Eclampsia and Severe Preeclampsia ESMOE Importance of preeclampsia
- Slides: 21
Eclampsia and Severe Preeclampsia ESMOE
Importance of pre-/eclampsia No 1 direct cause of Maternal Mortality (MM) and No 2 overall cause of MM in RSA ü 60% of deaths are associated with substandard care Pre-eclampsia is a disease of the endothelium and therefore potentially always multi-organ
Diagnosis: Hypertension (HT) in pregnancy Systolic BP > 140 mm. Hg or a diastolic BP > 90 mm. Hg on more than 2 occasions at least 6 hours apart Severe HT is a BP of more than 160/110 mm. Hg Gestational HT and pre-eclampsia are diagnosed after 20 weeks.
Diagnosis of Pre-eclampsia Hypertension after 20 weeks with 1 or more of the following: – Proteinuria – Renal impairment – Liver impairment – Haematological impairment – Neurological impairment – Growth restriction The range of organs affected are a result of endothelial dysfunction
Principles of management Stabilise mother and then deliver fetus Treat and prevent fits Treat raised blood pressure (BP) Attention to fluid balance Be aware of and prevent complications
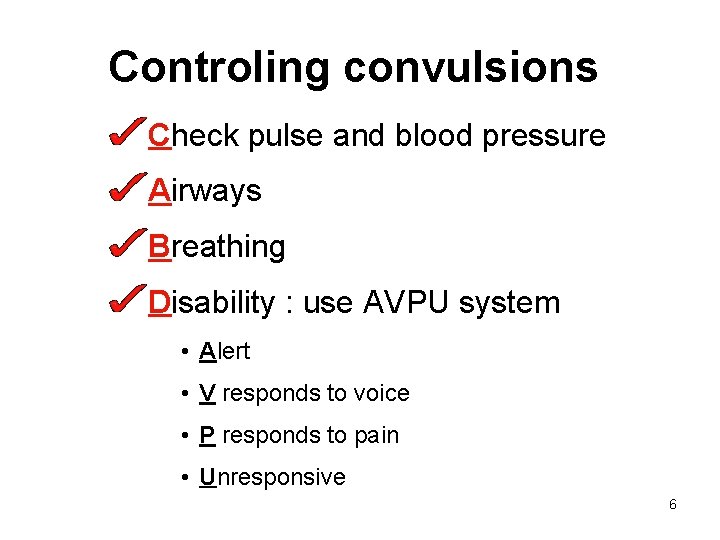
Controling convulsions Check pulse and blood pressure Airways Breathing Disability : use AVPU system • Alert • V responds to voice • P responds to pain • Unresponsive 6
Fitting or unconscious Call for help Left lateral position Check pulse and blood pressure Assess and if necessary, maintain airway Oxygen and assess breathing Establish fluid balance – urinary catheter 7
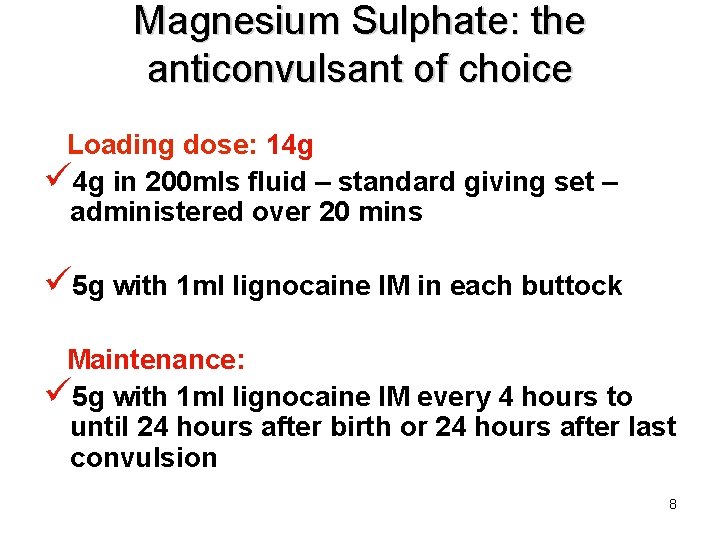
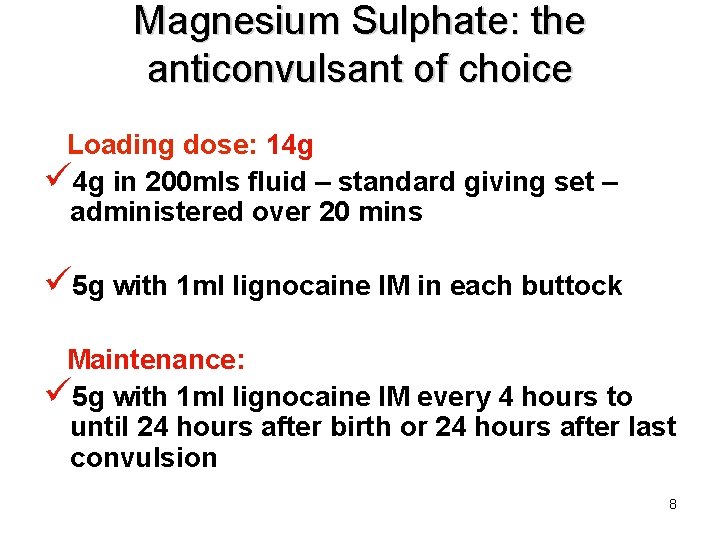
Magnesium Sulphate: the anticonvulsant of choice Loading dose: 14 g ü 4 g in 200 mls fluid – standard giving set – administered over 20 mins ü 5 g with 1 ml lignocaine IM in each buttock Maintenance: ü 5 g with 1 ml lignocaine IM every 4 hours to until 24 hours after birth or 24 hours after last convulsion 8
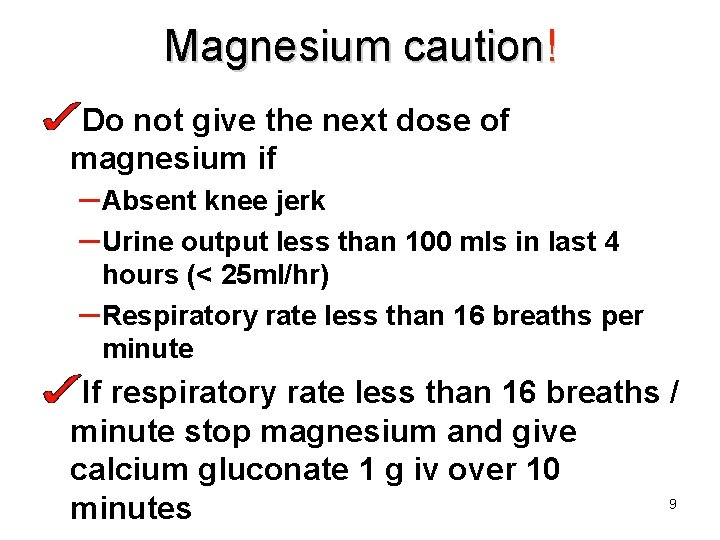
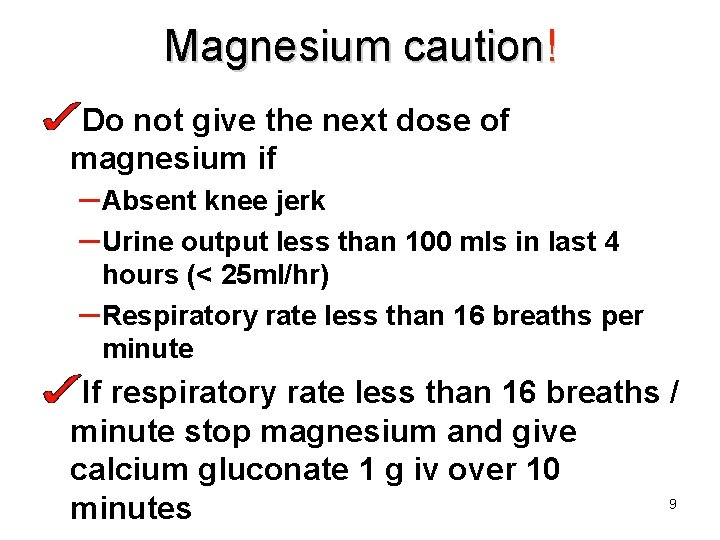
Magnesium caution! Do not give the next dose of magnesium if – Absent knee jerk – Urine output less than 100 mls in last 4 hours (< 25 ml/hr) – Respiratory rate less than 16 breaths per minute If respiratory rate less than 16 breaths / minute stop magnesium and give calcium gluconate 1 g iv over 10 9 minutes
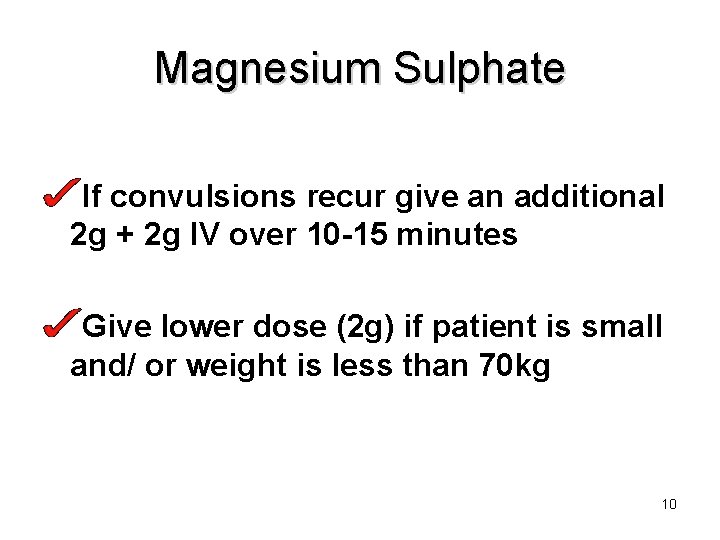
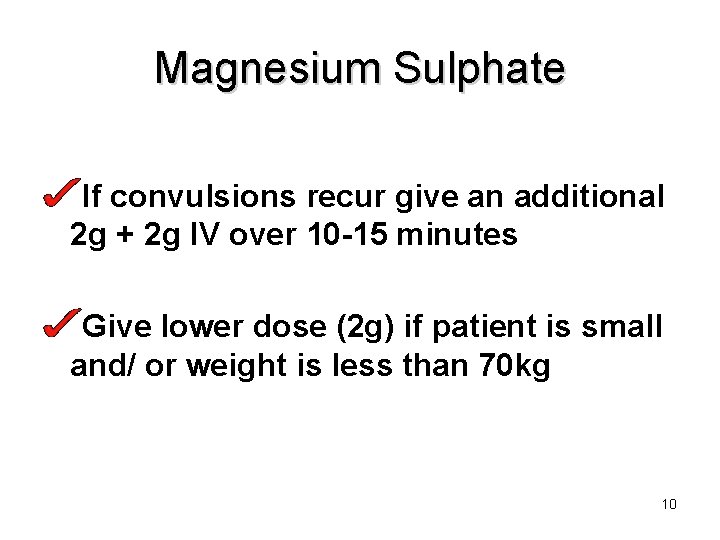
Magnesium Sulphate If convulsions recur give an additional 2 g + 2 g IV over 10 -15 minutes Give lower dose (2 g) if patient is small and/ or weight is less than 70 kg 10
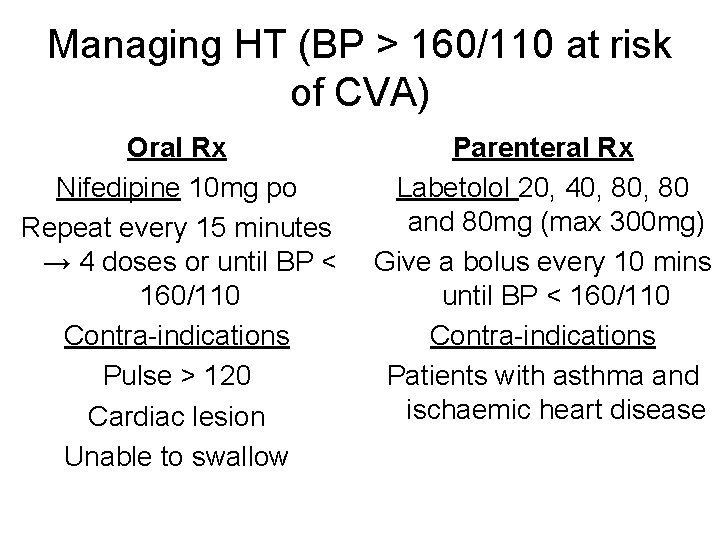
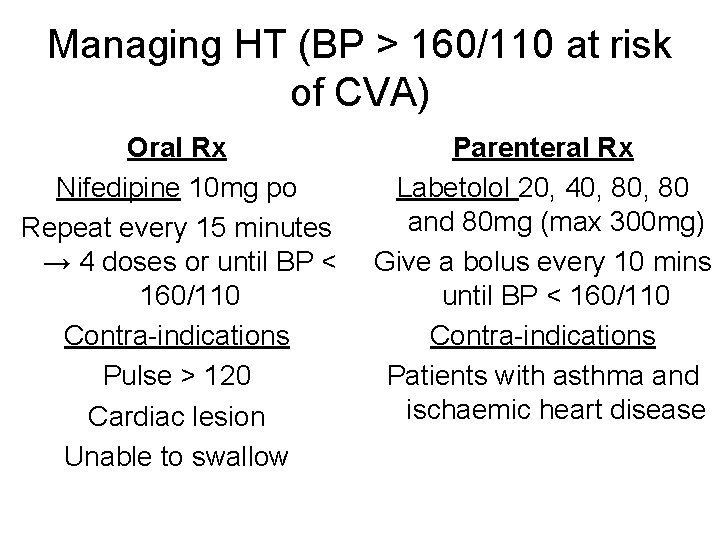
Managing HT (BP > 160/110 at risk of CVA) Oral Rx Nifedipine 10 mg po Repeat every 15 minutes → 4 doses or until BP < 160/110 Contra-indications Pulse > 120 Cardiac lesion Unable to swallow Parenteral Rx Labetolol 20, 40, 80 and 80 mg (max 300 mg) Give a bolus every 10 mins until BP < 160/110 Contra-indications Patients with asthma and ischaemic heart disease
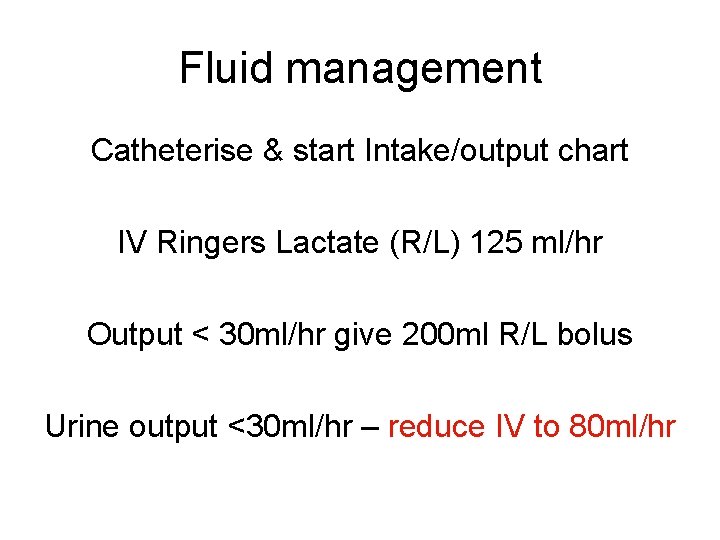
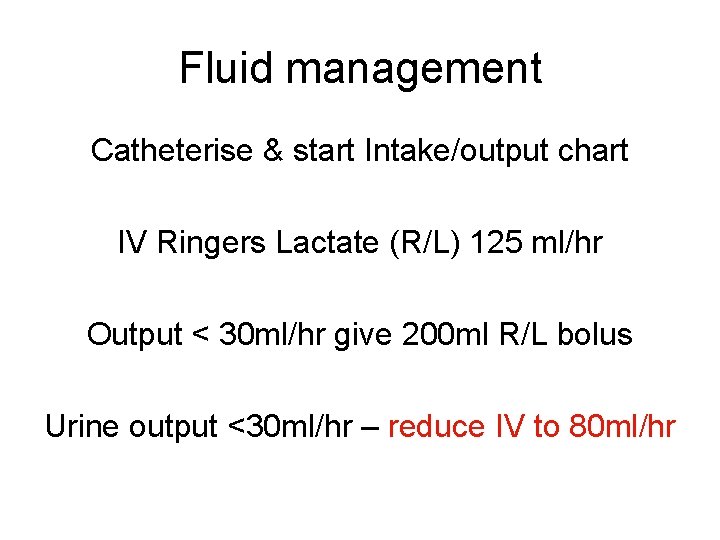
Fluid management Catheterise & start Intake/output chart IV Ringers Lactate (R/L) 125 ml/hr Output < 30 ml/hr give 200 ml R/L bolus Urine output <30 ml/hr – reduce IV to 80 ml/hr
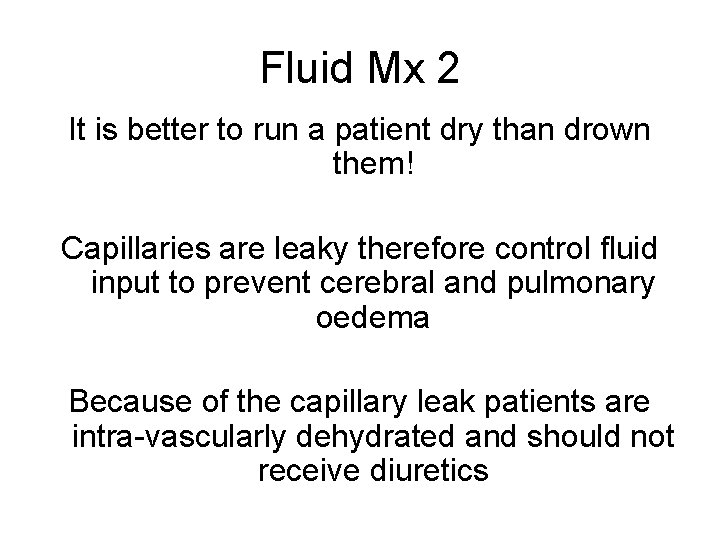
Fluid Mx 2 It is better to run a patient dry than drown them! Capillaries are leaky therefore control fluid input to prevent cerebral and pulmonary oedema Because of the capillary leak patients are intra-vascularly dehydrated and should not receive diuretics
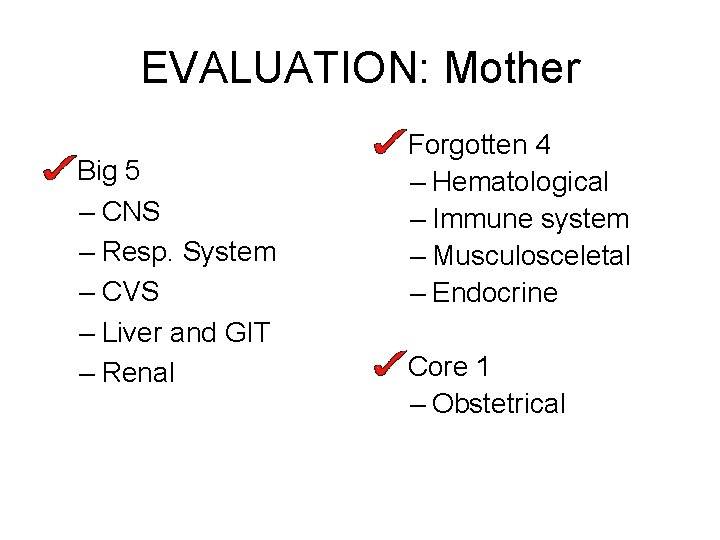
EVALUATION: Mother Big 5 – CNS – Resp. System – CVS – Liver and GIT – Renal Forgotten 4 – Hematological – Immune system – Musculosceletal – Endocrine Core 1 – Obstetrical
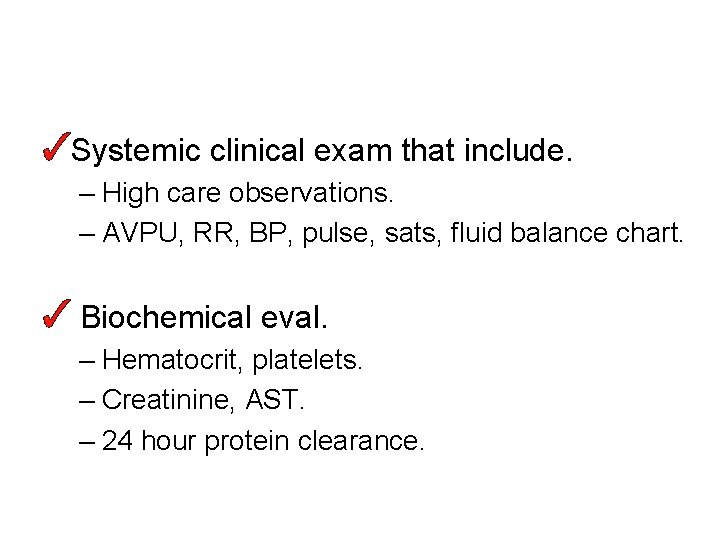
Systemic clinical exam that include. – High care observations. – AVPU, RR, BP, pulse, sats, fluid balance chart. Biochemical eval. – Hematocrit, platelets. – Creatinine, AST. – 24 hour protein clearance.
Maternal stabilisation Is only complete when the lab results are back and this allows evaluation of the organ systems (can do bedside Hb & clotting time if lab slow/unavailable) It is not appropriate to monitor the fetus prior to this
Evaluation of fetus Evaluate fetus for viability If viable give 12 mg betamethasone Arrange transfer or Consult re-termination of pregnancy There is no place for expectant management in district hospitals!
Delivery Pre-eclampsia is a disease of pregnancy and the only cure is to end the pregnancy Terminate pre-viable pregnancies Vaginal delivery at an appropriate level of care is optimal It is often necessary to individualise Mx
After delivery Monitor in a “designated area” until diuresis occurs Remember (pre-)eclampsia can get worse or first fit can occur in post partum period Continue magnesium for 24 hours – no need to “tail off” Continue antihypertensives 19
Recap Recognition of Eclampsia and Severe preeclampsia Resuscitation and drug management Use of Magnesuim sulphate Monitoring of patients on magnesium sulphate Fluid management Complications of (pre-) eclampsia Delivery of a patient with eclampsia or preeclampsia
 Magnesium sulfate toxicity level
Magnesium sulfate toxicity level Anc card
Anc card Eden's criteria for eclampsia
Eden's criteria for eclampsia Mgso4 mechanism of action in eclampsia
Mgso4 mechanism of action in eclampsia Complications of eclampsia
Complications of eclampsia Eclampsia definicion
Eclampsia definicion Eclampsia symptoms
Eclampsia symptoms Maternal causes of polyhydramnios
Maternal causes of polyhydramnios Hellp syndrome symptoms
Hellp syndrome symptoms Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Preeclampsia teaching
Preeclampsia teaching Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Superimposed preeclampsia
Superimposed preeclampsia Diagnosticos de enfermeria para preeclampsia
Diagnosticos de enfermeria para preeclampsia Pregnancy trimester breakdown
Pregnancy trimester breakdown Magnesium sulfate and urine output
Magnesium sulfate and urine output Management
Management Diagnostic criteria of preeclampsia
Diagnostic criteria of preeclampsia Norma 017 epidemiologia
Norma 017 epidemiologia Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms