hanem Wartburg
Wartburg