HYPERTENSION pharmacological treatment Etiopathogenesis of essential hypertension EH
















- Slides: 91

HYPERTENSION pharmacological treatment
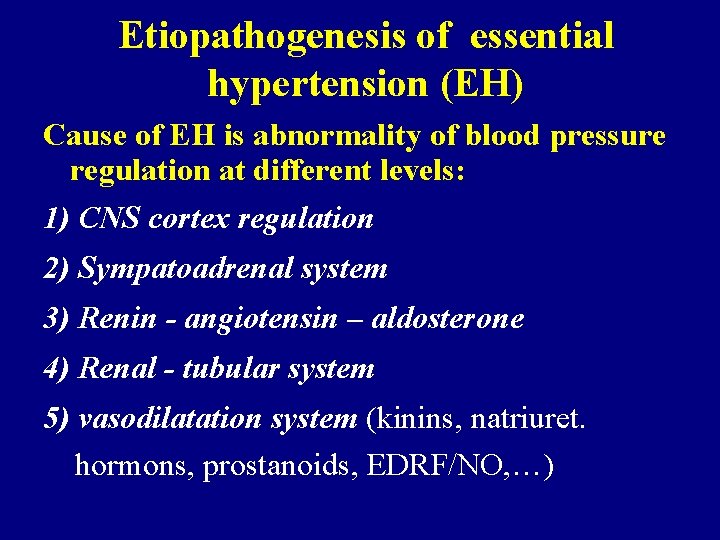
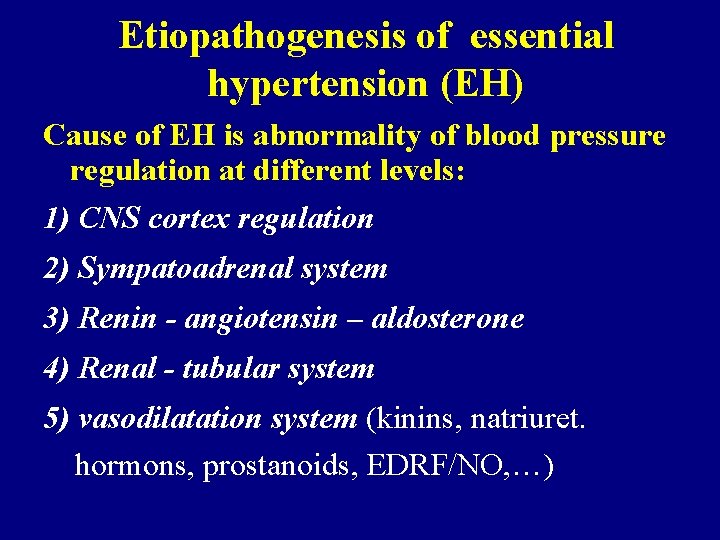
Etiopathogenesis of essential hypertension (EH) Cause of EH is abnormality of blood pressure regulation at different levels: 1) CNS cortex regulation 2) Sympatoadrenal system 3) Renin - angiotensin – aldosterone 4) Renal - tubular system 5) vasodilatation system (kinins, natriuret. hormons, prostanoids, EDRF/NO, …)
Important and probably decisive bases for regulatory systems abnormalities are their genetic polymorphism
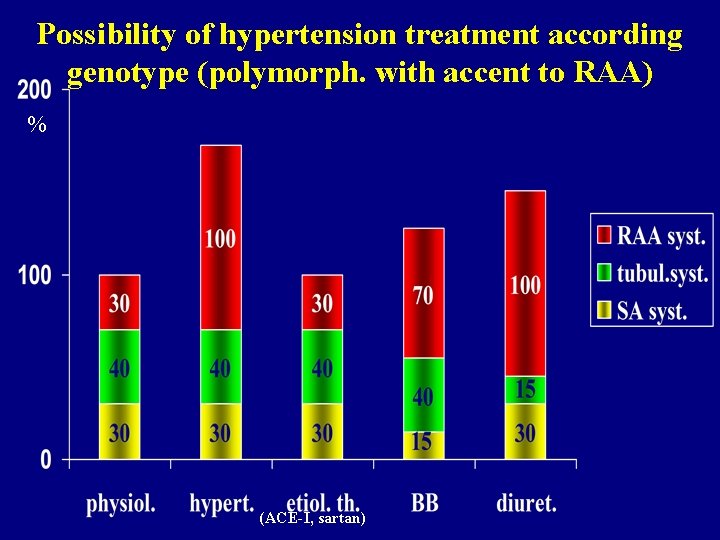
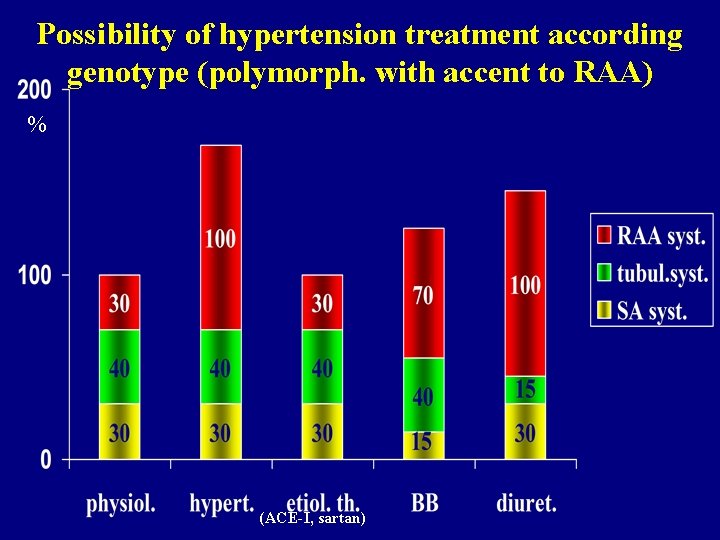
Possibility of hypertension treatment according genotype (polymorph. with accent to RAA) % (ACE-I, sartan)
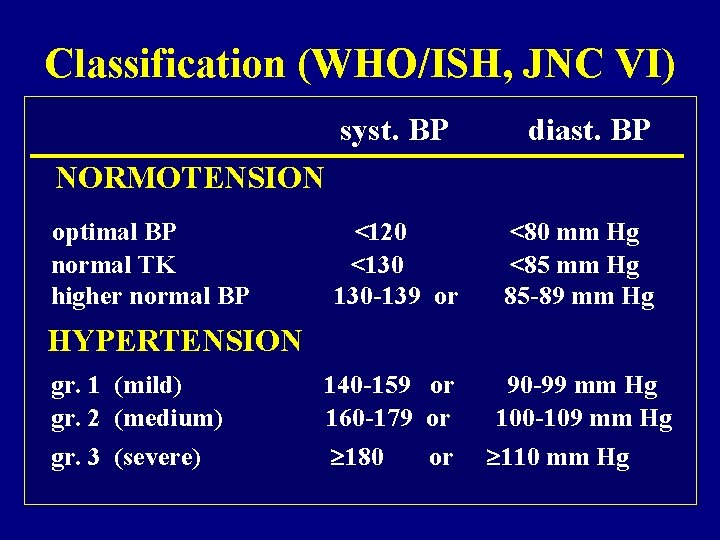
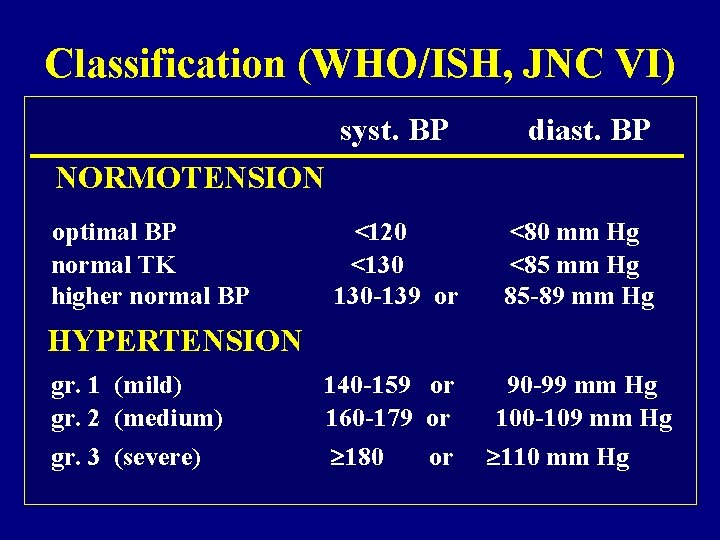
Classification (WHO/ISH, JNC VI) syst. BP diast. BP NORMOTENSION optimal BP normal TK higher normal BP <120 <130 130 -139 or <80 mm Hg <85 mm Hg 85 -89 mm Hg 140 -159 or 160 -179 or 180 or 90 -99 mm Hg 100 -109 mm Hg 110 mm Hg HYPERTENSION gr. 1 (mild) gr. 2 (medium) gr. 3 (severe)
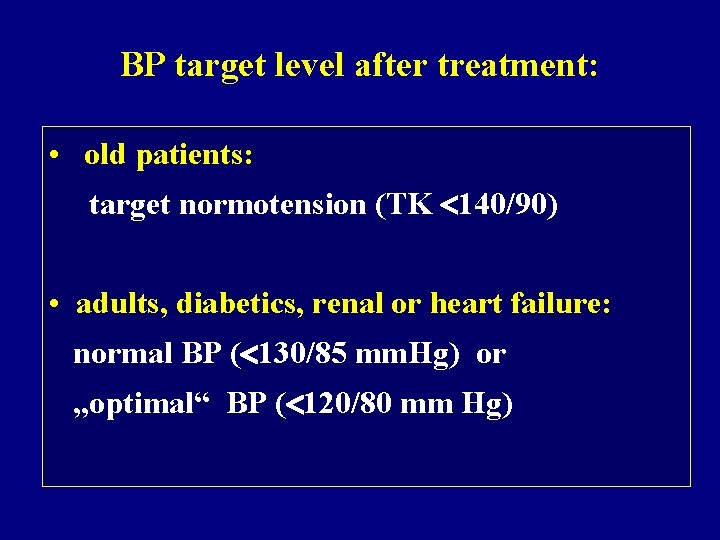
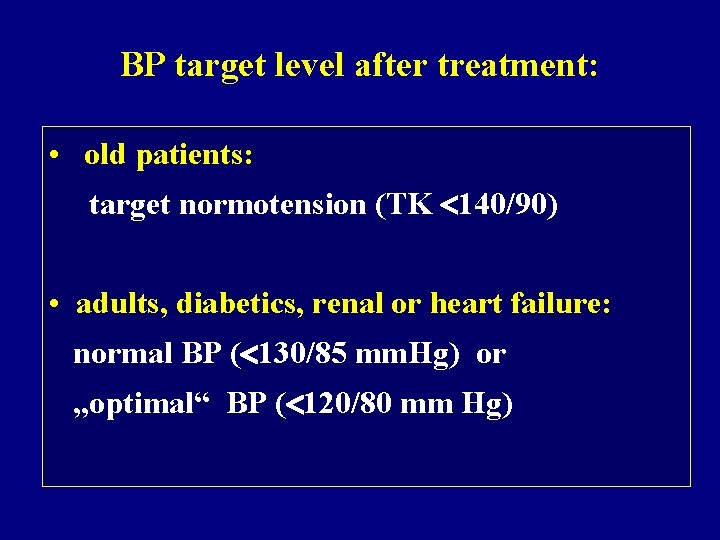
BP target level after treatment: • old patients: target normotension (TK 140/90) • adults, diabetics, renal or heart failure: normal BP ( 130/85 mm. Hg) or „optimal“ BP ( 120/80 mm Hg)
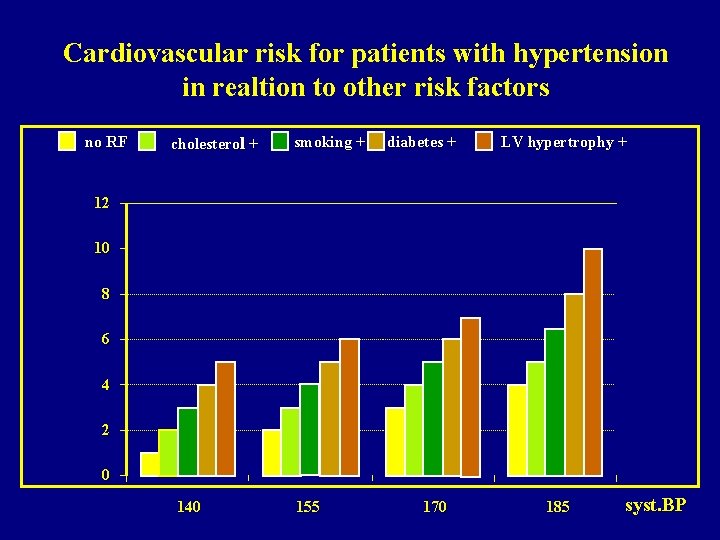
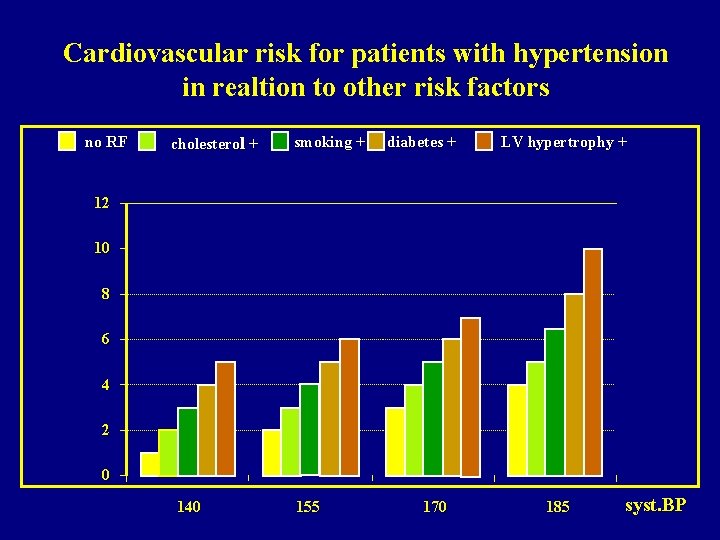
Cardiovascular risk for patients with hypertension in realtion to other risk factors no RF cholesterol + smoking + diabetes + LV hypertrophy + 12 10 8 6 4 2 0 140 155 170 185 syst. BP
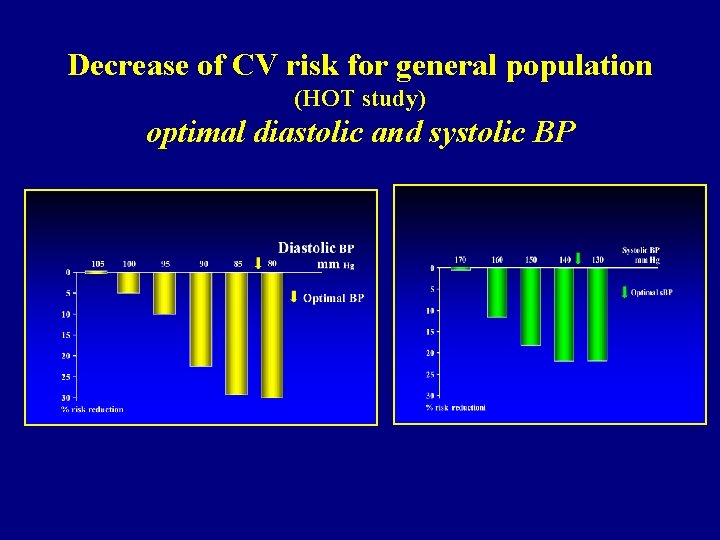
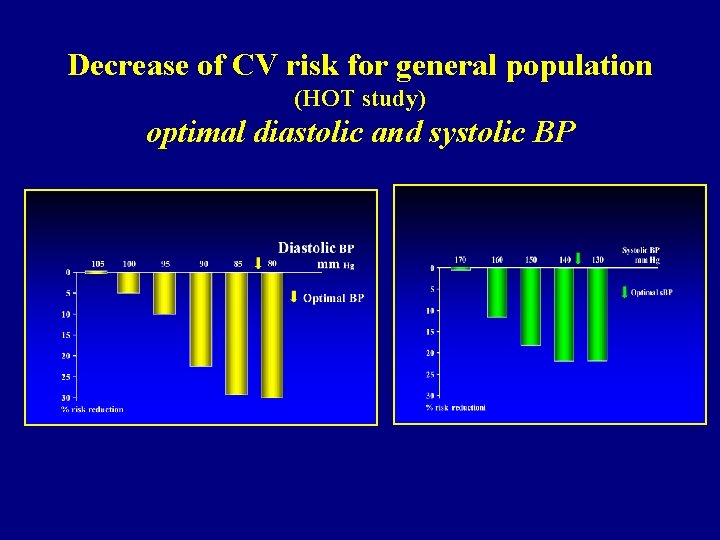
Decrease of CV risk for general population (HOT study) optimal diastolic and systolic BP
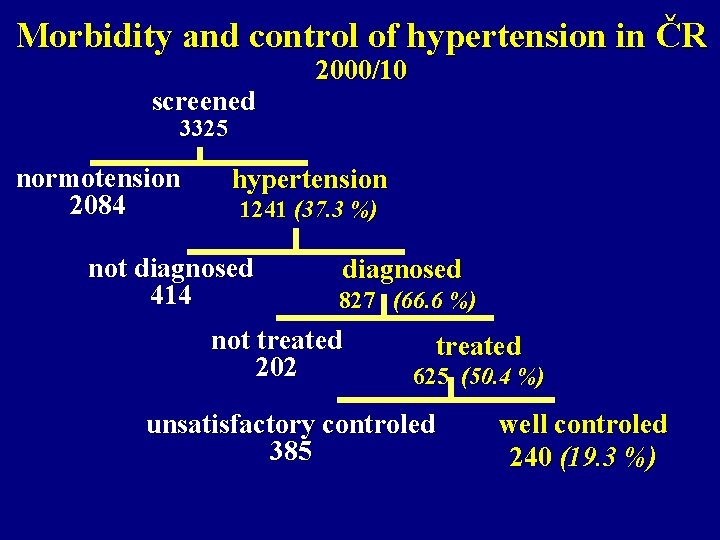
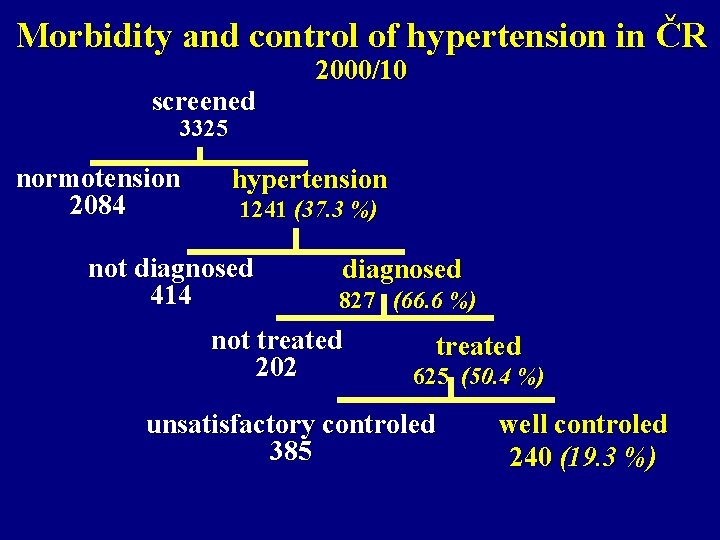
Morbidity and control of hypertension in ČR screened 2000/10 3325 normotension 2084 hypertension 1241 (37. 3 %) not diagnosed 414 diagnosed 827 (66. 6 %) not treated 202 treated 625 (50. 4 %) unsatisfactory controled 385 well controled 240 (19. 3 %)
Hypertension is badly controled all over the world (also in Czech Republic) More tough criteria for controle hypertension Necessary to increase detection and treatment! Combination therapy offers better control
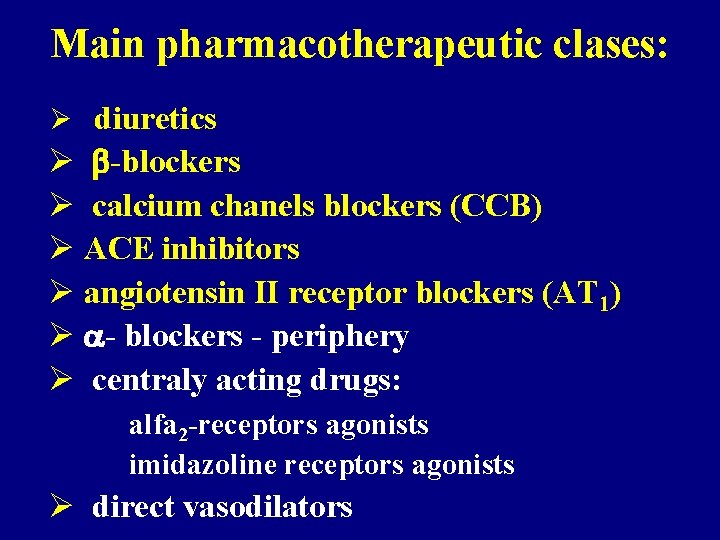
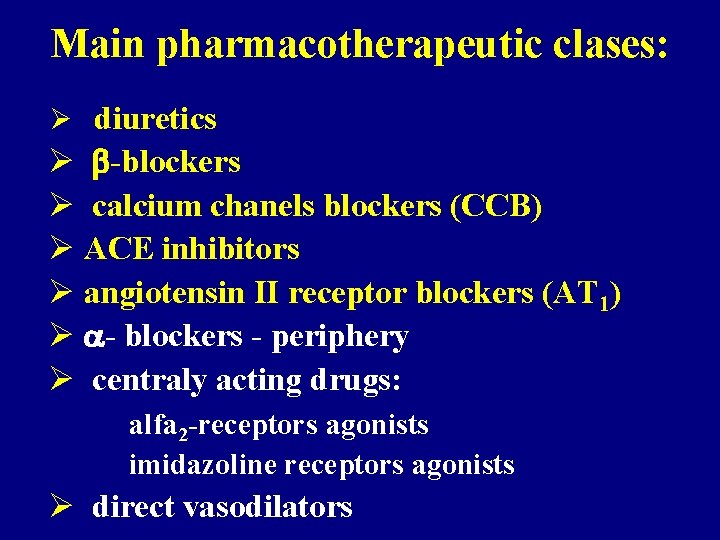
Main pharmacotherapeutic clases: Ø diuretics Ø -blockers Ø calcium chanels blockers (CCB) Ø ACE inhibitors Ø angiotensin II receptor blockers (AT 1) Ø - blockers - periphery Ø centraly acting drugs: alfa 2 -receptors agonists imidazoline receptors agonists Ø direct vasodilators
DIURETICS FOR TREATMENT HYPERTENSION
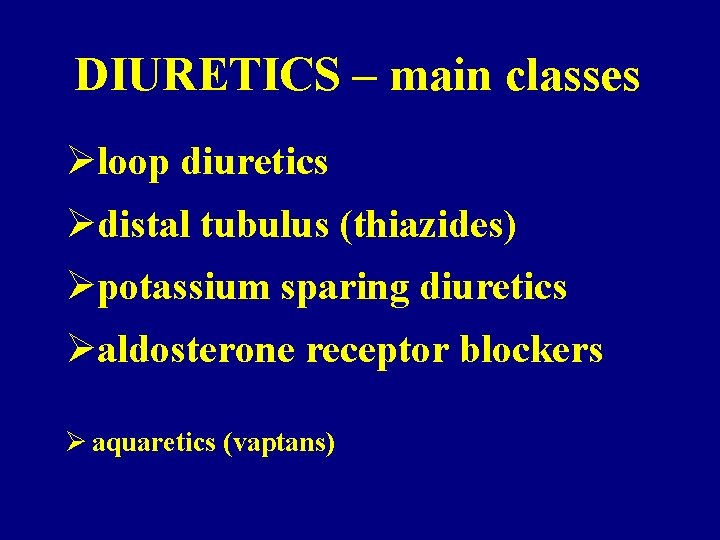
DIURETICS – main classes Øloop diuretics Ødistal tubulus (thiazides) Øpotassium sparing diuretics Øaldosterone receptor blockers Ø aquaretics (vaptans)
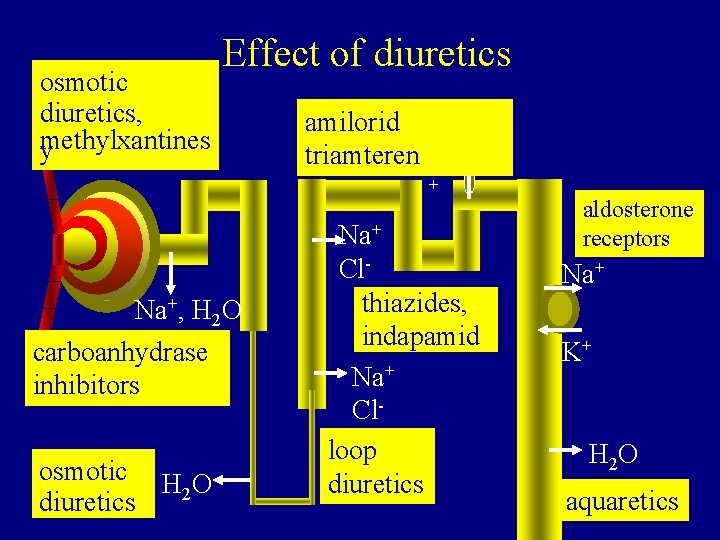
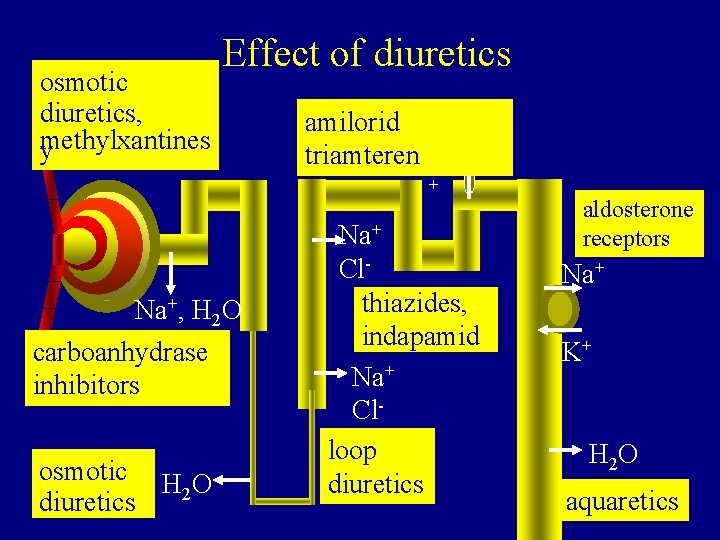
osmotic diuretics, methylxantines y Effect of diuretics amilorid triamteren Na + Na+, H 2 O carboanhydrase inhibitors osmotic H O 2 diuretics Na+ Clthiazides, indapamid Na+ Clloop diuretics aldosterone receptors Na+ K+ H 2 O aquaretics
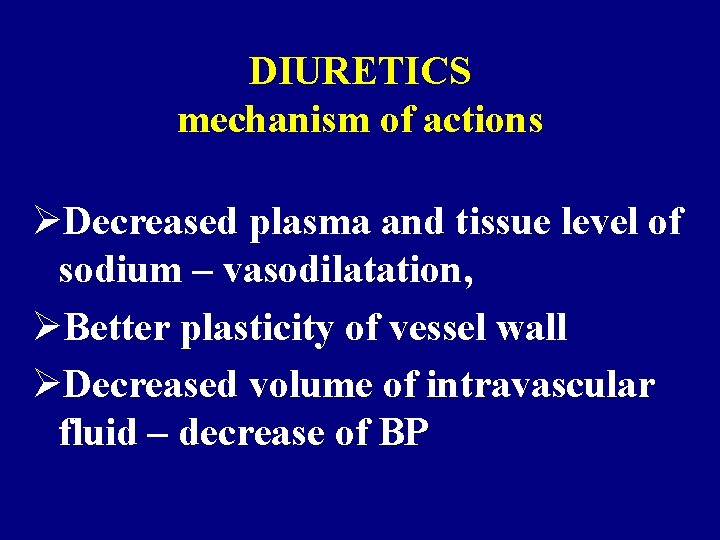
DIURETICS mechanism of actions ØDecreased plasma and tissue level of sodium – vasodilatation, ØBetter plasticity of vessel wall ØDecreased volume of intravascular fluid – decrease of BP
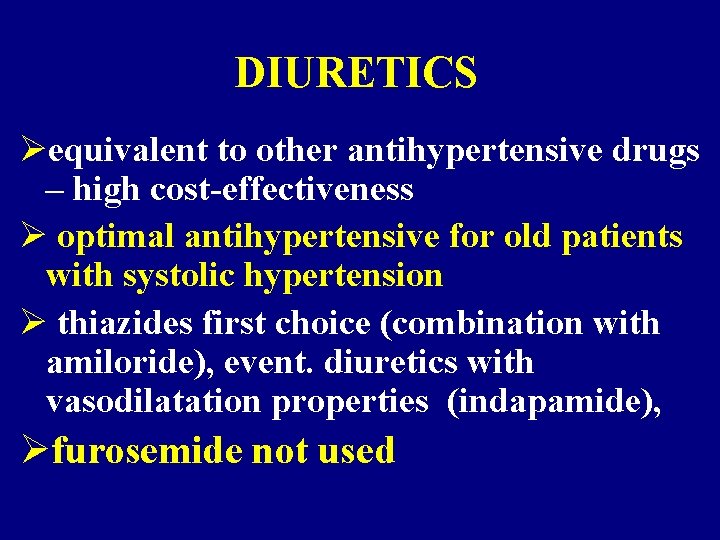
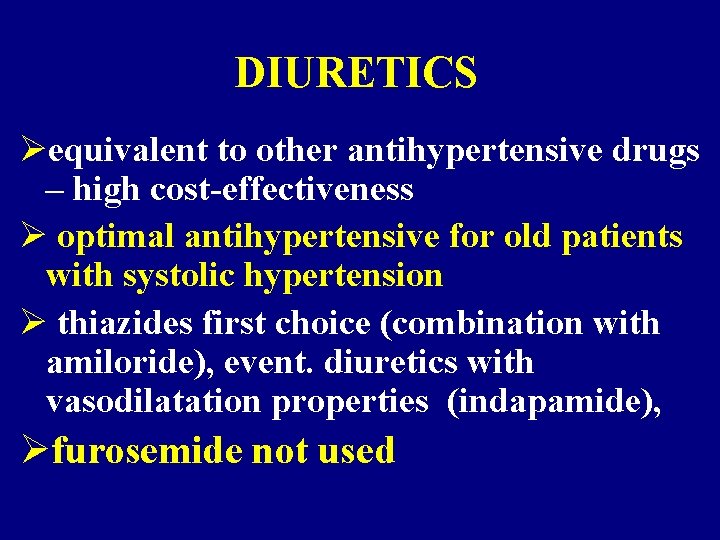
DIURETICS Øequivalent to other antihypertensive drugs – high cost-effectiveness Ø optimal antihypertensive for old patients with systolic hypertension Ø thiazides first choice (combination with amiloride), event. diuretics with vasodilatation properties (indapamide), Øfurosemide not used
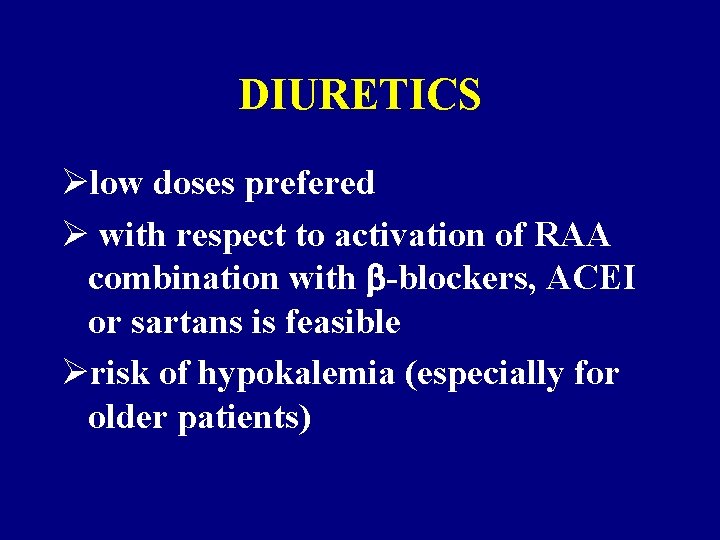
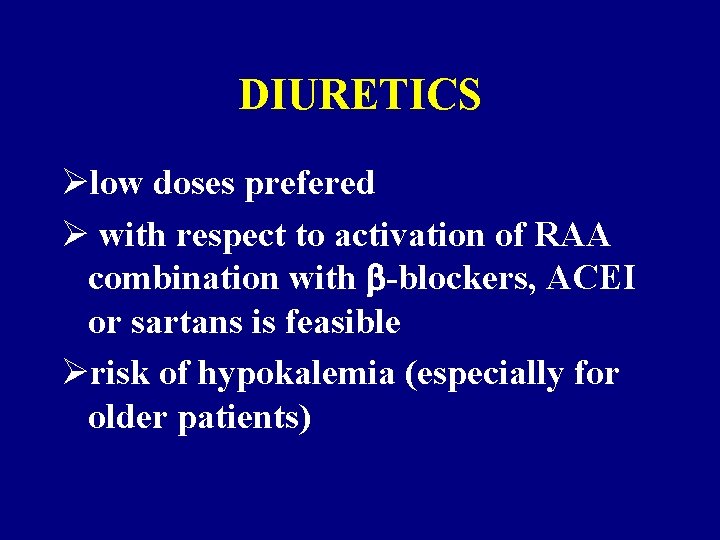
DIURETICS Ølow doses prefered Ø with respect to activation of RAA combination with -blockers, ACEI or sartans is feasible Ørisk of hypokalemia (especially for older patients)
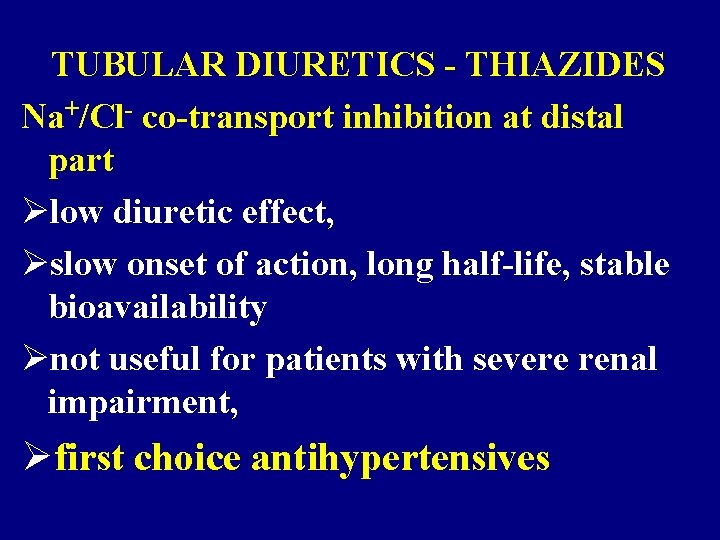
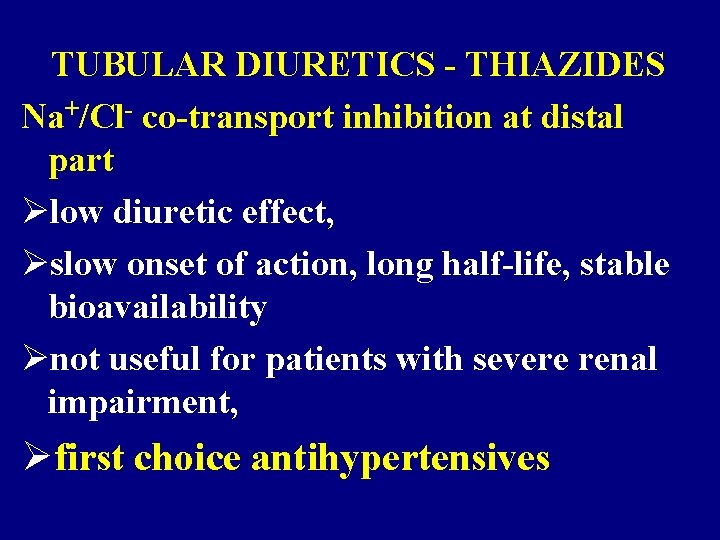
TUBULAR DIURETICS - THIAZIDES Na+/Cl- co-transport inhibition at distal part Ølow diuretic effect, Øslow onset of action, long half-life, stable bioavailability Ønot useful for patients with severe renal impairment, Øfirst choice antihypertensives
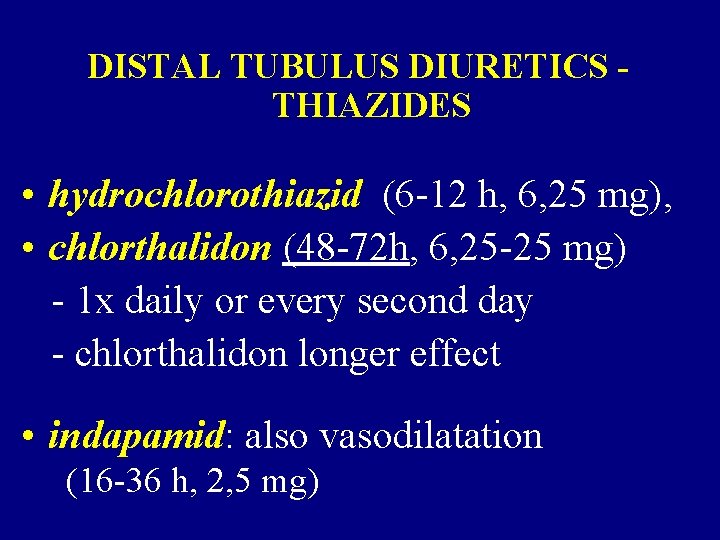
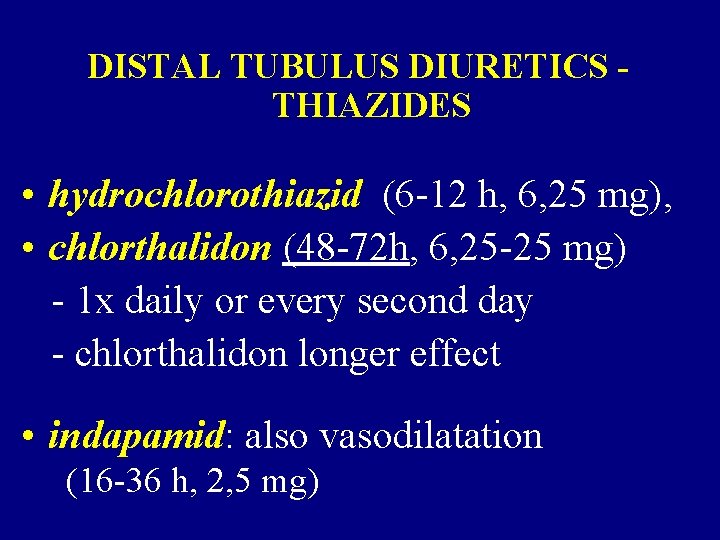
DISTAL TUBULUS DIURETICS THIAZIDES • hydrochlorothiazid (6 -12 h, 6, 25 mg), • chlorthalidon (48 -72 h, 6, 25 -25 mg) - 1 x daily or every second day - chlorthalidon longer effect • indapamid: also vasodilatation (16 -36 h, 2, 5 mg)
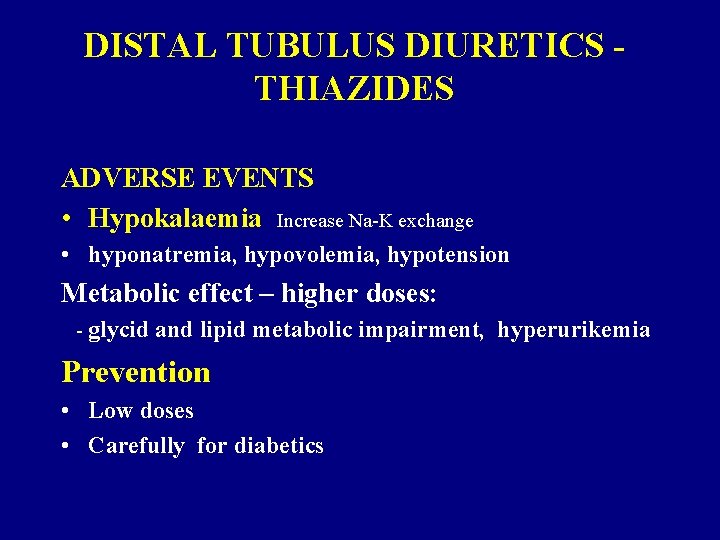
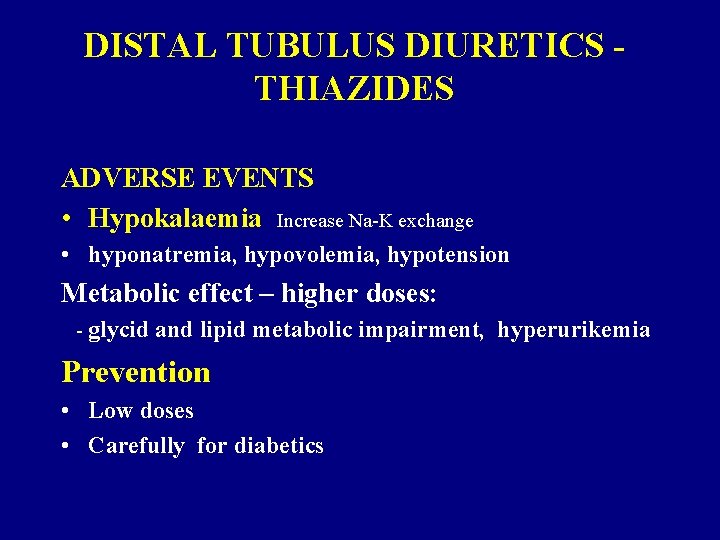
DISTAL TUBULUS DIURETICS THIAZIDES ADVERSE EVENTS • Hypokalaemia Increase Na-K exchange • hyponatremia, hypovolemia, hypotension Metabolic effect – higher doses: - glycid and lipid metabolic impairment, hyperurikemia Prevention • Low doses • Carefully for diabetics

KALIUM SPARING DIURETICS Ø Na+ chanel inhibition – distal part Ø amiloride: small diuretic effect, slow onset of action, long half-live (days), suitable for combination with other diuretics, also for IHD Ø triamteren: less favourable, short diuretic effect Ø combination with loop diuretics has better patients prognosis Ø Side effects: hyperkalemia
Diuretics should be a part of any combination therapy of hypertension, they are safe, effective and cheap
PHARMACOLOGY of ß-BLOCKERS AND CLINICAL USE

a -adrenergic stimulation effect 1 smooth muscle (vasc. , GU) liver heart 2 pankreas ( -bb. ) smooth muscle (vasc. ) contraction glykogenolysis contractility insulin secretion contraction 1 myocard HR + conduct. , contractility juxtaglom. aparatus renin 2 smooth muscle (vasc. , bronch. , GU) relaxation liver glyconeogenesis, glycogenolysis 3 fat tissue lipolysis
-BLOCKERS - mechanism of action Ø heart rate and output Øeffect in CNS Ø renin release Ømyocardial stabilization ( fibril. treshhold) Ø apoptosis (remodeling) Ø response to stress
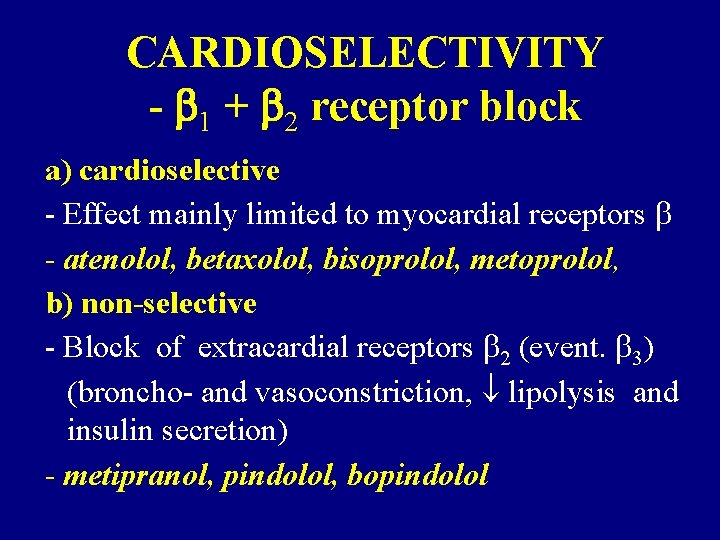
CARDIOSELECTIVITY - 1 + 2 receptor block a) cardioselective - Effect mainly limited to myocardial receptors - atenolol, betaxolol, bisoprolol, metoprolol, b) non-selective - Block of extracardial receptors 2 (event. 3) (broncho- and vasoconstriction, lipolysis and insulin secretion) - metipranol, pindolol, bopindolol

The impact of CARDIOSELECTIVITY Ø higher impact on mortality + morbidity secondary prevention in HF treatment Ø incidence of adverse metabolic events Ø better tolerance (vaso-, bronchoconstriction)
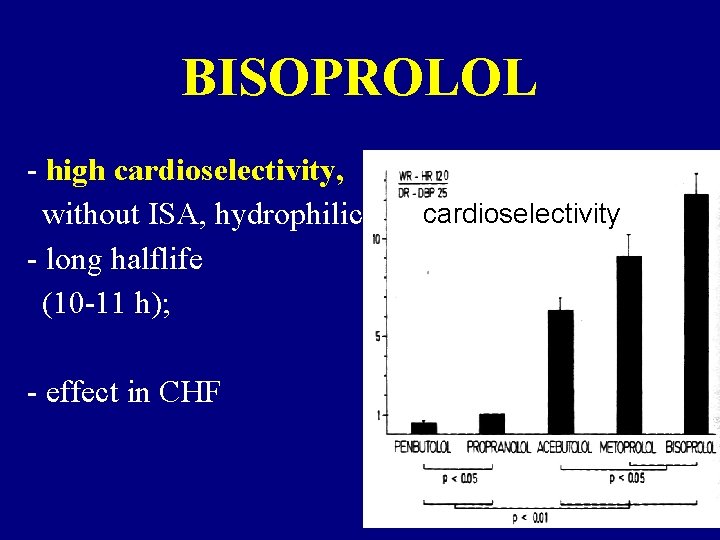
Comparison of selectivity index in essential cardioselective -blockers %
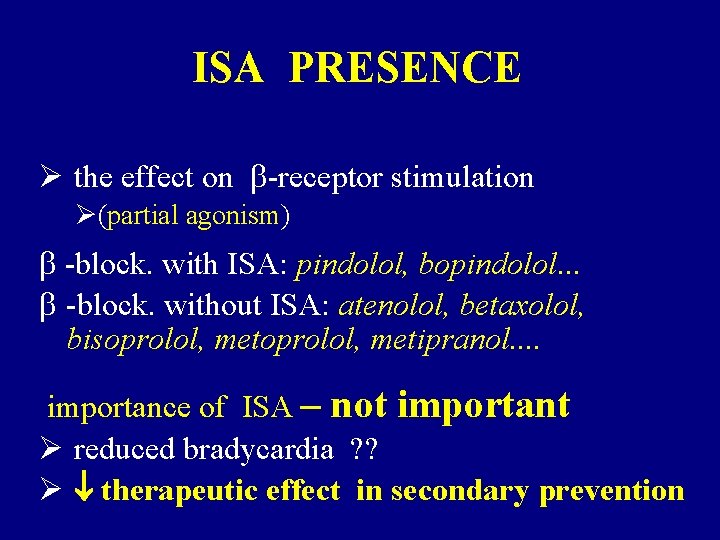
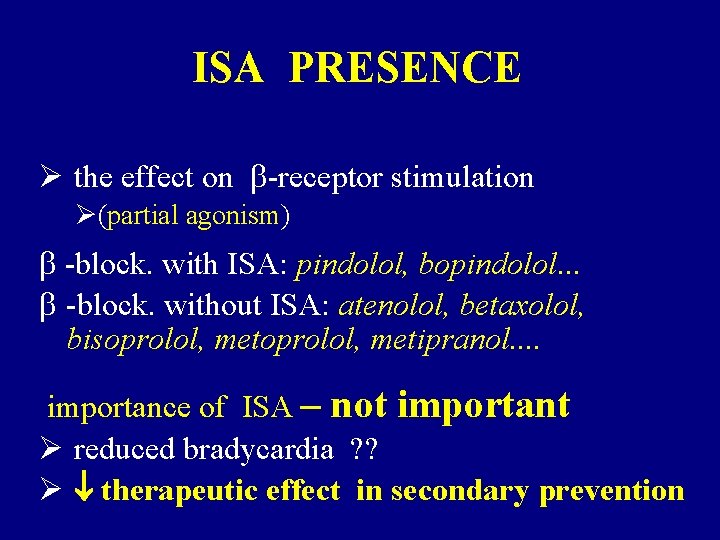
ISA PRESENCE Ø the effect on -receptor stimulation Ø(partial agonism) -block. with ISA: pindolol, bopindolol. . . -block. without ISA: atenolol, betaxolol, bisoprolol, metipranol. . importance of ISA – not important Ø reduced bradycardia ? ? Ø therapeutic effect in secondary prevention
Inverse relation between the heart rate and life length
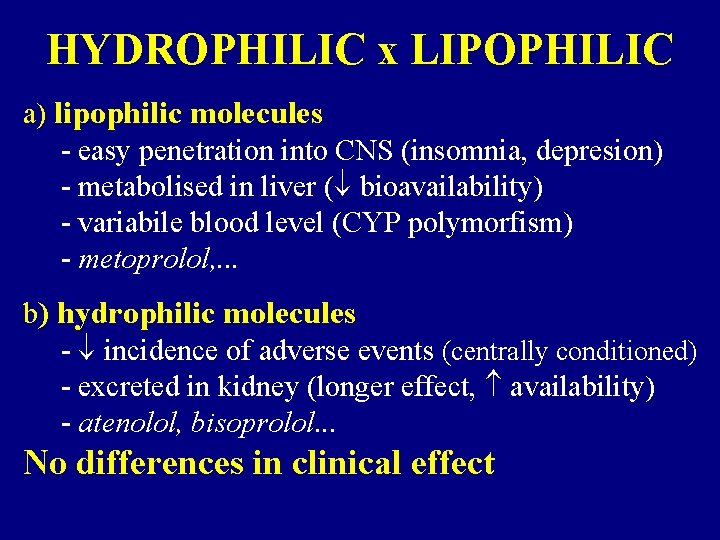
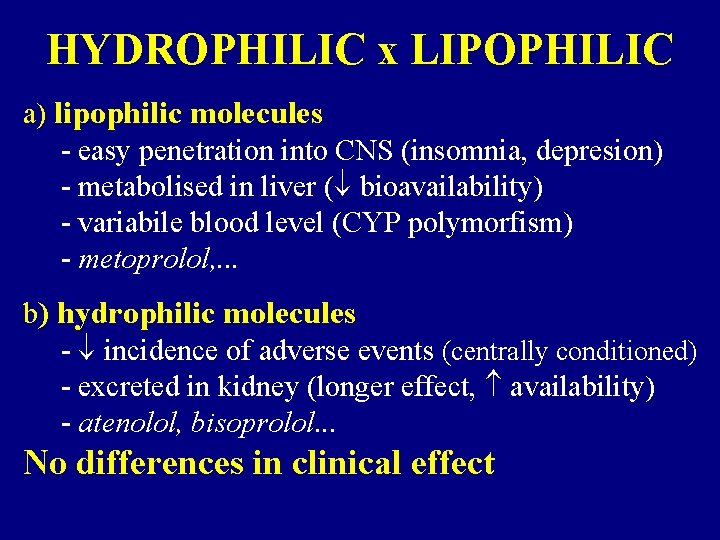
HYDROPHILIC x LIPOPHILIC a) lipophilic molecules - easy penetration into CNS (insomnia, depresion) - metabolised in liver ( bioavailability) - variabile blood level (CYP polymorfism) - metoprolol, . . . b) hydrophilic molecules - incidence of adverse events (centrally conditioned) - excreted in kidney (longer effect, availability) - atenolol, bisoprolol. . . No differences in clinical effect
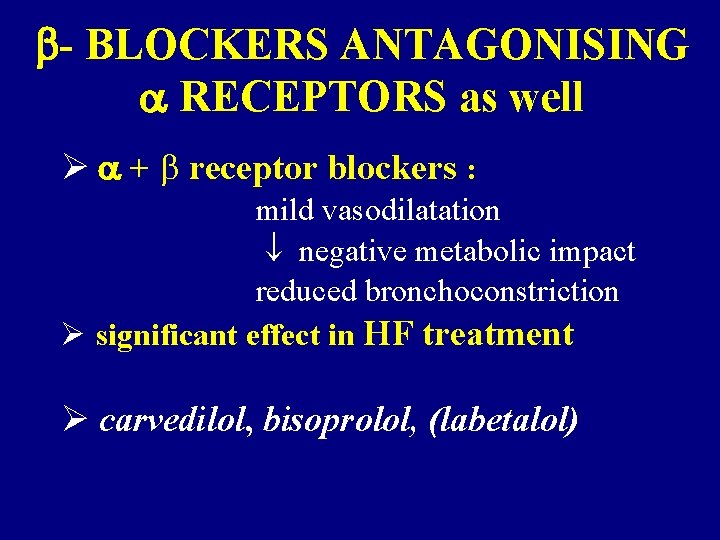
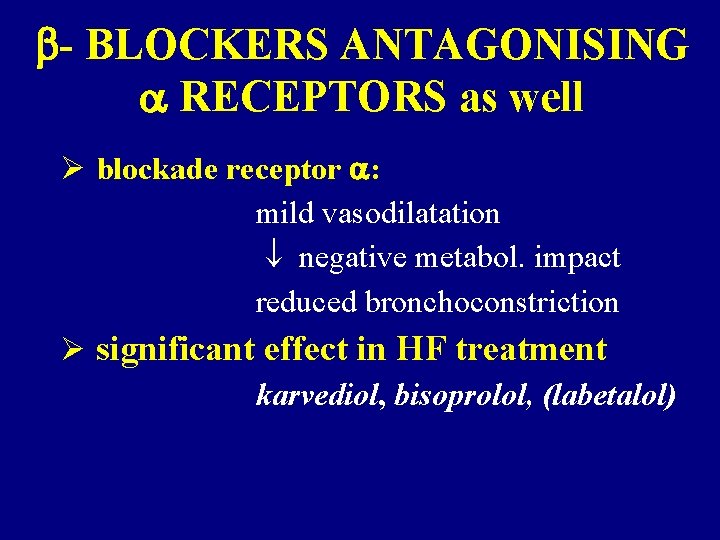
- BLOCKERS ANTAGONISING RECEPTORS as well Ø + receptor blockers : mild vasodilatation negative metabolic impact reduced bronchoconstriction Ø significant effect in HF treatment Ø carvedilol, bisoprolol, (labetalol)
Comparison of biological half-life of essential cardioselective -blockers
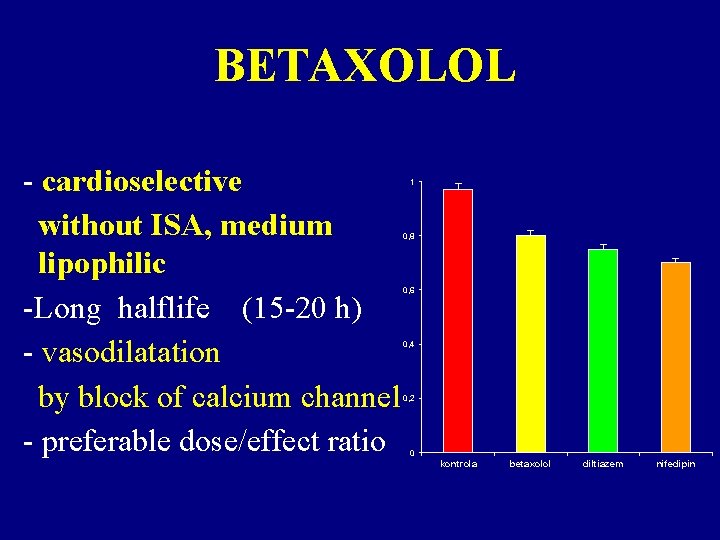
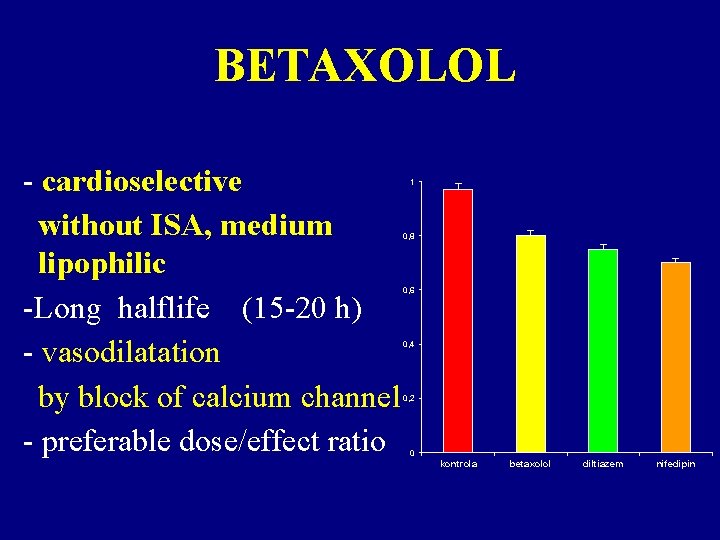
BETAXOLOL - cardioselective without ISA, medium lipophilic -Long halflife (15 -20 h) - vasodilatation by block of calcium channel - preferable dose/effect ratio 1 0, 8 0, 6 0, 4 0, 2 0 kontrola betaxolol diltiazem nifedipin
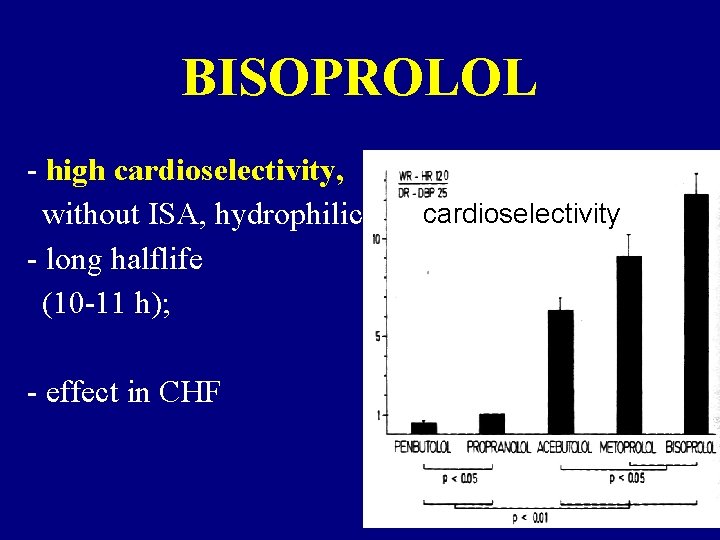
BISOPROLOL - high cardioselectivity, without ISA, hydrophilic - long halflife (10 -11 h); - effect in CHF cardioselectivity
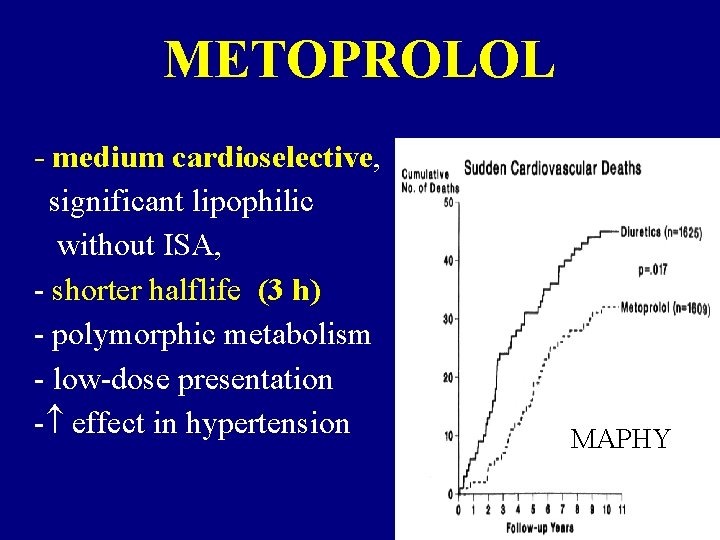
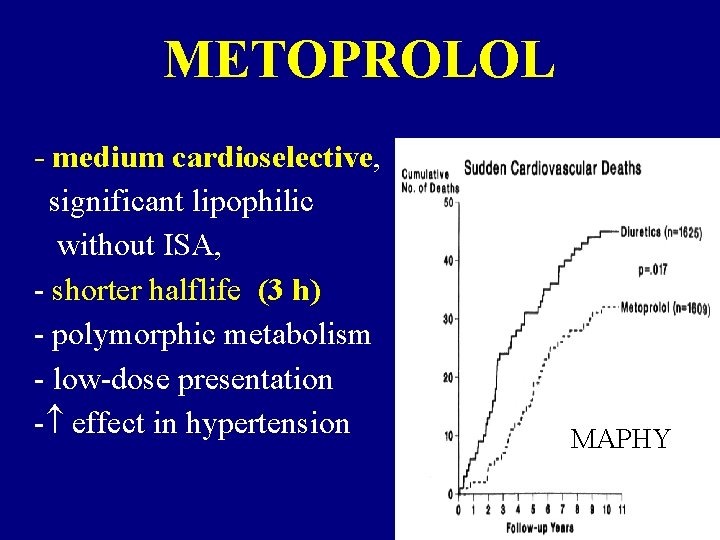
METOPROLOL - medium cardioselective, significant lipophilic without ISA, - shorter halflife (3 h) - polymorphic metabolism - low-dose presentation - effect in hypertension MAPHY

ATENOLOL medium cardioselectivity, hydrophilic, without ISA, - medium lasting effect (t 1/2 6 -9 h) - low incidence of „central“ adverse events

NEBIVOLOL • medium cardioselectivity, hydrophilic without ISA • biological halflife 8 -27 h. (polymorphism in metabolism) • Significant vasodilatation nitrate like effect

CELIPROLOL • • high cardioselectivity hydrophilic with ISA longer biological halflife (6 -8 h) vasodilatation (mediated via 2 receptor stimulation)

ESMOLOL • high cardioselectivity, without ISA very short halflife (minutes) • parenteral aplication in acute state ACEBUTOLOL • medium cardioselectivity, hydrophilic with low ISA • long biological halflife (8 -12 h)
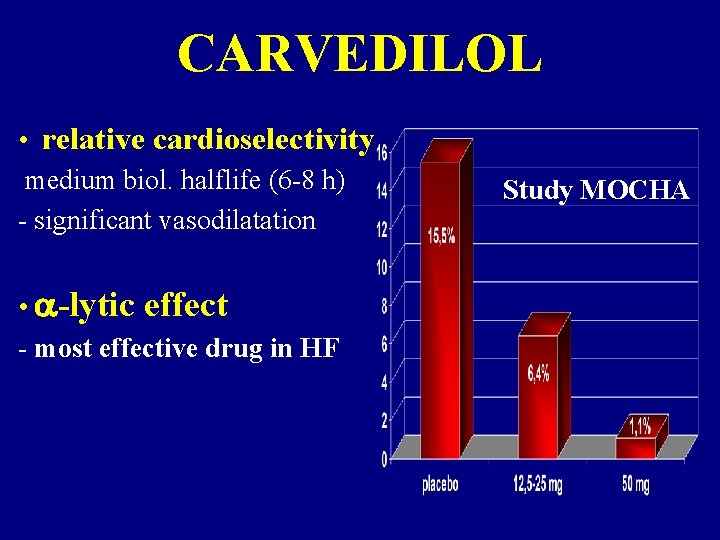
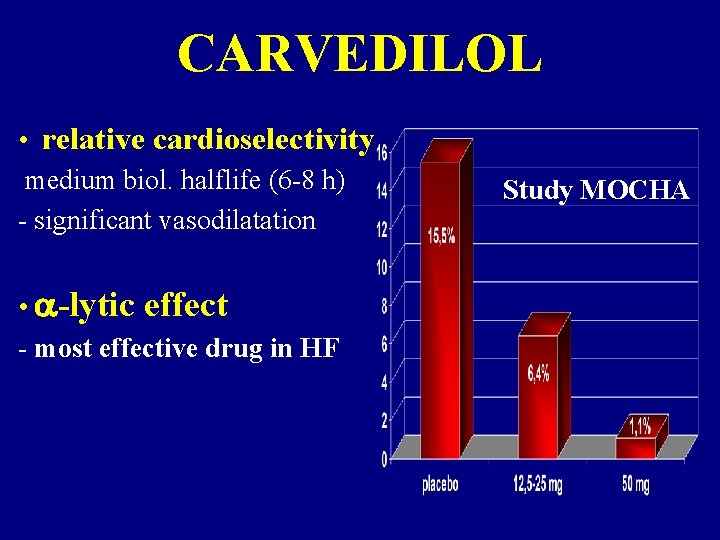
CARVEDILOL • relative cardioselectivity medium biol. halflife (6 -8 h) - significant vasodilatation • -lytic effect - most effective drug in HF Study MOCHA
CARDIOVASCULAR INDICATIONS -BLOCKERS ØHypertension ØIschemic heart disease: ØAMI ØMI – secondary prevention ØAP, silent ischemia ØHeart failure ØArrhythmias

-blockers - contraindications nonselective • conductivity disturb. • signif. bradycardia • feochromocytoma • asthma, • ischemia lower extremities, • depression • diabetes • dyslipidemia selective • conductivity disturb. • signif. bradycardia • feochromocytoma • asthma, bronchospasm.
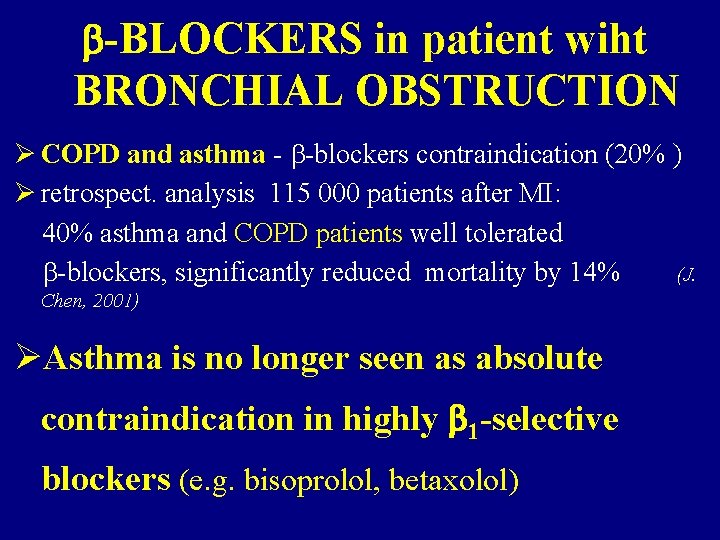
-BLOCKERS in patient wiht BRONCHIAL OBSTRUCTION Ø COPD and asthma - -blockers contraindication (20% ) Ø retrospect. analysis 115 000 patients after MI: 40% asthma and COPD patients well tolerated -blockers, significantly reduced mortality by 14% (J. Chen, 2001) ØAsthma is no longer seen as absolute contraindication in highly 1 -selective blockers (e. g. bisoprolol, betaxolol)
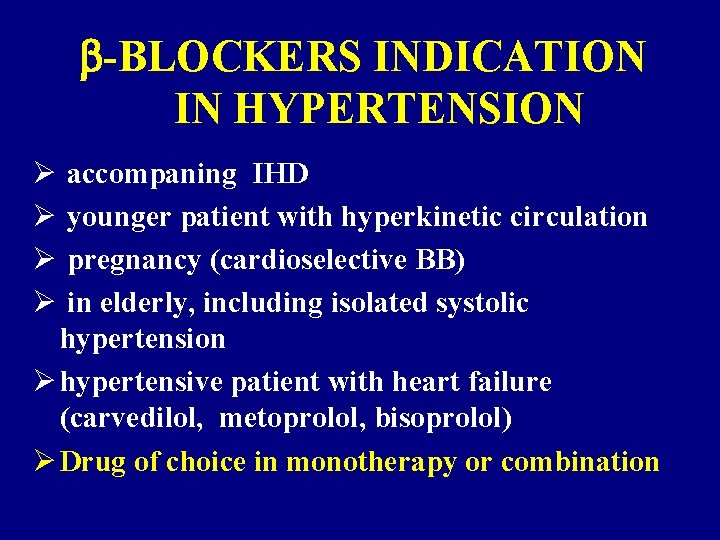
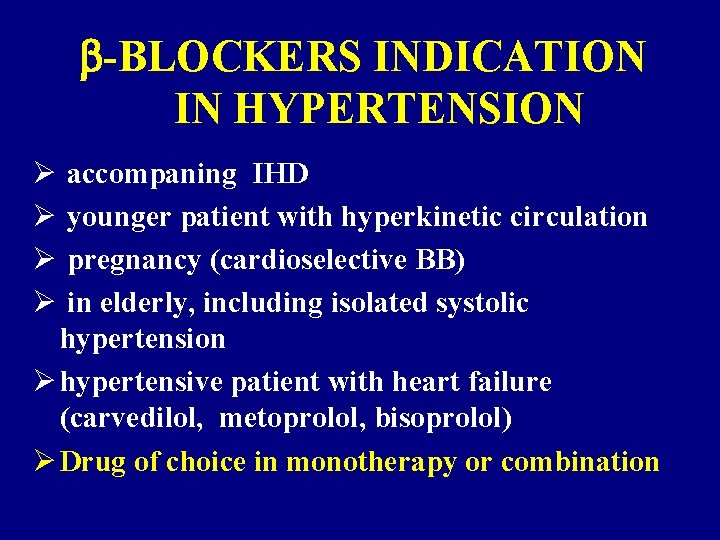
-BLOCKERS INDICATION IN HYPERTENSION Ø Ø accompaning IHD younger patient with hyperkinetic circulation pregnancy (cardioselective BB) in elderly, including isolated systolic hypertension Ø hypertensive patient with heart failure (carvedilol, metoprolol, bisoprolol) Ø Drug of choice in monotherapy or combination

ANTIHYPERTENSION DRUGS SUITABLE FOR COMBINATION with -BLOCKERS Ø diuretics Ø CCB dihydropyridine type Ø(verapamil, diltiazem causing bradycardia – attention) Ø ACE inhibitors and sartanes Ø -blockers Ø vasodilators and centrally acting drugs
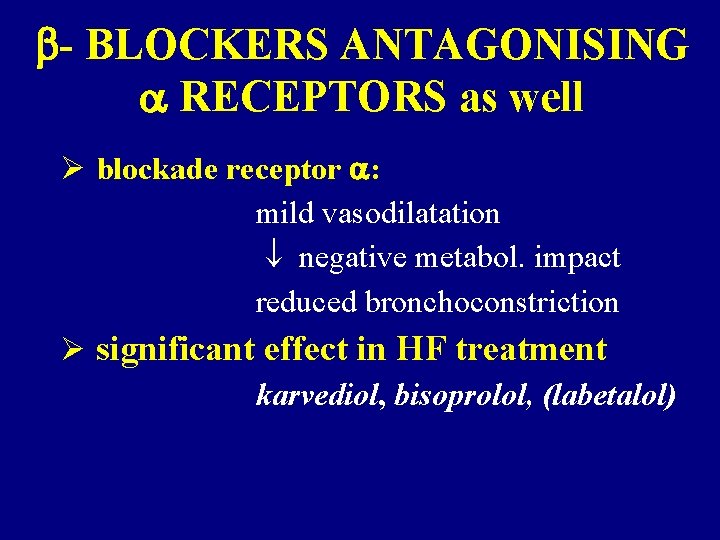
- BLOCKERS ANTAGONISING RECEPTORS as well Ø blockade receptor : mild vasodilatation negative metabol. impact reduced bronchoconstriction Ø significant effect in HF treatment karvediol, bisoprolol, (labetalol)
ACE INHIBITORS and SARTANES in HYPERTENSION
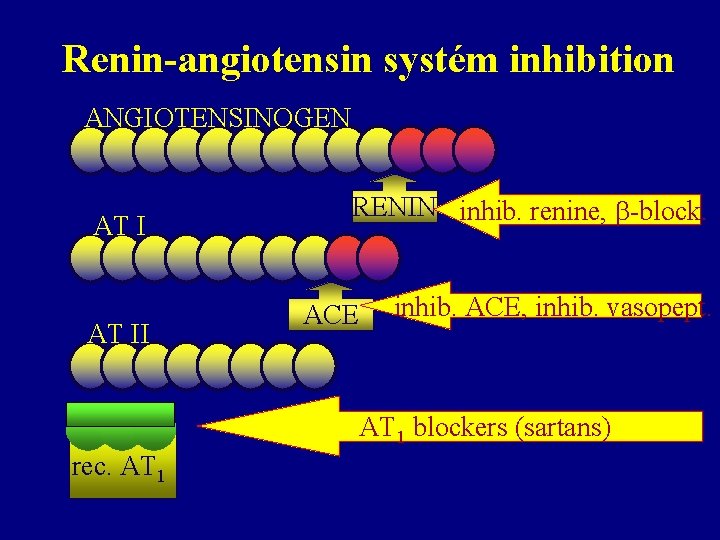
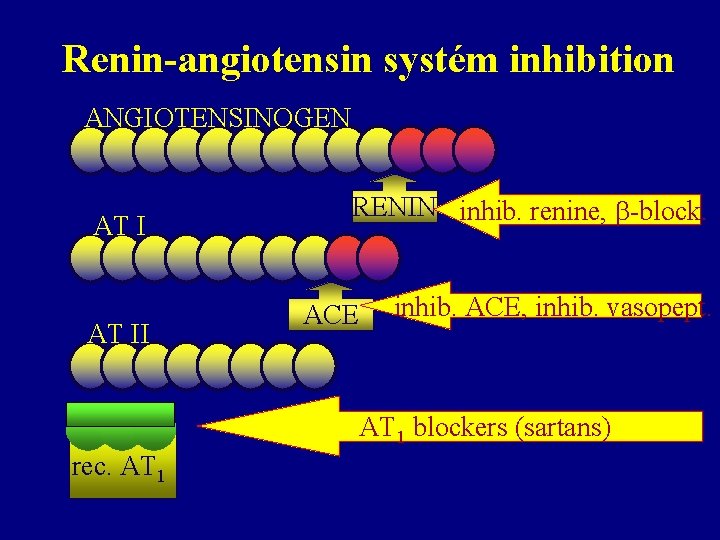
Renin-angiotensin systém inhibition ANGIOTENSINOGEN AT II RENIN inhib. renine, -block. ACE inhib. ACE, inhib. vasopept. AT 1 blockers (sartans) rec. AT 1
ACE INHIBITORS MECHANISM of ACTION 1) AI to AII conversion inhibition 2) Slow down degradation of bradykinin and neurokinins

ACE INHIBITORS PHARMACODYNAMIC EFFECT Ø peripheral resistance -VASODILATATION Ø aldosterone and ADH release + thirst Ø SODIUM and WATER RETENTION Ø NOREPINEHRINE RELEASE Ø specific dilatation of vas efferens NEPHROPROTECTION Ø fibrinolysis stimulation ( t-PA/PAI-1) Ø antimitogenic activity + apoptosis inhibition Ø endothelial dysfunction adjustment
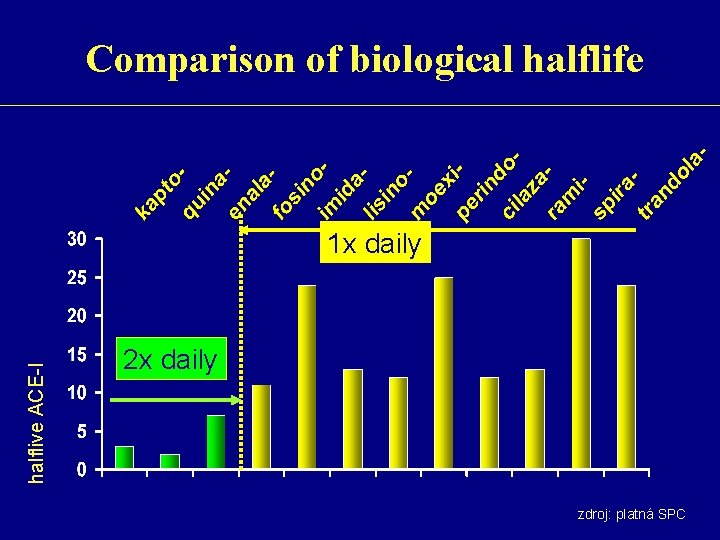
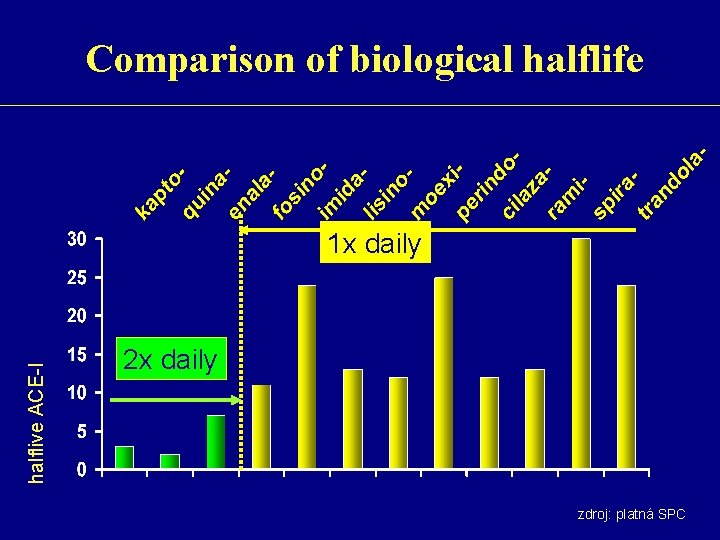
Comparison of biological halflife halflive ACE-I 1 x daily 2 x daily zdroj: platná SPC

List of ACE Enalapril Fosinopril Imidapril Lisinopril 2 x 5 -20 mg 1 x 10 -20 mg 1 x 5 -10 mg 1 x 20 -80 mg Moexipril 1 x 7, 5 -15 mg Perindopril 1 x 4 -8 mg Quinapril 1 -2 x 5 -20 mg Ramipril 1 x 2, 5 -10 mg Spirapril 1 x 6 mg 1 x 2 -4 mg Trandolapril
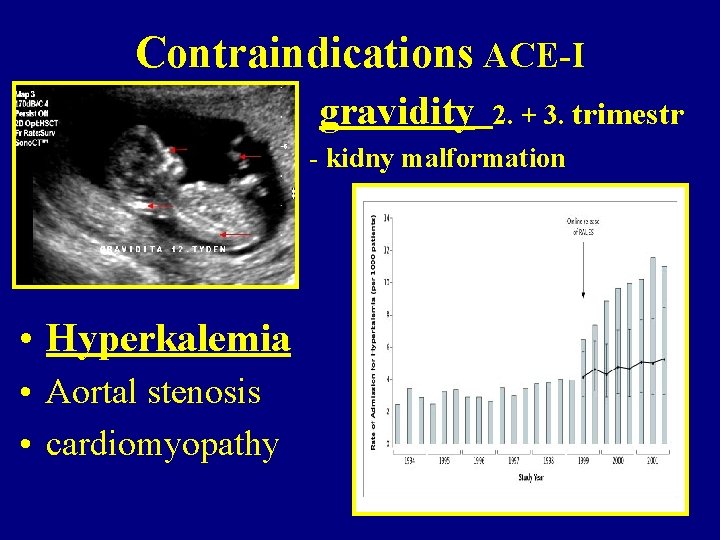
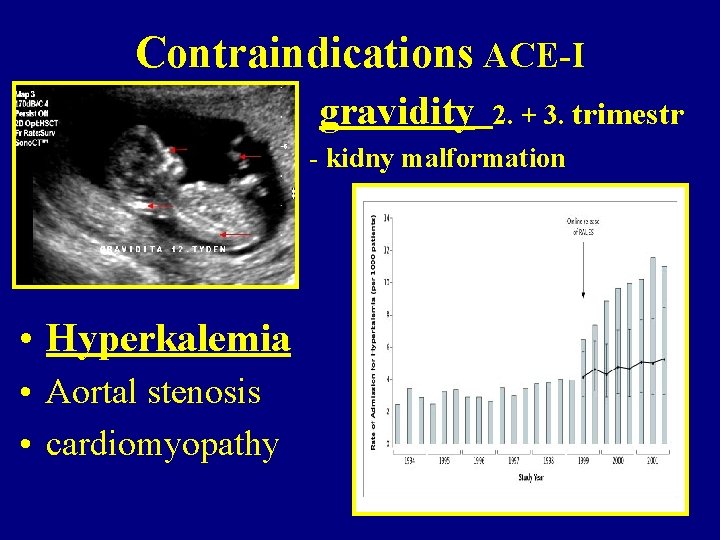
Contraindications ACE-I gravidity 2. + 3. trimestr - kidny malformation • Hyperkalemia • Aortal stenosis • cardiomyopathy
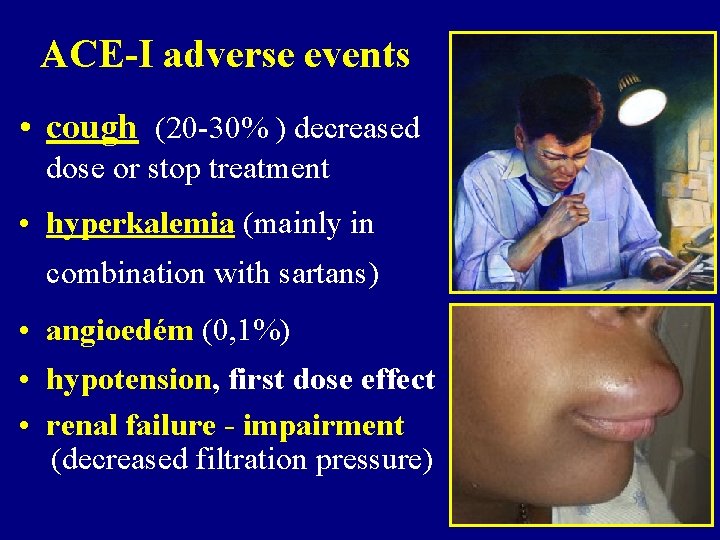
ACE-I adverse events • cough (20 -30% ) decreased dose or stop treatment • hyperkalemia (mainly in combination with sartans) • angioedém (0, 1%) • hypotension, first dose effect • renal failure - impairment (decreased filtration pressure)
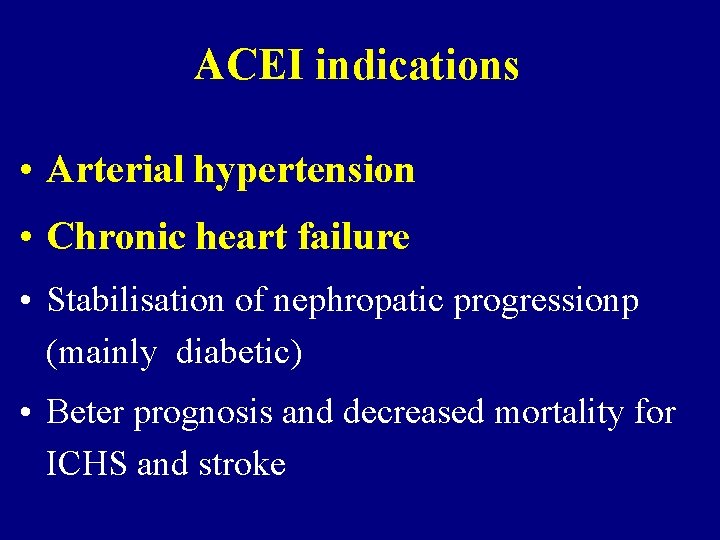
ACEI indications • Arterial hypertension • Chronic heart failure • Stabilisation of nephropatic progressionp (mainly diabetic) • Beter prognosis and decreased mortality for ICHS and stroke
ACEI advantages in hypertension • No metabolic effects, (no influence on glucose and lipid metabolism) • Most effective inhibition of heart hypertrophy • Regresion of myocardial fibrosis
Sartans (AT 1 receptor inhibitors)
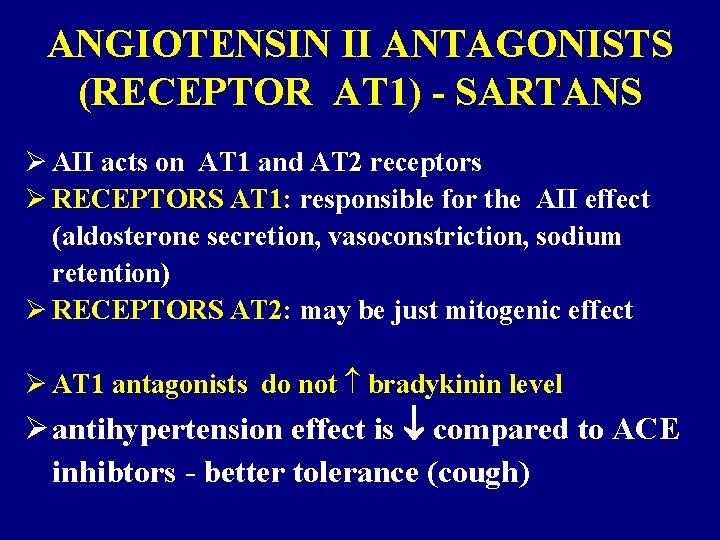
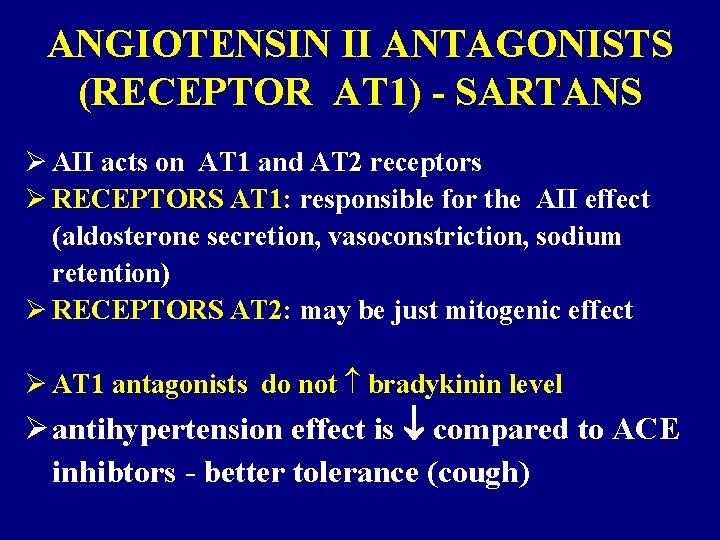
ANGIOTENSIN II ANTAGONISTS (RECEPTOR AT 1) - SARTANS Ø AII acts on AT 1 and AT 2 receptors Ø RECEPTORS AT 1: responsible for the AII effect (aldosterone secretion, vasoconstriction, sodium retention) Ø RECEPTORS AT 2: may be just mitogenic effect Ø AT 1 antagonists do not bradykinin level Ø antihypertension effect is compared to ACE inhibtors - better tolerance (cough)
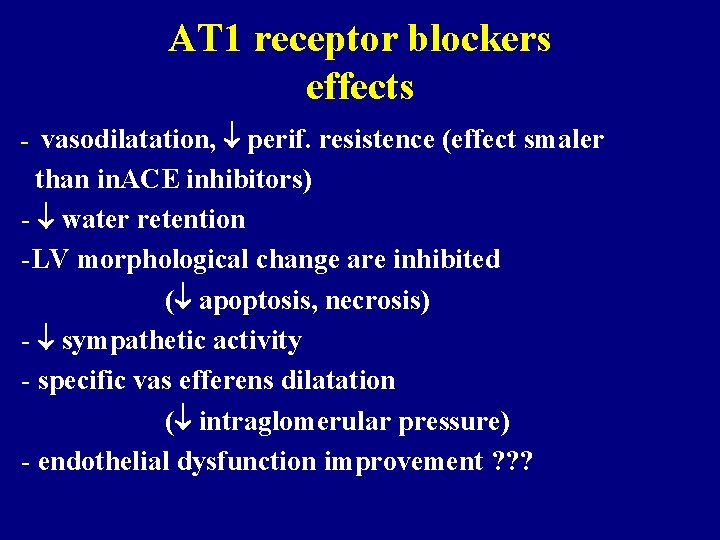
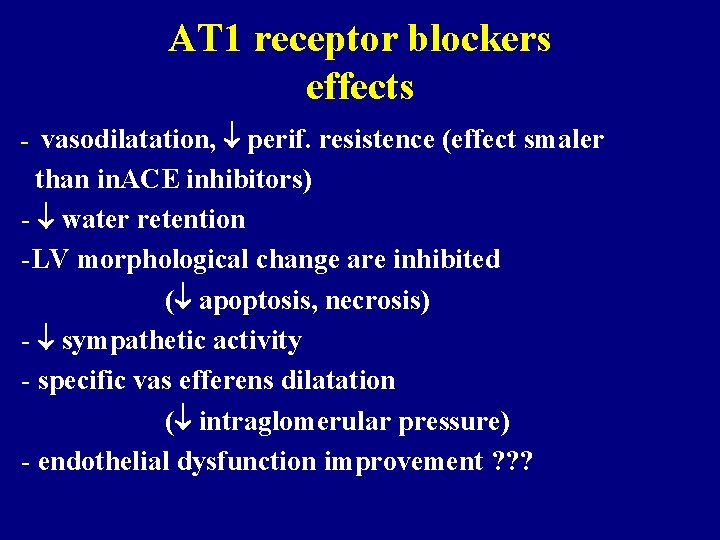
AT 1 receptor blockers effects - vasodilatation, perif. resistence (effect smaler than in. ACE inhibitors) - water retention -LV morphological change are inhibited ( apoptosis, necrosis) - sympathetic activity - specific vas efferens dilatation ( intraglomerular pressure) - endothelial dysfunction improvement ? ? ?
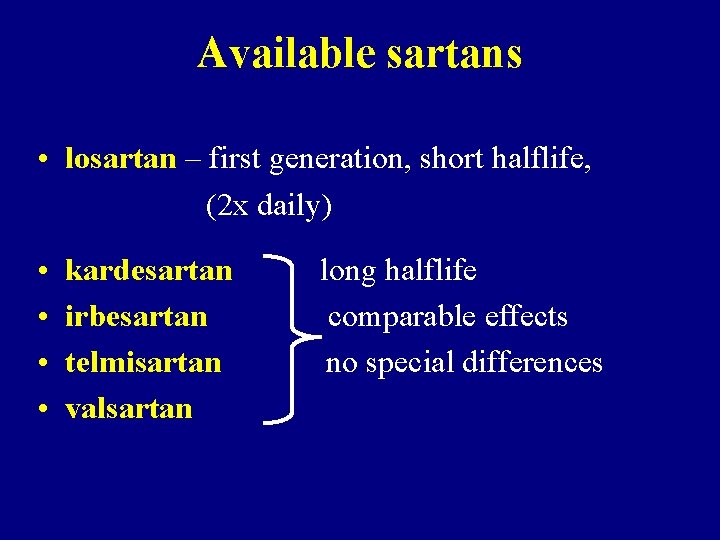
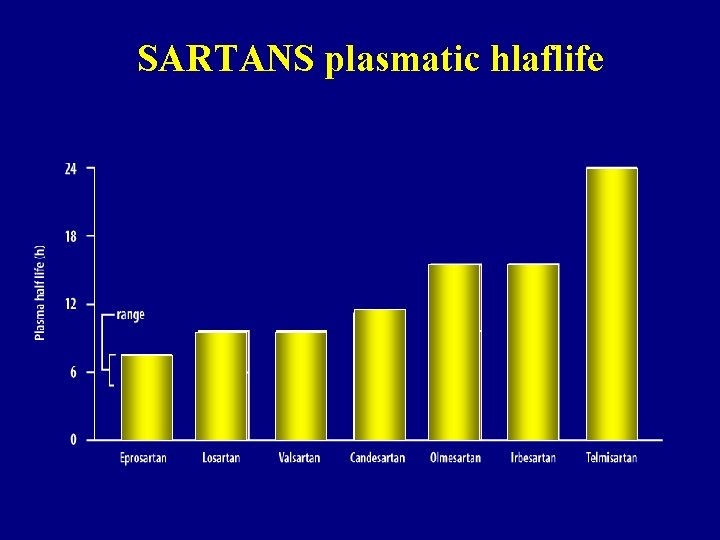
Available sartans • losartan – first generation, short halflife, (2 x daily) • • kardesartan irbesartan telmisartan valsartan long halflife comparable effects no special differences
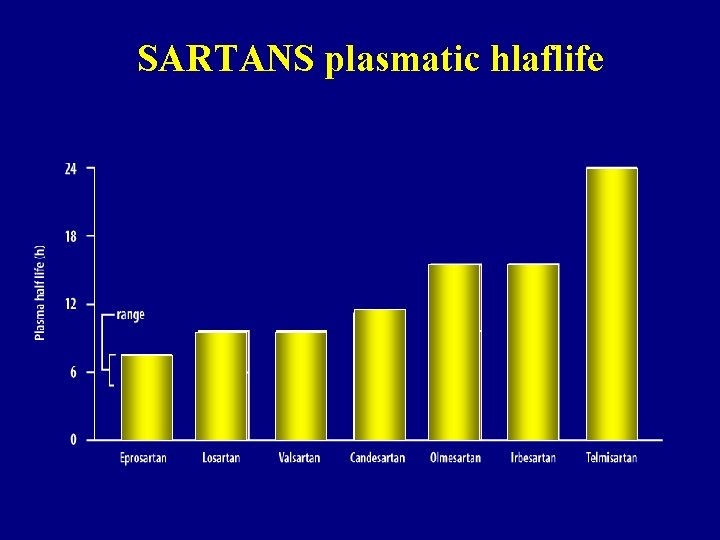
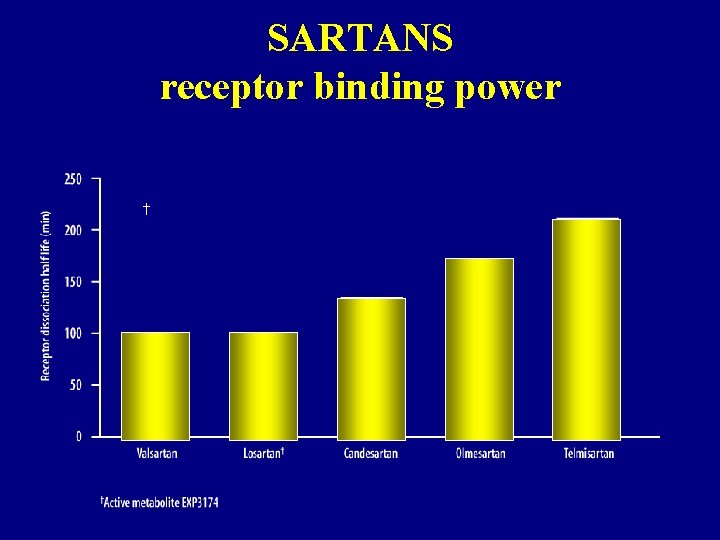
SARTANS plasmatic hlaflife
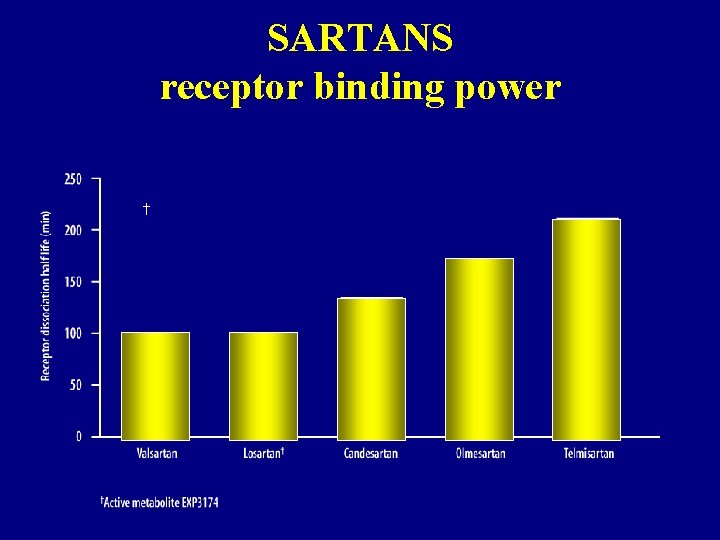
SARTANS receptor binding power †
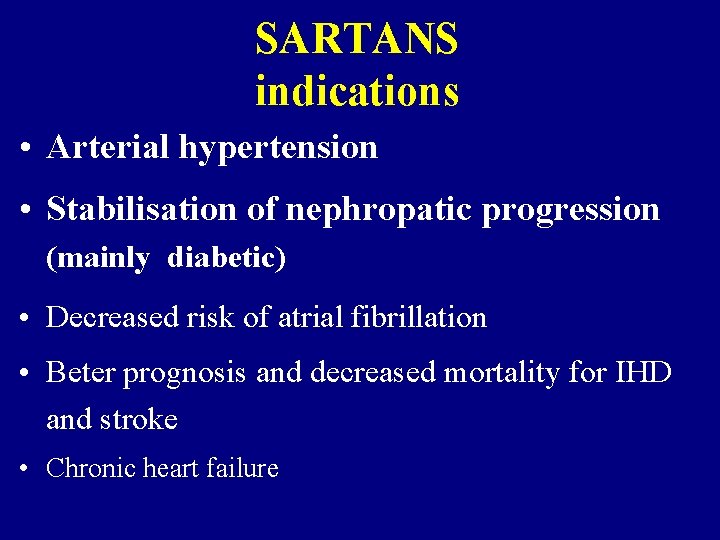
SARTANS indications • Arterial hypertension • Stabilisation of nephropatic progression (mainly diabetic) • Decreased risk of atrial fibrillation • Beter prognosis and decreased mortality for IHD and stroke • Chronic heart failure
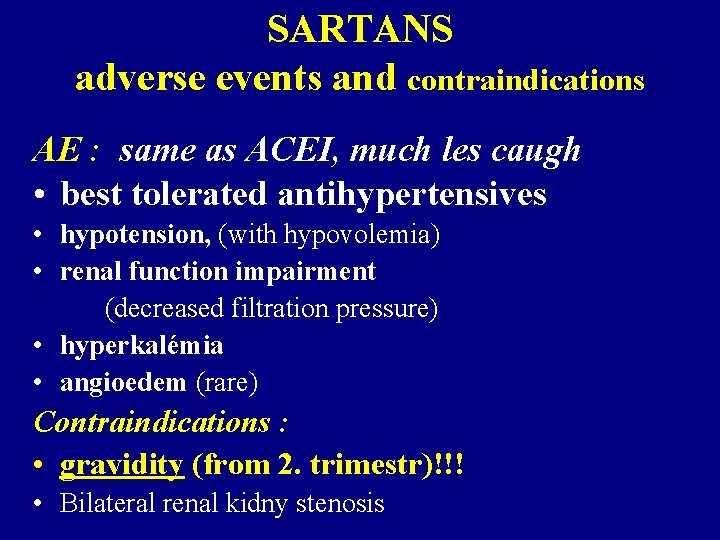
SARTANS adverse events and contraindications AE : same as ACEI, much les caugh • best tolerated antihypertensives • hypotension, (with hypovolemia) • renal function impairment (decreased filtration pressure) • hyperkalémia • angioedem (rare) Contraindications : • gravidity (from 2. trimestr)!!! • Bilateral renal kidny stenosis
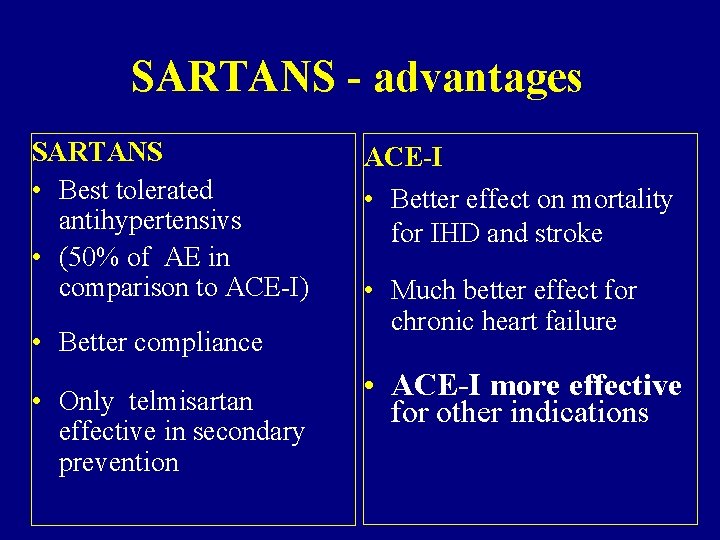
SARTANS - advantages SARTANS • Best tolerated antihypertensivs • (50% of AE in comparison to ACE-I) • Better compliance • Only telmisartan effective in secondary prevention ACE-I • Better effect on mortality for IHD and stroke • Much better effect for chronic heart failure • ACE-I more effective for other indications
ALDOSTERONE RECEPTOR INHIBITORS
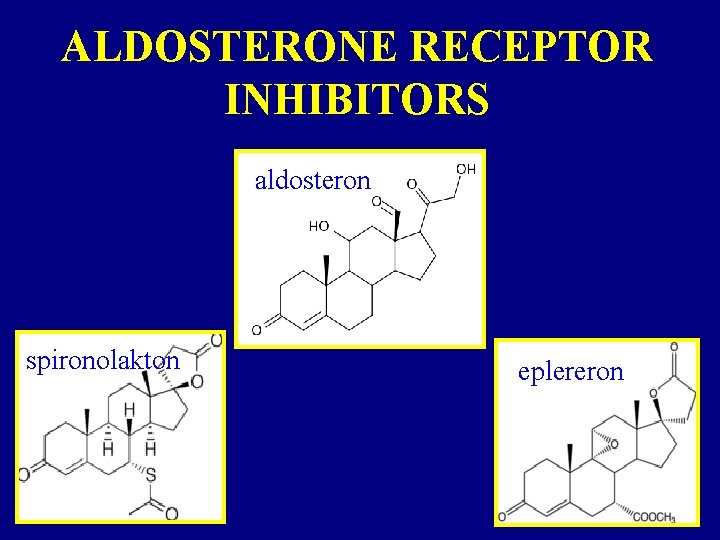
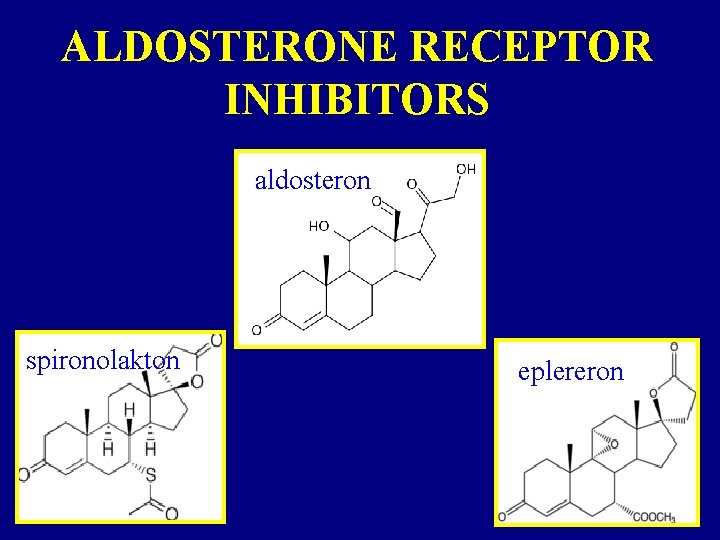
ALDOSTERONE RECEPTOR INHIBITORS aldosteron spironolakton eplereron
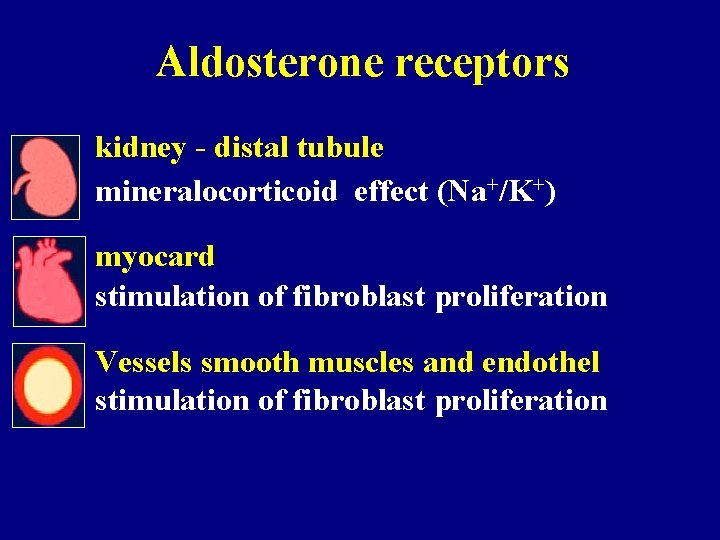
Aldosterone receptors kidney - distal tubule mineralocorticoid effect (Na+/K+) myocard stimulation of fibroblast proliferation Vessels smooth muscles and endothel stimulation of fibroblast proliferation
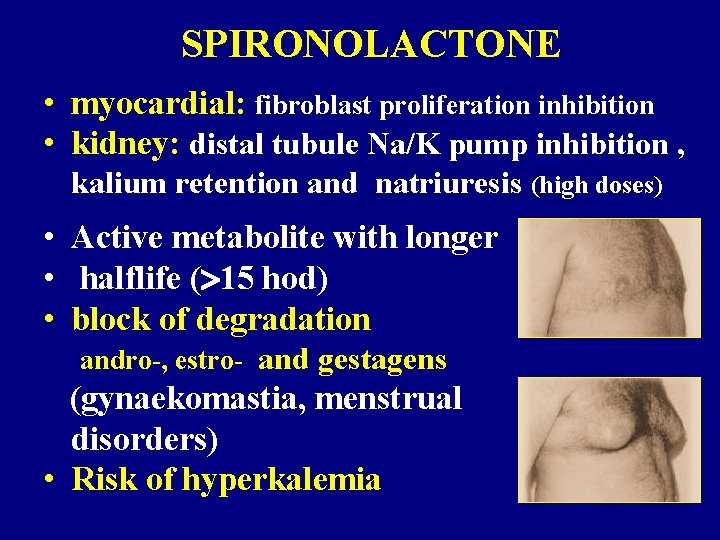
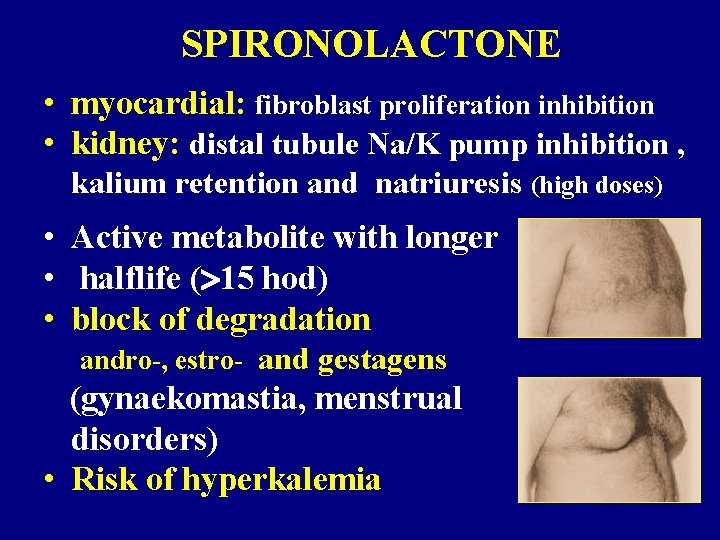
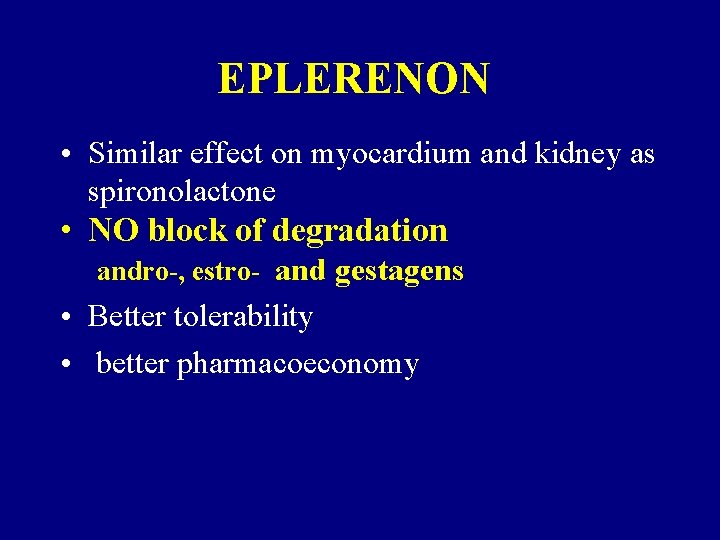
SPIRONOLACTONE • myocardial: fibroblast proliferation inhibition • kidney: distal tubule Na/K pump inhibition , kalium retention and natriuresis (high doses) • Active metabolite with longer • halflife ( 15 hod) • block of degradation andro-, estro- and gestagens (gynaekomastia, menstrual disorders) • Risk of hyperkalemia
EPLERENON • Similar effect on myocardium and kidney as spironolactone • NO block of degradation andro-, estro- and gestagens • Better tolerability • better pharmacoeconomy

CALCIUM CHANNEL BLOCKERS (CCB) in HYPERTENSION THERAPY
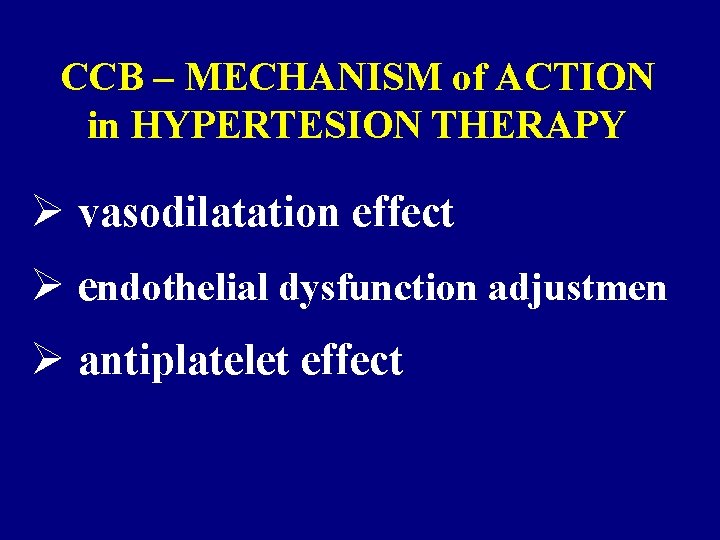
CCB – MECHANISM of ACTION in HYPERTESION THERAPY Ø vasodilatation effect Ø endothelial dysfunction adjustmen Ø antiplatelet effect

CALCIUM CHANNEL BLOCKERS (CCB) • antihypertensive effect (arteriolar relaxation ) • antiischemic effect (coronary arteries relaxation et stenotic region) • antiarrythmic effect (decreased excitability, conductivity and production of impulses)
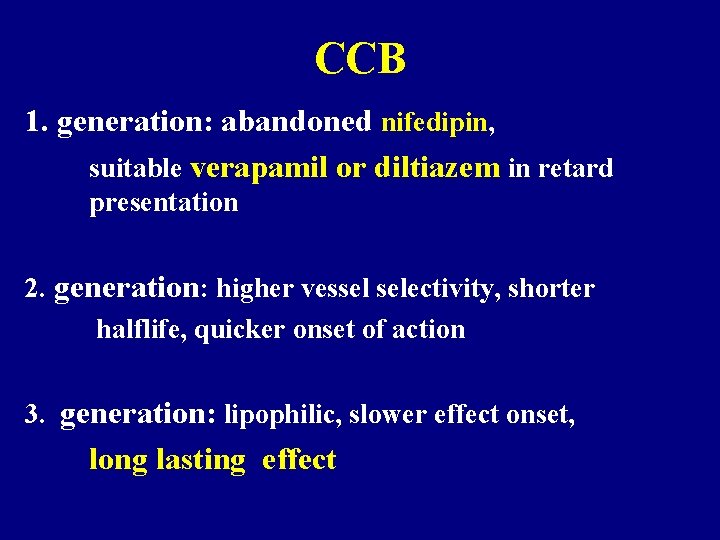
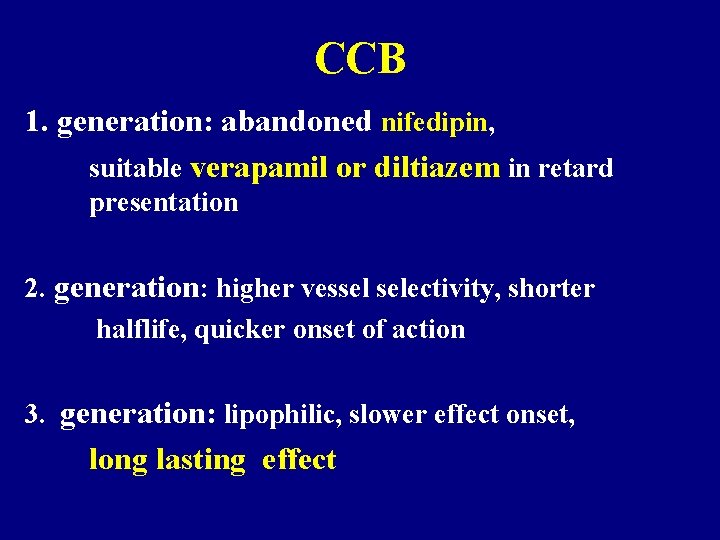
CCB 1. generation: abandoned nifedipin, suitable verapamil or diltiazem in retard presentation 2. generation: higher vessel selectivity, shorter halflife, quicker onset of action 3. generation: lipophilic, slower effect onset, long lasting effect
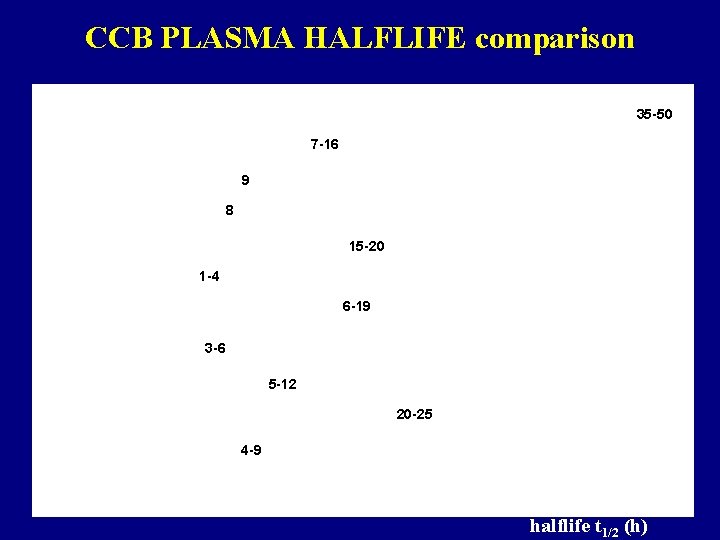
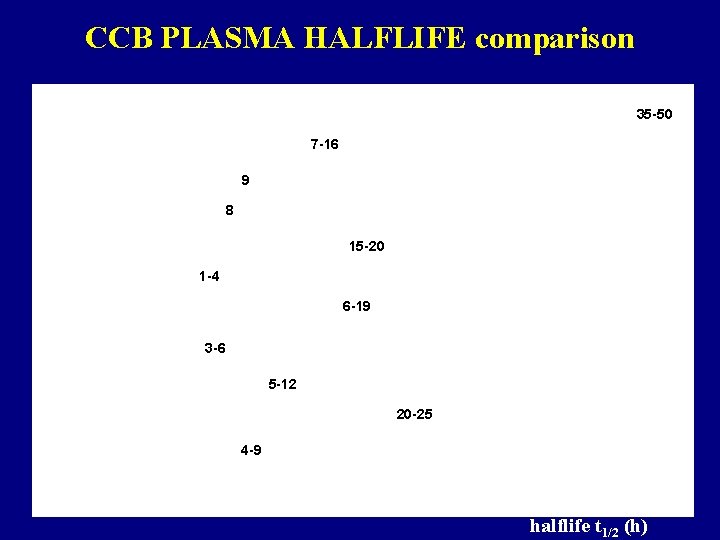
CCB PLASMA HALFLIFE comparison 35 -50 7 -16 9 8 15 -20 1 -4 6 -19 3 -6 5 -12 20 -25 4 -9 halflife t 1/2 (h)
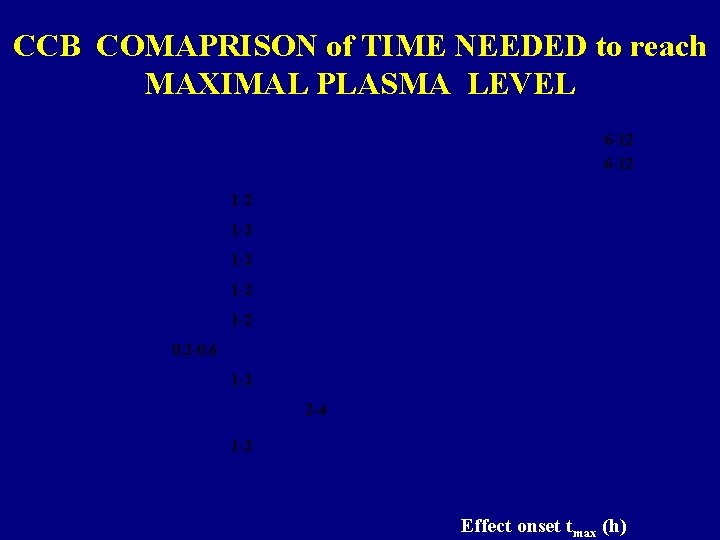
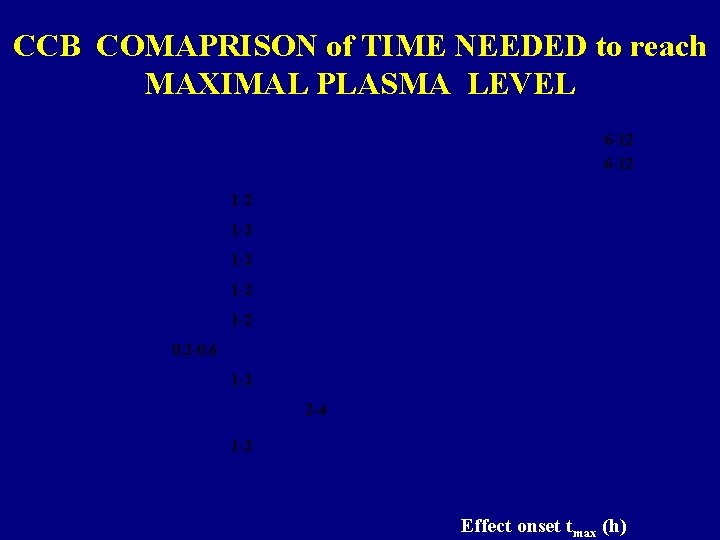
CCB COMAPRISON of TIME NEEDED to reach MAXIMAL PLASMA LEVEL 6 -12 1 -2 1 -2 1 -2 0. 2 -0. 6 1 -2 2 -4 1 -2 Effect onset tmax (h)
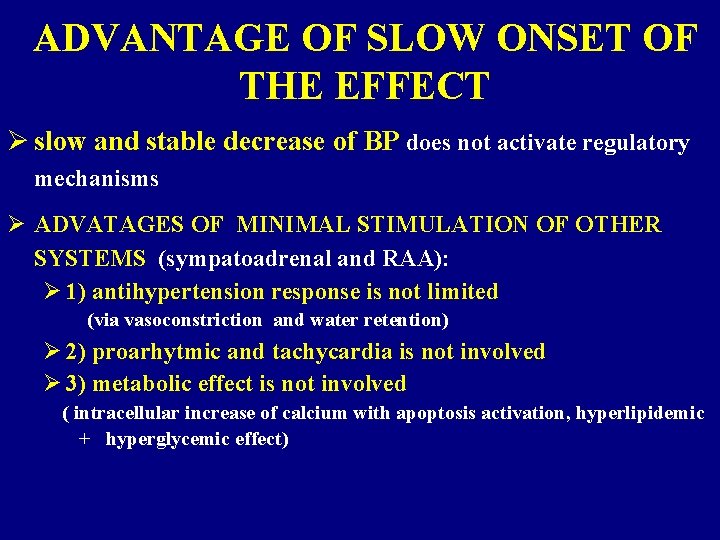
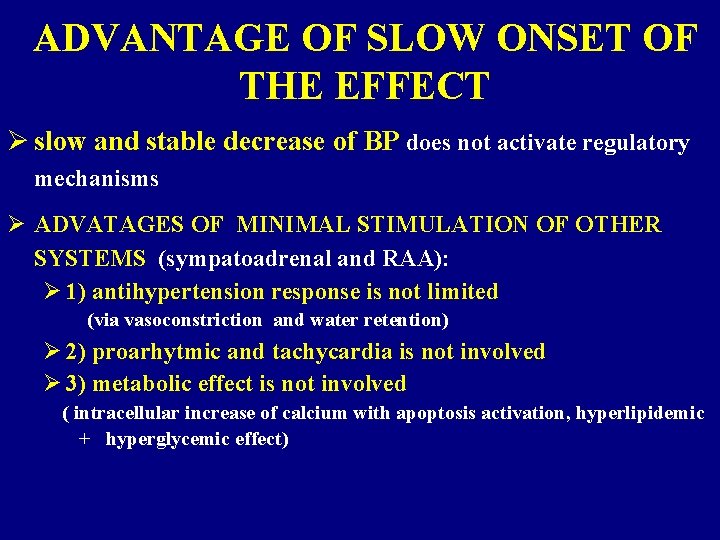
ADVANTAGE OF SLOW ONSET OF THE EFFECT Ø slow and stable decrease of BP does not activate regulatory mechanisms Ø ADVATAGES OF MINIMAL STIMULATION OF OTHER SYSTEMS (sympatoadrenal and RAA): Ø 1) antihypertension response is not limited (via vasoconstriction and water retention) Ø 2) proarhytmic and tachycardia is not involved Ø 3) metabolic effect is not involved ( intracellular increase of calcium with apoptosis activation, hyperlipidemic + hyperglycemic effect)
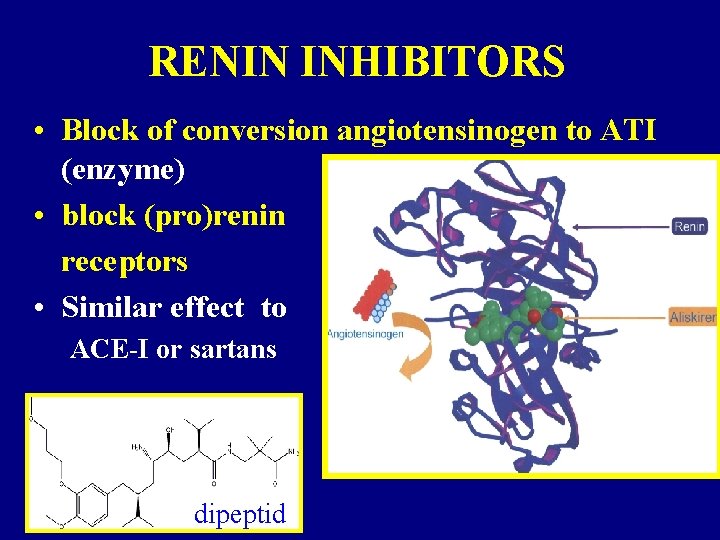
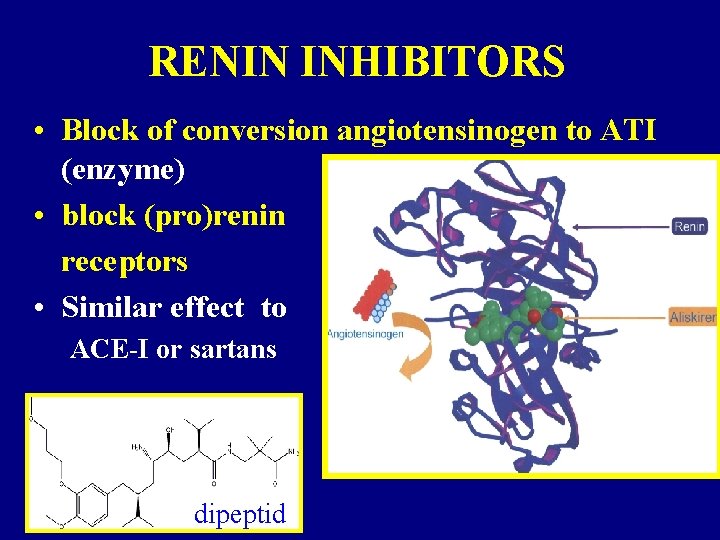
RENIN INHIBITORS • Block of conversion angiotensinogen to ATI (enzyme) • block (pro)renin receptors • Similar effect to ACE-I or sartans • aliskiren dipeptid
When inhibits RAAS? • hypertension • secondary prevention IHD, stroke, • prophylaxis of left ventricular remodeling and heart failure • prophylaxis of diabetic nephropathy
ANTIHYPERTENSIVES 2. CHOICE (EFFECT ON MORTALITY AND MORBIDITY NOT PROVED)
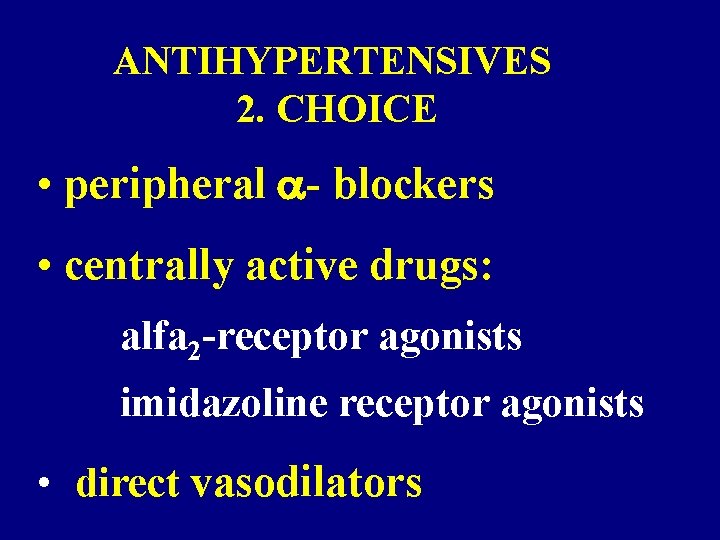
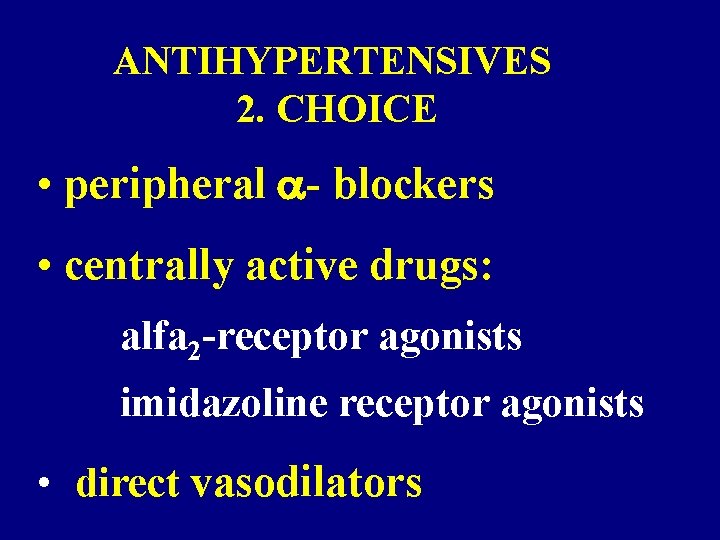
ANTIHYPERTENSIVES 2. CHOICE • peripheral - blockers • centrally active drugs: alfa 2 -receptor agonists imidazoline receptor agonists • direct vasodilators
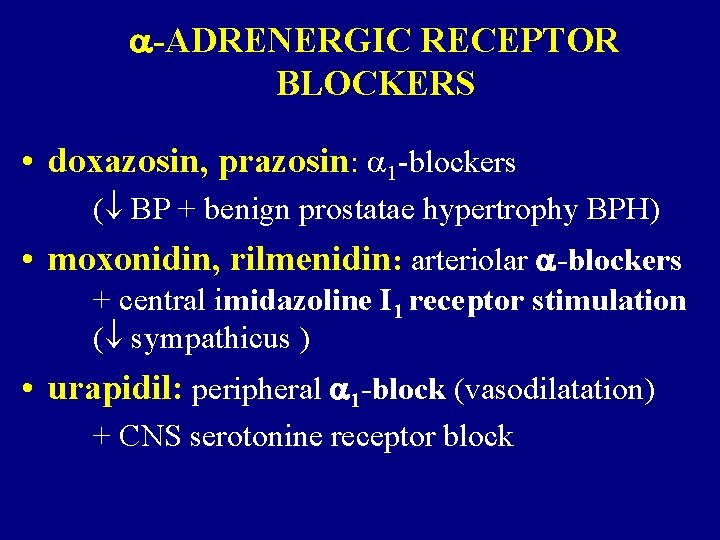
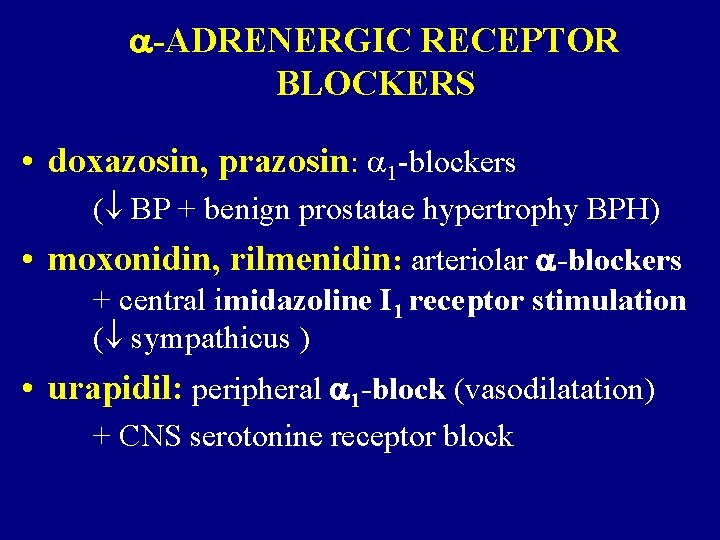
-ADRENERGIC RECEPTOR BLOCKERS • doxazosin, prazosin: 1 -blockers ( BP + benign prostatae hypertrophy BPH) • moxonidin, rilmenidin: arteriolar -blockers + central imidazoline I 1 receptor stimulation ( sympathicus ) • urapidil: peripheral 1 -block (vasodilatation) + CNS serotonine receptor block
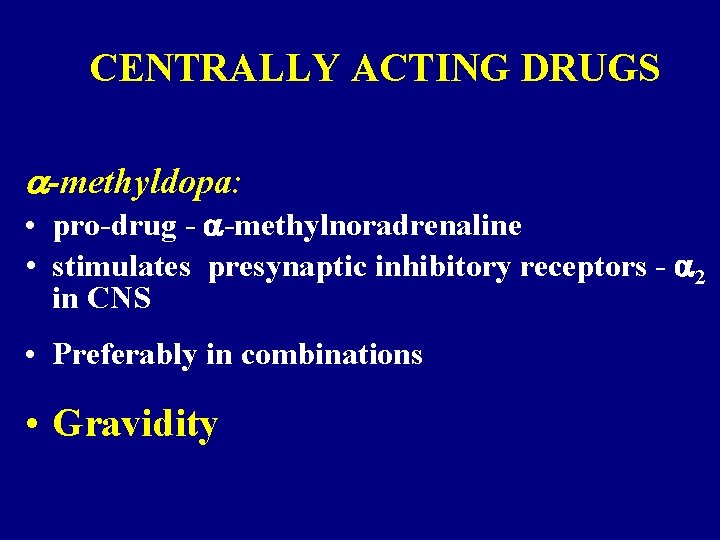
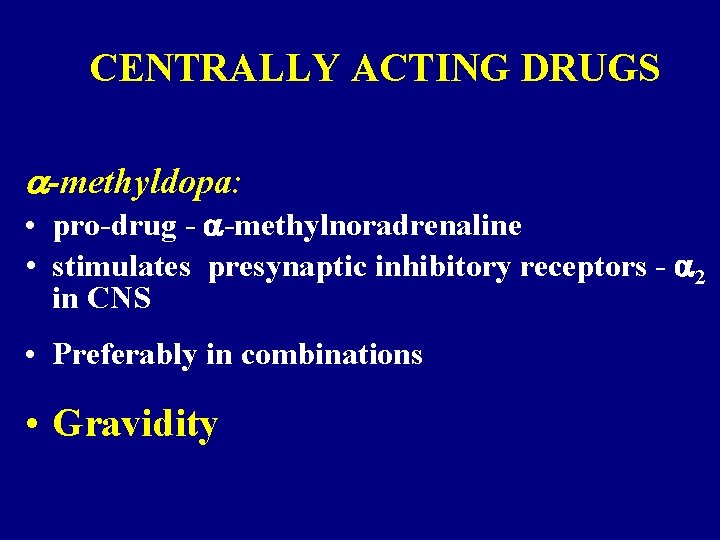
CENTRALLY ACTING DRUGS -methyldopa: • pro-drug - -methylnoradrenaline • stimulates presynaptic inhibitory receptors - 2 in CNS • Preferably in combinations • Gravidity

WHY combinations How to combine
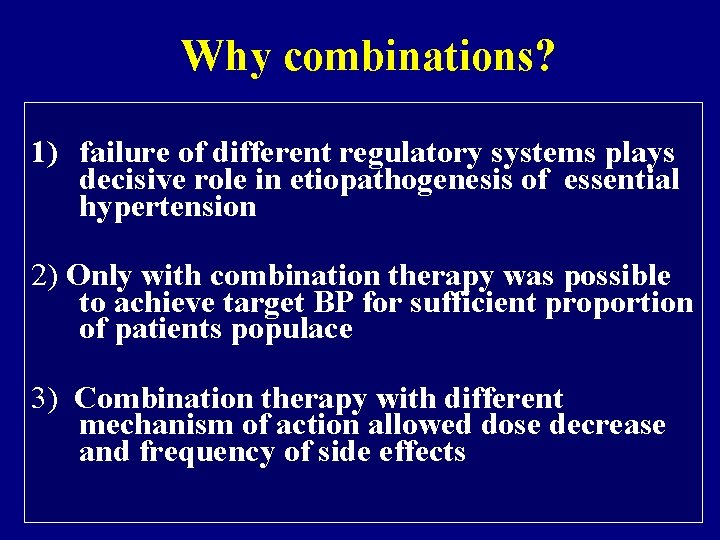
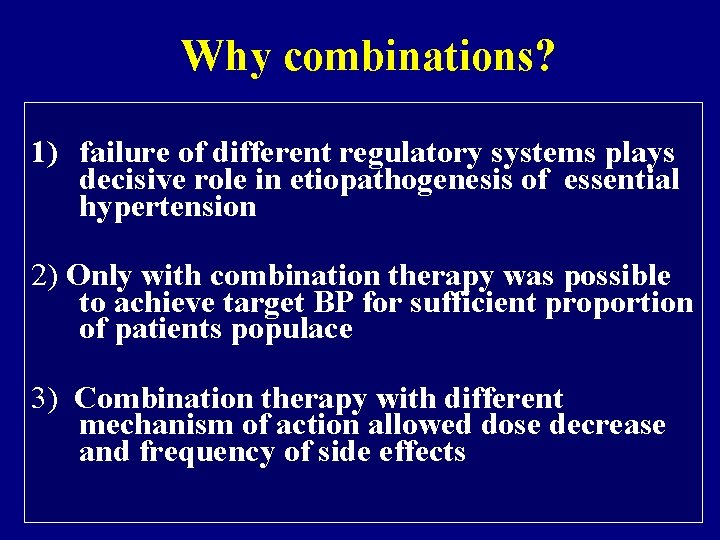
Why combinations? 1) failure of different regulatory systems plays decisive role in etiopathogenesis of essential hypertension 2) Only with combination therapy was possible to achieve target BP for sufficient proportion of patients populace 3) Combination therapy with different mechanism of action allowed dose decrease and frequency of side effects
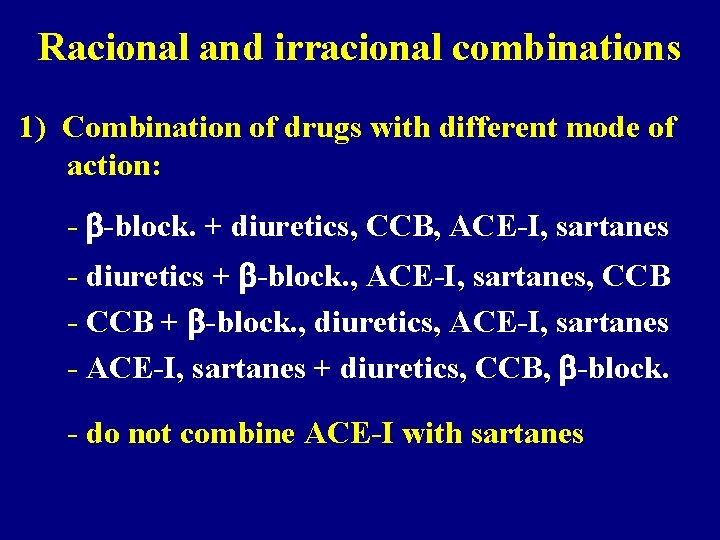
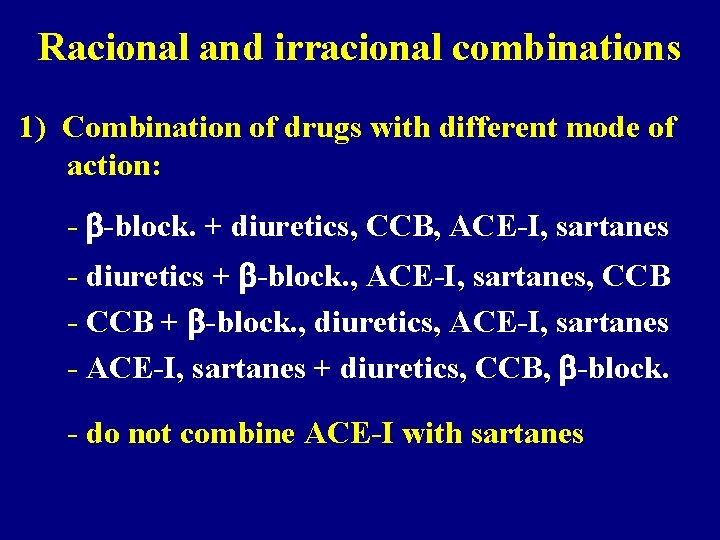
Racional and irracional combinations 1) Combination of drugs with different mode of action: - -block. + diuretics, CCB, ACE-I, sartanes - diuretics + -block. , ACE-I, sartanes, CCB - CCB + -block. , diuretics, ACE-I, sartanes - ACE-I, sartanes + diuretics, CCB, -block. - do not combine ACE-I with sartanes
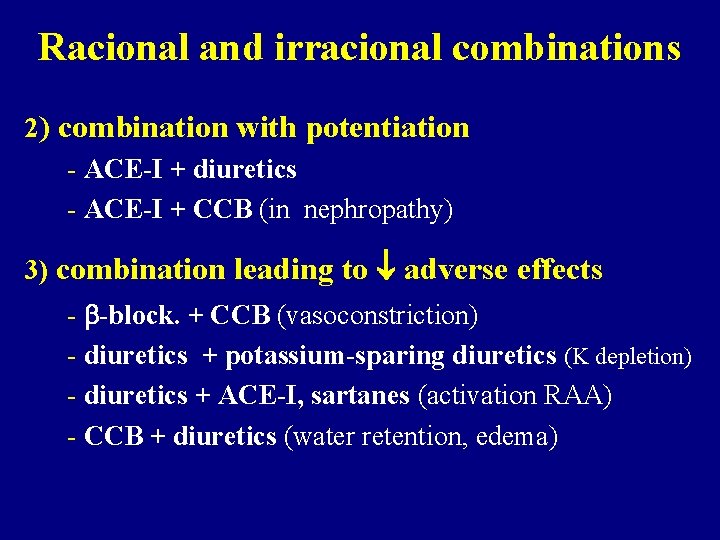
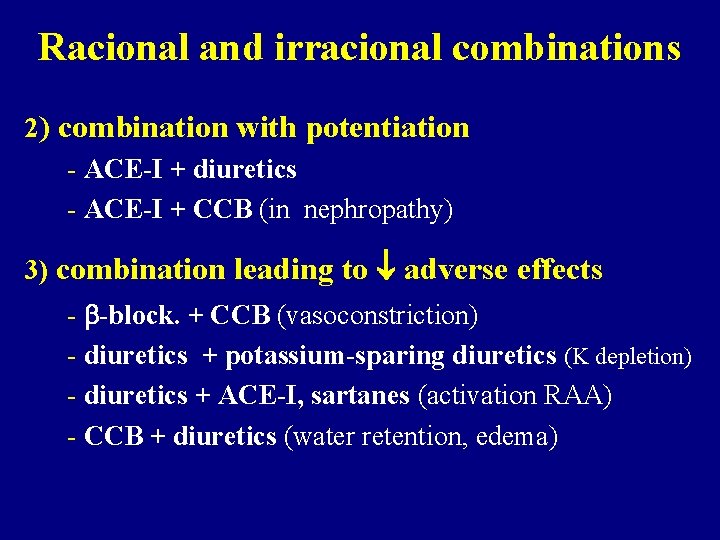
Racional and irracional combinations 2) combination with potentiation - ACE-I + diuretics - ACE-I + CCB (in nephropathy) 3) combination leading to adverse effects - -block. + CCB (vasoconstriction) - diuretics + potassium-sparing diuretics (K depletion) - diuretics + ACE-I, sartanes (activation RAA) - CCB + diuretics (water retention, edema)
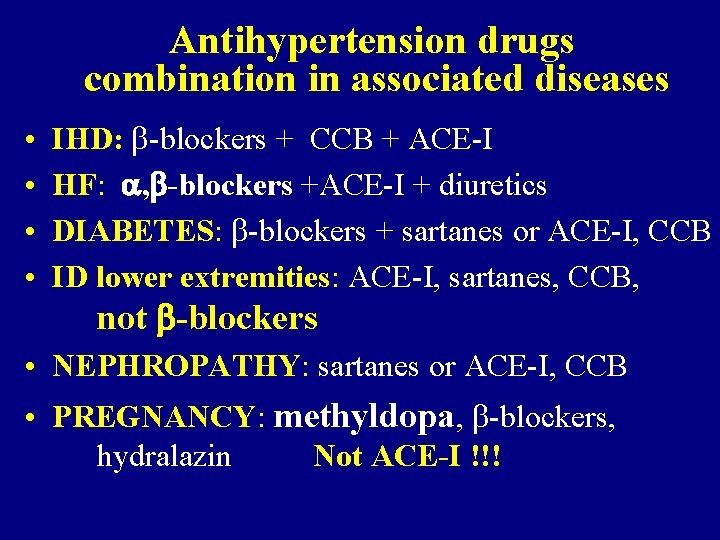
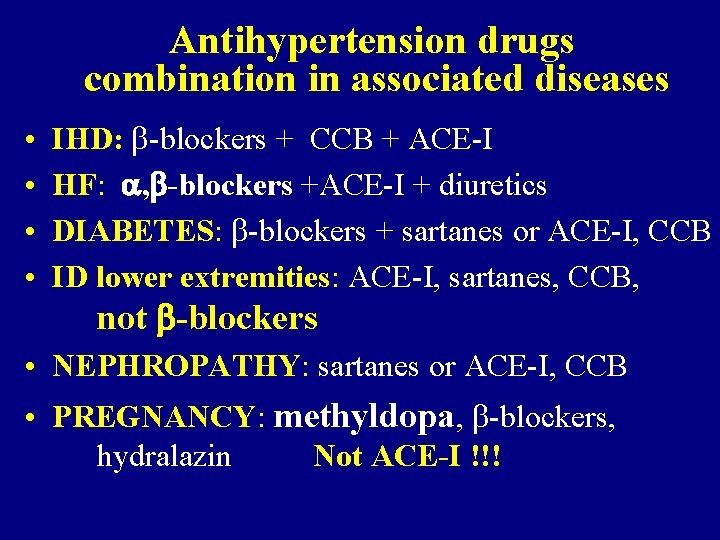
Antihypertension drugs combination in associated diseases • • IHD: -blockers + CCB + ACE-I HF: , -blockers +ACE-I + diuretics DIABETES: -blockers + sartanes or ACE-I, CCB ID lower extremities: ACE-I, sartanes, CCB, not -blockers • NEPHROPATHY: sartanes or ACE-I, CCB • PREGNANCY: methyldopa, -blockers, hydralazin Not ACE-I !!!
The main goal of therapy is to decrease BP. The choice of the antihypertension drug should be made acording to associated diseases, potential adverse effects and pharmacoeconomic aspects.

 Non pharmacological management of hypertension
Non pharmacological management of hypertension Hypertension
Hypertension Non pharmacological treatment for copd
Non pharmacological treatment for copd Hypertensive encephalopathy
Hypertensive encephalopathy Background
Background Urapidil rcp
Urapidil rcp Essential hypertension
Essential hypertension Chemical classification of crude drugs
Chemical classification of crude drugs Pharmacological and parenteral therapies
Pharmacological and parenteral therapies The pharmacological basis of therapeutics
The pharmacological basis of therapeutics The pharmacological basis of therapeutics
The pharmacological basis of therapeutics Pharmacological antagonist
Pharmacological antagonist The pharmacological basis of therapeutics
The pharmacological basis of therapeutics Essential non essential fatty acids
Essential non essential fatty acids Chief complaint present illness
Chief complaint present illness What is a good pico question
What is a good pico question Cataractectomy
Cataractectomy Conclusion of hypertension
Conclusion of hypertension Causes of secondary hypertension
Causes of secondary hypertension Classification of hypertension
Classification of hypertension Definition of hypertension
Definition of hypertension Hypertension
Hypertension Hypertension
Hypertension Hypertensive urgency
Hypertensive urgency Talipes equinovarus in varicose veins
Talipes equinovarus in varicose veins Pulmonary hypertension definition
Pulmonary hypertension definition Neonatal liver failure
Neonatal liver failure Portal hypertension signs
Portal hypertension signs Calcium channel blockers examples
Calcium channel blockers examples Tete de meduse hypertension portale
Tete de meduse hypertension portale Stages of pulmonary hypertension
Stages of pulmonary hypertension Disease state awareness
Disease state awareness Complication of liver cirrhosis
Complication of liver cirrhosis Conclusion of hypertension
Conclusion of hypertension What is the dash diet
What is the dash diet Nervous mechanism for regulation of blood pressure
Nervous mechanism for regulation of blood pressure Chronic liver stigmata
Chronic liver stigmata Hypertension
Hypertension Masked hypertension
Masked hypertension Dianne zwicke
Dianne zwicke Pneumotrieste
Pneumotrieste Equivalence hbpm
Equivalence hbpm Intracranial hypertension
Intracranial hypertension Conclusion of hypertension
Conclusion of hypertension Bmpr gene
Bmpr gene Left ventricular hypertrophy
Left ventricular hypertrophy Pulmonary hypertension
Pulmonary hypertension Esterman efficiency score driving
Esterman efficiency score driving Presinusoidal portal hypertension
Presinusoidal portal hypertension Modifiable risk factors for hypertension
Modifiable risk factors for hypertension Pachyméninges
Pachyméninges Health coaches for hypertension control
Health coaches for hypertension control Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension What is office blood pressure
What is office blood pressure Dr douglas simonetto
Dr douglas simonetto Hypertension vs hypotension
Hypertension vs hypotension Jnc 8 classification of hypertension pdf
Jnc 8 classification of hypertension pdf Definition of pulmonary hypertension
Definition of pulmonary hypertension Isolated systolic hypertension
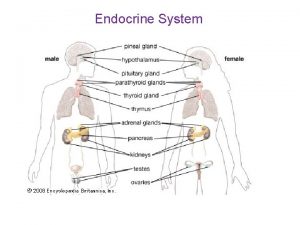
Isolated systolic hypertension Endorine
Endorine Nursing management of portal hypertension
Nursing management of portal hypertension Vital signs cpr
Vital signs cpr Hypertensive emergency
Hypertensive emergency Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Hypertension investigation chart
Hypertension investigation chart Gestational hypertension symptoms
Gestational hypertension symptoms Diueritique
Diueritique Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Classification of hypertension
Classification of hypertension Systemic vascular resistance
Systemic vascular resistance Sachin gupta md
Sachin gupta md Pah vs pulmonary hypertension
Pah vs pulmonary hypertension Rules of halves in hypertension
Rules of halves in hypertension Hypertensive crisis classification
Hypertensive crisis classification Amas faa
Amas faa Conclusion of hypertension
Conclusion of hypertension Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis Antihypertensive drugs
Antihypertensive drugs Jnc 7 hypertension
Jnc 7 hypertension Traitement hypertension
Traitement hypertension Hypertension
Hypertension Decerebrate posturing
Decerebrate posturing Foxglove use
Foxglove use Design treatment
Design treatment Ashbridges model
Ashbridges model Menorrhagia treatment
Menorrhagia treatment Paso 3
Paso 3 Asthma treatment
Asthma treatment Thymus
Thymus Iddt training
Iddt training Heat treatment calculations
Heat treatment calculations Suspension trauma treatment
Suspension trauma treatment