Gestational hypertension formerly termed pregnancyinduced hypertension If preeclampsia









- Slides: 47

서론 ① Gestational hypertension —formerly termed pregnancy-induced hypertension. If preeclampsia syndrome does not develop and hypertension resolves by 12 weeks postpartum, it is redesignated as transient hypertension ② Preeclampsia and eclampsia syndrome ③ Preeclampsia syndrome superimposed on chronic hypertension ④ Chronic hypertension
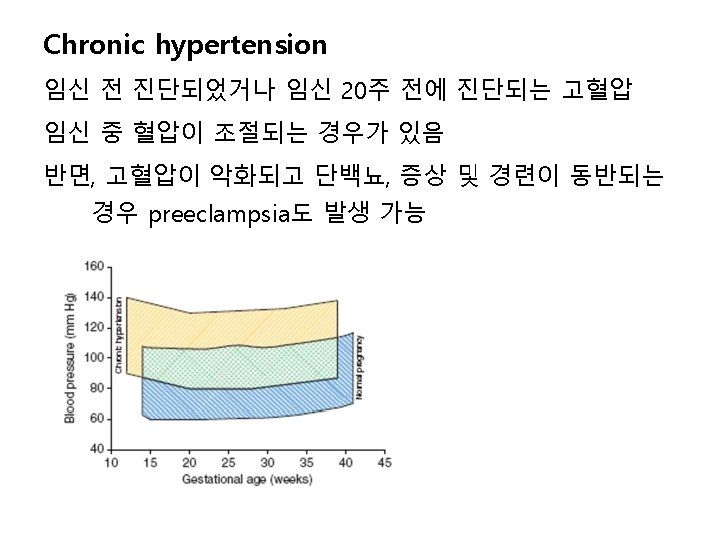
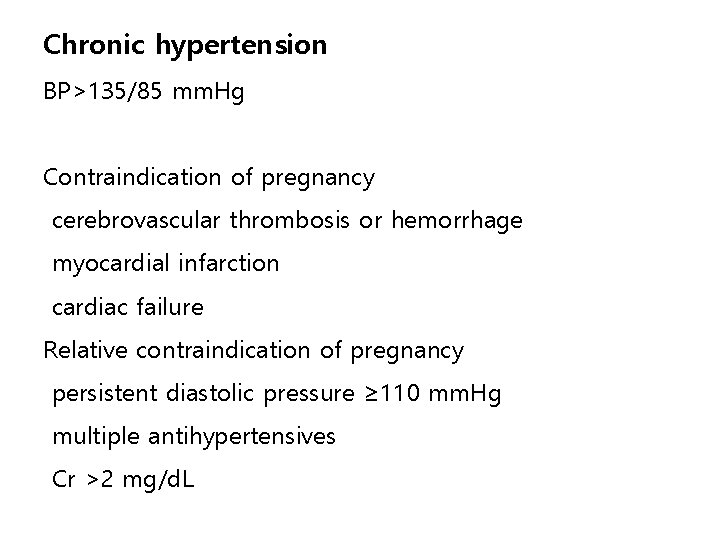
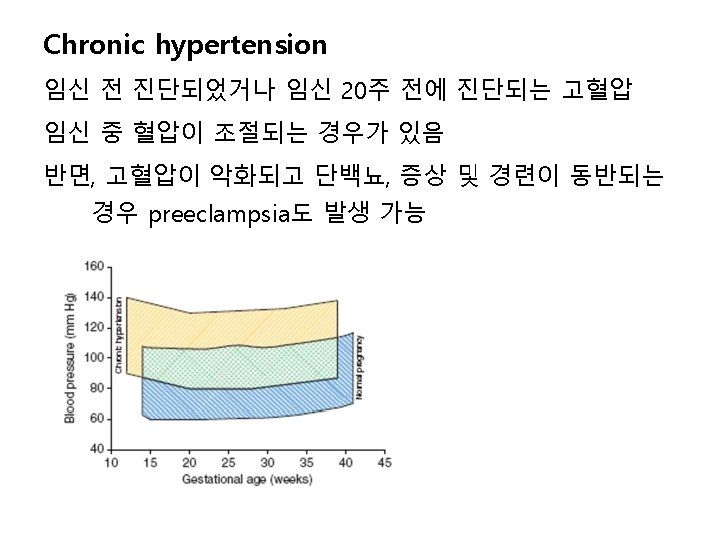
Chronic hypertension BP>135/85 mm. Hg Contraindication of pregnancy cerebrovascular thrombosis or hemorrhage myocardial infarction cardiac failure Relative contraindication of pregnancy persistent diastolic pressure ≥ 110 mm. Hg multiple antihypertensives Cr >2 mg/d. L
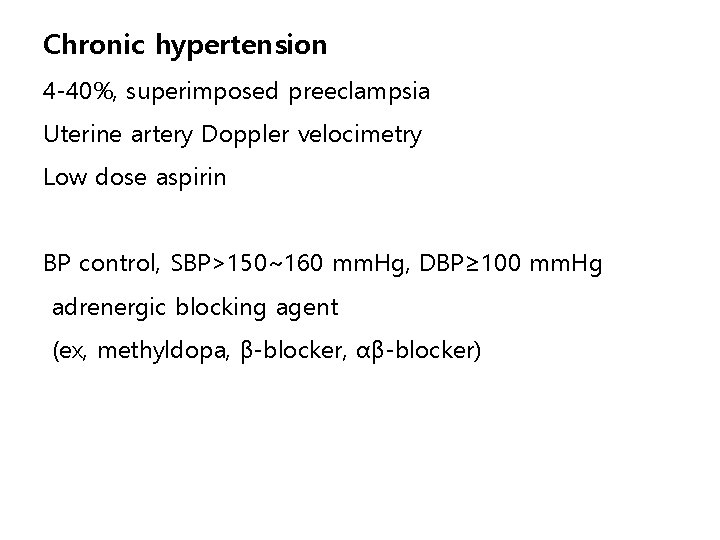
Chronic hypertension 4 -40%, superimposed preeclampsia Uterine artery Doppler velocimetry Low dose aspirin BP control, SBP>150~160 mm. Hg, DBP≥ 100 mm. Hg adrenergic blocking agent (ex, methyldopa, β-blocker, αβ-blocker)
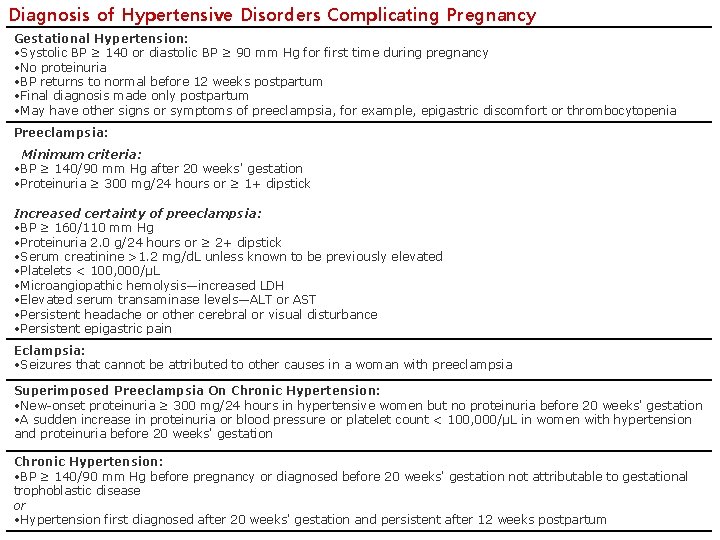
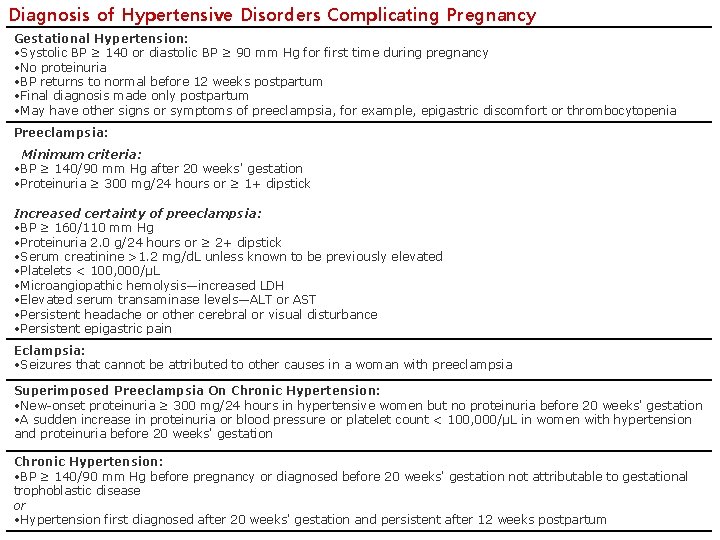
Diagnosis of Hypertensive Disorders Complicating Pregnancy Gestational Hypertension: • Systolic BP ≥ 140 or diastolic BP ≥ 90 mm Hg for first time during pregnancy • No proteinuria • BP returns to normal before 12 weeks postpartum • Final diagnosis made only postpartum • May have other signs or symptoms of preeclampsia, for example, epigastric discomfort or thrombocytopenia Preeclampsia: Minimum criteria: • BP ≥ 140/90 mm Hg after 20 weeks' gestation • Proteinuria ≥ 300 mg/24 hours or ≥ 1+ dipstick Increased certainty of preeclampsia: • BP ≥ 160/110 mm Hg • Proteinuria 2. 0 g/24 hours or ≥ 2+ dipstick • Serum creatinine >1. 2 mg/d. L unless known to be previously elevated • Platelets < 100, 000/µL • Microangiopathic hemolysis—increased LDH • Elevated serum transaminase levels—ALT or AST • Persistent headache or other cerebral or visual disturbance • Persistent epigastric pain Eclampsia: • Seizures that cannot be attributed to other causes in a woman with preeclampsia Superimposed Preeclampsia On Chronic Hypertension: • New-onset proteinuria ≥ 300 mg/24 hours in hypertensive women but no proteinuria before 20 weeks' gestation • A sudden increase in proteinuria or blood pressure or platelet count < 100, 000/µL in women with hypertension and proteinuria before 20 weeks' gestation Chronic Hypertension: • BP ≥ 140/90 mm Hg before pregnancy or diagnosed before 20 weeks' gestation not attributable to gestational trophoblastic disease or • Hypertension first diagnosed after 20 weeks' gestation and persistent after 12 weeks postpartum
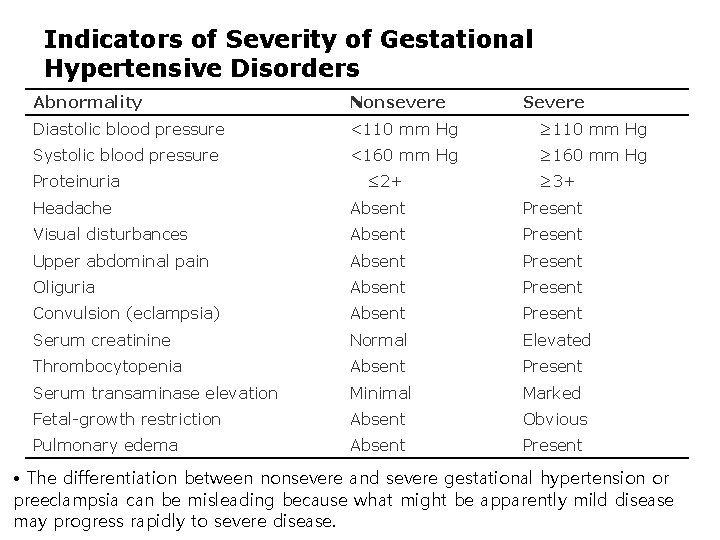
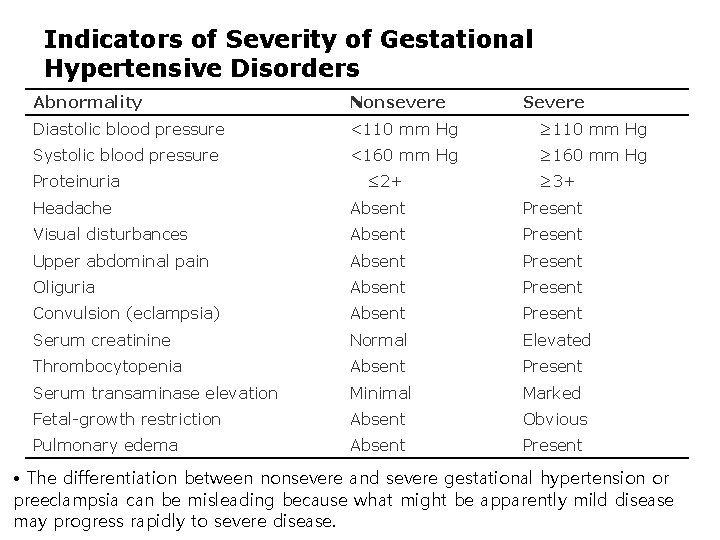
Indicators of Severity of Gestational Hypertensive Disorders Abnormality Nonsevere Severe Diastolic blood pressure <110 mm Hg ≥ 110 mm Hg Systolic blood pressure <160 mm Hg ≥ 160 mm Hg Proteinuria ≤ 2+ ≥ 3+ Headache Absent Present Visual disturbances Absent Present Upper abdominal pain Absent Present Oliguria Absent Present Convulsion (eclampsia) Absent Present Serum creatinine Normal Elevated Thrombocytopenia Absent Present Serum transaminase elevation Minimal Marked Fetal-growth restriction Absent Obvious Pulmonary edema Absent Present • The differentiation between nonsevere and severe gestational hypertension or preeclampsia can be misleading because what might be apparently mild disease may progress rapidly to severe disease.
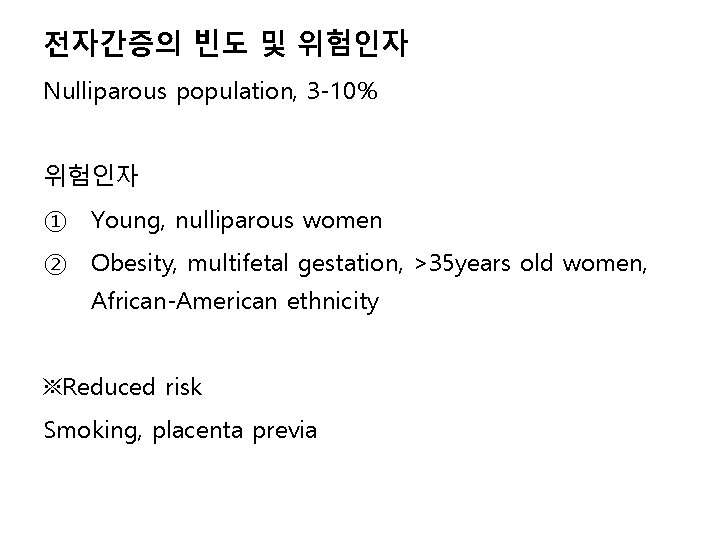
전자간증의 빈도 및 위험인자 Nulliparous population, 3 -10% 위험인자 ① Young, nulliparous women ② Obesity, multifetal gestation, >35 years old women, African-American ethnicity ※Reduced risk Smoking, placenta previa
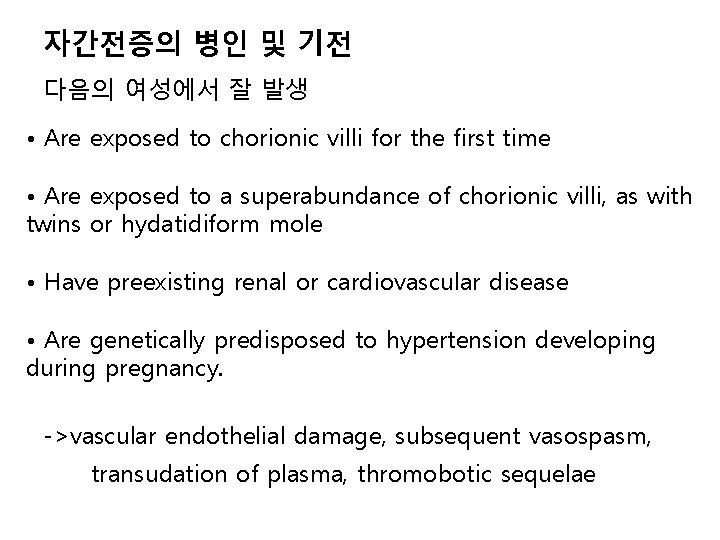
자간전증의 병인 및 기전 다음의 여성에서 잘 발생 • Are exposed to chorionic villi for the first time • Are exposed to a superabundance of chorionic villi, as with twins or hydatidiform mole • Have preexisting renal or cardiovascular disease • Are genetically predisposed to hypertension developing during pregnancy. ->vascular endothelial damage, subsequent vasospasm, transudation of plasma, thromobotic sequelae

원인 ① Placental implantation with abnormal trophoblastic invasion of uterine vessels ② Immunological maladaptive tolerance between maternal, paternal (placental), and fetal tissues ③ Maternal maladaptation to cardiovascular or inflammatory changes of normal pregnancy ④ Genetic factors including inherited predisposing genes as well as epigenetic influences.
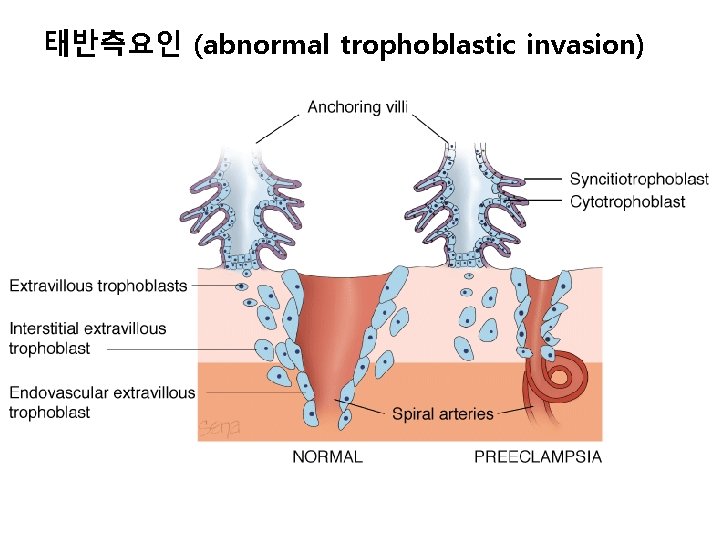
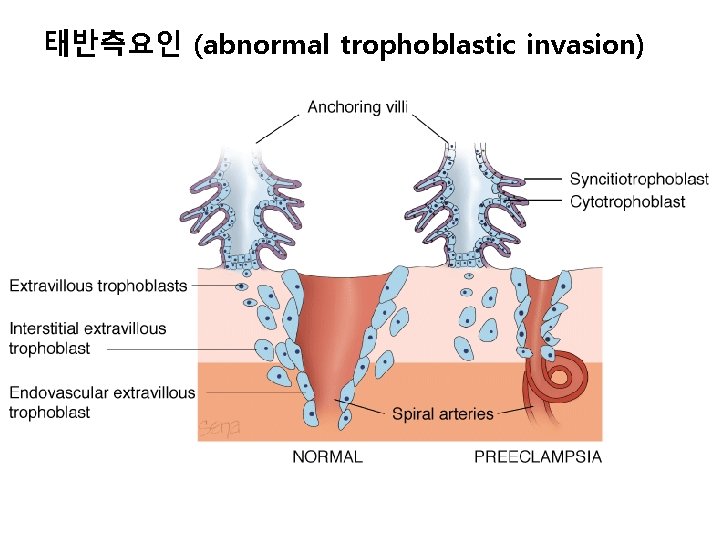
태반측요인 (abnormal trophoblastic invasion)
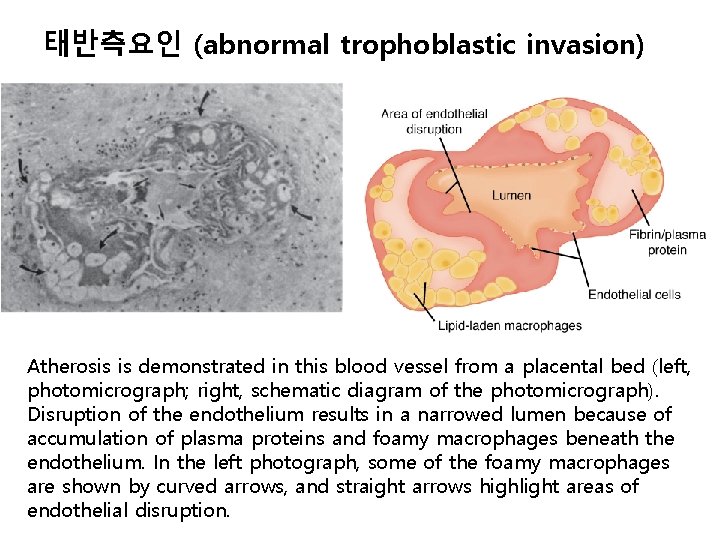
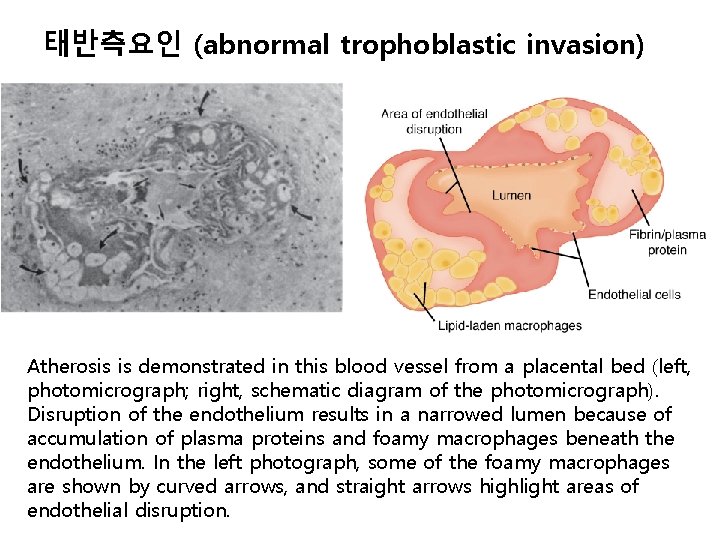
태반측요인 (abnormal trophoblastic invasion) Atherosis is demonstrated in this blood vessel from a placental bed (left, photomicrograph; right, schematic diagram of the photomicrograph). Disruption of the endothelium results in a narrowed lumen because of accumulation of plasma proteins and foamy macrophages beneath the endothelium. In the left photograph, some of the foamy macrophages are shown by curved arrows, and straight arrows highlight areas of endothelial disruption.
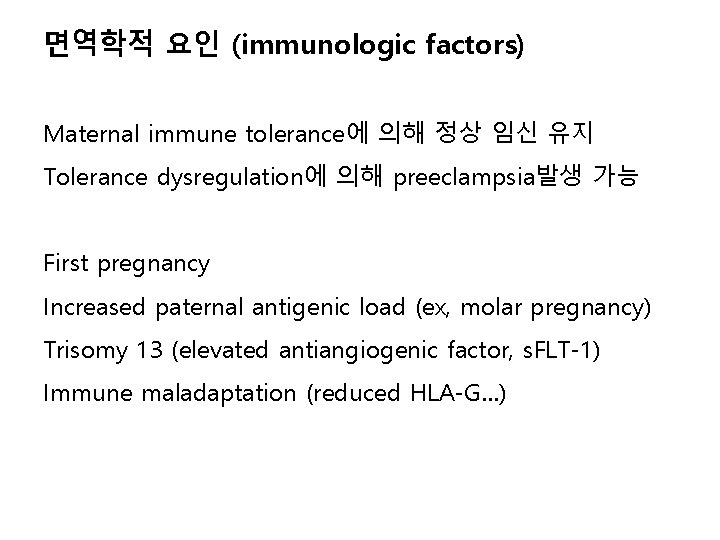
면역학적 요인 (immunologic factors) Maternal immune tolerance에 의해 정상 임신 유지 Tolerance dysregulation에 의해 preeclampsia발생 가능 First pregnancy Increased paternal antigenic load (ex, molar pregnancy) Trisomy 13 (elevated antiangiogenic factor, s. FLT-1) Immune maladaptation (reduced HLA-G…)
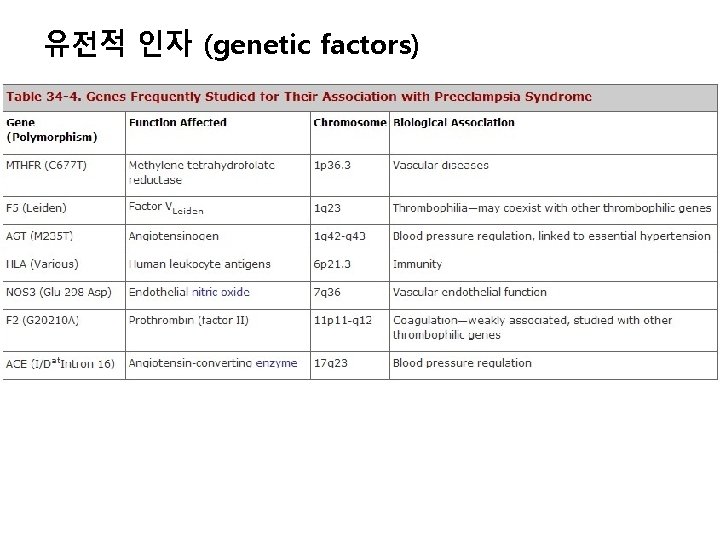
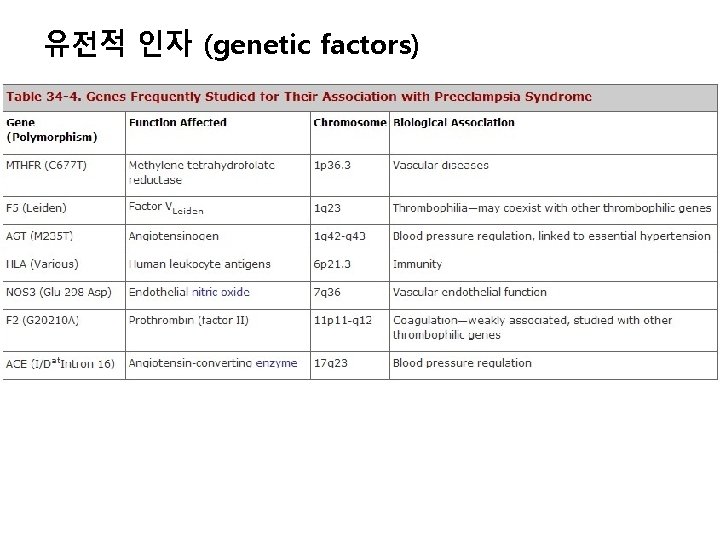
유전적 인자 (genetic factors)

Pathogenesis ① Vasospasm ② Endothelial cell activation ③ Endothelins ④ Angiogenic imbalance Angiogenic and antiangiogenic proteins: s. Flt-1, s. Eng

병태생리 Cardiovascular system - hyperdynamic Preeclampsia Normal pregnant women
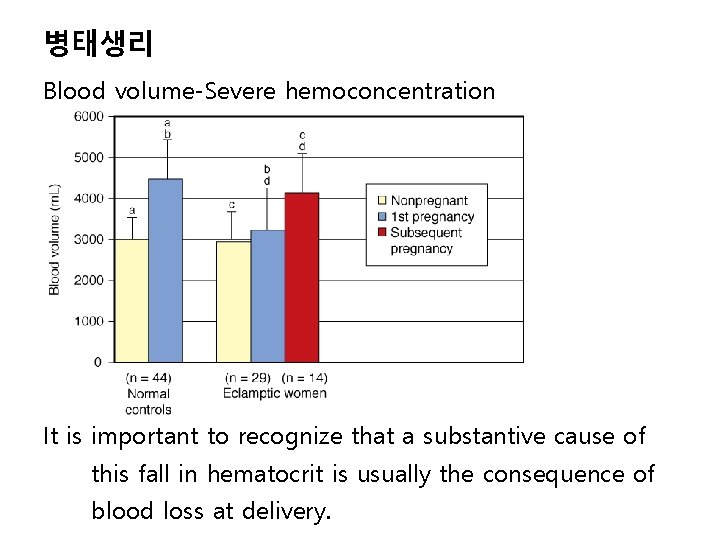
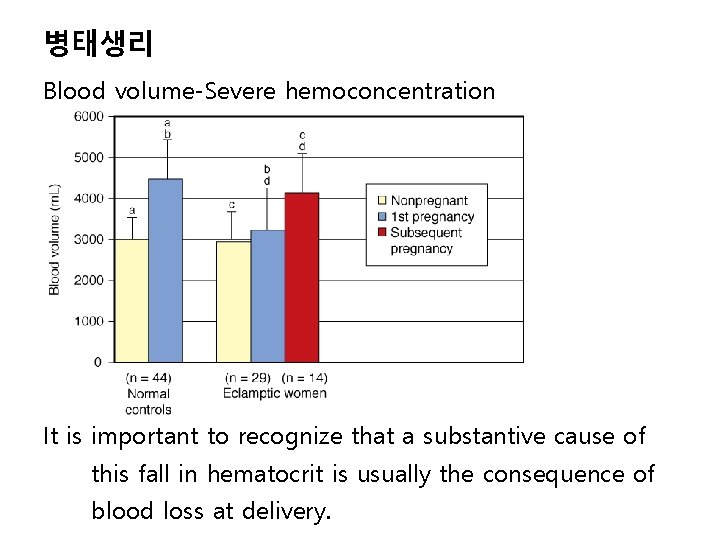
병태생리 Blood volume-Severe hemoconcentration It is important to recognize that a substantive cause of this fall in hematocrit is usually the consequence of blood loss at delivery.
병태생리 Blood and coagulation Thyrombocytopenia Hemolysis HELLP syndrome Coagulation – subtle changes like intravascular coagulation
병태생리 Volume homeostasis Endocrine changes: • renin, angiotensin II, angiotensin 1 -7, aldosterone의 감소 (정상임신에서는 증가) • Deoxycorticosterone 증가 • Vasopressin, atrial natriureic peptide 비슷 Fluid and electrolyte changes: • Extracellular fluid의 증가에 의한 edema
병태생리 Kidney – oliguria, prerenal ① Proteinuria (>300 mg/24 h) ② Anatomical changes ③ Acute renal failure (rare, mostly d/t hemorrhage)
병태생리 Liver HELLP syndrome – hemolysis, hepatocellular necrosis, thrombocytopenia • Symptomatic involvement – epigastric pain • Elevated AST and ALT • Hepatic hemorrhage, subcapsular hematoma, rupture ※ Acute fatty liver of pregnancy is sometimes confused with preelcampsia

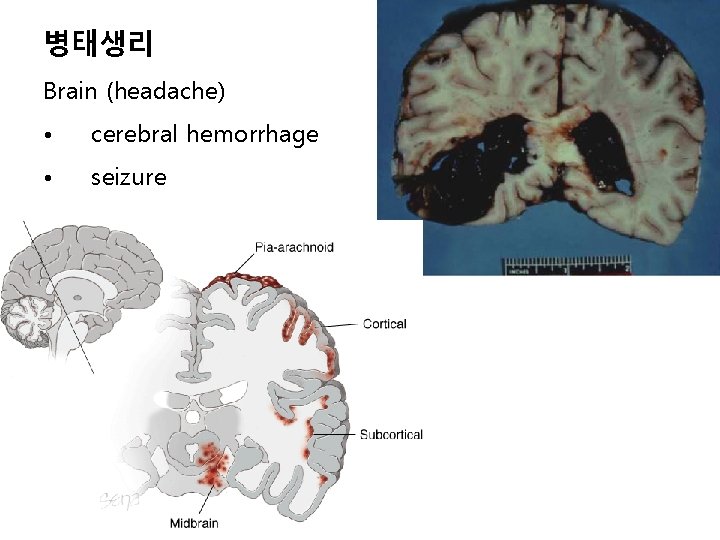
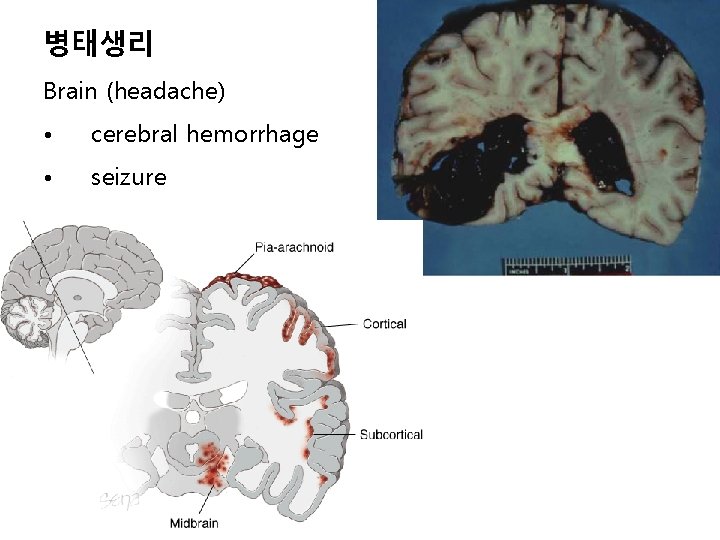
병태생리 Brain (headache) • cerebral hemorrhage • seizure
병태생리 Brain 임상증상 ① Headache and scotomata – magnesium sulfate투여 ② Convulsion – eclampsia ③ Blindness ④ Generalized cerebral edema – mental change
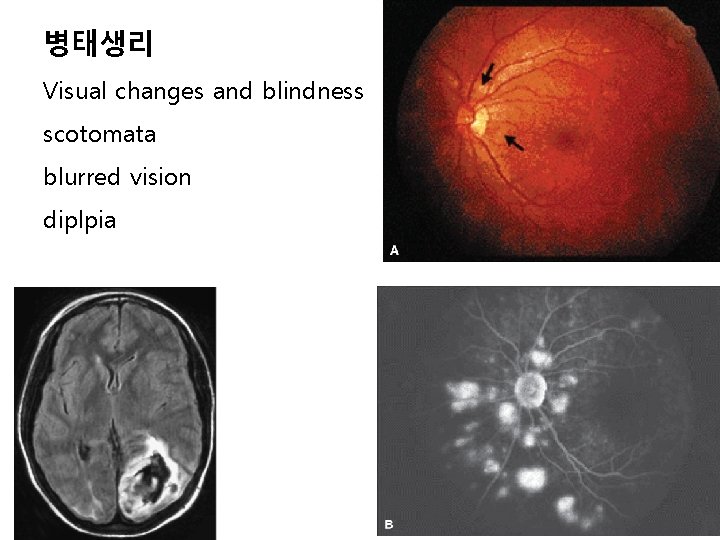
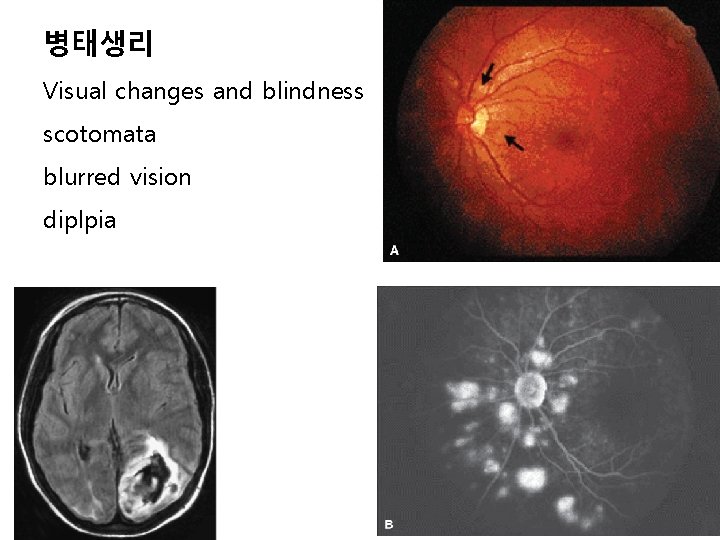
병태생리 Visual changes and blindness scotomata blurred vision diplpia
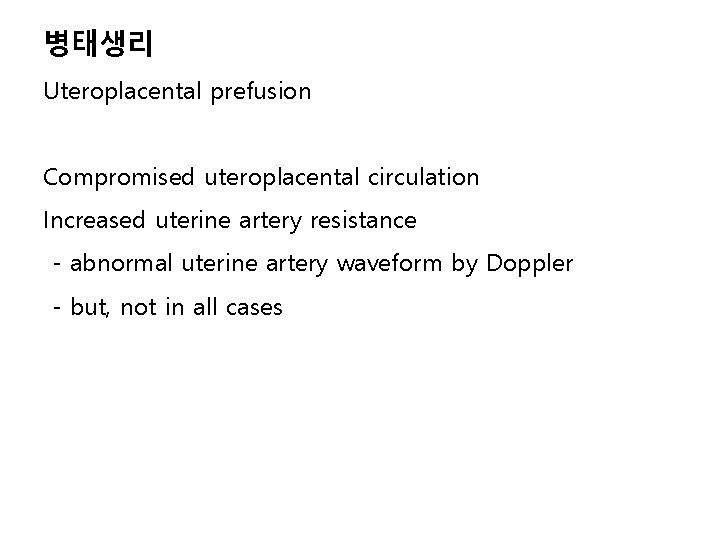
병태생리 Uteroplacental prefusion Compromised uteroplacental circulation Increased uterine artery resistance - abnormal uterine artery waveform by Doppler - but, not in all cases
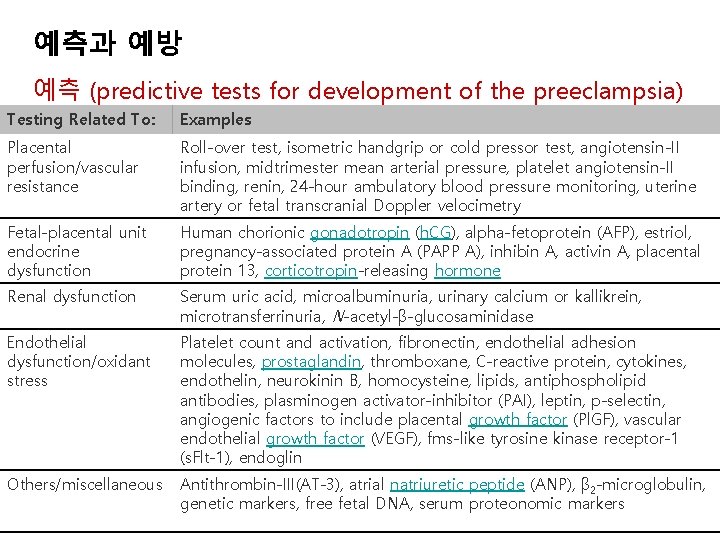
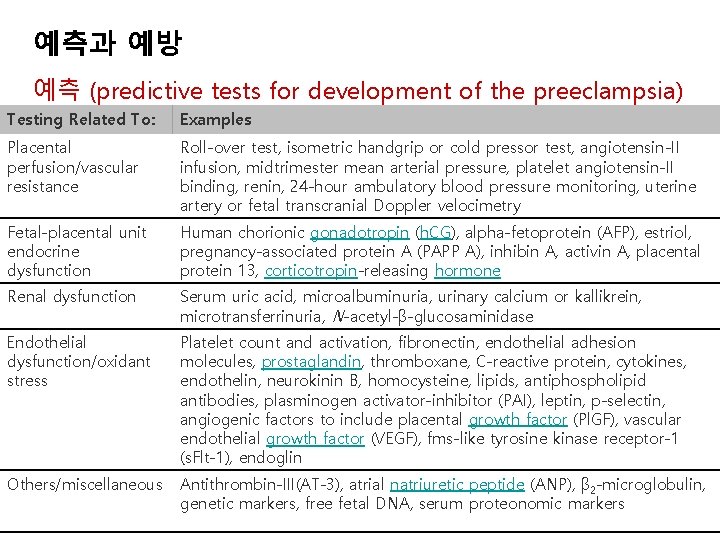
예측과 예방 예측 (predictive tests for development of the preeclampsia) Testing Related To: Examples Placental perfusion/vascular resistance Roll-over test, isometric handgrip or cold pressor test, angiotensin-II infusion, midtrimester mean arterial pressure, platelet angiotensin-II binding, renin, 24 -hour ambulatory blood pressure monitoring, uterine artery or fetal transcranial Doppler velocimetry Fetal-placental unit endocrine dysfunction Human chorionic gonadotropin (h. CG), alpha-fetoprotein (AFP), estriol, pregnancy-associated protein A (PAPP A), inhibin A, activin A, placental protein 13, corticotropin-releasing hormone Renal dysfunction Serum uric acid, microalbuminuria, urinary calcium or kallikrein, microtransferrinuria, N-acetyl-β-glucosaminidase Endothelial dysfunction/oxidant stress Platelet count and activation, fibronectin, endothelial adhesion molecules, prostaglandin, thromboxane, C-reactive protein, cytokines, endothelin, neurokinin B, homocysteine, lipids, antiphospholipid antibodies, plasminogen activator-inhibitor (PAI), leptin, p-selectin, angiogenic factors to include placental growth factor (Pl. GF), vascular endothelial growth factor (VEGF), fms-like tyrosine kinase receptor-1 (s. Flt-1), endoglin Others/miscellaneous Antithrombin-III(AT-3), atrial natriuretic peptide (ANP), β 2 -microglobulin, genetic markers, free fetal DNA, serum proteonomic markers
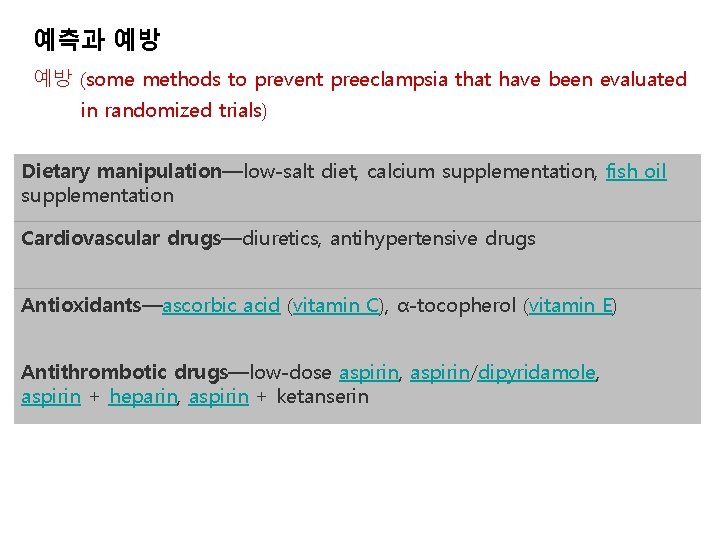
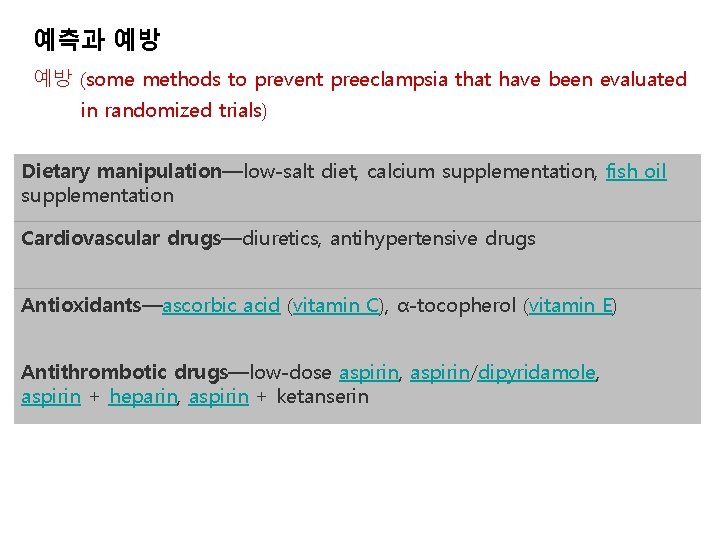
예측과 예방 예방 (some methods to prevent preeclampsia that have been evaluated in randomized trials) Dietary manipulation—low-salt diet, calcium supplementation, fish oil supplementation Cardiovascular drugs—diuretics, antihypertensive drugs Antioxidants—ascorbic acid (vitamin C), α-tocopherol (vitamin E) Antithrombotic drugs—low-dose aspirin, aspirin/dipyridamole, aspirin + heparin, aspirin + ketanserin

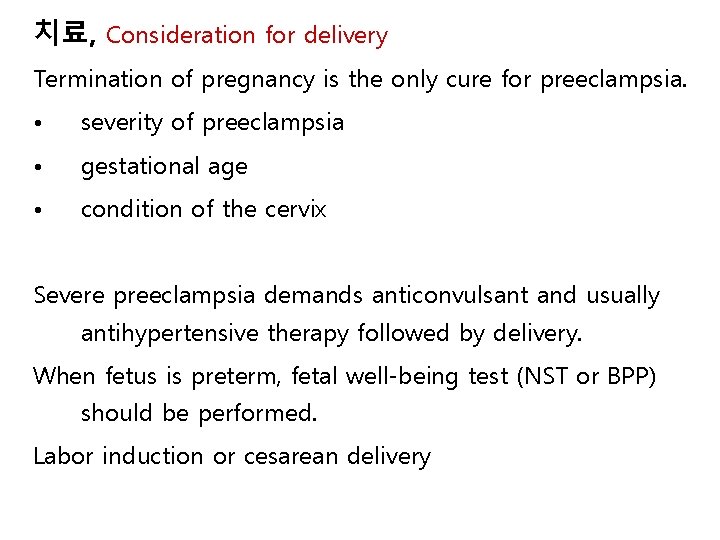
치료 ① Termination of pregnancy with the least possible trauma to mother and fetus ② Birth of an infant who subsequently thrives ③ Complete restoration of health to the mother One of the most important clinical questions for successful management is precise knowledge of fetal age.
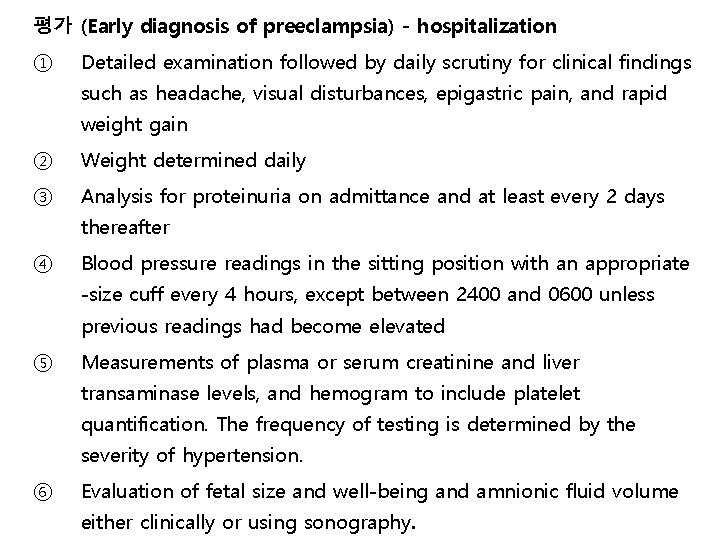
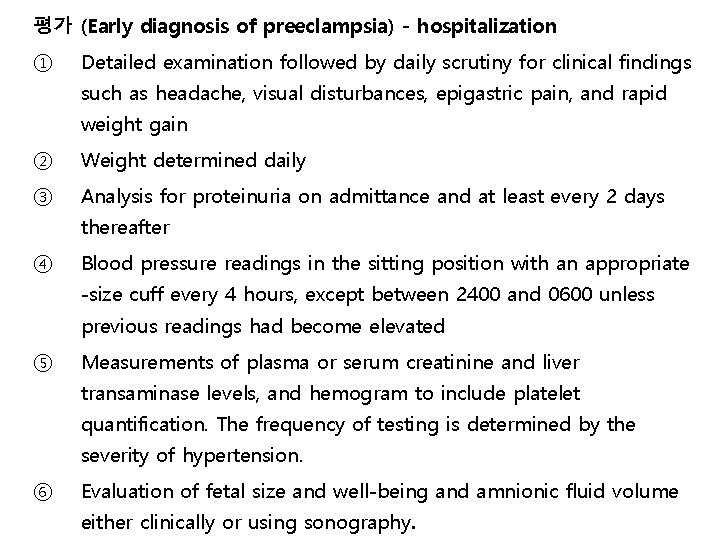
평가 (Early diagnosis of preeclampsia) - hospitalization ① Detailed examination followed by daily scrutiny for clinical findings such as headache, visual disturbances, epigastric pain, and rapid weight gain ② Weight determined daily ③ Analysis for proteinuria on admittance and at least every 2 days thereafter ④ Blood pressure readings in the sitting position with an appropriate -size cuff every 4 hours, except between 2400 and 0600 unless previous readings had become elevated ⑤ Measurements of plasma or serum creatinine and liver transaminase levels, and hemogram to include platelet quantification. The frequency of testing is determined by the severity of hypertension. ⑥ Evaluation of fetal size and well-being and amnionic fluid volume either clinically or using sonography.
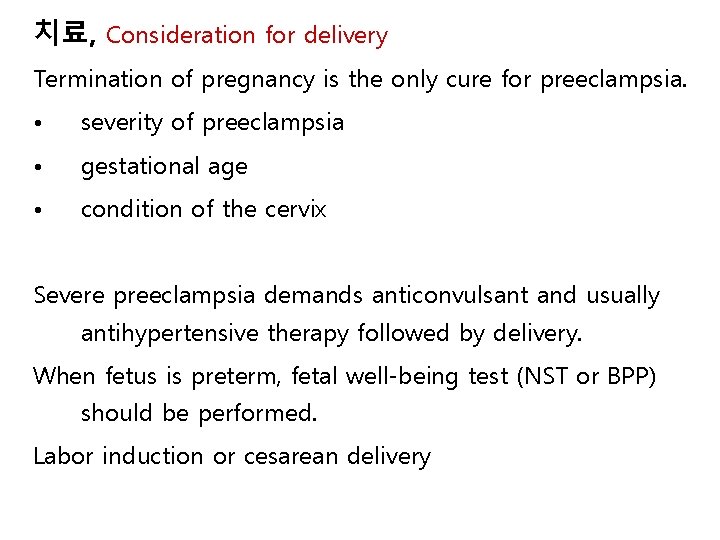
치료, Consideration for delivery Termination of pregnancy is the only cure for preeclampsia. • severity of preeclampsia • gestational age • condition of the cervix Severe preeclampsia demands anticonvulsant and usually antihypertensive therapy followed by delivery. When fetus is preterm, fetal well-being test (NST or BPP) should be performed. Labor induction or cesarean delivery

치료 Mild and moderate hypertension 1) hospitalization vs outpatient management 2) antihypertensive therapy
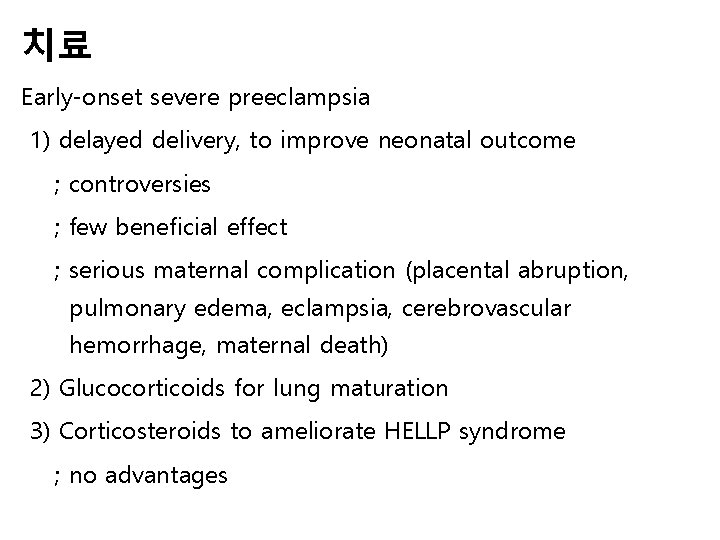
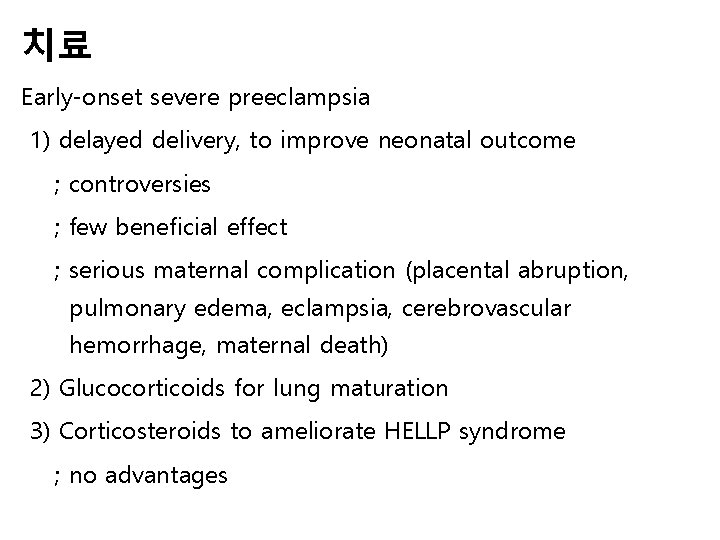
치료 Early-onset severe preeclampsia 1) delayed delivery, to improve neonatal outcome ; controversies ; few beneficial effect ; serious maternal complication (placental abruption, pulmonary edema, eclampsia, cerebrovascular hemorrhage, maternal death) 2) Glucocorticoids for lung maturation 3) Corticosteroids to ameliorate HELLP syndrome ; no advantages
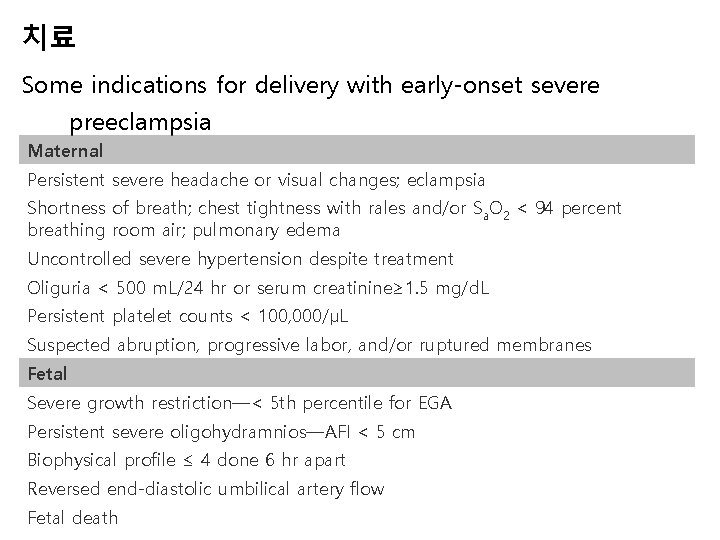
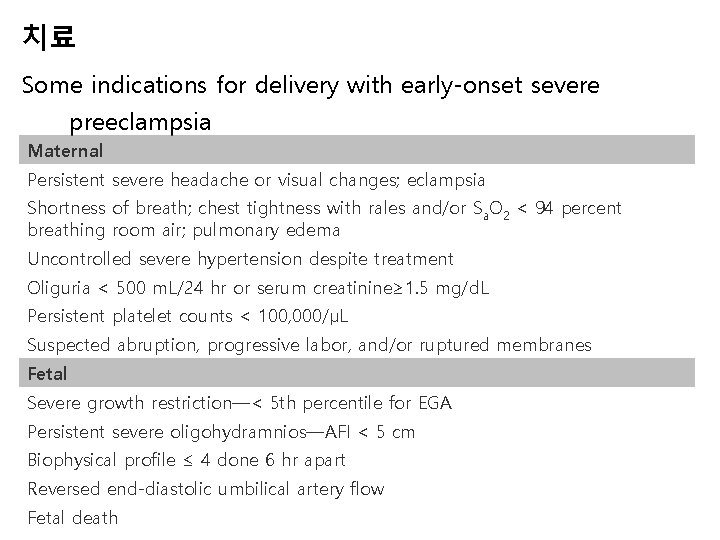
치료 Some indications for delivery with early-onset severe preeclampsia Maternal Persistent severe headache or visual changes; eclampsia Shortness of breath; chest tightness with rales and/or Sa. O 2 < 94 percent breathing room air; pulmonary edema Uncontrolled severe hypertension despite treatment Oliguria < 500 m. L/24 hr or serum creatinine≥ 1. 5 mg/d. L Persistent platelet counts < 100, 000/µL Suspected abruption, progressive labor, and/or ruptured membranes Fetal Severe growth restriction—< 5 th percentile for EGA Persistent severe oligohydramnios—AFI < 5 cm Biophysical profile ≤ 4 done 6 hr apart Reversed end-diastolic umbilical artery flow Fetal death
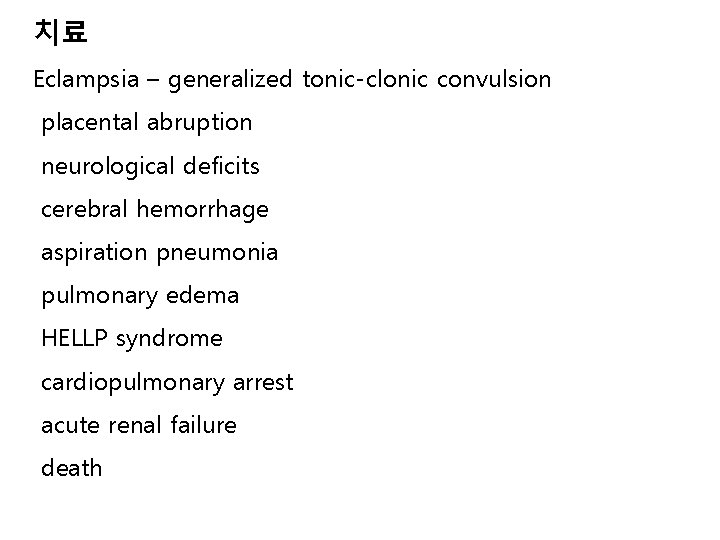
치료 Eclampsia – generalized tonic-clonic convulsion placental abruption neurological deficits cerebral hemorrhage aspiration pneumonia pulmonary edema HELLP syndrome cardiopulmonary arrest acute renal failure death

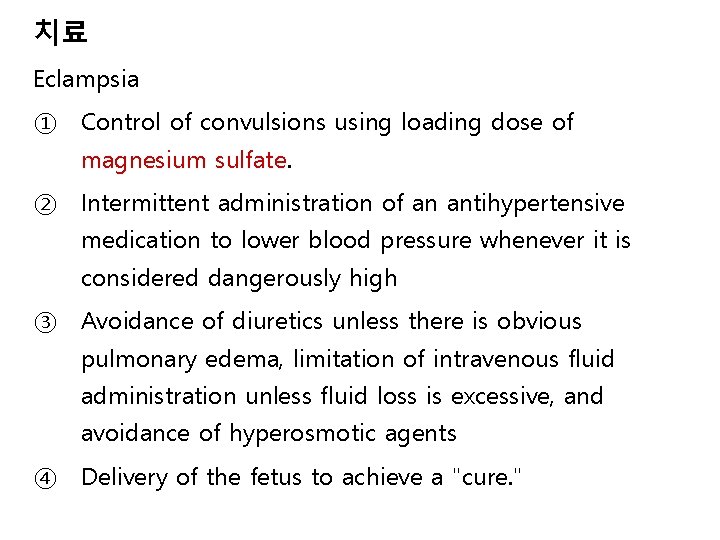
치료 Eclampsia ① Control of convulsions using loading dose of magnesium sulfate. ② Intermittent administration of an antihypertensive medication to lower blood pressure whenever it is considered dangerously high ③ Avoidance of diuretics unless there is obvious pulmonary edema, limitation of intravenous fluid administration unless fluid loss is excessive, and avoidance of hyperosmotic agents ④ Delivery of the fetus to achieve a "cure. "
Magnesium sulfate to control convulsions eclampsia severe preeclampsia given magnesium sulfate during labor and for 24 hours postpartum is not given to treat hypertension is continued for 24 hours after delivery for eclampsia, continued for 24 hours after the onset of convulsion
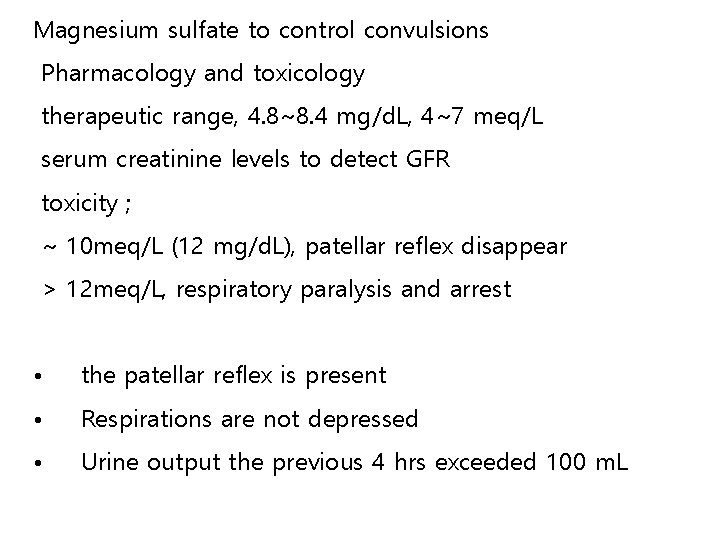
Magnesium sulfate to control convulsions Pharmacology and toxicology therapeutic range, 4. 8~8. 4 mg/d. L, 4~7 meq/L serum creatinine levels to detect GFR toxicity ; ~ 10 meq/L (12 mg/d. L), patellar reflex disappear > 12 meq/L, respiratory paralysis and arrest • the patellar reflex is present • Respirations are not depressed • Urine output the previous 4 hrs exceeded 100 m. L
Magnesium sulfate to control convulsions toxicology • calcium gluconate or calcium chloride, 1 g intravenously, along withholding further magnesium sulfate, usually reverses mild to moderate respiratory depression. • Prompt tracheal intubation and mechanical ventilation Uterine effects – did not significantly alter the need for oxytocin stimulation of labor Fetal effects – neuroprotection for VLBW
Management of severe hypertension SBP ≥ 160 mm. Hg or DBP ≥ 110 mm. Hg ① Hydralazine 5 mg (IV) q 15 -20 min ② Labetolol 10~20 mg (IV) q 10 min ③ Nifedipine 10 mg (PO) q 30 min ④ Diuretics-not used to lower blood pressure to treatment of pulmonary edema ※ fluid therapy – Lactated Ringer’s solution 60 -125 m. L/h
Prevention of eclampsia Who should be given magnesium sulfate? Severe preeclampsia should be given magnesium sulfate prophylaxis. Selective vs universal magnesium sulfate prophylaxis
Delivery Eclampsia Cesarean delivery Vaginal delivery, labor induction, often labor spontaneously These women, who consequently lack normal pregnancy hypervolemia, are much less tolerant of even normal blood loss than are normotensive pregnant women. Counseling for future pregnancies higher risk for hypertension in the second pregnancy
Long-term sequences Cardiovascular and neurovascular morbidity hypertension ischemic heart disease stroke Renal sequelae chronic renal disease Neurological sequelae

 Gestational hypertension
Gestational hypertension Absence management formerly aesop
Absence management formerly aesop Bank alfalah formerly
Bank alfalah formerly Salish design
Salish design Formerly restricted data
Formerly restricted data Spanish nanny goat
Spanish nanny goat Two pipe system drainage
Two pipe system drainage Term biodiversity was given by
Term biodiversity was given by Diagnostic criteria of preeclampsia
Diagnostic criteria of preeclampsia Nhbep
Nhbep Magnesium sulfate and urine output
Magnesium sulfate and urine output Pre eclampsia screening
Pre eclampsia screening Nom preeclampsia
Nom preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Preeclampsia teaching
Preeclampsia teaching Management
Management Superimposed preeclampsia
Superimposed preeclampsia Preeclampsia intervenciones de enfermeria
Preeclampsia intervenciones de enfermeria Superimposed preeclampsia
Superimposed preeclampsia Diagnostic criteria of preeclampsia
Diagnostic criteria of preeclampsia Magnesium sulfate toxicity level
Magnesium sulfate toxicity level Superimposed preeclampsia
Superimposed preeclampsia Mild preeclampsia
Mild preeclampsia Complications of gestational diabetes
Complications of gestational diabetes Labatalol
Labatalol Gestational age chart
Gestational age chart Asymmetrical iugr
Asymmetrical iugr Ponderal index in iugr
Ponderal index in iugr Macrosomia
Macrosomia Blighted ovum treatment
Blighted ovum treatment Gestational age in weeks
Gestational age in weeks Fidelma dunne
Fidelma dunne Complication of gestational diabetes
Complication of gestational diabetes Fundal height
Fundal height Classification of high risk newborn
Classification of high risk newborn Caci asthma worksheet
Caci asthma worksheet Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Conclusion of hypertension
Conclusion of hypertension Dash diet
Dash diet Pulmonary hypertension severity
Pulmonary hypertension severity Jnc 8 classification of hypertension
Jnc 8 classification of hypertension Demadex
Demadex Rules of halves in hypertension
Rules of halves in hypertension Hyperkaliémie cause
Hyperkaliémie cause Diagnosis hypertension
Diagnosis hypertension Chief complaint present illness
Chief complaint present illness Case scenario for hypertension
Case scenario for hypertension Diueritique
Diueritique