Preeclampsia Ismail Qattam Headlines Chronic Hypertension Gestational Hypertension


- Slides: 18
Pre-eclampsia Ismail Qattam
Headlines: Chronic Hypertension Gestational Hypertension Pre-Eclampsia
Chronic Hypertension: - Chronic/pre-existing hypertension – defined as hypertension that precedes pregnancy, or is detected on at least two separate occasions before the 20 th week of gestation or persists longer than 12 weeks postpartum. It can be primary (primary hypertension"essential hypertension") or secondary to a variety of medical disorders - A risk factor for Pre-eclampsia and can develop to a superimposed pre-eclampsia - The physiological fall in blood pressure that occurs in the first trimester secondary to peripheral vasodilatation can mask chronic hypertension.
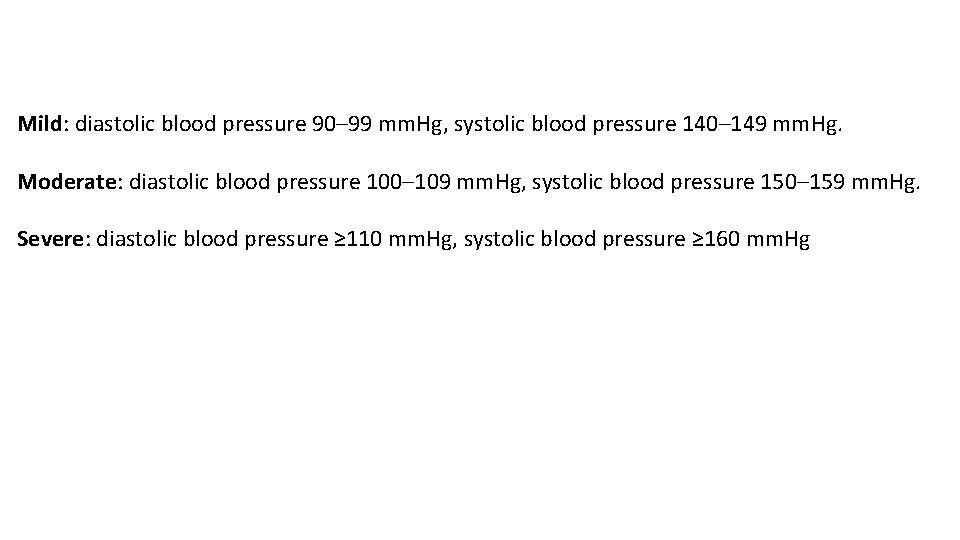
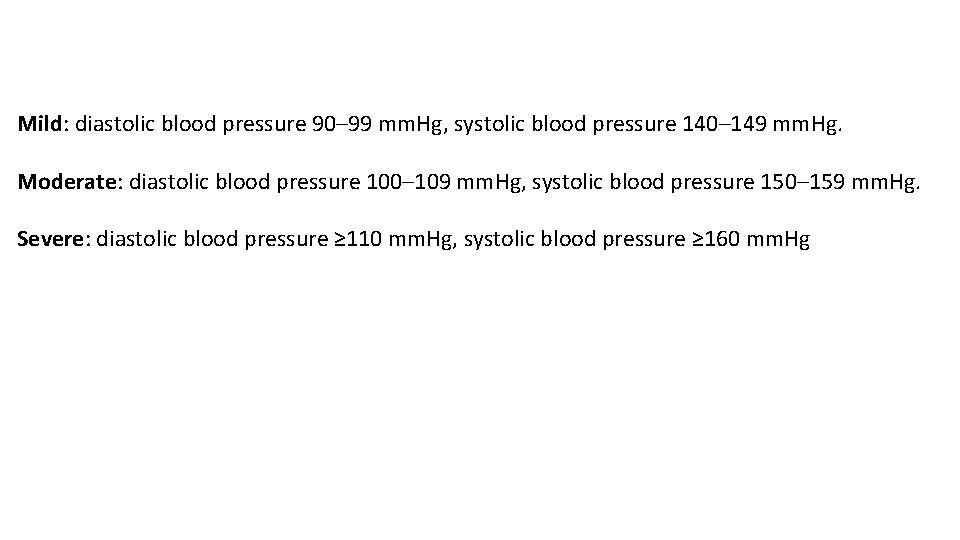
Mild: diastolic blood pressure 90– 99 mm. Hg, systolic blood pressure 140– 149 mm. Hg. Moderate: diastolic blood pressure 100– 109 mm. Hg, systolic blood pressure 150– 159 mm. Hg. Severe: diastolic blood pressure ≥ 110 mm. Hg, systolic blood pressure ≥ 160 mm. Hg
Treatment: Before pregnancy: we change the teratogenic anti-hypertensive drugs to safer drugs such as : - Goal BP ? - We monitor ?
Gestational Hypertension: Diagnosed with sustained elevation of BP 140/90 mmhg or more, after 20 weeks of pregnancy, without proteinurea. BP returns to normal baseline postpartum. Physical findings are unremarkable for pregnancy. Lab tests are unremarkable for pregnancy. Proteinuria is absent. Monitoring: ? Tx: same drugs.
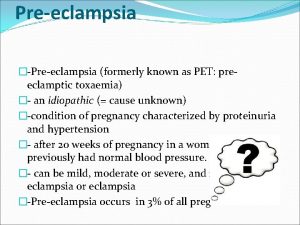
Pre-Eclampsia: Preeclampsia refers to the new onset of hypertension and proteinuria OR, hypertension and significant end-organ dysfunction with or without proteinuria after 20 weeks of gestation in a previously normotensive woman It may also develop postpartum Preeclampsia is less prevalent before 34 weeks of gestation

-It involves both maternal and fetal/placental factors. -Shallow placentation and failure to remodel the spiral arteries of the decidua and myometrium early in pregnancy, weeks to months before development of clinical manifestations of the disease, have been well documented. -Failure to establish an adequate Utero-placental blood flow can result in relatively hypoxic trophoblast tissue, which may promote an exaggerated state of oxidative stress in the placenta. -This appears to alter placental villous angiogenesis, leading to poor development of the fetoplacental vasculature and abnormal vascular reactivity. -Placental secretion of antiangiogenic factors (s. Flt-1 and endoglin) that bind vascular endothelial growth factor and placental growth factor in the maternal circulation appears to result in widespread maternal vascular dysfunction, leading to hypertension, proteinuria, and the other clinical manifestations of preeclampsia.
Risk factors for Preeclampsia: -Obesity (BMI >30)/ Age <18 -40< -Past history of preeclampsia/multi-gestational/ first pregnancy/ 10 years since last pregnancy -prior pregnancy complications: abruption placenta, IUGR -Diabetes / HTN/ chronic kidney disease/ systemic lupus erythematosus/ Antiphospholipid syndrome. -Assisted reproductive technology
Systolic blood pressure ≥ 140 mm. Hg or diastolic blood pressure ≥ 90 mm. Hg on at least two occasions at least four hours apart after 20 weeks of gestation in a previously normotensive patient AND the new onset of one or more of the following*: -Proteinuria ≥ 0. 3 g in a 24 -hour urine specimen or protein/creatinine ratio ≥ 0. 3 (mg/mg) (30 mg/mmol) in a random urine specimen or dipstick ≥ 2+ if a quantitative measurement is unavailable -Thrombocytopenia -Serum creatinine >1. 1 mg/d. L (97. 2 micromol/L) or doubling of the creatinine concentration in the absence of other renal disease -Liver transaminases at least twice the upper limit of the normal concentrations for the local laboratory -Pulmonary Edema -Cerebral or visual symptoms (eg, new-onset and persistent headaches not accounted for by alternative diagnoses and not responding to usual doses of analgesics; blurred vision, flashing lights or sparks, scotomata)
Patient evaluation -Accurate assessment of blood pressure -Routine laboratory evaluation: • Should have a complete blood count, serum creatinine level, liver chemistries (LDH, AST, ALT), and urinary protein determination (protein: creatinine ratio or 24 -hour urine protein). • Coagulation studies (prothrombin time, partial thromboplastin time, fibrinogen) are not routinely obtained but are indicated in patients with additional complications, such as abruptio placentae, severe bleeding, or severe liver dysfunction. -Assessment of fetal status: • At a minimum, a nonstress test or biophysical profile is performed. • Ultrasound is indicated to evaluate amniotic fluid volume and estimate fetal weight. • Doppler -Indications for neurology consultation: • in women with neurological deficits/ ocular signs and symptoms, or a severe persistent headache that does not respond to a dose of acetaminophen. • severe headache ("worst headache of my life") is sufficiently characteristic of subarachnoid hemorrhage that this diagnosis should prompt neurology consultation and consideration of imaging.
Treatment: -Antihypertensive drugs: -Seizures prophylactics: IV-Magnesium sulphate
Approach: -Term pregnancies: Delivery — at ≥ 37 weeks of gestation (HYPITAT trial ) • Women with preeclampsia benefited from early intervention, without incurring an increased risk of operative delivery or neonatal morbidity: • Routine induction was associated with a 30 % reduction in the composite maternal outcome • The induced group had a significantly lower rate of cesarean delivery. -At preterm gestational ages, the risks of serious sequelae from disease progression need to be balanced with the newborn risks from preterm birth. -Expectant management: • When mother and fetus are stable • However, at any gestational age, evidence of severe hypertension, or nonreassuring tests of fetal well-being are generally an indication for prompt delivery. • Prior to 34+0 weeks, guidelines from major medical organizations generally recommend expectant management of preeclampsia without features of severe disease,
Intrapartum management: -The route of delivery is based on standard obstetrical indications. -Intrapartum monitoring: Continuous maternal-fetal monitoring is indicated intrapartum -Fluids: Fluid balance should be monitored closely to avoid excessive administration, since women with preeclampsia are at risk of pulmonary edema and significant third-spacing, especially at the severe end of the disease spectrum. -Hypertension: Severe hypertension in labor should be treated promptly with intravenous labetalol (avoid in patients with asthma) or hydralazine or oral nifedipine to prevent stroke
Postpartum approach: -Monitor vital signs every two hours while the patient remains on magnesium sulfate, -Repeat laboratory tests: -Although nonsteroidal anti-inflammatory drugs (NSAIDs) sometimes exacerbate hypertension, NSAIDs should be used preferentially over opioid analgesics -We suggest frequently monitoring blood pressure in the hospital or at home for the first 72 hours postpartum and if it is in an acceptable range, then blood pressure is measured at a follow-up visit 7 to 10 days postdelivery.
Eclampsia: - Is defined as Onset of seizures in a woman with PET. -pathophysiology: is severe diffuse cerebral vasospasm resulting in cerebral perfusion deficits and cerebral edema. -same risks factors for pre-eclampsia. A primary seizure disorder doesn’t predispose to eclampsia. Approach: Administer Mg. SO 4 with an IV bolus of 5 g to stop seizures, continuing maintenance infusion rate of 2 g/h. continue IV Mg. SO 4 for 24 hours after delivery. Aggressive prompt delivery is indicated for eclampsia at any gestational age after stabilization of the mother and the fetus, attempt vaginal delivery with IV oxytocin infusion if mother and fetus are stable.

 Thyrombocytopenia
Thyrombocytopenia Management
Management Preeclampsia teaching
Preeclampsia teaching Diagnosticos de enfermeria para preeclampsia
Diagnosticos de enfermeria para preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Eclampsia definicion
Eclampsia definicion Superimposed preeclampsia
Superimposed preeclampsia Nom preeclampsia
Nom preeclampsia Mild preeclampsia
Mild preeclampsia Magnesium sulfate toxicity level
Magnesium sulfate toxicity level Diagnostic criteria of preeclampsia
Diagnostic criteria of preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Acute fulminating preeclampsia
Acute fulminating preeclampsia Nhbep
Nhbep Prof sandra lowe
Prof sandra lowe Phenytoin in eclampsia
Phenytoin in eclampsia Gestational age formula
Gestational age formula Gestational age chart
Gestational age chart Complications of gestational diabetes
Complications of gestational diabetes