Superimposed severe preeclampsia Management of severe hypertension Treatment
- Slides: 16
Superimposed severe preeclampsia Management of severe hypertension
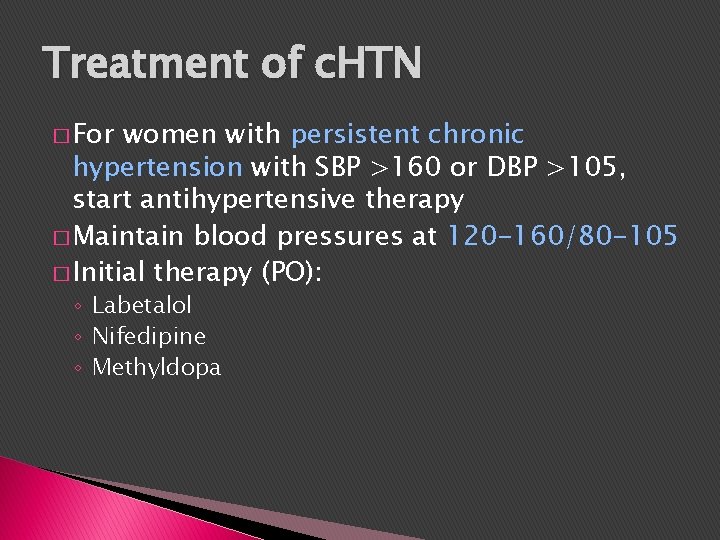
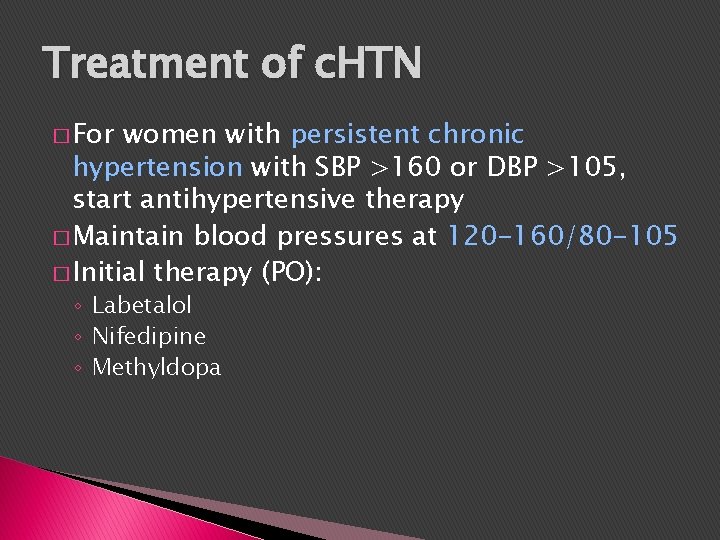
Treatment of c. HTN � For women with persistent chronic hypertension with SBP >160 or DBP >105, start antihypertensive therapy � Maintain blood pressures at 120 -160/80 -105 � Initial therapy (PO): ◦ Labetalol ◦ Nifedipine ◦ Methyldopa
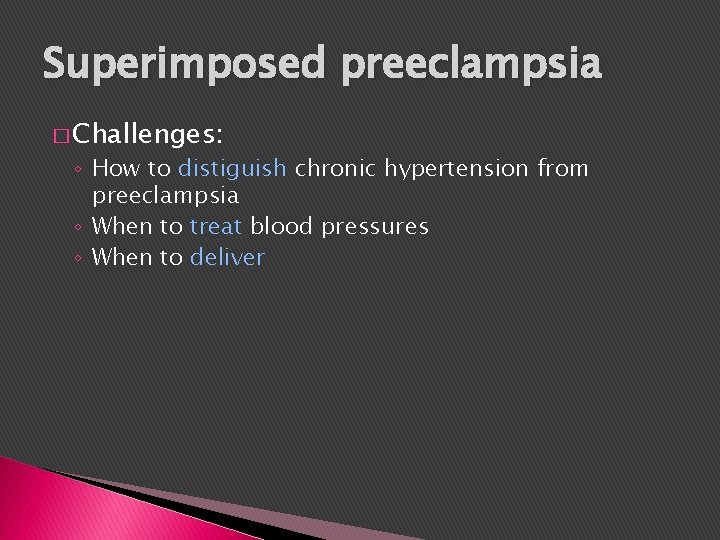
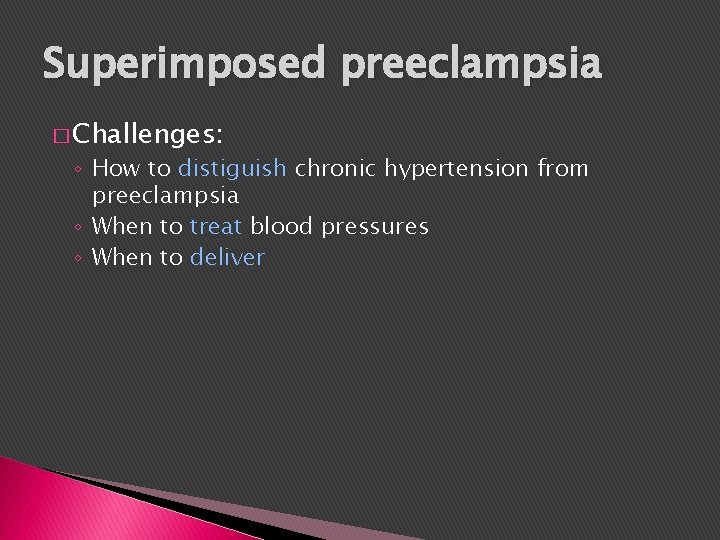
Superimposed preeclampsia � Challenges: ◦ How to distiguish chronic hypertension from preeclampsia ◦ When to treat blood pressures ◦ When to deliver
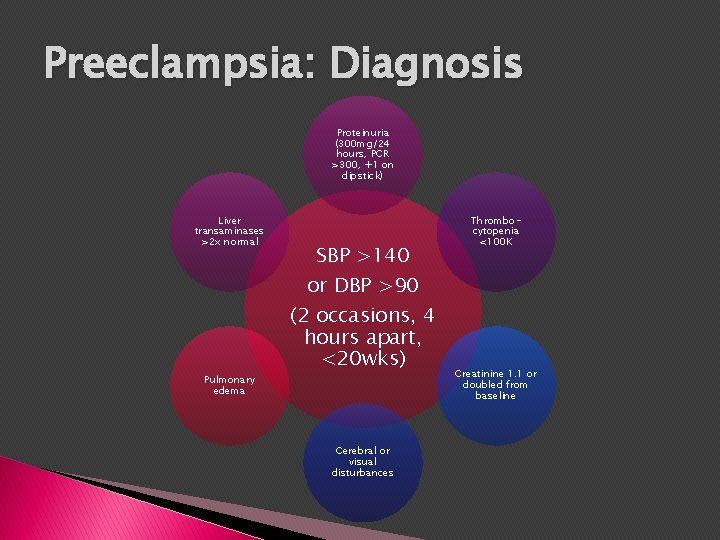
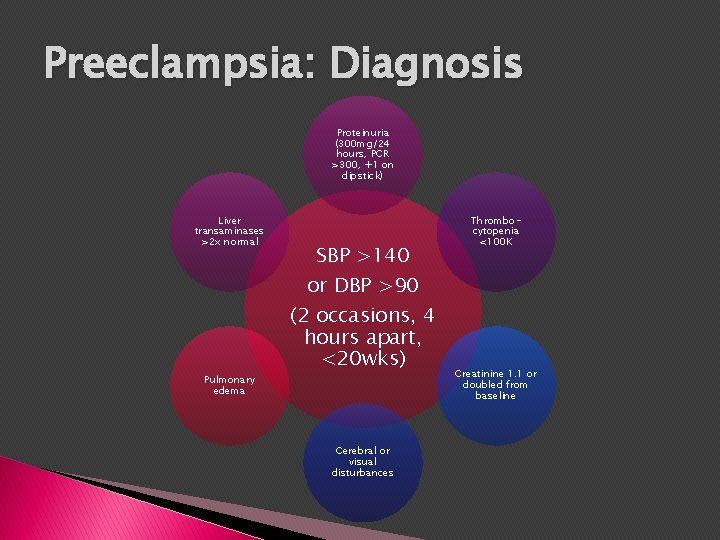
Preeclampsia: Diagnosis Proteinuria (300 mg/24 hours, PCR >300, +1 on dipstick) Liver transaminases >2 x normal Pulmonary edema SBP >140 or DBP >90 (2 occasions, 4 hours apart, <20 wks) Cerebral or visual disturbances Thrombocytopenia <100 K Creatinine 1. 1 or doubled from baseline
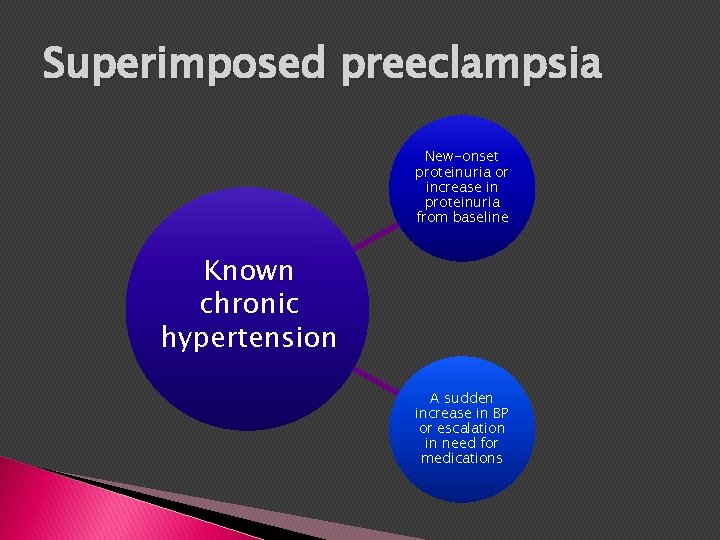
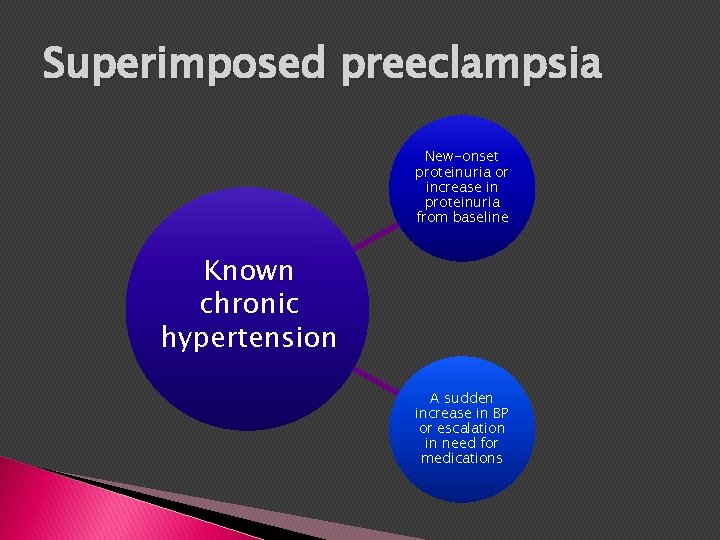
Superimposed preeclampsia New-onset proteinuria or increase in proteinuria from baseline Known chronic hypertension A sudden increase in BP or escalation in need for medications
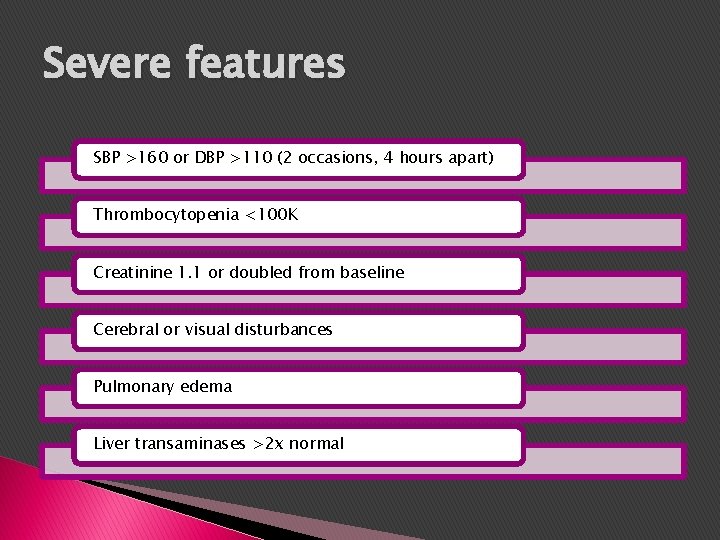
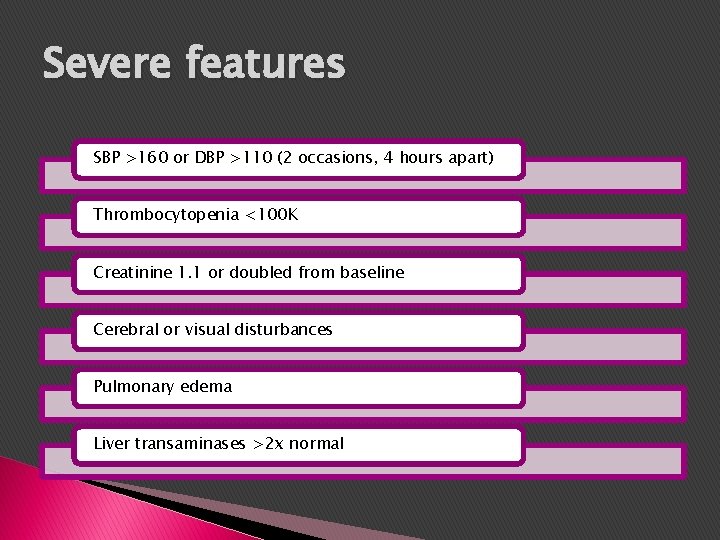
Severe features SBP >160 or DBP >110 (2 occasions, 4 hours apart) Thrombocytopenia <100 K Creatinine 1. 1 or doubled from baseline Cerebral or visual disturbances Pulmonary edema Liver transaminases >2 x normal
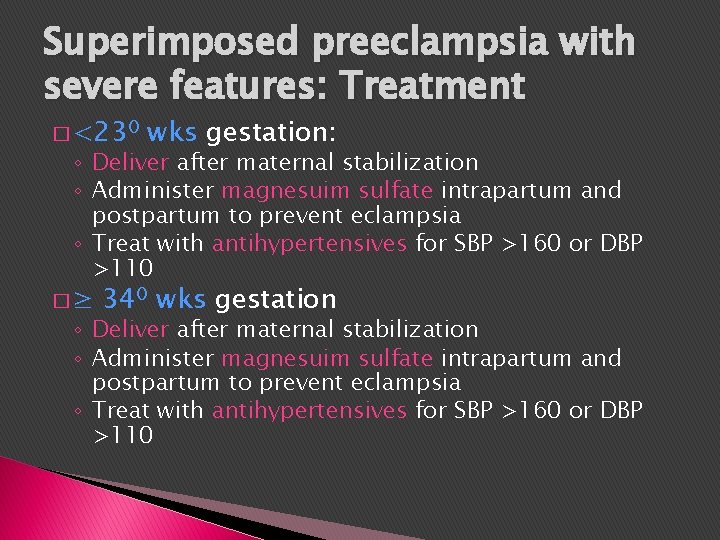
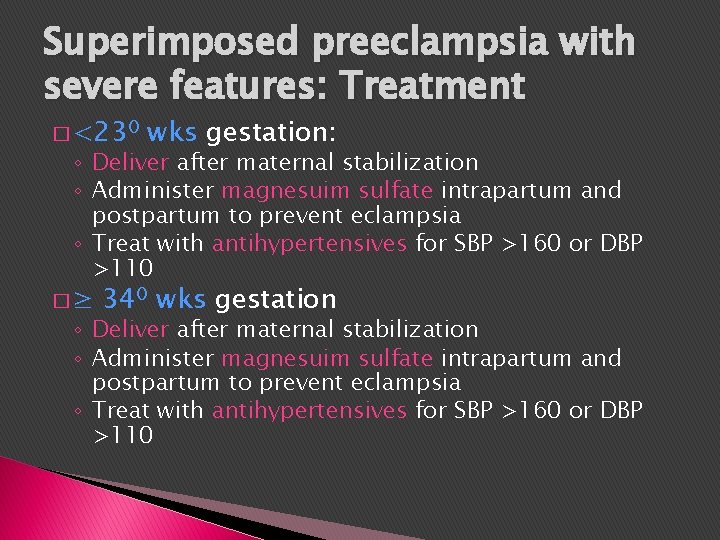
Superimposed preeclampsia with severe features: Treatment � <230 wks gestation: ◦ Deliver after maternal stabilization ◦ Administer magnesuim sulfate intrapartum and postpartum to prevent eclampsia ◦ Treat with antihypertensives for SBP >160 or DBP >110 �≥ 340 wks gestation ◦ Deliver after maternal stabilization ◦ Administer magnesuim sulfate intrapartum and postpartum to prevent eclampsia ◦ Treat with antihypertensives for SBP >160 or DBP >110
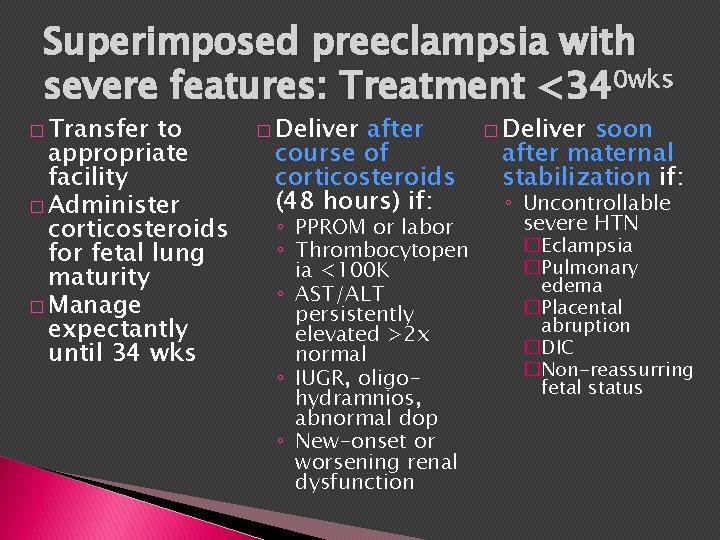
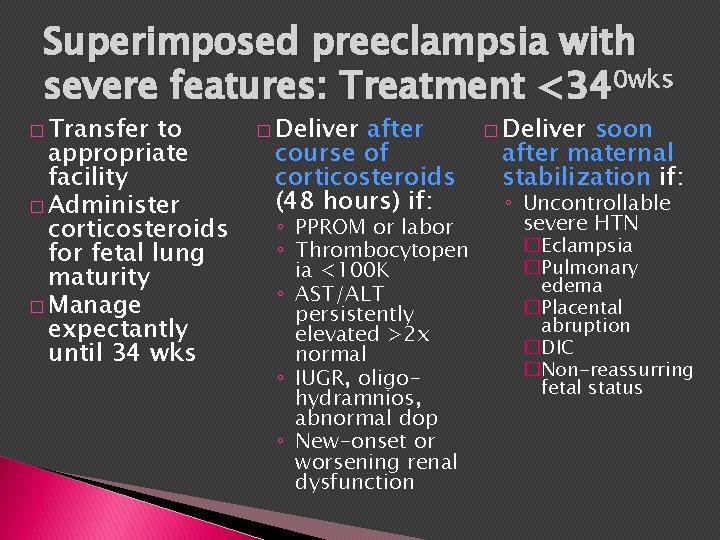
Superimposed preeclampsia with severe features: Treatment <340 wks � Transfer to appropriate facility � Administer corticosteroids for fetal lung maturity � Manage expectantly until 34 wks � Deliver after course of corticosteroids (48 hours) if: ◦ PPROM or labor ◦ Thrombocytopen ia <100 K ◦ AST/ALT persistently elevated >2 x normal ◦ IUGR, oligohydramnios, abnormal dop ◦ New-onset or worsening renal dysfunction � Deliver soon after maternal stabilization if: ◦ Uncontrollable severe HTN �Eclampsia �Pulmonary edema �Placental abruption �DIC �Non-reassurring fetal status
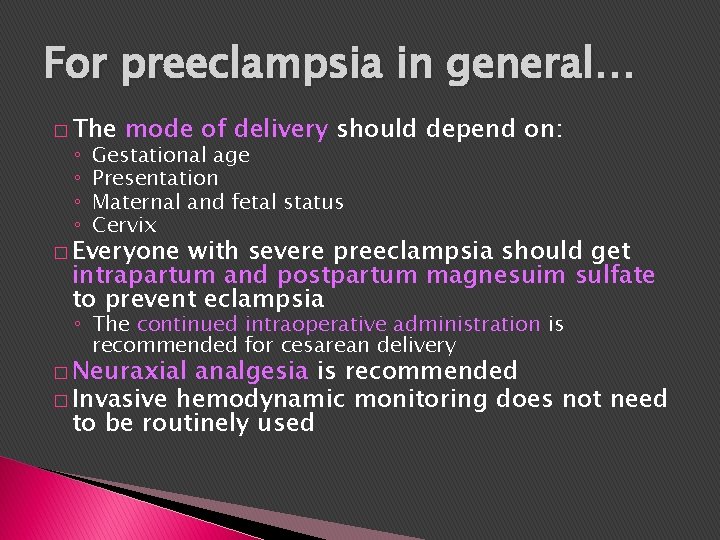
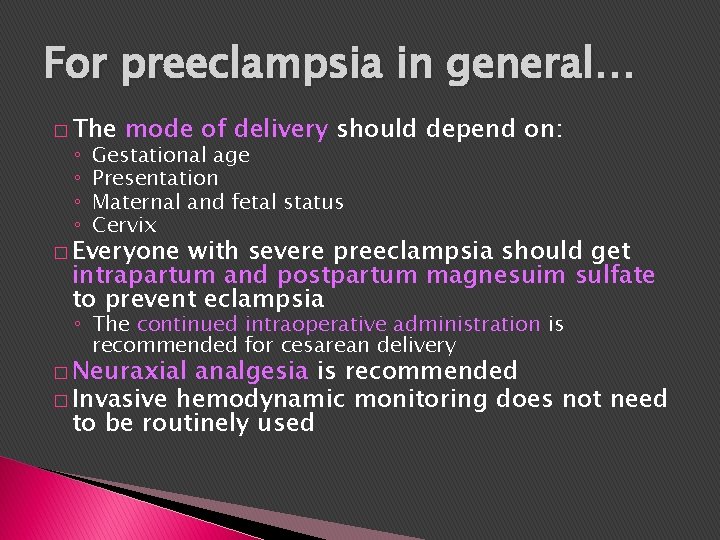
For preeclampsia in general… � The ◦ ◦ mode of delivery should depend on: Gestational age Presentation Maternal and fetal status Cervix � Everyone with severe preeclampsia should get intrapartum and postpartum magnesuim sulfate to prevent eclampsia ◦ The continued intraoperative administration is recommended for cesarean delivery � Neuraxial analgesia is recommended � Invasive hemodynamic monitoring does not need to be routinely used
Managing Severe Hypertension In preeclampsia or eclampsia
Severe hypertension � Hypertensive emergency ◦ Severe: SBP >160 or DBP >110 ◦ Persistent: lasting more than 15 minutes ◦ Acute onset
Severe hypertension � “Severe systolic hypertension may be the most important predictor of cerebral hemorrhage and infarction in these patients and, if not treated expeditiously, can result in maternal death. ” � UK report 2003 -2005: 2/3 of maternal deaths resulted from cerebral hemorrhage or infarction � Case series of 28 women with preeclampsia/stroke ◦ All but 1 had severe SBP ◦ 54% died
Severe hypertension � Goal of treatment is to reduce pressures to 140 -160/90 -100 � This should be accomplished before delivery, even if delivery is needed urgently
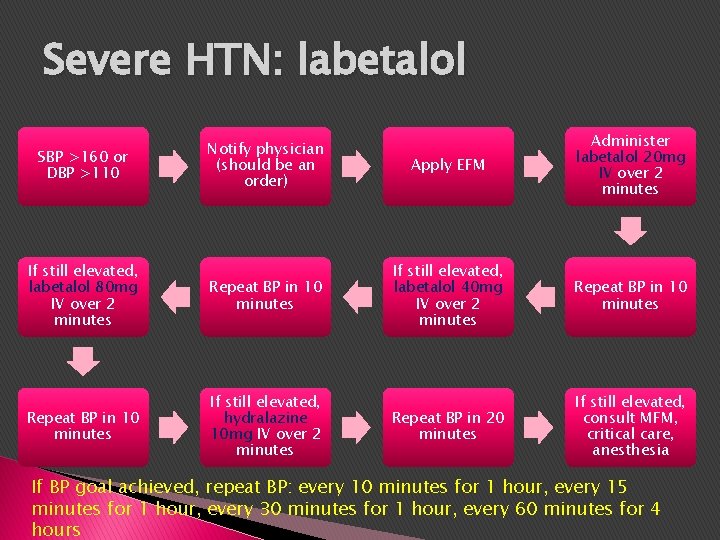
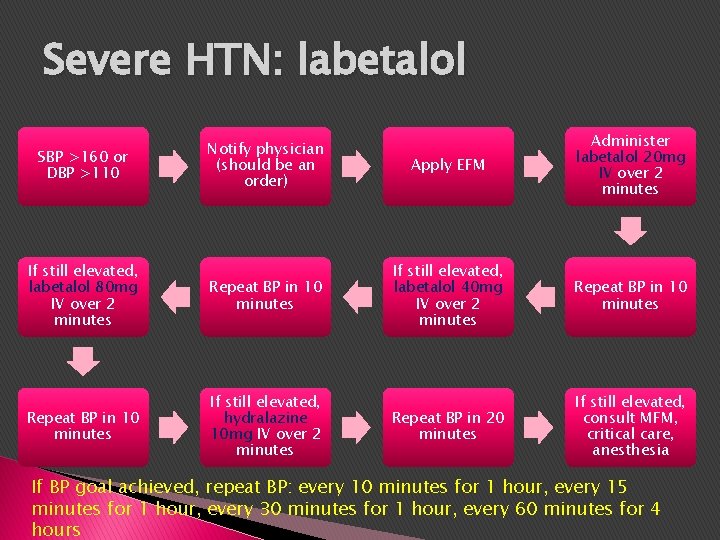
Severe HTN: labetalol Notify physician (should be an order) Apply EFM Administer labetalol 20 mg IV over 2 minutes If still elevated, labetalol 80 mg IV over 2 minutes Repeat BP in 10 minutes If still elevated, labetalol 40 mg IV over 2 minutes Repeat BP in 10 minutes If still elevated, hydralazine 10 mg IV over 2 minutes Repeat BP in 20 minutes If still elevated, consult MFM, critical care, anesthesia SBP >160 or DBP >110 If BP goal achieved, repeat BP: every 10 minutes for 1 hour, every 15 minutes for 1 hour, every 30 minutes for 1 hour, every 60 minutes for 4 hours
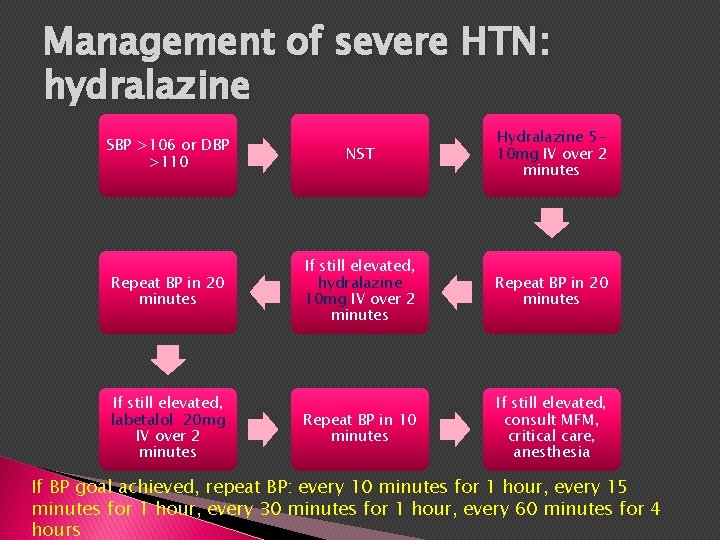
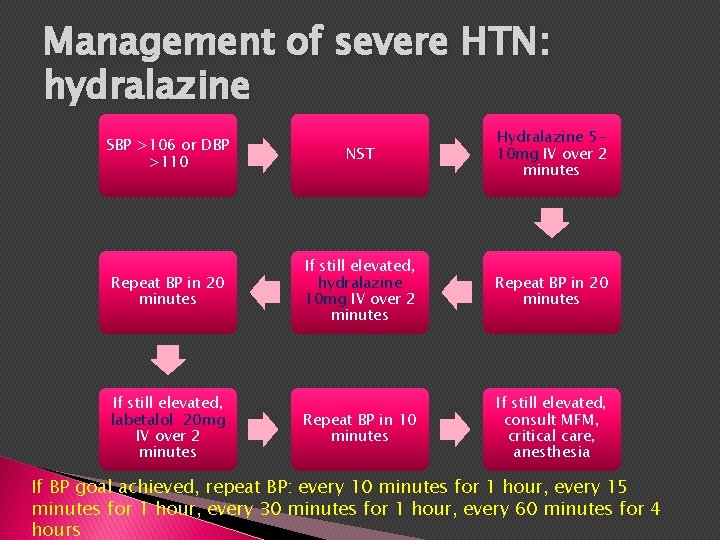
Management of severe HTN: hydralazine SBP >106 or DBP >110 NST Hydralazine 510 mg IV over 2 minutes Repeat BP in 20 minutes If still elevated, hydralazine 10 mg IV over 2 minutes Repeat BP in 20 minutes Repeat BP in 10 minutes If still elevated, consult MFM, critical care, anesthesia If still elevated, labetalol 20 mg IV over 2 minutes If BP goal achieved, repeat BP: every 10 minutes for 1 hour, every 15 minutes for 1 hour, every 30 minutes for 1 hour, every 60 minutes for 4 hours
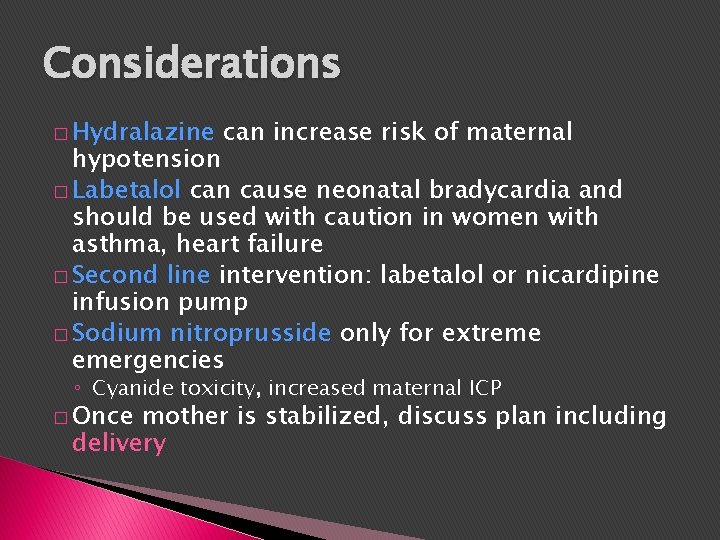
Considerations � Hydralazine can increase risk of maternal hypotension � Labetalol can cause neonatal bradycardia and should be used with caution in women with asthma, heart failure � Second line intervention: labetalol or nicardipine infusion pump � Sodium nitroprusside only for extreme emergencies ◦ Cyanide toxicity, increased maternal ICP � Once mother is stabilized, discuss plan including delivery
 Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Severe preeclampsia criteria
Severe preeclampsia criteria Malignant hypertension treatment
Malignant hypertension treatment Malignant hypertension
Malignant hypertension Severe hyponatremia treatment
Severe hyponatremia treatment What is life
What is life Phenytoin in eclampsia
Phenytoin in eclampsia Preeclampsia teaching
Preeclampsia teaching Preeclampsia intervenciones de enfermeria
Preeclampsia intervenciones de enfermeria Pregnancy trimester breakdown
Pregnancy trimester breakdown Magnesium sulfate and urine output
Magnesium sulfate and urine output Management
Management Phenytoin in eclampsia
Phenytoin in eclampsia