OPERATIVE INSTRUMENTAL VAGINAL DELIVERY AND CAESAREAN SECTION HANNAH


- Slides: 25
OPERATIVE (INSTRUMENTAL) VAGINAL DELIVERY AND CAESAREAN SECTION HANNAH AND OLIVER
CONTENTS • What is operative delivery? • Indications for operative delivery - Maternal - Fetal • Instrumental delivery • LSCS
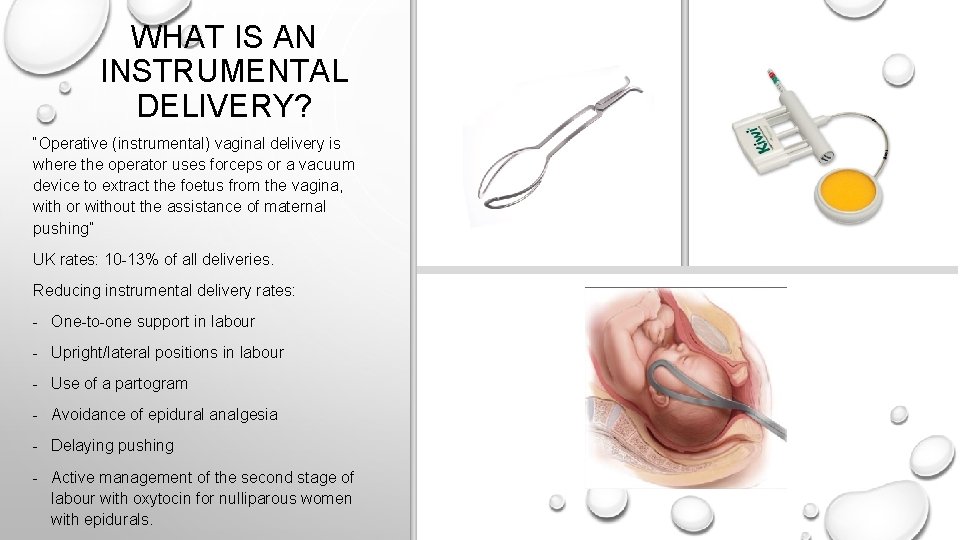
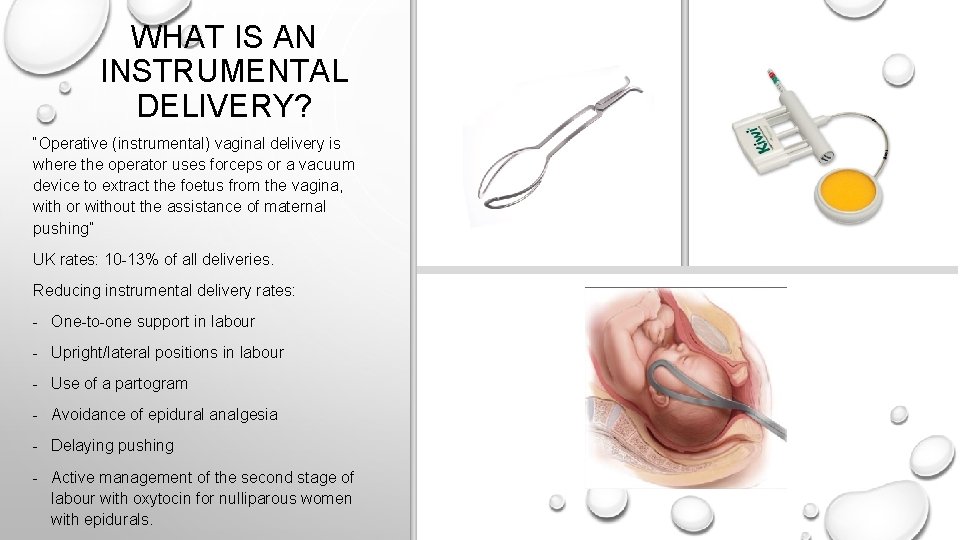
WHAT IS AN INSTRUMENTAL DELIVERY? “Operative (instrumental) vaginal delivery is where the operator uses forceps or a vacuum device to extract the foetus from the vagina, with or without the assistance of maternal pushing” UK rates: 10 -13% of all deliveries. Reducing instrumental delivery rates: - One-to-one support in labour - Upright/lateral positions in labour - Use of a partogram - Avoidance of epidural analgesia - Delaying pushing - Active management of the second stage of labour with oxytocin for nulliparous women with epidurals.
MATERNAL INDICATIONS • Inadequate progress - In primips, delivery is expected within about 2 hours of active second stage of labour (3 hours with regional analgesia). - In multiparous women, delivery is expected within 1 hour of starting active second stage of labour (2 hours with regional analgesia). • Maternal exhaustion - Unable to push • Maternal medical conditions that contraindicate prolonged pushing, e. g. severe hypertension, intercranial pathologies, cardiac disease.
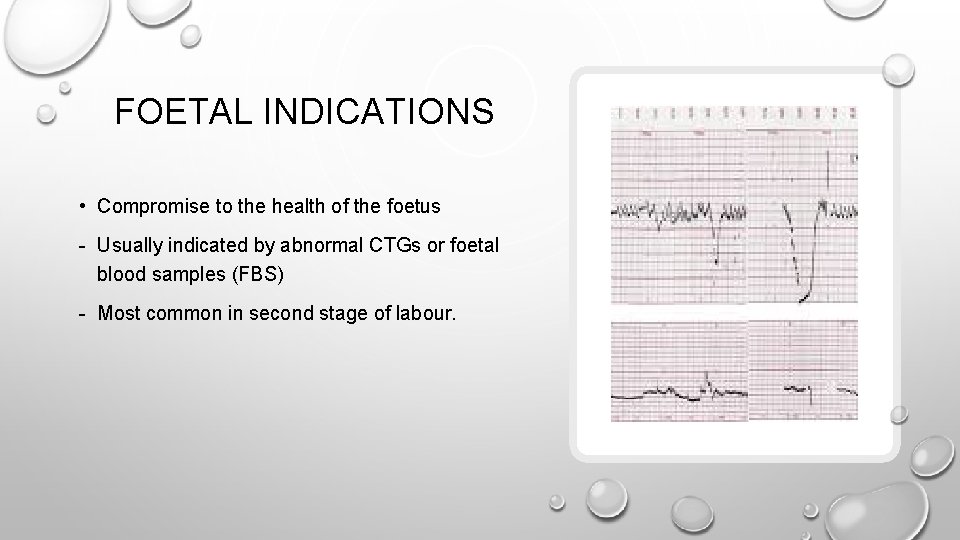
FOETAL INDICATIONS • Compromise to the health of the foetus - Usually indicated by abnormal CTGs or foetal blood samples (FBS) - Most common in second stage of labour.
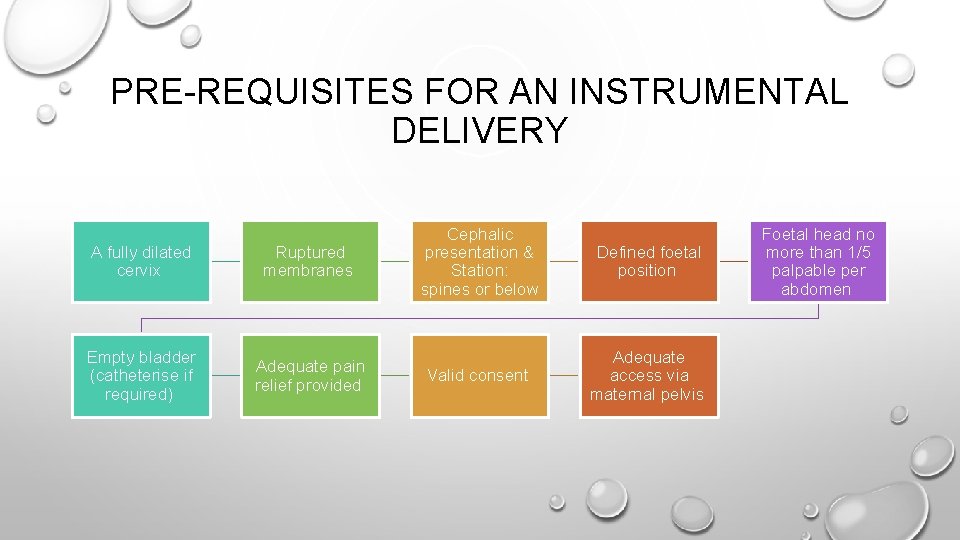
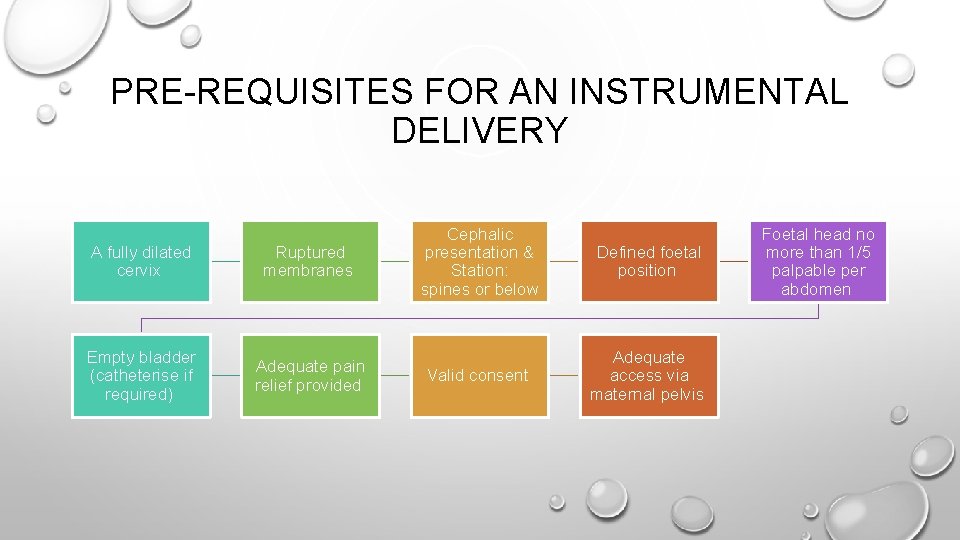
PRE-REQUISITES FOR AN INSTRUMENTAL DELIVERY A fully dilated cervix Ruptured membranes Empty bladder (catheterise if required) Adequate pain relief provided Cephalic presentation & Station: spines or below Defined foetal position Valid consent Adequate access via maternal pelvis Foetal head no more than 1/5 palpable per abdomen
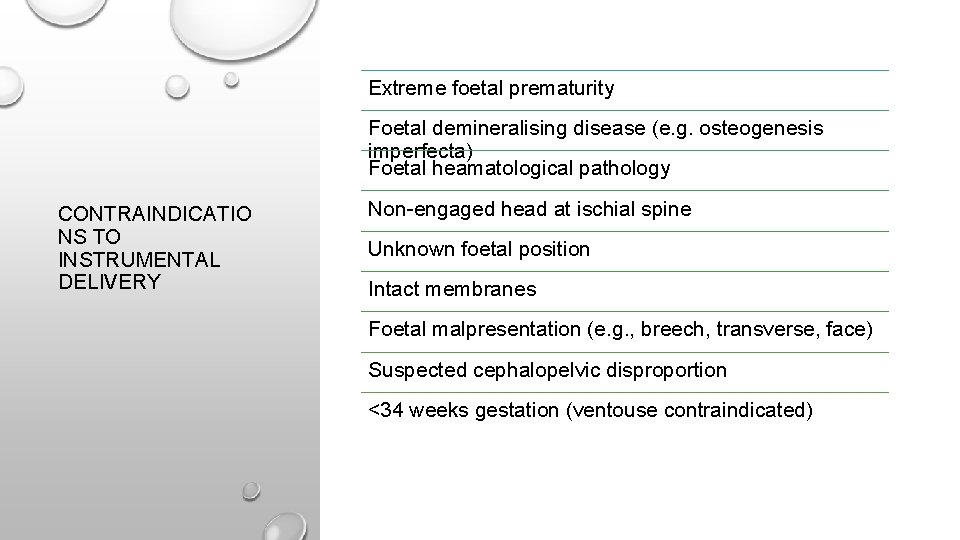
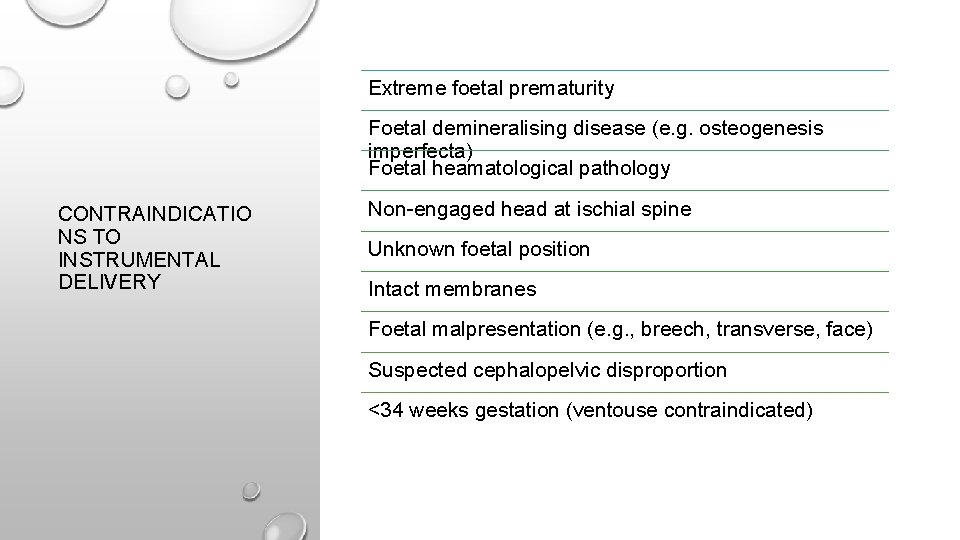
Extreme foetal prematurity Foetal demineralising disease (e. g. osteogenesis imperfecta) Foetal heamatological pathology CONTRAINDICATIO NS TO INSTRUMENTAL DELIVERY Non-engaged head at ischial spine Unknown foetal position Intact membranes Foetal malpresentation (e. g. , breech, transverse, face) Suspected cephalopelvic disproportion <34 weeks gestation (ventouse contraindicated)
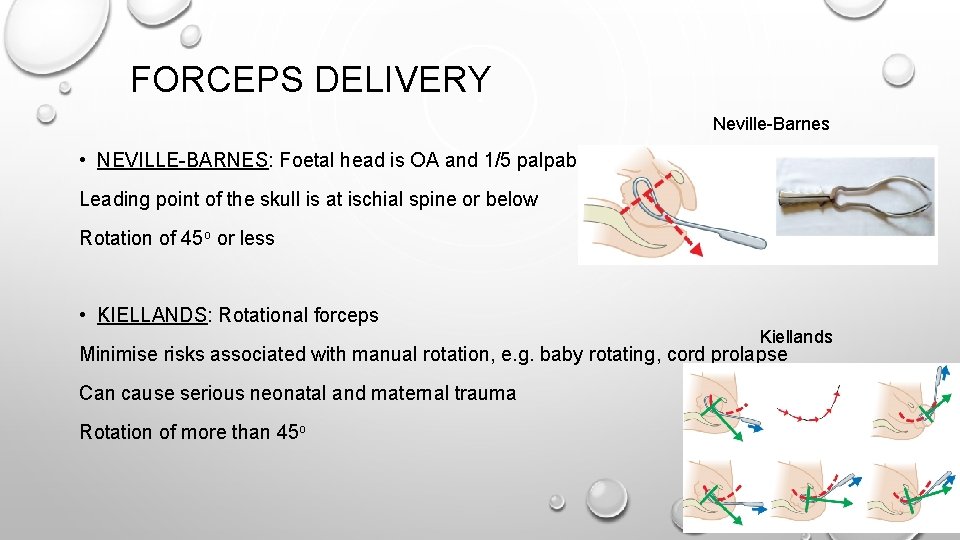
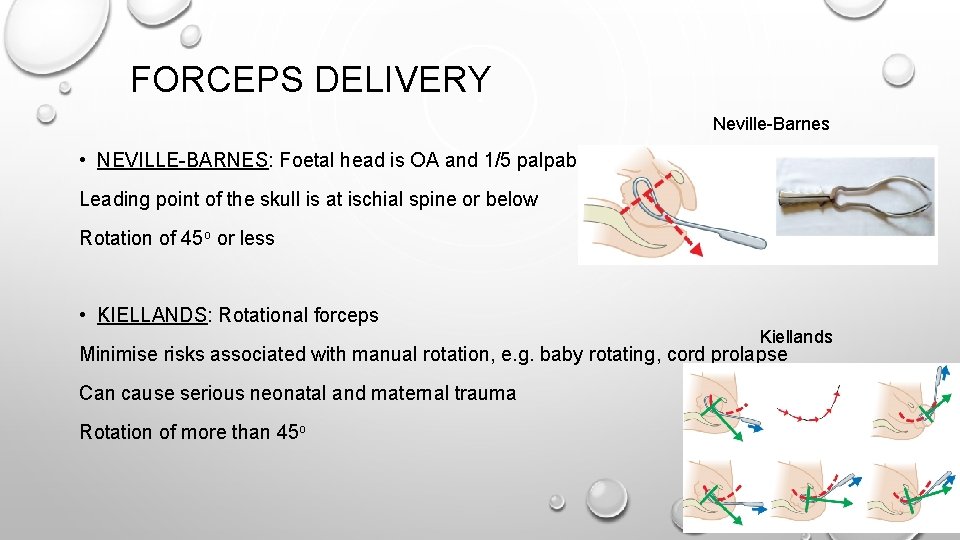
FORCEPS DELIVERY Neville-Barnes • NEVILLE-BARNES: Foetal head is OA and 1/5 palpable Leading point of the skull is at ischial spine or below Rotation of 45 o or less • KIELLANDS: Rotational forceps Kiellands Minimise risks associated with manual rotation, e. g. baby rotating, cord prolapse Can cause serious neonatal and maternal trauma Rotation of more than 45 o
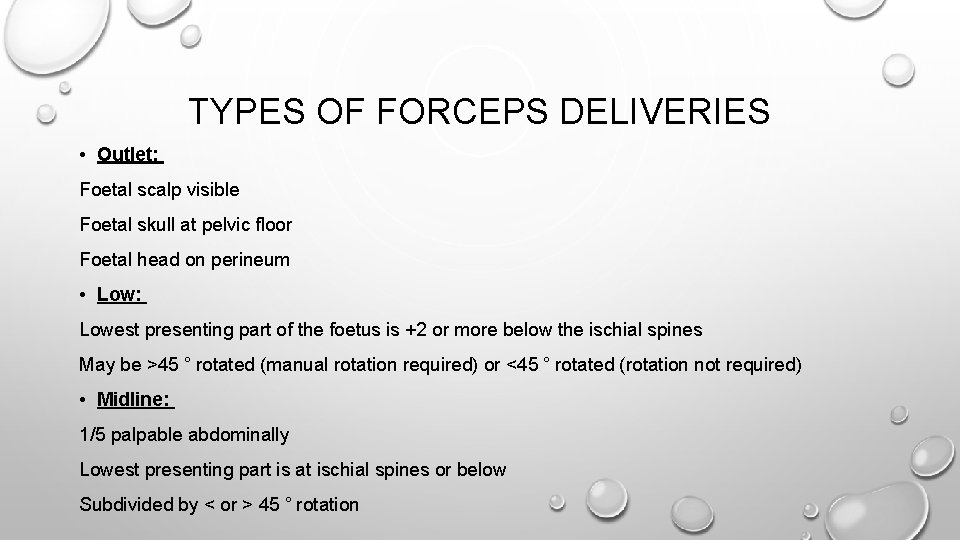
TYPES OF FORCEPS DELIVERIES • Outlet: Foetal scalp visible Foetal skull at pelvic floor Foetal head on perineum • Low: Lowest presenting part of the foetus is +2 or more below the ischial spines May be >45 ˚ rotated (manual rotation required) or <45 ˚ rotated (rotation not required) • Midline: 1/5 palpable abdominally Lowest presenting part is at ischial spines or below Subdivided by < or > 45 ˚ rotation
COMPLICATIONS OF FORCEPS Maternal complications: • Greater need for analgesia • Greater risk of tears, episiotomy or PPH than with ventouse • Injury to nearby structures Foetal complications: • Scalp laceration • Cephalo-haematoma • Neonatal jaundice • Skin markings

VENTOUSE / KIWI / VACUUM • Rubber or metal cap connected to a handle • Traction during maternal pushing: delivers the OA-positioned head • Also allows shape of pelvis to simultaneously rotate a malpositioned foetus to the OA position • Incorrect placement may result in: deflexed and asynclitic (tilted to one side) fetal head attitudes • Consequent failure of the vacuum extraction technique
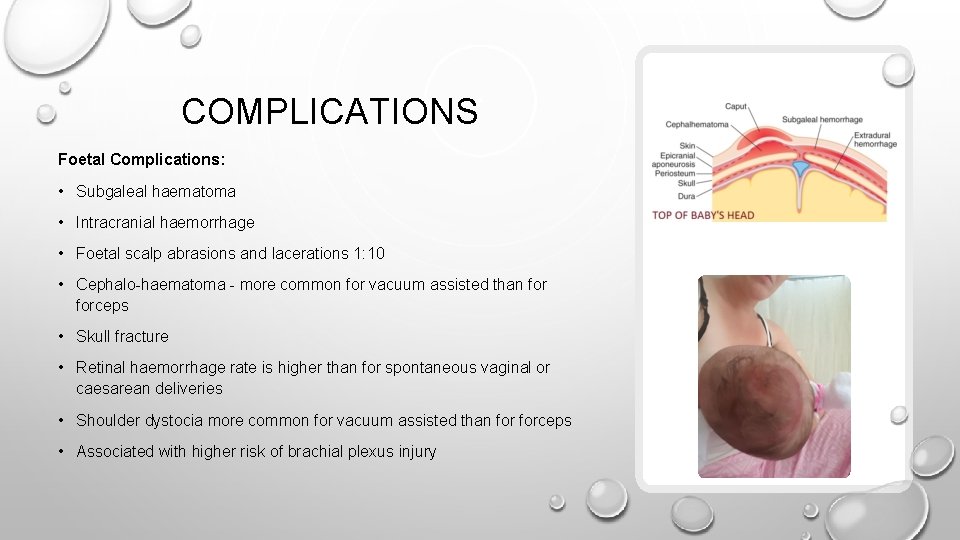
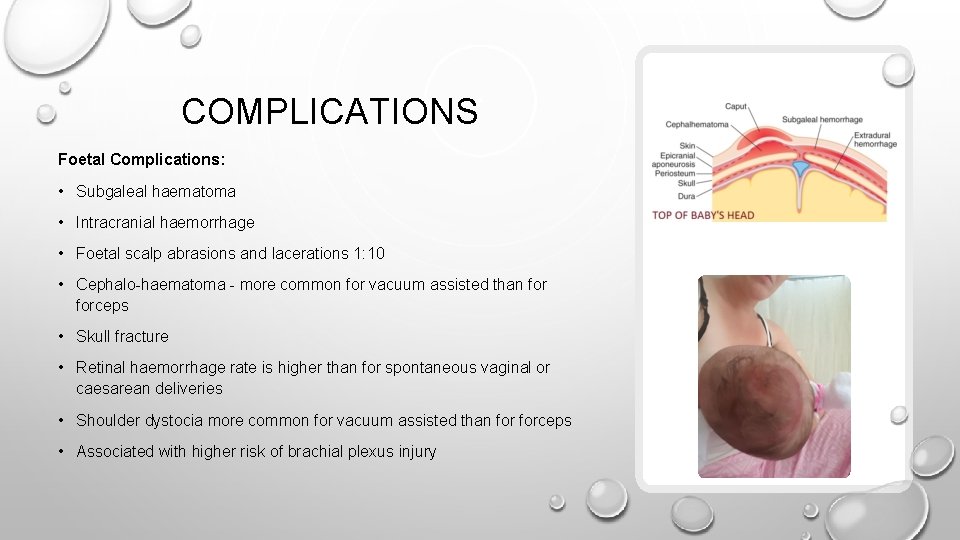
COMPLICATIONS Foetal Complications: • Subgaleal haematoma • Intracranial haemorrhage • Foetal scalp abrasions and lacerations 1: 10 • Cephalo-haematoma - more common for vacuum assisted than forceps • Skull fracture • Retinal haemorrhage rate is higher than for spontaneous vaginal or caesarean deliveries • Shoulder dystocia more common for vacuum assisted than forceps • Associated with higher risk of brachial plexus injury
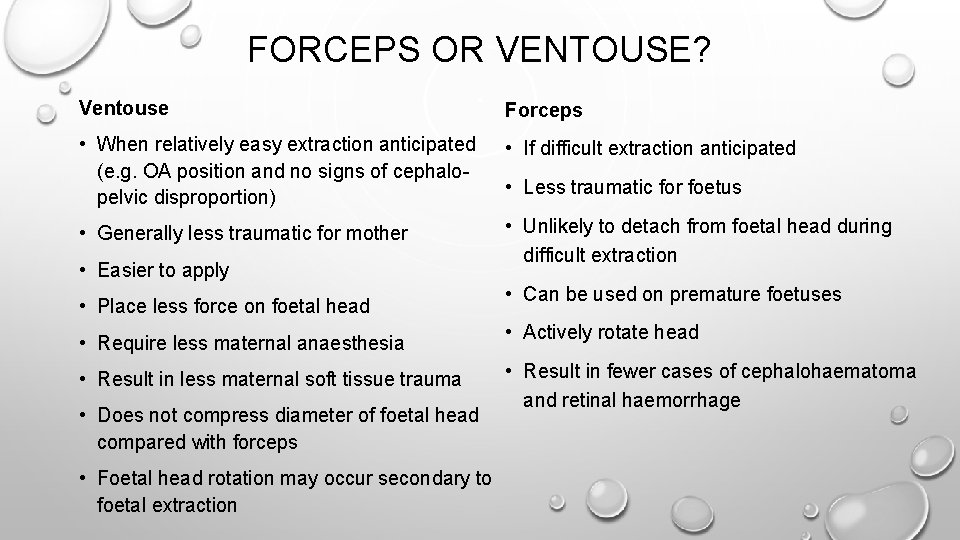
FORCEPS OR VENTOUSE? Ventouse Forceps • When relatively easy extraction anticipated (e. g. OA position and no signs of cephalopelvic disproportion) • If difficult extraction anticipated • Generally less traumatic for mother • Unlikely to detach from foetal head during difficult extraction • Easier to apply • Place less force on foetal head • Less traumatic for foetus • Can be used on premature foetuses • Require less maternal anaesthesia • Actively rotate head • Result in less maternal soft tissue trauma • Result in fewer cases of cephalohaematoma and retinal haemorrhage • Does not compress diameter of foetal head compared with forceps • Foetal head rotation may occur secondary to foetal extraction
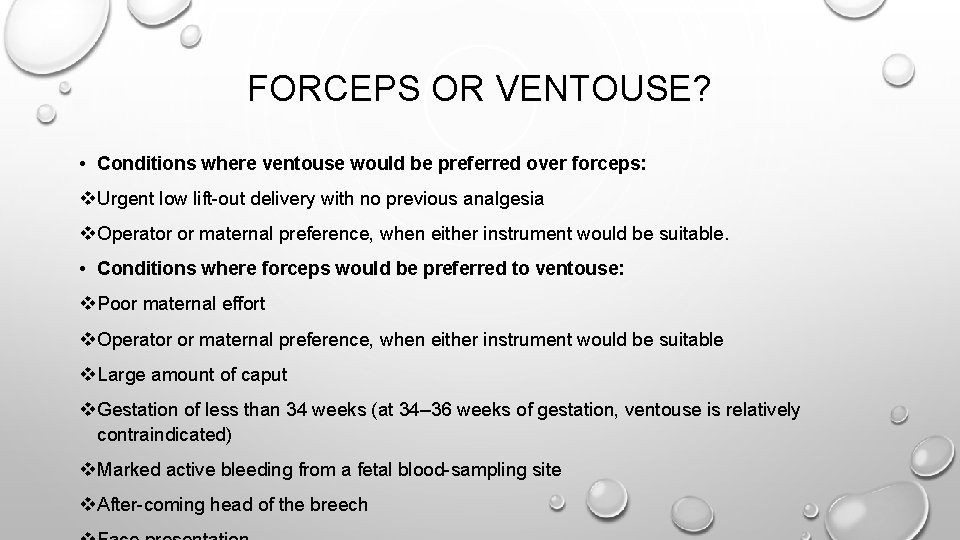
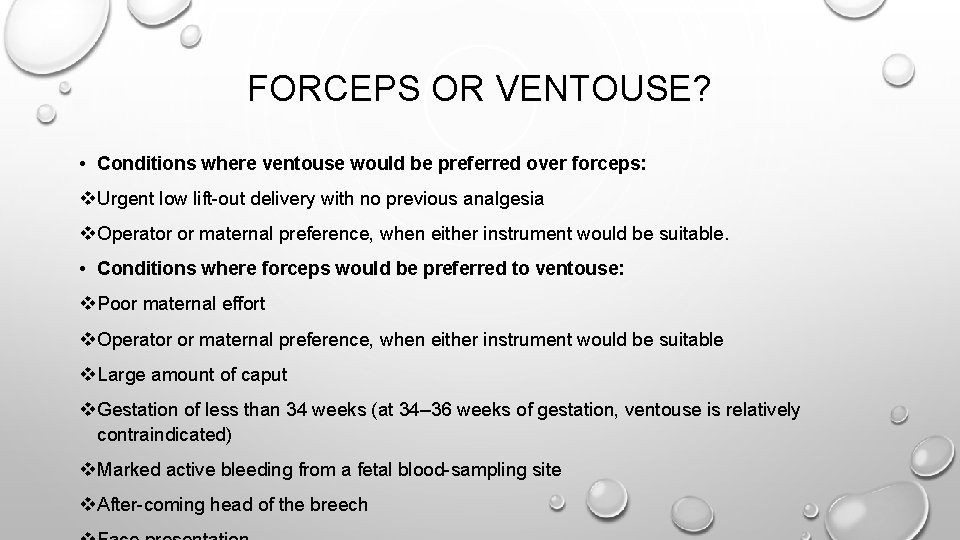
FORCEPS OR VENTOUSE? • Conditions where ventouse would be preferred over forceps: v Urgent low lift-out delivery with no previous analgesia v Operator or maternal preference, when either instrument would be suitable. • Conditions where forceps would be preferred to ventouse: v Poor maternal effort v Operator or maternal preference, when either instrument would be suitable v Large amount of caput v Gestation of less than 34 weeks (at 34– 36 weeks of gestation, ventouse is relatively contraindicated) v Marked active bleeding from a fetal blood-sampling site v After-coming head of the breech
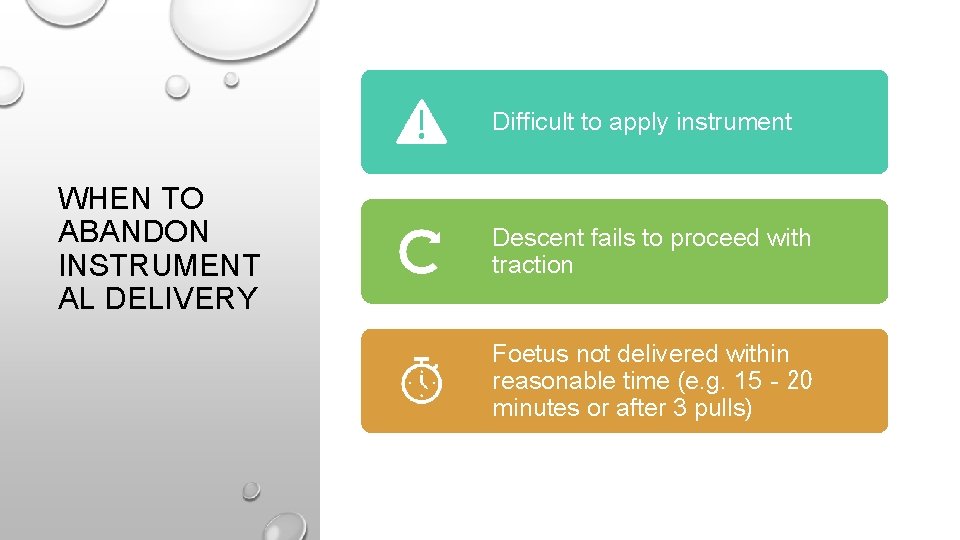
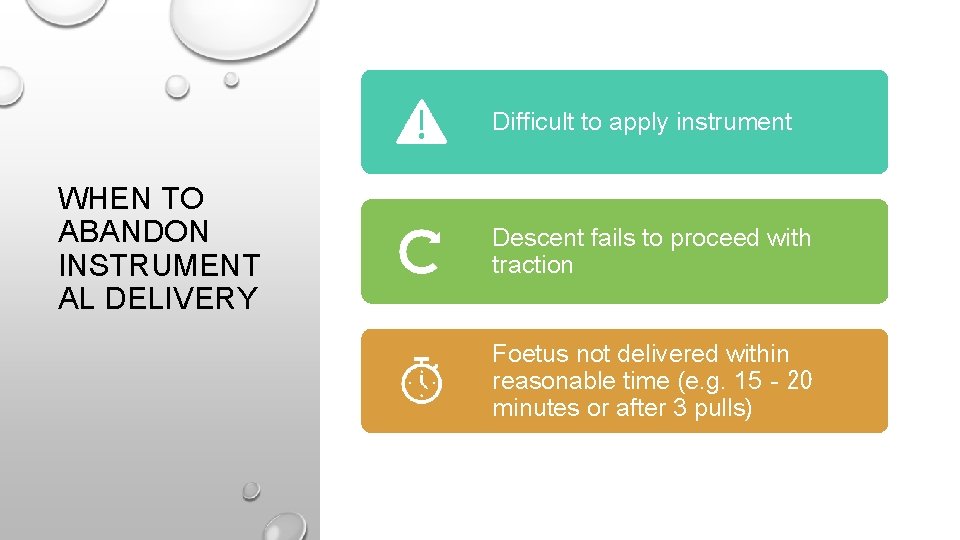
Difficult to apply instrument WHEN TO ABANDON INSTRUMENT AL DELIVERY Descent fails to proceed with traction Foetus not delivered within reasonable time (e. g. 15‐ 20 minutes or after 3 pulls)
CAESAREAN SECTION • Approx 1 in 4 women will have a caesarean section • Must be discussed during antenatal care as both an elective and emergency option, wherein the risks, benefits and possible complications are explained
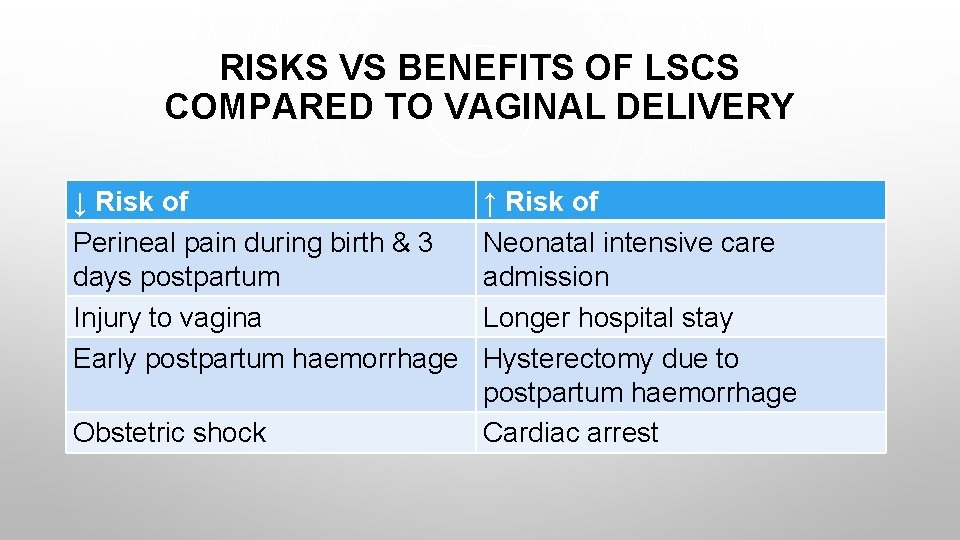
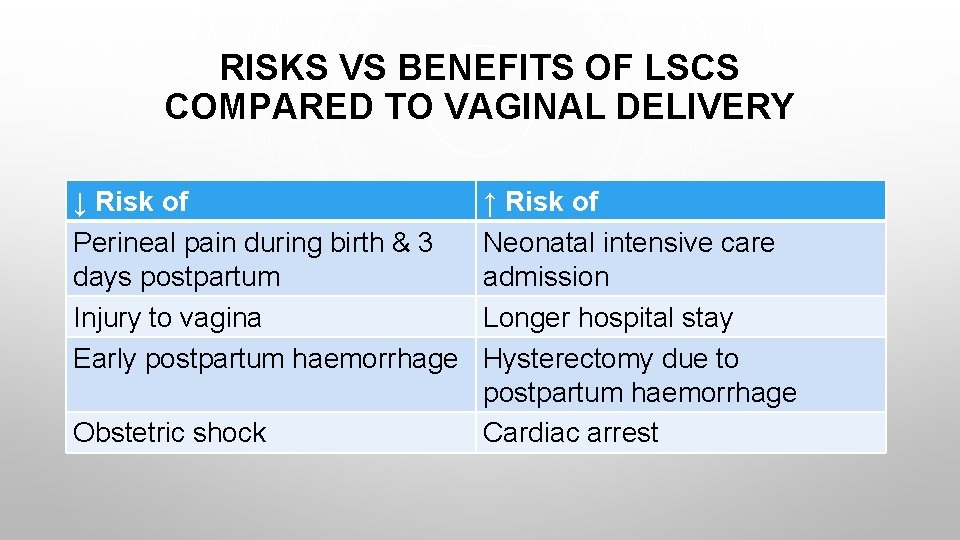
RISKS VS BENEFITS OF LSCS COMPARED TO VAGINAL DELIVERY ↓ Risk of Perineal pain during birth & 3 days postpartum Injury to vagina Early postpartum haemorrhage Obstetric shock ↑ Risk of Neonatal intensive care admission Longer hospital stay Hysterectomy due to postpartum haemorrhage Cardiac arrest
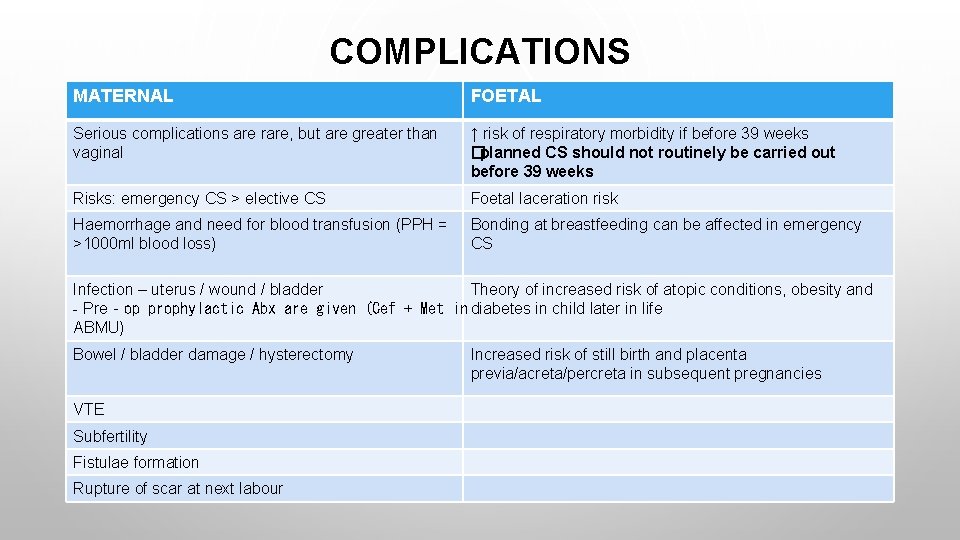
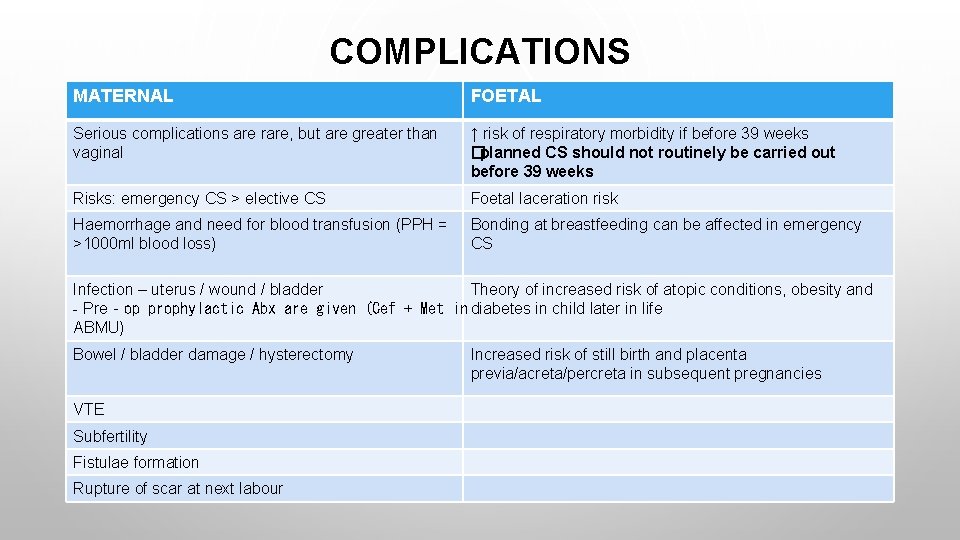
COMPLICATIONS MATERNAL FOETAL Serious complications are rare, but are greater than vaginal ↑ risk of respiratory morbidity if before 39 weeks �planned CS should not routinely be carried out before 39 weeks Risks: emergency CS > elective CS Foetal laceration risk Haemorrhage and need for blood transfusion (PPH = >1000 ml blood loss) Bonding at breastfeeding can be affected in emergency CS Infection – uterus / wound / bladder Theory of increased risk of atopic conditions, obesity and - Pre‐op prophylactic Abx are given (Cef + Met in diabetes in child later in life ABMU) Bowel / bladder damage / hysterectomy VTE Subfertility Fistulae formation Rupture of scar at next labour Increased risk of still birth and placenta previa/acreta/percreta in subsequent pregnancies
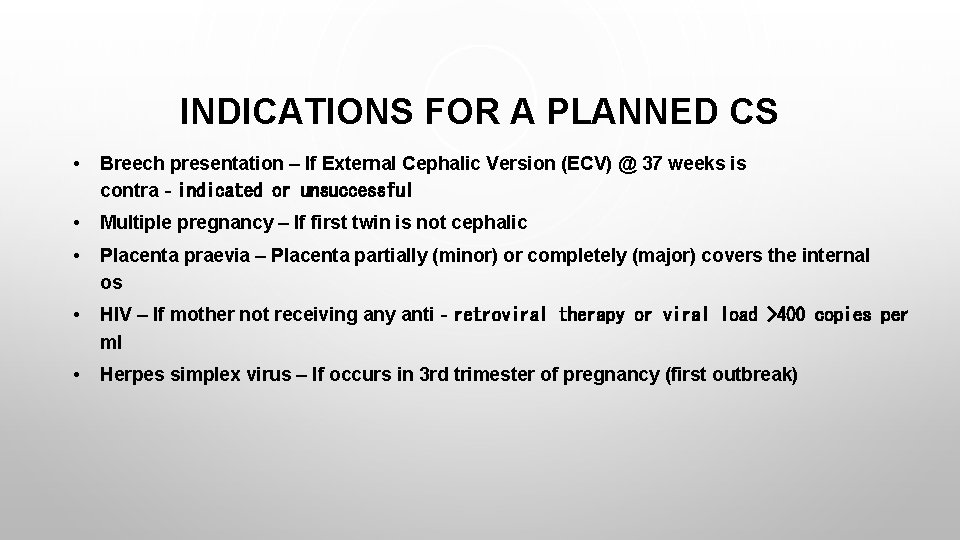
INDICATIONS FOR A PLANNED CS • Breech presentation – If External Cephalic Version (ECV) @ 37 weeks is contra‐indicated or unsuccessful • Multiple pregnancy – If first twin is not cephalic • Placenta praevia – Placenta partially (minor) or completely (major) covers the internal os • HIV – If mother not receiving any anti‐retroviral therapy or viral load >400 copies per ml • Herpes simplex virus – If occurs in 3 rd trimester of pregnancy (first outbreak)

INDICATIONS FOR AN UNPLANNED CS • Foetal compromise • Failure to progress • Breech presentation • Failed instrumental delivery
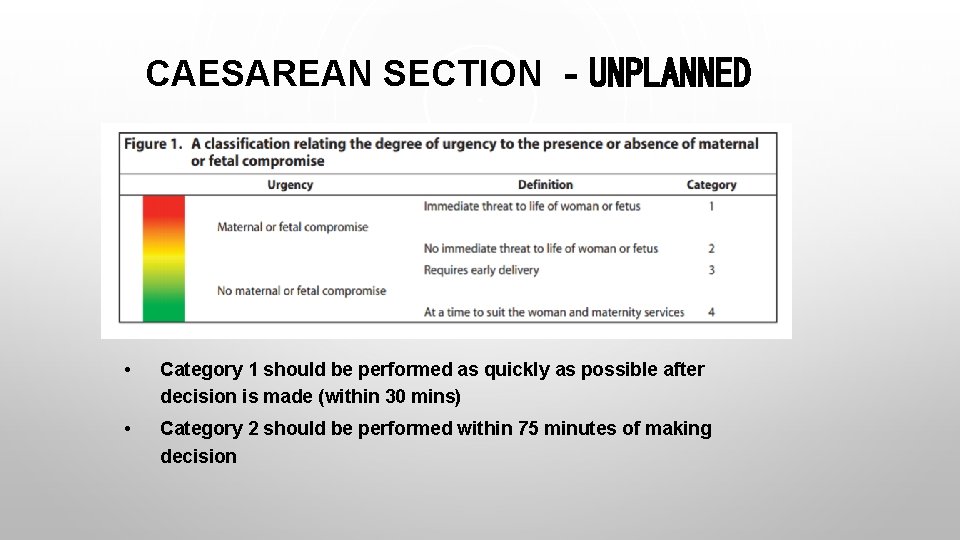
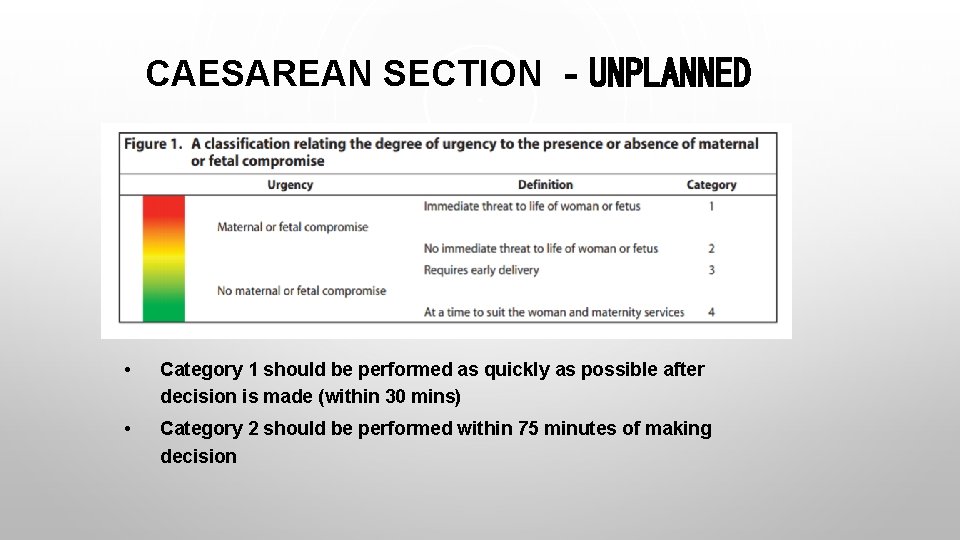
CAESAREAN SECTION ‐UNPLANNED • Category 1 should be performed as quickly as possible after decision is made (within 30 mins) • Category 2 should be performed within 75 minutes of making decision
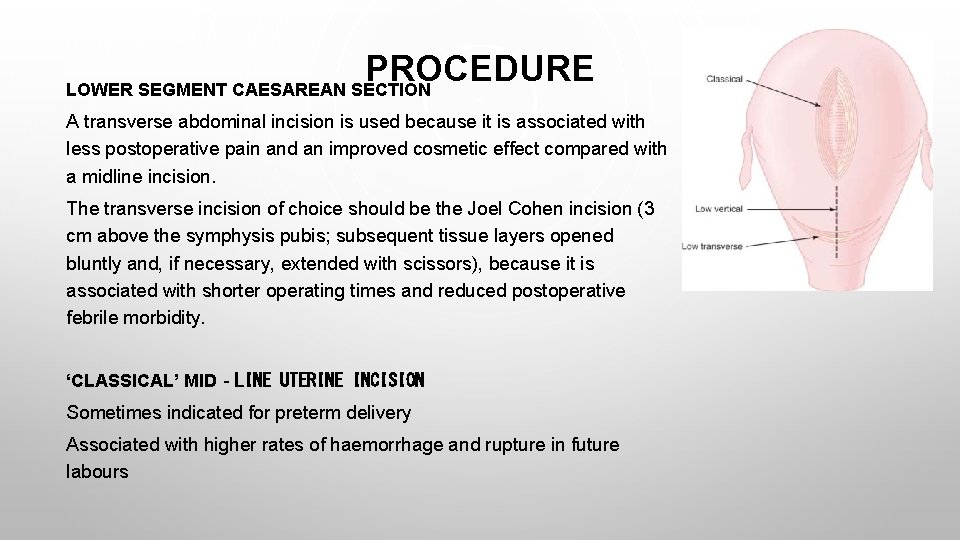
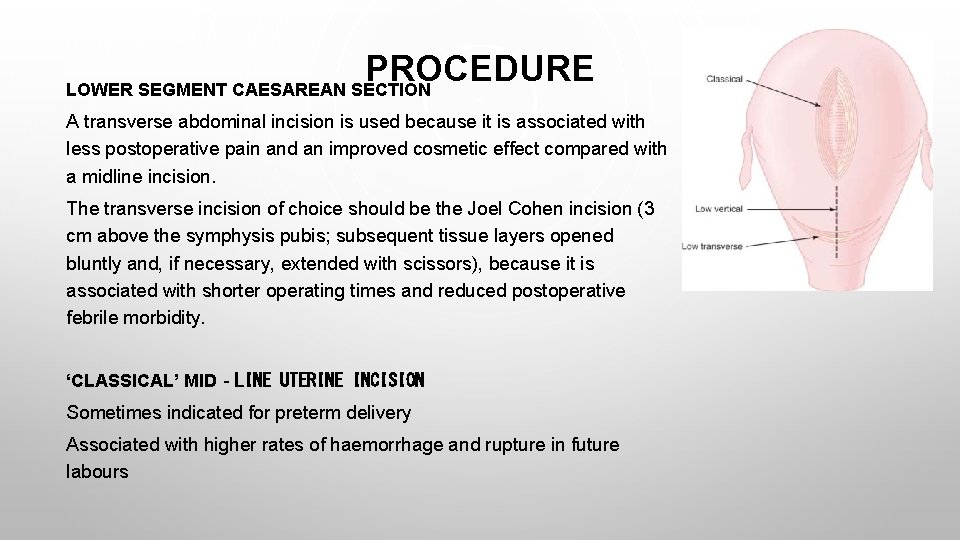
PROCEDURE LOWER SEGMENT CAESAREAN SECTION A transverse abdominal incision is used because it is associated with less postoperative pain and an improved cosmetic effect compared with a midline incision. The transverse incision of choice should be the Joel Cohen incision (3 cm above the symphysis pubis; subsequent tissue layers opened bluntly and, if necessary, extended with scissors), because it is associated with shorter operating times and reduced postoperative febrile morbidity. ‘CLASSICAL’ MID‐LINE UTERINE INCISION Sometimes indicated for preterm delivery Associated with higher rates of haemorrhage and rupture in future labours
PROCEDURE – EXTRA CONSIDERATIONS • Regional (vs general) anaesthesia is preferred as it is safer for mother and neonate • Antiemetics • Operating table should have a lateral tilt to reduce maternal hypotension & avoid inferior vena cava syndrome • Oxytocin IV to ↑ uterine contraction & ↓ blood loss • The placenta should be removed using controlled cord traction and not manual removal as this ↓ endometritis risk • Prophylactic antibiotics • Thromboprophylaxis
FUTURE PREGNANCIES • For those who have had ≥ 4 sections there is an ↑ risk of fever, bladder injury and surgical injuries that does not vary with planned delivery method • Risk of uterine rupture is rare (although higher for planned vaginal birth) • During induction of labour, women who have had a previous section should be monitored closely with electronic foetal monitoring ** WITH APPROPRIATE MONITORING, CAN EXPECT VAGINAL DELIVERY RATES OF APPROXIMATELY 70% (WITH SCAR RUPTURE RATE OF <1%)**
REFERENCES 1. OPERATIVE VAGINAL DELIVERY (RCOG GREEN-TOP GUIDELINE NO. 26). JANUARY 2017. 2. HTTPS: //STRATOG. RCOG. ORG. UK/OBSTETRICS/INSTRUMENTAL-DELIVERY
 Lower segment caesarean section ppt
Lower segment caesarean section ppt Criteria for normal vaginal delivery
Criteria for normal vaginal delivery Contraindications for vaginal delivery
Contraindications for vaginal delivery Definition of instrumental delivery
Definition of instrumental delivery Scalp mnemonic
Scalp mnemonic What is the website to access accenture delivery suits
What is the website to access accenture delivery suits Text types examples
Text types examples Classification of wedges in dentistry
Classification of wedges in dentistry Katharina reiss text types
Katharina reiss text types Co operative relationship between investor and entrepreneur
Co operative relationship between investor and entrepreneur Nursing diagnosis for vision impairment
Nursing diagnosis for vision impairment Pre- post- peri-
Pre- post- peri- Hernia nursing care plan
Hernia nursing care plan Vaginal process
Vaginal process Canal peritoneo inguinal
Canal peritoneo inguinal Depo-provera
Depo-provera Haivn
Haivn Processus vaginalis anatomy
Processus vaginalis anatomy Discharge from penis
Discharge from penis Silk glove sign
Silk glove sign Site:slidetodoc.com
Site:slidetodoc.com Ectocervix
Ectocervix Vagincal
Vagincal Vaginal discharge
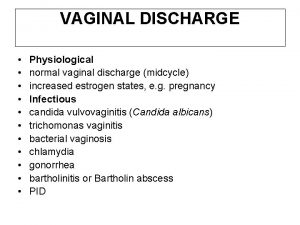
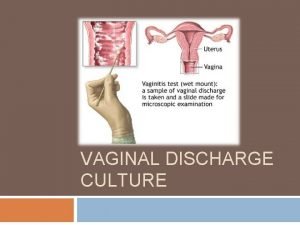
Vaginal discharge Vaginal length
Vaginal length Hernia reductible coercible
Hernia reductible coercible