ESMOE Safe Caesarean Delivery Aims To understand the

- Slides: 40
ESMOE Safe Caesarean Delivery
Aims • To understand the burden of mortality related to caesarean delivery (CD) in South Africa • To understand the clinical, administrative and managerial factors required to enable safe CD • To describe checklists for accrediting surgeon, anaesthetists and facility for safe CD • To discuss strategies to implement Safe CD action plans in a district, with rational use of resources • To acquire skills for monitoring CD rates and CD case fatality rates.
Background: Sixth Saving Mothers report 2011 -2013 • 655, 686 women were delivered with a Caesarean Delivery • CD rate for SA: 23. 1% (public sector), 67% (private sector) • 1243 maternal deaths where a Caesarean delivery was the mode of delivery • 1471 deaths after vaginal delivery
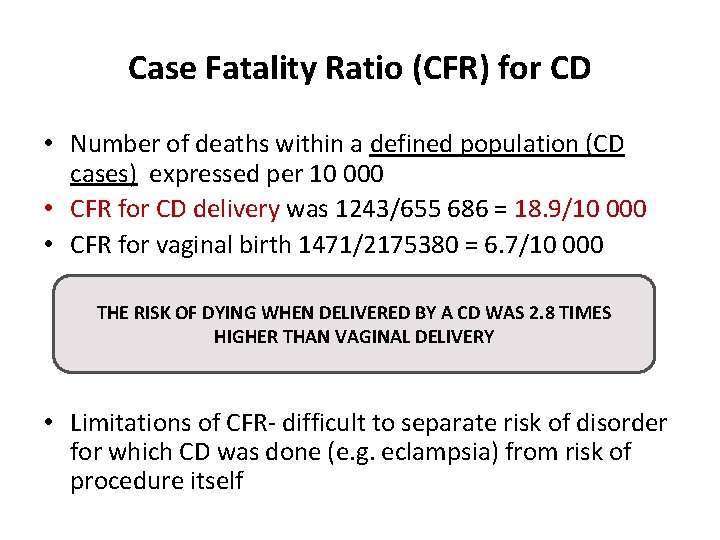
Case Fatality Ratio (CFR) for CD • Number of deaths within a defined population (CD cases) expressed per 10 000 • CFR for CD delivery was 1243/655 686 = 18. 9/10 000 • CFR for vaginal birth 1471/2175380 = 6. 7/10 000 THE RISK OF DYING WHEN DELIVERED BY A CD WAS 2. 8 TIMES HIGHER THAN VAGINAL DELIVERY • Limitations of CFR- difficult to separate risk of disorder for which CD was done (e. g. eclampsia) from risk of procedure itself
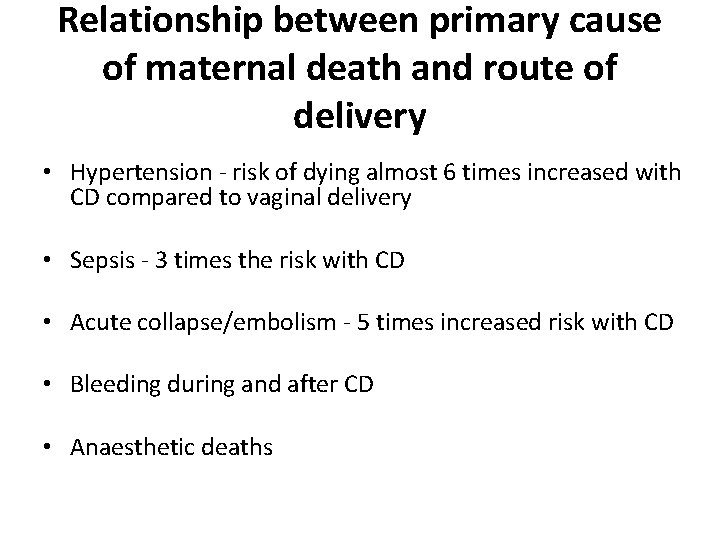
Relationship between primary cause of maternal death and route of delivery • Hypertension - risk of dying almost 6 times increased with CD compared to vaginal delivery • Sepsis - 3 times the risk with CD • Acute collapse/embolism - 5 times increased risk with CD • Bleeding during and after CD • Anaesthetic deaths
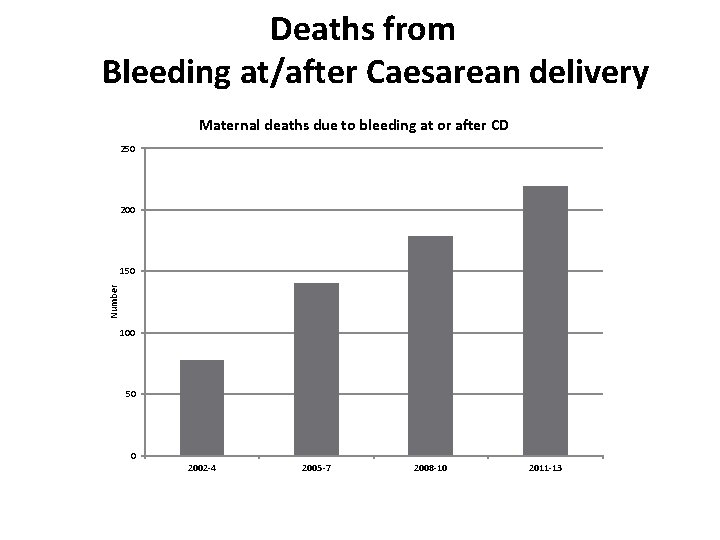
Deaths from Bleeding associated with Caesarean delivery
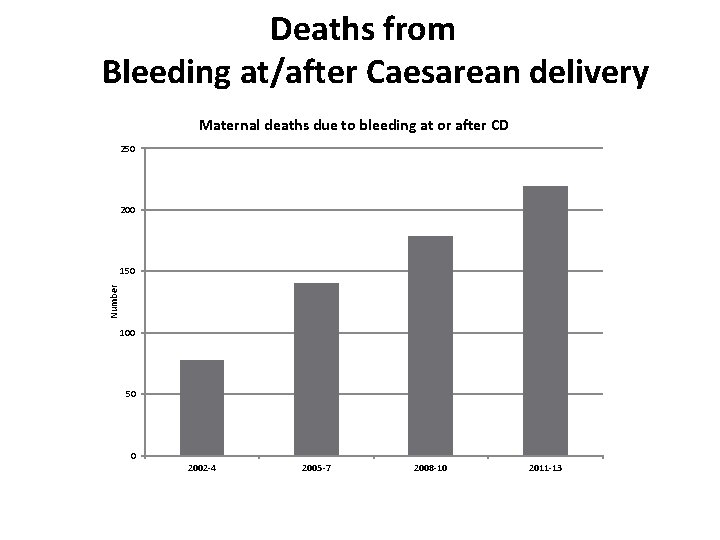
Deaths from Bleeding at/after Caesarean delivery Maternal deaths due to bleeding at or after CD 250 200 Number 150 100 50 0 2002 -4 2005 -7 2008 -10 2011 -13
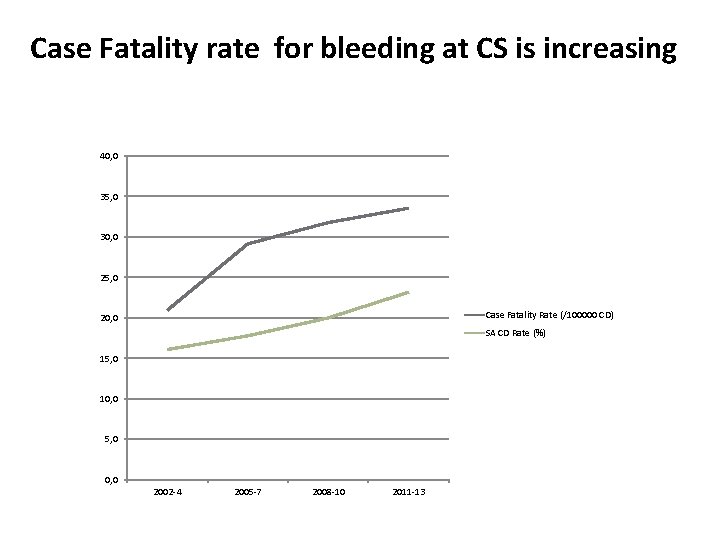
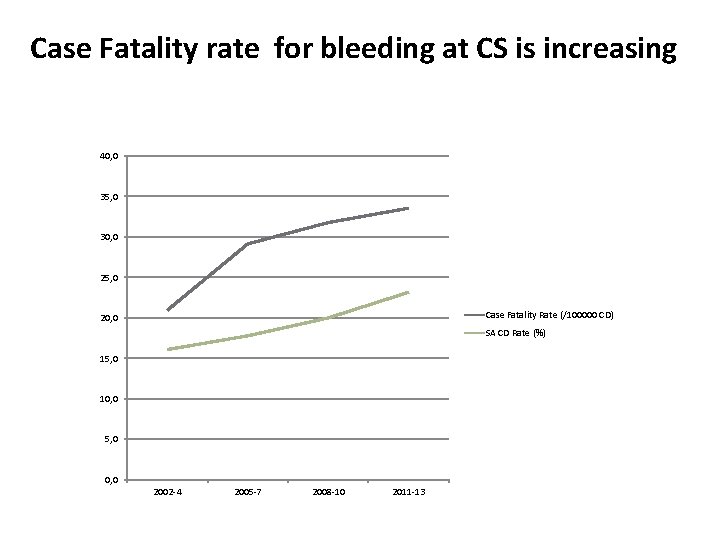
Case Fatality rate for bleeding at CS is increasing 40, 0 35, 0 30, 0 25, 0 Case Fatality Rate (/100000 CD) 20, 0 SA CD Rate (%) 15, 0 10, 0 5, 0 0, 0 2002 -4 2005 -7 2008 -10 2011 -13
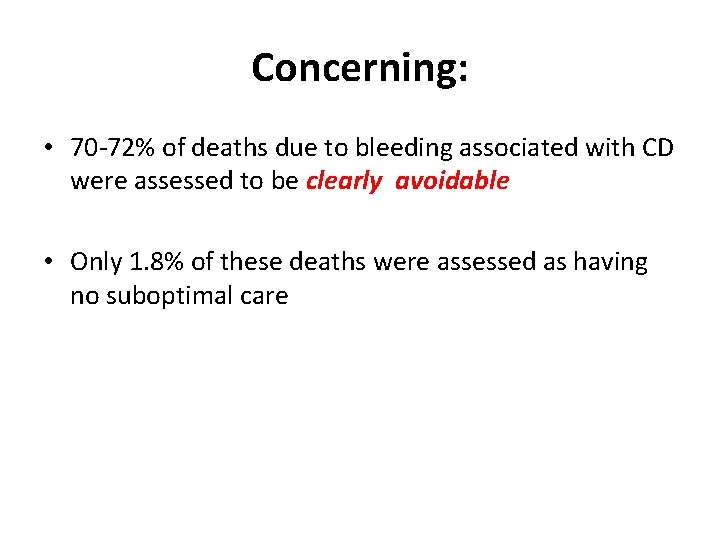
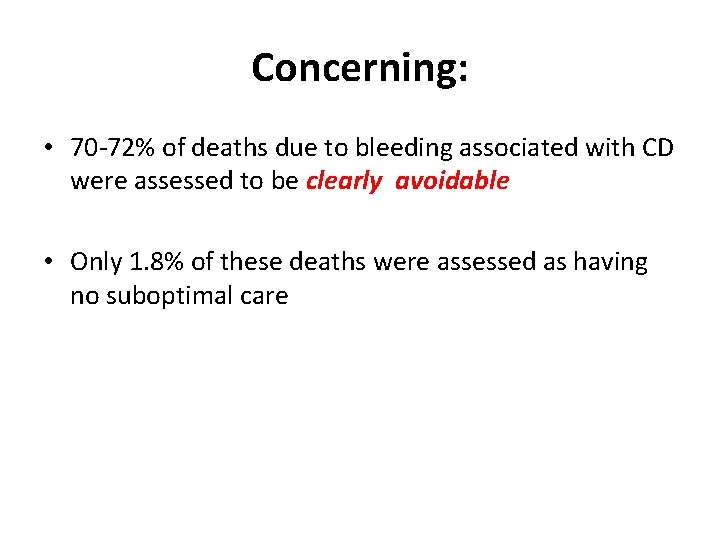
Concerning: • 70 -72% of deaths due to bleeding associated with CD were assessed to be clearly avoidable • Only 1. 8% of these deaths were assessed as having no suboptimal care
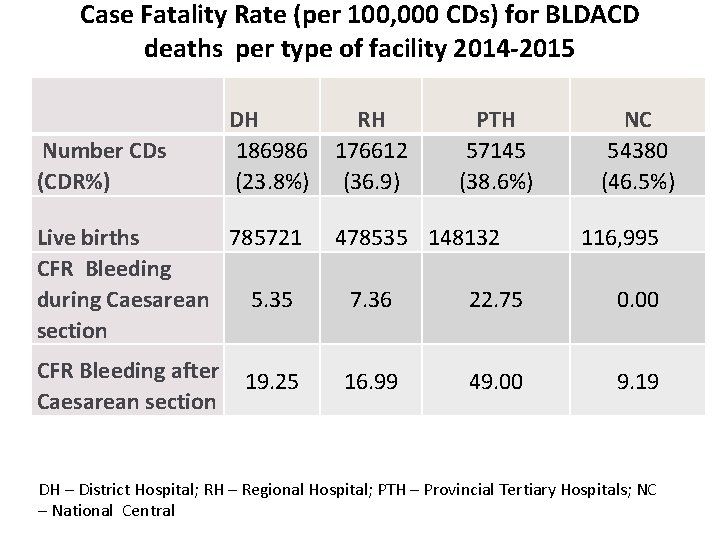
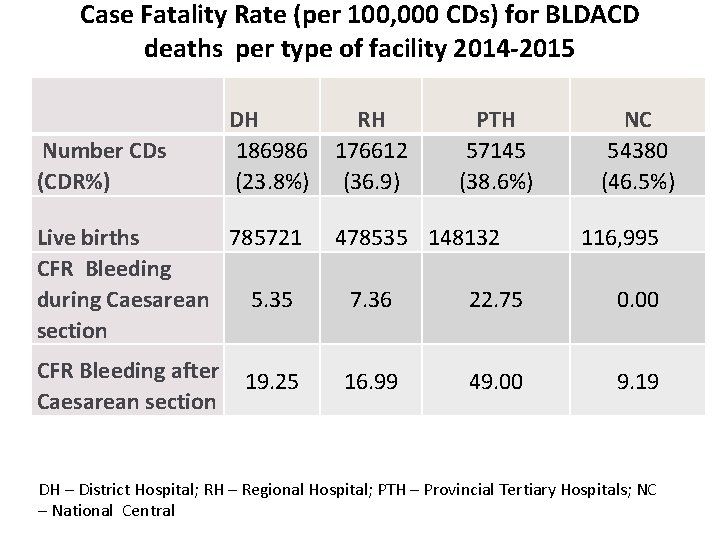
Case Fatality Rate (per 100, 000 CDs) for BLDACD deaths per type of facility 2014 -2015 Number CDs (CDR%) DH 186986 (23. 8%) Live births 785721 CFR Bleeding during Caesarean 5. 35 section CFR Bleeding after Caesarean section 19. 25 . RH 176612 (36. 9) PTH 57145 (38. 6%) 478535 148132 NC 54380 (46. 5%) 116, 995 7. 36 22. 75 0. 00 16. 99 49. 00 9. 19 DH – District Hospital; RH – Regional Hospital; PTH – Provincial Tertiary Hospitals; NC – National Central
QUESTION A 1. What can be done to reduce deaths due to bleeding associated with Caesarean delivery? List two interventions.
What can be done? • • • Prevention of excessive bleeding at/after CD Be prepared Early detection Immediate treatment Definitive treatment Timely, Safe and Appropriate referral Refer to PPH algorithms in PPH and CD monographs/ESMOE Aid.
Deaths from Anaesthesia at CD NB: Anaesthetic deaths: 2/3 spinal, 1/3 general
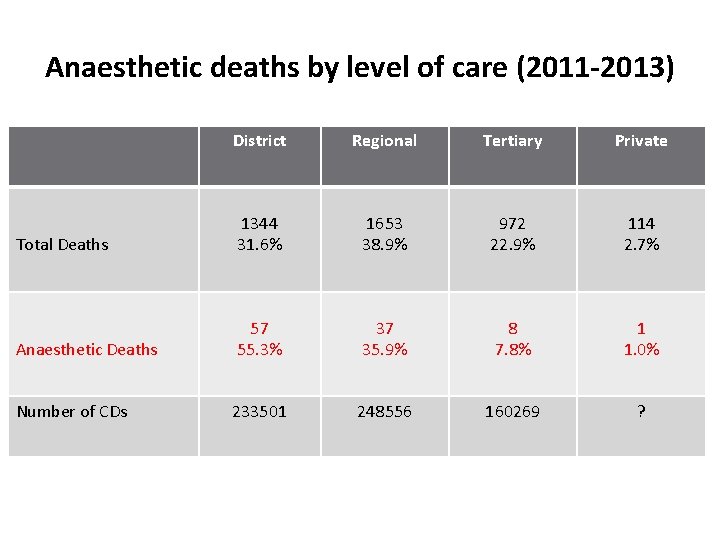
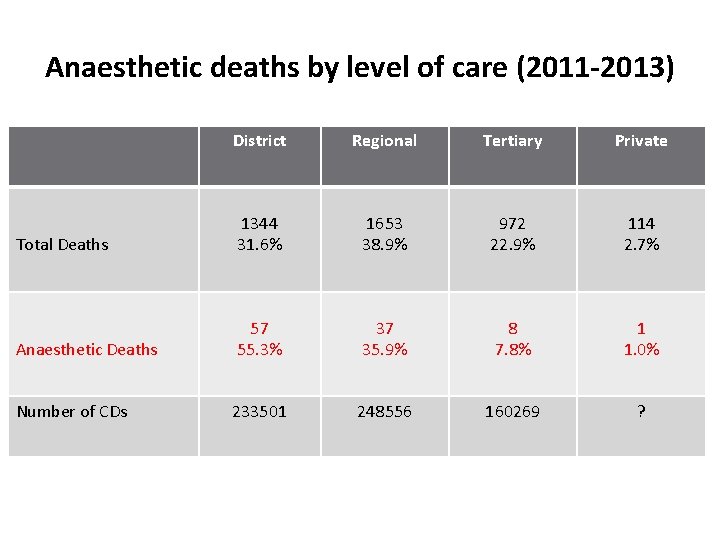
Anaesthetic deaths by level of care (2011 -2013) District Regional Tertiary Private Total Deaths 1344 31. 6% 1653 38. 9% 972 22. 9% 114 2. 7% Anaesthetic Deaths 57 55. 3% 37 35. 9% 8 7. 8% 1 1. 0% Number of CDs 233501 248556 160269 ?
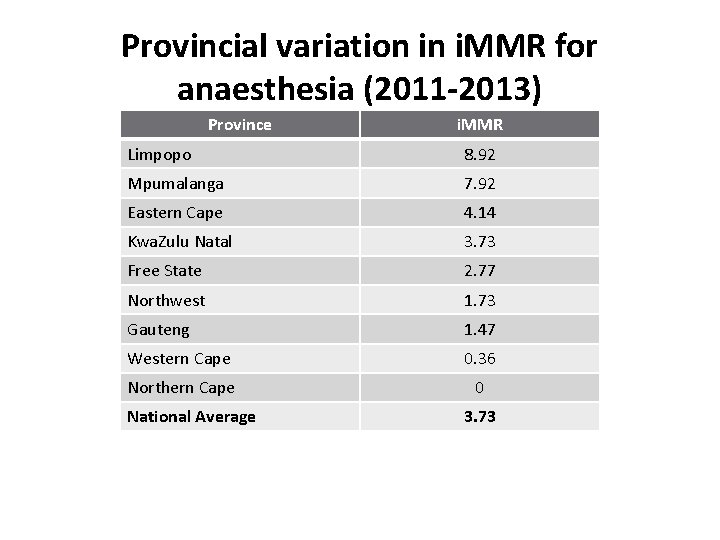
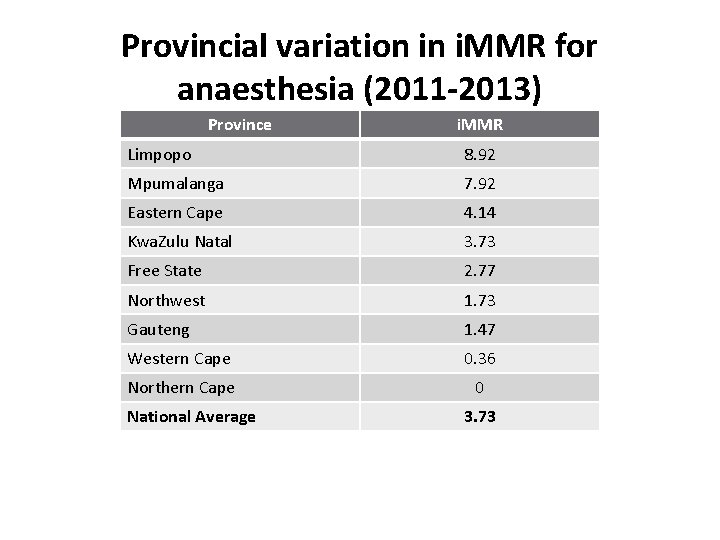
Provincial variation in i. MMR for anaesthesia (2011 -2013) Province i. MMR Limpopo 8. 92 Mpumalanga 7. 92 Eastern Cape 4. 14 Kwa. Zulu Natal 3. 73 Free State 2. 77 Northwest 1. 73 Gauteng 1. 47 Western Cape 0. 36 Northern Cape 0 National Average 3. 73
QUESTION A 2. What can be done to reduce deaths due to anaesthesia for CD? List two interventions.
What can be done? • Anaesthetic training/accreditation • Use of vasopressors for spinal anaesthesia • Difficult scenarios: massive OH and eclampsia • ESMOE module: spinal and GA • Anaesthetic outreach and support to district hospitals • Clinical officers? • Avoid single operator/anaesthetist
QUESTION A 3. What can be done to reduce deaths from Puerperal sepsis following CD List two interventions.
What can be done? • Prevent prolonged labour and multiple PVs • Prophylactic antibiotics • Adequate therapeutic antibiotics • Early surgical intervention • Postnatal care coverage
QUESTION A 4. What can be done to reduce deaths from Thrombo-embolism after CD ? List two interventions.
What can be done? • Hydration • Early mobilisation • Thromboprophylaxis • Early detection and treatment of VTE
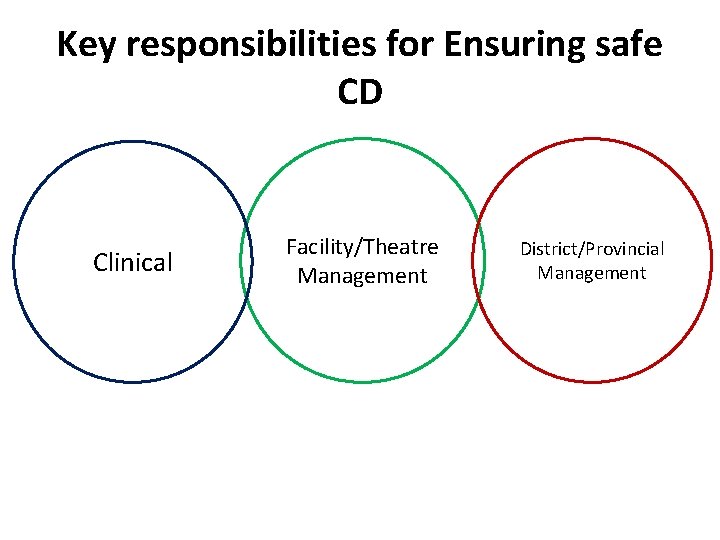
Key responsibilities for Ensuring safe CD Clinical Facility/Theatre Management District/Provincial Management
Clinical responsibilities for safe CD • Prevention of unnecessary CD • Prevention and treatment of mortality and morbidity from – Bleeding – Sepsis – Thromboembolism – Anaesthetic complications (protocols, training, competency checklists, M&M)
QUESTION B What are the responsibilities of: • facility /theatre mangers in reducing deaths from CD ? • district and provincial managers List two responsibilities for each
Facility management responsibilities for safe CD • • • Supplies Medicines Equipment Blood & FDPs Adequate numbers staff/ deployment (accreditation checklists/ needs analysis)
District/Provincial management responsibilities for safe CD • Diversion resources to improve CD safety in identified facilities • Stop CD at those which cannot provide safe service • Balance safety with accessibility • Prevention of overload at PTHs/ OMBUs • Leadership, monitoring and accountability
SETTING MINIMUM STANDARDS FOR CD
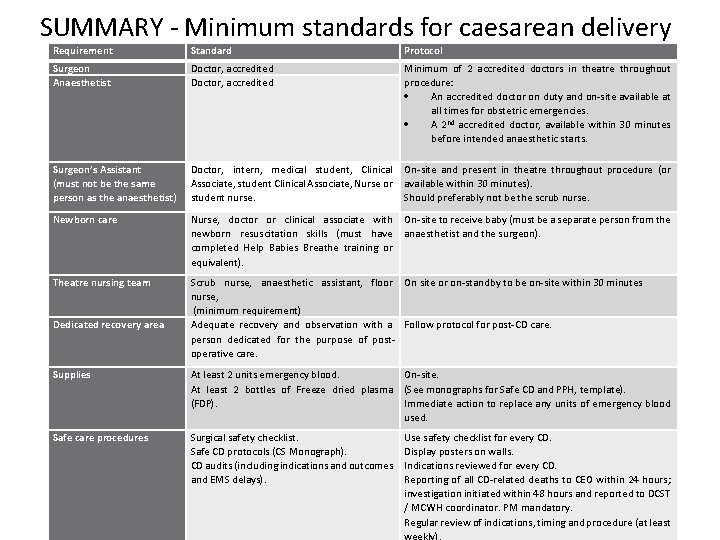
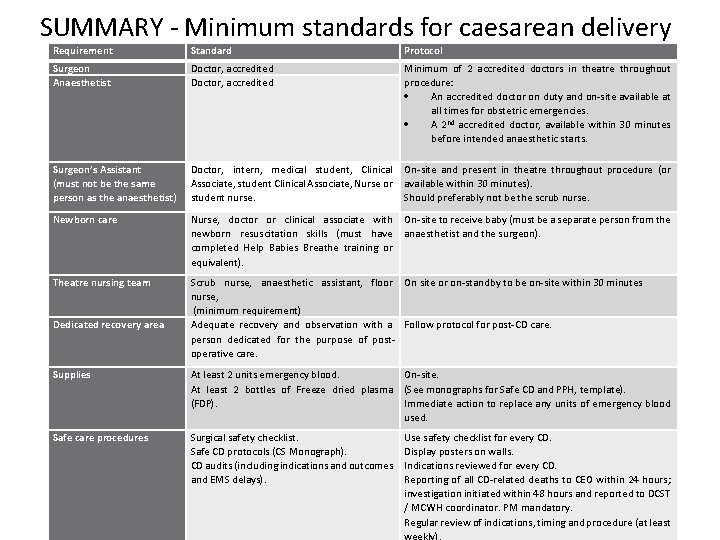
SUMMARY - Minimum standards for caesarean delivery Requirement Standard Protocol Surgeon Anaesthetist Doctor, accredited Minimum of 2 accredited doctors in theatre throughout procedure: An accredited doctor on duty and on-site available at all times for obstetric emergencies. A 2 nd accredited doctor, available within 30 minutes before intended anaesthetic starts. Surgeon’s Assistant (must not be the same person as the anaesthetist) Doctor, intern, medical student, Clinical Associate, student Clinical Associate, Nurse or student nurse. On-site and present in theatre throughout procedure (or available within 30 minutes). Should preferably not be the scrub nurse. Newborn care Nurse, doctor or clinical associate with newborn resuscitation skills (must have completed Help Babies Breathe training or equivalent). On-site to receive baby (must be a separate person from the anaesthetist and the surgeon). Theatre nursing team Scrub nurse, anaesthetic assistant, floor On site or on-standby to be on-site within 30 minutes nurse, (minimum requirement) Adequate recovery and observation with a Follow protocol for post-CD care. person dedicated for the purpose of postoperative care. Dedicated recovery area Supplies At least 2 units emergency blood. At least 2 bottles of Freeze dried plasma (FDP). On-site. (See monographs for Safe CD and PPH, template). Immediate action to replace any units of emergency blood used. Safe care procedures Surgical safety checklist. Safe CD protocols (CS Monograph). CD audits (including indications and outcomes and EMS delays). Use safety checklist for every CD. Display posters on walls. Indications reviewed for every CD. Reporting of all CD-related deaths to CEO within 24 hours; investigation initiated within 48 hours and reported to DCST / MCWH coordinator. PM mandatory. Regular review of indications, timing and procedure (at least weekly).
TOOLS • • • Checklists for facilities Competency Checklist – surgeon Competency Checklist – anaesthetist Surgical safety Checklist Detailed action plan
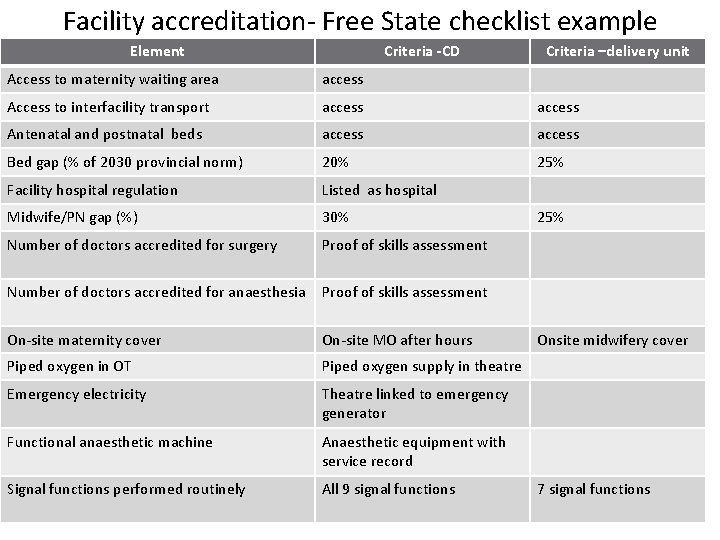
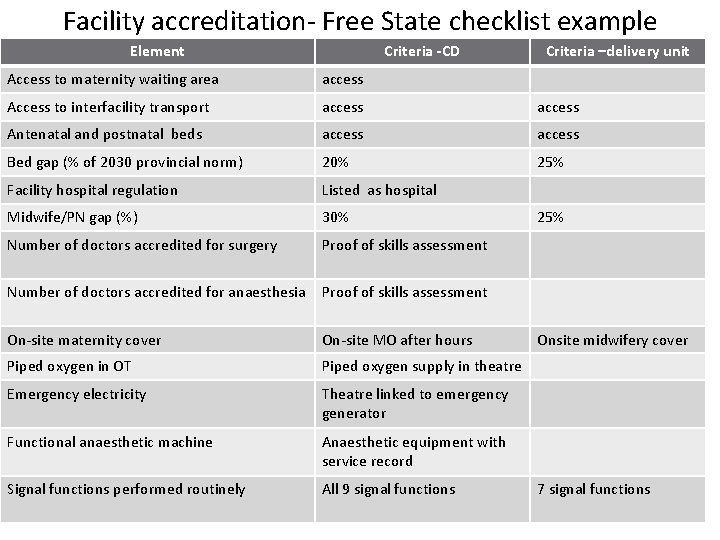
Facility accreditation- Free State checklist example Element Criteria -CD Criteria –delivery unit Access to maternity waiting area access Access to interfacility transport access Antenatal and postnatal beds access Bed gap (% of 2030 provincial norm) 20% 25% Facility hospital regulation Listed as hospital Midwife/PN gap (%) 30% Number of doctors accredited for surgery Proof of skills assessment Number of doctors accredited for anaesthesia Proof of skills assessment On-site maternity cover On-site MO after hours Piped oxygen in OT Piped oxygen supply in theatre Emergency electricity Theatre linked to emergency generator Functional anaesthetic machine Anaesthetic equipment with service record Signal functions performed routinely All 9 signal functions 25% Onsite midwifery cover 7 signal functions
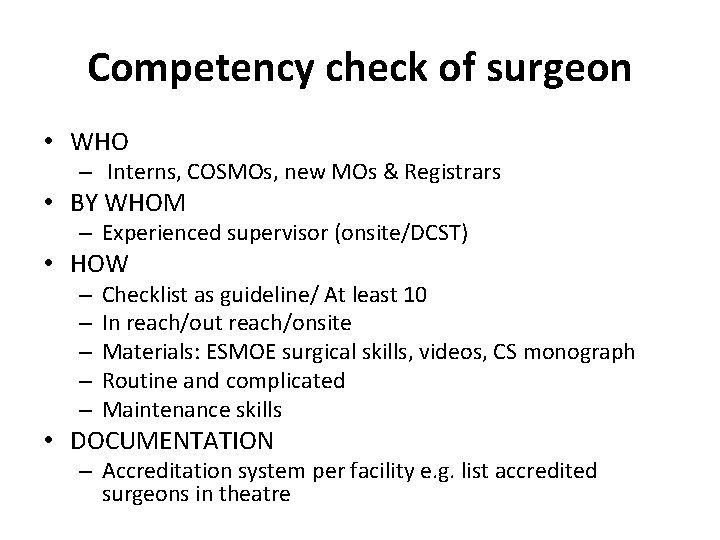
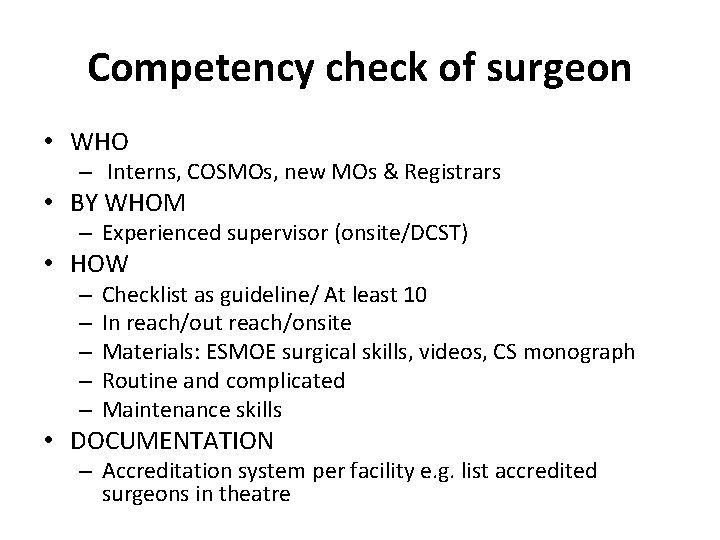
Competency check of surgeon • WHO – Interns, COSMOs, new MOs & Registrars • BY WHOM – Experienced supervisor (onsite/DCST) • HOW – – – Checklist as guideline/ At least 10 In reach/out reach/onsite Materials: ESMOE surgical skills, videos, CS monograph Routine and complicated Maintenance skills • DOCUMENTATION – Accreditation system per facility e. g. list accredited surgeons in theatre
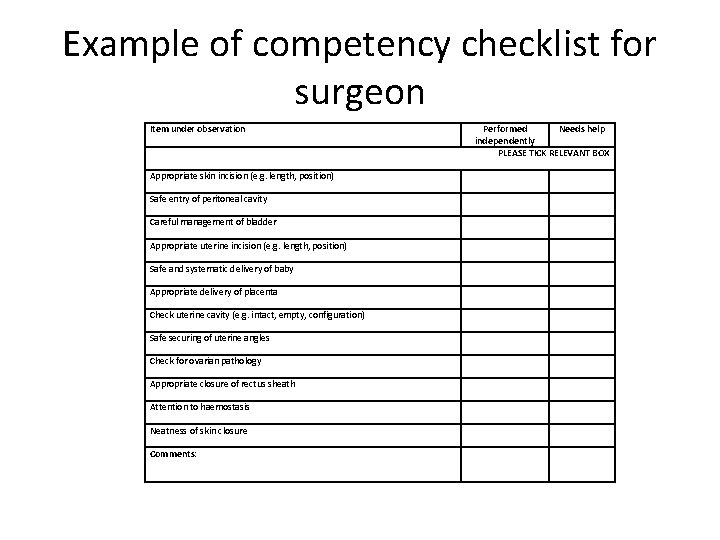
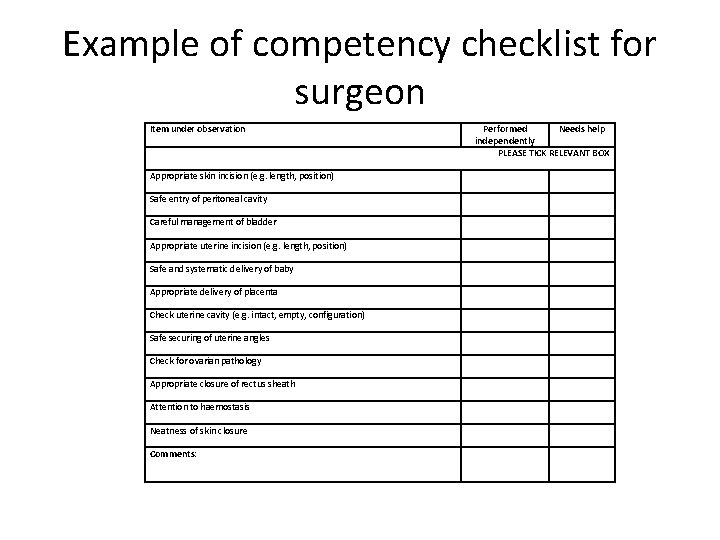
Example of competency checklist for surgeon Item under observation Appropriate skin incision (e. g. length, position) Safe entry of peritoneal cavity Careful management of bladder Appropriate uterine incision (e. g. length, position) Safe and systematic delivery of baby Appropriate delivery of placenta Check uterine cavity (e. g. intact, empty, configuration) Safe securing of uterine angles Check for ovarian pathology Appropriate closure of rectus sheath Attention to haemostasis Neatness of skin closure Comments: Performed Needs help independently PLEASE TICK RELEVANT BOX
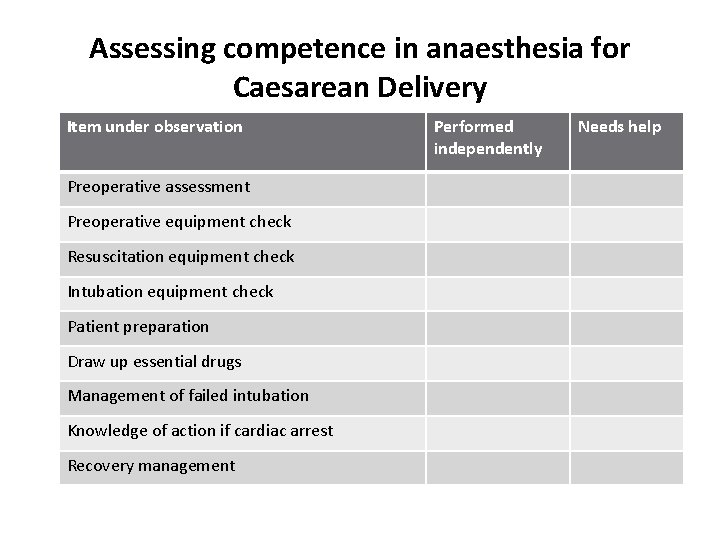
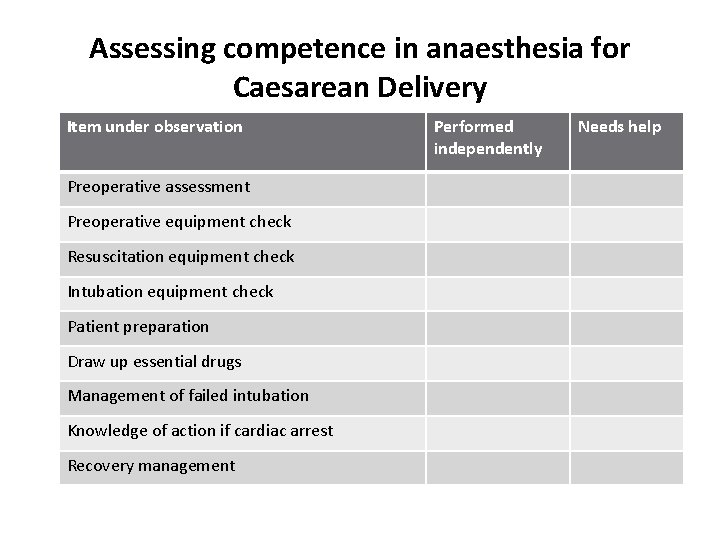
Assessing competence in anaesthesia for Caesarean Delivery Item under observation Preoperative assessment Preoperative equipment check Resuscitation equipment check Intubation equipment check Patient preparation Draw up essential drugs Management of failed intubation Knowledge of action if cardiac arrest Recovery management Performed independently Needs help
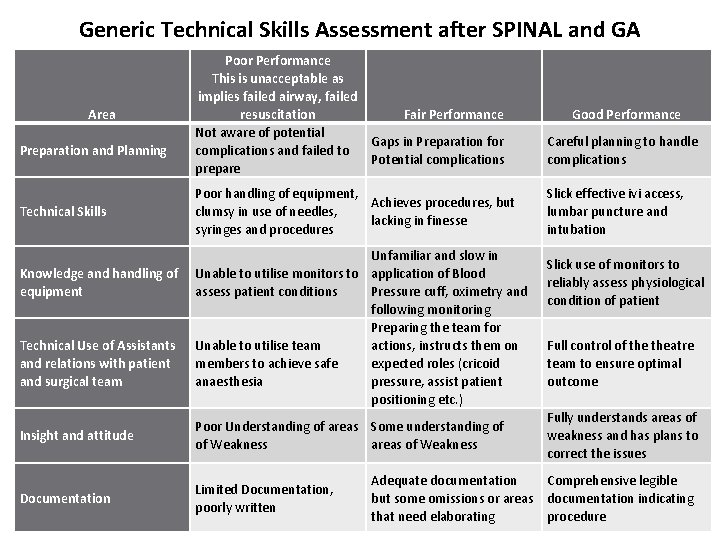
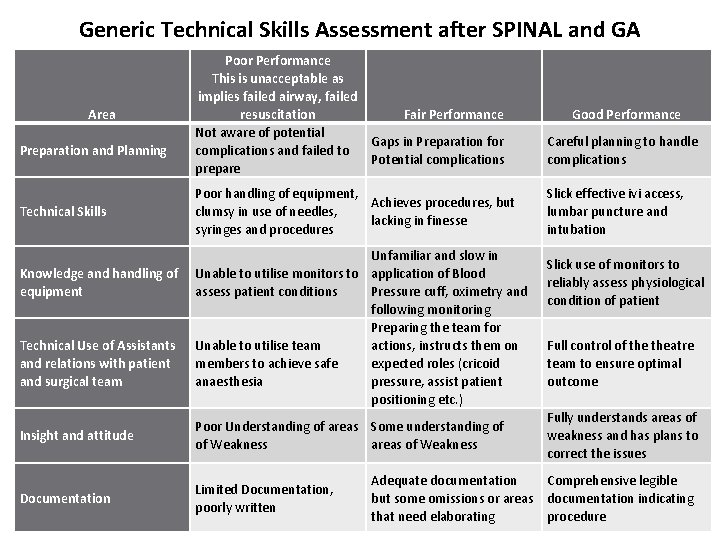
Generic Technical Skills Assessment after SPINAL and GA Area Preparation and Planning Technical Skills Knowledge and handling of equipment Technical Use of Assistants and relations with patient and surgical team Poor Performance This is unacceptable as implies failed airway, failed resuscitation Fair Performance Not aware of potential Gaps in Preparation for complications and failed to Potential complications prepare Poor handling of equipment, Achieves procedures, but clumsy in use of needles, lacking in finesse syringes and procedures Unfamiliar and slow in Unable to utilise monitors to application of Blood assess patient conditions Pressure cuff, oximetry and following monitoring Preparing the team for Unable to utilise team actions, instructs them on members to achieve safe expected roles (cricoid anaesthesia pressure, assist patient positioning etc. ) Insight and attitude Poor Understanding of areas Some understanding of of Weakness areas of Weakness Documentation Limited Documentation, poorly written Good Performance Careful planning to handle complications Slick effective ivi access, lumbar puncture and intubation Slick use of monitors to reliably assess physiological condition of patient Full control of theatre team to ensure optimal outcome Fully understands areas of weakness and has plans to correct the issues Adequate documentation Comprehensive legible but some omissions or areas documentation indicating that need elaborating procedure
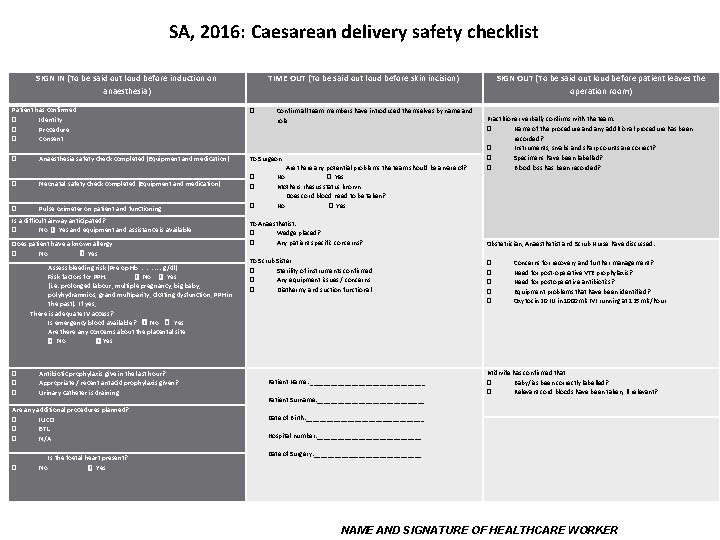
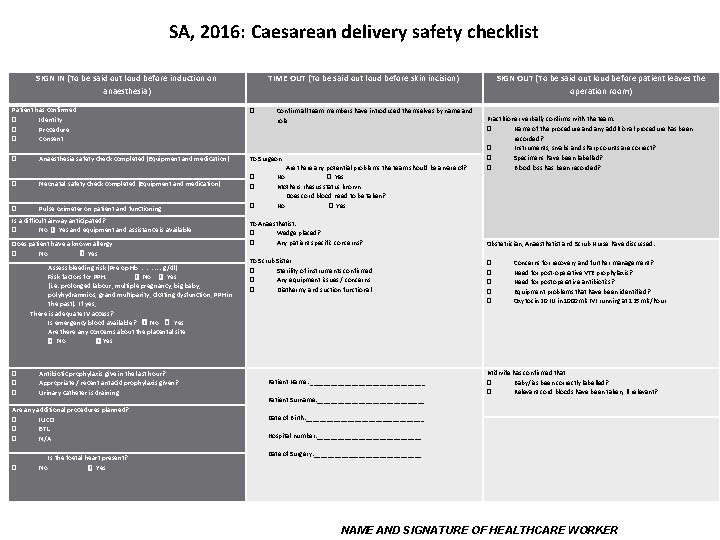
SA, 2016: Caesarean delivery safety checklist SIGN IN (To be said out loud before induction on anaesthesia) TIME OUT (To be said out loud before skin incision) Patient has confirmed � Identity � Procedure � Consent � � Anaesthesia safety check completed (Equipment and medication) To Surgeon � Neonatal safety check completed (Equipment and medication) � � � Pulse oximeter on patient and functioning � Is a difficult airway anticipated? � No � Yes and equipment and assistance is available Does patient have a known allergy � No � Yes Assess bleeding risk (Pre op Hb ………. . …g/dl) Risk factors for PPH. � No � Yes (i. e. prolonged labour, multiple pregnancy, big baby, polyhydramnios, grand multiparity, clotting dysfunction, PPH in the past). If yes, There is adequate IV access? Is emergency blood available? � No � Yes Are there any concerns about the placental site � No � Yes � � � Antibiotic prophylaxis give in the last hour? Appropriate / recent antacid prophylaxis given? Urinary catheter is draining Are any additional procedures planned? � IUCD � BTL � N/A � No Is the foetal heart present? � Yes Confirm all team members have introduced themselves by name and role Are there any potential problems the team should be aware of? No � Yes Mothers rhesus status known Does cord blood need to be taken? No � Yes To Anaesthetist: � Wedge placed? � Any patient specific concerns? To Scrub Sister � Sterility of instruments confirmed � Any equipment issues / concerns � Diathermy and suction functional Patient Name: _________________ Patient Surname: ________________ SIGN OUT (To be said out loud before patient leaves the operation room) Practitioner verbally confirms with the team: � Name of the procedure and any additional procedure has been recorded? � Instruments, swabs and sharp counts are correct? � Specimens have been labelled? � Blood loss has been recorded? Obstetrician, Anaesthetist and Scrub Nurse have discussed: � � � Concerns for recovery and further management? Need for post-operative VTE prophylaxis? Need for postoperative antibiotics? Equipment problems that have been identified? Oxytocin 20 IU in 1000 mls IVI running at 125 mls/hour Midwife has confirmed that � Baby/ies been correctly labelled? � Relevant cord bloods have been taken, if relevant? Date of Birth: _________________ Hospital number: _______________ Date of Surgery: ________________ NAME AND SIGNATURE OF HEALTHCARE WORKER
QUESTION C How could you monitor caesarean delivery outcomes and safety in your facility? List three indicators that could be used for this.
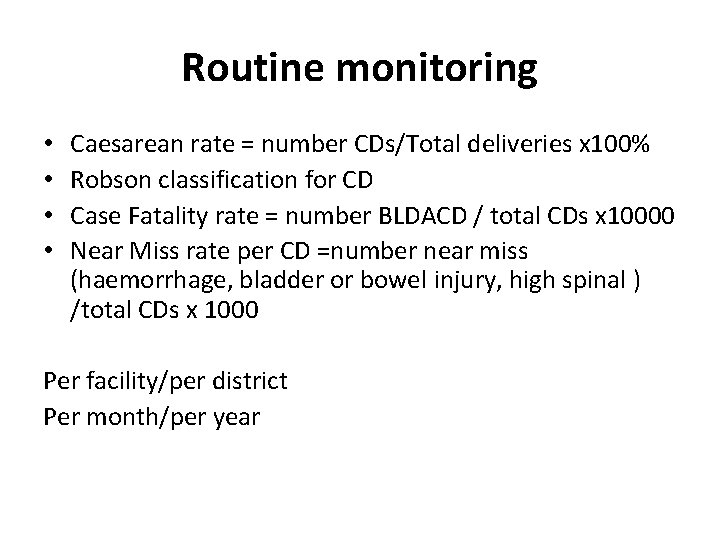
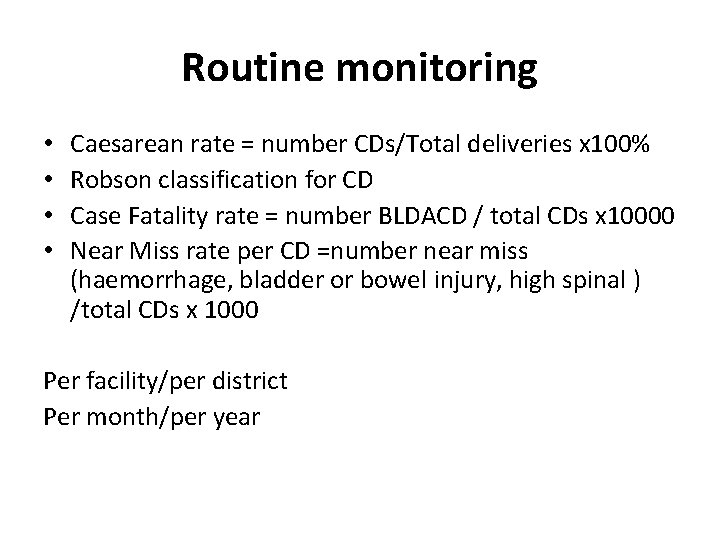
Routine monitoring • • Caesarean rate = number CDs/Total deliveries x 100% Robson classification for CD Case Fatality rate = number BLDACD / total CDs x 10000 Near Miss rate per CD =number near miss (haemorrhage, bladder or bowel injury, high spinal ) /total CDs x 1000 Per facility/per district Per month/per year
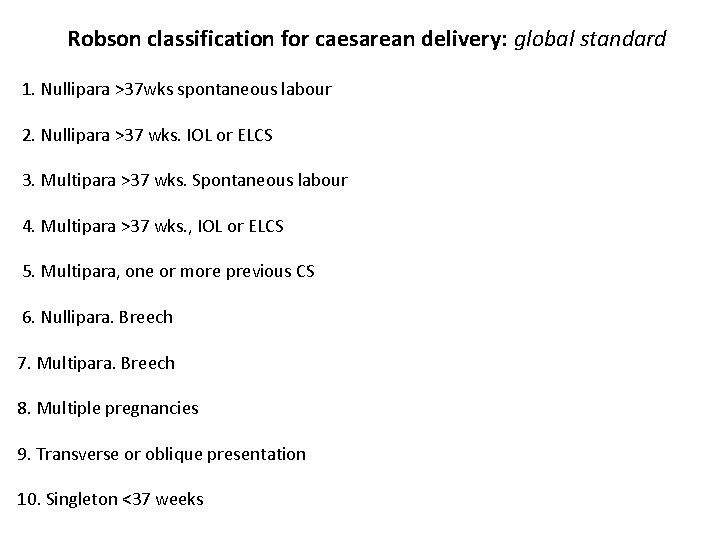
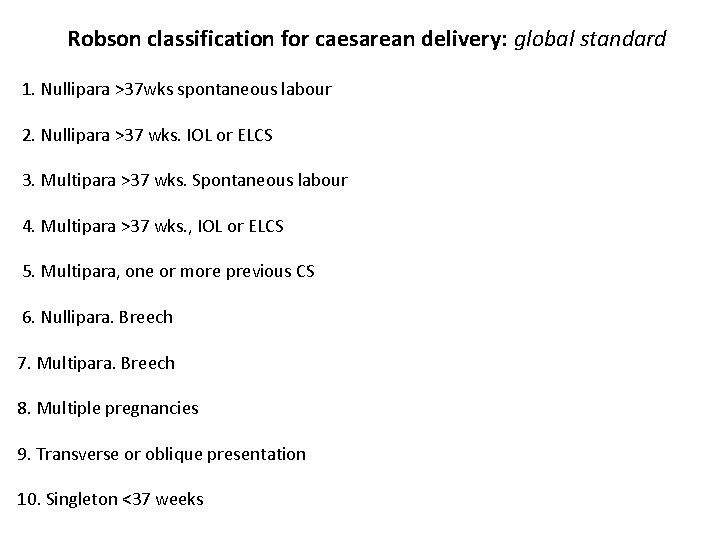
Robson classification for caesarean delivery: global standard 1. Nullipara >37 wks spontaneous labour 2. Nullipara >37 wks. IOL or ELCS 3. Multipara >37 wks. Spontaneous labour 4. Multipara >37 wks. , IOL or ELCS 5. Multipara, one or more previous CS 6. Nullipara. Breech 7. Multipara. Breech 8. Multiple pregnancies 9. Transverse or oblique presentation 10. Singleton <37 weeks

Recap Problem of CD mortality and morbidity in SA Clinical management of major problems Minimum standards for a facility providing CD Strategies to ensure compliance with minimum standards • District planning of maternity services to enable safe CD • Surgical safety checklist and accreditation tools • Monitoring and auditing • •
 Antenatal card
Antenatal card Doyen retractor contraindications
Doyen retractor contraindications To understand recursion you must understand recursion
To understand recursion you must understand recursion Safe feed safe food
Safe feed safe food Safe people safe places
Safe people safe places Prayer points for pregnant mothers
Prayer points for pregnant mothers Https methodology.accenture.com
Https methodology.accenture.com Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Số nguyên là gì
Số nguyên là gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Tia chieu sa te
Tia chieu sa te Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất ưu thế lai là gì
ưu thế lai là gì Sơ đồ cơ thể người
Sơ đồ cơ thể người Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Tư thế ngồi viết
Tư thế ngồi viết Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Tư thế ngồi viết
Tư thế ngồi viết Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Frameset trong html5
Frameset trong html5 Giọng cùng tên là
Giọng cùng tên là Phép trừ bù
Phép trừ bù Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Thang điểm glasgow
Thang điểm glasgow Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tiính động năng
Công thức tiính động năng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dot
Dot