First Antenatal Assessment 1 First Antenatal Assessment Once
- Slides: 15
First Antenatal Assessment 1
First Antenatal Assessment • Once pregnancy suspected, the women should seek prenatal care to promote a healthy outcome. • The assessment process begins at the initial prenatal visit and continues throughout the pregnancy. • Its Benefits: • 1 -Appropriate nursing management starts at conception and continuing through the pregnancy can have a positive impact on health of pregnant women and their unborn children. • 2 -The initial visit is an ideal time to screen for factors that might place the 2 women and her fetus at risk for problems such as preterm delivery.
First Antenatal Assessment • 3 -The initial visit is an optimal time to begin educating the client about changes that will affect her life. • 4 -Counseling and education of pregnant women and her partner are critical to ensure healthy outcomes for mother and her infant. • 5 -It gives an opportunity for pregnant to ask questions, misinformation, or misconceptions about what to eat, weight gain, physical discomforts, drug and alcohol use, sexuality, and birth process and the nurse answer them. 3
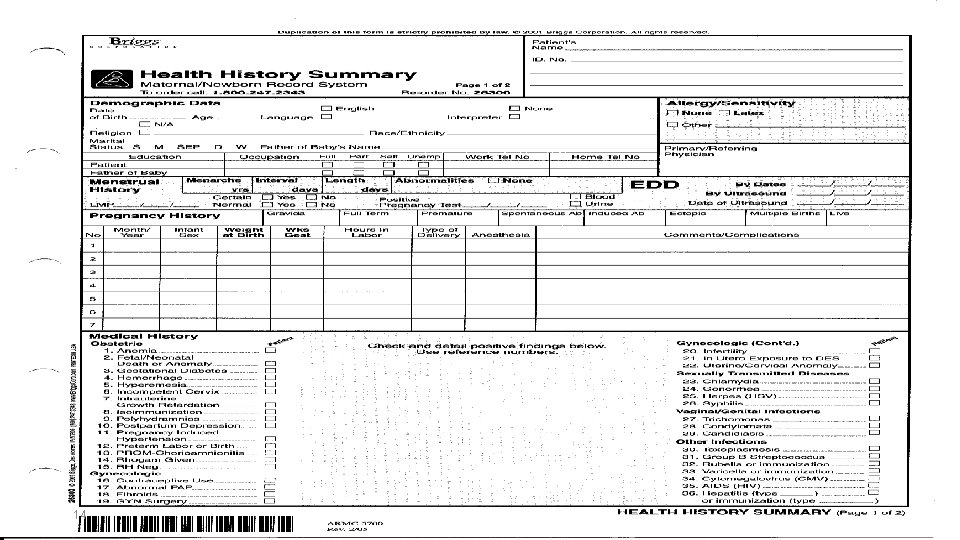
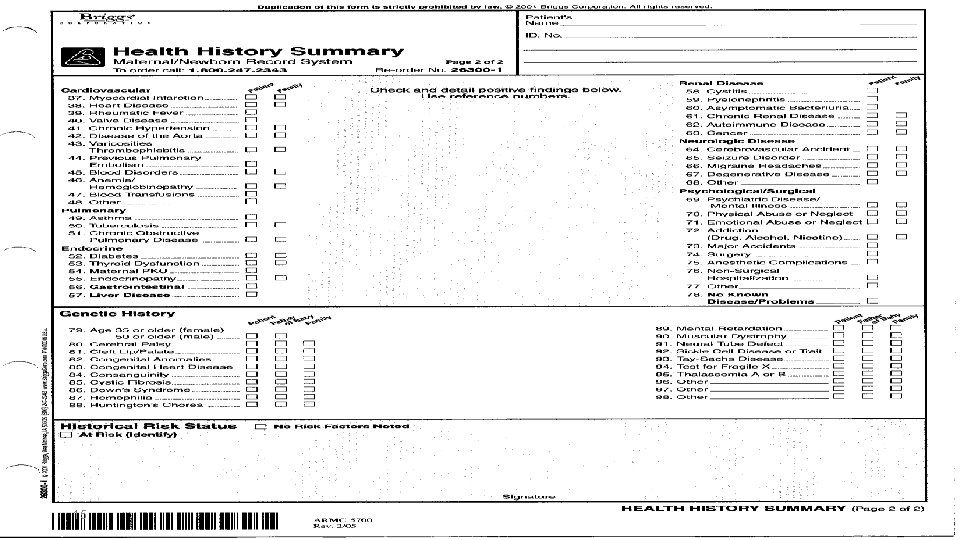
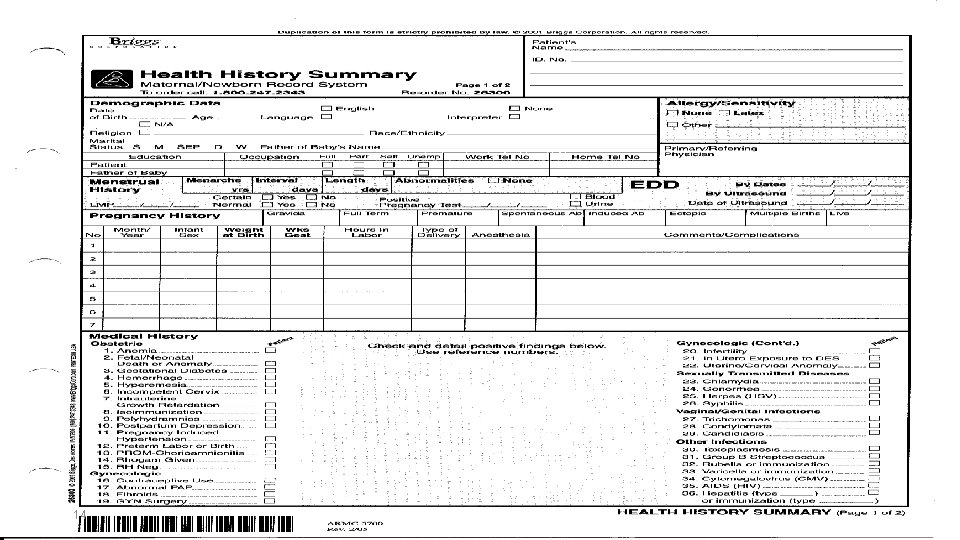
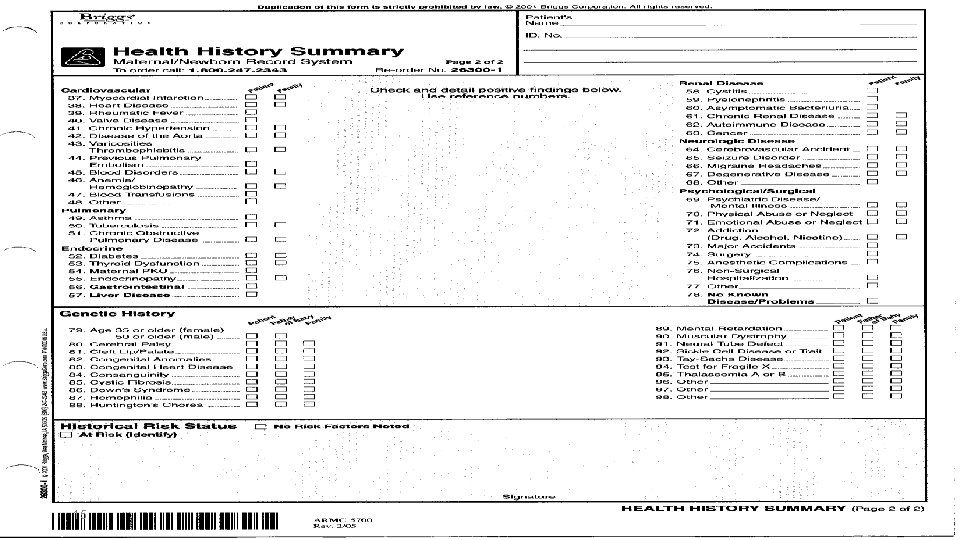
First Antenatal Assessment • It is a Comprehensive health history. • Is taken during the initial visit, including: *Demographic data *Menstrual history *Pregnancy History *Prior obstetric history *Prior Gynecologic History *Past medical and surgical/psychological history *Family history *Genetic screening 4
First Antenatal Assessment *Medications *History of exposure to infections (STDs) (Use the prenatal history form is the best way to document these data) -Prenatal history form includes questions about 3 major areas: 1 -Reason for seeking care 2 -Past heath history (medical, surgical, personal) 3 -Reproductive history 5
First Antenatal Assessment 1 - Reason for seeking care -When she missed her menstrual period or had a positive pregnancy test at home, she will seek for a care. -Ask the women about her last menstrual period (LMP), any probable signs of pregnancy and B-h. CG (Human Chrionic Gonadotropin) is made to confirm pregnancy 6
First Antenatal Assessment 2 - Past health history -Past medical and surgical history-urinary tract infections, chronic diseases like Diabetes mellitus, heart diseases, hypertension, and history of allergies from medications, foods, or environmental substances. -Mental health problems like depressions and anxiety -Personal history -occupation, possible exposure to teratogens, exercise and activity level, recreational patterns (alcohol, tobacco, and drugs), use of alternative or complementary therapies, sleep patterns, nutritional habits, and general lifestyle. 7
First Antenatal Assessment 3 - Reproductive History a-Menstrual history -describe the menstrual cycle including the her age at menarche, number of days in her cycle, typical flow characteristics , and any associated discomforts, and last time she used the contraception. -Ask the LMP to estimate the EDD (Expected Date of Deliver) Nagele's rule (Subtract 3 months and then add 7 days to the first day of LMP. Then add 1 to the year. The margin error is plus or minus 2 weeks. e. g. , 14 October 2014 LMP EDD is 21 July 2015. 8
First Antenatal Assessment b-Obstetric history -past pregnancies, any problems encountered in during past pregnancies, labors, deliveries. -G and P is used, G means Gravida-number of pregnancy, P means Para means number of deliveries. c-Gynecologic history-reproductive tract surgeries, tubal pregnancy, polyps, papilloma, endometriosis…etc. 9
Follow-up visits -Continuous prenatal care is important for a successful pregnancy outcome. -Recommended follow-up visit schedule for healthy pregnant women is: *Every 4 weeks up to 28 th weeks (7 months) *Every 2 weeks from 29 th till 36 th week *Every week from 37 th to birth. 10
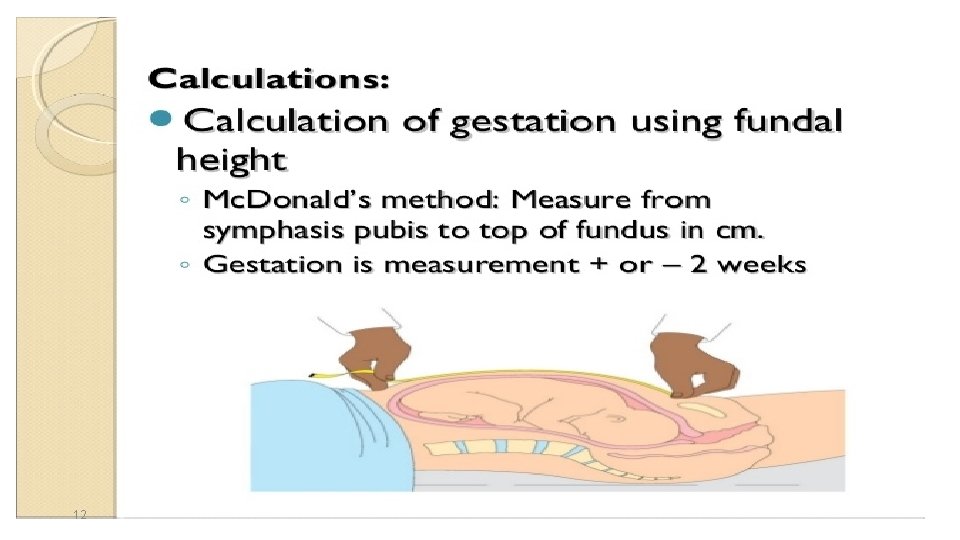
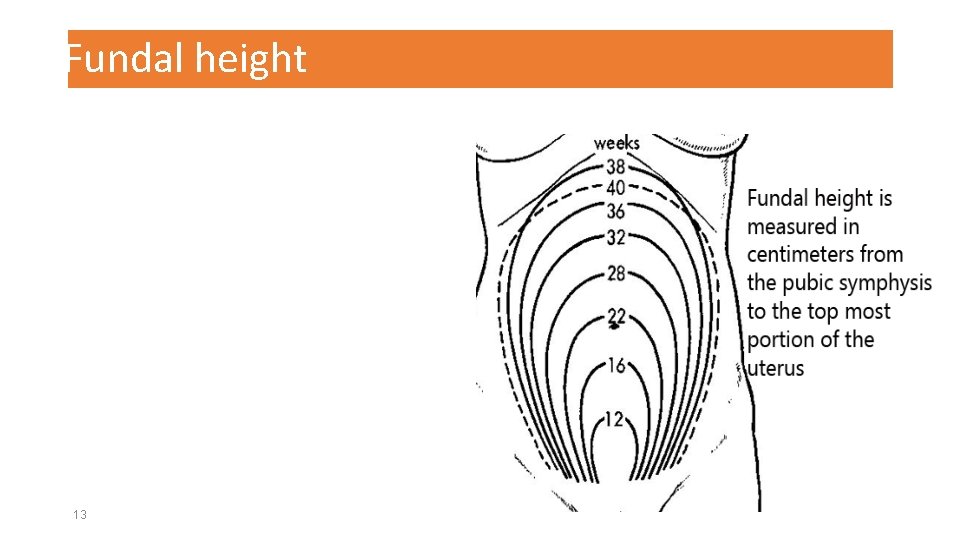
Follow-up visits -The following assessments are completed in each subsequent visit: *Weight and blood pressure *Urine test for protein, sugar, ketones, and nitrites *Fundal height measurement to assess fetal growth-A distance measured by a tape from pubic bone till top of uterus(fundus) while she is in supine position Mc. Donald's method. *Assessment the quickening/fetal movements to determine fetal well-being. Usually perceived between 16 th and 20 th week of gestation. 11 *Assessment of fetal heart rate (Normal is 110 -160 bpm)
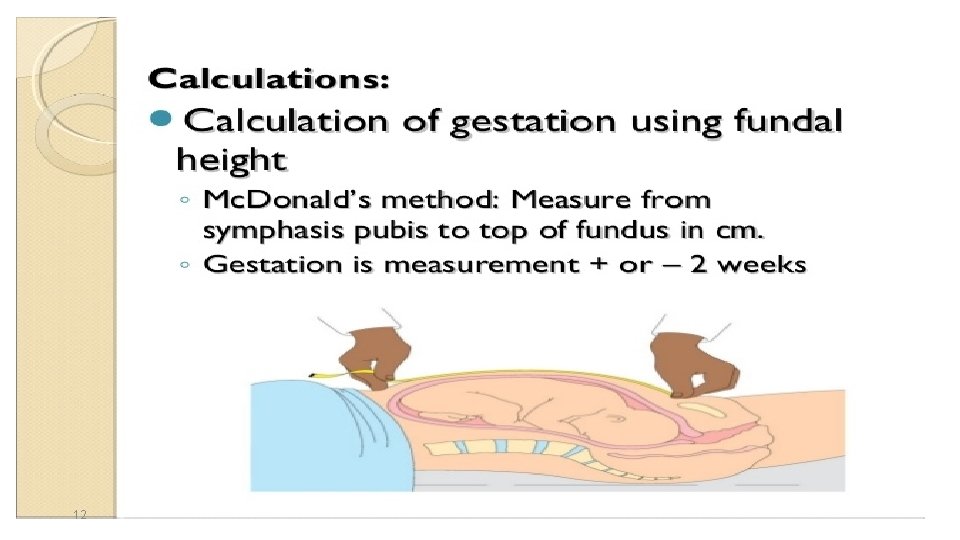
12
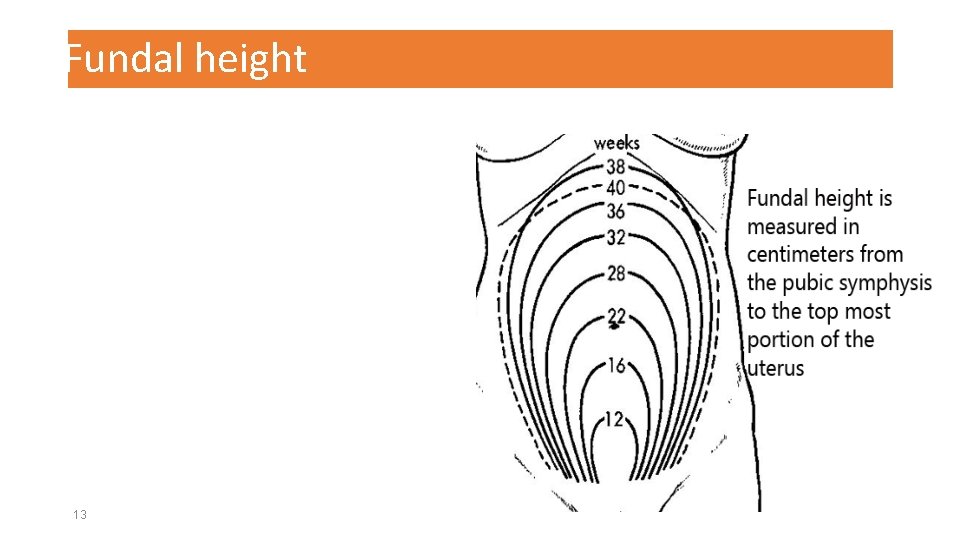
Fundal height 13
14
15
 Antenatal card
Antenatal card Antenatal class adalah
Antenatal class adalah Hegar's sign
Hegar's sign Antenatal card template south africa
Antenatal card template south africa Conclusion of antenatal care
Conclusion of antenatal care Antenatal visit
Antenatal visit Definition of antenatal care
Definition of antenatal care Importance of antenatal care
Importance of antenatal care Summary of antenatal care
Summary of antenatal care Antenatal intrapartum and postnatal
Antenatal intrapartum and postnatal Fundal grip
Fundal grip Nice guidelines postnatal depression
Nice guidelines postnatal depression 3 weeks pregnant ultrasound
3 weeks pregnant ultrasound Antenatal care definition
Antenatal care definition Antenatal
Antenatal Learning principle in portfolio assessment
Learning principle in portfolio assessment