Antenatal Care Rights of the Pregnant Woman Information
- Slides: 20
Antenatal Care
Rights of the Pregnant Woman • Information about her health • Discuss her concerns, thoughts, and worries • Know in advance about any planned procedure to be performed • Privacy • Express her views about the services she receives
Periodic antenatal care check-ups: • • • Opportunity to increase a woman’s confidence in her provider. Receive counseling related to her pregnancy. Identify and manage maternal complications or risk factors.
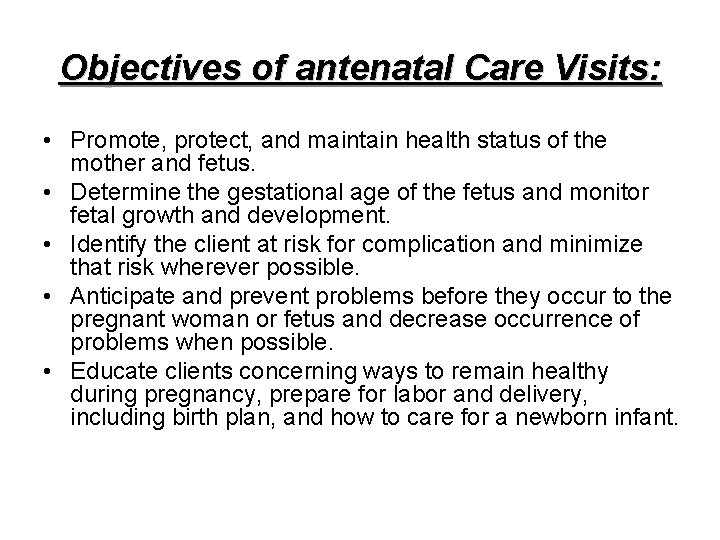
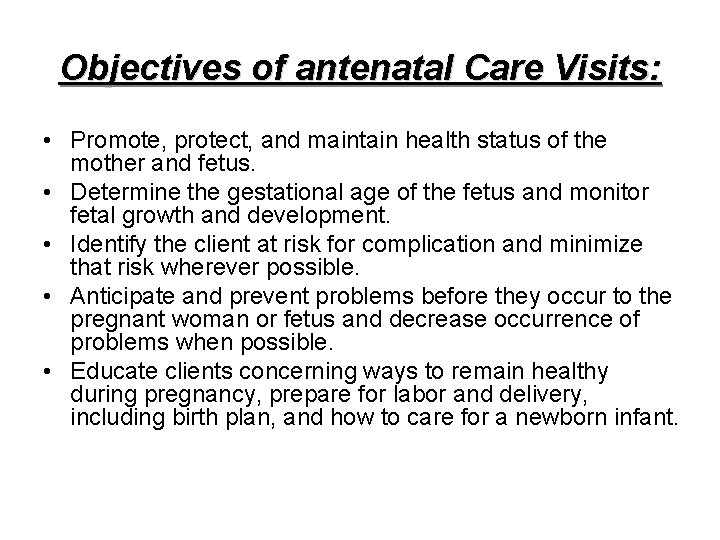
Objectives of antenatal Care Visits: • Promote, protect, and maintain health status of the mother and fetus. • Determine the gestational age of the fetus and monitor fetal growth and development. • Identify the client at risk for complication and minimize that risk wherever possible. • Anticipate and prevent problems before they occur to the pregnant woman or fetus and decrease occurrence of problems when possible. • Educate clients concerning ways to remain healthy during pregnancy, prepare for labor and delivery, including birth plan, and how to care for a newborn infant.
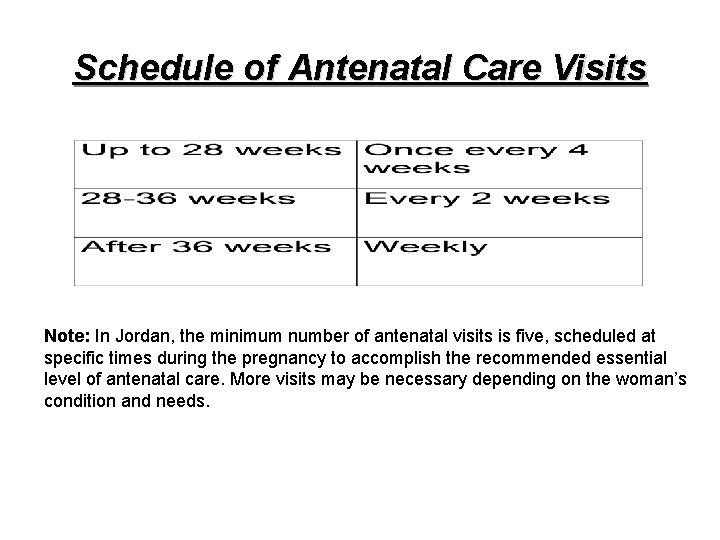
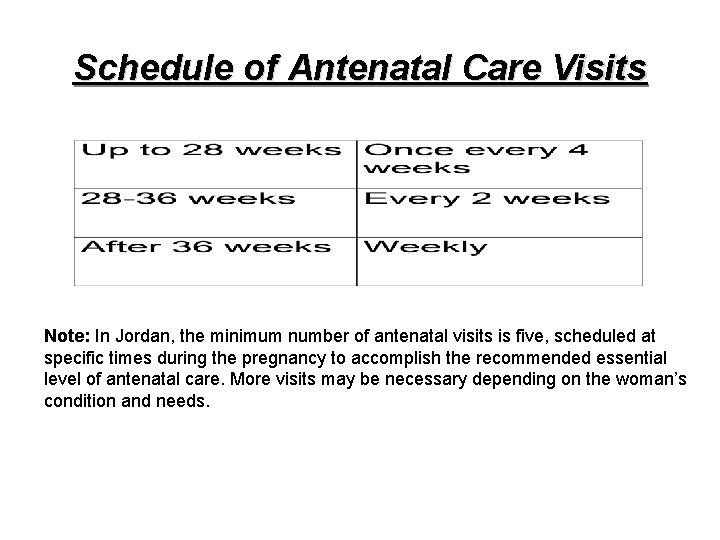
Schedule of Antenatal Care Visits Note: In Jordan, the minimum number of antenatal visits is five, scheduled at specific times during the pregnancy to accomplish the recommended essential level of antenatal care. More visits may be necessary depending on the woman’s condition and needs.
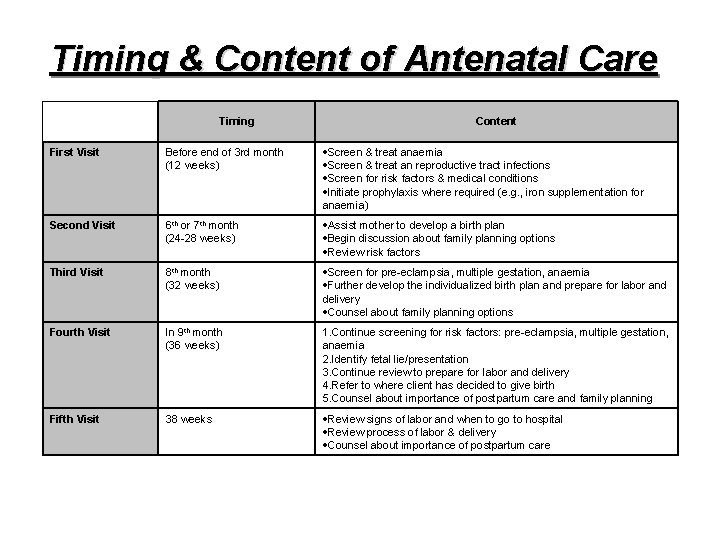
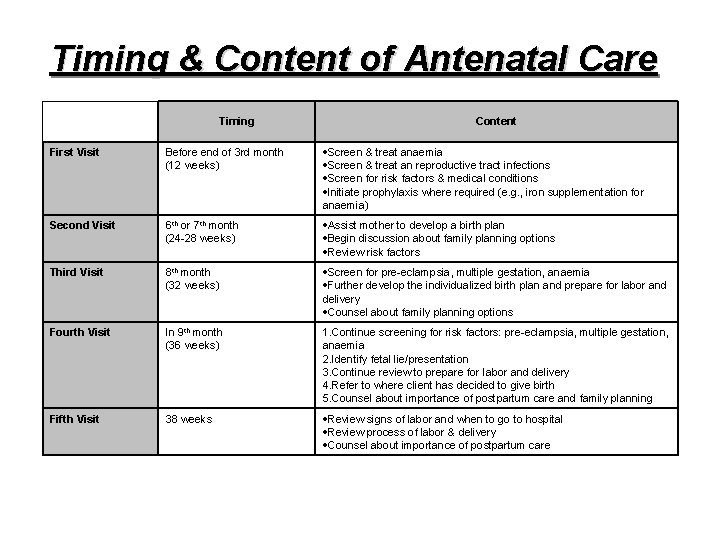
Timing & Content of Antenatal Care Timing Content First Visit Before end of 3 rd month (12 weeks) Screen & treat anaemia Screen & treat an reproductive tract infections Screen for risk factors & medical conditions Initiate prophylaxis where required (e. g. , iron supplementation for anaemia) Second Visit 6 th or 7 th month (24 -28 weeks) Assist mother to develop a birth plan Begin discussion about family planning options Review risk factors Third Visit 8 th month (32 weeks) Screen for pre-eclampsia, multiple gestation, anaemia Further develop the individualized birth plan and prepare for labor and delivery Counsel about family planning options Fourth Visit In 9 th month (36 weeks) 1. Continue screening for risk factors: pre-eclampsia, multiple gestation, anaemia 2. Identify fetal lie/presentation 3. Continue review to prepare for labor and delivery 4. Refer to where client has decided to give birth 5. Counsel about importance of postpartum care and family planning Fifth Visit 38 weeks Review signs of labor and when to go to hospital Review process of labor & delivery Counsel about importance of postpartum care
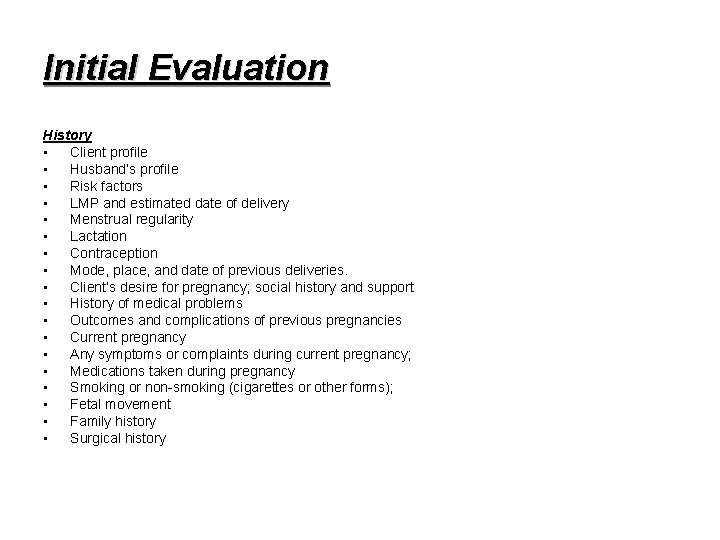
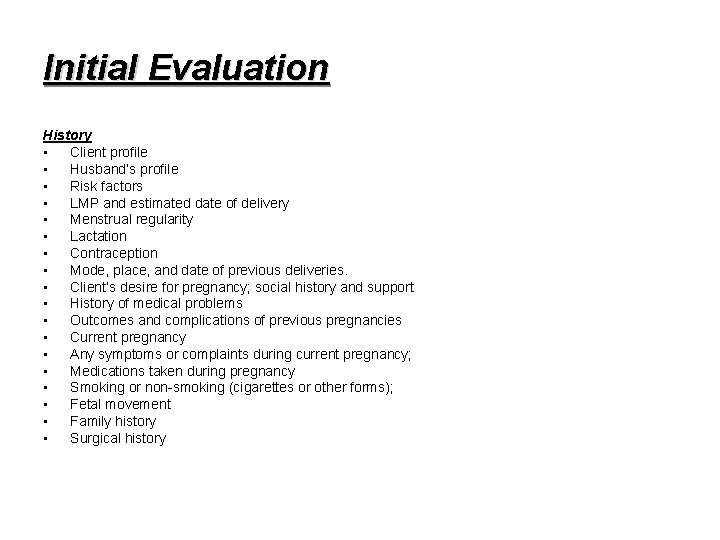
Initial Evaluation History • Client profile • Husband’s profile • Risk factors • LMP and estimated date of delivery • Menstrual regularity • Lactation • Contraception • Mode, place, and date of previous deliveries. • Client’s desire for pregnancy; social history and support • History of medical problems • Outcomes and complications of previous pregnancies • Current pregnancy • Any symptoms or complaints during current pregnancy; • Medications taken during pregnancy • Smoking or non-smoking (cigarettes or other forms); • Fetal movement • Family history • Surgical history
Initial Evaluation Physical Examination • Confirm diagnosis of pregnancy • Height and Weight • Blood Pressure • HEENT (Head, Eyes, Ears, Nose and Throat) • Breast • Chest • Extremities • Back • Abdominal Examination • Obstetrical Examination • Pelvic Examination when specific vaginal or pelvic complaints exist – Note that pelvic examination is not routinely required at the initial evaluation. • Ultrasound (U/S) • Electronic Fetal Monitoring
Health Education • • • • Birth planning Common complaints and symptoms of pregnancy Nutritional advice Immunizations during pregnancy Bathing and personal hygiene Clothing Relaxation and sleep Danger signs during pregnancy Travel Drug education and classification of drugs Work during pregnancy Sexual relationships Care of teeth and gums
Health Education • • • Breast care and breast self-examination Breastfeeding (lactation) counseling Bowel habits Birth spacing counseling Exercise Fetal movement Health hazards to pregnant women and infants: smoking and alcohol Childbirth education Warning signs of pre-term labor Physiology of labor Postnatal care Psychosocial problems
Follow-up Antenatal Visits: • History: – – Family and community support Complaints Advice Health Education • Physical Examination: – – – General appearance, Blood pressure Fundal Height Fetal assessment Lie and presentation Assessment of any specific complaints Any problems since the last visit. • Lab Investigations: – Urine for sugar and acetone.
Postnatal Care
Objectives of Postnatal Care • support the mother and her family • Prevention, early diagnosis, and treatment of common problems or complications in the mother and infant • Referral of mother and infant for specialist care when necessary. • Counseling and information for the mother on newborn care and breast feeding. • Support of optimal breastfeeding practices. • Education of the mother and her family concerning maternal nutrition and supplementation if necessary. • Counseling and provision of contraceptives before the resumption of sexual activity. • Immunization of the infant.
Schedule of Postnatal Care • Immediate Care • Early Care • Follow-up Care
I. Immediate Care (within first 24 hours at place of birth) Care of the Mother: • Exclude Postpartum Haemorhage • Exclude Puerperal Infection • Exclude Eclapmsia • Exclude Thromboembolic diseases • Provide guidance to the family on the needs of the mother and newborn • Provide immunization of mother • Teach mother danger signs for self and newborn and actions to be taken. • Arrange follow-up visit date.
I. Immediate Care (within first 24 hours at place of birth) Care of the Newborn: • Keep the infant warm and dry during the examination. • Review the birth record • Look at the infant’s general appearance • Assess bladder/bowel function, color of skin. • Care for the umbilical cord • Listen to the infant’s cry • Check the rate of breathing, heart rate, and temperature • Exclude preterm birth • Exclude low birth weight: • Inspect the infant’s body • Exclude congenital anomalies and malformations. • Exclude neonatal bacterial infection and neonatal tetanus. • Exclude birth trauma • Watch the infant breastfeed • Administer Vitamin K and antibiotic eye drops.
II. Early Care: (Within the first two weeks after delivery) Care of the Mother: • Assess the mother’s breastfeeding skills • Assess the progress of recovery • Assess for signs of infection or heavy bleeding. • Assess the mother’s manifestation of danger signs and actions to be taken. • Encourage prescribed supplementation; e. g. , iron tablets. • Introduce exercises • Remind or give postnatal clinic visit appointment. • Provide family planning counseling. • Answer the mother’s and family’s questions. • Blood test for hemoglobin and urine analysis.
II. Early Care: (Within the first two weeks after delivery) Care of the Newborn: • Breastfeeding • Sleep • Urination • Stool • Cord • General appearance, breathing, temperature, weight • Head, eyes, mouth, skin
III. Follow-up Care (Six weeks after delivery) • • Assess completion of involution Emotional feelings Relationship with infant. Identify client, infant, and/or familial problems. Assess breastfeeding practices. Examine infant growth. Assess need for or experience with current contraceptive method. • Give a resupply of contraceptives as requested or needed. • Give follow-up appointment, if needed. • Answer mother’s and family’s questions.
Health Education and Counseling • • Breastfeeding Postpartum Contraception Care of the Newborn Care and counseling of the mother
 Importance of antenatal care
Importance of antenatal care Conclusion of antenatal care
Conclusion of antenatal care Etiolgy
Etiolgy Antenatal care summary
Antenatal care summary Antenatal care meaning
Antenatal care meaning Antenatal care definition
Antenatal care definition Face recognition
Face recognition A woman travels in a lift. the mass of the woman is 50 kg
A woman travels in a lift. the mass of the woman is 50 kg Cones are to vision as ____ are to audition
Cones are to vision as ____ are to audition Once upon a time there lived a family of bears
Once upon a time there lived a family of bears Primary secondary tertiary health care
Primary secondary tertiary health care Positive vs negative rights
Positive vs negative rights Littoral water rights
Littoral water rights Characteristics of rights
Characteristics of rights Legal rights vs moral rights
Legal rights vs moral rights What is negative right
What is negative right Negative right
Negative right Positive vs negative rights
Positive vs negative rights Positive rights and negative rights
Positive rights and negative rights Antenatal assessment format
Antenatal assessment format Antenatal class adalah
Antenatal class adalah