UKONS 24 Hour Triage Philippa Jones Macmillan Acute



- Slides: 52
UKONS 24 Hour Triage Philippa Jones Macmillan Acute Oncology Nurse Advisor UKONS Acute Oncology Members Interest Group Lead
What is triage ? Why do we need triage ? What's available now ?

What is triage ? Triage in a medical setting can be described as a clinical assessment process that identifies and prioritises patients according to the current or potential severity of the presenting problem. (http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 2564046/)
In modern healthcare systems triage is used at significant points in the patient pathway to determine level of urgency and intervention required: Triage on arrival at ED or Medical Assessment Unit. (The Manchester Triage, the Canadian Triage Assessment Scale, and the Australian Triage Score are triage tools that are currently in wide use in this setting) Pre hospital triage – 999 or 111 or in our case 24 hour advice lines. On site triage by the first clinician attending the patient e. g. para-medics. In order to use triage effectively, the underpinning logistics of an emergency care system must be in place in order to manage the patient appropriately.
Why do we need Triage in Oncology/Haematology? We know that Systemic Anti Cancer Treatment will produce unwanted side effects/toxicities some of which can be life threatening We offer patients receiving Systemic Anti Cancer Treatment a 24 advice line service We know that we do not always identify those patients at risk from side effects/toxicities (NCEPOD , NPSA, Cancer Patients in Crisis)
Patient on chemotherapy with a temperature phoned ward in the early hours and was advised that patient would need admission and IV antibiotics as per policy but told no beds available and to ring again in four hours (against policy). Patient presented to an Oncology Day Unit when open (four hours after call). Patient was very unwell, in pain and found to be neutropenic – treatment commenced and patient transferred to ward. Patient later died of neutropenic sepsis and renal failure.
Patient on chemotherapy : • Pyrexia of 39. 10 c • Shaking, feeling very unwell • Vomiting and diarrhoea patients wife rang medical registrar, was told she had a choice she could telephone for an ambulance and attend A&E or call emergency GP- she opted to contact the G. P.
Patient contacted chemotherapy helpline – symptoms described in line with spinal cord compression. Advised to ring 999 for assessment in ED. Patient contacted help line again 3 days later – condition worse – had attended ED as directed previously but was discharged after a 5 hour wait. Patient now immobile. Patient was later admitted to ward and treated for MSCC.
The past No agreed triage process or pathway – multitude of numbers- changing admission points – different level of service out of hours No agreed training or competency assessment No quality control or review No data collection No recognition of need, value or importance
Poor quality Consistency – this varied greatly according to who received the call – what time of day the call was received – where the call was received. Robust – without consistency it is impossible to provide a hardy, reliable service. Evidence based – there appeared to be little information about the use of evidence based practice tools, advice given depended on the experience of the call handler.
Governance Little or no governance planning or process Reactive not pro-active - reviewing incidents individually No clear advice line process mapping or expectations of the service Little or no evidence relating to the calls and actions taken – impossible to prove quality or highlight areas of concern
Lack of training and education No formal education or training process – expected to answer calls based on knowledge and experience No assessment of competency – not included in the chemotherapy education and assessment programmes Learn from others in practice – but who has taught and/or assessed them?
Lack of data Scanty or non existent data collection processes Unable to assess level of activity – times , numbers appropriate contacts Unable to look at the groups of people calling and why they are calling – assessment of risk factors/groups Unable to assess and report on quality

The present
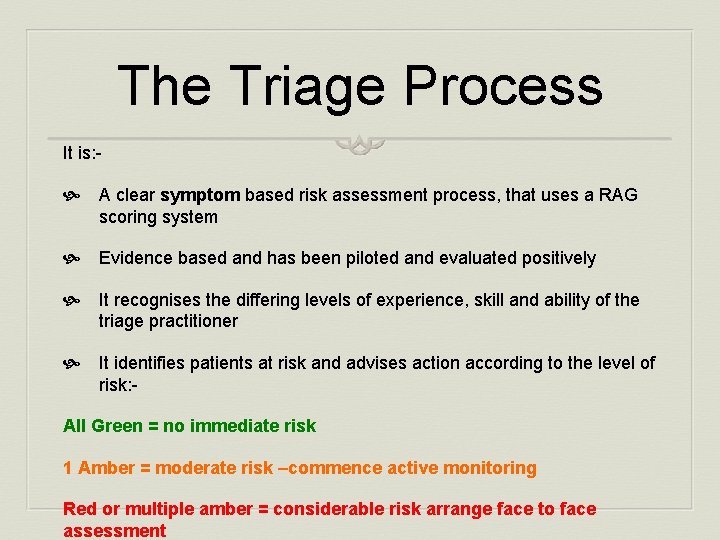
The Triage Process It is: - A clear symptom based risk assessment process, that uses a RAG scoring system Evidence based and has been piloted and evaluated positively It recognises the differing levels of experience, skill and ability of the triage practitioner It identifies patients at risk and advises action according to the level of risk: All Green = no immediate risk 1 Amber = moderate risk –commence active monitoring Red or multiple amber = considerable risk arrange face to face assessment
It does not: - Detail urgent initial management, this should commence at the assessment/admission portal. Initial management guidelines should be available in all admission portals Identify all possible treatment related problems, some will only be picked up during regular monitoring and review It may not pick up all signs and symptoms of concurrent health problems – though if completed properly it should alert the practitioner and prompt them to take action
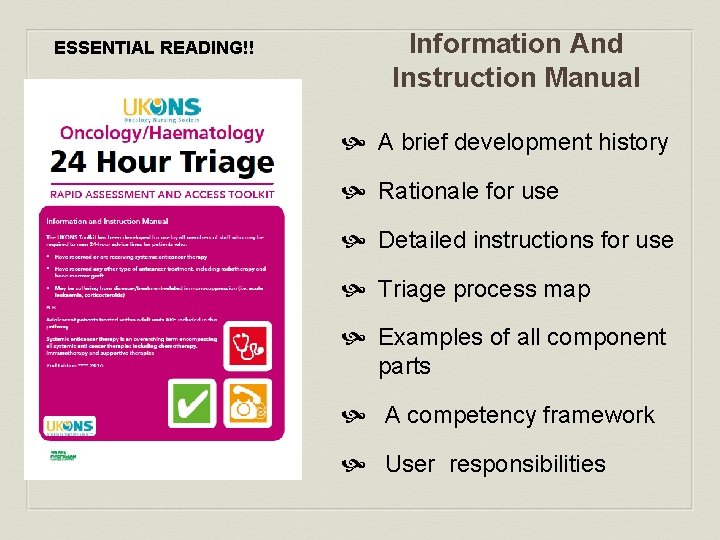
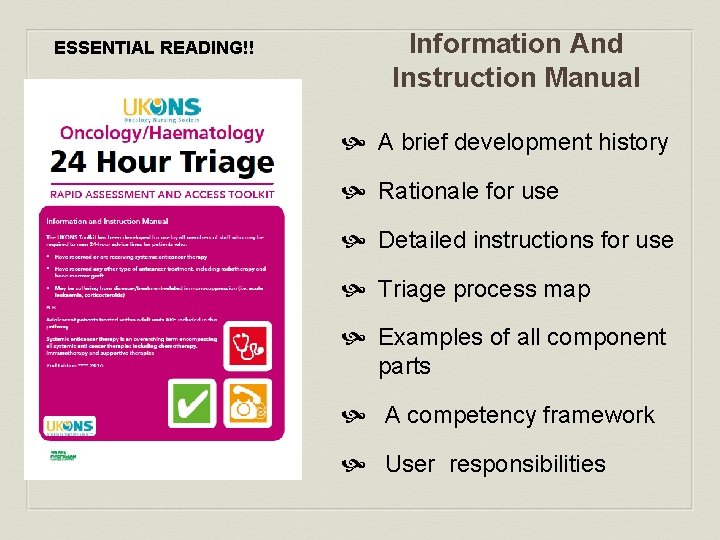
ESSENTIAL READING!! Information And Instruction Manual A brief development history Rationale for use Detailed instructions for use Triage process map Examples of all component parts A competency framework User responsibilities
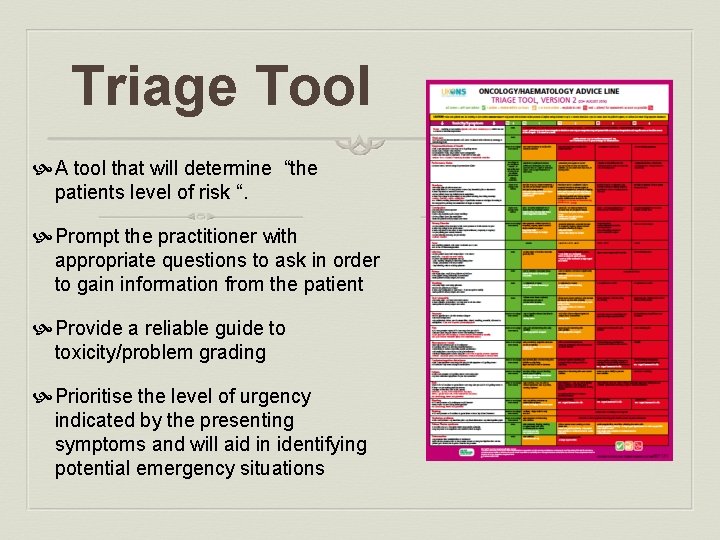
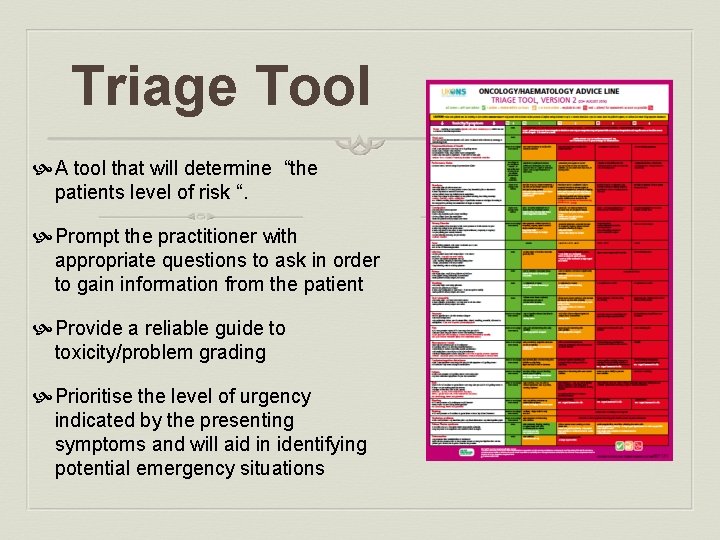
Triage Tool A tool that will determine “the patients level of risk “. Prompt the practitioner with appropriate questions to ask in order to gain information from the patient Provide a reliable guide to toxicity/problem grading Prioritise the level of urgency indicated by the presenting symptoms and will aid in identifying potential emergency situations
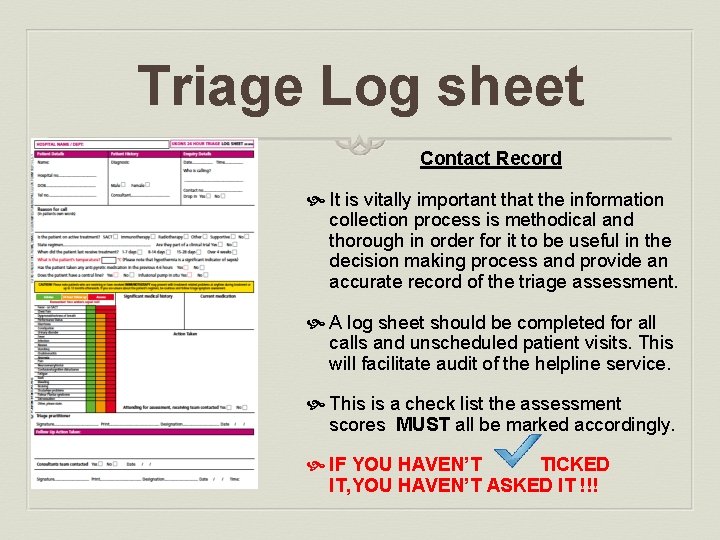
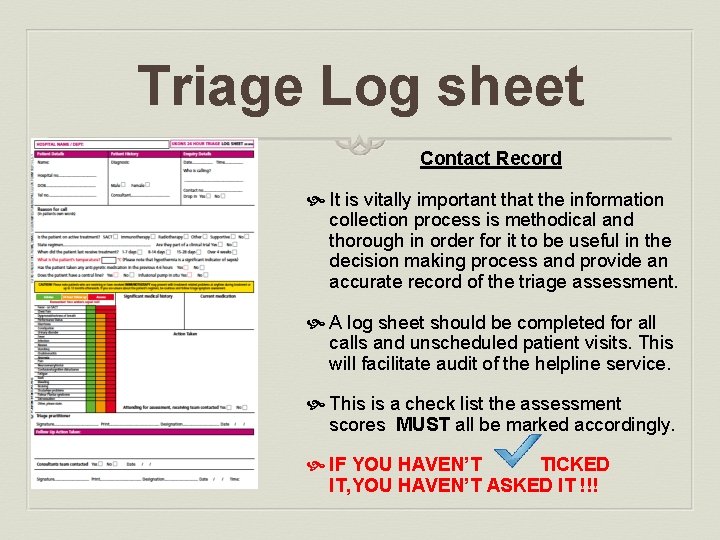
Triage Log sheet Contact Record It is vitally important that the information collection process is methodical and thorough in order for it to be useful in the decision making process and provide an accurate record of the triage assessment. A log sheet should be completed for all calls and unscheduled patient visits. This will facilitate audit of the helpline service. This is a check list the assessment scores MUST all be marked accordingly. IF YOU HAVEN’T TICKED IT, YOU HAVEN’T ASKED IT !!!
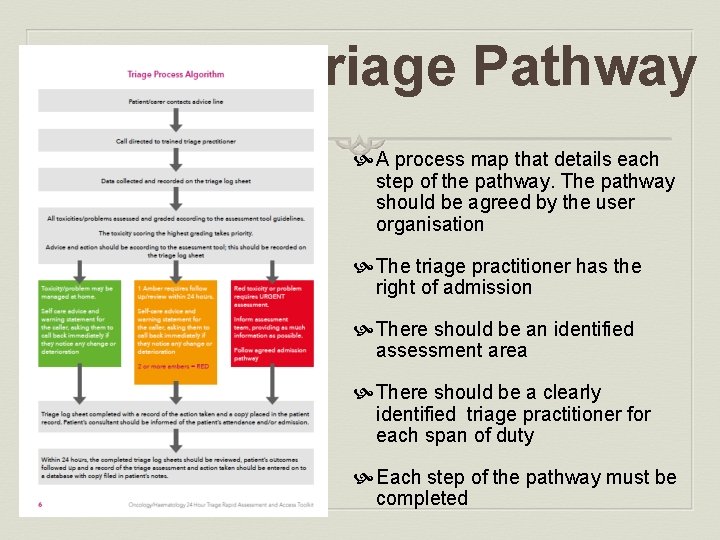
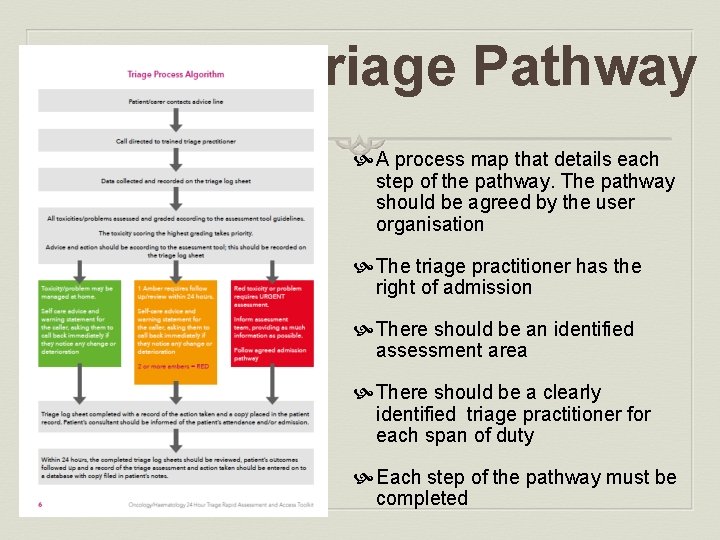
Triage Pathway A process map that details each step of the pathway. The pathway should be agreed by the user organisation The triage practitioner has the right of admission There should be an identified assessment area There should be a clearly identified triage practitioner for each span of duty Each step of the pathway must be completed
All Green = no immediate risk Reassurance and simple advice ask the patient to be vigilant and call again if concerned.

1 Amber = moderate risk Commence active monitoring
Red or multiple amber = considerable risk Arrange face to face assessment
Assessment ! Red or multiple amber = considerable risk arrange face to face assessment face to face consultation and assessment by an appropriately trained and qualified member of the clinical team. This assessment should take place in an appropriate area that provides access to investigation and treatment facilities. Patients should be asked to attend as soon as possible for assessment and transport arranged for them to do so if required
Step 1. Perform a rapid initial assessment of the situation: “is this an emergency? ” do you need to contact the emergency services Do you have any doubt about the patient/carers ability to provide information accurately or understand questions or instructions provided? If so then a face-to-face consultation should be arranged. Record Name and current contact details in case the call is interrupted and you need to get back to the caller.
Step 2. What is the patient/carers initial concern, why are they calling? You should assess and grade this problem first, ensuring that you record this on the log sheet. If this score is RED then you may decide to stop at this point and proceed to organising urgent face -to-face assessment. If the patient is stable you may decide to complete the assessment process in order to gather further information for the face-to-face assessment.
Step 3. If the patient/carers initial concern scores amber, record this on the log sheet and proceed with further assessment. Move methodically down the triage assessment tool, asking appropriate questions, e. g. do you have any nausea? If NO tick the green box on the log sheet and move on. If YES use the questions provided to help you grade the problem and note either amber or red and initiate action (tick the log sheet). If the patients’ symptoms score red or another
Step 4. Look back at your log sheet: Have you arranged assessment for patients who have scored RED? Have you arranged assessment for patients who have scored more than one AMBER? Have you fully assessed all the patients who have scored one AMBER, is there a tick in all the other green boxes of the log sheet? Have you fully assessed all the patients who have scored one GREEN, is there a tick in all the other green boxes of the log sheet? Have you recorded the action taken and advice given? Have you documented any decision you have taken or advice you have given that falls outside this guideline, and recorded
Training All staff who are expected to man a 24 Hour Triage Service should receive training and be assessed as competent Approved triage practitioners should be assessed annually in line with oncology annual assessment programme. Advice line calls should NOT be answered by untrained staff
Feedback No reports of increased or excessive attendance for assessment. Almost all patients who attend for assessment have some sort of physical examination, investigation and/or intervention to support diagnosis and management of the problem Admission rates following assessment have fallen slightly in some areas, particularly those with a functioning AOS team and/or assessment area, but patients still required investigation and intervention Please remember that it is easy with the gift of hindsight, following physical assessment and examination, to say that the patient who can go home, perhaps shouldn’t have attended. We are not privilege to the vital visual clues that have helped make this decision when assessing the patient over the phone
Clinical incidents! UKONS have been asked to comment on two coroners cases 1. A large trust that took it upon themselves to change the Alert temperature to 38. 0 o C. A patient rang twice with a temperature above 37. 5 the second time it was 37. 9 o. C – they were left at home and shortly after admitted with neutropenic sepsis. 2. A patient rang with chest pain the nurse taking the call decided not to follow the unequivocal red alert and referred the patient to the GP. The GP left the patient at home. Patient died shortly after following cardiac arrest. The patient was also on a 5 FU pump. Both of these cases have left families and staff devastated.
PILOT AND EVALUATION 32 12/3/2020
Background Developed over a 3 year period by a group of experienced senior nurses working within chemotherapy haematology and oncology. Supported by UK Oncology Nursing Society Multidisciplinary consultation. Supported by the U. K. National Patient Safety Agency Meets national recommendations , NCEPOD, NCAG and Acute Oncology Measures Extensive pilot in 26 cancer centres and units.
Aims and Objectives Improve patient safety and care by ensuring that patients receive a robust, reliable assessment (triage) every time they contact a helpline for advice. Consistency Those assessments (triage) are of a consistent quality and use an evidence based assessment (triage)tool. Evidence based That management and advice is appropriate to the patients ‟level of risk”. This will ensure that those patients who require urgent assessment in an acute area are identified and that action is taken, but also to identify and reassure those patients who are at lower risk and may safely be managed by the primary care team or a planned clinical review and avoid unnecessary attendance. Appropriate To develop guidelines that would form the basis of triage 34 12/3/2020 training and competency assessment for practitioners. Educational Philippa Jones
Key points Guidance and support to the practitioner at all steps of the helpline process A simple but reliable assessment process Safe and understandable advice Communication and record keeping Competency based training An audit tool Philippa Jones 35 12/3/2020
Pilot in September and October 2009 26 cancer centres and units were involved. A two step evaluation process; - Questionnaire A review of completed log sheets The pilot ran for a two month period or completion of 100 log sheets Supported by the U. K. National Patient Safety Agency Philippa Jones. 36 12/3/2020
48% of the patients who contacted the helpline were asked to attend hospital for assessment. Of this group; - 70% were admitted 30% were assessed and discharged following intervention. Philippa Jones 37 12/3/2020
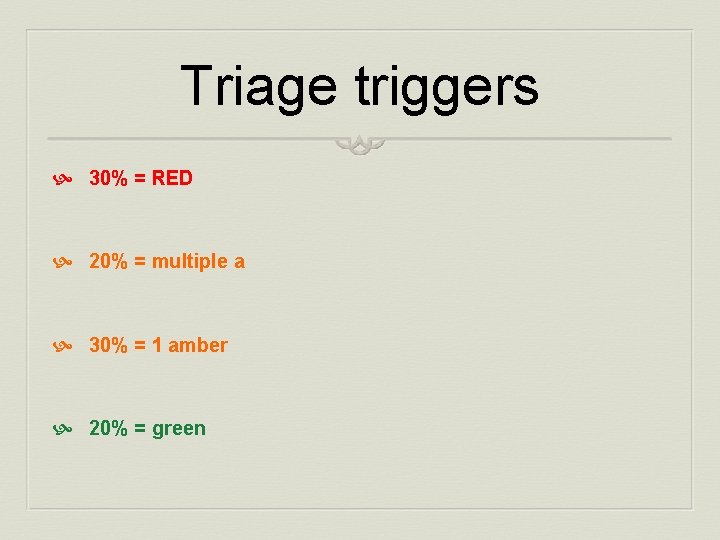
Triage triggers 30% = RED 20% = multiple a 30% = 1 amber 20% = green
30% = Red triggers The majority of patients (91%) who had a red trigger were asked to attend hospital for assessment This action was appropriate as 82% required admission to hospital Only 9% were able to go home following assessment Philippa Jones 39 12/3/2020
Caution! Only 44% of patients with a red trigger had pyrexia of 37. 50 c or above recorded, 20% of patients had no pyrexia and 36% had no recording of temperature. Conclusion. . . 56% of red trigger patients were not related to pyrexia, these patients still required assessment and most required hospital admission. Though it is recognised that the presence of a pyrexia in a patient who may be immuno-compromised is a significant indicator of risk, it is clear from the information collected on the log sheets that it is not the only indicator of risk. Philippa Jones 40 12/3/2020
Questionnaire feedback and comments The vast majority of comments and feedback included in the questionnaires were positive. There were also a small number of negative responses though these were on the whole constructive. Philippa Jones 41 12/3/2020
Positive Tool has standardised practice Toxicity assessment very popular Concertina card extremely popular Visible reassurance of assessment Aids inter departmental communication Trainers like the competency framework Philippa Jones 42 12/3/2020
Negative 2 ambers are not always red time consuming - feedback has been provided that lets us know that the time taken to complete the process lessens with experience There were a number of comments relating to the format of the tool kit, all of which were considered at the steering group evaluation meeting. All were addressed in the improved design of the final Tool Kit. Philippa Jones 43 12/3/2020
The Tool kit is a framework that can be used to; Improve patient safety and care by ensuring that they receive a robust, reliable assessment every time they contact a helpline for advice. Ensure those assessments are of a consistently high quality by the use an evidence based assessment tool. Identify action and advice that is appropriate to the patients’ level of risk. Ensure that those patients who require urgent assessment in an acute area are identified and that action is taken, but also to identify and reassure those patients who are at lower risk and may safely be managed by the primary care team or a planned clinical review and avoid unnecessary attendance. Philippa Jones 44 12/3/2020 Form the basis of triage training and competency assessment for
AUDIT High risk patient groups Activity Patient tracking Proof of quality Identify poor practice Service planning and development Pro-active monitoring Philippa Jones 45 12/3/2020
Standardised evidence based triage. Launched in 2010 Training and competency assessment Communication and data collection Quality and safety assessment Used widely across the UK and also internationally No reports of incidents or adverse events linked to the correct use of the tool
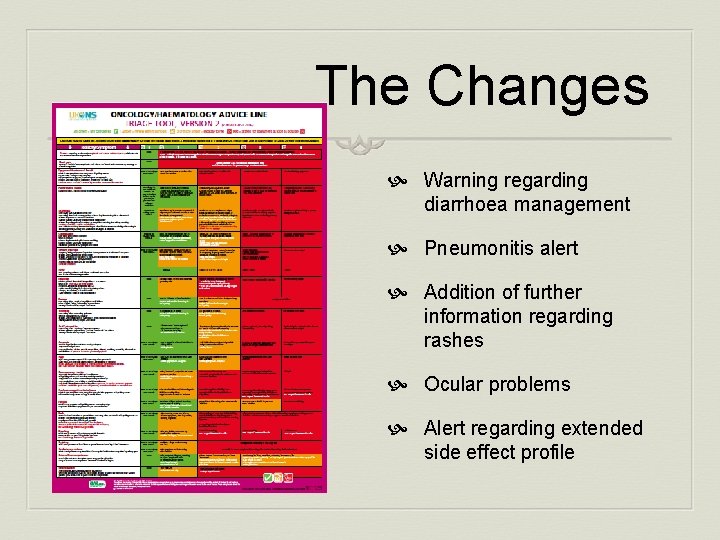
2016 Update and Review Initial testing with a small group of specialist nurse who manage a caseload of patients receiving immunotherapies The tool performed very well overall, and only required a small number of changes Revised tool and log sheet forwarded to the original development team and consultation group and a small number of specialist nurses. Excellent feedback regarding current use +a couple of suggestions for small changes/additions
The Changes Warning regarding diarrhoea management Pneumonitis alert Addition of further information regarding rashes Ocular problems Alert regarding extended side effect profile
WHY DO WE NEED TO SUCCEED? P. J. Jones UKONS 49 December 20
Patient receiving chemotherapy with a history of neutropaenic sepsis following each previous cycle of treatment. Telephoned A&E for advice as she had a raised temperature. She was advised to take regular paracetamol and to report if temperature of 38. 00 c whilst on paracetamol. Patient presented at chemotherapy clinic, unwell, pyrexia 38. 00 c and neutrophils 0. 1 x 10 x 9/L. P. J. Jones UKONS 50 December 20 Immediate admission for treatment of neutropaenic sepsis.
The patient was discharged post chemotherapy with recovering blood counts The Clinical Nurse Specialist contacted the patient and gave them aftercare advice and the emergency contact number. When the patient became pyrexial 380 c he followed CNS advice and contacted the Helpline number/Ward. The person who took the call told him to take some paracetamol. 51
Any questions? Thank you
 Ukons
Ukons Ukons acute oncology guidelines
Ukons acute oncology guidelines Thyroidtitis
Thyroidtitis Philippa doyle
Philippa doyle Philippa fawcett
Philippa fawcett Philippa costello
Philippa costello Sergio maffeis
Sergio maffeis Philippa lawson
Philippa lawson Philippa foot
Philippa foot How to write 24 hour time
How to write 24 hour time Clock hour to credit hour conversion
Clock hour to credit hour conversion Myeloma cure on the horizon
Myeloma cure on the horizon Macmillan professional
Macmillan professional Puntos de sutura macmillan
Puntos de sutura macmillan Ladbroke v todd
Ladbroke v todd Empresa e iniciativa emprendedora macmillan
Empresa e iniciativa emprendedora macmillan Macmillan concerns checklist
Macmillan concerns checklist Macmillan profesional
Macmillan profesional Why did harold macmillan resign
Why did harold macmillan resign Motores macmillan
Motores macmillan Recursos humanos macmillan
Recursos humanos macmillan Dr patrick macmillan
Dr patrick macmillan Macmillan publishers
Macmillan publishers Macmillan next steps
Macmillan next steps Macmillan professional
Macmillan professional Macmillan profesional
Macmillan profesional Macmillan plumbing
Macmillan plumbing Macmillan professional
Macmillan professional Glen macmillan
Glen macmillan Electricidad basica macmillan
Electricidad basica macmillan Atls triage scenarios answers 10th edition
Atls triage scenarios answers 10th edition Wat is triage
Wat is triage Education triage
Education triage Jump triage
Jump triage Brad keating
Brad keating Triage van waddell
Triage van waddell Psystart
Psystart Peec triage
Peec triage Reverse triage evacuation order
Reverse triage evacuation order Service desk triage process
Service desk triage process Disaster triage
Disaster triage Tarjetas de triage
Tarjetas de triage Start triage
Start triage Reverse triage lightning
Reverse triage lightning Oncology triage tool
Oncology triage tool Dr wuyts tienen
Dr wuyts tienen Triage 30 2 can do
Triage 30 2 can do Start triage rpm
Start triage rpm Start adult triage
Start adult triage Jump start in field traige assessment
Jump start in field traige assessment Field triage decision scheme steps
Field triage decision scheme steps Avpu schema
Avpu schema Goals of triage
Goals of triage