Acute severe asthma Acute severe asthma who is
- Slides: 20
Acute severe asthma
Acute severe asthma : who is at most risk ? l Previous life-threatening attacks l Severe disease (3 or >3 drugs for control; emergency steroid in past ; ever admitted in last 1 year) l Psychiatric morbidity l Non-compliance l Requiring 2 or > 2 Bronchodilator inhalers monthly
Near fatal episodes l l l l l Misuse of drugs/alcohol Psychiatric illness Denial Non compliance Learning difficulties Previous admission to ICU for asthma Brittle asthma Social isolation, income and employment difficulties Previous self discharge from hospital Br Med J 2005; 330585 -9
What is acute severe asthma ? ANYONE OF: l PEF 33 -50% best or predicted l RR 25/min l Heart rate 110/min l Inability to complete sentences in one breath
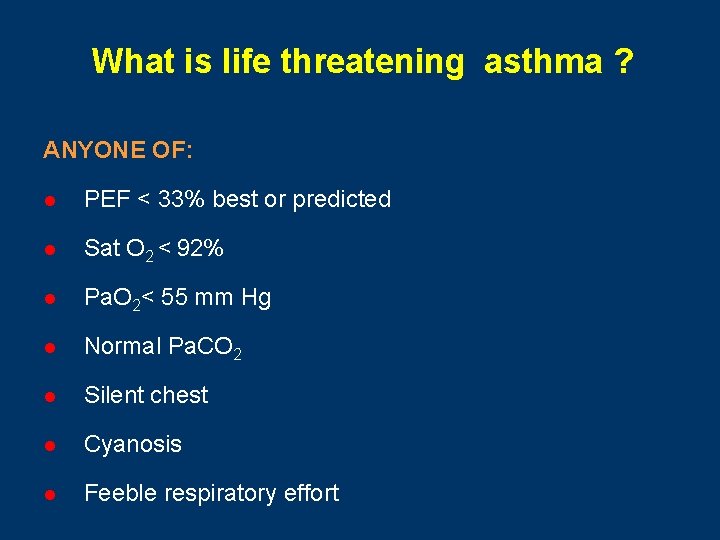
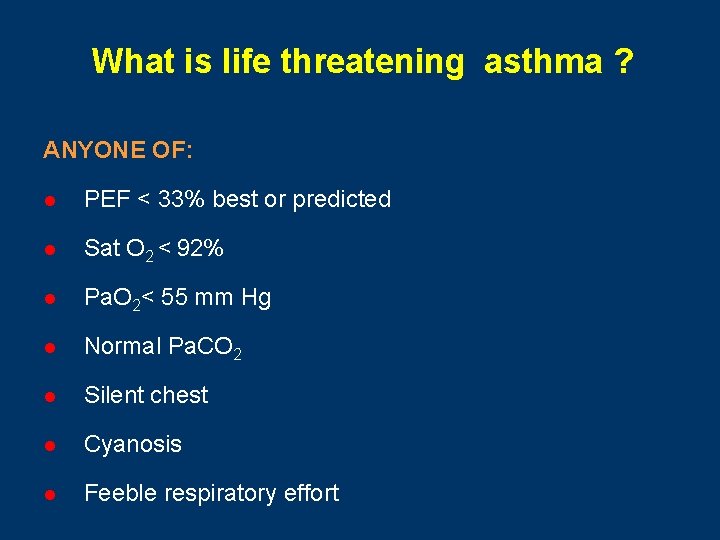
What is life threatening asthma ? ANYONE OF: l PEF < 33% best or predicted l Sat O 2 < 92% l Pa. O 2< 55 mm Hg l Normal Pa. CO 2 l Silent chest l Cyanosis l Feeble respiratory effort
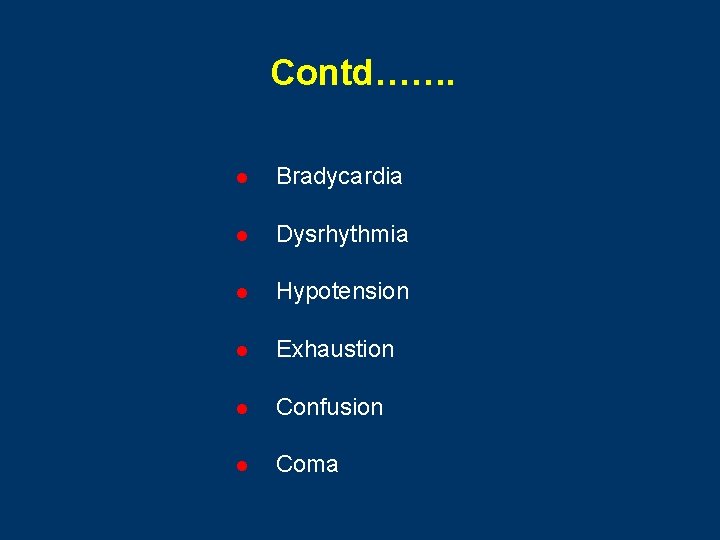
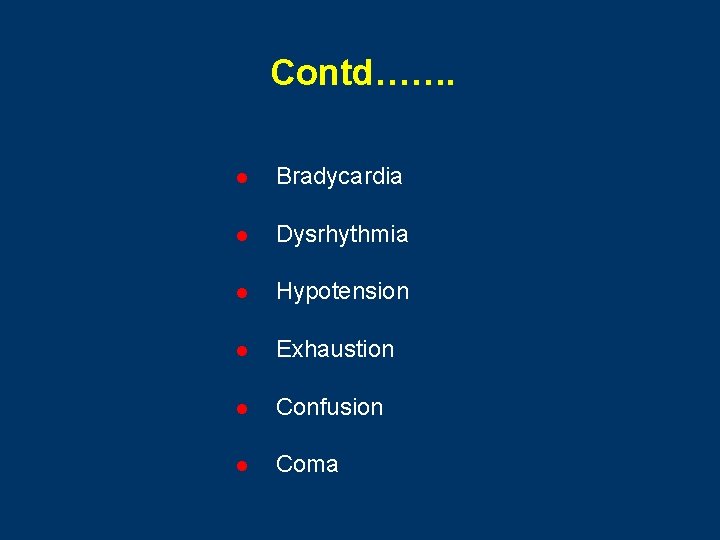
Contd……. l Bradycardia l Dysrhythmia l Hypotension l Exhaustion l Confusion l Coma
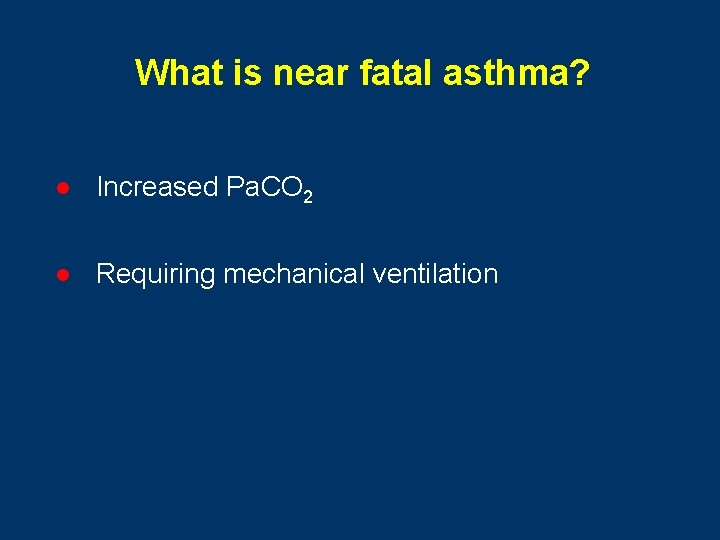
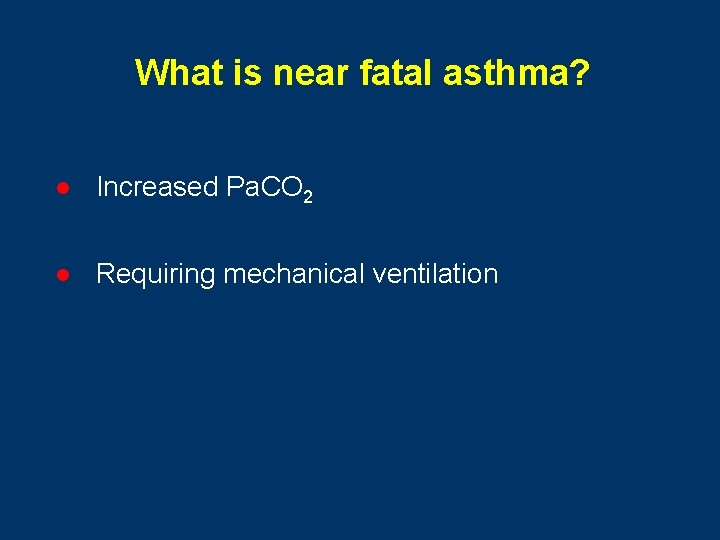
What is near fatal asthma? l Increased Pa. CO 2 l Requiring mechanical ventilation
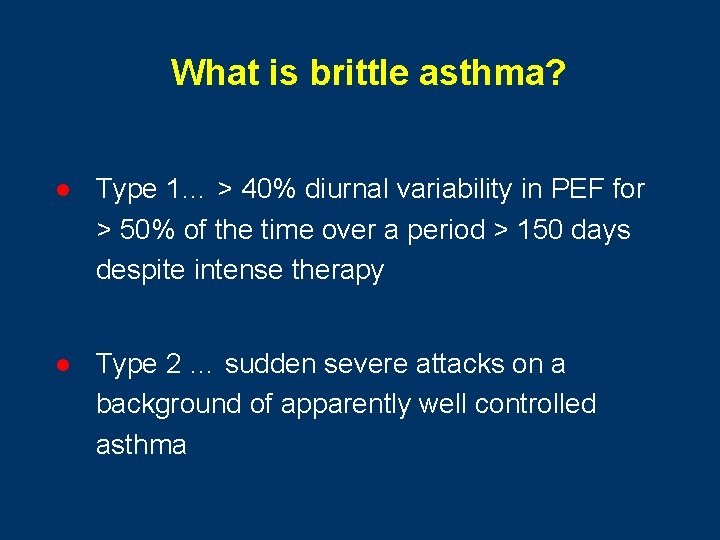
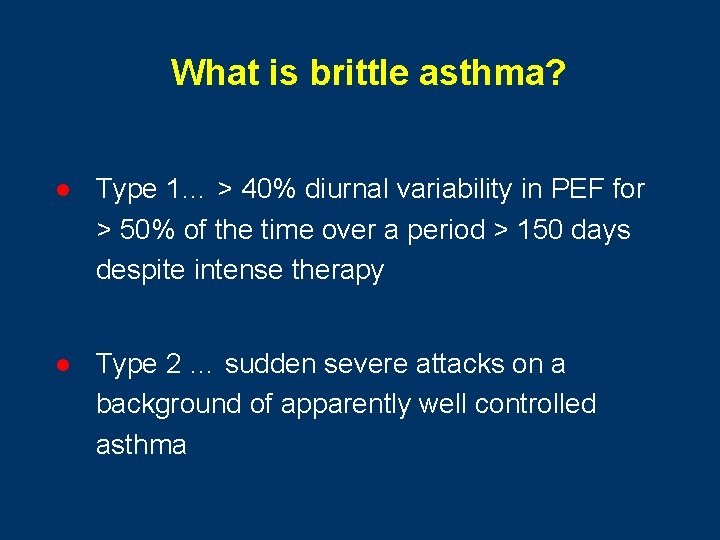
What is brittle asthma? l Type 1… > 40% diurnal variability in PEF for > 50% of the time over a period > 150 days despite intense therapy l Type 2 … sudden severe attacks on a background of apparently well controlled asthma
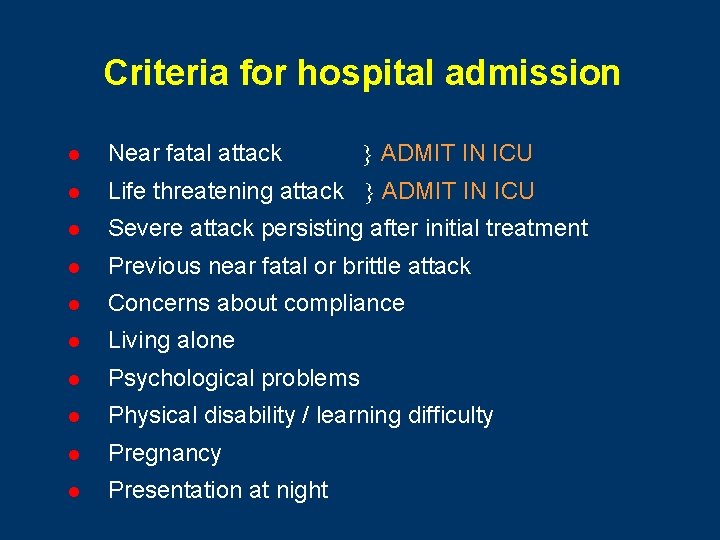
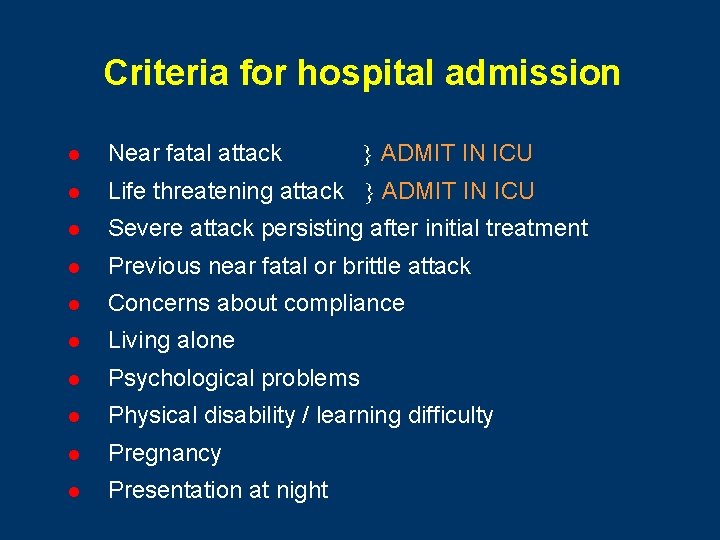
Criteria for hospital admission ADMIT IN ICU l Near fatal attack l Life threatening attack ADMIT IN ICU l Severe attack persisting after initial treatment l Previous near fatal or brittle attack l Concerns about compliance l Living alone l Psychological problems l Physical disability / learning difficulty l Pregnancy l Presentation at night
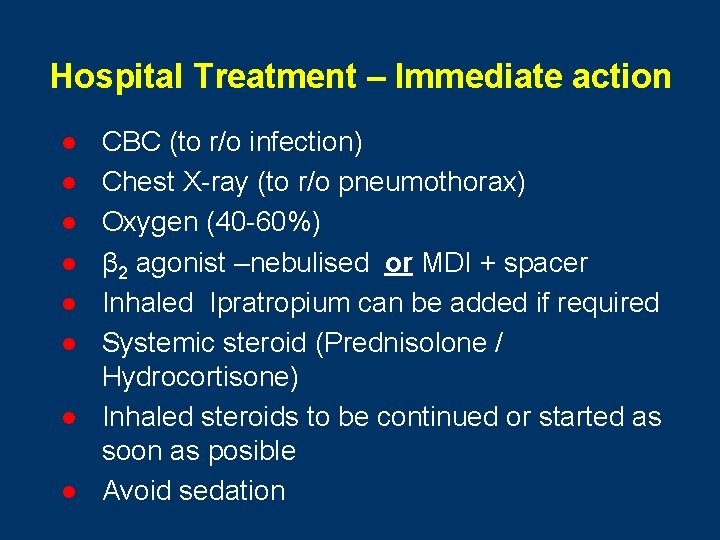
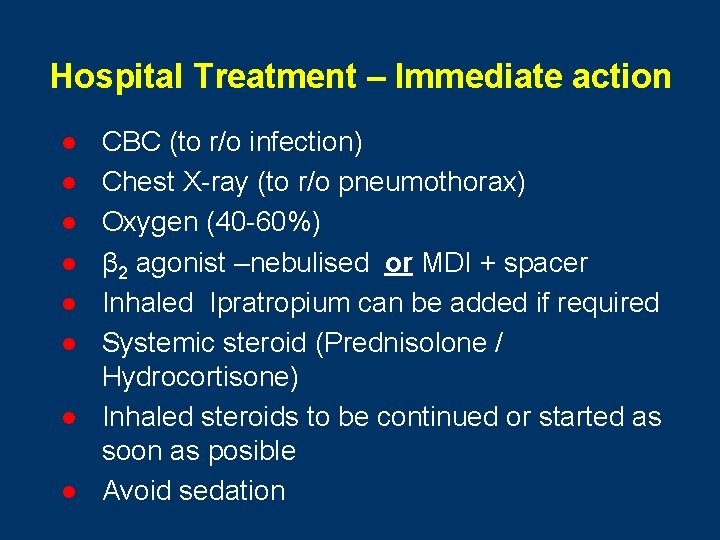
Hospital Treatment – Immediate action l l l l CBC (to r/o infection) Chest X-ray (to r/o pneumothorax) Oxygen (40 -60%) β 2 agonist –nebulised or MDI + spacer Inhaled Ipratropium can be added if required Systemic steroid (Prednisolone / Hydrocortisone) Inhaled steroids to be continued or started as soon as posible Avoid sedation
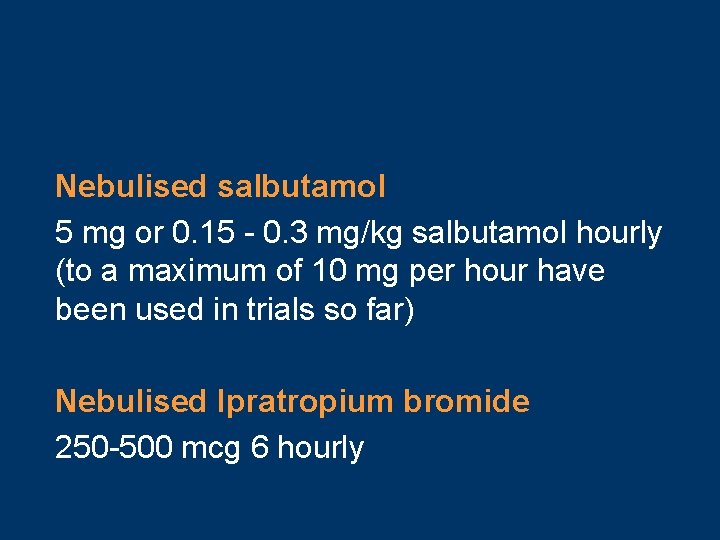
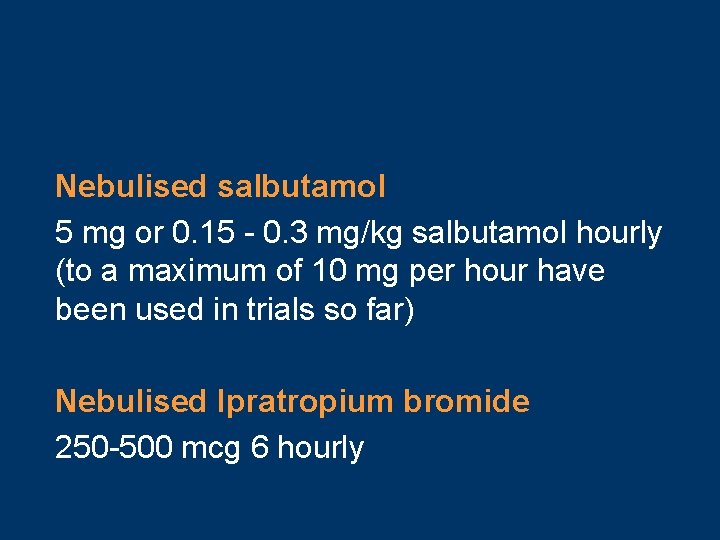
Nebulised salbutamol 5 mg or 0. 15 - 0. 3 mg/kg salbutamol hourly (to a maximum of 10 mg per hour have been used in trials so far) Nebulised Ipratropium bromide 250 -500 mcg 6 hourly
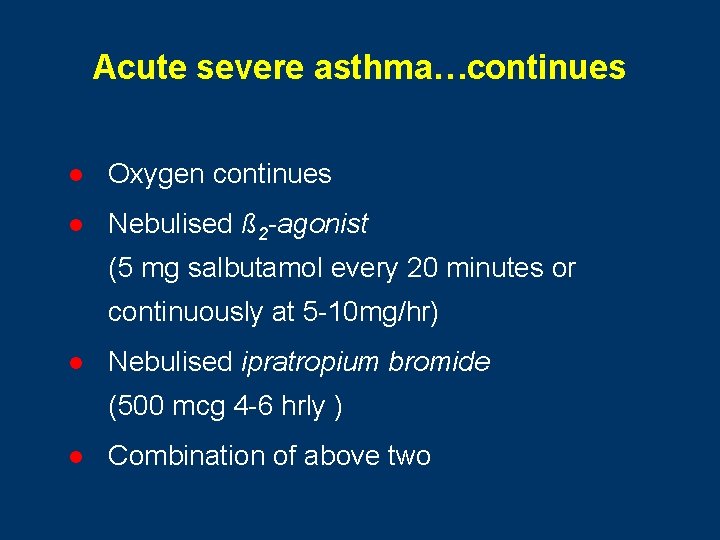
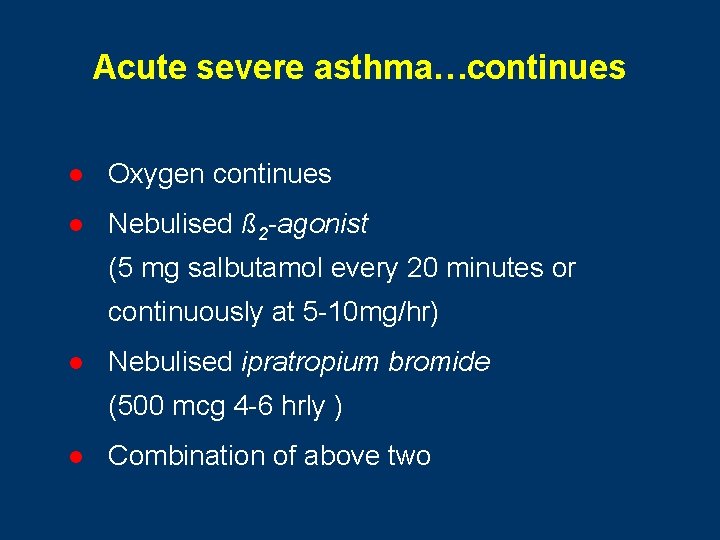
Acute severe asthma…continues l Oxygen continues l Nebulised ß 2 -agonist (5 mg salbutamol every 20 minutes or continuously at 5 -10 mg/hr) l Nebulised ipratropium bromide (500 mcg 4 -6 hrly ) l Combination of above two
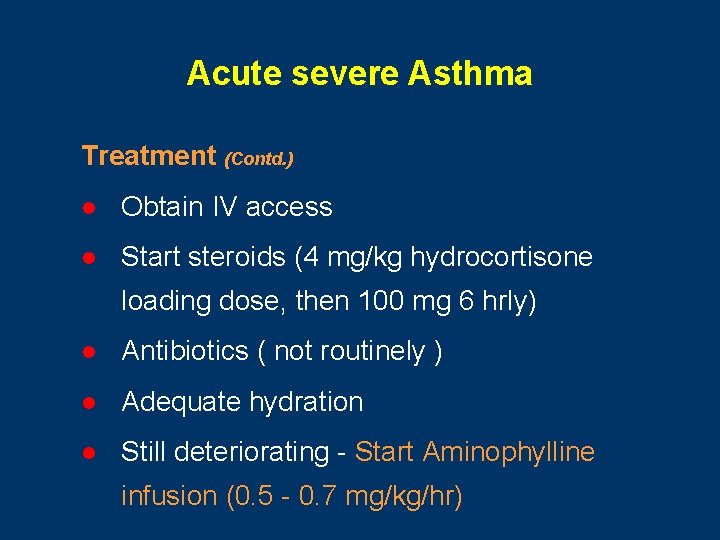
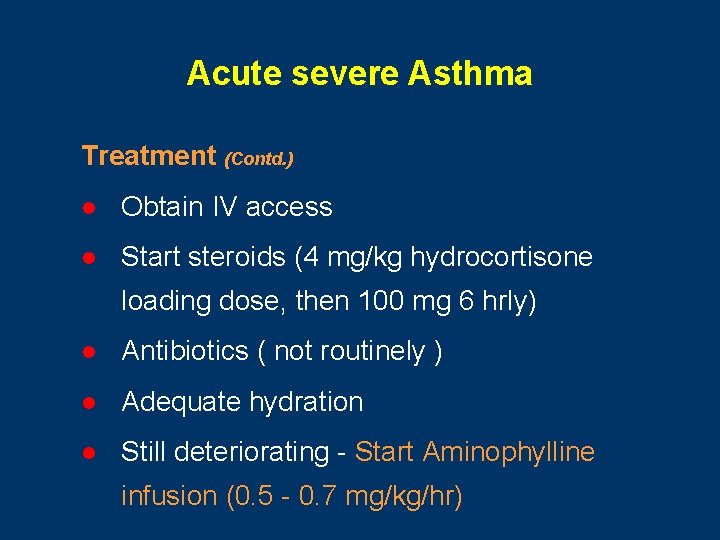
Acute severe Asthma Treatment (Contd. ) l Obtain IV access l Start steroids (4 mg/kg hydrocortisone loading dose, then 100 mg 6 hrly) l Antibiotics ( not routinely ) l Adequate hydration l Still deteriorating - Start Aminophylline infusion (0. 5 - 0. 7 mg/kg/hr)
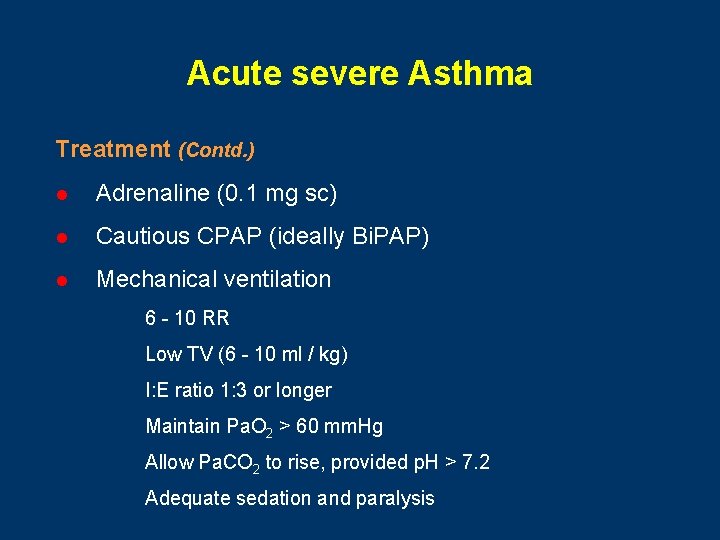
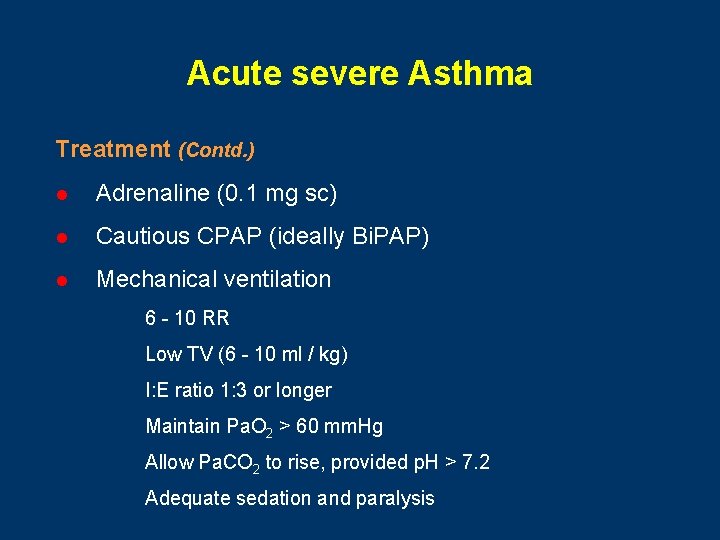
Acute severe Asthma Treatment (Contd. ) l Adrenaline (0. 1 mg sc) l Cautious CPAP (ideally Bi. PAP) l Mechanical ventilation – 6 - 10 RR – Low TV (6 - 10 ml / kg) – I: E ratio 1: 3 or longer – Maintain Pa. O 2 > 60 mm. Hg – Allow Pa. CO 2 to rise, provided p. H > 7. 2 – Adequate sedation and paralysis
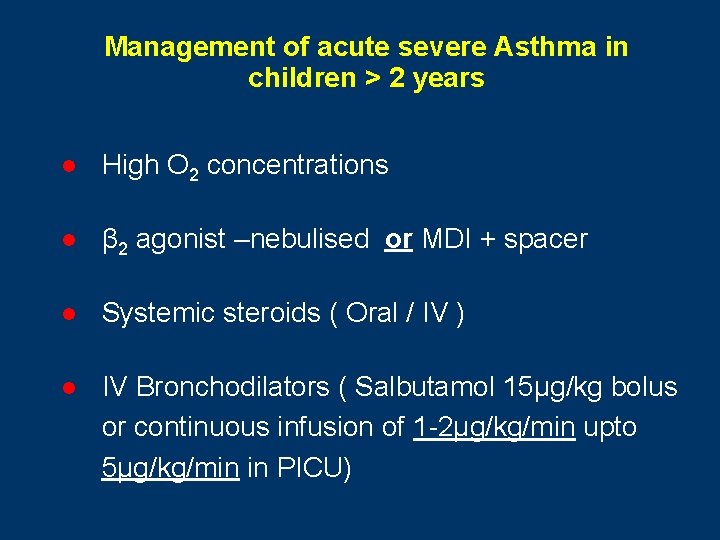
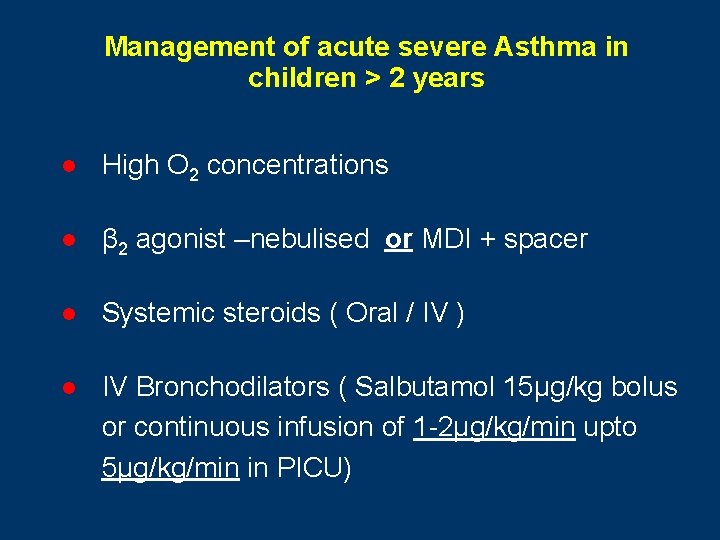
Management of acute severe Asthma in children > 2 years l High O 2 concentrations l β 2 agonist –nebulised or MDI + spacer l Systemic steroids ( Oral / IV ) l IV Bronchodilators ( Salbutamol 15μg/kg bolus or continuous infusion of 1 -2μg/kg/min upto 5μg/kg/min in PICU)
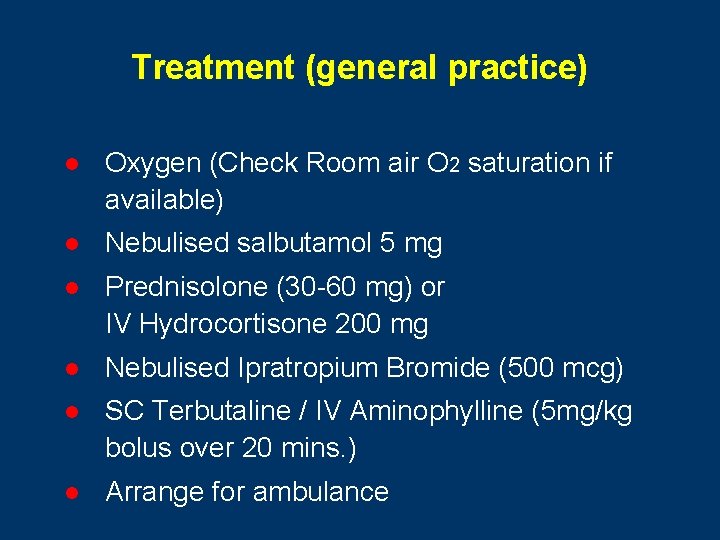
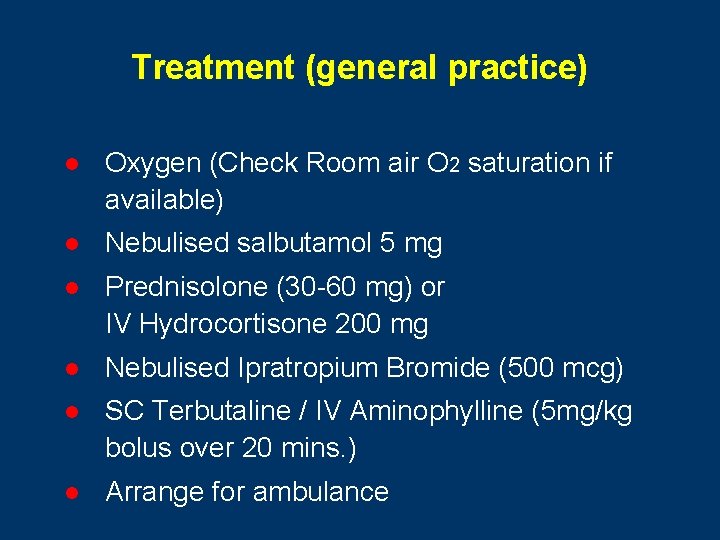
Treatment (general practice) l Oxygen (Check Room air O 2 saturation if available) l Nebulised salbutamol 5 mg l Prednisolone (30 -60 mg) or IV Hydrocortisone 200 mg l Nebulised Ipratropium Bromide (500 mcg) l SC Terbutaline / IV Aminophylline (5 mg/kg bolus over 20 mins. ) l Arrange for ambulance
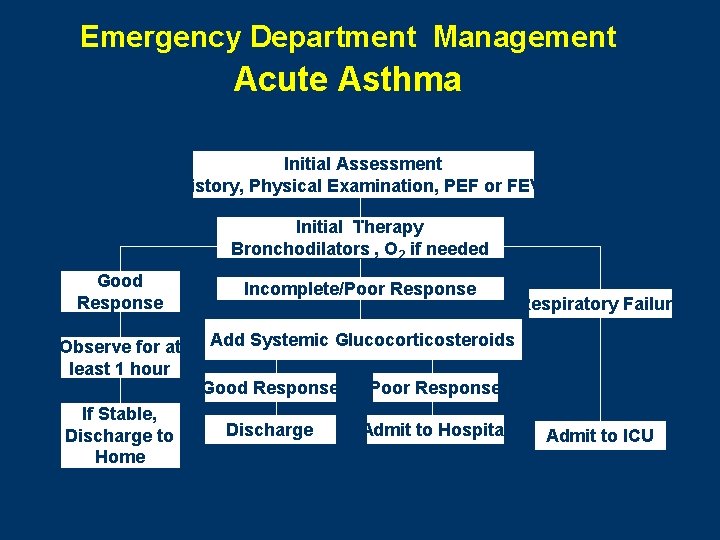
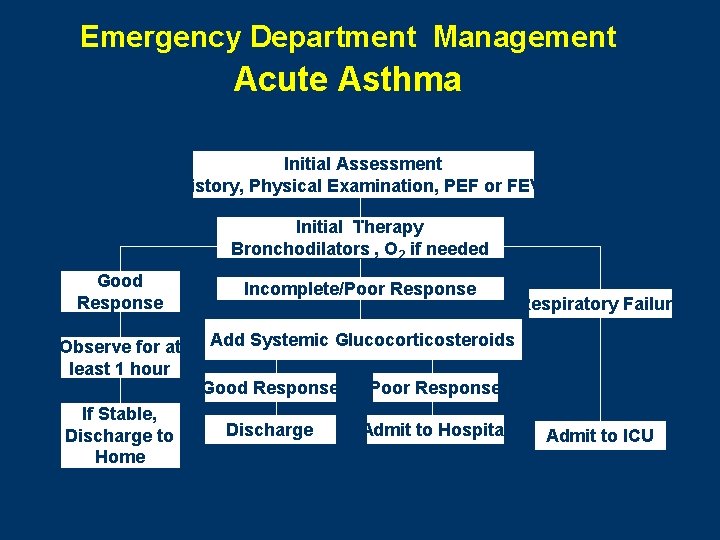
Emergency Department Management Acute Asthma Initial Assessment History, Physical Examination, PEF or FEV 1 Initial Therapy Bronchodilators , O 2 if needed Good Response Incomplete/Poor Response Observe for at least 1 hour Add Systemic Glucocorticosteroids If Stable, Discharge to Home Good Response Poor Response Discharge Admit to Hospital Respiratory Failure Admit to ICU
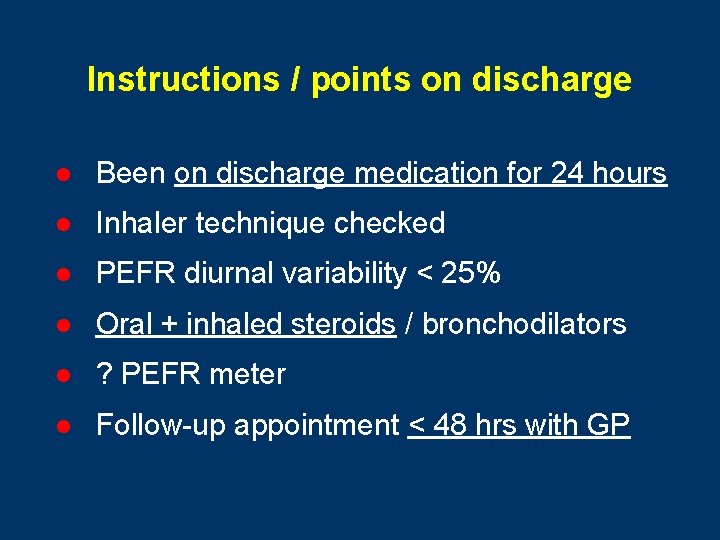
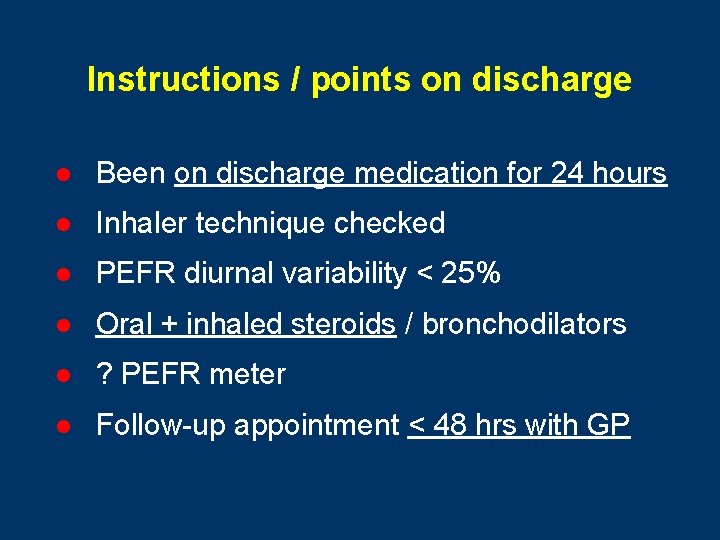
Instructions / points on discharge l Been on discharge medication for 24 hours l Inhaler technique checked l PEFR diurnal variability < 25% l Oral + inhaled steroids / bronchodilators l ? PEFR meter l Follow-up appointment < 48 hrs with GP
‘Treat acute severe asthma at least 4 days before it occurs’ Thomas Petty
PREVENT ACUTE ATTACKS OF ASTHMA BY TAKING REGULAR INHALED CORTICOSTEROID TREATMENT
 Unmet needs in severe asthma
Unmet needs in severe asthma Types of bronchial asthma
Types of bronchial asthma International severe asthma registry
International severe asthma registry Mild moderate severe asthma exacerbation
Mild moderate severe asthma exacerbation Severe asthma treatment
Severe asthma treatment Asthma clinical pathway
Asthma clinical pathway Pathology of asthma
Pathology of asthma Severe acute malnutrition case presentation
Severe acute malnutrition case presentation Adrogue madias formula
Adrogue madias formula Severe weather safety precautions worksheet
Severe weather safety precautions worksheet Potassium dose calculation
Potassium dose calculation Chapter 20 weather patterns and severe storms
Chapter 20 weather patterns and severe storms Swfdp
Swfdp Resomal composition
Resomal composition Chapter 16 section 1 water in the air answer key
Chapter 16 section 1 water in the air answer key Sds gasoline whmis 2015 answers
Sds gasoline whmis 2015 answers Bill nye severe weather
Bill nye severe weather Severe angle
Severe angle Domina severe
Domina severe Overflow diarrhea
Overflow diarrhea What cause metabolic acidosis
What cause metabolic acidosis