UPDATE ON PREDICTION PREVENTION OF PREECLAMPSIA Assist Prof

- Slides: 117
UPDATE ON PREDICTION & PREVENTION OF PREECLAMPSIA Assist. Prof. S. Rouholamin
HYPERTENSION IN PREGNANCY
Etiology & Definition Complicates 10 -20% of pregnancies Elevation of BP ≥ 140 mm. Hg systolic and/or ≥ 90 mm. Hg diastolic, on two occasions at least 6 hours apart.
Categories Chronic Hypertension Gestational Hypertension Preeclampsia superimposed on Chronic Hypertension
Chronic Hypertension “Preexisting Hypertension” Definition Systolic pressure ≥ 140 mm. Hg, diastolic pressure ≥ 90 mm. Hg, or both. Presents before 20 th week of pregnancy or persists longer then 12 weeks postpartum. Causes Primary = “Essential Hypertension” Secondary = Result of other medical condition (ie: renal disease)
Prenatal Care for Chronic Hypertensives Electrocardiogram should be obtained in women with long-standing hypertension. Baseline laboratory tests Urinalysis, urine culture, and serum creatinine, glucose, and electrolytes Tests will rule out renal disease, and identify comorbidities such as diabetes mellitus. Women with proteinuria on a urine dipstick should have a quantitative test for urine protein.
Treatment for Chronic Hypertension Avoid treatment in women with uncomplicated mild essential HTN as blood pressure may decrease as pregnancy progresses. May taper or discontinue meds for women with blood pressures less than 120/80 in 1 st trimester. Reinstitute or initiate therapy for persistent diastolic pressures >95 mm. Hg, systolic pressures >150 mm. Hg, or signs of hypertensive end-organ damage. Medication choices = Oral methyldopa and labetalol.
Preeclampsia Definition = New onset of hypertension and proteinuria after 20 weeks gestation. Systolic blood pressure ≥ 140 mm. Hg OR diastolic blood pressure ≥ 90 mm. Hg Proteinuria of 0. 3 g or greater in a 24 -hour urine specimen Preeclampsia before 20 weeks, think MOLAR PREGNANCY! Categories Mild Preeclampsia Severe Preeclampsia Eclampsia Occurrence of generalized convulsion and/or coma in the setting of preeclampsia, with no other neurological condition.
Preeclampsia Severe Preeclampsia must have one of the following: Symptoms of central nervous system dysfunction = Blurred vision, scotomata, altered mental status, severe headache Symptoms of liver capsule distention = Right upper quadrant or epigastric pain Nausea, vomiting Hepatocellular injury = Serum transaminase concentration at least twice normal Systolic blood pressure ≥ 160 mm Hg or diastolic ≥ 110 mm Hg on two occasions at least six hours apart Thrombocytopenia = <100, 000 platelets per cubic milimeter Proteinuria = 5 or more grams in 24 hours Oliguria = <500 m. L in 24 hours Severe fetal growth restriction Pulmonary edema or cyanosis Cerebrovascular accident
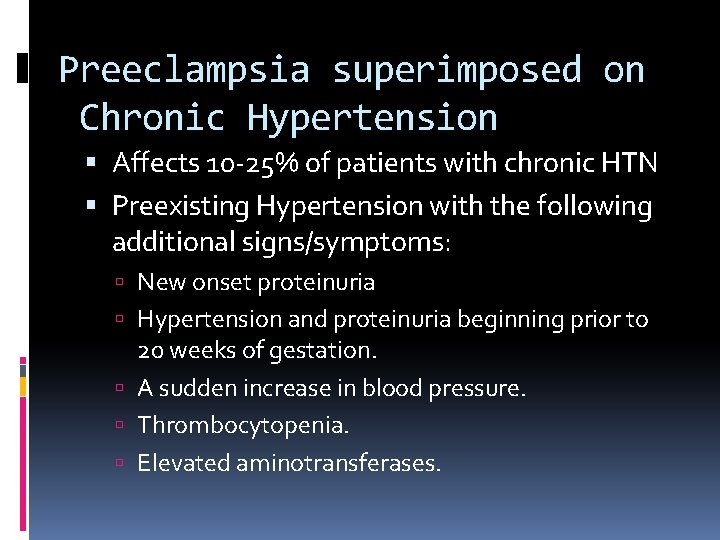
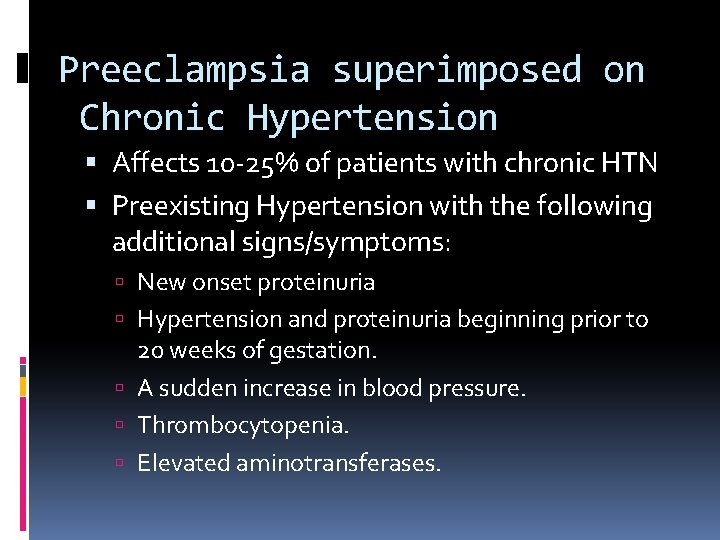
Preeclampsia superimposed on Chronic Hypertension Affects 10 -25% of patients with chronic HTN Preexisting Hypertension with the following additional signs/symptoms: New onset proteinuria Hypertension and proteinuria beginning prior to 20 weeks of gestation. A sudden increase in blood pressure. Thrombocytopenia. Elevated aminotransferases.
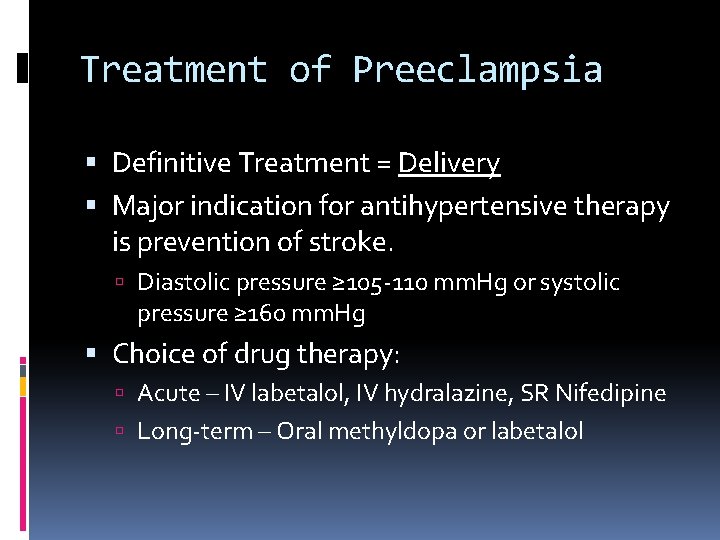
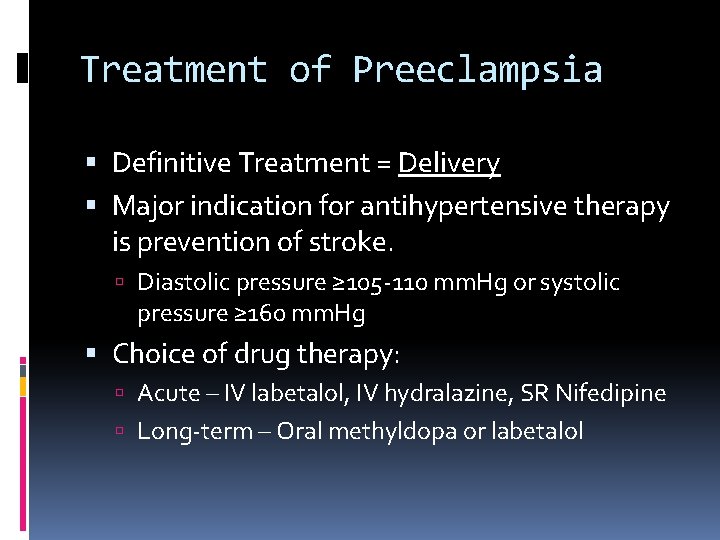
Treatment of Preeclampsia Definitive Treatment = Delivery Major indication for antihypertensive therapy is prevention of stroke. Diastolic pressure ≥ 105 -110 mm. Hg or systolic pressure ≥ 160 mm. Hg Choice of drug therapy: Acute – IV labetalol, IV hydralazine, SR Nifedipine Long-term – Oral methyldopa or labetalol
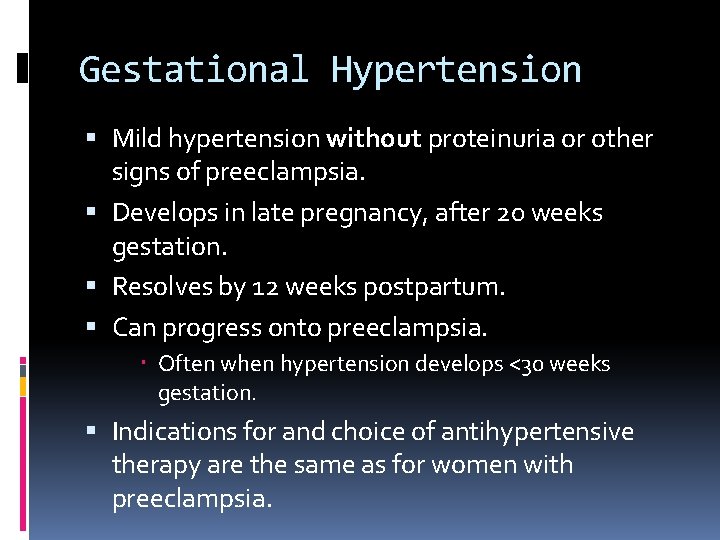
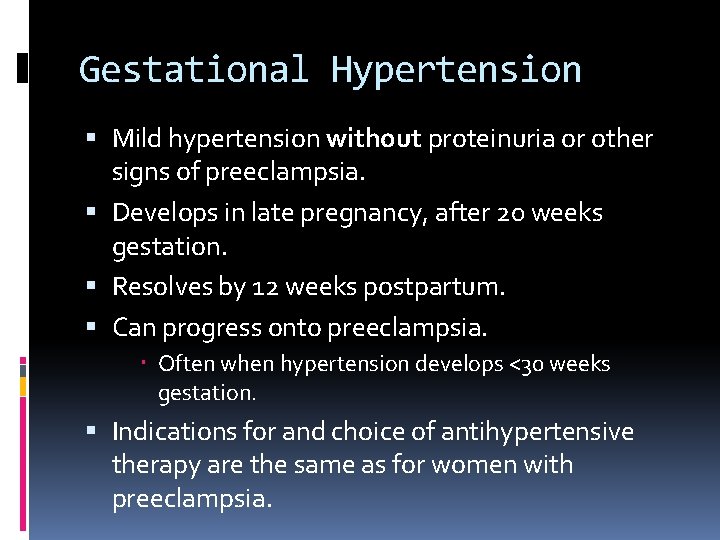
Gestational Hypertension Mild hypertension without proteinuria or other signs of preeclampsia. Develops in late pregnancy, after 20 weeks gestation. Resolves by 12 weeks postpartum. Can progress onto preeclampsia. Often when hypertension develops <30 weeks gestation. Indications for and choice of antihypertensive therapy are the same as for women with preeclampsia.
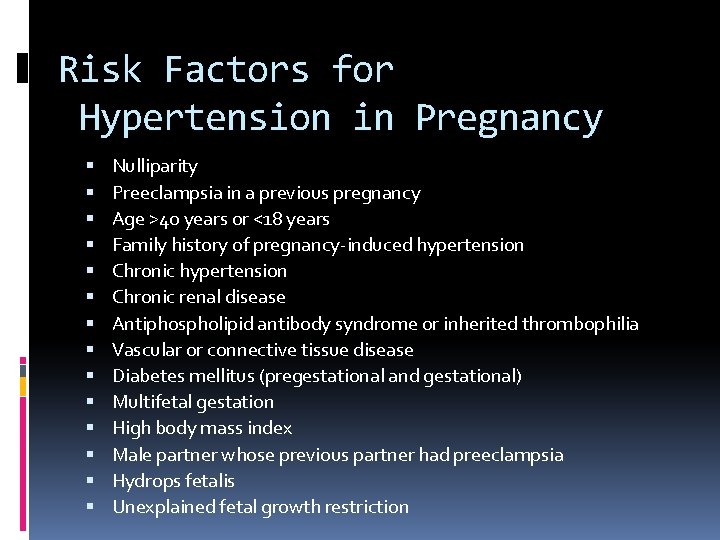
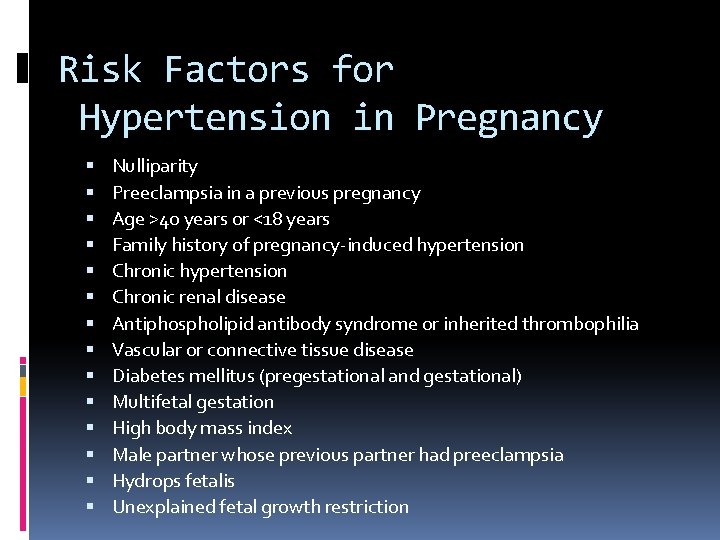
Risk Factors for Hypertension in Pregnancy Nulliparity Preeclampsia in a previous pregnancy Age >40 years or <18 years Family history of pregnancy-induced hypertension Chronic renal disease Antiphospholipid antibody syndrome or inherited thrombophilia Vascular or connective tissue disease Diabetes mellitus (pregestational and gestational) Multifetal gestation High body mass index Male partner whose previous partner had preeclampsia Hydrops fetalis Unexplained fetal growth restriction
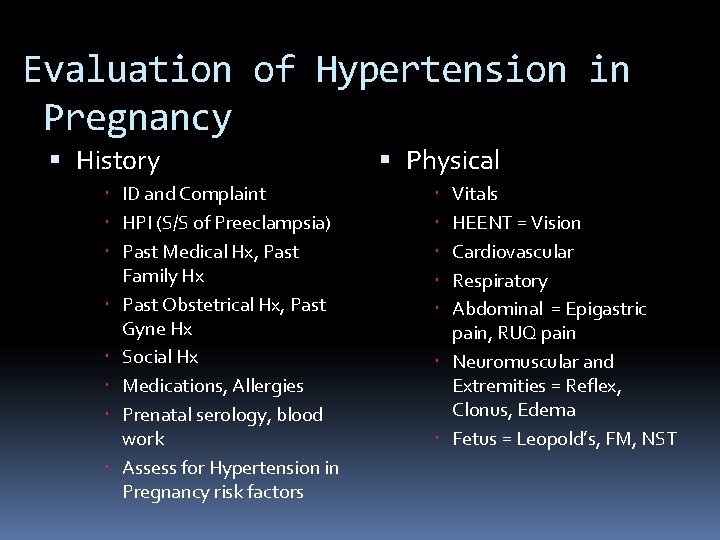
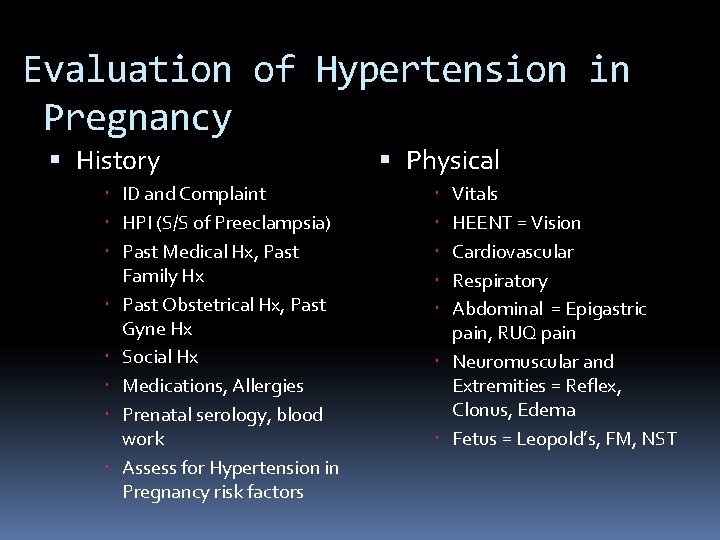
Evaluation of Hypertension in Pregnancy History ID and Complaint HPI (S/S of Preeclampsia) Past Medical Hx, Past Family Hx Past Obstetrical Hx, Past Gyne Hx Social Hx Medications, Allergies Prenatal serology, blood work Assess for Hypertension in Pregnancy risk factors Physical Vitals HEENT = Vision Cardiovascular Respiratory Abdominal = Epigastric pain, RUQ pain Neuromuscular and Extremities = Reflex, Clonus, Edema Fetus = Leopold’s, FM, NST
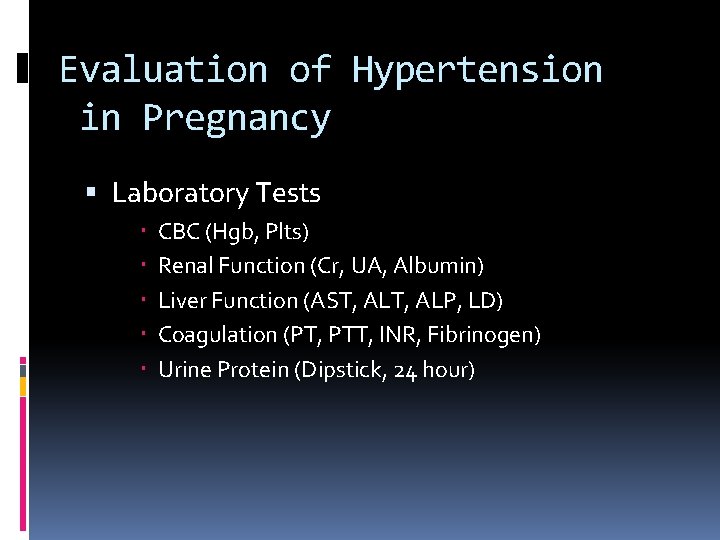
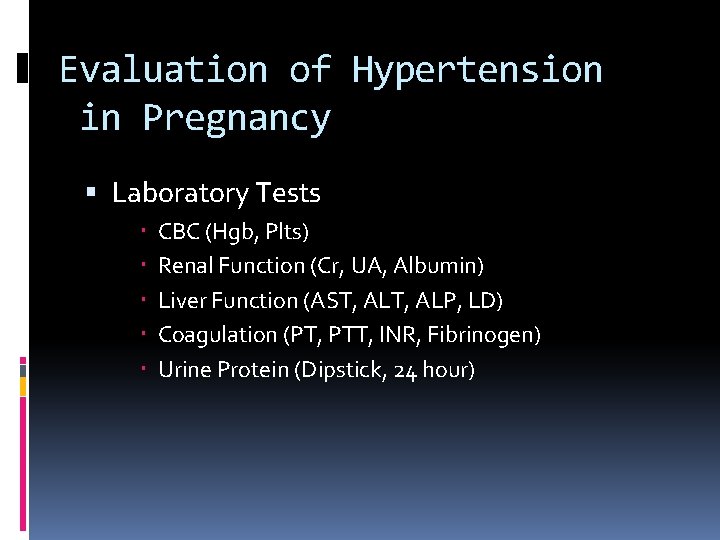
Evaluation of Hypertension in Pregnancy Laboratory Tests CBC (Hgb, Plts) Renal Function (Cr, UA, Albumin) Liver Function (AST, ALP, LD) Coagulation (PT, PTT, INR, Fibrinogen) Urine Protein (Dipstick, 24 hour)
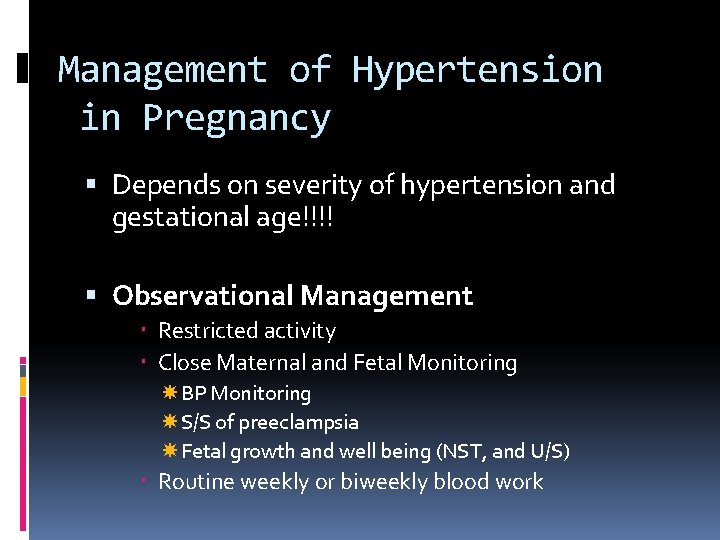
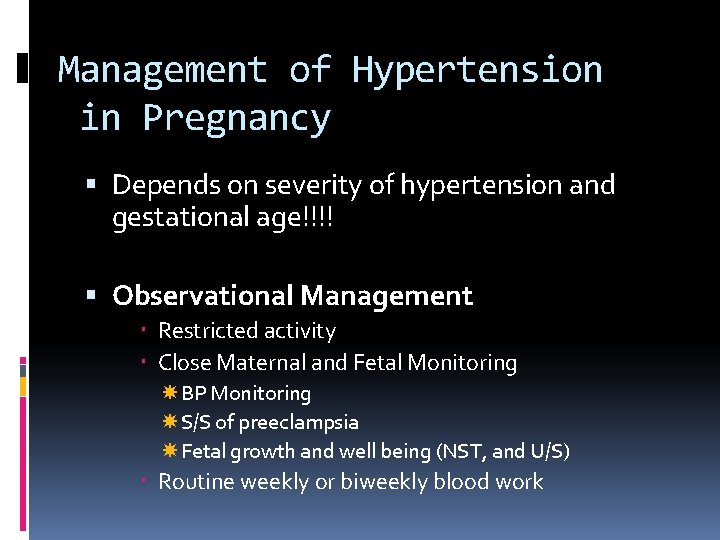
Management of Hypertension in Pregnancy Depends on severity of hypertension and gestational age!!!! Observational Management Restricted activity Close Maternal and Fetal Monitoring BP Monitoring S/S of preeclampsia Fetal growth and well being (NST, and U/S) Routine weekly or biweekly blood work
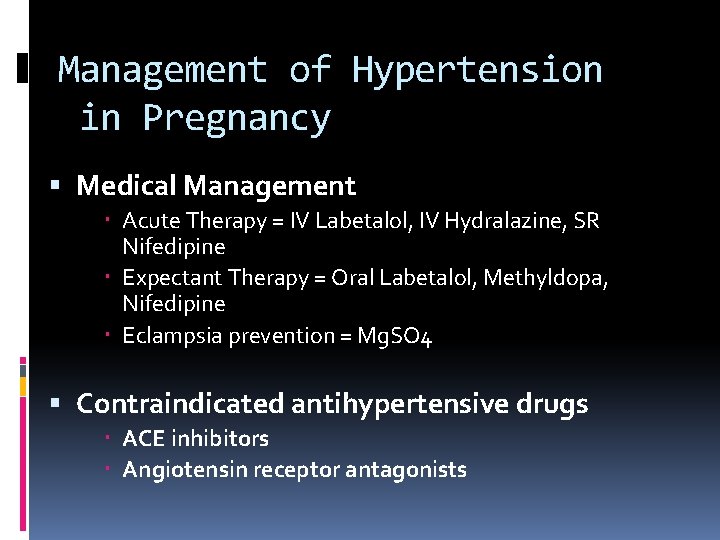
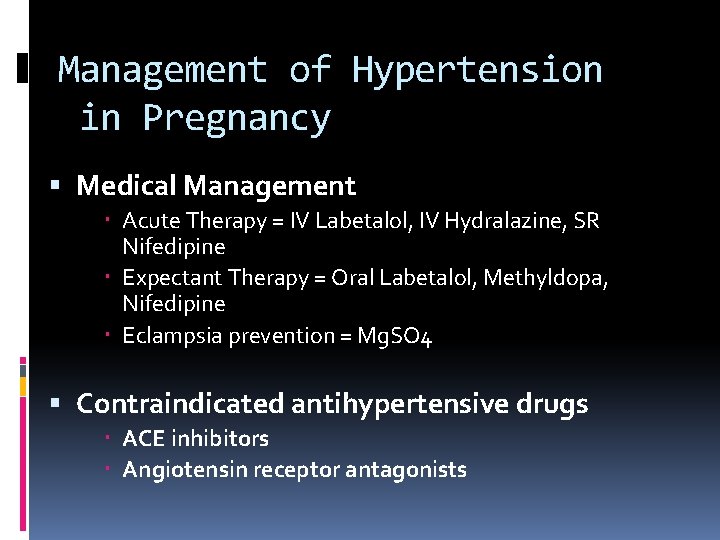
Management of Hypertension in Pregnancy Medical Management Acute Therapy = IV Labetalol, IV Hydralazine, SR Nifedipine Expectant Therapy = Oral Labetalol, Methyldopa, Nifedipine Eclampsia prevention = Mg. SO 4 Contraindicated antihypertensive drugs ACE inhibitors Angiotensin receptor antagonists
Management of Hypertension in Pregnancy Proceed with Delivery Vaginal Delivery VS Cesarean Section Depends on severity of hypertension! May need to administer antenatal corticosteroids depending on gestation! Only cure is DELIVERY!!!
• Prediction: Routine urine analysis • Prevention: Chocolate
Outline Introduction Prediction Prevention
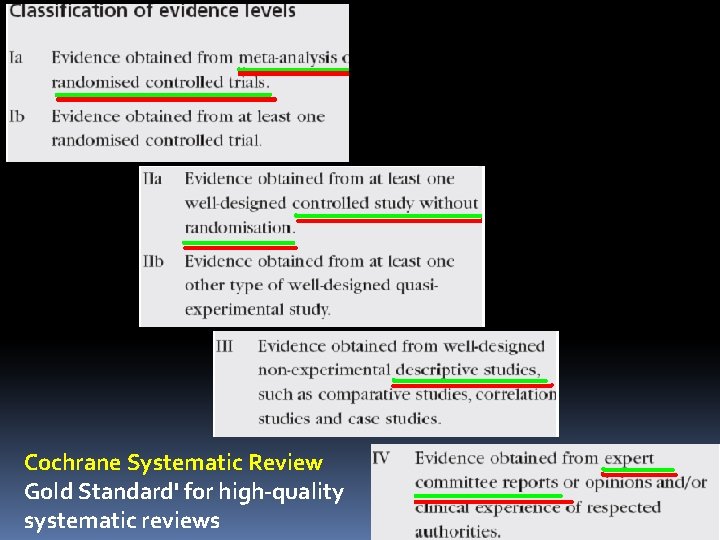
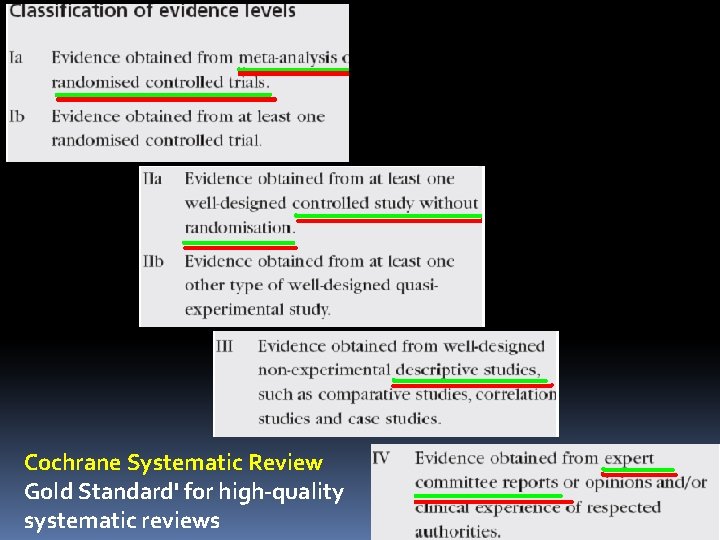
Cochrane Systematic Review Gold Standard' for high-quality systematic reviews
• Preeclampsia: Hypertension associated with proteinuria.
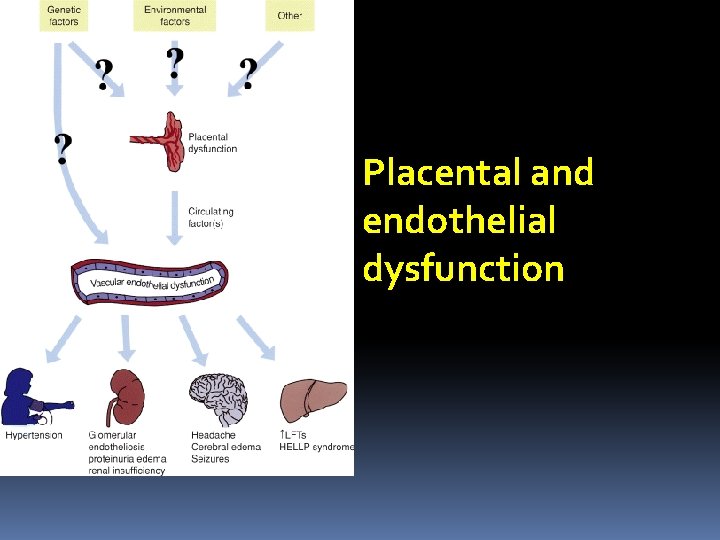
• Pathogenesis: • unknown (Barton& Sibai, 2008). ØImpaired trophoblast differentiation& invasion ØPlacental & endothelial dysfunction ØImmune maladaptation to paternal Ags ØExaggerated systemic inflam response.
• Pathogenesis: • Differs with various risk factors: PG Vs MG with previous PE preexisting vas dis preexisting DM or multifetal gestation.
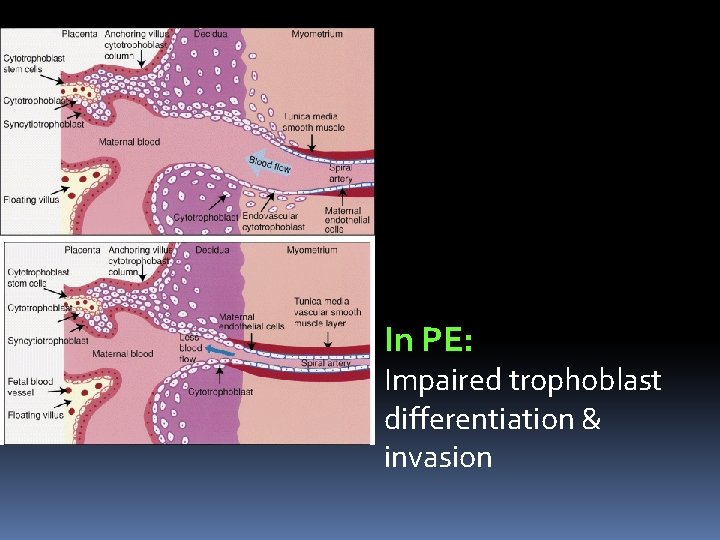
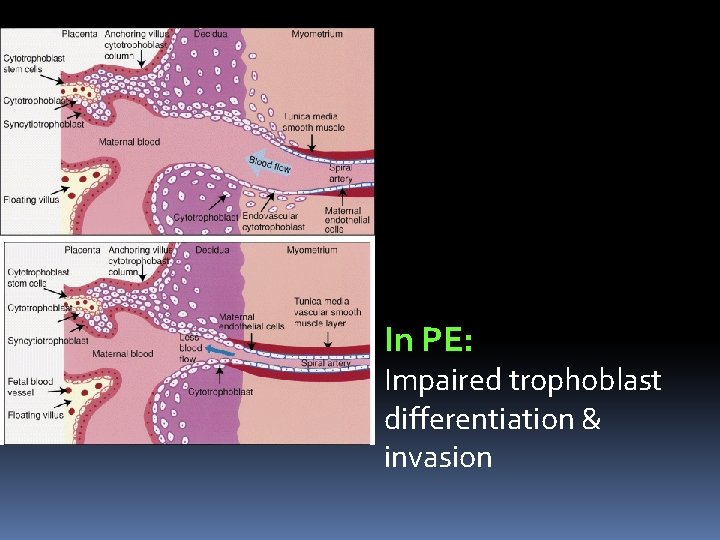
In PE: Impaired trophoblast differentiation & invasion
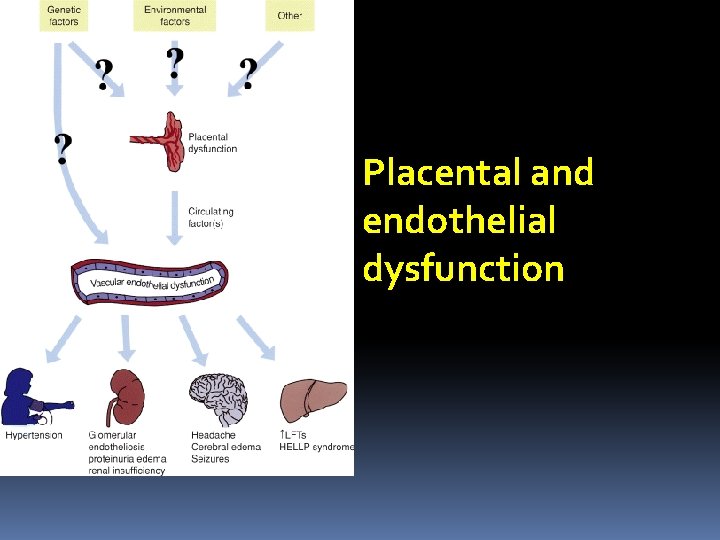
Placental and endothelial dysfunction
PREDICTION OF PE • Why prediction is important? • The ideal screening test • Methods I. Preconception factors II. Pregnancy-Related Factors 1. Risk factors 2. Markers
Why prediction is important: 1. The risk for recurrent PE can be as high as 65% (Barton& Sibai, 2008). 2. PE is associated with substantial maternal& perinatal complications
The ideal Screening test: Simple Noninvasive Rapid Inexpensive Easy to perform early in pregnancy Highly sensitivity & predictive.
I. Preconception factors st 1 step in the management of a woman with a history of PE is to conduct a detailed evaluation of potential risk factors (Barton& Sibai, 2008).
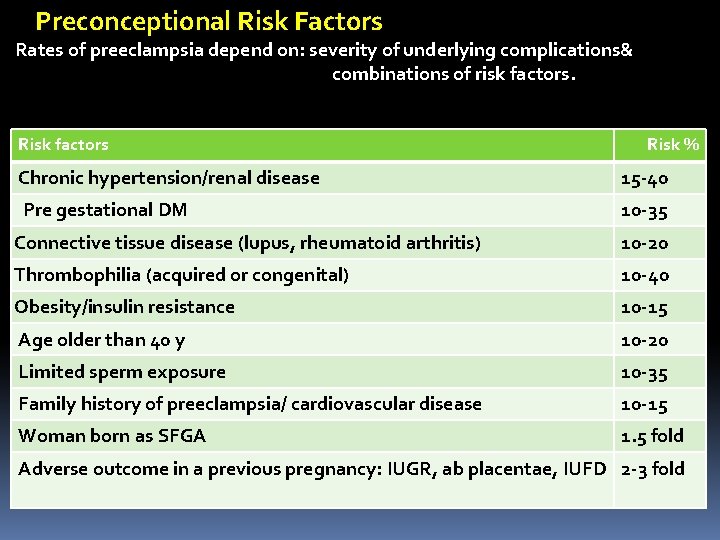
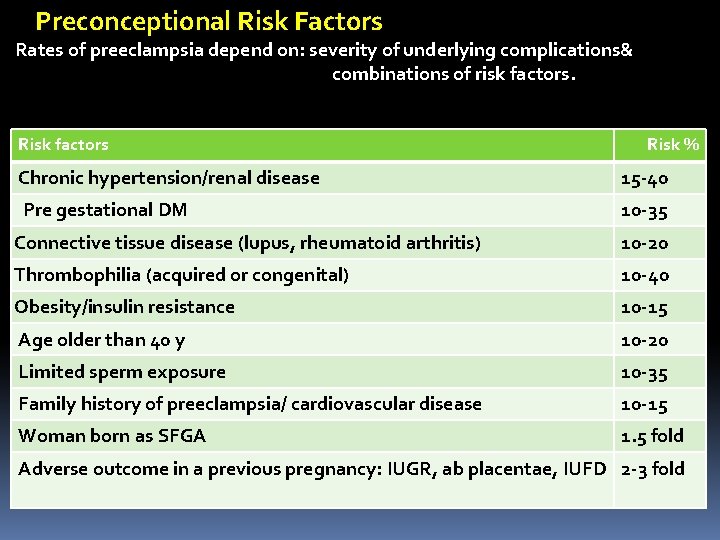
Preconceptional Risk Factors Rates of preeclampsia depend on: severity of underlying complications& combinations of risk factors. Risk factors Risk % Chronic hypertension/renal disease 15 -40 Pre gestational DM 10 -35 Connective tissue disease (lupus, rheumatoid arthritis) 10 -20 Thrombophilia (acquired or congenital) 10 -40 Obesity/insulin resistance 10 -15 Age older than 40 y 10 -20 Limited sperm exposure 10 -35 Family history of preeclampsia/ cardiovascular disease 10 -15 Woman born as SFGA 1. 5 fold Adverse outcome in a previous pregnancy: IUGR, ab placentae, IUFD 2 -3 fold
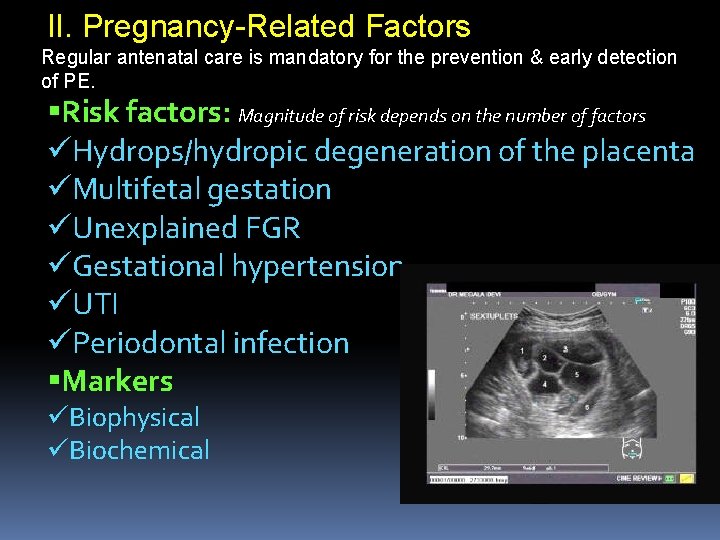
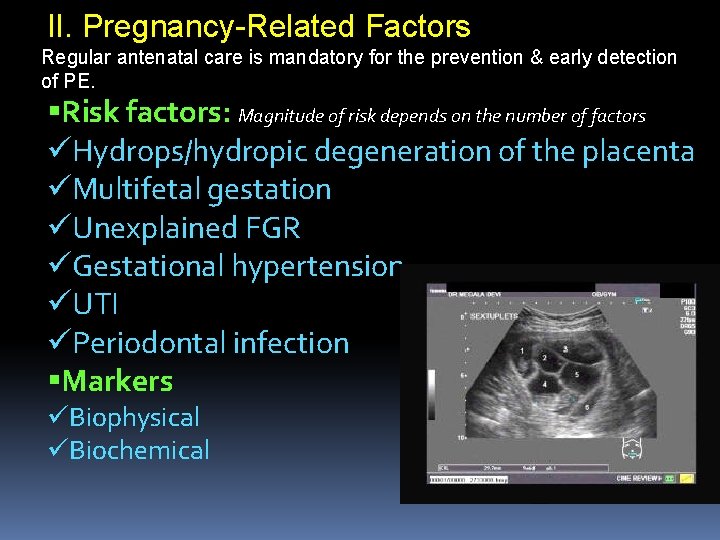
II. Pregnancy-Related Factors Regular antenatal care is mandatory for the prevention & early detection of PE. Risk factors: Magnitude of risk depends on the number of factors üHydrops/hydropic degeneration of the placenta üMultifetal gestation üUnexplained FGR üGestational hypertension üUTI üPeriodontal infection Markers üBiophysical üBiochemical
Markers üMany üBased on: pathophysiological abnormalities
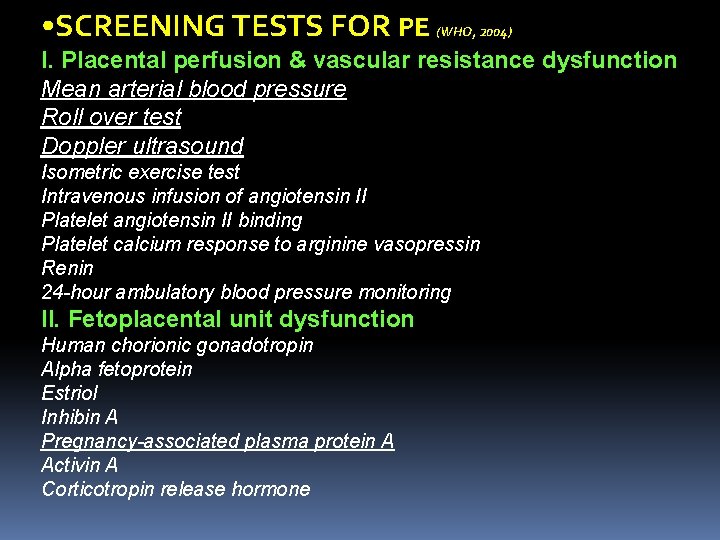
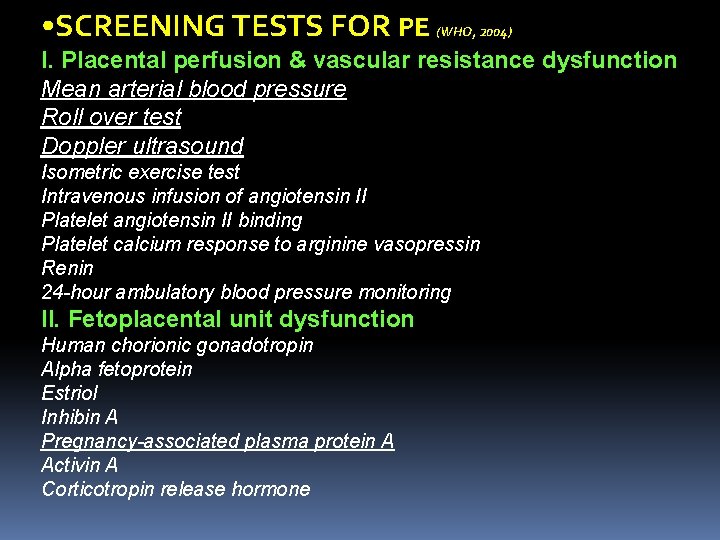
• SCREENING TESTS FOR PE (WHO, 2004) I. Placental perfusion & vascular resistance dysfunction Mean arterial blood pressure Roll over test Doppler ultrasound Isometric exercise test Intravenous infusion of angiotensin II Platelet angiotensin II binding Platelet calcium response to arginine vasopressin Renin 24 -hour ambulatory blood pressure monitoring II. Fetoplacental unit dysfunction Human chorionic gonadotropin Alpha fetoprotein Estriol Inhibin A Pregnancy-associated plasma protein A Activin A Corticotropin release hormone
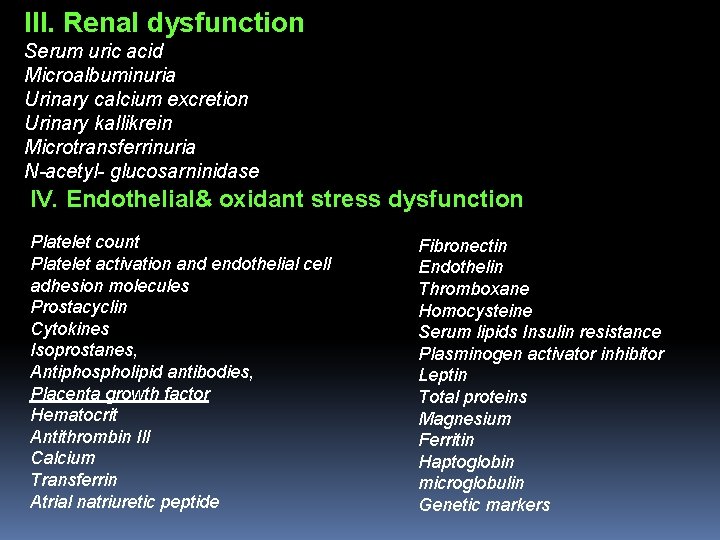
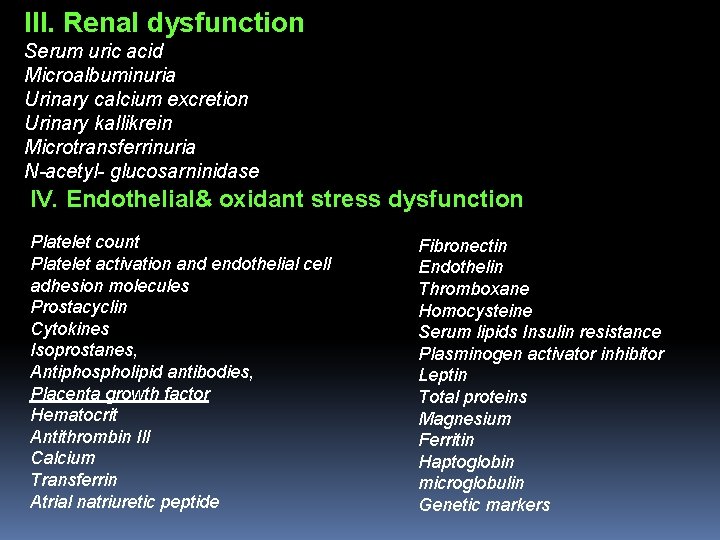
III. Renal dysfunction Serum uric acid Microalbuminuria Urinary calcium excretion Urinary kallikrein Microtransferrinuria N-acetyl- glucosarninidase IV. Endothelial& oxidant stress dysfunction Platelet count Platelet activation and endothelial cell adhesion molecules Prostacyclin Cytokines Isoprostanes, Antiphospholipid antibodies, Placenta growth factor Hematocrit Antithrombin Ill Calcium Transferrin Atrial natriuretic peptide Fibronectin Endothelin Thromboxane Homocysteine Serum lipids Insulin resistance Plasminogen activator inhibitor Leptin Total proteins Magnesium Ferritin Haptoglobin microglobulin Genetic markers
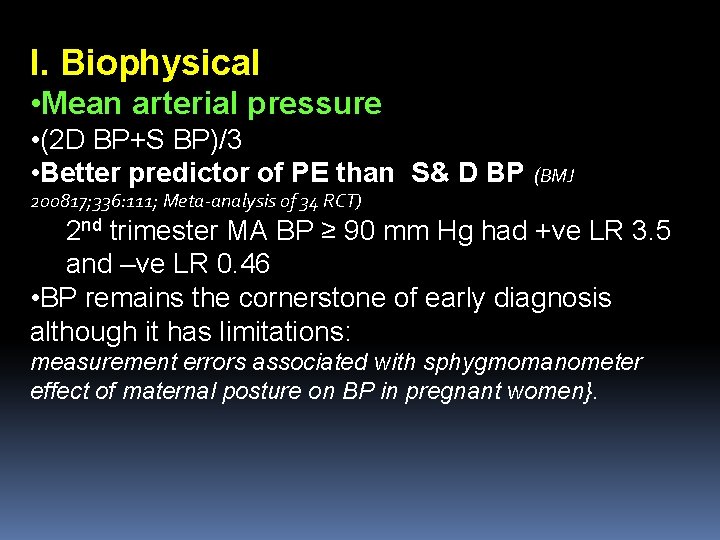
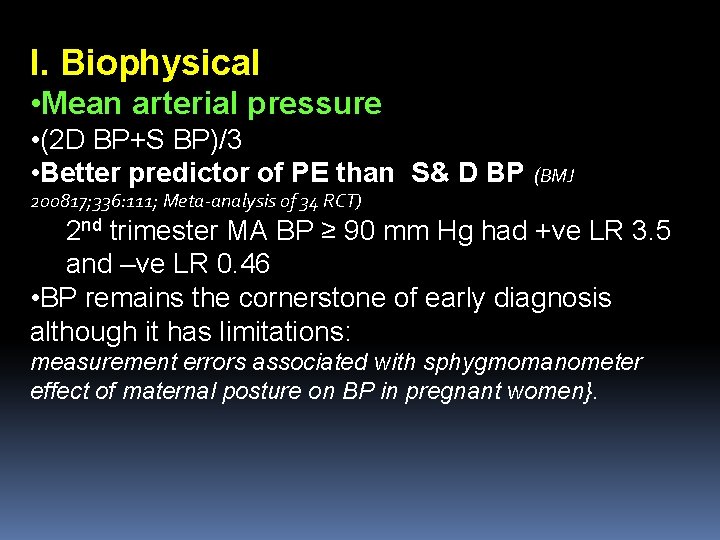
I. Biophysical • Mean arterial pressure • (2 D BP+S BP)/3 • Better predictor of PE than S& D BP (BMJ 200817; 336: 111; Meta-analysis of 34 RCT) 2 nd trimester MA BP ≥ 90 mm Hg had +ve LR 3. 5 and –ve LR 0. 46 • BP remains the cornerstone of early diagnosis although it has limitations: measurement errors associated with sphygmomanometer effect of maternal posture on BP in pregnant women}.
• Repeated routine urinalysis throughout pregnancy NOT useful for predicting PE (JAMA 2003: 12; 289(10): 1220)
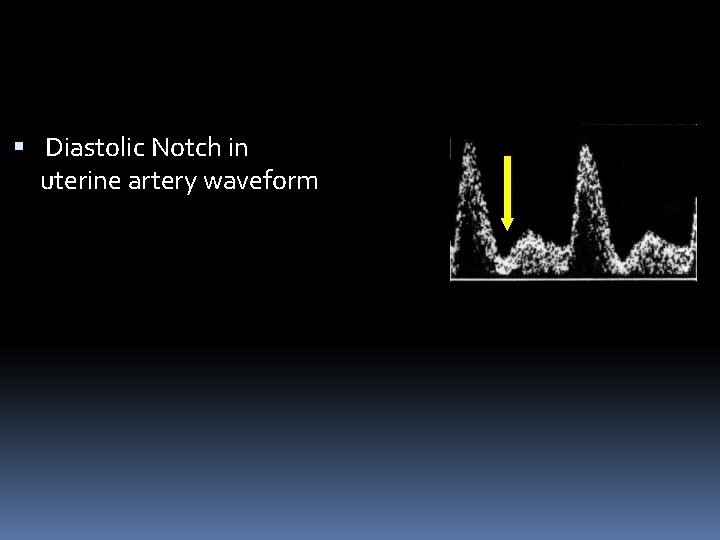
Uterine artery Doppler ultrasound • {impaired trophoblastic invasion of the spiral arteries: reduction in uteroplacental blood flow} • High pulsatility index and/or Notch in 1 st & 2 nd trimesters: poor predictor of PE(Papgeorghiou & Leslie, 2007) Uterine artery Doppler plus biochemical markers • Promising results • Current data do not support this combination for routine screening for PE (Barton& Sibai, 2008).
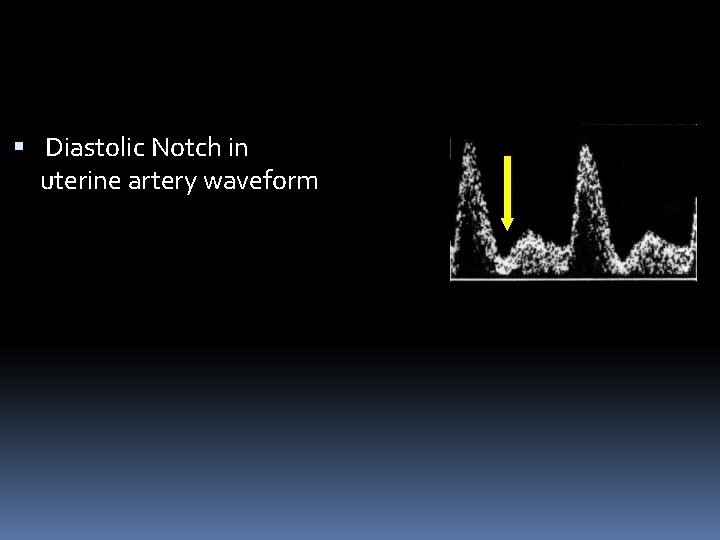
Diastolic Notch in uterine artery waveform
The Roll over test Not of value in predicting PE
II. Biochemical Markers Angiogenic factors before & after the onset of PE (Barton& Sibai, 2008). Serum placental growth factor: reduced Soluble fms-like tyrosine kinase: elevated Endoglin: elevated
Conclusion • BP remains the cornerstone of early diagnosis • Markers Reliability is inconsistent Many suffer from poor specificity & predictive values. None provided a cutoff value that could be clinically useful for the prediction of PE (Widmer et al, 2007).
• Currently: There is no clinically useful screening test to predict PE (WHO, 2004)
Prevention of PE Primary Secondary
Primary prevention • Avoiding occurrence of the disease • Obese: achieve an ideal b wt before conception (Villamor& Cnattingius, 2006) No RCT • Ch hypertension: Control BP before conception. No RCT
• Pregestational DM: -Complete her family as early as possible & before vascular complications develop -Control DM before conception & throughout pregnancy
Secondary • Breaking off the disease process before emergence of obvious clinical disease • {Etiology of the disease is unknown} • To correct theoretical pathophysiology • I. Non pharmacological II. Nutritional III. Pharmacological
I. Non pharmacological 1. Daily Bed rest Rest for 4 -6 h/d May reduce risk of PE for women with normal BP (level 2 evidence) (Cochrane Library 2006 Issue 2: CD 005939)
2. Life-style changes • High job stress: greater risk of PE(Sharma& Mittal, 2006) • Reducing job stress may be beneficial in the prevention of PE
3. Regular prenatal exercise • May prevent or oppose progression (Weissgerber et al, 2004) • {Stimulation of placental growth Reduction of oxidative stress Reversal of maternal endothelial dysfunction}. • Insufficient evidence Moderate intensity regular aerobic exercise (Cochrane Library 2006 Issue 2: CD 005942) Aerobic exercise =cardiovascular exercise=any sustained rhythmic activity that involves large muscle groups: makes the lungs work harder as the body's need for oxygen is increased.
• Stretching exercises are more effective at reducing the risk of PE than walking (University of North Carolina, 2008)
Smoking: Reduced risk for PE (Sibai et al, 2005). {Nicotine inhibition of interleukin-2 & tumor necrosis factor Effects of nicotine on angiogenic proteins}. Smoking: abnormal fetal growth preterm birth Abruption Adverse effects on maternal health.
II. Nutritional 1. Higher total dietary fiber intake in early pregnancy may reduce risk for PE (level 2 evidence) Prospective cohort study Am J Hypertens 2008 Aug; 21(8): 903
2. Increasing dietary protein & energy intake RCT: no benefit • 5 or more servings of chocolate/w in 3 rd trimester: 40% reduction (Triche, 2008; Epidemiology. 19: 459 -464), Yale University {Chocolate, especially dark chocolate, is rich in theobromine: stimulates the heart, relaxes smooth muscle & dilates blood vessels, and has been used to treat chest pain, high blood pressure}
3. Garlic Insufficient evidence to recommend for preventing PE Cochrane Library 2006 Issue 3: CD 006065)
4. Dietary sodium restriction • No significant differences (Cochrane Library 2005 Issue 4: CD 005548)
6. Fish Oil Supplementation • Observational studies: beneficial effects • {inhibition of platelet thromboxane A 2 without affecting prostacyclin: shifting the balance toward a reduced platelet aggregation and increased VD}. • RCT: No benefit (Olsen et al, 2000) • High doses: increase the risk of PIH (Olafasdottir et al, 2006). • Not recommended for the prevention of PE
5. Weight Reduction • Although obesity is a known risk factor, there is no evidence that limiting wt gain during pregnancy; reduces its occurrence. • Wt reduction is not recommended during pregnancy even in obese women (Kramer, 2004)
III. Pharmacological 1. Low-dose Aspirin • {inhibits biosynthesis of platelet thromboxane A 2 with little effect on vascular prostacyclin production: altering the balance in favor of prostacyclin}. • (50 -150 mg/day) For women with a previous history of hypertension or PE (n=6, 107): Small to moderate benefits, safe. level 2 evidence (Cochrane Library 2007 Issue 2: CD 004659)
2. Low-dose Aspirin/Heparin • History of severe preterm PE & LBW infants. (Sergio et al, 2006) • Lower incidence of PE (3 Vs 30%) Greater gestational age at delivery Higher birth wt
3. Calcium Supplementation • Reduces the risk of PIH, particularly in populations that have diets deficient in calcium level 1 evidence (Cochrane Syt review , 2006) • The relationship between cal & risk of PIH is inconsistent& inconclusive The relationship between cal & the risk of PE is highly unlikely. Evidence-based review by FDA (2007)
4. Antihypertensive Drugs • Mild to moderate hypertension: Halving in the risk of developing severe hypertension No difference in the risk of developing PE or proteinuria (Cochrane syst review, 2007)
5. Diuretics • No reduction in the incidence of PE or perinatal mortality • May have deleterious effects: reduced renal & placental perfusion. (Cochrane Library 2007 Issue 1: CD 004451)
6. Antioxidant supplementation may not affect risk of PE or clinical outcomes level 2 evidence (Cochrane Library 2008 Issue 1: CD 004227)
7. Concomitant Vit C& E supplementation • {PET: imbalance of oxidant & antioxidant activity: multiorgan endothelial dysfunction}. • Vit C (1, 000 mg/d) plus vit E (400 IU/ d) • Did not prevent PE level 2 evidence (Obstet Gynecol 2007 Dec; 110(6): 1311) • May increases rate of LBW infants& might be associated with higher rate of SB level 2 evidence (Lancet 2006 Apr 8; 367(9517): 1145
8. Magnesium • {Mg is beneficial for the prevention & tt of severe PE & E Decreased intracellular Mg in PE} • No effect • (365 mg& 500 mg). Cochrane syst review, 2004
9. Folic acid& other B-vits • {Deficiency of vit B 2 may cause biochemical changes simulating abnormalities of PE} • No evidence that any of B vits can prevent PE (Shrama& Mittal, 2006).
10. Zinc supplementation • {Zinc concentrations are reduced in PE} • RCT: No benefit (Jonsson et al, 1996)
11. Nitric oxide Insufficient evidence for preventing PE Cochrane Library 2007 Issue 2: CD 006490
12. Progesterone Insufficient evidence for preventing PE Cochrane review, 2006
Conclusion Regular antenatal care is mandatory for the prevention & early detection of PE. For prevention of PE Bed rest Reduction of job stress High dietary fiber intake Low dose aspirin/heparin Ca supplementation

PREECLAMPSIA
PREECLAMPSIA Hypertensive disorder specific to pregnancy affects nearly 6% of all pregnancies a major cause of maternal and neonatal mortality and morbidity 15 to 20 % of maternal mortality in developed countries
PREECLAMPSIA Severity ranges from: a mild disorder (transient hypertension in the later part of the pregnancy) to a life-threatening disorder with seizures, HELLP syndrome, fetal hypoxia, and growth retardation more severe disease: 0. 56 per 1000 deliveries
PREECLAMPSIA Predisposes women to other serious complications: placental abruption acute renal failure cerebral hemorrhage disseminated intravascular coagulation circulatory collapse
PREECLAMPSIA The etiology is unknown believed to be involved: immune maladaptation placental ischemia oxidative stress genetic susceptibility
PREECLAMPSIA Classification of hypertension in pregnancy Gestational hypertension Preeclampsia / eclampsia Chronic hypertension Preeclampsia superimposed on chronic hypertension
PREECLAMPSIA Definition of hypertension a systolic blood pressure of 140 mm. Hg or above, or a diastolic blood pressure of 90 mm. Hg or above, on two occasions 6 hours apart Abnormal proteinuria the excretion of 300 mg or more of protein in 24 hours
PREECLAMPSIA Criteria for severe preeclampsia Blood pressure: > 160 mm. Hg systolic or > 110 mm Hg diastolic Proteinuria: > 5 g in 24 hours Persistent and severe cerebral or visual disturbances (headache, scotoma, blurred vision) Persistent and severe epigastric pain or right upper quadrant pain
PREECLAMPSIA Criteria for severe preeclampsia Pulmonary edema or cyanosis Oliguria (< 500 m. L of urine in 24 hours) Eclampsia (grand mal seizures) HELLP syndrome
PREECLAMPSIA Screening tests for gestational hypertension routine components of antepartum care trimester early detection of vasoconstriction early detection of altered renal function early detection of altered hemodynamics detection of placental hypoperfusion / ischemia detection of endothelial activation or injury detection of an activated coagulation / fibrinolytic system
PREECLAMPSIA Prevention of preeclampsia women at risk: multifetal gestation, vascular or renal disease, previous severe preeclampsia-eclampsia, abnormal uterine artery Doppler velocimetry antihypertensive drugs magnesium zinc fish oil calcium low-dose aspirin
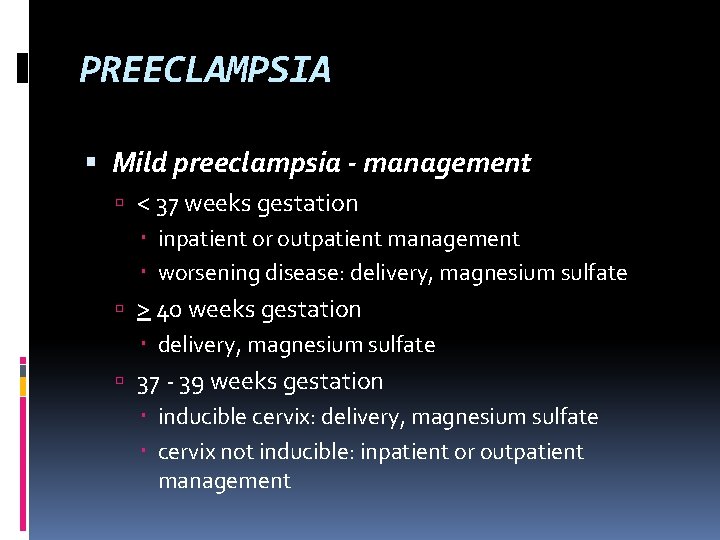
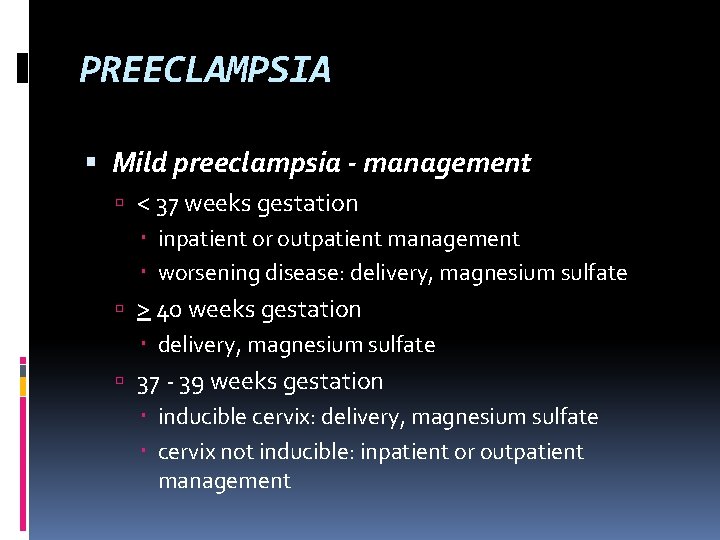
PREECLAMPSIA Mild preeclampsia - management < 37 weeks gestation inpatient or outpatient management worsening disease: delivery, magnesium sulfate > 40 weeks gestation delivery, magnesium sulfate 37 - 39 weeks gestation inducible cervix: delivery, magnesium sulfate cervix not inducible: inpatient or outpatient management
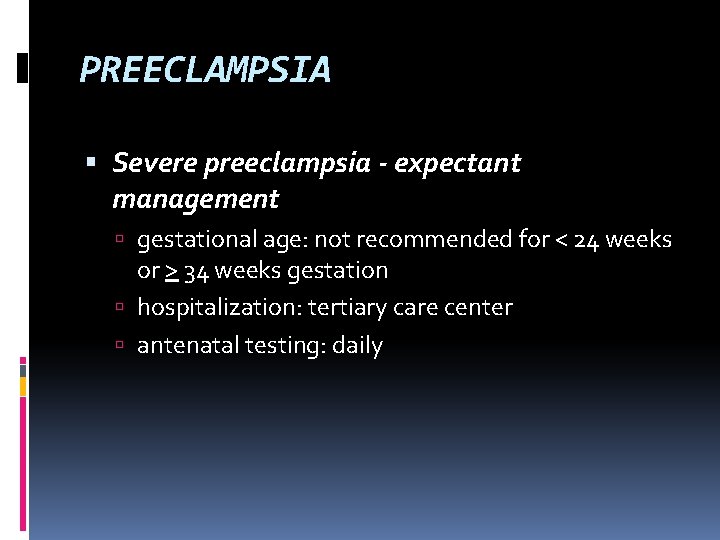
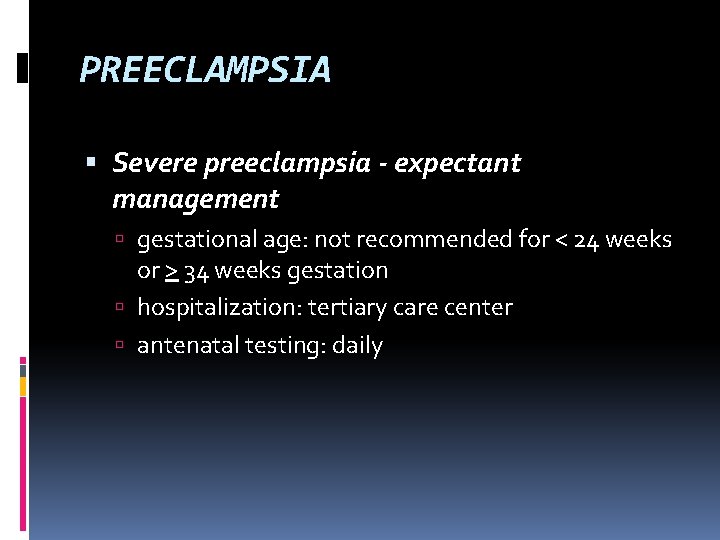
PREECLAMPSIA Severe preeclampsia - expectant management gestational age: not recommended for < 24 weeks or > 34 weeks gestation hospitalization: tertiary care center antenatal testing: daily
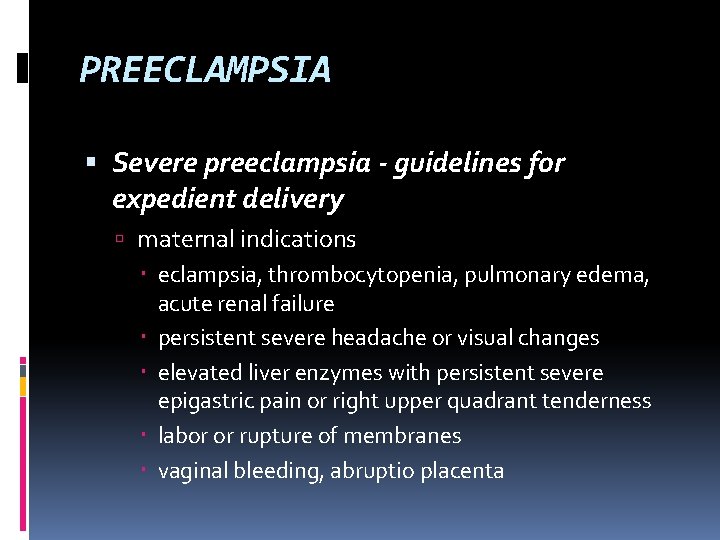
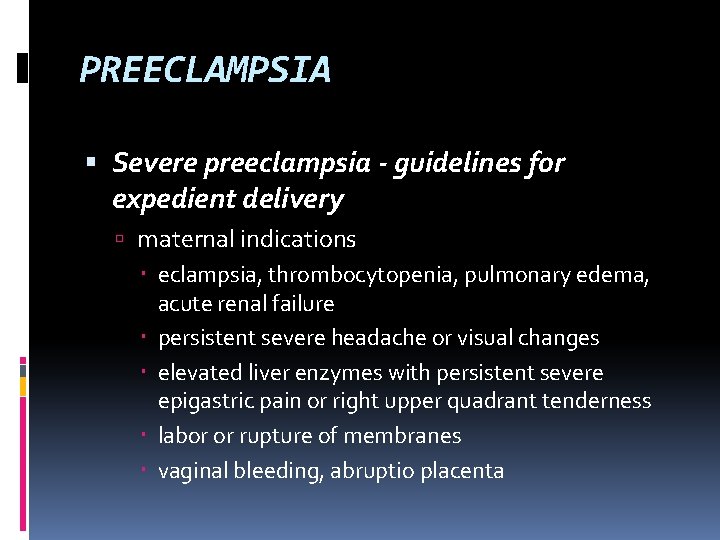
PREECLAMPSIA Severe preeclampsia - guidelines for expedient delivery maternal indications eclampsia, thrombocytopenia, pulmonary edema, acute renal failure persistent severe headache or visual changes elevated liver enzymes with persistent severe epigastric pain or right upper quadrant tenderness labor or rupture of membranes vaginal bleeding, abruptio placenta
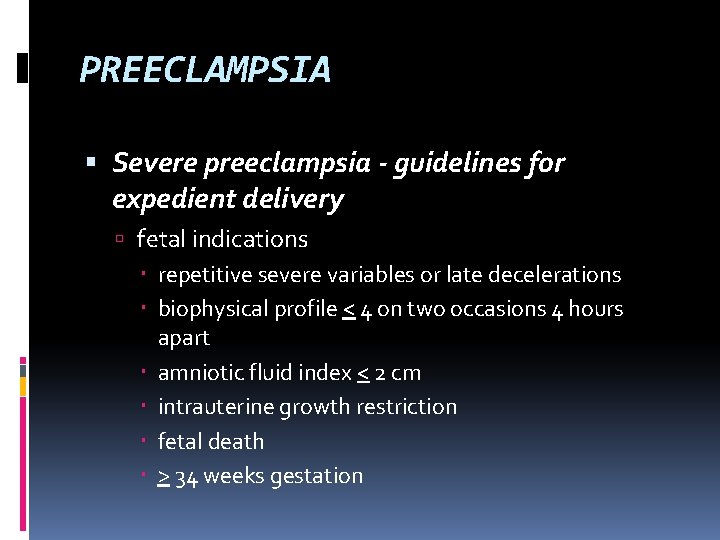
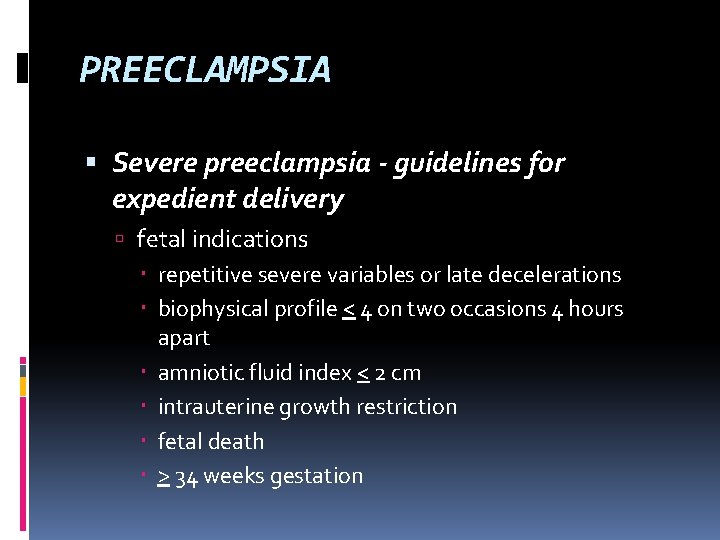
PREECLAMPSIA Severe preeclampsia - guidelines for expedient delivery fetal indications repetitive severe variables or late decelerations biophysical profile < 4 on two occasions 4 hours apart amniotic fluid index < 2 cm intrauterine growth restriction fetal death > 34 weeks gestation
PREECLAMPSIA Severe preeclampsia - management protocol admission to labor and delivery for 24 hours magnesium sulfate IV for 24 hours antihypertensives if diastolic blood pressure 110 mm. Hg meet guidelines for expedited delivery? yes? delivery >
PREECLAMPSIA Severe preeclampsia - management protocol Expedited delivery? no? < 23 weeks: counseling for termination of pregnancy 23 -32 weeks: steroids, antihypertensive medications, daily maternal and fetal evaluation, delivery at 34 weeks 32 -33 weeks: amniocentesis immature fluid - steroids, delivery in 48 hours
PREECLAMPSIA HELLP syndrome - diagnosis 10% before 27 weeks 20% after 37 weeks 70% between 27 and 37 weeks slow initial phase with accelerated final phase versus secondary expression of sepsis, ARDS, renal failure
PREECLAMPSIA HELLP syndrome parameters used to diagnose preeclampsia are not reflective of disease severity target organ systems liver brain kidneys coagulation system increased maternal and perinatal risk
PREECLAMPSIA HELLP syndrome - diagnostic criteria hemolysis abnormal peripheral smear lactate dehydrogenase > 600 U/L elevated liver enzymes serum aspartate aminotransferase > 70 U/L lactate dehydrogenase > 600 U/L low platelets platelet count < 100, 000/mm 3
PREECLAMPSIA HELLP syndrome - differential diagnosis acute fatty liver of pregnancy appendicitis diabetes insipidus gallbladder disease gastroenteritis glomerulonephritis hemolytic uremic syndrome hepatic encephalopathy
PREECLAMPSIA HELLP syndrome - differential diagnosis idiopathic thrombocytopenia kidney stones pancreatitis pyelonephritis systemic lupus erythematosus thrombotic thrombocytopenia purpura viral hepatitis
PREECLAMPSIA HELLP syndrome - antepartum management assess and stabilize the maternal condition correct coagulopathy if DIC is present give intravenous magnesium sulfate to prevent seizures provide treatment for severe hypertension to prevent stroke transfer to tertiary center if appropriate if subcapsular hematoma of liver, computed tomography or ultrasound of the abdomen
PREECLAMPSIA HELLP syndrome - antepartum management evaluate fetal well-being non stress test biophysical profile timing of delivery if > 34 weeks gestation, deliver if < 34 weeks gestation, administer corticosteroids, then deliver in 48 hours
PREECLAMPSIA HELLP syndrome - management for cesarean birth use general anesthesia if platelet count is < 75, 000 / mm 3 transfuse 5 to 10 units of platelets before surgery if platelet count is < 50, 000 / mm 3 leave vesicouterine peritoneum open install subfascial drain
PREECLAMPSIA HELLP syndrome - management for cesarean birth schedule secondary closure of skin incision or subcutaneous drain administer postoperative transfusions as needed perform intensive monitoring for at least 48 hours postpartum consider dexamethasone (10 mg IV every 12 hours) until postpartum resolution of disease occurs
PREECLAMPSIA HELLP syndrome - management of women with a subcapsular liver hematoma general considerations - blood bank aware for potential need of many units of blood general or vascular surgeon consultation avoid direct and indirect manipulation of liver closely monitor hemodynamic status management of hematoma depends on whether it is ruptured or not
PREECLAMPSIA Eclampsia occurrence of convulsions or coma unrelated to other associated conditions all new onset seizures during pregnancy eclampsia until proven otherwise incidence: 1 in 500 pregnancies 3% in multiple gestations
PREECLAMPSIA Eclampsia precise cause unknown theories vasospasm ischemia edema multisystem organ failure
PREECLAMPSIA Eclampsia seizures usually occur without aura hypertension not severe in 20% edema absent in 30% proteinuria absent in 20% hyperreflexia is not predictive of seizure headache or visual changes - most common precipitating event
PREECLAMPSIA Eclampsia 80% of convulsions occur before or during the delivery 1/3 of cases may be not preventable atypical less than 20 weeks gestation more than 48 hours postpartum
PREECLAMPSIA Eclampsia - risk factors low socioeconomic status extremes in childbearing age African-American no prenatal care substance abuse
PREECLAMPSIA Eclampsia - management control convulsions correction of hypoxia and acidosis blood pressure control delivery after maternal stabilization
PREECLAMPSIA Eclampsia - anticonvulsant therapy magnesium sulfate mechanism of action - smooth muscle relaxation by displacement of calcium dosage - 4 -6 g intravenous loading dose, followed by 2 g per hour may be given intramuscularly
PREECLAMPSIA Eclampsia - magnesium sulfate side effects: maternal hypotonia respiratory depression cardiac arrest neonatal depression contraindicated in myasthenia gravis use with caution in renal insufficiency
PREECLAMPSIA Eclampsia - anticonvulsant therapy phenytoin used extensively in Europe may be used in myasthenia gravis mechanism of action - may increase gamma aminobutyric acid-mediated chloride conduction in postsynaptic membranes may inhibit neurotransmitter inhibitory systems
PREECLAMPSIA Eclampsia - phenytoin dosage - 1 g loading dose over 1 hour cardiac monitoring during administration side effects arrhythmias with rapid administration hepatitis Steven-Johnson syndrome
PREECLAMPSIA Eclampsia - anticonvulsant therapy diazepam useful for status seizures mechanism of action - facilitate the binding of GABA to its receptor benzodiazepine receptors dosage - 10 mg at a rate of 5 mg per min may be repeated at 10 to 15 minute intervals
PREECLAMPSIA Eclampsia - diazepam side effects - loss of consciousness, hypotension, respiratory depression caution - may increase risk of aspiration causes prolonged depression of the neonate sodium thiopentotal long acting barbiturate used when sedation, paralysis and intubation needed
PREECLAMPSIA Eclampsia - which anticonvulsant to use? magnesium is associated with decreased recurrence risks of seizures when compared with diazepam or phenytoin diazepam is associated with increased need for mechanical ventilation
PREECLAMPSIA Eclampsia - management of fetus fetal bradycardia during seizure ~ 5 minutes after the onset of the seizure may be associated with rebound tachycardia recovery phase may show late decelerations monitor for uterine hypertonicity allow for fetal recovery monitor for signs of abruption
PREECLAMPSIA Eclampsia delivery is indicated regardless of gestational age immediate cesarean delivery is not necessary
PREECLAMPSIA Eclampsia - radiographic evaluation should be reserved for women with neurological deficit, recurrent seizures, or atypical presentation abnormal CT findings - 50% edema, hemorrhage, infarction cerebral angiography has limited use 90% of EEG evaluations may be abnormal
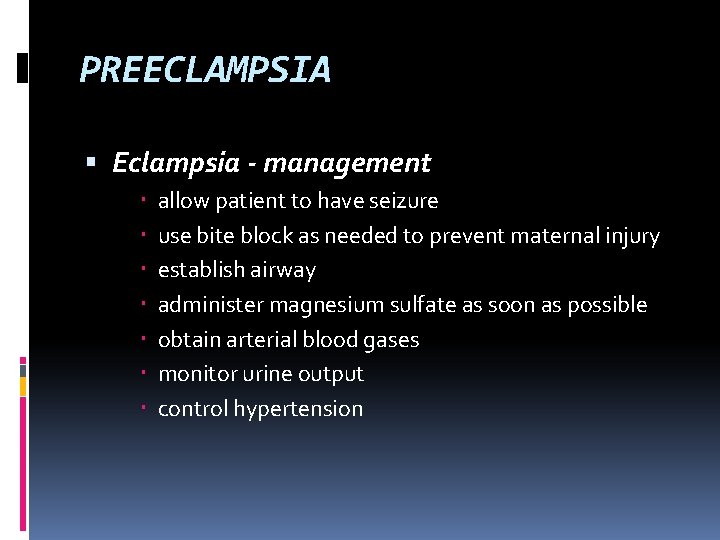
PREECLAMPSIA Eclampsia - management allow patient to have seizure use bite block as needed to prevent maternal injury establish airway administer magnesium sulfate as soon as possible obtain arterial blood gases monitor urine output control hypertension
PREECLAMPSIA Eclampsia - management rebolus with magnesium sulfate if repeat seizure occurs do not intervene for fetal status while mother is unstable if seizure continues, paralyze and intubate.
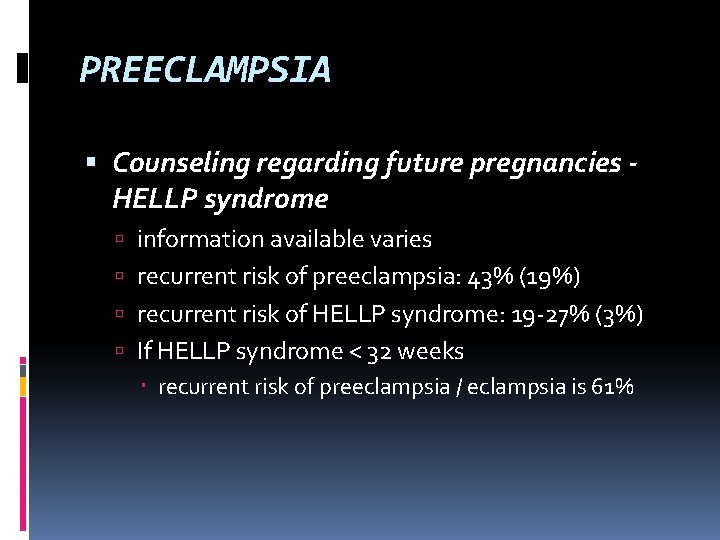
PREECLAMPSIA Counseling regarding future pregnancies HELLP syndrome information available varies recurrent risk of preeclampsia: 43% (19%) recurrent risk of HELLP syndrome: 19 -27% (3%) If HELLP syndrome < 32 weeks recurrent risk of preeclampsia / eclampsia is 61%
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Is an alternative of log based recovery.
Is an alternative of log based recovery. Severe preeclampsia criteria
Severe preeclampsia criteria Norma 017 epidemiologia
Norma 017 epidemiologia Superimposed preeclampsia
Superimposed preeclampsia Magnesium sulfate and urine output
Magnesium sulfate and urine output Nhbep
Nhbep Prof sandra lowe
Prof sandra lowe Pre eclampsia screening
Pre eclampsia screening Preeclampsia definicion
Preeclampsia definicion Preeclampsia teaching
Preeclampsia teaching Preeclampsia intervenciones de enfermeria
Preeclampsia intervenciones de enfermeria Superimposed preeclampsia
Superimposed preeclampsia Diagnostic criteria of preeclampsia
Diagnostic criteria of preeclampsia Phenytoin in eclampsia
Phenytoin in eclampsia Superimposed preeclampsia
Superimposed preeclampsia Trimester breakdown
Trimester breakdown Als assist
Als assist Assist electrical
Assist electrical Business essentials smbs springchambers9to5mac
Business essentials smbs springchambers9to5mac Brake assist system
Brake assist system Brakes unit 3 quiz 1
Brakes unit 3 quiz 1 Second heart assist
Second heart assist Missionassist
Missionassist School mental health assist
School mental health assist The whips assist the party leaders by
The whips assist the party leaders by Emory cr assist
Emory cr assist Hengityspalje
Hengityspalje Assist user guide
Assist user guide Intelligent assist device
Intelligent assist device Cisco smart assist
Cisco smart assist Humoral stimulus
Humoral stimulus What cognitive strategies assist our problem solving
What cognitive strategies assist our problem solving Mediassistindia login
Mediassistindia login Travel guard ez tips
Travel guard ez tips Mcdp 1 states that trust between marines
Mcdp 1 states that trust between marines Gx assist side effects
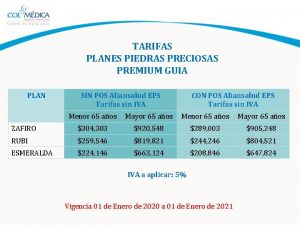
Gx assist side effects Plan zafiro guía premium colmédica
Plan zafiro guía premium colmédica One teach, one assist pros and cons
One teach, one assist pros and cons Peer assist adalah
Peer assist adalah Info assist
Info assist Fire team echelon
Fire team echelon Pam eap
Pam eap Quality assist
Quality assist Park assist 2
Park assist 2 Pbx call assist 2
Pbx call assist 2 Attrition prediction model in excel
Attrition prediction model in excel Chapter 22 hunger games questions
Chapter 22 hunger games questions Branch prediction in computer architecture
Branch prediction in computer architecture Kma price prediction
Kma price prediction Micosis
Micosis Make a prediction about kenny and franchesca
Make a prediction about kenny and franchesca Extrapolation vs prediction
Extrapolation vs prediction Ft prediction
Ft prediction Ncash prediction
Ncash prediction Championship branch prediction
Championship branch prediction 2011
2011 Stable prediction across unknown environments
Stable prediction across unknown environments Diagram pattern
Diagram pattern Ec prediction
Ec prediction Integer pipeline stages of pentium processor
Integer pipeline stages of pentium processor Branch prediction
Branch prediction Steteria prediction
Steteria prediction Prediction of nba games based on machine learning methods
Prediction of nba games based on machine learning methods Demographic parity
Demographic parity Niangjun chen
Niangjun chen Proyeksi bonne (equal area)
Proyeksi bonne (equal area) Baseline logic aba
Baseline logic aba Going to is used for plans, decisions and intentions.
Going to is used for plans, decisions and intentions. Inversion attacks
Inversion attacks Variance in regression
Variance in regression Difference between prediction and inference in reading
Difference between prediction and inference in reading Gene prediction in prokaryotes and eukaryotes
Gene prediction in prokaryotes and eukaryotes Drag prediction workshop
Drag prediction workshop Branch prediction in computer architecture
Branch prediction in computer architecture Withdrawal designs
Withdrawal designs Branch prediction in computer architecture
Branch prediction in computer architecture Prediction error variance
Prediction error variance Dsp n
Dsp n Rna secondary structure prediction
Rna secondary structure prediction Branch prediction
Branch prediction Dot transfer papers
Dot transfer papers Koji tsuda
Koji tsuda Good readers making predictions by
Good readers making predictions by Ebusiness metrics
Ebusiness metrics Zonation and succession
Zonation and succession Corner prediction
Corner prediction Hypothesis vs prediction
Hypothesis vs prediction Nearshore wave prediction system
Nearshore wave prediction system Hypothesis example
Hypothesis example Difference between prediction and forecasting
Difference between prediction and forecasting Revenue prediction machine learning
Revenue prediction machine learning Foabit review
Foabit review Coefficient of determination formula in regression
Coefficient of determination formula in regression Polygon prediction
Polygon prediction Stealing machine learning models via prediction apis
Stealing machine learning models via prediction apis Masta prediction
Masta prediction Prediction vs inference venn diagram
Prediction vs inference venn diagram Hypothesis vs prediction
Hypothesis vs prediction Derition
Derition Example of drawing conclusion
Example of drawing conclusion Merit pridiction
Merit pridiction Perceptual linear prediction
Perceptual linear prediction Dr. zareen syed
Dr. zareen syed Prediction pip
Prediction pip Prediction format
Prediction format Mathematical models for impact prediction
Mathematical models for impact prediction Static branch prediction in computer architecture
Static branch prediction in computer architecture Dr jack soaring forecast
Dr jack soaring forecast Noaa african desk
Noaa african desk Two brown-eyed parents blue-eyed child
Two brown-eyed parents blue-eyed child Iterative prediction of motion
Iterative prediction of motion Make a prediction
Make a prediction Wpc snow probabilities
Wpc snow probabilities Freedico prediction
Freedico prediction Matthew 26 35
Matthew 26 35 Hunger games chapter 21 questions and answers
Hunger games chapter 21 questions and answers B'kalmar teater', b'se'
B'kalmar teater', b'se'