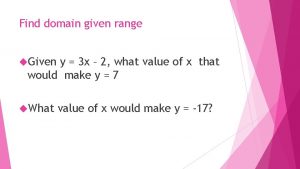
Antenatal care Antenatal care refers to care given



- Slides: 23
Antenatal care • Antenatal care refers to care given to a pregnant woman from the time conception is confirmed until the beginning of labour. The midwife should provide a woman-centred approach to the care of the woman and her family by sharing information with the woman to help her make informed choices about her care.
Antenatal care aims • provide effective antenatal care • monitor the progress of pregnancy and fetal development • the midwife critically evaluates the physical, psychological and sociological effects of pregnancy on the woman and her family • discuss the initial assessment visit, define its objectives and consider the significance of the different components of the woman's history taken by the midwife. • describe the physical examination and psychological support of the woman at the initial assessment and during subsequent visits • Discover early pregnancy complication
Five steps to help to sensitivity and evidence for practice • Finding out what is important to the woman and her family. • Using information from the clinical examination. • Seeking and assessing evidence to inform decisions. • Talking it through. • Reflecting on outcomes, feelings and consequences.
Antenatal visiting pattern • • • Booking appointment(s) with midwife by 10 weeks if possible • 10– 14 weeks: ultrasound scan for gestational age • 16 weeks: midwife • 18– 20 weeks: ultrasound scan for fetal anomalies • 25 weeks: midwife (nulliparous women) • 28 weeks: midwife • 31 weeks: midwife (nulliparous women) • 34 weeks: midwife • 36, 38 weeks: midwife • 40 weeks: midwife (nulliparous women) • 41 weeks: midwife (discuss options).
Objectives for the initial assessment • To assess levels of health by taking a detailed history and to offer appropriate screening tests • To ascertain baseline recordings of blood pressure, urinalysis, • To identify risk factors by taking accurate details of past and present midwifery, obstetric, medical, family and personal history • To provide an opportunity for the woman to express and discuss any concerns • To give public health advice • To build a trusting relationship with pregnant women
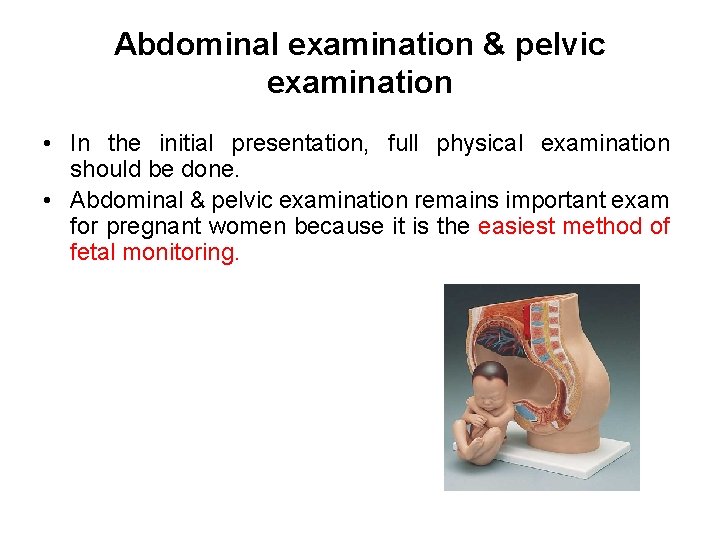
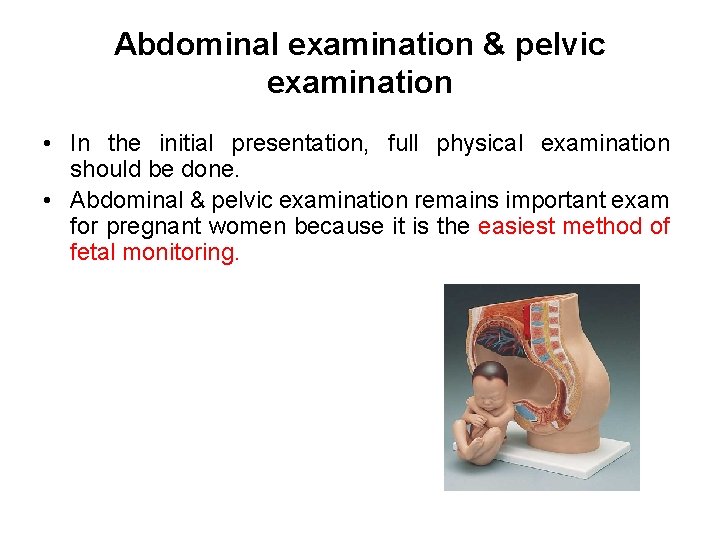
Abdominal examination & pelvic examination • In the initial presentation, full physical examination should be done. • Abdominal & pelvic examination remains important exam for pregnant women because it is the easiest method of fetal monitoring.
• Abdominal examination is carried out from 25 weeks' gestation to establish and affirm that fetal growth is consistent with gestational age during the pregnancy. • The specific aims are to: • • observe the signs of pregnancy • • assess fetal size and growth • • auscultate the fetal heart when indicated • • locate fetal parts • • detect any deviation from normal.
Methods of examination • 1 - Inspection – Size of the uterus: assess • If the length & breadth are both increased multiple pregnancies, polyhydramnios • If the length is increased only large baby – Shape of the uterus: length should be larger than broad this indicates longitudinal lie. But if the uterus is low and broad indicates transverse fetus lie. – Fetal movement – Contour of the abdomen: full bladder may be visible in late pregnancy. Umbilicus may become everted – Skin changes: look for stretch marks, linea nigra, scars that indicates previous surgeries
Methods of examination • 2 - Palpation (A): by Leopold maneuver-4 maneuvers – Palpate the fundus (to determine if it contains breech, head) • By gentle pressure: – if soft consistency/ indefinite outline breech – If hard, smooth, well defined head • Move your fingertips over the fetal mass to determine mobility and sixe – If can’t move independent from the body breech – If moves freely between fingertips head

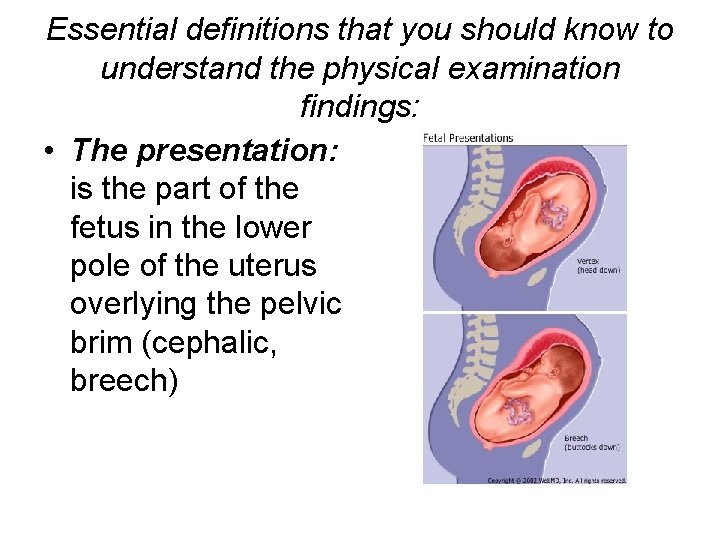
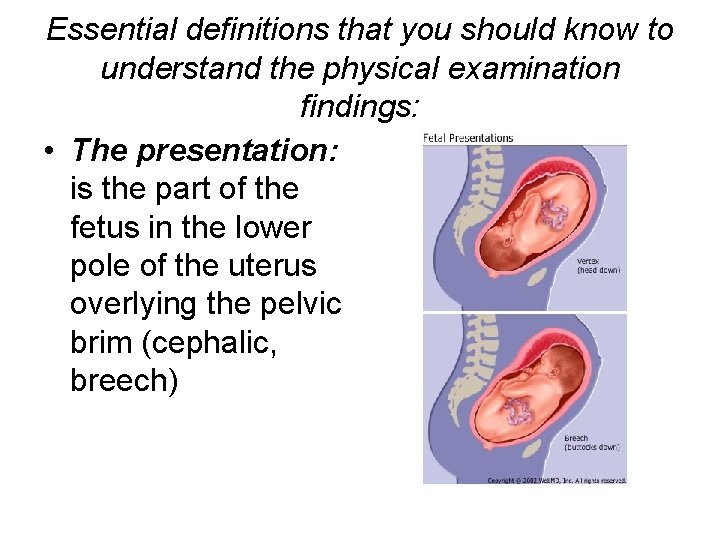
Essential definitions that you should know to understand the physical examination findings: • The presentation: is the part of the fetus in the lower pole of the uterus overlying the pelvic brim (cephalic, breech)
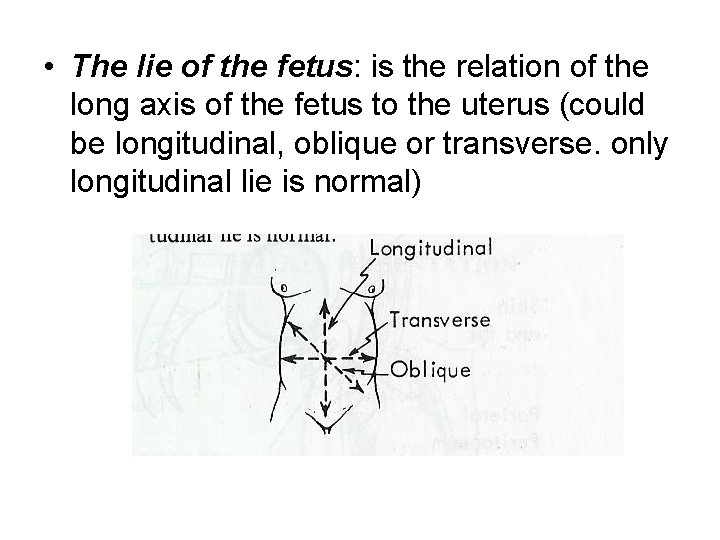
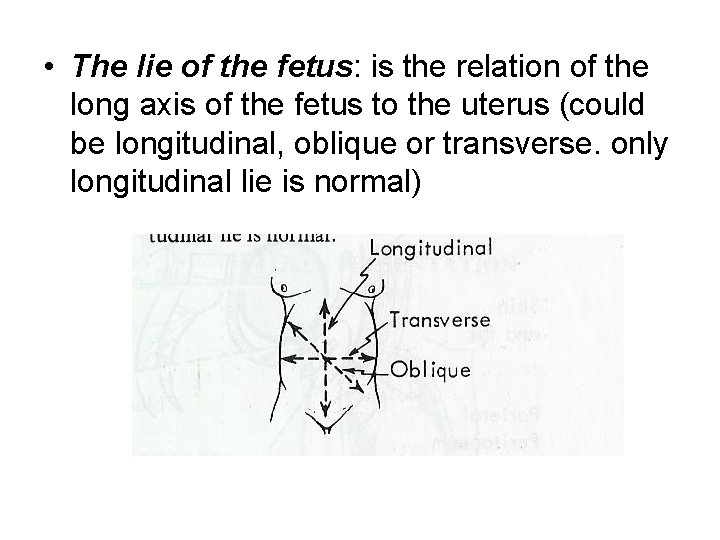
• The lie of the fetus: is the relation of the long axis of the fetus to the uterus (could be longitudinal, oblique or transverse. only longitudinal lie is normal)
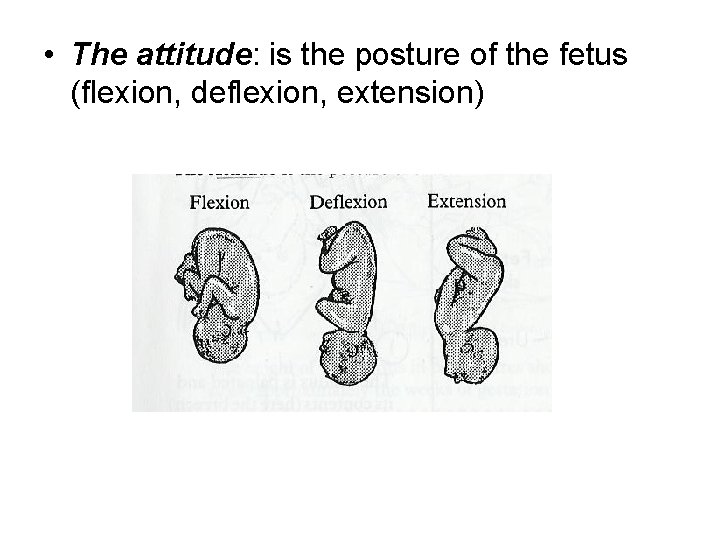
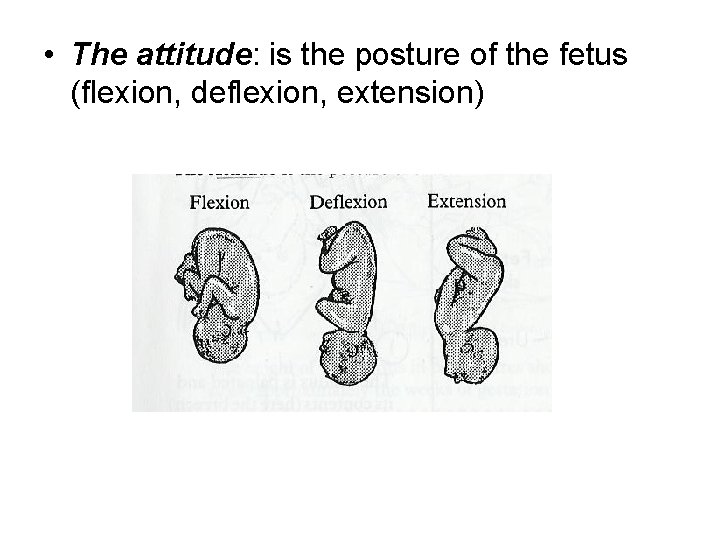
• The attitude: is the posture of the fetus (flexion, deflexion, extension)
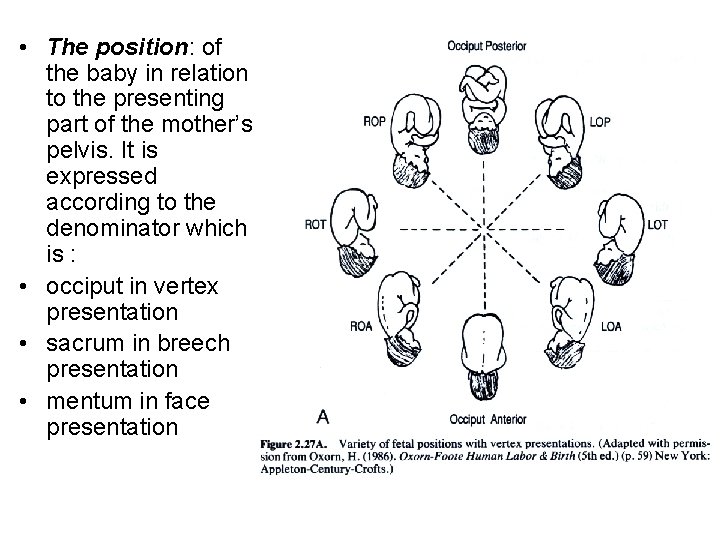
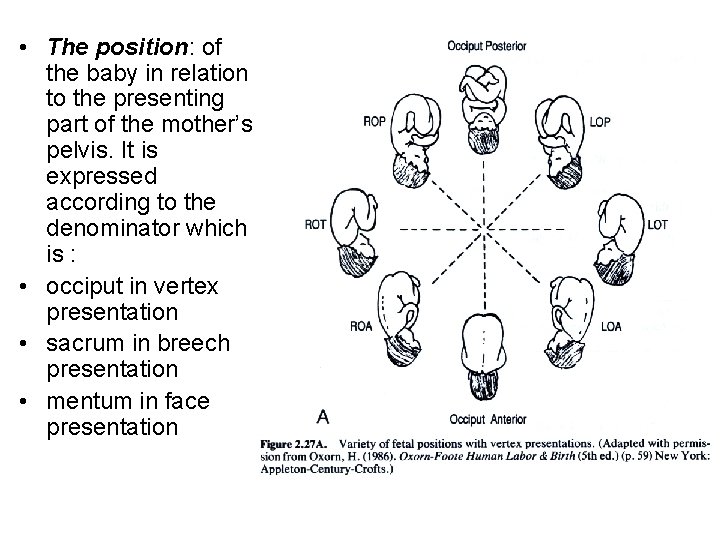
• The position: of the baby in relation to the presenting part of the mother’s pelvis. It is expressed according to the denominator which is : • occiput in vertex presentation • sacrum in breech presentation • mentum in face presentation
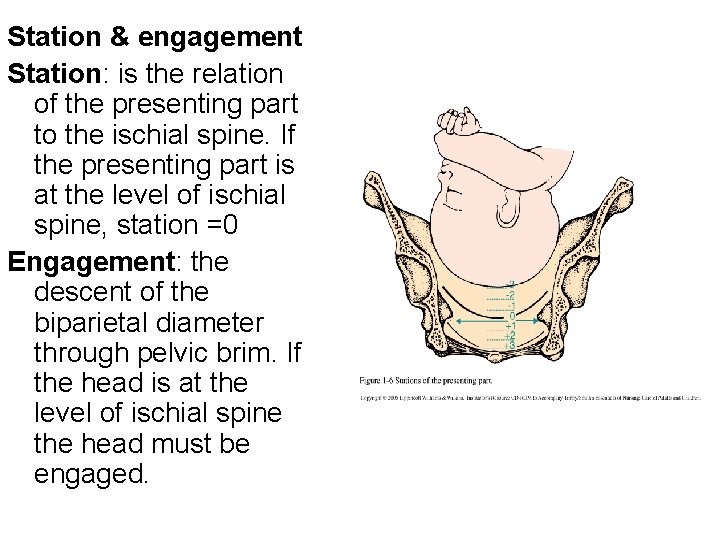
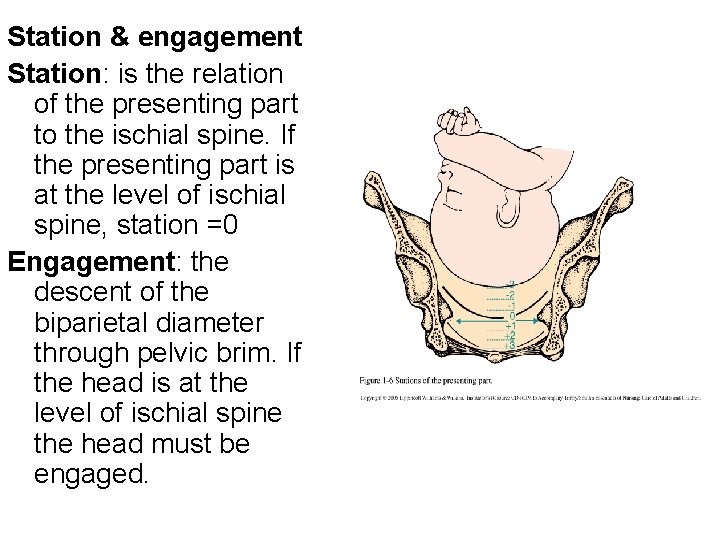
Station & engagement Station: is the relation of the presenting part to the ischial spine. If the presenting part is at the level of ischial spine, station =0 Engagement: the descent of the biparietal diameter through pelvic brim. If the head is at the level of ischial spine the head must be engaged.
Method of abdominal exam • Lateral Palpation (B): (determine the position of the fetal back and small parts) • Hands are placed on each side of the umbilicus. The fetal spine will palpate as firm, flat and linear. The fetal extremities are palpable by their varying contour and movements. The purpose of this maneuver is to determine whether the fetal back is left or right.

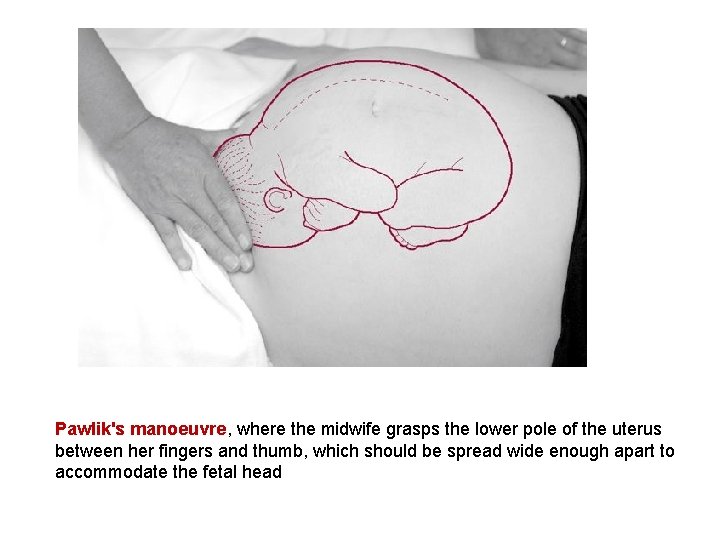
Method of abdominal exam • Pelvic palpation (C): 2 maneuvers • Grasp the lower poles of the uterus between fingers and thumbs and comment of the size, flexion and mobility of the head. • To determine the position of the vertex presentation: try to palpate the prominences (occiput @ the same side of the back & sincipital @ the opposite side of the back)
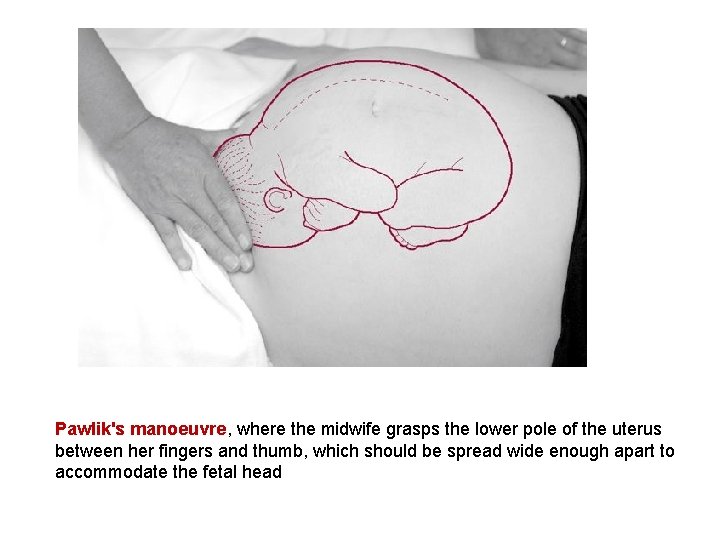
Pawlik's manoeuvre, where the midwife grasps the lower pole of the uterus between her fingers and thumb, which should be spread wide enough apart to accommodate the fetal head
Method of abdominal exam • 3 - Auscultation: help assess fetal well being Auscult the whole abdomen trying to locate the point of maximum intensity
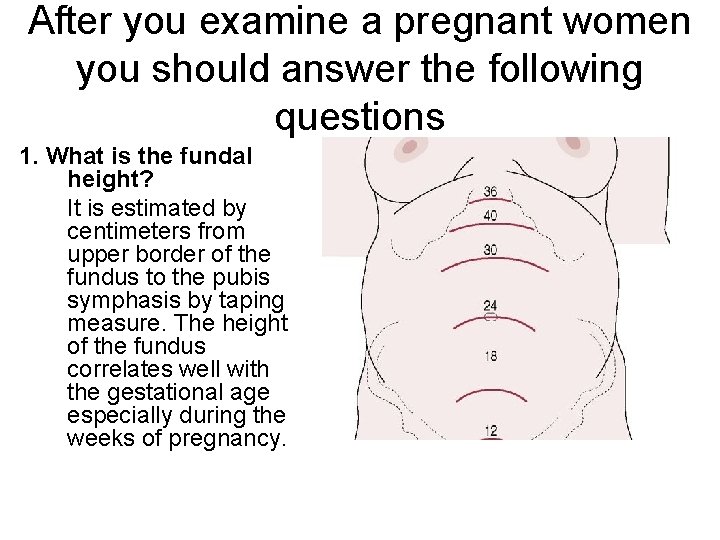
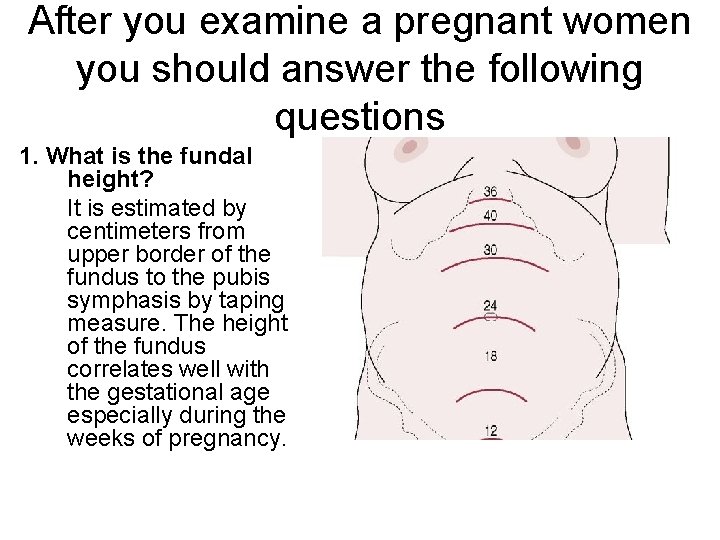
After you examine a pregnant women you should answer the following questions 1. What is the fundal height? It is estimated by centimeters from upper border of the fundus to the pubis symphasis by taping measure. The height of the fundus correlates well with the gestational age especially during the weeks of pregnancy.
After you examine a pregnant women you should answer the following questions 2. lie of the fetus: only longitudinal lie is normal 3. Attitude: normally it is full flexion and every fetal joint is flexed. 4. presentation: normally cephalic 5. position: according to the dominator 6. Is the vertex engaged?

• THANKS for your Attention
 Antenatal care definition
Antenatal care definition Etiolgy
Etiolgy Antenatal care summary
Antenatal care summary Introduction of antenatal care
Introduction of antenatal care Antenatal care definition
Antenatal care definition Antenatal care conclusion
Antenatal care conclusion Name given to judah by romans refers to the philistines
Name given to judah by romans refers to the philistines Leopold's maneuver
Leopold's maneuver Banc plus
Banc plus Nice antenatal and postnatal mental health
Nice antenatal and postnatal mental health Antenatal visit according to who
Antenatal visit according to who Mcug
Mcug Antenatal investigations
Antenatal investigations Antenatal assessment format
Antenatal assessment format Antenatal intrapartum and postnatal
Antenatal intrapartum and postnatal Antenatal class adalah
Antenatal class adalah An immediate and temporary care
An immediate and temporary care Primary secondary and tertiary care
Primary secondary and tertiary care In the given below statement what does the pf indicate
In the given below statement what does the pf indicate Assuming a 1 kb page size
Assuming a 1 kb page size Background information in a plot is given in the:
Background information in a plot is given in the: How to calculate average speed
How to calculate average speed Construction of a line parallel to a given line
Construction of a line parallel to a given line The gui for metasploit is given by
The gui for metasploit is given by