1 Hypertensive Crises Diagnosis and Treatment Hypertensive Crises





- Slides: 33

1
Hypertensive Crises Diagnosis and Treatment
Hypertensive Crises • Severely elevated(BP>220/130 mmhg) blood pressure with signs and symptoms of acute end organ damage • Requires hospitalization • Requires parenteral medication
Hypertensive Urgency • Severely elevated blood pressure(BP>=220/130 mmhg) without signs and symptoms of acute end organ damage • Can be managed as an outpatient • Can be managed with short acting oral medications
Severe Hypertension • BP 180/110 to 220/130 without symptoms or acute organ damage • Almost always occur in chronic HTN patients who stop their medication • Treat with long acting oral drugs
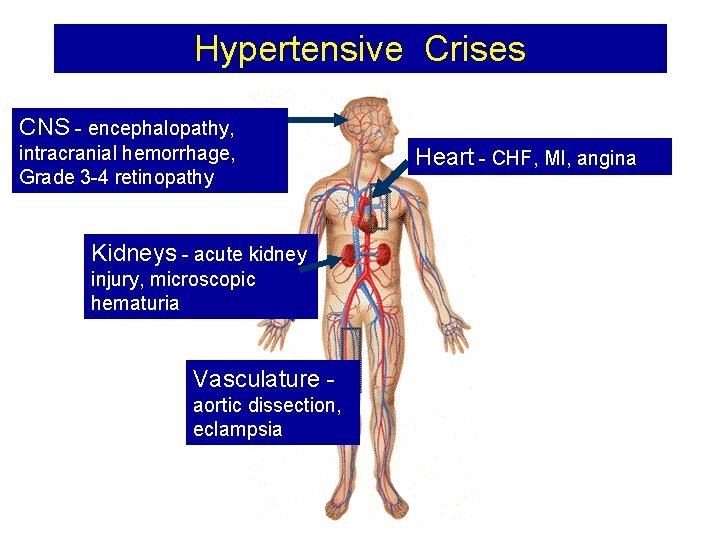
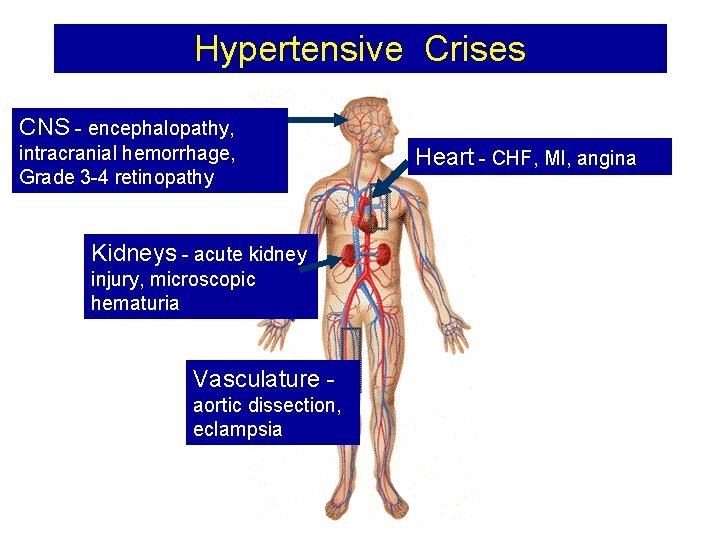
Hypertensive Crises CNS - encephalopathy, • Damage intracranial hemorrhage, Grade 3 -4 retinopathy Kidneys - acute kidney injury, microscopic hematuria Vasculature Vasculatur e aortic dissection, eclampsia Heart - CHF, MI, angina
Epidemiology • Hypertensive emergencies are common – Occur in 1 -2% of the hypertensive population – But, 50 million hypertensive Americans – 500, 000 hypertensive emergencies/year • Higher in the elderly • Incidence in men 2 times higher than in women
Initial Evaluation • Assess for end-organ damage • Vascular Disease – Assess pulses in all extremities – Auscultate over renal arteries for bruits • Cardiopulmonary – Listen for rales (CHF) – Murmurs or gallops
Initial Evaluation • Neurologic Exam – Hypertensive Encephalopathy - mental status changes, nausea, vomiting, seizures – Lateralizing signs uncommon and suggest cerebrovascular accident • Retinal Exam
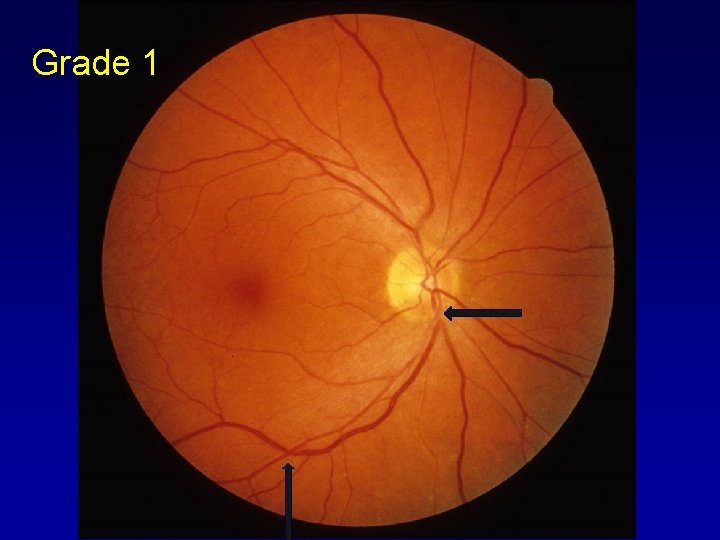
Retinopathy Grading • Grade 1 – Mild narrowing of the arterioles – “Copper Wire” • Grade 2 – Moderate narrowing Copper wire and AV nicking
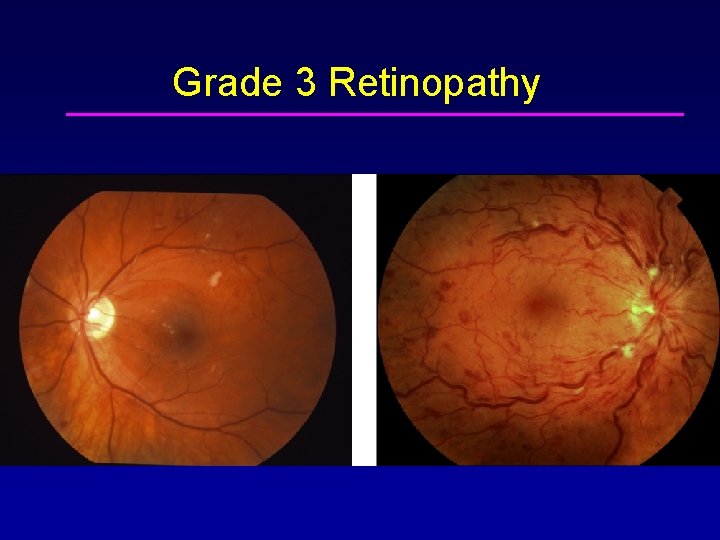
Retinopathy Grading • Grade 3 – Severe Narrowing Silver wire changes, hemorrhage, cotton wool spots, hard exudates • Grade 4 – Grade 3 + Papilledema • Grade 3 and 4 highly correlated with progression to end organ damage and decreased survival
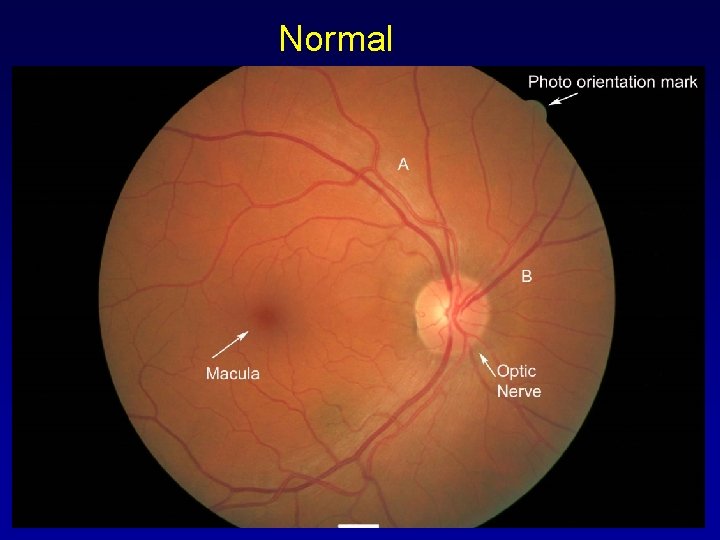
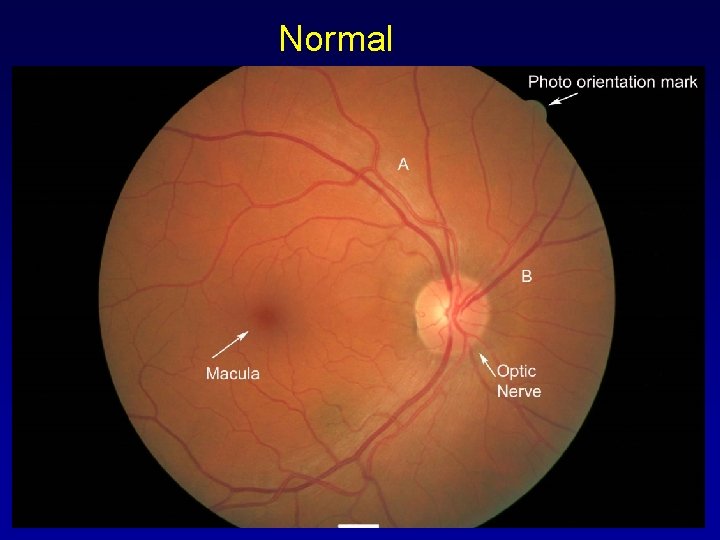
Normal
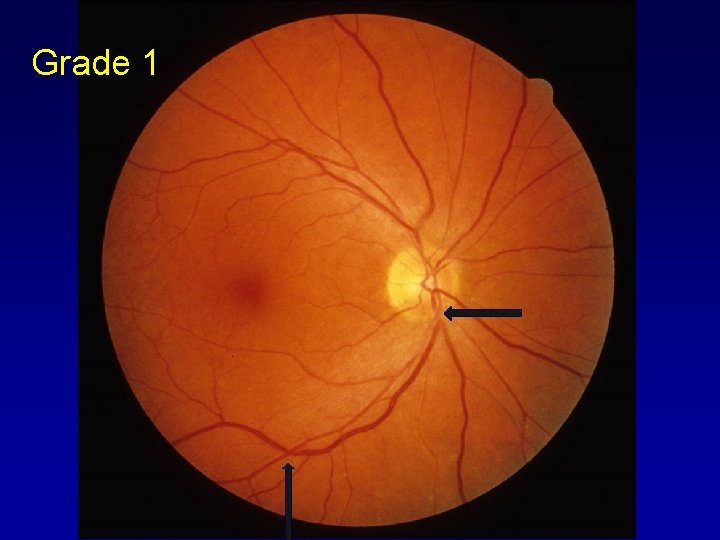
Grade 1

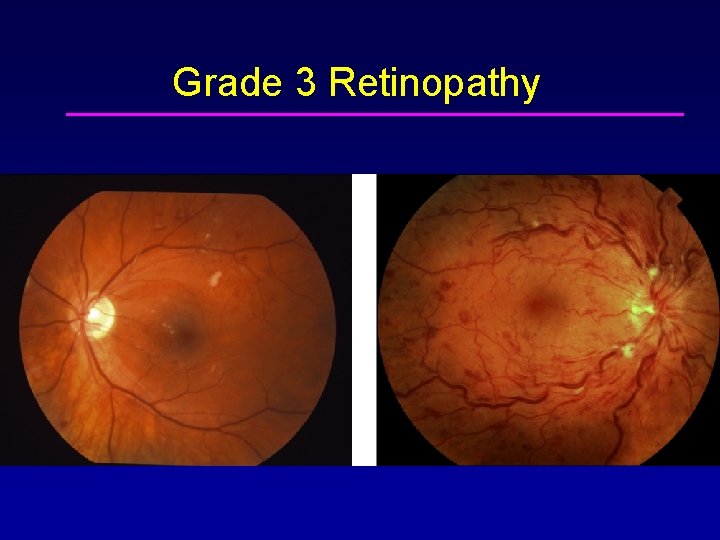
Grade 3 Retinopathy

Lab Testing • ECG – LVH, look for signs of ischemia, injury, infarct • Renal Function Tests (urine included) – Elevated BUN, Creatinine, proteinuria, hematuria • CBC • CXR - pulmonary edema, aortic arch, cardiac enlargement
Lab Testing • Aortic Dissection? – Suspect with severe tearing chest pain, unequal pulses, widened mediastinum – Contrast Chest CT Scan or MRI • Pulmonary Edema/CHF – Transthoracic Echocardiogram
Cerebral Blood Flow Autoregulation • Cerebral Blood Flow Autoregulation – Cerebral Blood constant in normotensive individuals over range of MAPs of 60 -120 mm Hg. – In chronically hypertensive patients autoregulatory range is higher – MAP Range 100 -120 to 150 -160 mm Hg • Autoregulation also impaired in the elderly and those with cerebrovascular disease
Management • Hypertensive Crises(elevated BP with target organ damage) • Parenteral meds • Goal - Reduce diastolic BP by 10 -15% or to 110 mm Hg over a period of 30 60 minutes
Management • Where? – ICU with close monitoring – Severe requires intra-arterial BP monitoring • Which Parenteral meds? • Depends on the situation
Sodium nitroprusside • Disadvantages of sodium nitroprusside – Decrease cerebral blood flow and increases intracranial pressure – Can reduce regional blood flow in coronary artery disease – Risk of cyanide toxicity • Use when other agents not effective – – Monitor thiocyanate levels Avoid in renal or hepatic dysfunction Choice in Aortic Dissection, CHF 0. 3 -10 microgm/kg/min
Urapidil • New central sympatholytic drug • Selective alpha -1 receptor blocks • Dose 12. 5 -25 mg /kg bolus and 5 -40 mg/hr iv infusion • Choice in HTN after CABG&After craniotomy
Labetalol • Alpha&Beta Blocker(Beta>Alpha) • Choice in Hypertensive encephalopathy, Ischemic&Hemorrhagic Stroke, Severe preeclampsia/eclampsia, Aortic Dissection • 2 -4 mg/min
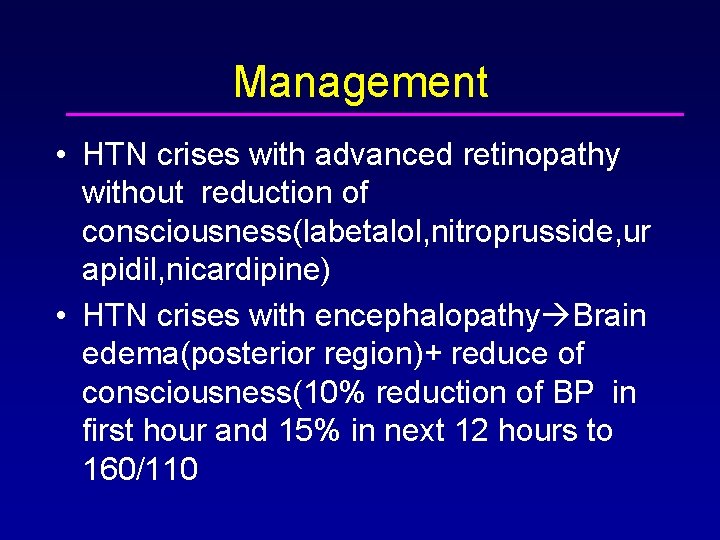
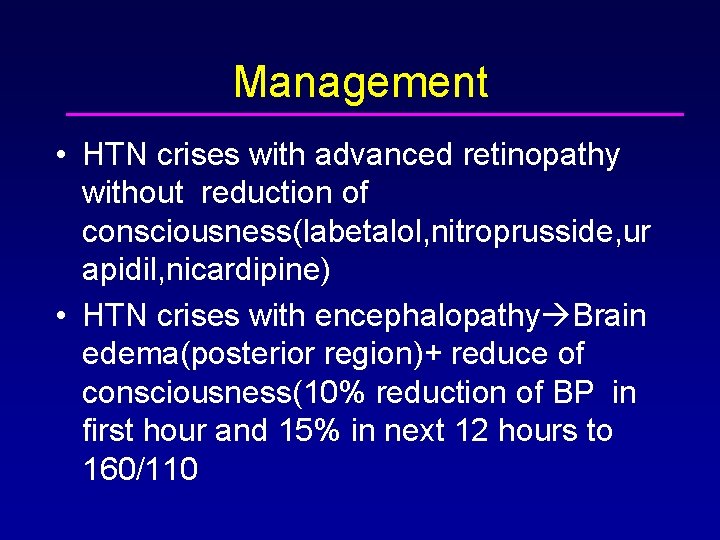
Management • HTN crises with advanced retinopathy without reduction of consciousness(labetalol, nitroprusside, ur apidil, nicardipine) • HTN crises with encephalopathy Brain edema(posterior region)+ reduce of consciousness(10% reduction of BP in first hour and 15% in next 12 hours to 160/110
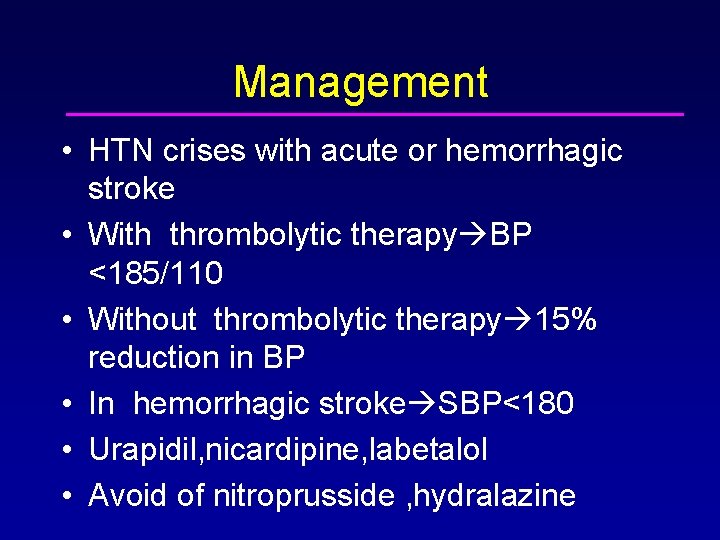
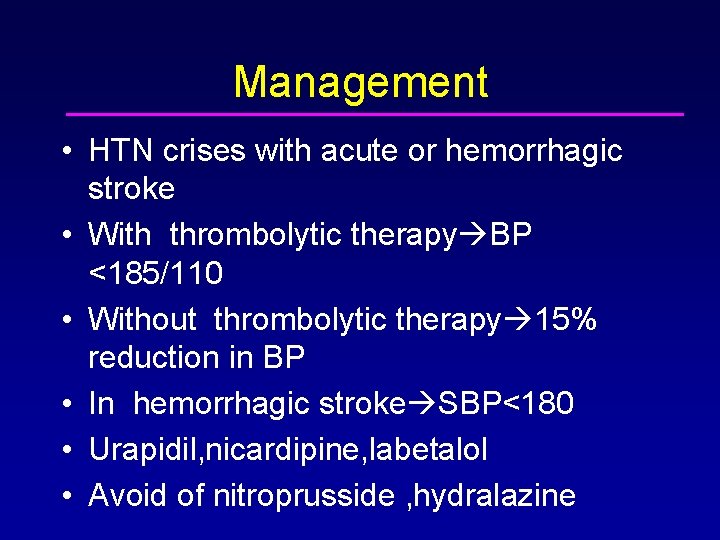
Management • HTN crises with acute or hemorrhagic stroke • With thrombolytic therapy BP <185/110 • Without thrombolytic therapy 15% reduction in BP • In hemorrhagic stroke SBP<180 • Urapidil, nicardipine, labetalol • Avoid of nitroprusside , hydralazine
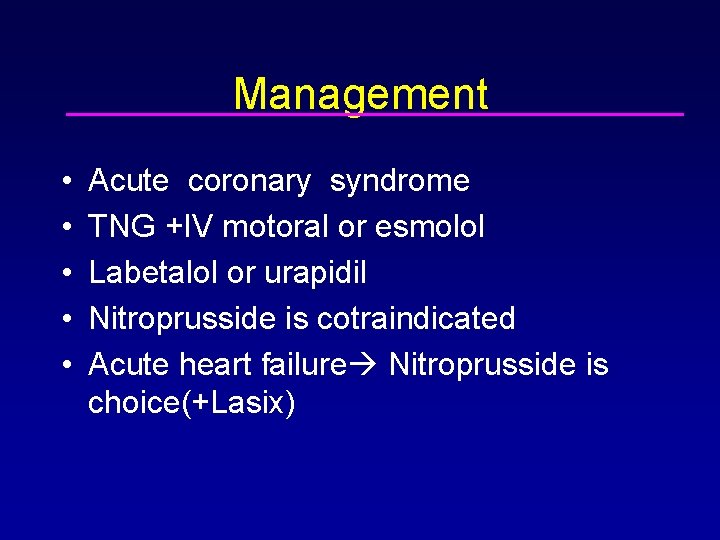
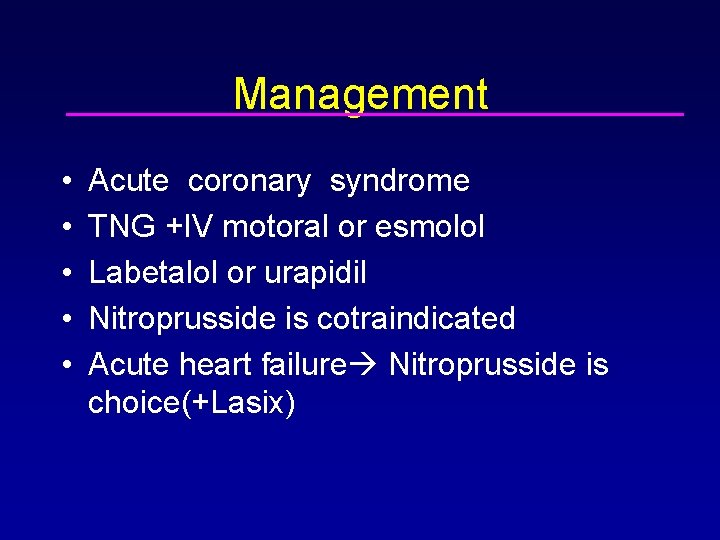
Management • • • Acute coronary syndrome TNG +IV motoral or esmolol Labetalol or urapidil Nitroprusside is cotraindicated Acute heart failure Nitroprusside is choice(+Lasix)
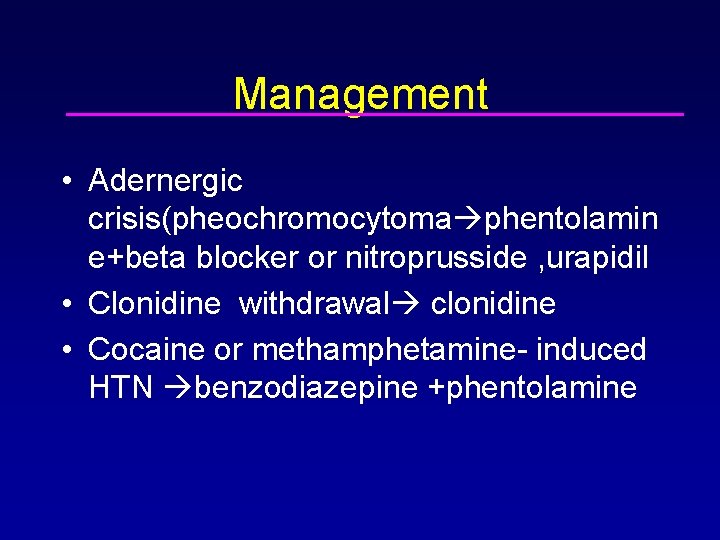
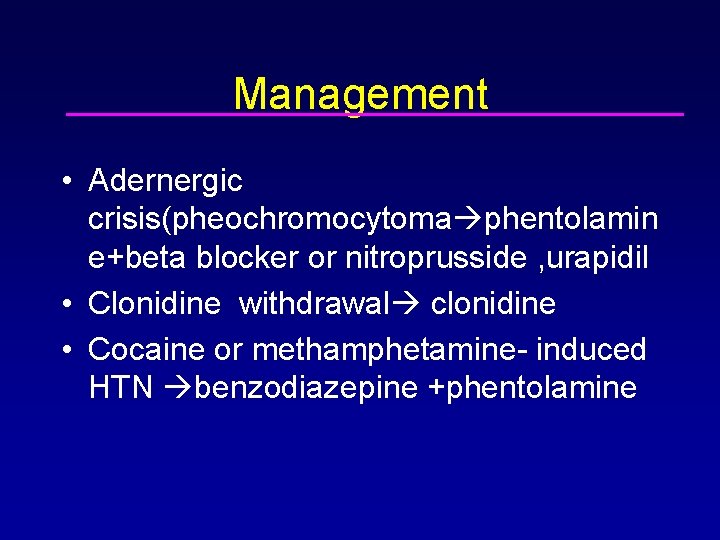
Management • Adernergic crisis(pheochromocytoma phentolamin e+beta blocker or nitroprusside , urapidil • Clonidine withdrawal clonidine • Cocaine or methamphetamine- induced HTN benzodiazepine +phentolamine
Aortic Dissection • Standard therapy – Beta-adrenergic blocker plus vasodilator – Esmolol + Nicardipine • Nitroprusside can be used as well
Management • Elevated BP without target organ damage • Hypertensive urgency • Oral meds • Goal - gradual reduction of BP over 24 48 hours


Thank you! Questions?
 The crises
The crises Meervoud crisis
Meervoud crisis Ongoing planning in nursing
Ongoing planning in nursing Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Objectives of nursing process
Objectives of nursing process Charting exercise chapter 28
Charting exercise chapter 28 Diagnosis and treatment planning in complete denture
Diagnosis and treatment planning in complete denture Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Oral diagnosis and treatment planning ppt
Oral diagnosis and treatment planning ppt Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Crao vs crvo
Crao vs crvo Urgency hypertension
Urgency hypertension Malignant hypertension treatment
Malignant hypertension treatment Hypertension urgency vs emergency
Hypertension urgency vs emergency Htn emergency vs urgency
Htn emergency vs urgency Case scenario for hypertension
Case scenario for hypertension Bonnet sign
Bonnet sign Périlimbique
Périlimbique Nursing interventions for thyroid storm
Nursing interventions for thyroid storm Hypertensive kardiopathie definition
Hypertensive kardiopathie definition Hypertensive uveitis
Hypertensive uveitis Anatomy blood vessels
Anatomy blood vessels Hypertensive emergency
Hypertensive emergency Increase bp
Increase bp Malignant hypertension
Malignant hypertension Hypertensive emergency
Hypertensive emergency Background
Background Power brake system
Power brake system Electronic suspension system
Electronic suspension system Chapter 42 gasoline injection diagnosis and repair
Chapter 42 gasoline injection diagnosis and repair Automotive technology principles diagnosis and service
Automotive technology principles diagnosis and service Community as client
Community as client Pedal reserve distance
Pedal reserve distance