COMPLICATIONS OF HYPERTENSIVE DISORDER Acute fulminating preeclampsiaSevere Eclampsia
- Slides: 27
COMPLICATIONS OF HYPERTENSIVE DISORDER
• • Acute fulminating preeclampsia(Severe) Eclampsia Hypertensive Crisis HELLP (Hemolysis, elevated liver enzyme and low platelets) Syndrome DIC (disseminated intravascular coagulation) Neurovascular accident Abruptio placentae Pulmonary Edema
Eclampsia Preeclampsia when complicated by grandmal seizure and/ or coma is called Eclampsia. Majority of it (80%) is preceded by preeclampsia. Incidence: 1 in 30 -500 deliveries Common in twin, primigravida, and after 36 weeks of gestation(antenatal, intranatal & postnatal period) Recurrence risk varies from 2 -25%. Risk of PE and Eclampsia in daughter is 25% and 3% respectivly. Causes: Anoxia- due to spasm of cerebral vessels Cerebral edema- contributes to irritation Cerebral Dysrhythmia – due to Excessive release of excitatory neurotransmitters
Clinical features • Previous manifestations of acute severe preeclamsia • Grandmal seizure with Premonitory, Tonic clonic and stage of coma v. It may occur in quick succession- Status eclampticus Differential Diagnosis: Epilepsy, Encephalitis, Meningitis, Cerebral Thrombosis, cerebral malaria, Intracranial tumor
Complications of Eclampsia Injuries Pulmonary edema, embolism, Pneumonia, ARDS Cerebral Hemorrhage Hepatic Necrosis/ Sub-capsular hemorrhage Ac left ventricular failure Renal failure All the complications associated to severe preeclampsia • Maternal and Perinatal Mortality (2 -30%) • •
Management Immediate Management: 1. Maintain airway/ breathing and circulation 2. Oxygen administration 3. Lateral Recumbent position 4. Measure to prevent from Injury 5. Preventing from injury 6. Monitoring of oxygen saturation 7. Control of seizure – Magnesium sulfate
Magnesium Sulfate § Works as a centrally acting anticonvulsant • Blocks neuromuscular conduction Pritchard Regime: 4 gm (20% solution) slow Intravenous, and 10 gm of 50% Mgso 4 intramuscular (5 gm in each buttock) followed by 5 gm (50%) IM 4 hourly in alternate buttocks Monitoring : § Respiratory Rate § urine output § Deep tendon reflex Ø With renal dysfunction, may require a lower dose Ø Serum levels: 6 -8 mg/d. L are considered therapeutic Ø Continued for 24 hrs of delivery or last seizure whichever is later
Toxicity • • Respiratory rate < 12 DTR not detectable Altered sensorium Urine output < 25 -30 cc/hour Ø Stop Magnesium sulfate Ø Antidote: 10 ml of 10% solution of calcium gluconate IV over 3 minutes
Alternate Anticonvulsants • Have not been shown to be as efficacious as magnesium sulfate and may result in sedation that makes evaluation of the patient more difficult – Diazepam 5 - 10 mg iv – Phenytoin 500 -1000 mg IV infusion/ enteral – Lytic Cocktail Regime (Promethazine + Chlopromazine+ Pethidine)
After the Seizure • • • Assess maternal condition Fetal well-being Effect delivery Transport when indicated No need for immediate cesarean delivery If BP remain high – Antihypertension should be given(Labetalol/ Hydrallazine) to keep the BP 140 -160/ 90 - 100 mm. Hg
Delivery Ø Delivery is decided after seizure is over. Not necessary to go for C-section to all a) Baby mature: If cervix is favorable/ no contraindication to vaginal delivery – Induction is done by ARM/ oxytocin infusion Unfavorable cervix- PGE 2 for ripening b) Baby premature: Steroid if < 34 weeks c) Baby Dead: May need induction d) Immediate delivery: If fits not controlled/ Maternal and/ or fetal condition is unstable. Ø Indications of C-section: Uncontrolled fits, Unconscious patients, Obstetrical indication
Hypertensive Emergencies • • • Fetal monitoring IV access IV hydration The reason to treat is mother, not fetus May require ICU
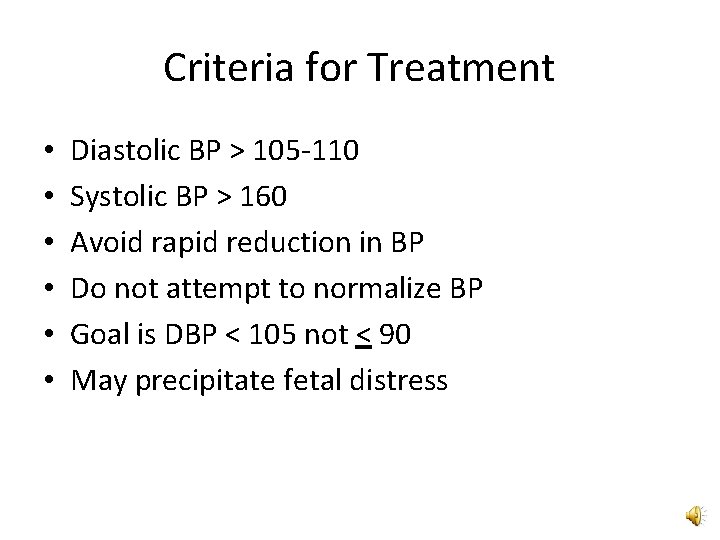
Criteria for Treatment • • • Diastolic BP > 105 -110 Systolic BP > 160 Avoid rapid reduction in BP Do not attempt to normalize BP Goal is DBP < 105 not < 90 May precipitate fetal distress
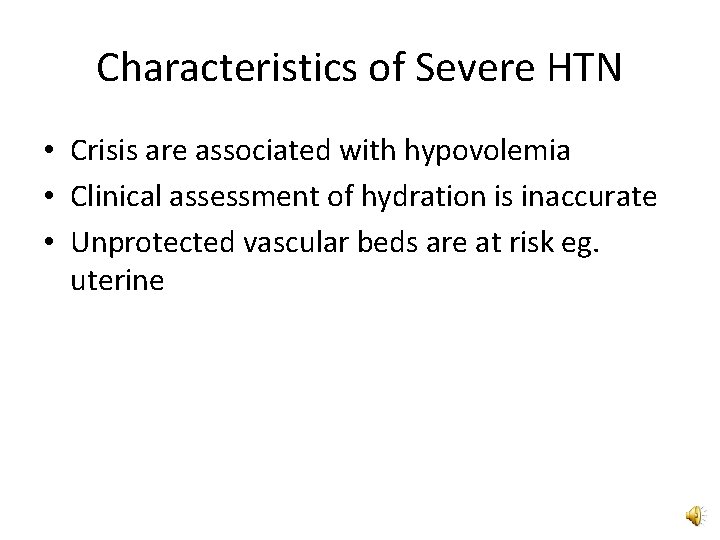
Characteristics of Severe HTN • Crisis are associated with hypovolemia • Clinical assessment of hydration is inaccurate • Unprotected vascular beds are at risk eg. uterine
Acute Medical Therapy • Hydralazine • Labetalol • Nifedipine
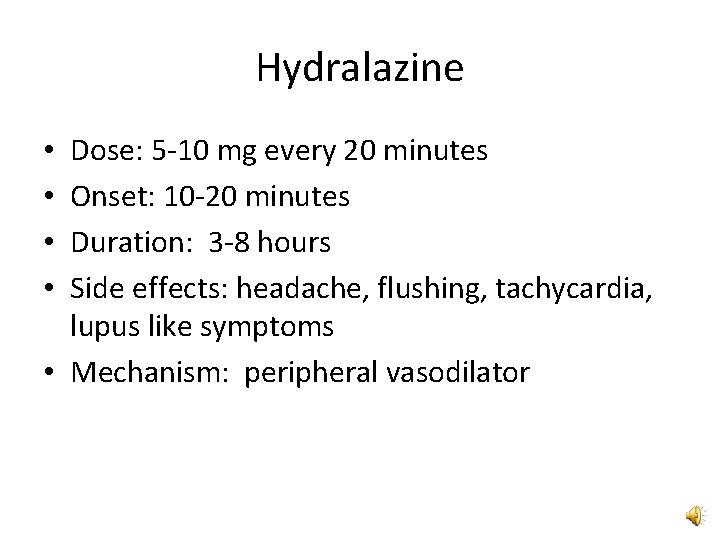
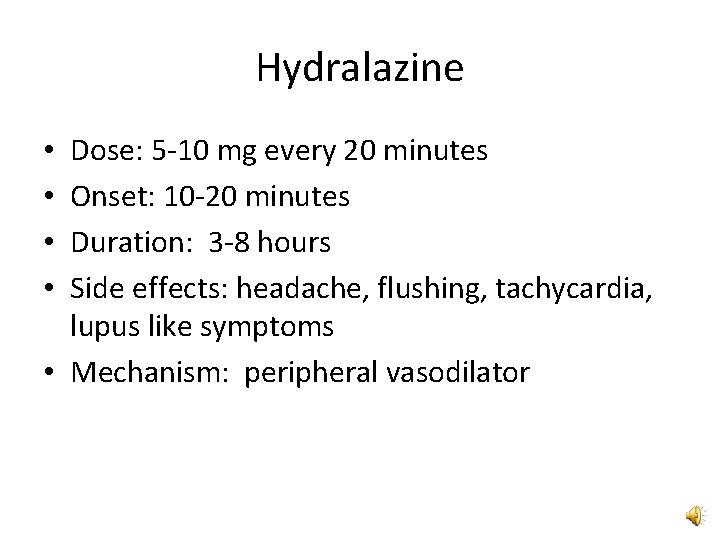
Hydralazine Dose: 5 -10 mg every 20 minutes Onset: 10 -20 minutes Duration: 3 -8 hours Side effects: headache, flushing, tachycardia, lupus like symptoms • Mechanism: peripheral vasodilator • •
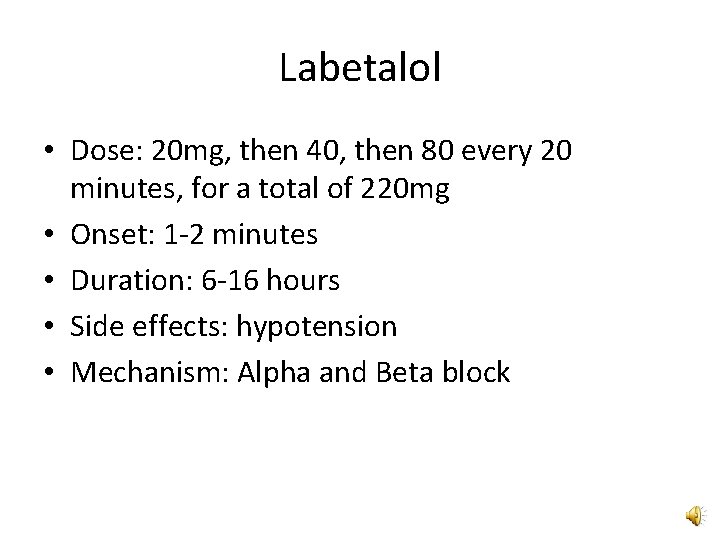
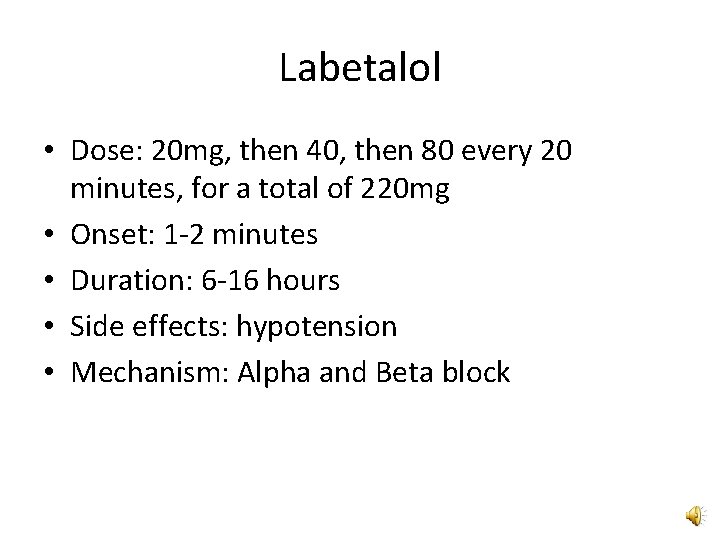
Labetalol • Dose: 20 mg, then 40, then 80 every 20 minutes, for a total of 220 mg • Onset: 1 -2 minutes • Duration: 6 -16 hours • Side effects: hypotension • Mechanism: Alpha and Beta block
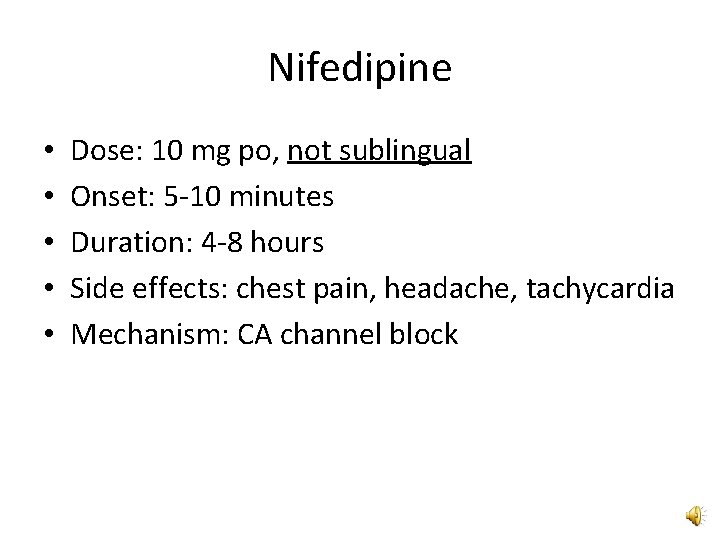
Nifedipine • • • Dose: 10 mg po, not sublingual Onset: 5 -10 minutes Duration: 4 -8 hours Side effects: chest pain, headache, tachycardia Mechanism: CA channel block
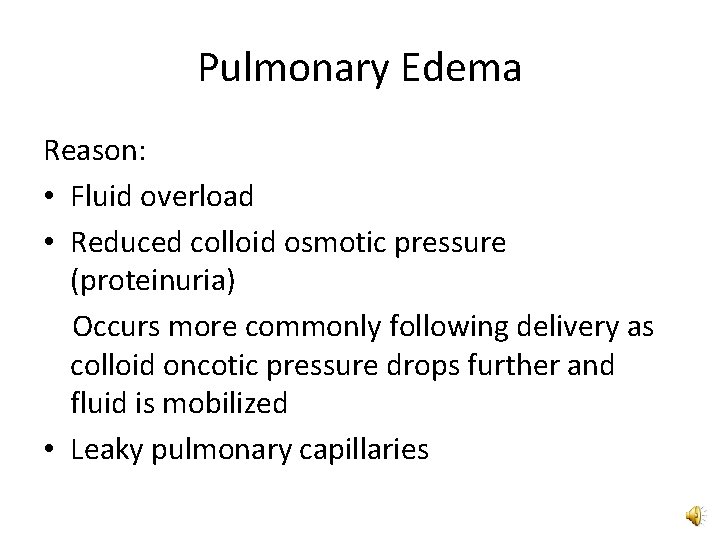
Pulmonary Edema Reason: • Fluid overload • Reduced colloid osmotic pressure (proteinuria) Occurs more commonly following delivery as colloid oncotic pressure drops further and fluid is mobilized • Leaky pulmonary capillaries
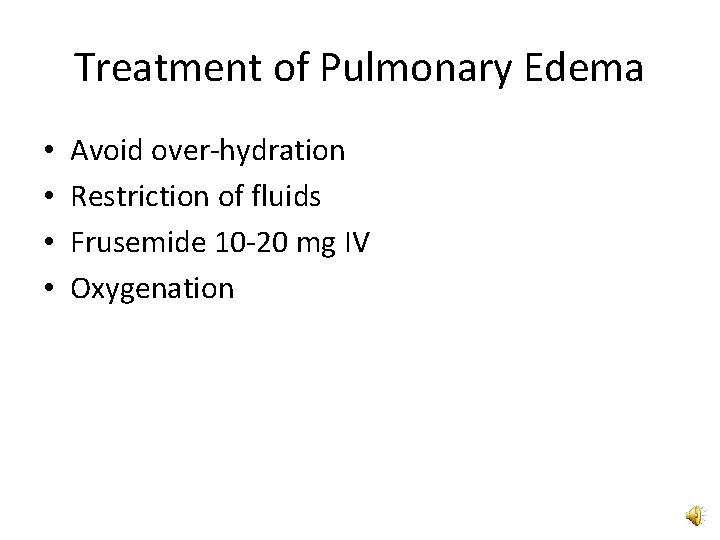
Treatment of Pulmonary Edema • • Avoid over-hydration Restriction of fluids Frusemide 10 -20 mg IV Oxygenation
HELLP Syndrome • He-hemolysis • EL-elevated liver enzymes • LP-low platelets Ø Incidence: 3% of a case of preeclampsia
HELLP Syndrome Is a variant of severe preeclampsia Platelets < 100, 000 LFT’s - 2 x normal May occur against a background of what appears to be mild disease Ø Management is symptomatic and need blood product. Need delivery as early as possible. • •
Oliguria • 25 -30 ml per hour is acceptable • If less, small fluid boluses of 250 -500 ml as needed • Frusemide is not necessary (Except in heart failure/ Pulmonary edema) • Postpartum diuresis is common • Persistent oliguria – my need Dopamininfusion
Persistent Hypertension • BP may remain elevated for several days • Diastolic BP less than 100 do not require treatment • By definition, preeclampsia resolves by 6 weeks
Disseminated Intravascular Coagulopathy • Rarely occurs without abruption • Low platelets is not DIC • Requires replacement blood products and delivery
Prevention • Low dose Aspirin(60 -80 mg daily) is recommended in patients with a history of early onset preeclampsia and delivery less than 34 weeks or H/O preeclampsia in more than one prior pregnancy • Calcium supplementation • Antioxidants • Heparin - Helpful in patients with Thrombophilia or Antiphospholipid Syndrome
Thank You!
 Acute fulminating preeclampsia
Acute fulminating preeclampsia Eclampsia definicion
Eclampsia definicion Diagnosis of post traumatic stress disorder
Diagnosis of post traumatic stress disorder Dsm 5 munchausen by proxy
Dsm 5 munchausen by proxy Eclampsia
Eclampsia Eclampsia symptoms
Eclampsia symptoms Eden criteria eclampsia
Eden criteria eclampsia Oligohydramnios management
Oligohydramnios management Magnesium in preeclampsia mechanism
Magnesium in preeclampsia mechanism Hellp syndrome symptoms
Hellp syndrome symptoms Hypertensive encephalopathy
Hypertensive encephalopathy Htn urgency vs emergency
Htn urgency vs emergency Bonnet sign
Bonnet sign Hypertensive uveitis
Hypertensive uveitis Htn emergency vs urgency
Htn emergency vs urgency Malignant hypertension
Malignant hypertension Hypertensive crisis classification
Hypertensive crisis classification Hemmorragie
Hemmorragie The cardiovascular system chapter 11
The cardiovascular system chapter 11 Malignant hypertension treatment
Malignant hypertension treatment Hypertensive emergency
Hypertensive emergency Thyroid storm pathophysiology
Thyroid storm pathophysiology Gagandeep singh bedi
Gagandeep singh bedi Hypertension urgency vs emergency
Hypertension urgency vs emergency Silver wiring retina
Silver wiring retina Malignant hypertension treatment
Malignant hypertension treatment Meto zerok 25 mg nebenwirkungen
Meto zerok 25 mg nebenwirkungen Faranoush
Faranoush