Review of Antenatal Care ESMOE What is the






- Slides: 69
Review of Antenatal Care ESMOE

What is the aim of Antenatal Care? To end up with a happy mum and healthy baby
What Are The Principles Of Antenatal Care?
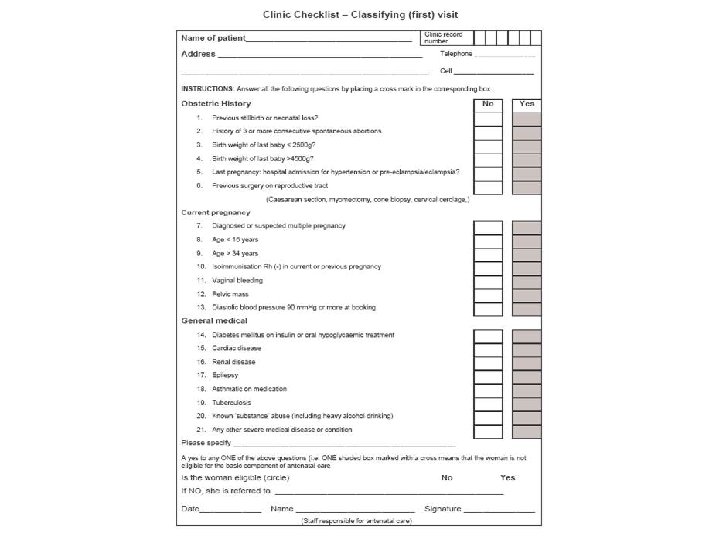
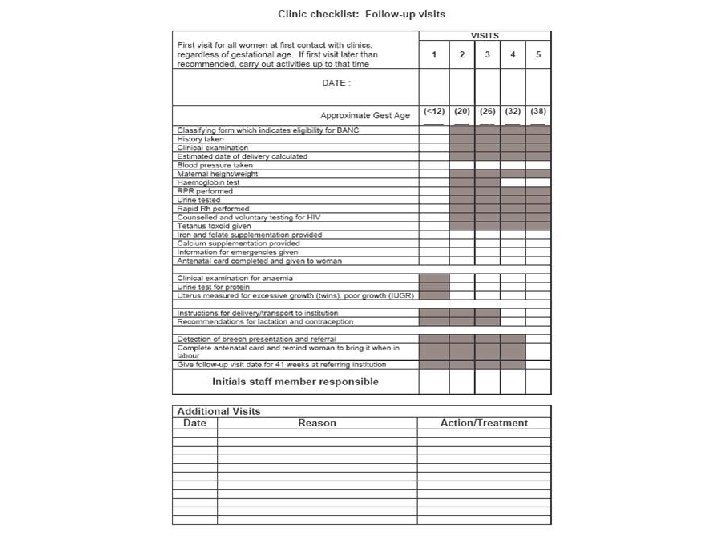
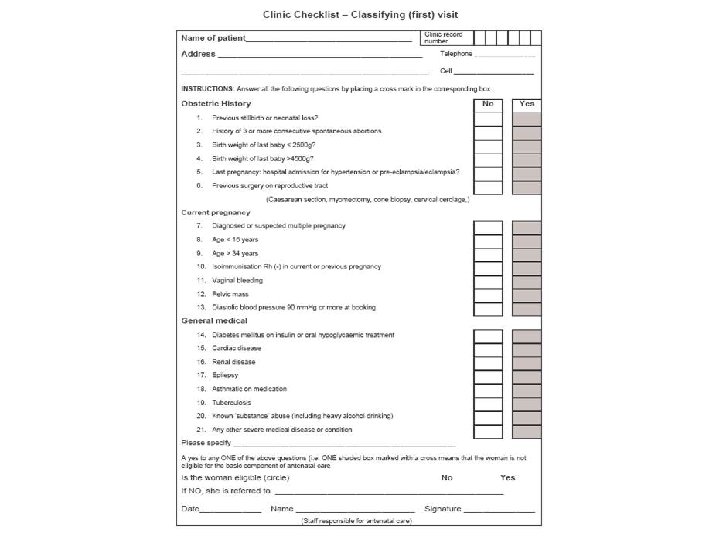
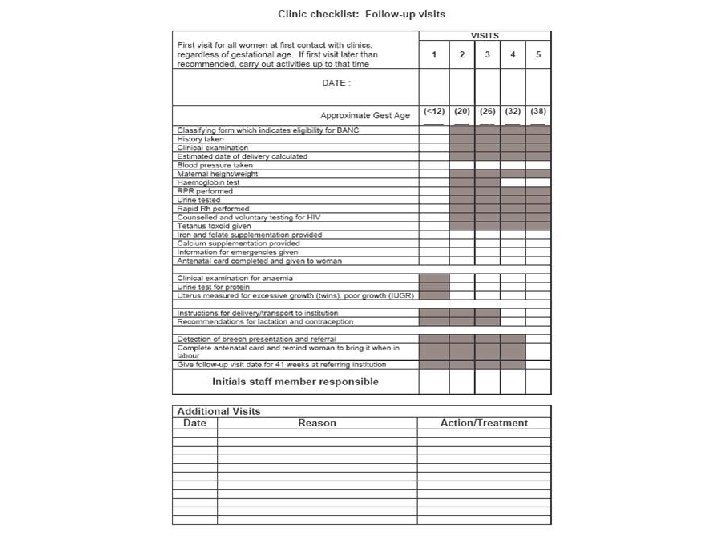
The Principles of Basic Antenatal Care (BANC) • Simple checklist for problem identification • Risk assessment & appropriate level of care • Balancing visit: benefit ratio • Only doing appropriate On-site testing • Having a definite plan for ANC • Respectful care
It is essential to understand the importance of antenatal care and realise that a poorly planned ANC programme is little better than no antenatal care
Past obstetric history Past pregnancy performance is the single most important outcome predictor for the current pregnancy • Past perinatal death • Previous preterm labour • Previous caesarean section (C/S) • History of ante- or postpartum haemorrhage
The Bottom Line Is……. You cannot manage a problem if you have not identified it!!!
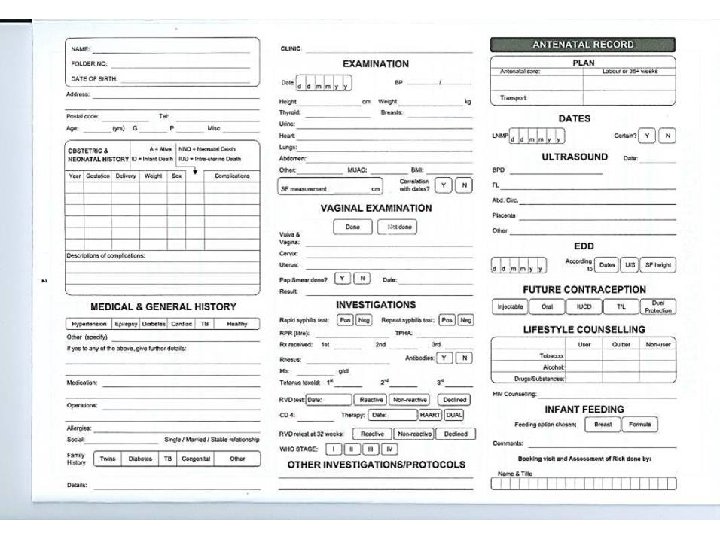
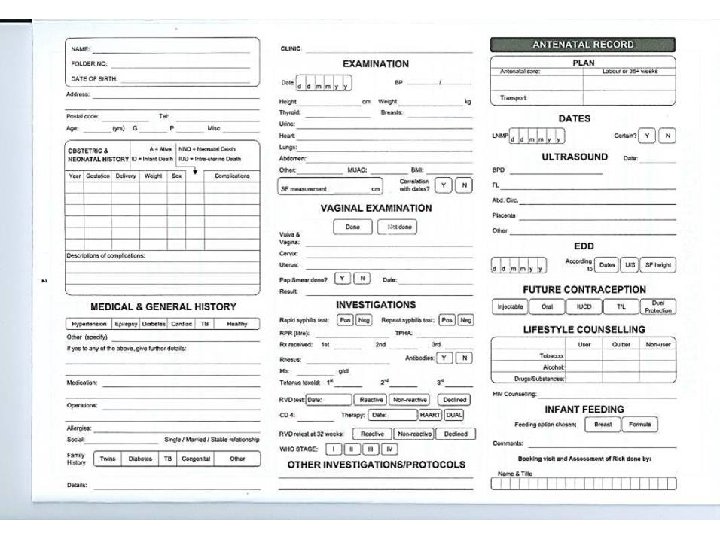
Booking visit Full history (including TB screen) Examination Pregnancy duration established and recorded Screening tests First assessment of risk factors (Problem list)
Dating this pregnancy - EDD Gestational age LNMP/LMP Uterine size - 4 -12 weeks - 13 -24 weeks - 24 -36 weeks Ultrasound (up to 24 weeks) Estimated fetal mass RECORD AND EXPLAIN
Definitions Gravidity (G) Number of previous pregnancies Parity (P) Number of pregnancies to reach viability irrespective of outcome or number
General examination General impression Pulse, BP, temperature, respiratory rate System examination Abdominal examination Per vaginal examination (PV) if indicated Side room investigations
Routine testing – must be done on-site Rapid RPR Rapid Rh Anaemia screen HIV MUAC Dipstix for protein and glucose
Final assessment Identification of problems and risks Antenatal care plan
Subsequent Visits Screen card History (including TB screen) Check EDD Examination Update the problem list Modify the plan

Educational Opportunity ü Encourage ANC attendance ü Pregnancy warning signs: • Reduced fetal movements • Vaginal bleeding • Rupture of membranes • Abdominal pain (not discomfort) • Severe headache • Report early in labour ü Self care & delivery ü Breast feeding ü Immunization ü Contraception ü HIV & STD’s ü MOM connect
Why Is It Important To Complete The Card? Because if it is not done problems will be not be identified The patient will not be treated correctly
Problem List & Notes Ø Be aware that the problems change as pregnancy progresses Ø Short and to the point! Ø Alert HCW at next visit to intervention

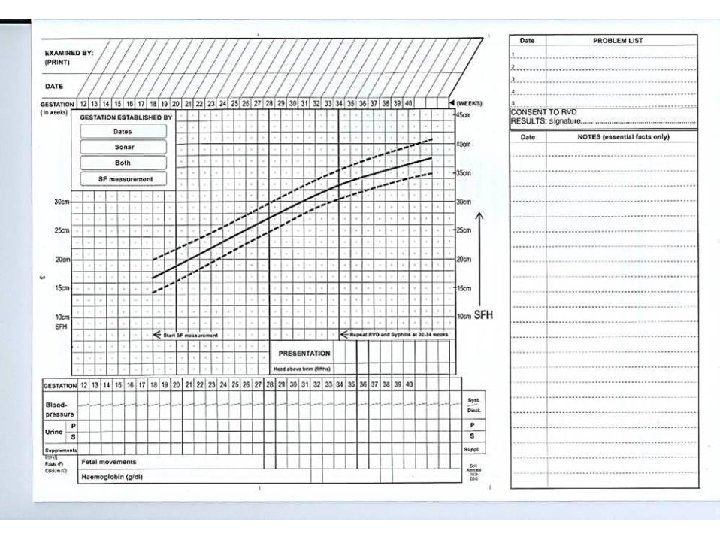
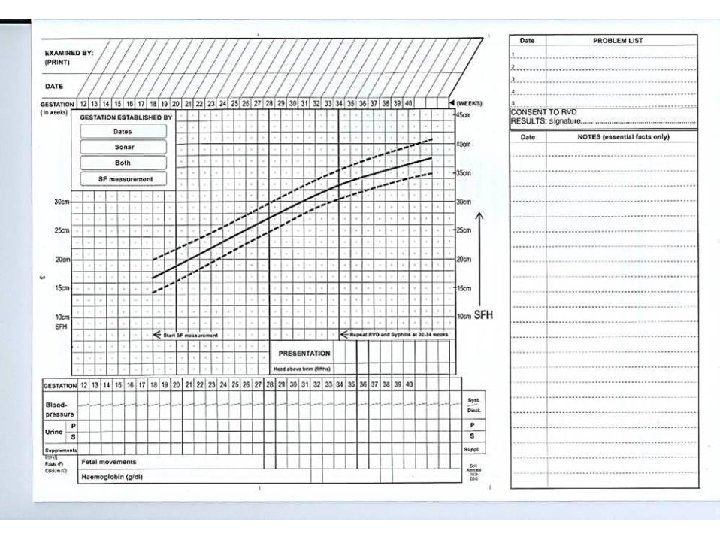
Monitoring Fetal Growth
Measuring The SFH • Make sure the bladder is not full • Let the woman lie comfortably on her back • Identify highest point of fundus. This might not be in the midline

Measuring The SFH • Mark the highest point of the fundus with a ball-point pen (ask for permission first) • Do not correct dextroversion of the uterus or exert pressure on the fundus

Measuring The SFH • Fix the zero of the tape measure at the top of the symphysis and stretch the tape over the curve of the uterus up to the pen mark • Read the measurement to nearest cm

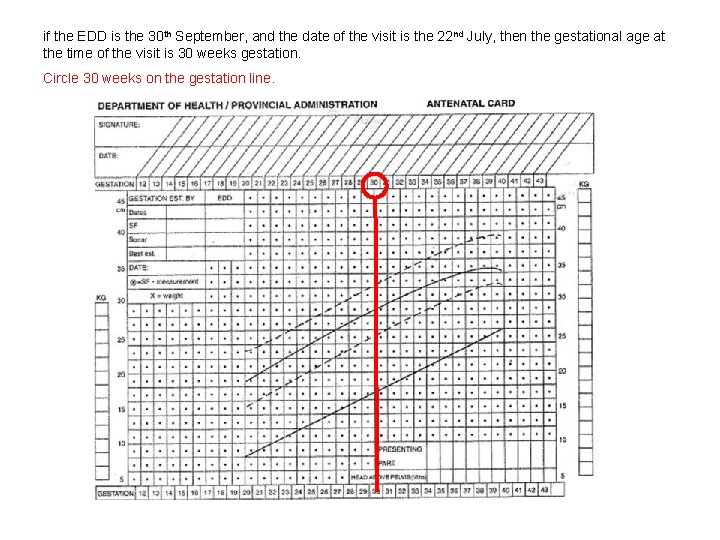
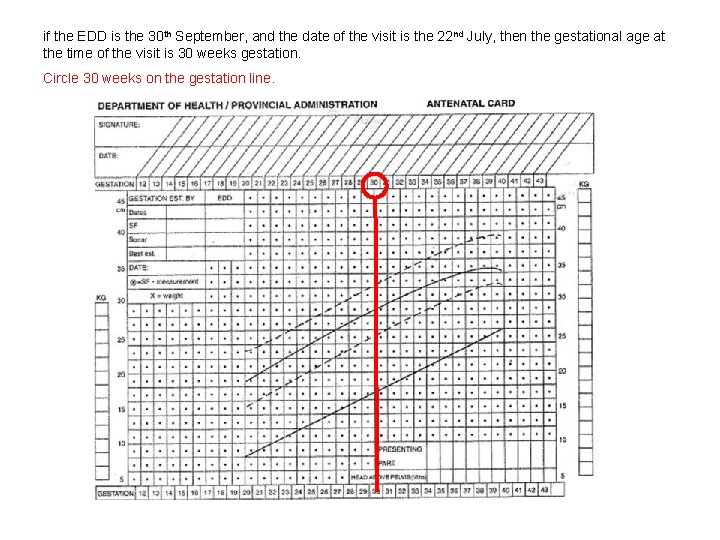
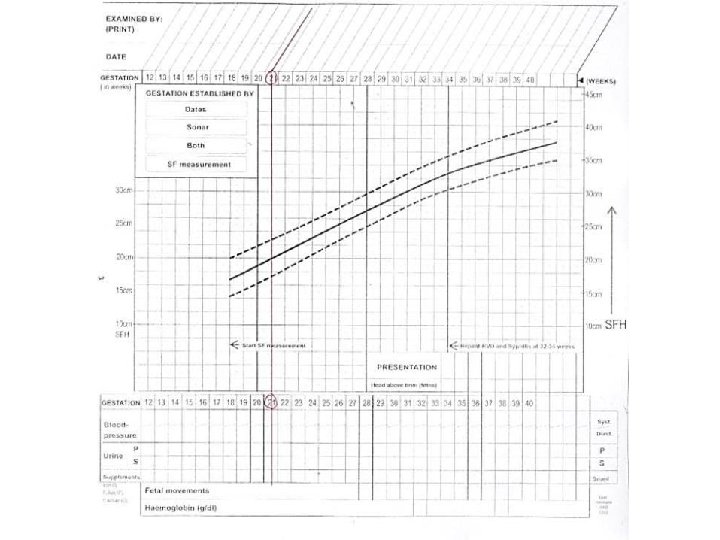
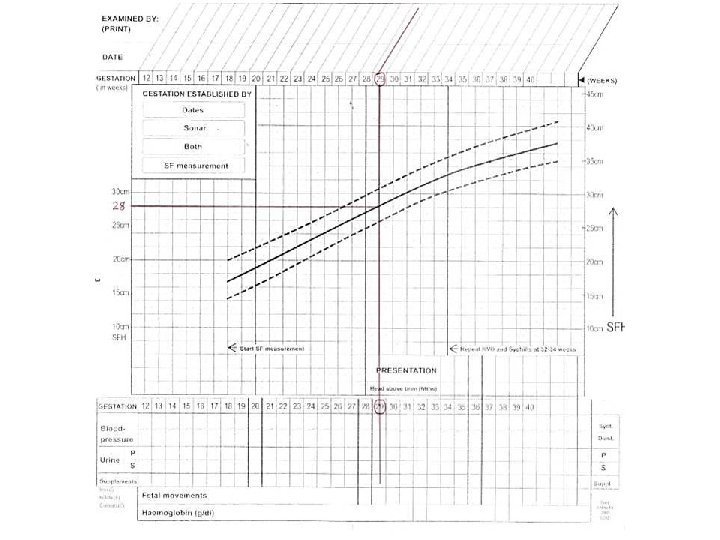
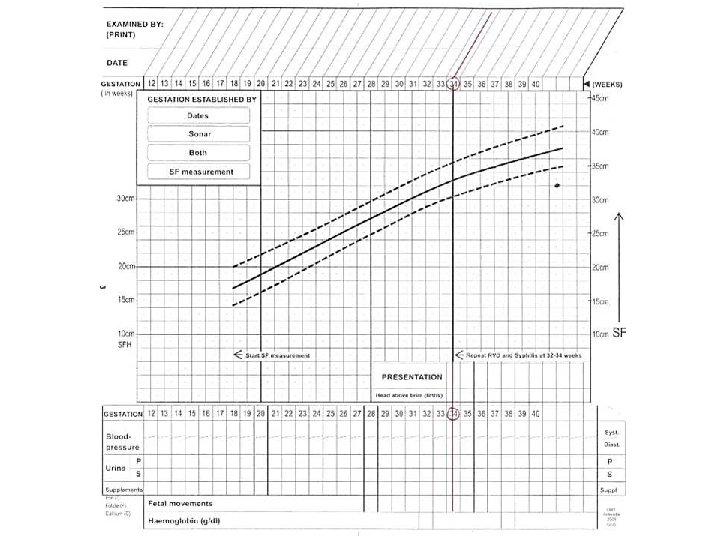
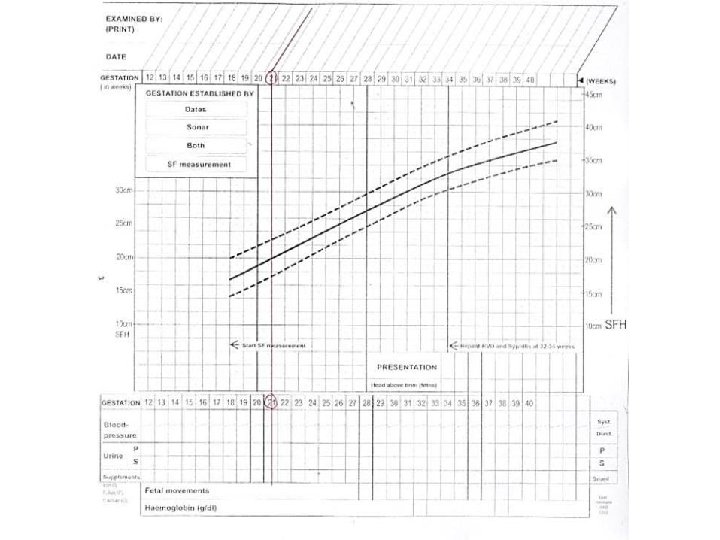
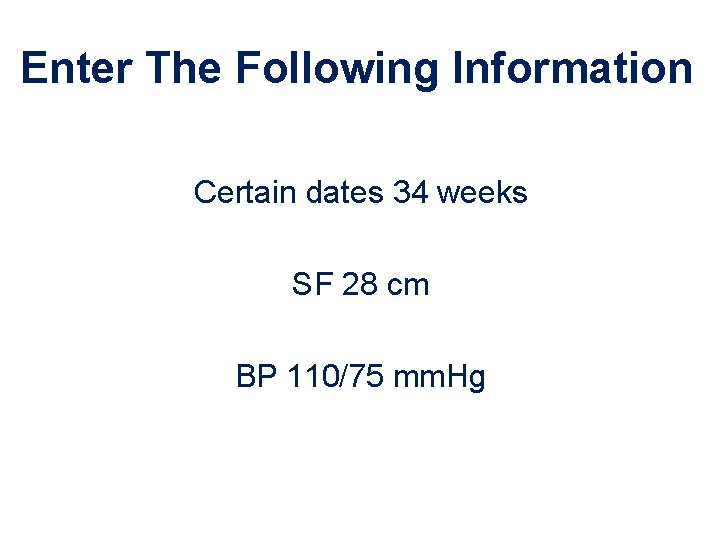
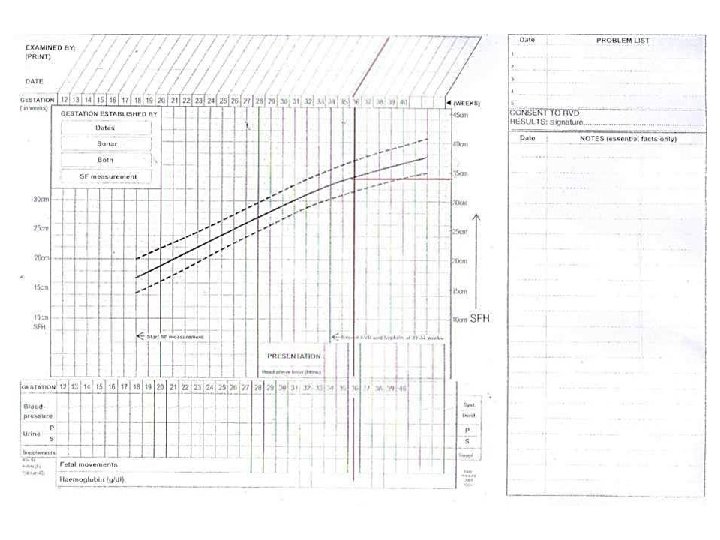
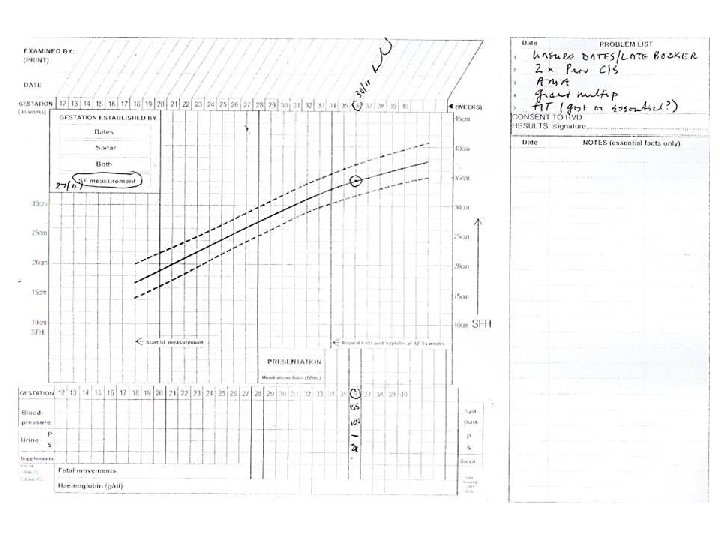
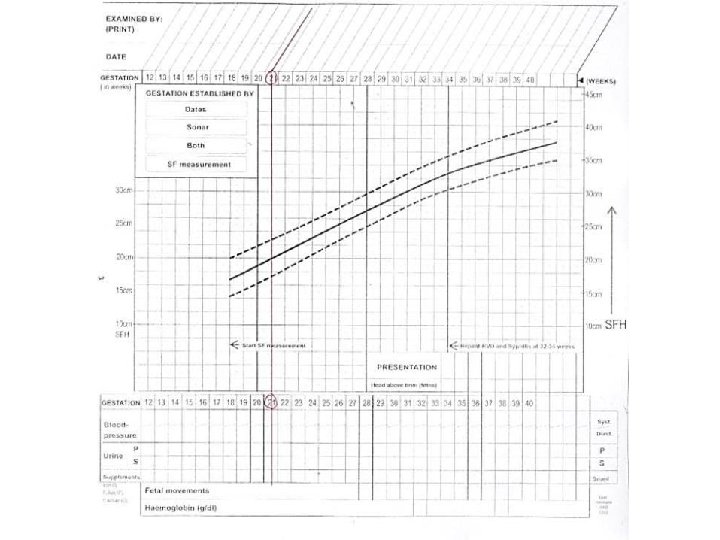
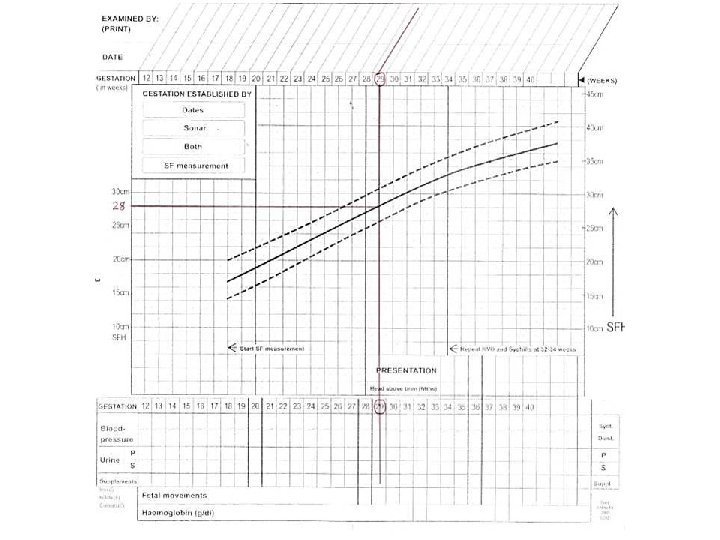
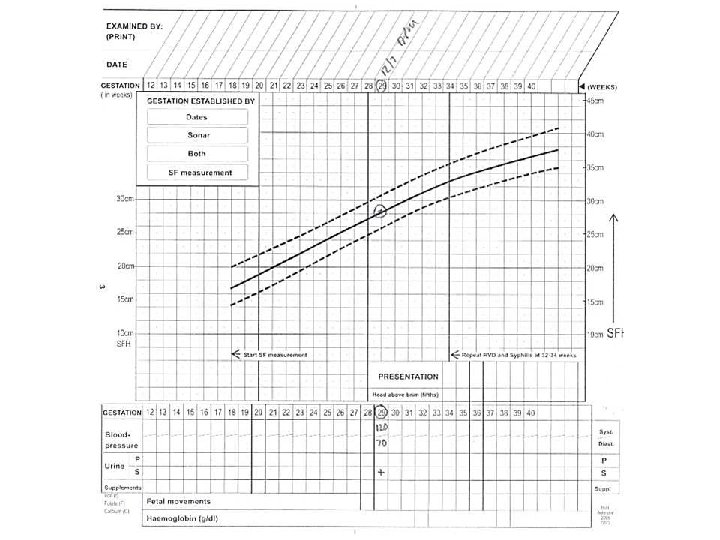
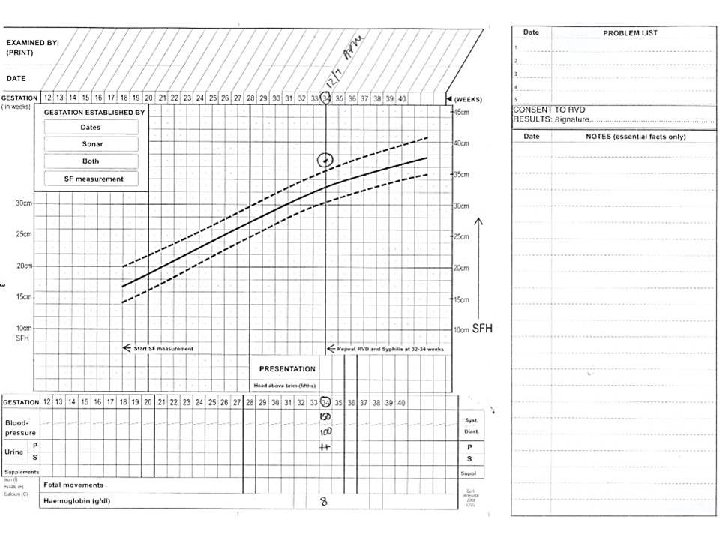
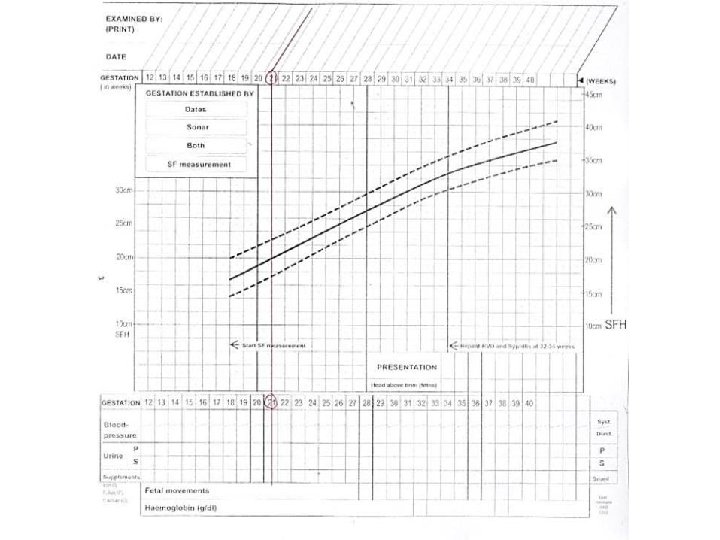
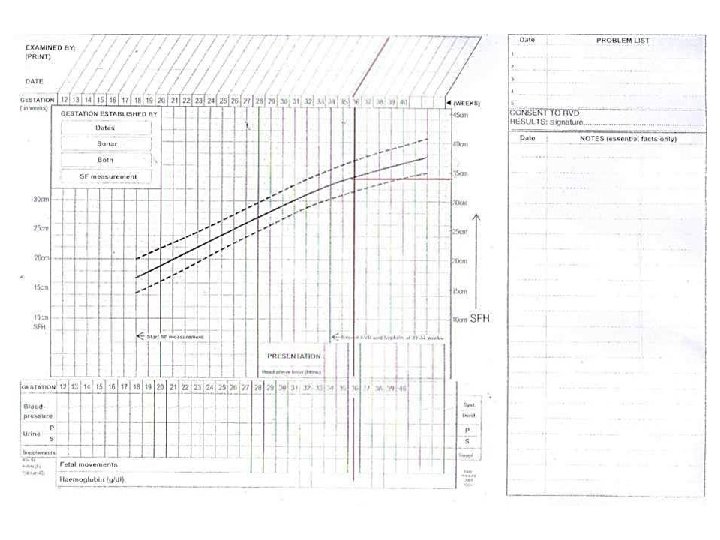
if the EDD is the 30 th September, and the date of the visit is the 22 nd July, then the gestational age at the time of the visit is 30 weeks gestation. Circle 30 weeks on the gestation line.
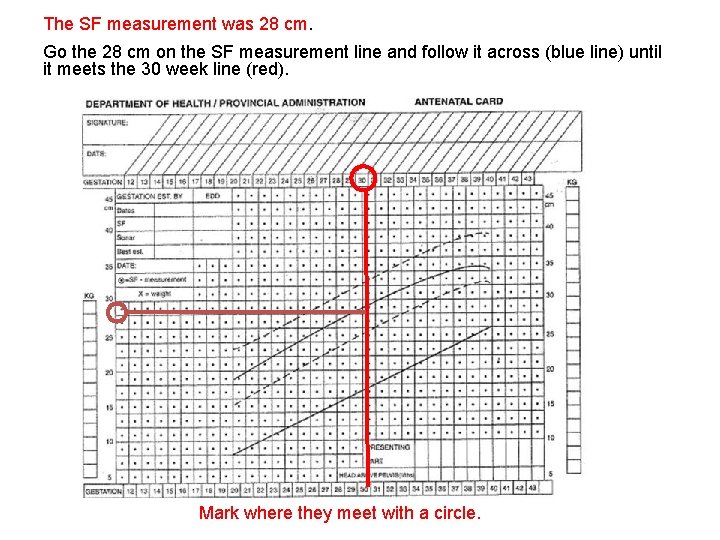
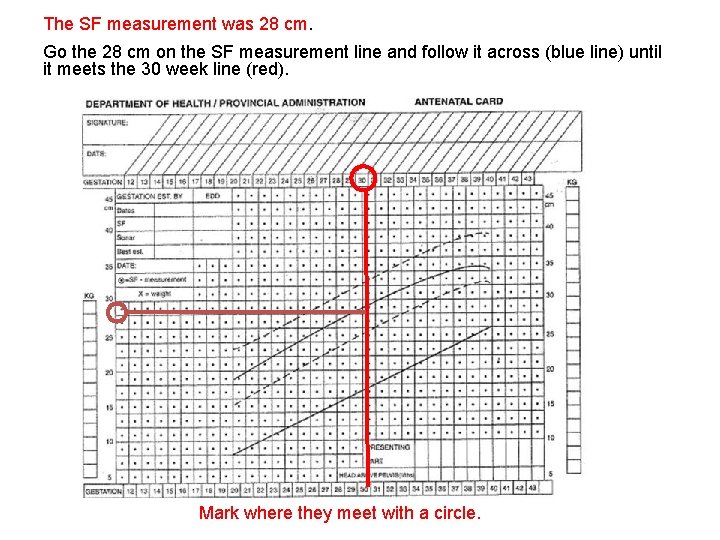
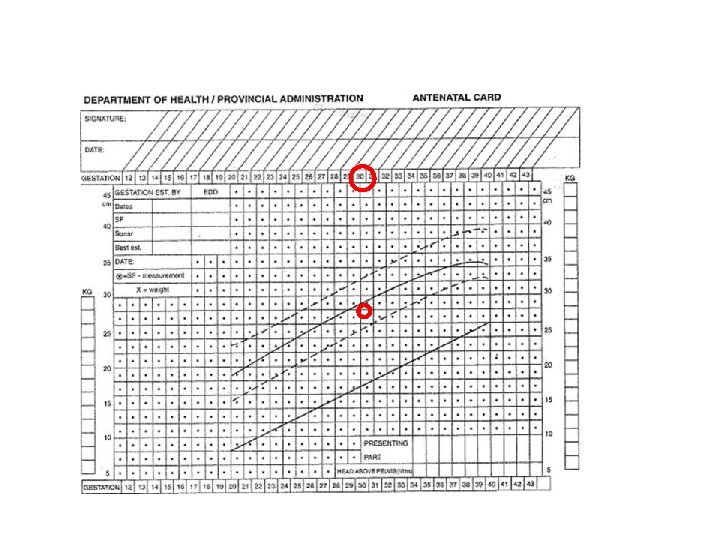
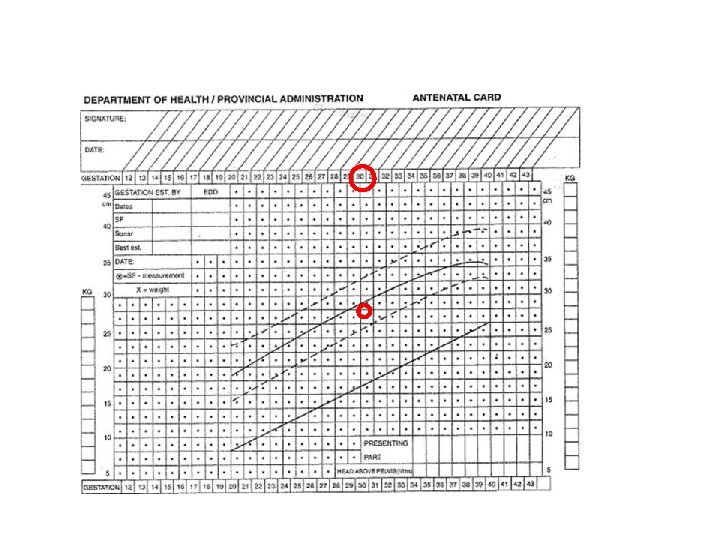
The SF measurement was 28 cm. Go the 28 cm on the SF measurement line and follow it across (blue line) until it meets the 30 week line (red). Mark where they meet with a circle.
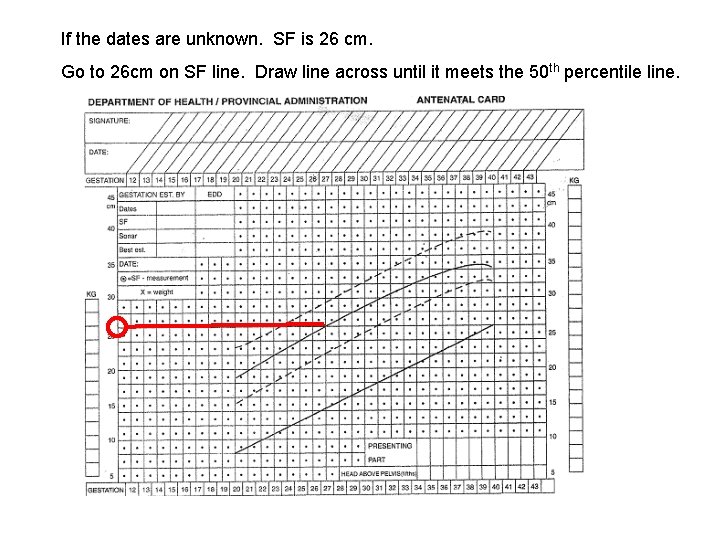
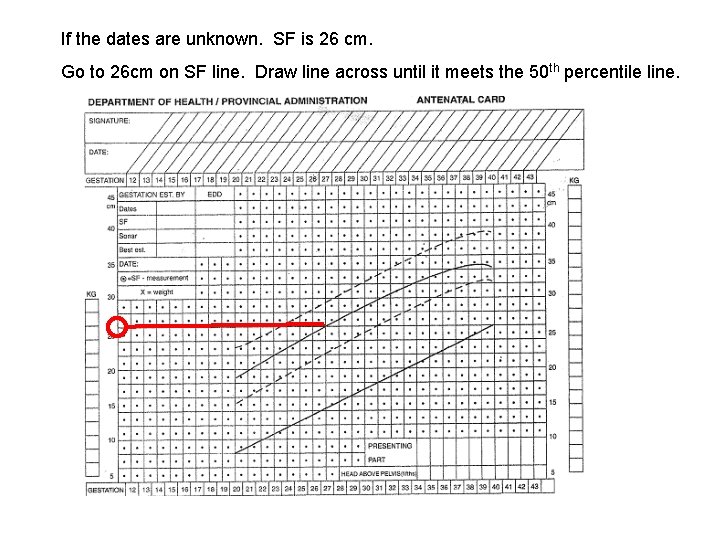
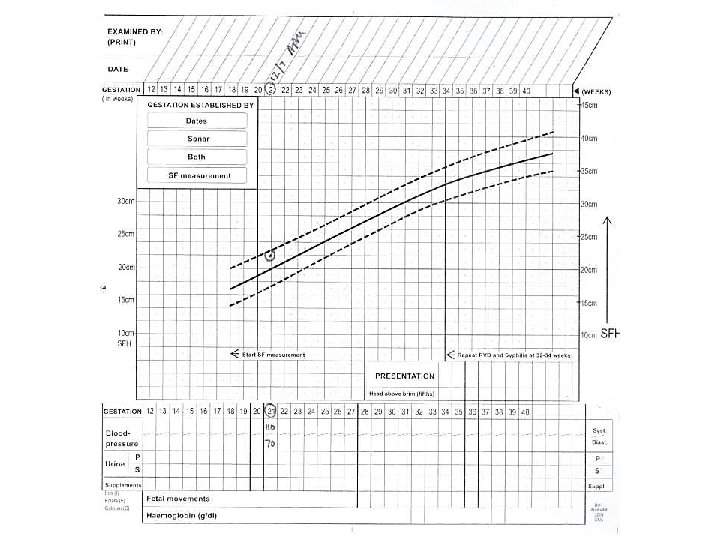
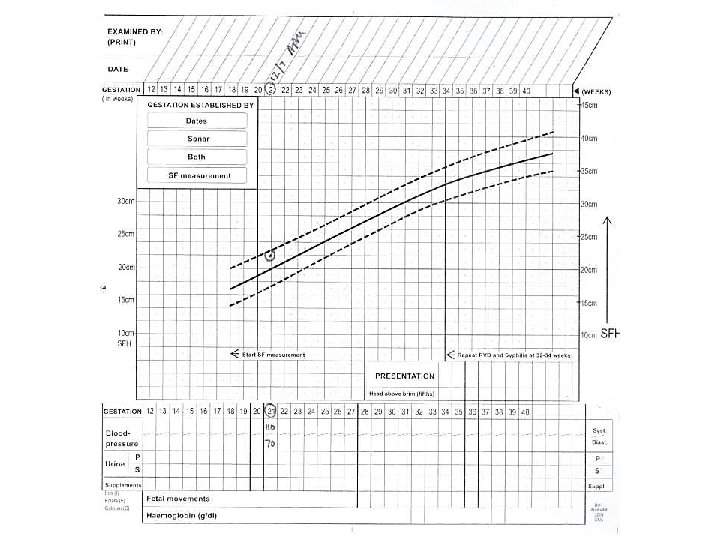
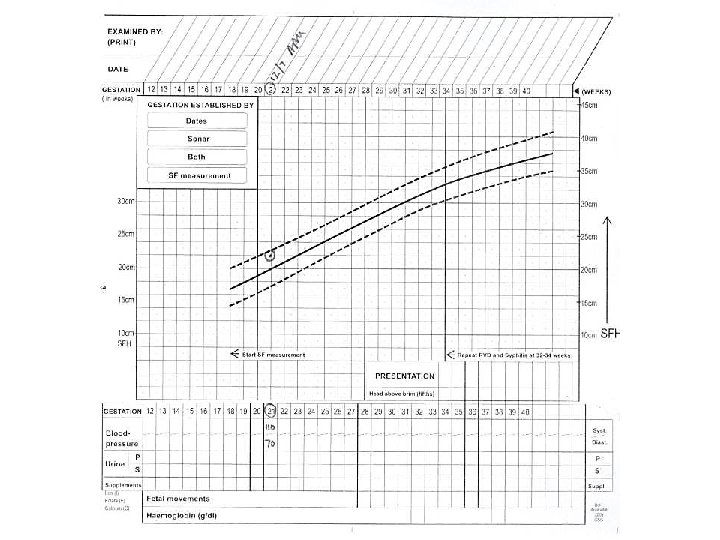
If the dates are unknown. SF is 26 cm. Go to 26 cm on SF line. Draw line across until it meets the 50 th percentile line.
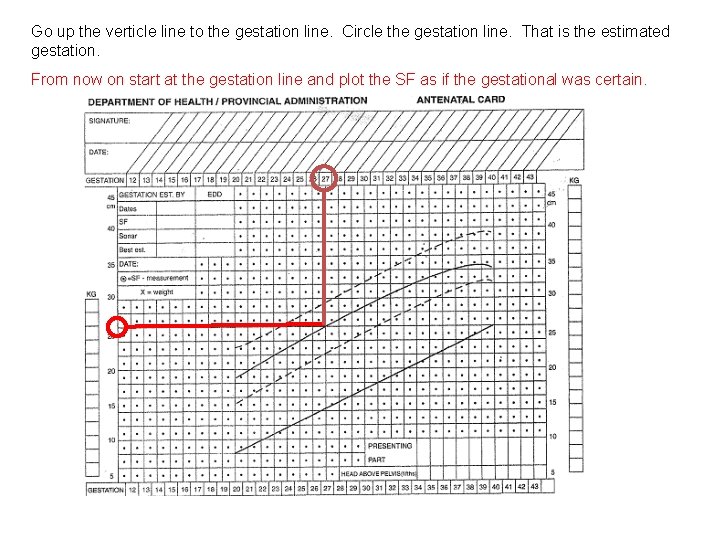
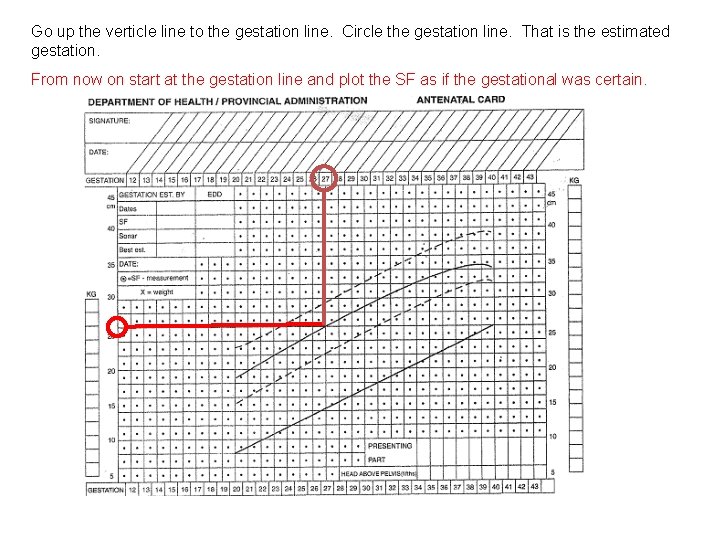
Go up the verticle line to the gestation line. Circle the gestation line. That is the estimated gestation. From now on start at the gestation line and plot the SF as if the gestational was certain.
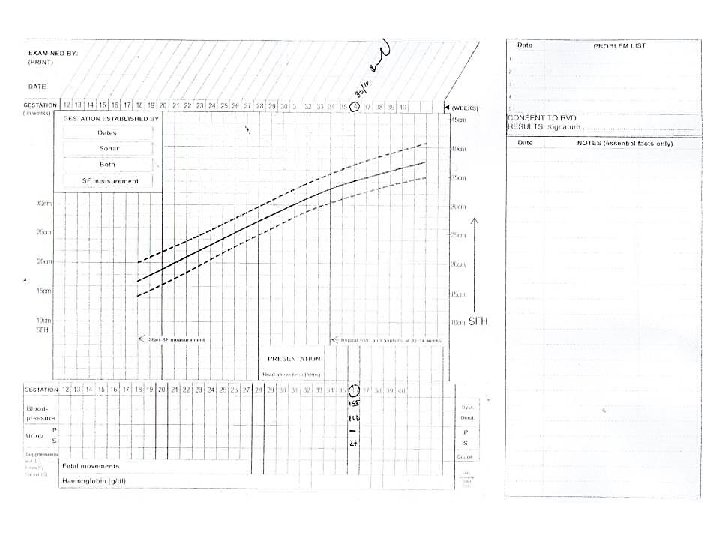
Enter The Following Information LMP - certain Now 21 weeks SF 22 cm BP 110/70 mm. Hg
What Is The 1 st Question To Ask? Do we have certain gestation? Yes Why? Because we have certain dates (21 wks)
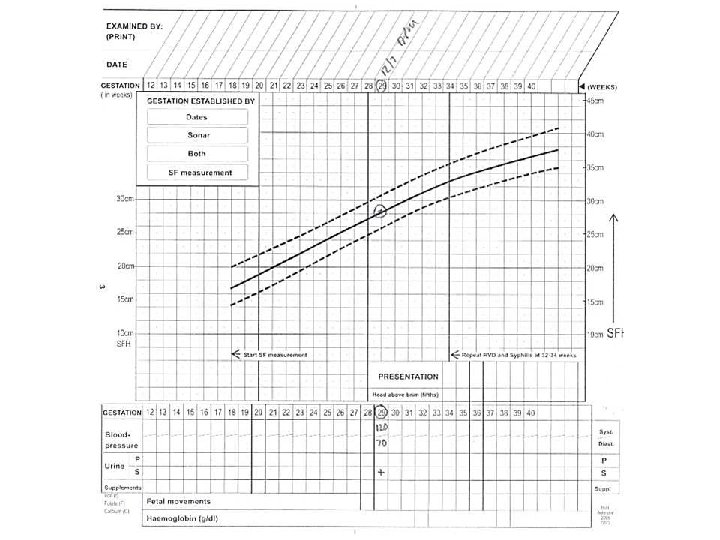
Enter The Following Data • LMP? • SF 28 cm • B/P 120/70 • Urine 1+ glucose
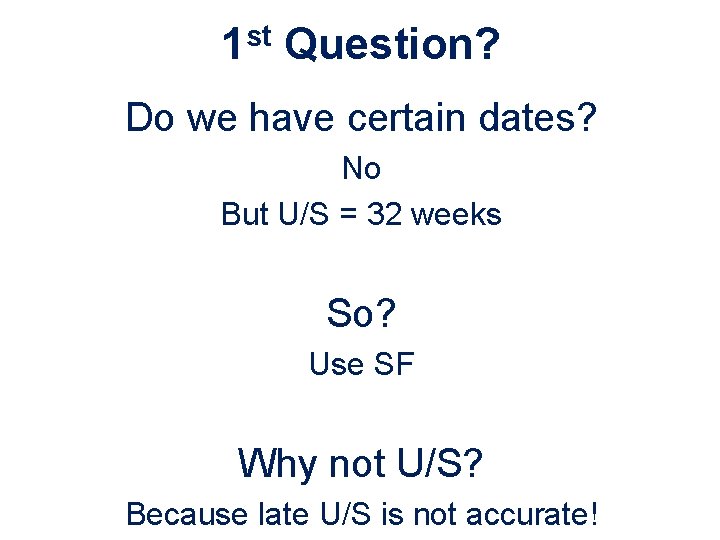
What Is the 1 st Question To Ask? Do we have certain gestation? No So? Use the SF measurement
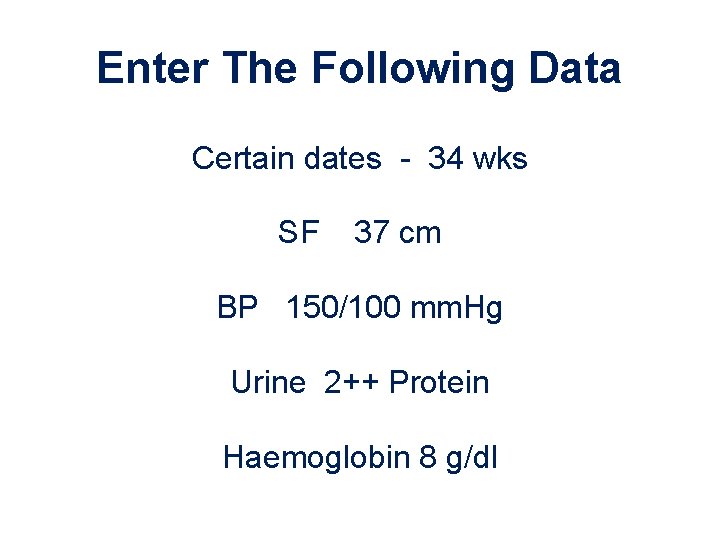
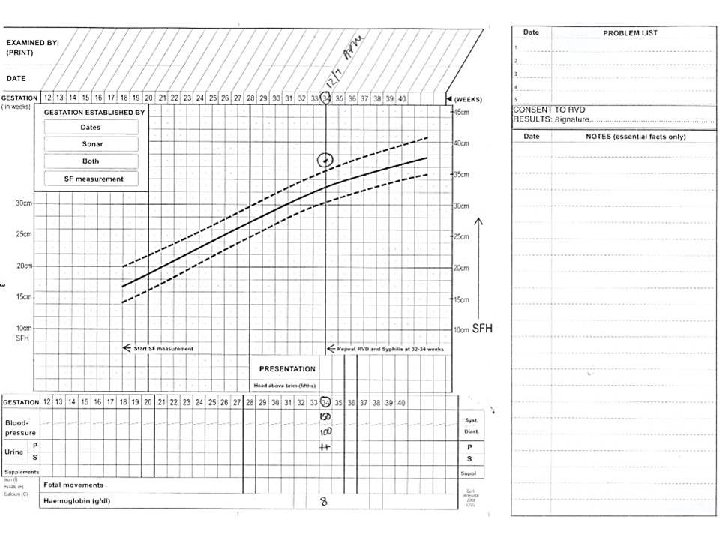
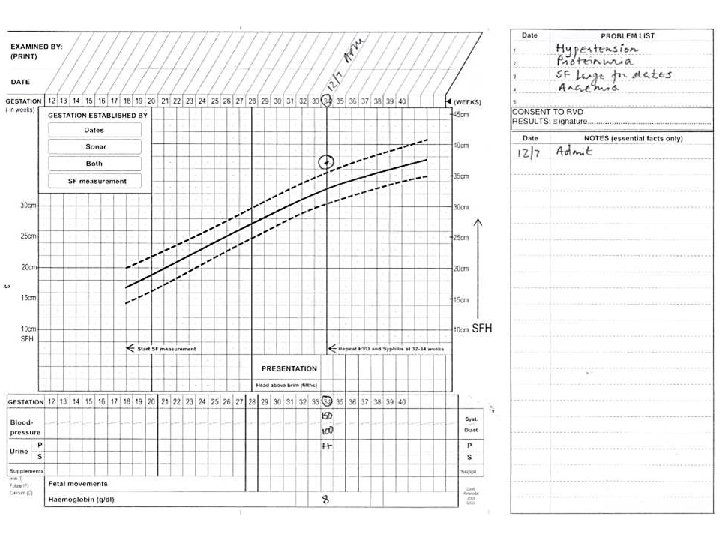
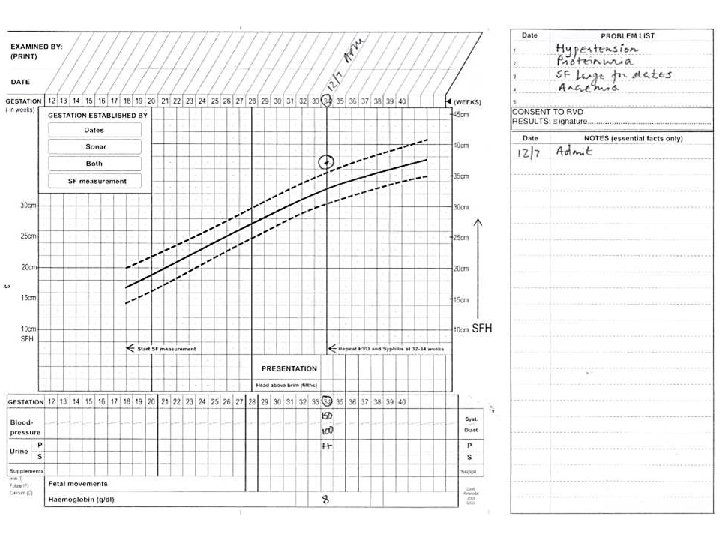
Enter The Following Data Certain dates - 34 wks SF 37 cm BP 150/100 mm. Hg Urine 2++ Protein Haemoglobin 8 g/dl
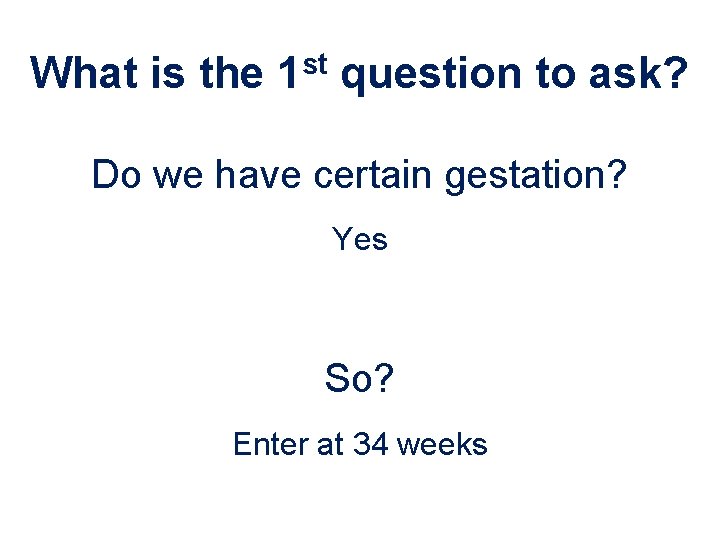
What is the 1 st question to ask? Do we have certain gestation? Yes So? Enter at 34 weeks
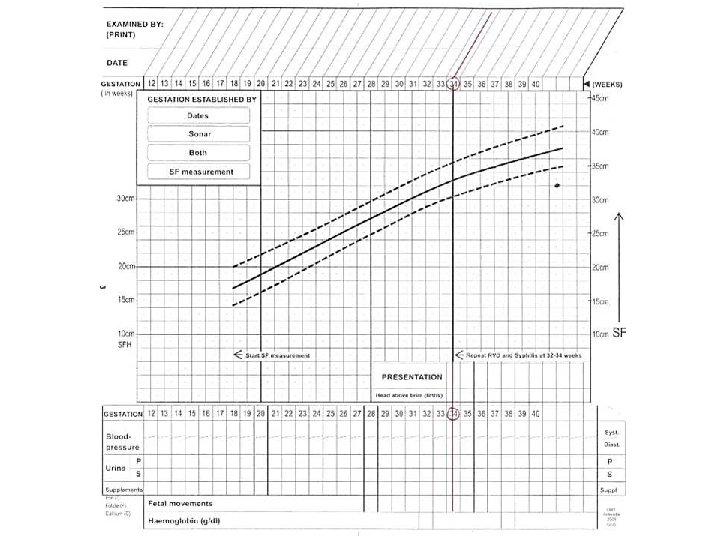
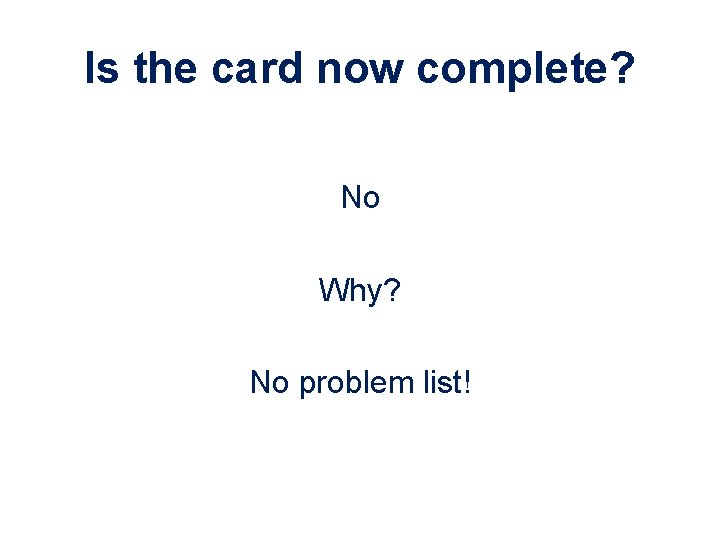
Is the card now complete? No Why? No problem list!
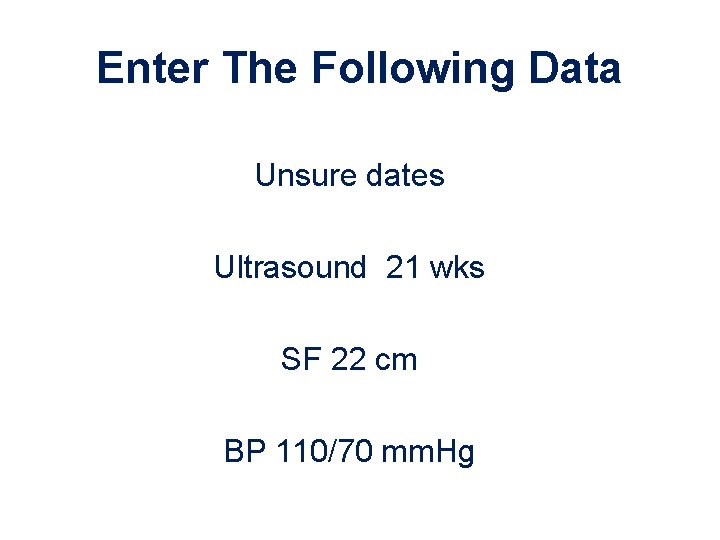
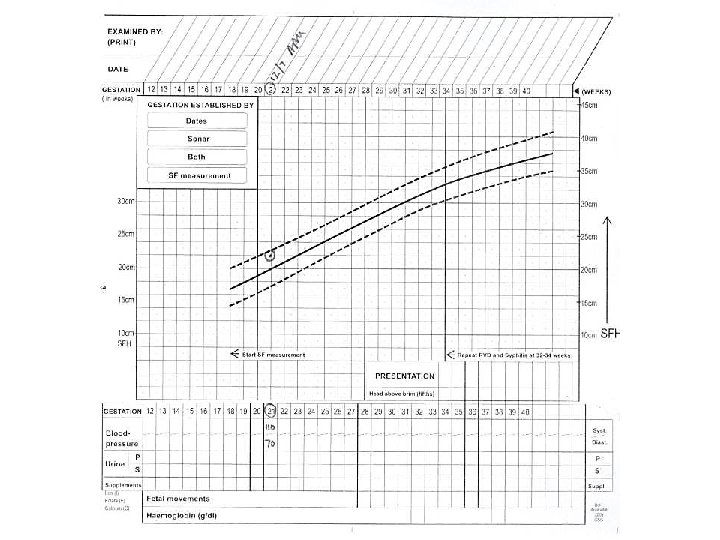
Enter The Following Data Unsure dates Ultrasound 21 wks SF 22 cm BP 110/70 mm. Hg
What Is The 1 st Question To Ask? Do we have certain gestation? Yes Why? Because we have early ultrasound
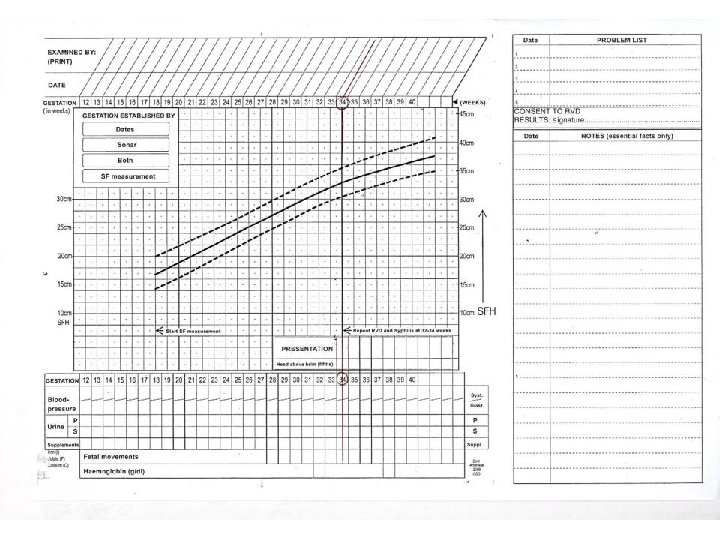
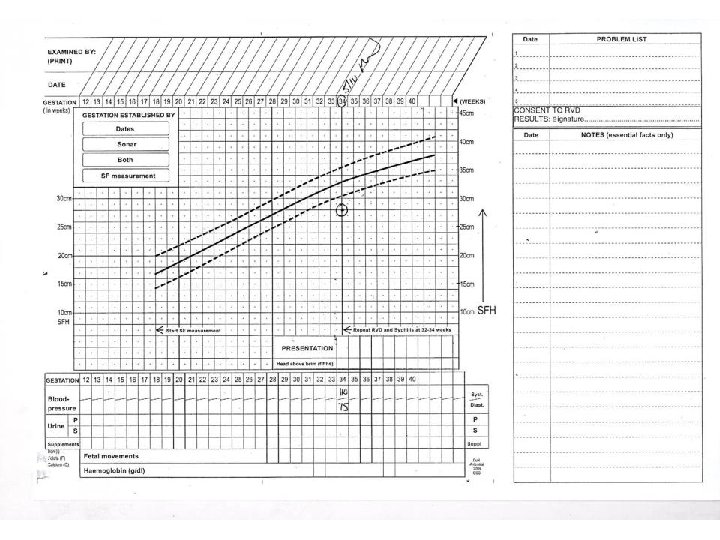
Enter The Following Information Certain dates 34 weeks SF 28 cm BP 110/75 mm. Hg
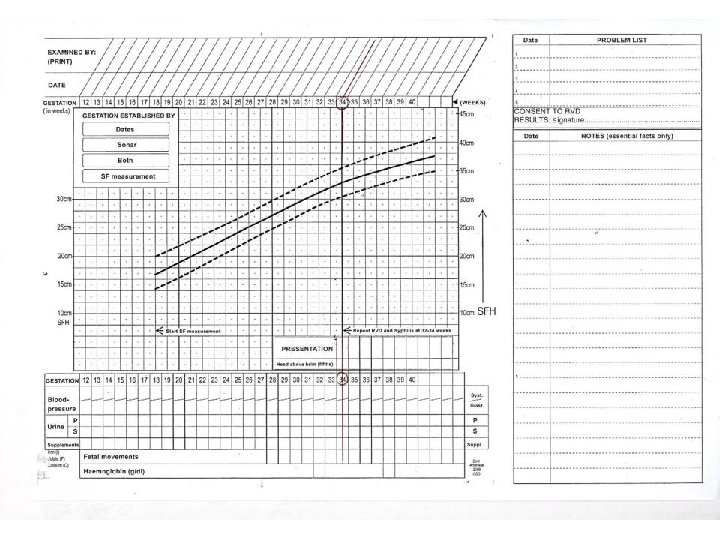
What Is The Problem? Certain dates and SF do not correspond So? IUGR or incorrect dates and a late booker
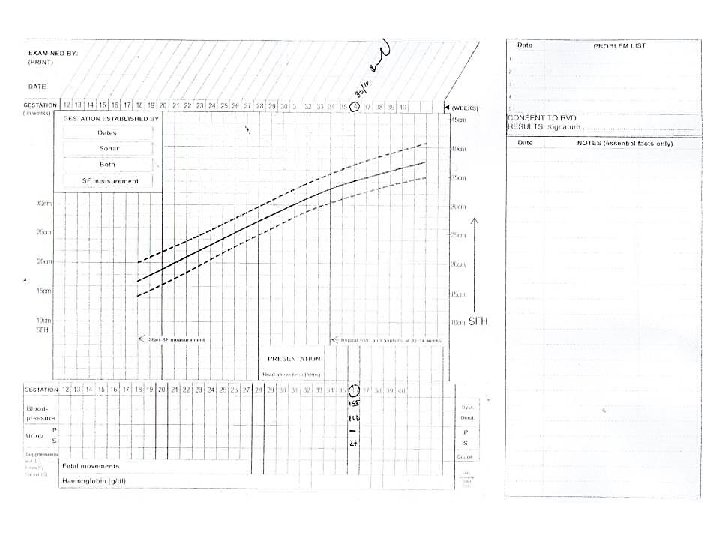
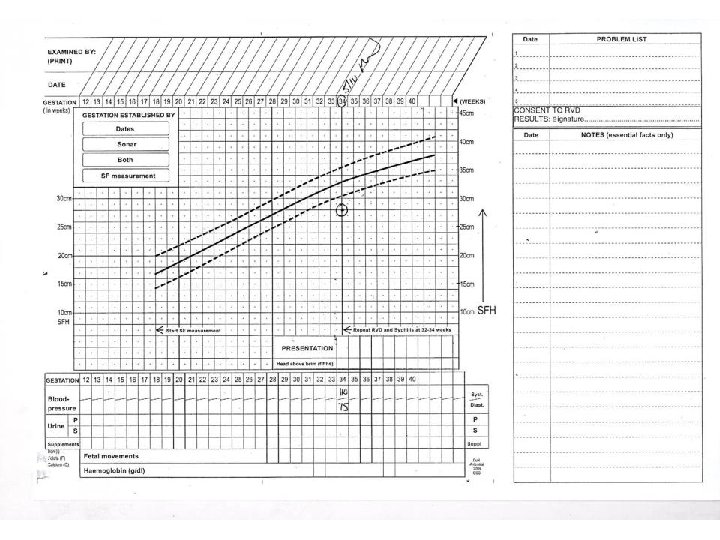
Enter The Following Information 38 yr old G 6 P 5 ( 2 x prev C/S) LMP ? ? ? Ultrasound 32 weeks SF 34 cm BP 155/100 mm. Hg Urine: Protein –ve, 2+ glucose
1 st Question? Do we have certain dates? No But U/S = 32 weeks So? Use SF Why not U/S? Because late U/S is not accurate!
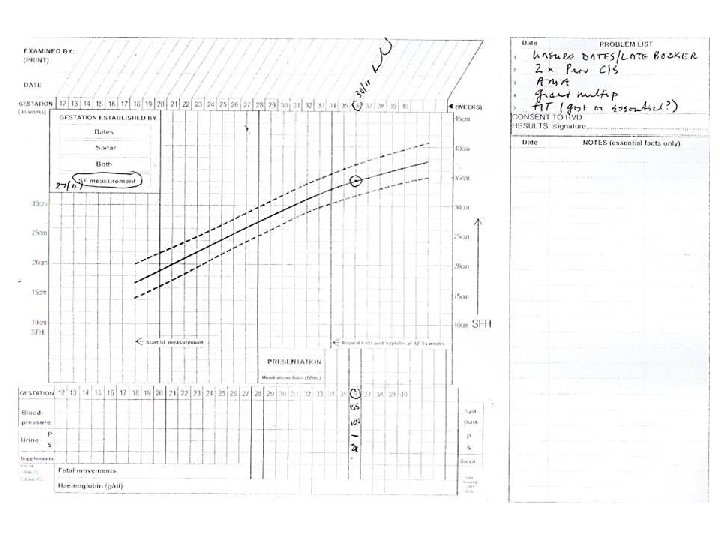
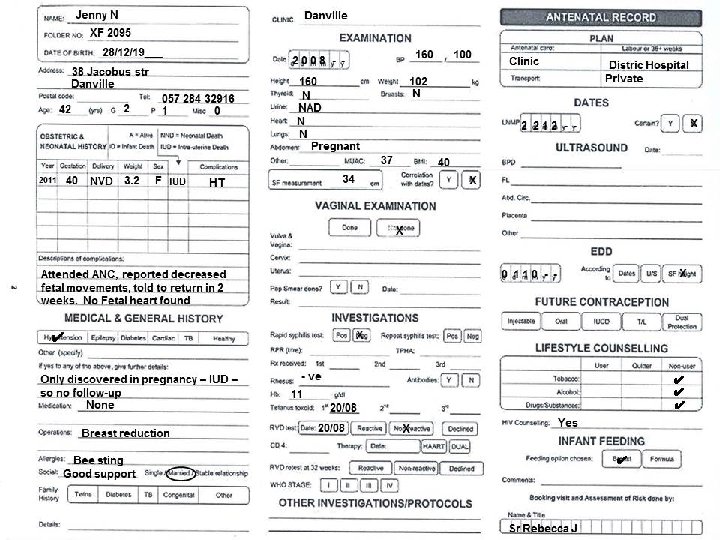
Work out problem lists for the following antenatal card, and start SF graph
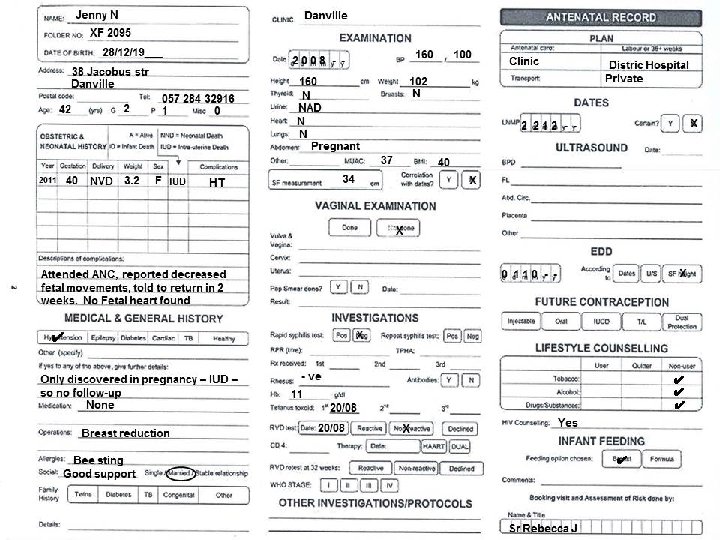
Problem List • Previous IUD • Pregnancy was complicated by hypertension (HT) with no follow-up • Advanced maternal age (AMA) • Unsure dates & late booker • HT and obesity (BMI = 40, UMAC = 37) • Rh –ve (no Ab titre done) • Inappropriate level of care
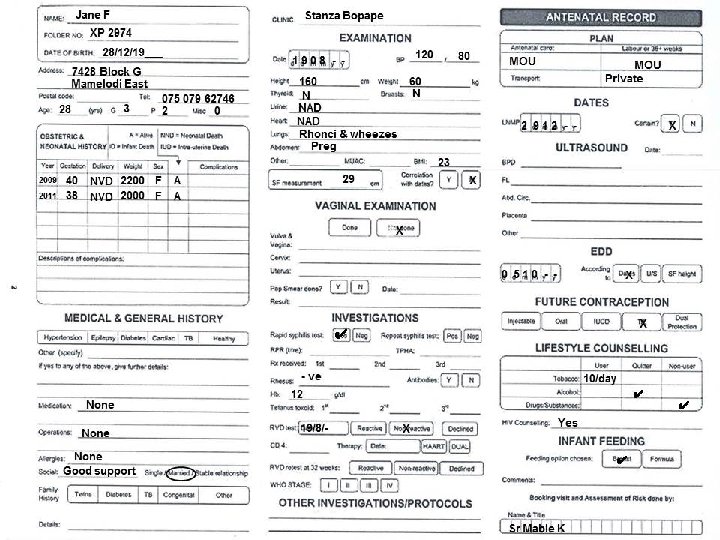
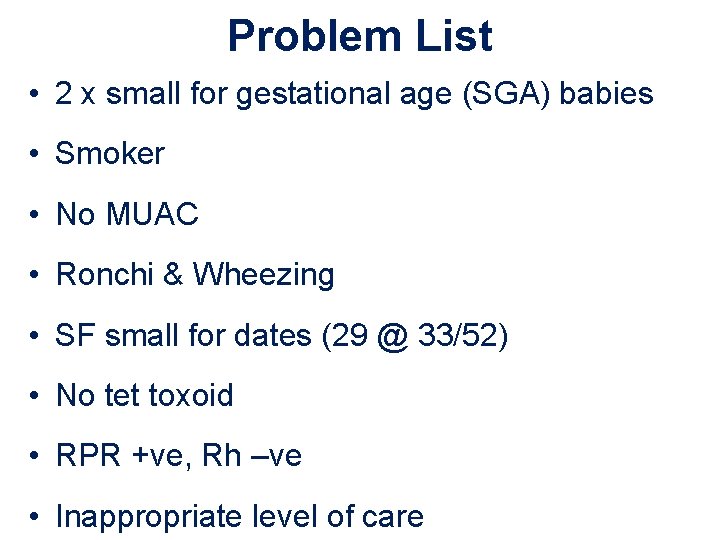
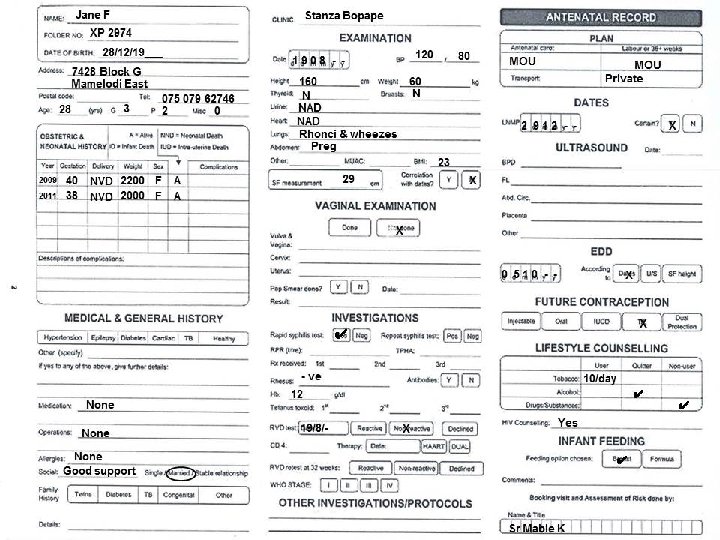
Problem List • 2 x small for gestational age (SGA) babies • Smoker • No MUAC • Ronchi & Wheezing • SF small for dates (29 @ 33/52) • No tet toxoid • RPR +ve, Rh –ve • Inappropriate level of care
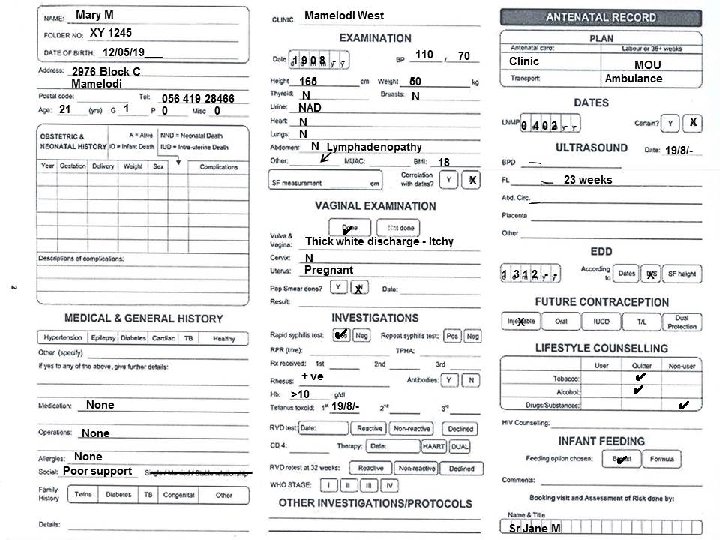
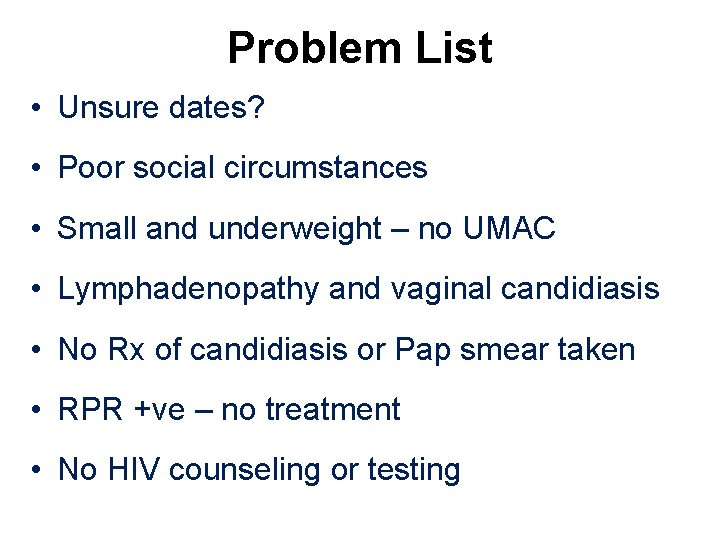
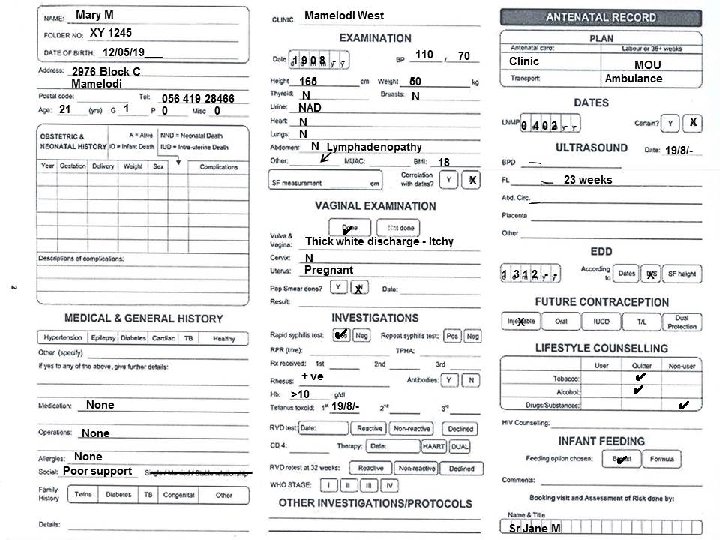
Problem List • Unsure dates? • Poor social circumstances • Small and underweight – no UMAC • Lymphadenopathy and vaginal candidiasis • No Rx of candidiasis or Pap smear taken • RPR +ve – no treatment • No HIV counseling or testing
Any Questions ?
 Clinic card for pregnancy
Clinic card for pregnancy Site:slidetodoc.com
Site:slidetodoc.com Conclusion for antenatal care
Conclusion for antenatal care Importance of antenatal care
Importance of antenatal care Antenatal care summary
Antenatal care summary Antenatal visit
Antenatal visit Antenatal care definition
Antenatal care definition Level of care primary secondary tertiary
Level of care primary secondary tertiary Antenatal class adalah
Antenatal class adalah Banc plus visits
Banc plus visits Antenatal visit according to who
Antenatal visit according to who Antenatal intrapartum and postnatal
Antenatal intrapartum and postnatal Leopold maneuvers
Leopold maneuvers Nice antenatal and postnatal mental health
Nice antenatal and postnatal mental health 3 weeks pregnant ultrasound
3 weeks pregnant ultrasound Antenatal
Antenatal Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa sống lại
Chúa sống lại Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc cc
V cc cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Các số nguyên tố
Các số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Uncontrollable spending ap gov
Uncontrollable spending ap gov Narrative review vs systematic review
Narrative review vs systematic review What is inclusion and exclusion
What is inclusion and exclusion Narrative review vs systematic review
Narrative review vs systematic review Care first counselling
Care first counselling Chapter 3 careers in healthcare
Chapter 3 careers in healthcare Care certificate standard 3
Care certificate standard 3 Ce atrage magnetul
Ce atrage magnetul Palliative care vs hospice care
Palliative care vs hospice care Inmultirea animalelor
Inmultirea animalelor Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate